Abstract
Background
Anaplastic meningioma is very rare and is generally known to have a poor prognosis. However, due to its rarity, the relationship between clinical prognosis and prognostic factors is not clear. We analyzed the prognostic factors influencing survival outcomes of patients with anaplastic meningioma. Moreover, we analyzed on the progression pattern and the response to treatment about anaplastic meningioma.
Methods
Retrospective review of 48 patients with diagnosis of World Health Organization (WHO) grade 3 meningioma was performed. According to diagnosis type, primary anaplastic meningioma was included in 28 cases and secondary anaplastic meningioma in 20 cases. Gross total resection was performed in 36 patients (75.0%), and 32 patients (66.7%) received adjuvant radiotherapy after tumor resection with confirmed WHO grade 3 meningioma. Kaplan-Meier survival curve and Cox proportional hazards modeling were used for outcome analysis.
Results
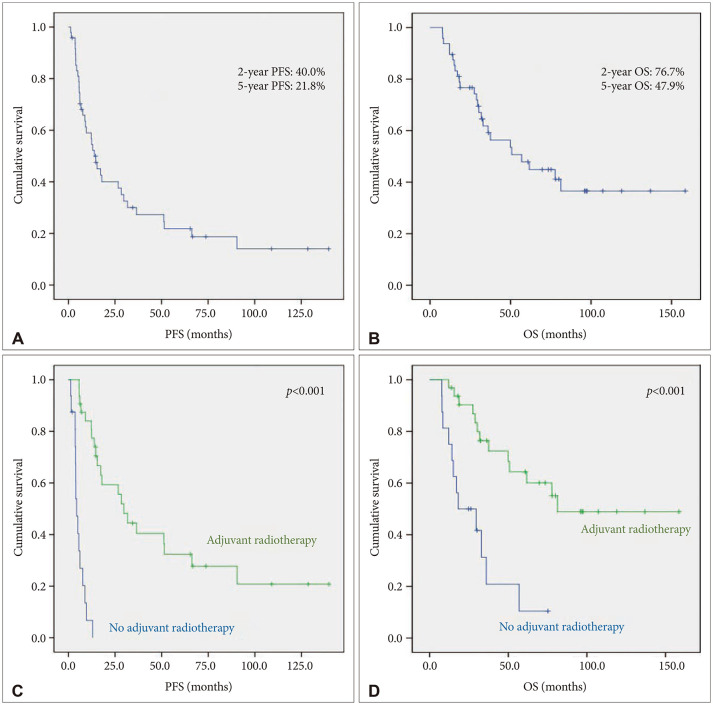
The median progression-free survival (PFS) and overall survival (OS) were 13.9 months (95% confidence interval [CI], 8.8 to 19.1) and 56.9 months (95% CI, 24.1 to 89.7), respectively. Adjuvant radiotherapy was a robust prognostic factor for PFS and OS. Extent of resection and diagnosis type which appeared to be significant prognostic factors in univariate analysis were failed to prove statistical significance in multivariate analysis.
Conclusion
Adjuvant radiotherapy is an essential treatment arm in patients with anaplastic meningiomas. Stereotactic radiosurgery seems to play an important role as a salvage treatment. But chemotherapy seems to have limited efficacy. Because of the disseminated nature of the disease, further investigations to improve survival outcome are needed.
Keywords: Anaplastic meningioma, Surgery, Adjuvant radiotherapy, Prognosis, Progression
INTRODUCTION
Meningiomas are the most common primary intracranial tumors in adults, accounting for about 36% [1]. Most meningiomas are benign, and have favorable outcomes with treatment using “wait and scan” or “stereotactic radiosurgery,” or “surgical resection” [2]. Anaplastic meningioma (World Health Organization [WHO] grade 3) consists of 1%–2% of all meningiomas and presents a particularly aggressive clinical course and a poor survival outcome [2,3,4,5,6,7]. In United States, population based study showed 5-year survival rate of patients with anaplastic meningiomas was 41.4% and factors associated with increased risk of death were older age, high comorbidity score, and subtotal resection [1]. According to the study from Korea Central Cancer Registry, in patients with anaplastic meningioma, 1-year, 2-year, and 5-year relative survival rates were 89.2%, 79.4%, and 68.9%, respectively [8].
The prognostic factors in patients with anaplastic meningioma are unclear and controversial. Several retrospective studies have reported the importance of gross total resection (GTR) and its association with better survival outcomes. There has been a consensus in the literature that adjuvant irradiation is essential regardless of the extent of resection in patients with anaplastic meningioma [5,7,9,10]. However, due to the rarity of the anaplastic meningioma itself, there are few studies that have proven its prognostic value statistically [2,3,4,6,10,11].
The purpose of the present study was to analyze the prognostic factors influencing survival outcomes. Moreover, we analyzed the progression patterns in patients with anaplastic meningioma and determine the clinical efficacy of stereotactic radiosurgery and chemotherapy after the recurrence of anaplastic meningioma. To our knowledge, this study involved largest cohort of anaplastic meningioma among the clinical studies from a single institute. In this regard, we expected that this study can deliver a practical nuance to the multi-disciplinary team involved neuro-oncology beyond the statistical results in this rare tumor.
MATERIALS AND METHODS
This retrospective study was approved by the Institutional Review Board of Asan Medical Center (IRB no. 2021-0487). The need for informed consent was waived due to the retrospective nature of the study. Based on prospectively collected adult brain tumor database, 76 consecutive patients were diagnosed with malignant meningioma or anaplastic meningioma after surgical resection from 1995 to 2020. Among these patients, a total of 48 patients were enrolled in this study; we excluded 18 patients who did not meet the criteria of 2016 WHO classification for anaplastic meningioma, 5 patients without available clinical radiological data, 3 patients with a follow-up duration shorter than 12 months, one patient with intracranial metastasis of spinal meningioma, and one patient with neurofibromatosis.
