Abstract
Purpose
To describe a patient with orbital apocrine hidrocystoma presenting with ptosis and subsequent management.
Observations
A 43-year-old woman presented to the oculoplastic surgery clinic with a left-sided ptosis and enlarging but painless mass in the sulcus of the left upper eyelid. Magnetic resonance imaging demonstrated a large, circumscribed T2 bright cystic lesion in the extraconal space. Surgical excision and histopathology confirmed a diagnosis of apocrine hidrocystoma.
Conclusions
Although uncommon, ptosis may be a presenting symptom of an orbital apocrine hidrocystoma, which should be considered in the differential diagnosis for an extraconal cystic lesion. Apocrine hidrocystomas are benign tumors and are cured with surgical excision with rare recurrence.
Keywords: Apocrine hidrocystoma, Ptosis, Cystic orbital mass
1. Introduction
Apocrine hidrocystomas are benign tumors arising from apocrine sweat glands that are associated with hair follicles. Apocrine sweat glands are the predominant sweat glands of the head and neck region. In the eyelids, they are modified sweat glands located at the eyelid margin and are referred to as glands of Moll. The exact process leading to their growth is unknown. In the head and neck region, apocrine hidrocystomas most commonly occur intradermally at the eyelid margin or within the external auditory canal.1 Intraorbital apocrine hidrocystomas are especially rare in adults and of the few reported cases, may be associated with facial trauma.2, 3, 4 We report the case of a previously healthy woman with an orbital apocrine hidrocystoma in the setting of unilateral ptosis and enlarging orbital mass.
2. Case report
A 43-year-old woman presented with left-sided ptosis that had progressed over the prior two years. She noticed a gradually enlarging, nontender mass centrally located in the sulcus of the left upper eyelid. She denied any visual changes, discharge, or bleeding. She also denied prior orbital trauma or surgeries. Distance visual acuity with her current eyeglasses was 20/20 in the right eye and 20/40 in the left. Ocular motility was full, and pupils were equal, round, and reactive to light. External examination was notable for a firm, mobile, subcutaneous mass in the center of her left supratarsal fold with a few overlying feeder vessels but without erythema, warmth, scaling, or ulceration (Fig. 1). No lesions were observed on eyelid eversion. Margin-reflex distance (MRD1) on the left was 2.5 mm with good levator function. The remainder of her examination was normal. Magnetic resonance imaging (MRI) demonstrated an 18× 8 mm circumscribed T2/Short Tau Inversion Recovery (STIR) bright lesion with thin internal septations and trace delayed enhancement without bony erosion (Fig. 2).
Fig. 1.
External photograph demonstrating ptosis of left eyelid and arborizing feeder vessels overlying subcutaneous lesion (black arrow) in center of left supratarsal crease.
Fig. 2.
A, T1 weighted axial MRI demonstrating an 18 × 8 mm circumscribed lesion with internal septations and mild peripheral enhancement (white arrow) anterior to the left globe. B, T2 weighted STIR sequence axial MRI demonstrating same fluid-filled lesion with hyperintense signal. C, Coronal MRI demonstrating same T2/STIR bright lesion superior to the left globe.
An incision through the eyelid crease revealed a multilobed cystic-appearing lesion partly embedded within the superior tarsal muscle and involving the anterior orbital portion of the lacrimal gland. The cyst was first drained and then filled with fluorescein-stained fibrin glue. The glue was allowed to harden, and the cyst was completely excised as previously described.5,6 It was then submitted to pathology. Histopathology revealed an arborizing, cystic space lined by a double epithelium exhibiting apical snouting, consistent with an apocrine hidrocystoma (Fig. 3).
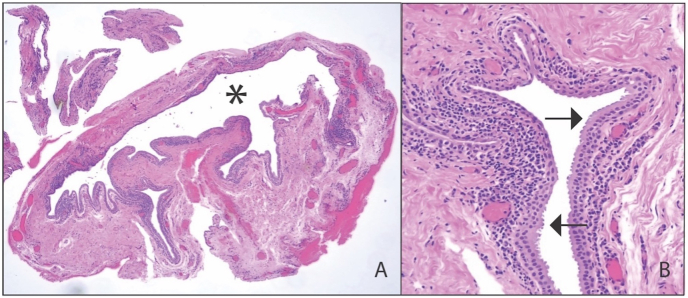
Fig. 3.
Photomicrograph of apocrine hidrocystoma A, at low power, demonstrating large, arborizing cystic lesion (asterisk); B, lined by a two-layer thick epithelium with characteristic apical snouting (arrows). Mild chronic inflammation is also present. (Hematoxylin-eosin stain at 2.5X (A) and 10X (B)).
On follow up examination at 1 month, the patient's MRD1 improved with no recurrence of the lesion (Fig. 4). The patient was reassured and advised to follow up for recurrence or new concerns.
Fig. 4.
External photograph at 4-month postoperative visit demonstrating mild residual ptosis of left eyelid with MRD1 of 4 mm.
