Summary
Objective
The aim of this study was to analyse the understanding of heart failure (HF) by the general public and find the best way to raise people’s awareness of this issue.
Methods
This prospective, survey-based registry involved 501 people over 18 years old. The survey included information on the participants’ gender, education, place of residence, medical history, involvement in any area of healthcare, and having relatives suffering from HF. The participants were divided into three age groups, young (< 40 years), middle aged (40–65 years) and elderly (> 65 years), and two groups, depending on whether the participant’s relative was a HF sufferer or not.
Conclusion
Despite an increasing prevalence of heart failure, the general public still has insufficient knowledge on symptoms, causes and treatment methods of this disease. New methods of disseminating information should be considered in order to stop an escalating problem of low awareness of heart failure.
Keywords: prevention, heart failure, risk factors of heart failure, healthy lifestyle, public awareness
Following the European Society of Cardiology (ESC) definition, heart failure (HF) can be defined as a clinical syndrome characterised by typical symptoms, such as breathlessness, ankle swelling and fatigue, which may be accompanied by signs, for example elevated jugular venous pressure, pulmonary crackles and peripheral oedema, caused by a structural and/or functional cardiac abnormality, resulting in a reduced cardiac output and/ or elevated intracardiac pressures at rest or during stress.1
HF represents the possible end stage of any cardiovascular disease, while its prevalence and clinical relevance are steadily increasing.2 It affects almost 26 million people worldwide. In Europe approximately 15 million are affected, and a lifetime risk of developing HF is one in five.2-7 Overall, it appears that chronic heart failure (CHF) affects one to 3% of the general population and approximately 10% of the very elderly.8 In developed countries, the number of patients with CHF is increasing. This trend is the result of an increasing number of elderly people and an improvement in survival rate after acute states, for example, acute myocardial infarction.9
Although HF is an important epidemiological problem, awareness of most of its features in the general population in Europe is low. There are also clear misconceptions on the nature, severity, treatment options and costs of HF.10 In addition, the majority of studies reveal lack of knowledge of HF among patients.11-13
The HF Awareness and Perception in Europe study (SHAPE), one of the most detailed European studies on HF awareness, has shown several misbeliefs, and public knowledge on HF was found to be low.10 Although as many as 86% of respondents had heard of HF, only 3% identified the typical clinical presentation and 67% thought that HF patients live longer than cancer patients.10
The majority of information concerning HF gathered from countries such as Poland and Slovenia was collected during HF Awareness Day, under the patronage of the HF Association of the ESC.14,15 The data present a significant difference between the level of declared knowledge and correctly matched symptoms, and real-life situations show insufficient awareness of HF both among patients as well as the general population.14,15
Awareness of HF is not only necessary for patients to obtain appropriate understanding of their condition, but also in order for them to apply it and make proper decisions regarding their treatment. It is also crucial for the entire population in order to apply prophylaxis or to recognise initial symptoms of the disease, so as to begin diagnosis.
The aim of this study was to assess the understanding of HF by the general public and to find the best way to raise people’s awareness of this issue.
Methods
This was a prospective registry based on an anonymous internet survey, which was distributed for six months through various online sites, such as hospital websites, sites concerning healthy lifestyle and patient organisations. The group of respondents involved people over 18 years old. The study was approved by the Poznan University of Medical Sciences bioethical committee.
The participants of the study were divided into three groups, according to age: young (< 40 years), middle aged (40–65 years) and elderly (> 65 years), and two groups, depending on whether the participant’s relative was a HF sufferer or not. Accompanying heart diseases were not a variable determining the group of respondents.