Prior to 2000, WHO classification had ambiguous criteria for grading meningioma. Based on the studies from Mayo Clinic published in the late 1990s [12], the 2000 WHO classification presented a more objective criteria in meningioma grading [13]. And for WHO grade 3 meningioma, the revised 4th edition of WHO classification still applies this criteria as it is [14,15]. The biggest part that changed the diagnostic criteria for anaplastic or malignant meningioma around 2000 is the brain invasion. Brain invasion was considered as a solid criterion for malignant meningioma before 2000, but current WHO criteria for anaplastic meningioma excludes brain invasion. According to the diagnostic criteria for anaplastic meningioma in the 2000s, 18 cases diagnosed with malignant meningioma by brain invasion before 2000 were excluded from this study. In 2022, the 5th edition of the WHO classification of central nervous system tumors was published. According to this, it is emphasized that the criteria defining anaplastic meningioma should be applied regardless of the underlying subtype. And, several molecular biomarkers are also associated with classification and grading of meningioma [16,17]. In this study, there were two cases of rhabdoid subtype and none of the papillary subtype. In the two cases diagnosed as rhabdoid subtypes, mitotic indices were 12 and 9 per 10 high-power field, respectively, and were included in this study. Evaluation for TERT promoter mutation, homozygous deletion of CDKN2A/B and H3K-27me3 loss of nuclear expression were not carried routinely in the patients included in this study.
Baseline characteristics of clinico-radiologic data were retrospectively collected and are summarized in Table 1. The mean and median follow-up durations were 42 months and 30 months, respectively (range, 4–140 months). Thirty patients (62.5%) were male and 18 (37.5%) were female, with a median age of 57 years (range, 32–77 years). Twenty-eight patients (58.3%) were initially diagnosed with anaplastic meningioma and 20 (41.7%) were secondary anaplastic meningioma from atypical or benign meningioma. We analyzed radiologic data in the following way: location (superficial location vs. deep location), tumor size (<45 mm vs. ≥45 mm), peri-tumoral edema (none or mild vs. moderate to severe), tumor shape (round vs. mushroom). The locations of tumors were divided into superficial location (including convexity and parasagittal location) and deep location (including falcine, skull base, and intraventricular location). Tumor size was defined as the largest tumor diameter on gadolinium-enhanced T1-weighted MRI. Peri-tumoral edema was estimated by the longest distance from the margin of the tumor on fluid-attenuated inversion recovery images or T2 weighted images. The edema index (EI) was defined as the ratio of edema diameter to tumor diameter. The grading of edema severity according to EI was performed as follows: no edema or negligible edema (EI<0.1); mild edema (0.1<EI<1.0); moderate edema (1.0<EI<2.0); severe edema (EI>2), and then the patients were divided into two groups: one with minimal to mild edema (EI<1.0) and the other with moderate to severe edema (EI>1.0) [18]. The shape of the tumor was classified as one of round and mushroom shape. Mushroom-shaped tumors were defined as having a prominent pannus extending over the cerebral surface from the globoid portion of the tumor [19]. The degree of resection was preferentially determined by a review of postoperative and follow-up MRI studies or CT scanning. GTR was defined when no residual tumor was seen on contrast T1-weighted or T2-weighted images or on contrast CT images; otherwise, cases were defined as a subtotal resection. The Simpson grading scale which considered the gold standard for defining the surgical extent of resection was collected through surgical records and was dichotomized for statistical analysis (Simpson grade 1 or 2 vs. Simpson grade 3 or 4 or 5).
Table 1. Summary of characteristics in 48 patients.
| Parameter | No. of patients (%) | |
|---|---|---|
| Sex | ||
| Male | 30 (62.5) | |
| Female | 18 (37.5) | |
| Age | ||
| <57 yrs | 20 (41.7) | |
| ≥57 yrs | 28 (58.3) | |
| Location | ||
| Convexity | 35 (72.9) | |
| Deep or skull base | 13 (27.1) | |
| Tumor size | ||
| <45 mm | 19 (39.6) | |
| ≥45 mm | 29 (60.4) | |
| Peritumoral edema | ||
| None or mild | 18 (37.5) | |
| Moderate to severe | 30 (62.5) | |
| Tumor shape | ||
| Round | 17 (35.4) | |
| Mushroom | 31 (64.6) | |
| Simpson grade | ||
| 1 | 20 (41.7) | |
| 2 | 11 (22.9) | |
| 3 | 8 (16.7) | |
| 4 | 8 (16.7) | |
| 5 | 1 (2) | |
| Subtype of pathology | ||
| Grade 3, anaplastic | 46 (95.9) | |
| Grade 3, rhabdoid | 2 (4.1) | |
| Grade 3, papillary | 0 | |
| Dichotomized Ki-67 index | ||
| Ki-67 <20% | 21 (43.8) | |
| Ki-67 ≥20% | 27 (56.2) | |
| Diagnosis type | ||
| Primary | 28 (58.3) | |
| Secondary (malignant transformation) | 20 (41.7) | |
| Adjuvant radiotherapy | ||
| No | 16 (33.3) | |
| Yes | 32 (66.7) | |
Statistical analysis
Statistical analyses were performed with the Statistical Package for the Social Sciences version 21.0 (IBM Corp., Armonk, NY, USA). The means of numeric variables and the distributions of categorical variables between subgroups were compared with independent-samples t-tests and χ2 test, respectively. Progression-free survival (PFS) was calculated from the date of initial surgery diagnosed as anaplastic or malignant meningioma to the date of recurrence, progression, death or last radiologic follow-up, whereas overall survival (OS) was calculated from the date of surgery to the date of death. Data for patients who were alive were classified as censored at the time of the last follow-up. PFS and OS were analyzed by Kaplan-Meier curves, and comparisons between groups were performed using the log-rank tests. A Cox proportional hazards model was used to adjust for covariates which showed p<0.2 on univariate test. Simpson grade contains subjective elements based on the intraoperative visual assessment, so we included only extent of resection based on the postoperative image in the multivariate analysis.
RESULTS
Treatment summary
GTR was performed in 36 patients (75.0%) and Simpson grade 1 or 2 resection was achieved 31 patients (64.6%). Thirty-two patients (66.7%) received external beam radiation as an adjuvant therapy after tumor resection with confirmed WHO grade 3 meningioma. Of the 28 patients diagnosed with primary anaplastic meningioma, 26 patients (92.8%) received adjuvant radiotherapy. In patients with secondary anaplastic meningioma, only 30% of patients (6 patients out of 20) received adjuvant radiotherapy. Adjuvant chemotherapy was performed in two patients with secondary anaplastic meningioma.