3. Discussion
Apocrine hidrocystomas are benign cystic tumors that grow from apocrine sweat glands. Unlike eccrine hidrocystomas, apocrine hidrocystomas rarely occur as multiple lesions in the general adult population, usually presenting instead as a solitary lesion.7 However, multiple apocrine hidrocystomas have been associated with inherited conditions, including Schopf-Schulz-Passarge syndrome and Goltz-Gorlin syndrome.8 Since they arise from apocrine glands, extension beyond the eyelid margin is rare. It is hypothesized that trauma may introduce epithelial cells into the orbit, seeding their growth,3 but no history of trauma was present in our patient. Apocrine hidrocystomas usually range from 3 mm to 15 mm in diameter and remain asymptomatic. Larger lesions may cause ocular discomfort and pressure sensation. Mukherjee et al. reported a 3 cm hidrocystoma causing proptosis and mechanical ptosis secondary to mass effect.9 Ferraz et al. reported cases of ptosis resulting from occult hidrocystomas discovered only at the time of surgery arising within the levator muscle and adherent to the levator aponeurosis.10 There are many potential mechanisms for acquired ptosis.11 While our patient is approaching the appropriate age range for the development of aponeurotic ptosis, this would not be expected to resolve with only resection of the cyst and without additional manipulation of the levator or superior tarsal muscle. Similarly, neurogenic and myogenic causes of ptosis would not be expected to resolve without additional intervention. With regard to mechanical ptosis, our patient's mild degree of ptosis would be consistent with direct impingement of the superior tarsal muscle supported by intraoperative visualization of superior tarsal muscle infiltration with additional contribution from mass effect and weight of the lesion.
Additional imaging may be used to further characterize orbital masses and inform surgical approach. MRI of an apocrine hidrocystoma usually demonstrates a circumscribed, cystic mass with variable T1 signal and high T2 signal.12,13 STIR is a fat suppression technique used to enhance sensitivity to tissue fluid and may highlight the cystic contents.14 Unfortunately, an isointense T1 and hyperintense T2/STIR signal can also be seen in vascular lesions, such as a cavernous hemangioma,15 which was the original radiologic interpretation in this patient.
Because the clinical presentation of an apocrine hidrocystoma may resemble that of other orbital lesions, such as dermoid cysts, mucoceles, or hemangiomas, definitive diagnosis is made by histopathology. Apocrine hidrocystomas may be unilocular or multilocular cystic spaces and characteristically have a bilaminar epithelium composed of an inner cuboidal to columnar cell layer with eosinophilic cytoplasm and prominent apical snouts and an outer layer of more flattened cells.16 Chronic inflammation may also be seen in the interstitium.
Small, asymptomatic apocrine hidrocystomas may be observed, and treatment of symptomatic lesions is surgical excision, which almost always leads to complete resolution. Recurrence has been reported with incomplete excision of the cyst wall.17 Excision of the intact cyst may be complicated by cyst rupture, so fibrin glue mixed with fluorescein was utilized in this patient's surgery to fill the cyst cavity and facilitate delineation of margins for complete excision. This method has been previously described using fibrin glue mixed with other dyes, including indocyanine green, trypan blue, and methylene blue.5,6 Postoperative scarring may occur, so less invasive methods are currently under investigation. Del Pozo et al. described the use of carbon dioxide laser ablation to treat multiple small scattered hidrocystomas.18 Osaki et al. reported successful treatment of small hidrocystomas with hypertonic gluose sclerotherapy.19 For lesions as large as 15 mm, chemical cauterization with trichloroacetic acid proved effective.20
4. Conclusions
Although apocrine hidrocystomas are benign, they should remain on the differential for an extraconal cystic lesion, and concerning lesions should undergo surgical excision and biopsy to rule out other malignancies. Histopathology leads to definitive diagnosis, which demonstrates a characteristic apical snouting, and complete excision is the standard treatment.
Patient consent
Written informed general consent was obtained from the patient.
Funding
This work was supported in part by Yanoff Endowment Fund (VL).
Authorship
All authors attest that they meet ICMJE criteria for authorship.
Declaration of competing interest
The following authors have no financial disclosures: VH, VL, CAB.
Acknowledgments
We thank the patient for granting permission to publish this information.