The survey was designed to examine epidemiological information such as age, gender, educational status, place of residence, as well as answers to 16 questions related to symptoms of HF and methods of treatment of this condition. The patients were asked:
whether they were connected to any area of healthcare
whether they suffered from HF
whether their relatives suffered from HF
whether they suffered from other cardiovascular diseases
to evaluate their knowledge about HF (scale of 1–5); 1: no knowledge, 2: poor, 3: fair, 4: good, 5: very good
whether the following symptoms relate to HF: fatigue, upper/ lower limb oedema, excessive thirst, sweating, dyspnoea, cough, nausea, headache, chest pain, increase in body mass, excessive appetite, dizziness, loss of body mass, insomnia, hot flush, palpitation, anxiety, syncope
whether HF is equivalent to myocardial infarction • whether HF is a fatal disease
to assess their knowledge about the risk factors of HF (scale of 1–5); 1: no knowledge, 2: poor, 3: fair, 4: good, 5: very good • whether the following symptoms have an influence on HF: arterial hypertension, thyroid disease, diabetes, nicotine addiction, obesity, stress, excessive physical activity, female gender, hypercholesterolaemia, renal disease, alcohol abuse, lack of physical activity, neoplasm/tumour
whether the person suffering from HF should avoid physical activity
whether the person suffering from HF can play sport
to choose methods of treatment of HF: heart surgery, stimulator, physical activity, diet, pharmacotherapy, psychologist support, don’t know
whether HF is treatable
to name their source of knowledge on diseases and healthy lifestyle: general practitioner, specialist, registered nurse, relatives, other ill people, radio, television, internet, professional leaflets
whether they need more information about HF.
Statistical analysis
Statistical analysis was performed using STATISTICA 12 Statsoft. The probability of distribution of continuous variables was tested with the Shapiro–Wilk test and Liffefors. The Student’s t-test was used to compare continuous variables with a normal distribution and the Mann–Whitney U-test was used for continuous variables with a non-normal distribution. Chi-squared tests were used for categorical variables, with Yate’s correction where applicable. A p-value of < 0.05 was considered statistically significant for all the tests.
Results
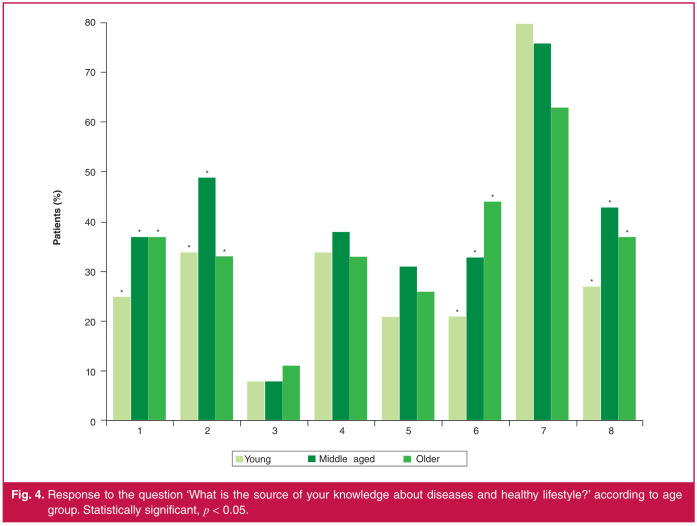
The study analysed responses from 501 participants gathered in an internet survey carried out in 2020. The mean age of the research group was 32 ± 14 years (76% < 40 years) and 74% of the respondents were women; 50% of the participants lived in cities with > 60 000 inhabitants and 57% had obtained higher education. A respectively large group of respondents (45%) consisted of people associated with the health services. Only 6% of the participants were affected by HF, whereas 33% of responders had relatives suffering from HF (Table 1). Among the study group, 27% of respondents assessed their knowledge of HF symptoms inclusively as good or very good, and 29% of participants assessed their understanding of HF risk factors as good or very good (Fig. 1).
Table 1. Baseline characteristics of the study population (n = 501).