Analysis of survival
In terms of PFS rates, we analyzed the correlation between risk factors and survival rate (Table 2). The median PFS of the entire population was 13.9 months (95% confidence interval [CI]=8.8 through 19.1). Estimated PFS rates at 1, 2, 5, and 10 years were 59.0%, 40.0%, 21.8%, and 20.8%, respectively (Fig. 1). Male, primary anaplastic meningioma, GTR, and adjuvant radiotherapy were associated with longer PFS upon univariate analysis . However, as seen in Table 2, adjuvant radiotherapy (p<0.001, hazard ratio [HR] 0.113, 95% CI=0.034–0.374) was shown to be only prognostic factor for a better PFS in the multivariate analysis. On the other hand, superficial tumor location (p=0.079) and GTR (p=0.114) failed to show significance in a multivariate analysis.
Table 2. Progression-free survival rates in intracranial anaplastic meningioma.
| Variables | No. of progression/no. of patients (%) | Univariate analysis | Multivariate analysis | ||||
|---|---|---|---|---|---|---|---|
| Survival (month, mean±SE) | p value (log-rank) | HR | 95% CI | p value | |||
| Overall | 34/48 (70.8) | 13.9±2.6 | - | ||||
| Age (years) | 0.552 | ||||||
| <57 | 16/20 (80.0) | 9.6±10.4 | |||||
| ≥57 | 18/28 (64.3) | 13.9±1.7 | |||||
| Sex | 0.016 | 1.387 | 0.673–2.859 | 0.375 | |||
| Male | 18/30 (60.0) | 28.4±8.7 | |||||
| Female | 16/18 (89.9) | 8.8±1.9 | |||||
| Diagnosis type | <0.001 | 1.569 | 0.614–4.006 | 0.346 | |||
| Primary | 16/28 (57.1) | 29.7±10.9 | |||||
| Secondary | 18/20 (90.0) | 5.7±0.8 | |||||
| Location | 0.080 | 1.987 | 0.923–4.278 | 0.079 | |||
| Superficial | 22/35 (62.9) | 17.9±8.1 | |||||
| Deep or skull base | 12/13 (92.3) | 6.2±3.9 | |||||
| Tumor size | 0.083 | ||||||
| <4.5 cm | 17/19 (89.5) | 12.5±3.7 | |||||
| ≥4.5 cm | 17/29 (58.6) | 26.7±13.4 | |||||
| Peritumoral edema | 0.668 | ||||||
| Mild | 12/18 (66.7) | 14.7±6.3 | |||||
| Moderate to severe | 22/30 (73.3) | 13.9±4.7 | |||||
| Tumor shape | 0.470 | ||||||
| Round | 13/17 (76.5) | 13.9±2.2 | |||||
| Mushroome | 21/31 (67.7) | 15.4±5.9 | |||||
| Preoperative ECOG | 0.278 | ||||||
| 0 or 1 | 15/24 (62.5) | 17.3±10.3 | |||||
| ≥2 | 19/24 (79.2) | 13.0±3.3 | |||||
| Extent of resection | <0.001 | 1.896 | 0.858–4.191 | 0.114 | |||
| GTR | 22/36 (61.1) | 26.7±9.6 | |||||
| STR | 12/12 (100) | 5.7±0.6 | |||||
| Simpson grade | 0.125 | ||||||
| 1 or 2 | 20/31 (64.5) | 17.9±9.6 | |||||
| 3 or 4 or 5 | 14/17 (82.4) | 8.8±3.5 | |||||
| Adjuvant radiation | <0.001 | 0.113 | 0.034–0.374 | <0.001 | |||
| No | 15/16 (93.7) | 4.4±0.7 | |||||
| Yes | 19/32 (59.4) | 29.7±4.2 | |||||
SE, standard error; HR, hazard ratio; 95% CI, 95% confidence interval; ECOG, Eastern Cooperative Oncology Group; GTR, gross total resection; STR, subtotal resection
Fig. 1. Kaplan–Meier survival analysis. A and B: The 2-year and 5-year progression-free survival (PFS) rate 40.0% and 21.8%, respectively (A). The 2-year and 5-year overall survival (OS) rate 76.7% and 47.9%, respectively (B). C and D: Adjuvant radiotherapy showed statistically meaningful result in both PFS (C) and OS (D).
Twenty-five patients (52.1%) died during the follow-up period. The median OS of the entire population was 56.9 months (95% CI=24.1–89.7). Estimated OS rates at 1, 2, 5, and 10 years were 93.8%, 76.7%, 47.9%, and 36.6%, respectively. On univariate analysis, primary anaplastic meningioma, GTR, and adjuvant radiotherapy were found to be variables associated with a longer OS (Table 3). On multivariate analysis, adjuvant radiotherapy (p<0.001, HR 0.161, 95% CI=0.036–0.731) was the only variable found to be associated with a longer OS.
Table 3. Overall survival rates in intracranial anaplastic meningioma.
