Abstract
Anisakiasis is a parasitic disease caused by Anisakis simplex and has become an emerging zoonosis as preferences for eating raw or undercooked seafood have become more common. Few case reports of asymptomatic anisakiasis have been published to date. A 79-year-old asymptomatic man underwent esophagogastroduodenoscopy (EGD) for gastric cancer screening. The gastroenterologist diagnosed superficial gastritis without any malignant lesions but found an Anisakis larva while reviewing EGD images. The physician performed a second EGD and removed the larva. The patient reported that he ate the flatfish sashimi for dinner on the day before the first EGD. This case indicates the existence of asymptomatic gastric anisakiasis, indicating that anisakiasis incidence may have previously been underestimated.
Keywords: Anisakiasis, Parasite infections, Esophagogastroduodenoscopy, Cancer screening, Raw fish eating habit, Case report
Highlights
-
•
Anisakiasis is an emerging zoonosis due to eating undercooked marine products.
-
•
Gastric anisakiasis often causes severe epigastric pain and allergic reactions.
-
•
Few case reports on gastric anisakiasis have identified an asymptomatic form.
-
•
Our case indicates the potential for underdiagnosis of anisakiasis.
-
•
Anchor bias overlooking anisakiasis may occur during gastric cancer screening.
Introduction
Anisakiasis is a parasitic disease caused by nematodes of the species Anisakis simplex that infect the body after the consumption of raw or undercooked seafood. Anisakiasis can be divided into three categories: gastric, intestinal, and ectopic anisakiasis; among these, gastric anisakiasis is the most prevalent [1], [2]. The most common symptom of gastric anisakiasis is severe epigastric pain within hours of ingestion of Anisakis nematodes. Subsequently, nausea and vomiting with allergic reactions such as urticaria occur. Gastric anisakiasis can be diagnosed by esophagogastroduodenoscopy (EGD), which reveals the presence of Anisakis nematodes in the stomach [1]. Anisakiasis has become an emerging zoonosis as preferences for eating raw or lightly cooked seafood have increased [3].
Clinical management of anisakiasis is the surgical removal of the larva by endoscopy or surgery if the larva is localized in a lesion where the endoscopic removal is not applied, such as the small intestine or omentum [4]. It is reasonable because the definite diagnosis of anisakiasis is made by endoscopic or pathological observation. The anti-parasitic medication with albendazole is a treatment option; however, it is rare to be applied in our clinical practice [5].
Here, we present a case of incidental detection of asymptomatic gastric anisakiasis during EGD for routine health examination in a Japanese community with habits of eating raw fish. Our case suggests the existence of asymptomatic cases of anisakiasis.
Case report
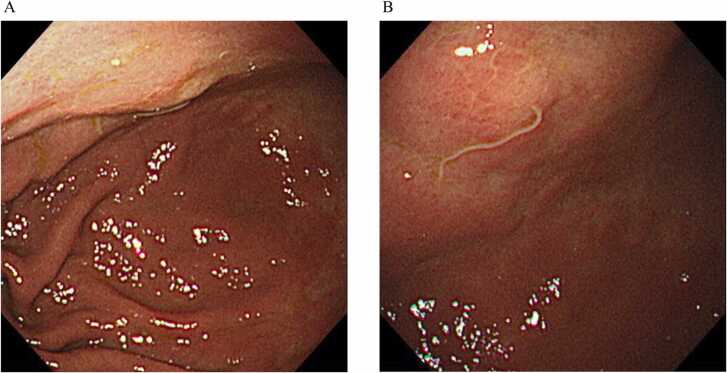
An asymptomatic 79-year-old man underwent EGD for gastric cancer screening in a community medical institute (Some Central Hospital, Soma, Fukushima, Japan). The examination was performed as part of a health checkup program run by the local government. The patient had no specific history of the present illness. The patient denied any history of anisakiasis. The patient had a history of successful eradication of Helicobacter pylori at the age of 74 years. The patient also had a history of colorectal polypectomy. He was diagnosed with hypertension; however, he was not taking any prescribed medication at the time of examination. The patient had no relevant family histories. On arrival, his vital sign was normal. Urticaria was also not observed. Laboratory results were within the normal range. A gastroenterologist performed EGD at 10:00 a.m. and diagnosed superficial gastritis, which did not require treatment. The patient went home after EGD. The physician then asked the patient to return to the hospital because an Anisakis larva was recognized on the anterior wall of the gastric antrum in EGD images. At 11:00 a.m., the physician performed a second EGD. No erythematous lesions were observed around the Anisakis bite area on the anterior wall of the gastric horn (Fig. 1). The diagnosis of gastric anisakiasis was made by the EGD. The gastroenterologist removed an Anisakis larva during the second EGD. The physician interviewed the patient after the second EGD. The interview revealed that he ate flatfish sashimi around 5:00 p.m. on the day before the examination. He obtained the raw flatfish from his friend in a non-commercial exchange. The patient did not show recurrence of gastric anisakiasis for up to 1 year after EGD.