| Characteristics | Number (percent) |
| Age (years), mean + SD | 32 +14 |
| Male gender | 130 (26) |
| Age < 40 years | 381 (76) |
| Age 40-65 years | 93 (19) |
| Age > 65 years | 27 (5) |
| Village | 121 (24) |
| City < 10 000 | 28 (6) |
| City 10 000-60 000 | 101 (20) |
| City > 60 000 | 252 (50) |
| Elementary education | 8 (2) |
| Vocational education | 24 (5) |
| Secondary education | 182 (36) |
| Higher education | 287 (57) |
| People connected with health services | 225 (45) |
| People suffering from HF | 32 (6) |
| People whose relatives suffer from HF | 164 (33) |
| Arterial hypertension | 65 (13) |
| Heart arrhythmia, e.g. atrial fibrillation | 37 (7) |
| Ischaemic heart disease (coronary heart disease) | 10 (2) |
| Previous myocardial infarction | 10 (2) |
| Valve disease | 3 (1) |
| Cardiac pacemaker (or ICD, or CRT) | 11 (2) |
| Aortic aneurysm | 2 (0) |
| Deep venous thrombosis | 5 (1) |
| Stroke/TIA | 3 (1) |
HF, heart failure; ICD, implantable cardioverter defibrillator; CRT, cardiac resynchronisation therapy; TIA, transient ischaemic attack.
Fig. 1.
Awareness of symptoms and risk factors of HF among the study groups (n = 501). HF, heart failure.
The most characteristic symptoms of HF for each of the age groups were dyspnoea (p = 0.08), palpitation (p = 0.26), lowerlimb oedema (p = 0.94) and fatigue (p = 0.95) (in descending order). The most frequently indicated symptom of HF was dyspnoea; 94% of young people chose this symptom, 90% of middle-aged people and 81% of elderly people. A significant number of respondents also indicated syncope (83, 75 and 59%, respectively; p < 0.01) and headache (52, 38 and 44%, respectively; p = 0.02) (Table 2).
Table 2. ‘Do the following symptoms relate to HF?’ Responses by age group, and group of relatives suffering/ not suffering from HF and positive answers.
| Symptoms | Young (<40 years) (%) | Middle aged (40-65 years) (%) | Elderly (>65 years) (%) | p-value | Relatives suffering from HF (%) | Relatives not suffer- ing from HF (%) | p-value |
| Fatigue | 87 | 81 | 70 | 0.95 | 89 | 85 | 0.08 |
| Lower-limb oedema | 84 | 87 | 81 | 0.94 | 91 | 82 | 0.02* |
| Upper-limb oedema | 46 | 34 | 26 | 0.06 | 45 | 44 | 0.60 |
| Excessive thirst | 27 | 16 | 22 | < 0.01* | 30 | 23 | 0.01* |
| Sweating | 54 | 56 | 52 | 0.10 | 64 | 51 | 0.01* |
| Dyspnoea | 94 | 90 | 81 | 0.08 | 96 | 91 | 0.30 |
| Cough | 48 | 46 | 44 | 0.34 | 55 | 45 | 0.01* |
| Nausea | 19 | 14 | 4 | < 0.01* | 23 | 15 | 0.06 |
| Headache | 52 | 38 | 44 | 0.02* | 59 | 45 | 0.05 |
| Chest pain | 90 | 82 | 89 | 0.27 | 92 | 86 | 0.33 |
| Increase in body mass | 26 | 24 | 19 | 0.72 | 30 | 23 | 0.14 |
| Excessive appetite | 5 | 4 | 4 | 0.82 | 7 | 5 | 0.33 |
| Dizziness | 73 | 60 | 63 | 0.16 | 77 | 66 | 0.10 |
| Loss of body mass | 18 | 12 | 15 | 0.40 | 16 | 18 | 0.66 |
| Insomnia | 41 | 33 | 41 | 0.30 | 47 | 34 | 0.05 |
| Hot flush | 53 | 41 | 37 | 0.08 | 53 | 49 | 0.31 |
| Palpitation | 91 | 86 | 81 | 0.26 | 93 | 87 | 0.26 |
| Anxiety | 79 | 74 | 74 | 0.52 | 83 | 74 | 0.14 |
| Syncope | 83 | 75 | 59 | < 0.01* | 84 | 81 | 0.03* |
*Statistical significance with p < 0.05. HF, heart failure.
Based on the ESC guidelines, we chose three main symptoms of HF, namely lower-limb oedema, dyspnoea and fatique, and checked how many respondents correctly indentified at least one of these.1 At least one sign of HF was correctly identified by 98% of the young group, 95% of the middle-aged group and 89% of the elderly group (p = 0.03).