References
- 1.Koumaki D., Papadakis M., Lagoudaki E., et al. Apocrine and eccrine hidrocystomas: a clinicopathological study. Acta Dermatovenerol Alp Pannonica Adriat. Jun 2021;30(2):53–56. [PubMed] [Google Scholar]
- 2.Rosen W.J., Li Y. Sudoriferous cyst of the orbit. Ophthalmic Plast Reconstr Surg. Jan 2001;17(1):73–75. doi: 10.1097/00002341-200101000-00014. [DOI] [PubMed] [Google Scholar]
- 3.Mehta A., Rao A., Khanna A. Sudoriferous cyst of the orbit of adult origin after trauma. Indian J Ophthalmol. May-Jun 2008;56(3):235–237. doi: 10.4103/0301-4738.40365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Valenzuela A.A., Heathcote J.G. Apocrine hidrocystoma of the orbit. Orbit. Dec 2011;30(6):316–317. doi: 10.3109/01676830.2011.621170. [DOI] [PubMed] [Google Scholar]
- 5.Boyle N.S., Chang E.L. Intraoperative use of indocyanine green and trypan blue mixed with fibrin glue in the excision of periocular cystic lesions. Am J Ophthalmol Case Rep. Dec 2020;20 doi: 10.1016/j.ajoc.2020.100990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pitak-Arnnop P., Subbalekha K., Sirintawat N., Auychai P., Klaisiri A., Neff A. Intraoperative injection of combined fibrin sealant and methylene blue dye for surgery of branchial cleft cysts: a case report. J Stomatol Oral Maxillofac Surg. Sep. 2019;120(4):378–382. doi: 10.1016/j.jormas.2019.02.013. [DOI] [PubMed] [Google Scholar]
- 7.Langer K., Konrad K., Smolle J. Multiple apocrine hidrocystomas on the eyelids. Am J Dermatopathol. Dec 1989;11(6):570–573. doi: 10.1097/00000372-198912000-00011. [DOI] [PubMed] [Google Scholar]
- 8.Vani D., T Rd, H Bs, M B, Kumar H.R., Ravikumar V. Multiple apocrine hidrocystomas: a case report. J Clin Diagn Res. Jan 2013;7(1):171–172. doi: 10.7860/JCDR/2012/4879.2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mukherjee B., Desai A., Krishnakumar S., Biswas J. A giant apocrine hidrocystoma presenting as lacrimal gland mass. Orbit. 2015;34(6):342–344. doi: 10.3109/01676830.2015.1078367. [DOI] [PubMed] [Google Scholar]
- 10.Ferraz L.B., Burroughs J.R., Satto L.H., et al. Three adult cases of orbital hidrocystoma presenting with blepharoptosis. J Clin Med. Jan 13 2015;4(1):150–158. doi: 10.3390/jcm4010150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bacharach J., Lee W.W., Harrison A.R., Freddo T.F. A review of acquired blepharoptosis: prevalence, diagnosis, and current treatment options. Eye (Lond) Sep 2021;35(9):2468–2481. doi: 10.1038/s41433-021-01547-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kharrat I., Achour I., Thabet W., et al. Apocrine hidrocystoma of the parotid gland. Ear Nose Throat J. Jul 5 2021 doi: 10.1177/01455613211031028. [DOI] [PubMed] [Google Scholar]
- 13.Tachibana T., Sasaki T., Wani Y., et al. Apocrine hidrocystoma of the external auditory canal in a child. Otol Neurotol. Sep 1 2021;42(8):e1181–e1183. doi: 10.1097/MAO.0000000000003220. [DOI] [PubMed] [Google Scholar]
- 14.Laitt R.D., Hoh B., Wakeley C., et al. The value of the short tau inversion recovery sequence in magnetic resonance imaging of thyroid eye disease. Br J Radiol. Mar 1994;67(795):244–247. doi: 10.1259/0007-1285-67-795-244. [DOI] [PubMed] [Google Scholar]
- 15.Khan S.N., Sepahdari A.R. Orbital masses: CT and MRI of common vascular lesions, benign tumors, and malignancies. Saudi J Ophthalmol. Oct 2012;26(4):373–383. doi: 10.1016/j.sjopt.2012.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jakobiec F.A., Zakka F.R. A reappraisal of eyelid eccrine and apocrine hidrocystomas: microanatomic and immunohistochemical studies of 40 lesions. Am J Ophthalmol. Feb 2011;151(2):358–374 e2. doi: 10.1016/j.ajo.2010.08.028. [DOI] [PubMed] [Google Scholar]
- 17.Ssi-Yan-Kai I.C., Pearson A.R. Recurrent giant orbital apocrine hidrocystoma. Eye (Lond) Jun 2012;26(6):895–896. doi: 10.1038/eye.2012.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.del Pozo J., Garcia-Silva J., Pena-Penabad C., Fonseca E. Multiple apocrine hidrocystomas: treatment with carbon dioxide laser vaporization. J Dermatolog Treat. Jun 2001;12(2):97–100. doi: 10.1080/095466301317085381. [DOI] [PubMed] [Google Scholar]
- 19.Osaki T.H., Osaki M.H., Osaki T., Viana G.A. A minimally invasive approach for apocrine hidrocystomas of the eyelid. Dermatol Surg. Jan 2016;42(1):134–136. doi: 10.1097/DSS.0000000000000567. [DOI] [PubMed] [Google Scholar]
- 20.Dailey R.A., Saulny S.M., Tower R.N. Treatment of multiple apocrine hidrocystomas with trichloroacetic acid. Ophthalmic Plast Reconstr Surg. Mar 2005;21(2):148–150. doi: 10.1097/01.iop.0000155509.54813.93. [DOI] [PubMed] [Google Scholar]