| Variables | No. of progression/no. of patients (%) | Univariate analysis | Multivariate analysis | ||||
|---|---|---|---|---|---|---|---|
| Survival (month, mean±SE) | p value (log-rank) | HR | 95% CI | p value | |||
| Overall | 25/48 (52.1) | 56.90±16.75 | |||||
| Age | 0.881 | ||||||
| <57 yrs | 12/20 (60) | 50.73±31.31 | |||||
| ≥57 yrs | 13/28 (46.4) | 56.9±15.59 | |||||
| Sex | 0.055 | 1.377 | 0.615–3.084 | 0.437 | |||
| Male | 12/30 (46.7) | 77.70 | |||||
| Female | 13/18 (72.2) | 32.93±4.71 | |||||
| Diagnosis type | 0.049 | 0.523 | 0.125–2.182 | 0.374 | |||
| Primary | 13/28 (53.6) | 81.27 | |||||
| Secondary | 12/20 (60.0) | 36±5.48 | |||||
| Location | 0.146 | 2.214 | 0.909–5.394 | 0.080 | |||
| Superficial | 16/35 (51.4) | 61.70±19.23 | |||||
| Deep or skull base | 9/13 (69.2) | 18.60±8.91 | |||||
| Tumor size | 0.341 | ||||||
| <4.5 cm | 12/19 (63.2) | 37.53±18.40 | |||||
| ≥4.5 cm | 13/29 (51.7) | 77.70 | |||||
| Peritumoral edema | 0.918 | ||||||
| Mild | 10/18 (61.1) | 50.73±31.55 | |||||
| Moderate to severe | 15/30 (53.3) | 56.90±15.97 | |||||
| Tumor shape | 0.602 | ||||||
| Round | 10/17 (64.7) | 77.70 | |||||
| Mushroome | 15/31 (51.6) | 49.90±10.25 | |||||
| Preoperative ECOG | 0.267 | ||||||
| 0 or 1 | 10/24 (45.8) | 77.70 | |||||
| ≥2 | 15/24 (66.7) | 49.90±13.80 | |||||
| Extent of resection | <0.001 | 2.296 | 0.926–5.693 | 0.073 | |||
| GTR | 14/36 (44.4) | - | |||||
| STR | 11/12 (91.7) | 28.90±11.29 | |||||
| Simpson grade | 0.058 | ||||||
| 1 or 2 | 14/31 (51.6) | 81.27 | |||||
| 3 or 4 or 5 | 11/17 (64.7) | 32.93±14.83 | |||||
| Adjuvant radiation | <0.001 | 0.161 | 0.036–0.731 | 0.018 | |||
| No | 12/16 (75.0) | 18.20±10.71 | |||||
| Yes | 13/32 (46.9) | 81.27 | |||||
SE, standard error; HR, hazard ratio; 95% CI, 95% confidence interval; ECOG, Eastern Cooperative Oncology Group; GTR, gross total resection; STR, subtotal resection
Progression pattern and salvage treatment
Disease progression patterns and salvage treatments at progression in all patients were summarized in Table 4. Disease progression occurred in 34 patients (70.8%). Extra-cranial dissemination was in 8 patients. Common sites for extra-cranial metastasis were lung (in 4 patients) and bone (in 3 patients). Intra-cranial dissemination was in 26 patients and leptomeningeal seeding in 4 patients.
Table 4. Relapse patterns and treatment at progression in intracranial anaplastic meningioma.
| No | Sex | Age (yr) | Primary or secondary | Location | Extent of resection | Adjuvant therapy | PFS (mo) | Relapse patterns | Treatment at recurrence | Chemotherapy agent | Effect of chemotherapy | Survival status | OS (mo) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | F | 46 | Secondary | Sphenoidal ridge | STR | - | 6 | ICD | Observation | - | - | Death | 29 |
| 2 | F | 56 | Secondary | Spheno-orbital | STR | - | 1 | ICD | Op | - | - | Death | 36 |
| 3 | M | 52 | Primary | Parasagittal | GTR | RTx | 27 | Local, ICD, ECD (lung) | CTx, Op | Hydroxyurea | PD | Death | 78 |
| 4 | M | 46 | Secondary | Sphenoid ridge | STR | - | 4 | Local | Op | - | - | Death | 17 |
| 5 | F | 66 | Secondary | Frontal | GTR | - | 6 | Local, ICD | Op, SRS | - | - | Death | 18 |
| 6 | M | 66 | Primary | Parietal | GTR | - | 15 | Local, ICD | Op | - | - | Death | 28 |
| 7 | F | 48 | Primary | Temporal | STR | - | 15 | ICD | Op | - | - | Death | 51 |
| 8 | F | 67 | Primary | Tuberculum sellae | STR | - | 12 | Local, ECD (lung) | Op | - | - | Death | 19 |
| 10 | F | 55 | Secondary | Sphenoid ridge | GTR | - | 4 | LMS | Op, RTx | - | - | Death | 12 |
| 12 | F | 49 | Primary | 4th ventricle | GTR | RTx | 18 | LMS | RTx | - | - | Death | 81 |
| 13 | M | 60 | Secondary | Frontal | GTR | RTx | 14 | ICD | Op #2, SRS | - | - | Death | 62 |
| 15 | M | 51 | Secondary | Temporal | GTR | 4 | ICD | Op, SRS, CTx | ICE #2 | PD | Death | 14 | |
| Adriamycin #2 | PD | ||||||||||||
| Irinotecan #1 | PD | ||||||||||||
| 16 | M | 56 | Primary | Convexity | GTR | RTx | 35 | Local, ICD | Op #2, CTx, SRS | TMZ #6 | PD | Alive | 100 |
| 18 | M | 32 | Primary | Sphenoid ridge | GTR | RTx | 66 | Local, ECD (lung) | SRS, lung | - | - | Alive | 90 |
| 21 | M | 68 | Primary | Parasagittal | STR | - | 4 | Local, ICD | Denial to treat | - | - | Death | 8 |
| 22 | M | 59 | Secondary | Parasagittal | STR | - | 5 | ICD (skull base) | SRS #3 | - | - | Death | 57 |
| 23 | F | 72 | Primary | Sphenoid ridge | GTR | RTx | 13 | Local, ICD | SRS #2 | - | - | Alive | 72 |
| 25 | F | 77 | Primary | Scalp, convexity | STR | RTx | 32 | ICD, ECD (lung) | Denial to treat | - | - | Death | 50 |
| 27 | M | 57 | Primary | Intraventricular | STR | RTx | 6 | Local | Observation | - | - | Death | 12 |
| 29 | M | 69 | Primary | Convexity | GTR | RTx | 30 | Local | SRS | - | - | Death | 38 |
| 30 | F | 75 | Secondary | Falx | GTR | RTx | 52 | Local, ICD | Denial to treat | - | - | Alive | 63 |
| 31 | F | 63 | Primary | Frontal | GTR | RTx | 6.7 | Local, ECD (spine) | Op (brain, spine), SRS | - | - | Death | 16 |
| 32 | M | 53 | Secondary | Convexity | GTR | RTx | 28 | ICD | Op, RTx | - | - | Alive | 61 |
| 33 | F | 50 | Secondary | Convexity | GTR | - | 6 | Local, LMS | Denial to treat | - | - | Death | 8 |
| 34 | F | 77 | Secondary | Convexity | GTR | - | 2 | ICD, ECD (multiple bone) | OP, SRS, RTx | - | - | Death | 8 |