To assess their awareness of characteristic symptoms of HF, an analysis was conducted among the group of people whose relatives suffer/do not suffer from HF. In both groups the most frequently distinguished symptoms of HF were: dyspnoea (96 vs 91%; p = 0.30) or fatigue (89 vs 85%; p = 0.08). In the group where respondents’ relatives suffered from HF, participants were much more convinced symptoms such as lower-limb oedema (91 vs 82%; p = 0.02), excessive thirst (30 vs 23%, p = 0.01), sweating (64 vs 51%, p = 0.01), cough (55 vs 45%; = 0.01) and syncope (84 vs 81%; p = 0.03) were related to HF (Table 2).
The majority of respondents stated that HF patients should not avoid physical activity (83 vs 83 vs 67%, respectively; p = 0.25), regardless of the age group, however a high percentage of them said they should avoid activity or did not have any idea on this issue. Half of the respondents in the elderly group indicated that HF patients may play sport, whereas the situation looked better in the younger groups (75 vs 69 vs 52%, respectively; p = 0.01) (Table 3).
Table 3. Awareness of physical activity and HF treatment by age group.
| Responses | Young (< 40 years), % (n) | Middle aged (40-65 years), % (n) | Elderly (> 65 years), % (n) | p-value |
| 'Should HF patients avoid | physical activity?' | 0.25 | ||
| Yes | 9 (36) | 8 (7) | 15 (4) | |
| No | 83 (315) | 83 (77) | 67 (18) | |
| Don't know | 8 (30) | 10 (9) | 19 (5) | |
| 'Can the HF patient play | sport?' | 0.01* | ||
| Yes | 75 (285) | 69 (64) | 52 (14) | |
| No | 14 (52) | 10 (9) | 22 (6) | |
| Don't know | 12 (44) | 22 (20) | 26 (7) | |
| 'What are the methods of | HF treatment?' | |||
| Heart surgery | 52 (200) | 47 (44) | 59 (16) | 0.79 |
| Stimulator | 62 (237) | 54 (50) | 44 (12) | 0.08 |
| Rest | 37 (141) | 35 (33) | 30 (8) | 0.73 |
| Physical activity | 57 (217) | 61 (57) | 48 (13) | 0.46 |
| Diet | 75 (284) | 77 (72) | 67 (18) | 0.53 |
| Pharmacotherapy | 82 (311) | 85 (79) | 81 (22) | 0.75 |
| Psychologist support | 18 (69) | 20 (19) | 26 (7) | 0.56 |
| No idea | 6 (21) | 9 (8) | 7 (2) | 0.52 |
*Statistical significance with p < 0.05. HF, heart failure.
Most of the respondents in each group pointed to pharmacotherapy as a method of treatment of HF. However, change of lifestyle, determined by physical activity (57, 61 and 48%, respectively; p = 0.46) and diet (75, 77 and 67%, respectively; p = 0.53) were much less often chosen. Other methods of treatment were less frequently chosen by respondents but the answers did not differ significantly between the age groups (Table 3).
The issue of physical activity was also studied in two groups of people: one group suffering from HF and the other not suffering from HF. Surprisingly, significantly more people suffering from HF claimed that physical activity should be avoided (p = 0.03) but in both groups, respondents believed that HF patients can play sport (p = 0.60) (Table 4).
Table 4. Awareness of physical activity by group of people suffering/not suffering from HF and relatives suffering/not suffering from HF.
| Responses | Respondent suffering from HF, % (n) | Resopndent not suffering from HF, % (n) p-value | Relatives suffering from HF, % (n) | Relatives not suffering from HF, % (n) | p-value |
| 'Should the | HF patient | avoid physical activity?' | |||
| Yes | 19 (6) | 8 (35) 0.03* | 4 (7) | 11 (30) | 0.01* |
| No | 81 (26) | 83 (343) | 91 (150) | 79 (221) | |
| No idea | 0 (0) | 9 (36) | 4 (7) | 10 (29) | |
| 'Can the HF | patient play | sport?' | |||
| Yes | 66 (21) | 73 (304) 0.60 | 79 (129) | 71 (200) | 0.02* |
| No | 16 (5) | 14 (56) | 10 (16) | 13 (36) | |
| No idea | 19 (6) | 13 (54) | 12 (19) | 16 (44) |
*Statistical significance with p < 0.05. HF, heart failure.