Fig. 1.
Esophagogastroduodenoscopy images of the anterior wall of the gastric antrum are shown (wide [A] and closed [B] views). An Anisakis larva is seen on the anterior wall of the gastric antrum during the first endoscopy.
Discussion
We present a case in which an Anisakis larva was incidentally identified in the stomach during EGD performed as a routine health examination for gastric cancer screening. This case indicates the existence of asymptomatic gastric anisakiasis and suggests that gastric anisakiasis can be underdiagnosed. Only a single report on asymptomatic gastric anisakiasis was found, in which the larvae of Anisakis were simultaneously identified in the stomach and colon by EGD and colonoscopy, respectively[6].
Endoscopic detection of Anisakis nematodes may not occur if the endoscopist does not suspect anisakiasis in asymptomatic patients. In our case, the endoscopist did not identify the Anisakis larva during the initial EGD observation because the allergic reaction around the larva in the stomach mucosa was mild. The small size of the larva (2–3 cm in length) could contribute to the failure of immediate endoscopic identification. Another reason could be an anchoring bias since the endoscopist was focused on detecting malignant lesions during gastric cancer screening[6]. Multiple conditions were therefore involved in the error of the initial EGD. Even skilled endoscopists may not observe Anisakis nematodes if they do not consider it as a differential finding. Only three cases of asymptomatic anisakiasis were found by chance among 1496 gastric cancer screenings between April 2008 to July 2012 in our institution; however, we might overlook the anisakiasis in the past.
In the present case, the patient consumed raw fish following a non-commercial exchange. Visual inspection for Anisakis is regularly performed before commercial distribution; however, no inspection is commonly performed in private exchanges[3]. Physicians should consider anisakiasis as a differential diagnosis in communities with habits of consuming raw or undercooked fish. Our institute is located in Soma, Fukushima Prefecture, which is the leading fishing area in Japan. Residents habitually eat raw fish that is not commercially distributed. Our institute has identified 26 patients with Anisakis larvae among 47 suspected cases in the last five years. The number of reports of anisakiasis is increasing worldwide, along with the consumption of raw fish[7], [8], [9]. Reassessment of the incidence of anisakiasis is necessary to understand its epidemiology. Serologic evaluation of anisakiasis may be helpful, although the sensitivity and specificity of such evaluations are limited[10], [11], [12].
The endoscopist removed the larva in the present case because of possible sequelae. However, long-term complications of anisakiasis are not fully understood. Hemorrhagic gastric ulcers due to chronic gastric anisakiasis and anisakiasis-induced eosinophilic esophagitis were reported[13], [14]. A possible association with malignant gastrointestinal diseases was suggested albeit a definite relationship with cancer development remains unclear[15], [16]. Long-term follow-up is warranted to elucidate any chronic influences.
Conclusion
Anisakiasis is an emerging parasitic disease, as the habit of eating raw or undercooked fish is growing globally. We encountered a patient with asymptomatic gastric anisakiasis diagnosed incidentally during EGD for cancer screening. The endoscopist failed to identify the larva during the initial EGD, but detected it while reviewing the EGD images. Anisakis nematode was then removed during the second EGD. This case suggests underdiagnosis of anisakiasis. The long-term effects of anisakiasis remain unknown; thus, a follow-up study on anisakiasis is warranted.
Ethical approval
Not applicable.
Funding support
This study is supported in part by a grant of the collaborative studies for radiation disasters and medical science in the Fukushima Medical University (Fukushima, Japan), the internal fund of the Soma Central Hospital (Soma, Fukushima, Japan), and the Medical Governance Research Institute (Minato-ward, Tokyo, Japan). The study sponsors had no involvement in any study procedures, including data collection, analysis, and interpretation.
CRediT authorship contribution statement
Fumiue Harada: Conceptualization, Data collection, Writing – original draft, Writing – review & editing. Kana Yamamoto: Writing – original draft, Writing – review & editing. Akio Takeuchi: Data collection, Writing – review & editing. Hiroshi Uenishi: Data collection, Writing – review & editing. Yosuke Tachiya: Data collection, Writing – review & editing. Chika Yamamoto: Writing – review & editing. Yuta Tani: Writing – review & editing. Mutsuko Ohnishi: Writing – review & editing. Morihito Takita: Writing – original draft, Writing – review & editing. Tetsuya Tanimoto: Writing – review & editing. Masahiro Kami: Writing – review & editing. Ryusaburo Shineha: Supervision.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Conflict of interest statement
The authors report there are no competing interests to declare.
Acknowledgments
We would like to thank the medical and administrative staff in the Endoscopy Division of Soma Central Hospital (Fukushima, Japan) for their professional support.