| 35 | M | 46 | Primary | Intraventricular | GTR | RTx | 6 | ICD, ECD (rib) | OP, RTx, CTx | ICE #3 | PD | Death | 32 |
| 36 | F | 56 | Primary | Parasagittal | GTR | - | 10 | Local, ICD | OP, RTx, CTx | ICE #2 | PD | Death | 30 |
| Avastine #3 | PD | ||||||||||||
| Sunitinib #2 | PD | ||||||||||||
| 37 | M | 52 | Secondary | Sphenoid ridge | GTR | CTx (TMZ #4) | 4 | Local, LMS | OP, SRS, CTx, WBRT | ICE #6 | SD (6 mo) → PD | Death | 15 |
| 38 | M | 60 | Primary | Convexity | GTR | RTx | 9 | Local | OP, CTx | ICE #6 | SD (5 mo) | Death | 30 |
| Avastine #6 | PD | ||||||||||||
| 39 | F | 57 | Secondary | Parietal | STR | CKRS | 8 | ICD | OP, CTx | ICE #4 | SD (4 mo) → PD | Death | 33 |
| 42 | M | 59 | Secondary | Convexity | GTR | RTx | 17 | ICD | OP | - | - | Alive | 32 |
| 43 | M | 57 | Secondary | Convexity, scalp | STR | CTx (ICE #6) | 13 | ICD | SRS #2, CTx | ICE #6 | PR → PD | Alive | 30 |
| Avastine #3 | PD | ||||||||||||
| 44 | F | 71 | Secondary | Convexity | GTR | No | 9 | Local | Salvage RTx | - | - | Alive | 26 |
| 45 | M | 47 | Secondary | Convexity | GTR | No | 4 | 4 ICD, ECD (scalp) | CTx | ICE #4 | SD (7 mo) → PD | Alive | 25 |
PFS, prgression-free survival; OS, overall survival; M, male; F, female; GTR, gross total resection; STR, subtotal resection; ICD, intracranial dissemination; LMS, leptomeningeal seeding; ECD, extracranial dissemination; CKRS, CyberKnife radiosurgery; WBRT, whole brain radio therapy; ICE, ifosfamide, carboplatin, etoposide; TMZ, temozolomide; Op, operation; RTx, radiation therapy; SRS, stereotactic radiosurgery; CTx, chemotherapy; PD, progressive disease; SD, stable disease
After disease progression was confirmed, surgical resection was performed in 20 patients, and salvage radiotherapy was performed in 9 patients. Chemotherapy was performed in 9 patients. Stereotactic radiosurgery (SRS) was performed 23 times in 16 patients. Six patients received conservative care due to a poor performance status or unwillingness to undergo treatment.
Response to salvage treatment
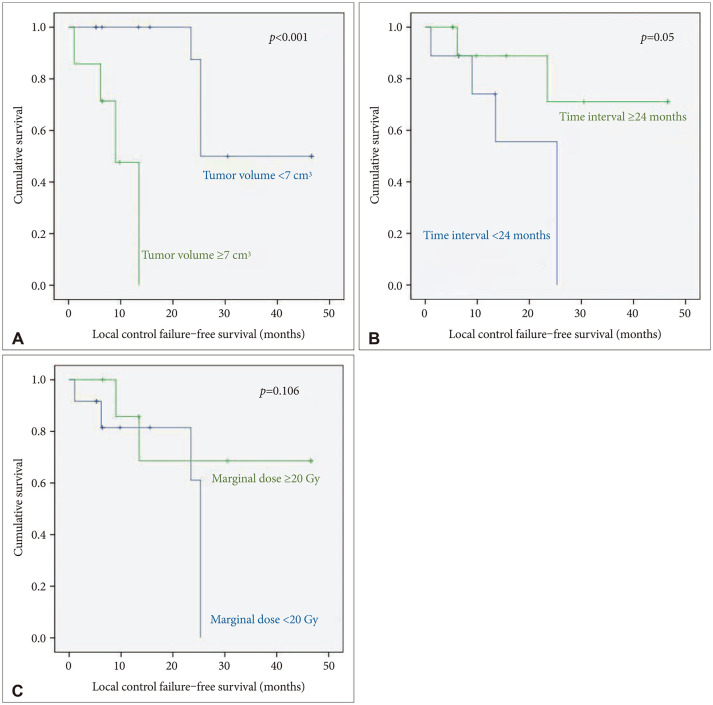
SRS using Gamma Knife was performed 12 times, and SRS using CyberKnife was performed 11 times. Tumor local control and distant failure were analyzed for 20 target lesions in 13 patients with follow-up brain MR images. The 1- and 2-year local control rates were 74.3% and 65%, respectively. In univariate analysis, small tumor volume (less than 7 cm3) and the longer interval between the diagnosis of anaplastic meningioma and SRS (more than 2 years) were found to be positive prognostic factors for local tumor control. However, in the multivariate analysis, no significant prognostic factors could be found due to the small sample size (Fig. 2). Distant failure occurred in 9 patients (69.2%) and the median time to distant failure was 5 months (range, 1–14 months).
Fig. 2. Kaplan-Meier survival analysis of local control. A: When the tumor volume was smaller than 7 cm3, the local control rate of steretactic radiosurgery (SRS) was higher (p<0.001). B: If the time interval between diagnosis of anaplastic meningioma and SRS was shorter than 24 months, local control rate was statistically lower (p≤0.05). C: Although the marginal dose is not statistically significant, it shows a trend that is helpful for local control as it is higher.
Salvage chemotherapy were used in 10 patients, and a total of 6 chemotherapeutic agent were used. Ifosfamide, carboplatin, etoposide (ICE) was used in 8 patients. Bevacizumab was used in three patients, and hydroxyurea, temozolomide, adriamycin, irinotecan, and sunitinib were used once each (Table 4). The only chemotherapeutic agent which showed a clinical effect was ICE, but the effect was marginal. In 8 patients treated with ICE, partial response was in one and stable diseases in 4 patients, but there was no effect in the remaining 3 patients. Unfortunately, all other chemotherapeutic agents were not effective in our cohort. In all 3 patients using bevacizumab, bevacizumab did not prevent disease progression.
DISCUSSION
Anaplastic meningioma is very rare and is generally known to have a poor prognosis [11,17,20]. In a study of 755 patients from an US national database, the 5-year OS rate in patients with anaplastic meningioma was 41.4% [11]. Our study showed a 5-year OS rate was 47.9%, similar to that from US national cancer database. However, due to its rarity, there are very few reports in the literature on the progression pattern and the response to treatment about anaplastic meningioma. Although many studies have been conducted by combining anaplastic meningioma and atypical meningioma, the clinical pattern and the response to treatment of anaplastic meningioma is clearly different from that of atypical meningioma. Our study included the largest number of patients among the articles that studied only anaplastic meningioma from a single institution. In this study, 28 patients with primary anaplastic meningioma and 20 patients with secondary anaplastic meningioma were analyzed, so the characteristics of each group could be well understood. In addition, since most patients were treated aggressively as possible as clinically permitted, the response to salvage therapeutic arms could be observed well.