The analysis was also conducted in two groups of people whose relatives either suffered or did not suffer from HF. Relatives of HF patients indicated that HF patients should not avoid physical activity (p = 0.01) and may play sport (79%; p = 0.02) more frequently than those in the group in which relatives did not suffer from HF (Table 4).
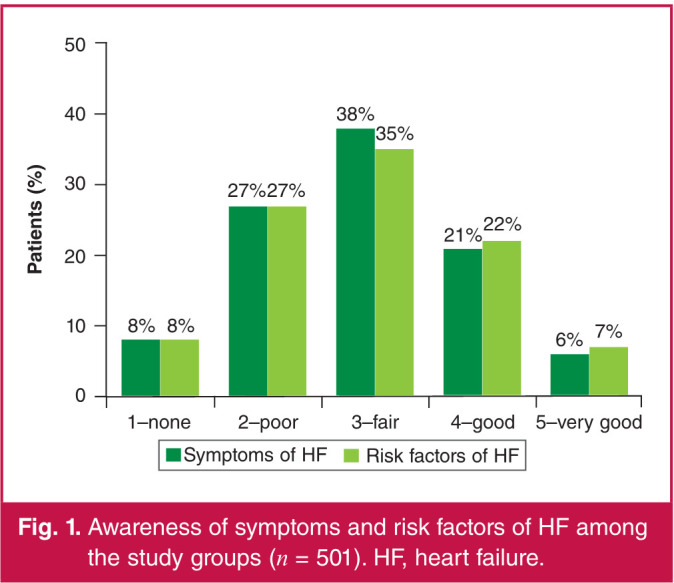
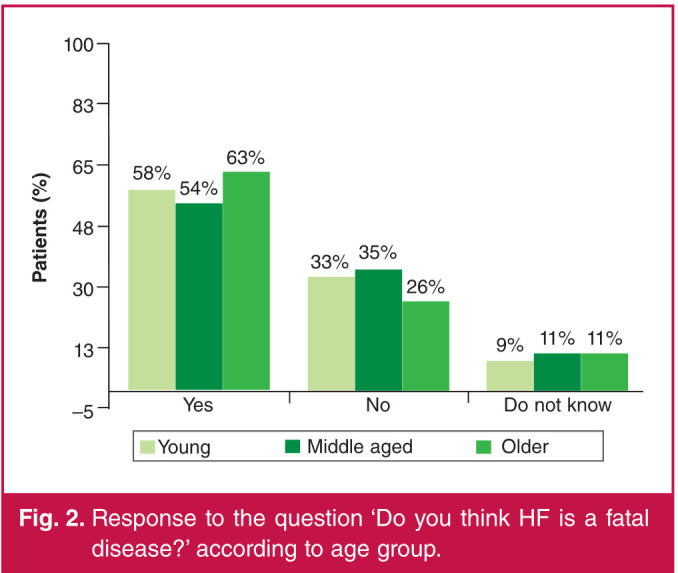
The majority of respondents who were analysed by age, considered HF a fatal disease and no significant difference was observed between the groups (58 vs 54 vs 63%, respectively; p = 0.89) (Fig. 2). Almost half of the participants (47%; p < 0.05) in the younger adult group believed HF to be incurable, whereas only about one-third or fewer (28%; p < 0.05) respondents in each group judged HF to be a curable disease (Fig. 3).
Fig. 2.
Response to the question ‘Do you think HF is a fatal disease?’ according to age group.
Fig. 3.
Response to the question ‘Do you think HF is curable?’ according to age group. *Statistical significance with p-value < 0.05
The most important risk factors for HF for all three age groups were: hypertension, nicotine addiction, obesity and stress. The older the respondents, the less frequently they pointed to excessive physical activity (p = 0.04) and renal disease (p = 0.01) as one of the risk factors for HF. The data were not consistent as to whether respondents’ gender influenced their opinions. Only 48% of elderly respondents referred to hypercholesterolaemia and 78% pointed to both stress and lack of physical activity (Table 5).