References
- 1.Audicana M.T., Kennedy M.W. Anisakis simplex: from obscure infectious worm to inducer of immune hypersensitivity. Clin Microbiol Rev. 2008;21(2):360–379. doi: 10.1128/CMR.00012-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rama T.A., Silva D. Anisakis allergy: raising awareness. Acta Med Port. 2021 doi: 10.20344/amp.15908. Epub 20211027. [DOI] [PubMed] [Google Scholar]
- 3.Bao M., Pierce G.J., Pascual S., Gonzalez-Munoz M., Mattiucci S., Mladineo I., et al. Assessing the risk of an emerging zoonosis of worldwide concern: anisakiasis Sci Rep. 2017;7:43699. doi: 10.1038/srep43699. . Epub 20170313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Repiso Ortega A., Alcantara Torres M., Gonzalez de Frutos C., de Artaza Varasa T., Rodriguez Merlo R., Valle Munoz J., et al. [Gastrointestinal anisakiasis. Study of a series of 25 patients] Gastroenterol Hepatol. 2003;26(6):341–346. doi: 10.1016/s0210-5705(03)70370-7. [DOI] [PubMed] [Google Scholar]
- 5.Moore D.A., Girdwood R.W., Chiodini P.L. Treatment of anisakiasis with albendazole. Lancet. 2002;360(9326):54. doi: 10.1016/s0140-6736(02)09333-9. [DOI] [PubMed] [Google Scholar]
- 6.Nakaji K., Kumamoto M., Wada Y., Nakae Y. Asymptomatic Gastric and Colonic Anisakiasis Detected Simultaneously Intern Med. 2019;58(15):2263–2264. doi: 10.2169/internalmedicine.2657-19. . Epub 20190417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Caldeira A.J.R., Pereira Alves C.P., Santos M.J. Anisakis notification in fish: An assessment of the cases reported in the European Union rapid alert system for food and feed (RASFF) database. Food Control. 2021;124 doi: 10.1016/j.foodcont.2021.107913. [DOI] [Google Scholar]
- 8.Santos M.J., Matos M., Guardone L., Golden O., Armani A., Caldeira A.J.R., et al. Preliminary Data on the Occurrence of Anisakis spp. in European Hake (Merluccius merluccius) Caught Off the Portuguese Coast and on Reports of Human Anisakiosis in Portugal Microorganisms. 2022;10(2) doi: 10.3390/microorganisms10020331. . Epub 20220201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Suzuki J., Murata R., Kodo Y. Current Status of Anisakiasis and Anisakis Larvae in Tokyo, Japan. Food Saf (Tokyo) 2021;9(4):89–100. doi: 10.14252/foodsafetyfscj.D-21-00004. Epub 20211207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Daschner A., Cuellar C., Rodero M. The Anisakis allergy debate: does an evolutionary approach help? Trends Parasitol. 2012;28(1):9–15. doi: 10.1016/j.pt.2011.10.001. Epub 20111111. [DOI] [PubMed] [Google Scholar]
- 11.Ventura M.T., Rodriguez-Perez R., Caballero M.L., Garcia-Alonso M., Antonicelli L., Asero R. IgE, IgG1 and IgG4 response to specific allergens in sensitized subjects showing different clinical reactivity to Anisakis simplex. Eur Ann Allergy Clin Immunol. 2017;49(2):52–58. PubMed PMID: 28294584. [PubMed] [Google Scholar]
- 12.Heffler E., Sberna M.E., Sichili S., Intravaia R., Nicolosi G., Porto M., et al. High prevalence of Anisakis simplex hypersensitivity and allergy in Sicily, Italy. Ann Allergy Asthma Immunol. 2016;116(2):146–150. doi: 10.1016/j.anai.2015.12.014. . PubMed PMID: 26815707. [DOI] [PubMed] [Google Scholar]
- 13.Kang D.B., Park W.C., Lee J.K. Chronic gastric anisakiasis provoking a bleeding gastric ulcer. Ann Surg Treat Res. 2014;86(5):270–273. doi: 10.4174/astr.2014.86.5.270. Epub 20140424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Decruyenaere P., Van de Maele B., Hulstaert E., Van Vlierberghe H., Decruyenaere J., Lapeere H. IgE-mediated gastroallergic anisakiasis with eosinophilic oesophagitis: a case report Acta Clin Belg. 2022;77(2):396–399. doi: 10.1080/17843286.2020.1822627. . Epub 20200924. [DOI] [PubMed] [Google Scholar]
- 15.Garcia-Perez J.C., Rodriguez-Perez R., Ballestero A., Zuloaga J., Fernandez-Puntero B., Arias-Diaz J., et al. Previous Exposure to the Fish Parasite Anisakis as a Potential Risk Factor for Gastric or Colon Adenocarcinoma. Med (Baltim) 2015;94(40) doi: 10.1097/MD.0000000000001699. PubMed PMID: 26448021; PubMed Central PMCID: PMCPMC4616760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mineta S., Shimanuki K., Sugiura A., Tsuchiya Y., Kaneko M., Sugiyama Y., et al. Chronic anisakiasis of the ascending colon associated with carcinoma. J Nippon Med Sch. 2006;73(3):169–174. doi: 10.1272/jnms.73.169. . PubMed PMID: 16790986. [DOI] [PubMed] [Google Scholar]