Extent of resection is associated with prognosis of patients with all WHO grades of meningioma [5,10,21,22,23]. However, the statistical evidence for the positive effect of GTR on the prognosis in patient with anaplastic meningioma has been controversial because of the rarity of the tumors. We found that GTR was associated with significant better PFS and OS (p<0.001, p<0.001) in univariate analysis. However, multivariate analysis failed to prove the association with PFS and OS (p=0.114, p=0.073). Although our results do not ignore the positive effects of GTR on prognosis, it means that the importance of adjuvant therapy is relatively more emphasized in anaplastic meningioma compared with WHO grade 2 meningiomas.
The use of adjuvant radiotherapy after the surgical resection of anaplastic meningiomas is essential to their treatment [5,11,24,25]. In most of the reported series, there is a consensus that patients with anaplastic meningiomas should be treated with adjuvant radiotherapy irrespective of the extent of resection. Our findings are also consistent with those of other studies. In our multivariate analysis, adjuvant radiotherapy was found to be the only prognostic factors affecting PFS and OS (p<0.001, p=0.018). In our study, patients with secondary anaplastic meningiomas seems to have poor PFS and OS (p<0.001, p=0.049) in univariate analysis, but in multivariate analysis, diagnosis type did not affect to PFS and OS (p=0.346, p=0.374). Other groups have reported a better prognosis in patients with primary anaplastic meningioma because of the predominance of superficial location and surgical advantage for GTR [21,23,26]. In our study, there were more incidence of superficial location (75% vs. 70%, p=0.750) and more achieved GTR cases (82.1% vs. 65%, p=0.155) in primary anaplastic glioma, but there was no statistical difference. We postulated that the cause of our statistical result was that the proportion of patients who received radiotherapy was significantly higher in primary anaplastic meningioma than in secondary anaplastic meningioma (92.8% vs. 30%, p<0.001).
There is debate about the prognosis according to sex. Cain et al. [27] reported that 3-year OS was 31% higher for women than for men, on the contrary, that the female recurrence rates were 2 times higher than the male recurrence rates [21]. In our univariate study, the poor prognosis in females may be attributed to the high rate (55.6%) of secondary anaplastic meningioma and low proportion (50%) of adjuvant radiotherapy. In multivariate analysis, sex was not a prognostic factor. It is widely known that specific radiographic findings are related to histologic grade in meningioma: tumor size [28,29]; tumor location [28,30]; peri-tumoral edema [28,31,32]; irregularities in the shape of meningiomas such as “mushroom” [33,34]; presence of tumor heterogeneity such as necrosis, cystic degeneration, and hemorrhage [28,35,36]. However, our study results showed that radiological findings were not related to prognosis in anaplastic meningioma.
A significant number of patients with anaplastic meningiomas will eventually relapse despite appropriate treatment. A considerable proportion of relapsed patients had intracranial dissemination (76.4%), and leptomeningeal seeding was also present in 11.7% of relapsed patients. Therefore, it is common to show low surgical resectability at disease progression. SRS and chemotherapy could be considered as salvage treatment options. Despite the risk of radiation necrosis, it cannot be ignored that SRS has some therapeutic effect in patients with anaplastic meningioma. Helis et al. [37] reported distant control failure (49.1%) and local control failure (36.0%). In this study, 2-years local control rates was 65% and distant control failures in 69.2% cases. Although the optimal timing of radiosurgery for atypical and anaplastic meningioma remains the subject of ongoing debate [37,38,39,40], SRS should be considered in patients who cannot afford additional radiotherapy. There have been several attempts at chemotherapy for anaplastic meningioma, but most of them had poor results [2,41]. In this study, only ICE regimen have modest beneficial effect on anaplastic meningioma.
Also, 16.6% of all patients had extracranial metastasis. Because routine systemic workup was not performed in all patients, it is considered to be an underestimated result. Although treatment options in the presence of extracranial metastasis are quite limited, but it is necessary to consider the need for a systemic workup to evaluate extracranial dissemination in the event of disease relapse.
This study has inevitable limitations as shown in the previous reports about anaplastic meningiomas from single institution, such as a long study span, retrospective study design, which limits the statistical power. Above all, there was a lack of consideration of TERT promoter mutation, homozygous deletion of CDKN2A/B and H3K27me3 loss of nuclear expression, which are newly emerging molecular findings. We expect that future studies explore the molecular biology in anaplastic meningioma and lead to the development of effective target agents in the near future.
In conclusion, adjuvant radiotherapy is an essential treatment arm in patients with anaplastic meningiomas. SRS seems to play an important role as a salvage treatment. But chemotherapy seems to have limited efficacy. Because of the disseminated nature of the disease, further investigations to improve prognosis are needed.
Footnotes
- Conceptualization: Dong Ok Seo, Sang Woo Song.
- Data curation: Dong Ok Seo, Sang Woo Song.
- Formal analysis: Sang Woo Song.
- Funding acquisition: Sang Woo Song.
- Investigation: Sang Woo Song.
- Methodology: Sang Woo Song.
- Project administration: Sang Woo Song.
- Resources: Sang Woo Song.
- Software: Sang Woo Song.
- Supervision: Sang Woo Song, Young-Hoon Kim, Chang-Ki Hong, Jeong Hoon Kim.
- Validation: Sang Woo Song, Young-Hoon Kim, Chang-Ki Hong, Jeong Hoon Kim.
- Visualization: Sang Woo Song, Young-Hoon Kim, Chang-Ki Hong, Jeong Hoon Kim.
- Writing—original draft: Dong Ok Seo.
- Writing—review & editing: Sang Woo Song, Young-Hoon Kim, Chang-Ki Hong, Jeong Hoon Kim.
Conflicts of Interest: The authors have no potential conflicts of interest to disclose.
Funding Statement: None
Availability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author on reasonable request.