Table 5. Response to the question: ‘Do the following risk factors apply to HF?’ by age group and positive answers.
| Young (< 40 years), | Middle aged (40-65 | Elderly ( > 65 years), | ||
| Risk factors | % | years), % | % | p-value |
| Arterial hypertension | 91 | 91 | 85 | 0.30 |
| Thyroid diseases | 41 | 43 | 30 | 0.70 |
| Diabetes | 70 | 58 | 70 | 0.32 |
| Nicotine addiction | 84 | 87 | 89 | 0.90 |
| Obesity | 90 | 88 | 81 | 0.18 |
| Stress | 90 | 87 | 78 | 0.07 |
| Excessive physical activity | 31 | 24 | 15 | 0.04* |
| Female gender | 11 | 4 | 7 | 0.03* |
| Hypercholesterolaemia | 65 | 58 | 48 | 0.06 |
| Renal diseases | 39 | 32 | 26 | 0.01* |
| Alcohol abuse | 80 | 75 | 70 | 0.11 |
| Lack of physical activity | 88 | 84 | 78 | 0.16 |
| Neoplasm/tumour | 49 | 34 | 52 | 0.08 |
*Statistical significance with p < 0.05.
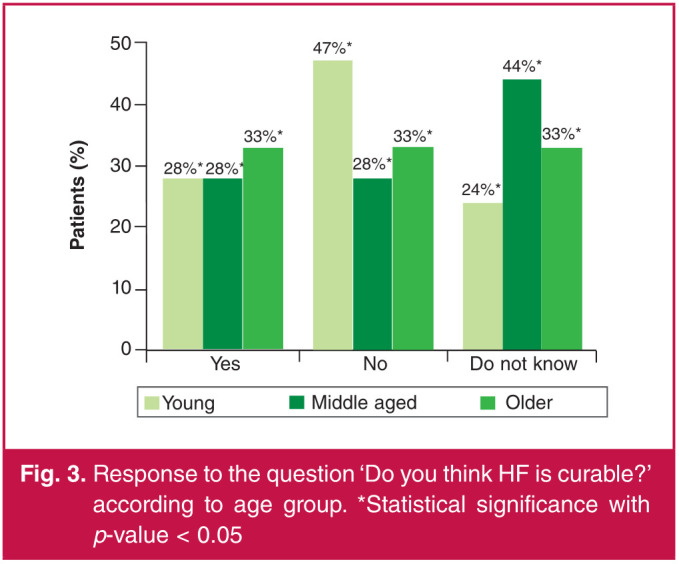
According to all three age groups of respondents, the most important source of information on diseases and healthy lifestyle was the internet. However, radio and television seemed to play a crucial role in elderly people, amounting to 44% of those respondents’ choices. On the other hand, in the middle-aged group, almost half of the respondents indicated specialists as their important source of information. Nevertheless, independent of age, the majority of people in each age group (77, 73, 78%, respectively; p = 0.21) stated that they felt they needed more information on disease and healthy lifestyle (Figs 4, 5).
Fig. 4.
Response to the question ‘What is the source of your knowledge about diseases and healthy lifestyle?’ according to age group. Statistically significant, p < 0.05.
Fig. 5.