References
- 1.Ostrom QT, Cioffi G, Gittleman H, Patil N, Waite K, Kruchko C, et al. CBTRUS statistical report: primary brain and other central nervous system tumors diagnosed in the United States in 2012-2016. Neuro Oncol. 2019;21(Suppl 5):v1–v100. doi: 10.1093/neuonc/noz150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ogasawara C, Philbrick BD, Adamson DC. Meningioma: a review of epidemiology, pathology, diagnosis, treatment, and future directions. Biomedicines. 2021;9:319. doi: 10.3390/biomedicines9030319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kim JK, Jung TY, Jung S, Lee KH, Kim SK, Lee EJ. Meningiomas with rhabdoid or papillary components: prognosis and comparison with anaplastic meningiomas. J Korean Neurosurg Soc. 2016;59:357–362. doi: 10.3340/jkns.2016.59.4.357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Masalha W, Heiland DH, Delev D, Fennell JT, Franco P, Scheiwe C, et al. Survival and prognostic predictors of anaplastic meningiomas. World Neurosurg. 2019;131:e321–e328. doi: 10.1016/j.wneu.2019.07.148. [DOI] [PubMed] [Google Scholar]
- 5.Palma L, Celli P, Franco C, Cervoni L, Cantore G. Long-term prognosis for atypical and malignant meningiomas: a study of 71 surgical cases. J Neurosurg. 1997;86:793–800. doi: 10.3171/jns.1997.86.5.0793. [DOI] [PubMed] [Google Scholar]
- 6.Sughrue ME, Sanai N, Shangari G, Parsa AT, Berger MS, McDermott MW. Outcome and survival following primary and repeat surgery for World Health Organization Grade III meningiomas. J Neurosurg. 2010;113:202–209. doi: 10.3171/2010.1.JNS091114. [DOI] [PubMed] [Google Scholar]
- 7.Dziuk TW, Woo S, Butler EB, Thornby J, Grossman R, Dennis WS, et al. Malignant meningioma: an indication for initial aggressive surgery and adjuvant radiotherapy. J Neurooncol. 1998;37:177–188. doi: 10.1023/a:1005853720926. [DOI] [PubMed] [Google Scholar]
- 8.Kang H, Song SW, Ha J, Won YJ, Park CK, Yoo H, et al. A nationwide, population-based epidemiology study of primary central nervous system tumors in Korea, 2007-2016: a comparison with United States data. Cancer Res Trea. 2021;53:355–366. doi: 10.4143/crt.2020.847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hug EB, Devries A, Thornton AF, Munzenride JE, Pardo FS, Hedley-Whyte ET, et al. Management of atypical and malignant meningiomas: role of high-dose, 3D-conformal radiation therapy. J Neurooncol. 2000;48:151–160. doi: 10.1023/a:1006434124794. [DOI] [PubMed] [Google Scholar]
- 10.Kaur G, Sayegh ET, Larson A, Bloch O, Madden M, Sun MZ, et al. Adjuvant radiotherapy for atypical and malignant meningiomas: a systematic review. Neuro Oncol. 2014;16:628–636. doi: 10.1093/neuonc/nou025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Orton A, Frandsen J, Jensen R, Shrieve DC, Suneja G. Anaplastic meningioma: an analysis of the National Cancer Database from 2004 to 2012. J Neurosurg. 2018;128:1684–1689. doi: 10.3171/2017.2.JNS162282. [DOI] [PubMed] [Google Scholar]
- 12.Hassoun J. [New WHO classification of central nervous system tumors] Bull Cancer Radiother. 1994;81:330–334. French. [PubMed] [Google Scholar]
- 13.Kleihues P, Sobin LH. World Health Organization classification of tumors. Cancer. 2000;88:2887. doi: 10.1002/1097-0142(20000615)88:12<2887::aid-cncr32>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- 14.Kobyakov GL, Absalyamova OV, Poddubskiy AA, Lodygina KS, Kobyakova EA. [The 2016 WHO classification of primary central nervous system tumors: a clinician's view] Zh Vopr Neirokhir Im N N Burdenko. 2018;82:88–96. doi: 10.17116/neiro201882388. Russian. [DOI] [PubMed] [Google Scholar]
- 15.DeWitt JC, Mock A, Louis DN. The 2016 WHO classification of central nervous system tumors: what neurologists need to know. Curr Opin Neurol. 2017;30:643–649. doi: 10.1097/WCO.0000000000000490. [DOI] [PubMed] [Google Scholar]
- 16.Louis DN, Perry A, Wesseling P, Brat DJ, Cree IA, Figarella-Branger D, et al. The 2021 WHO classification of tumors of the central nervous system: a summary. Neuro Oncol. 2021;23:1231–1251. doi: 10.1093/neuonc/noab106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wen PY, Packer RJ. The 2021 WHO classification of tumors of the central nervous system: clinical implications. Neuro Oncol. 2021;23:1215–1217. doi: 10.1093/neuonc/noab120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Paek SH, Kim CY, Kim YY, Park IA, Kim MS, Kim DG, et al. Correlation of clinical and biological parameters with peritumoral edema in meningioma. J Neurooncol. 2002;60:235–245. doi: 10.1023/a:1021186401522. [DOI] [PubMed] [Google Scholar]
- 19.Yoshioka H, Hama S, Taniguchi E, Sugiyama K, Arita K, Kurisu K. Peritumoral brain edema associated with meningioma: influence of vascular endothelial growth factor expression and vascular blood supply. Cancer. 1999;85:936–944. doi: 10.1002/(sici)1097-0142(19990215)85:4<936::aid-cncr23>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- 20.Yang SY, Park CK, Park SH, Kim DG, Chung YS, Jung HW. Atypical and anaplastic meningiomas: prognostic implications of clinicopathological features. J Neurol Neurosurg Psychiatry. 2008;79:574–580. doi: 10.1136/jnnp.2007.121582. [DOI] [PubMed] [Google Scholar]
- 21.Zhao P, Hu M, Zhao M, Ren X, Jiang Z. Prognostic factors for patients with atypical or malignant meningiomas treated at a single center. Neurosurg Rev. 2015;38:101–107. doi: 10.1007/s10143-014-0558-2. discussion 107. [DOI] [PubMed] [Google Scholar]
- 22.Choi Y, Lim DH, Jo K, Nam DH, Seol HJ, Lee JI. Efficacy of postoperative radiotherapy for high grade meningiomas. J Neurooncol. 2014;119:405–412. doi: 10.1007/s11060-014-1507-1. [DOI] [PubMed] [Google Scholar]
- 23.Moliterno J, Cope WP, Vartanian ED, Reiner AS, Kellen R, Ogilvie SQ, et al. Survival in patients treated for anaplastic meningioma. J Neurosurg. 2015;123:23–30. doi: 10.3171/2014.10.JNS14502. [DOI] [PubMed] [Google Scholar]
- 24.McCarthy BJ, Davis FG, Freels S, Surawicz TS, Damek DM, Grutsch J, et al. Factors associated with survival in patients with meningioma. J Neurosurg. 1998;88:831–839. doi: 10.3171/jns.1998.88.5.0831. [DOI] [PubMed] [Google Scholar]
- 25.Pollock BE, Stafford SL, Link MJ, Garces YI, Foote RL. Stereotactic radiosurgery of World Health Organization grade II and III intracranial meningiomas: treatment results on the basis of a 22-year experience. Cancer. 2012;118:1048–1054. doi: 10.1002/cncr.26362. [DOI] [PubMed] [Google Scholar]
- 26.Krayenbühl N, Pravdenkova S, Al-Mefty O. De novo versus transformed atypical and anaplastic meningiomas: comparisons of clinical course, cytogenetics, cytokinetics, and outcome. Neurosurgery. 2007;61:495–503. doi: 10.1227/01.NEU.0000290895.92695.22. discussion 503-4. [DOI] [PubMed] [Google Scholar]
- 27.Cain SA, Smoll NR, Van Heerden J, Tsui A, Drummond KJ. Atypical and malignant meningiomas: considerations for treatment and efficacy of radiotherapy. J Clin Neurosci. 2015;22:1742–1748. doi: 10.1016/j.jocn.2015.03.054. [DOI] [PubMed] [Google Scholar]
- 28.Hale AT, Wang L, Strother MK, Chambless LB. Differentiating meningioma grade by imaging features on magnetic resonance imaging. J Clin Neurosci. 2018;48:71–75. doi: 10.1016/j.jocn.2017.11.013. [DOI] [PubMed] [Google Scholar]
- 29.Chernov MF, Kasuya H, Nakaya K, Kato K, Ono Y, Yoshida S, et al. 1H-MRS of intracranial meningiomas: what it can add to known clinical and MRI predictors of the histopathological and biological characteristics of the tumor? Clin Neurol Neurosurg. 2011;113:202–212. doi: 10.1016/j.clineuro.2010.11.008. [DOI] [PubMed] [Google Scholar]
- 30.Kane AJ, Sughrue ME, Rutkowski MJ, Shangari G, Fang S, McDermott MW, et al. Anatomic location is a risk factor for atypical and malignant meningiomas. Cancer. 2011;117:1272–1278. doi: 10.1002/cncr.25591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hsu CC, Pai CY, Kao HW, Hsueh CJ, Hsu WL, Lo CP. Do aggressive imaging features correlate with advanced histopathological grade in meningiomas? J Clin Neurosci. 2010;17:584–587. doi: 10.1016/j.jocn.2009.09.018. [DOI] [PubMed] [Google Scholar]
- 32.Pistolesi S, Fontanini G, Camacci T, De Ieso K, Boldrini L, Lupi G, et al. Meningioma-associated brain oedema: the role of angiogenic factors and pial blood supply. J Neurooncol. 2002;60:159–164. doi: 10.1023/a:1020624119944. [DOI] [PubMed] [Google Scholar]
- 33.Coroller TP, Bi WL, Huynh E, Abedalthagafi M, Aizer AA, Greenwald NF, et al. Radiographic prediction of meningioma grade by semantic and radiomic features. PLoS One. 2017;12:e0187908. doi: 10.1371/journal.pone.0187908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Liu Y, Chotai S, Chen M, Jin S, Qi ST, Pan J. Preoperative radiologic classification of convexity meningioma to predict the survival and aggressive meningioma behavior. PLoS One. 2015;10:e0118908. doi: 10.1371/journal.pone.0118908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Buetow MP, Buetow PC, Smirniotopoulos JG. Typical, atypical, and misleading features in meningioma. Radiographics. 1991;11:1087–1106. doi: 10.1148/radiographics.11.6.1749851. [DOI] [PubMed] [Google Scholar]
- 36.Nakasu S, Nakasu Y, Nakajima M, Matsuda M, Handa J. Preoperative identification of meningiomas that are highly likely to recur. J Neurosurg. 1999;90:455–462. doi: 10.3171/jns.1999.90.3.0455. [DOI] [PubMed] [Google Scholar]
- 37.Helis CA, Hughes RT, Cramer CK, Tatter SB, Laxton AW, Bourland JD, et al. Stereotactic radiosurgery for atypical and anaplastic meningiomas. World Neurosurg. 2020;144:e53–e61. doi: 10.1016/j.wneu.2020.07.211. [DOI] [PubMed] [Google Scholar]
- 38.Basalamah A, Al-Bolbol M, Ahmed O, Ali N, Al-Rashed S. Stereotactic radiosurgery (SRS) induced higher-grade transformation of a benign meningioma into atypical meningioma. Case Rep Surg. 2022;2022:4478561. doi: 10.1155/2022/4478561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Shepard MJ, Xu Z, Kearns K, Li C, Chatrath A, Sheehan K, et al. Stereotactic radiosurgery for atypical (World Health Organization II) and anaplastic (World Health Organization III) meningiomas: results from a multicenter, international cohort study. Neurosurgery. 2021;88:980–988. doi: 10.1093/neuros/nyaa553. [DOI] [PubMed] [Google Scholar]
- 40.Hasegawa H, Vakharia K, Link MJ, Stafford SL, Brown PD, Parney IF, et al. The role of single-fraction stereotactic radiosurgery for atypical meningiomas (WHO grade II): treatment results based on a 25-year experience. J Neurooncol. 2021;155:335–342. doi: 10.1007/s11060-021-03882-9. [DOI] [PubMed] [Google Scholar]
- 41.Kaley T, Barani I, Chamberlain M, McDermott M, Panageas K, Raizer J, et al. Historical benchmarks for medical therapy trials in surgery- and radiation-refractory meningioma: a RANO review. Neuro Oncol. 2014;16:829–840. doi: 10.1093/neuonc/not330. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated or analyzed during the study are available from the corresponding author on reasonable request.