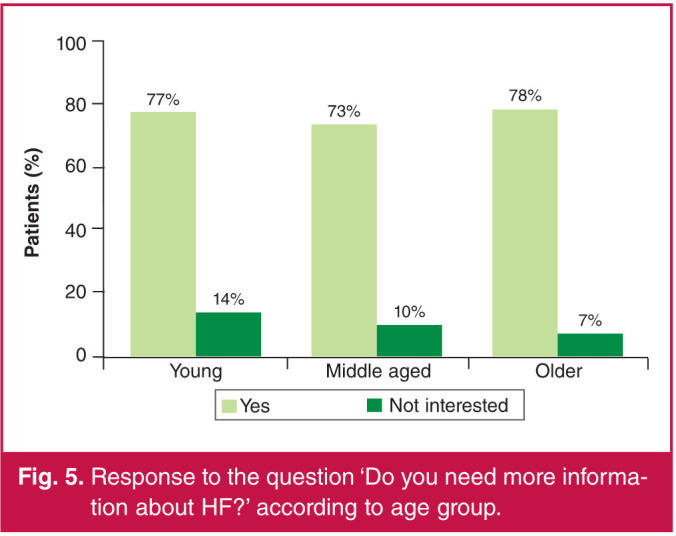
Response to the question ‘Do you need more information about HF?’ according to age group.
Discussion
In our study, we analysed knowledge of the general population on heart failure: risk factors, symptoms, treatment strategies and possible sources of information on this topic. The prevalence of HF is increasing and the prognosis of survival is similar to that of cancer.16 It is paramount then that public awareness on the issue be greater, which may contribute to more effective diagnosis and quicker implementation of the desired treatment, ultimately improving patient outcomes. Therefore, we decided to design a non-standardised survey in such a way that the subjects could freely choose which part of treatment and communication should be improved.
The population in our study consisted primarily of young individuals, with a mean age of 32 ± 14 years, most of whom were women (74%). In other surveys, respondents were older, with a mean age of 56 ± 15 years in the European Heart Failure Awareness Day 2011, and 58 ± 15 years in the Polish study.15,17 One of the factors influencing age distribution in our study may have been the fact that it was internet based, as opposed to a printed survey.
The majority of respondents had higher education (57%), 45% were in some way involved with the healthcare system, and only 6% reported suffering from HF.
The analysed study group reported a poor understanding of HF. Only 27% of respondents described their understanding of symptoms as good or very good. A similar result was shown with regard to risk factors for HF, where only 29% of participants described their understanding of the issue as good or very good. According to the SHAPE study from 2005, only 29% of respondents identified HF signs and symptoms as indicative of a severe condition.10
With regard to specific symptoms discussed in the survey, respondents in our survey indicated that as many as 84, 87 and 81%, respectively, of people in the given age groups correctly identified lower-limb oedema as a HF symptom (Table 2). These results are very different from those obtained during the HF Awareness Day in Poland in 2019, where only 50.6% of the Awareness Day participants and 32.2% of other participants indicated this symptom as indicative of HF.14 Similar results were obtained in a study from 2015 in Germany, Lithuania, Romania and Slovenia, where 52% of the respondents correctly identified lower-leg oedema as typical of HF and 31% indicated growing old as a reason for HF.18
Moreover, one of the characteristic symptoms of HF, dyspnoea, was indicated in our study by 94, 90 and 81%, respectively, for each age group (Table 2). In addition, fatigue, typical of HF, was indicated by 87, 75 and 70%, respectively (Table 2). Comparing this with the 2015 study in Germany, Lithuania, Romania and Slovenia, where almost 60% of the respondents were over 60 years of age, our study obtained a higher percentage of correct answers, particularly in the younger group of respondents.18 In the 2015 study, only 61% indicated fatigue as a typical symptom of HF, and dyspnoea was chosen by 71% of respondents.18 Analysing these results, we found a trend, where the older the age group, the smaller the percentage correctly indicated the typical symptoms of HF. Undoubtedly, the elderly group of people deserves appropriate education because they are particularly vulnerable to HF.
One important issue raised in our survey was physical activity and its avoidance by HF patients. In all the questioned groups (the three age groups, HF and non-HF patients, HF patients’ relatives and respondents without family members who were HF sufferers) the majority of respondents believed that patients should not abstain from physical activity. Looking at the negative or indecisive answers to the question whether HF patients should play sport, approximately one-third of respondents believed sport was not advisable or they did not know the answer to this question.
Despite the passage of years and increased efforts in education of the general public, awareness on this most elemental issue of disease prevention remains unchanged. This has been confirmed in the compilation of the results of our study, which are slightly better in this regard but still not satisfactory, compared with the 2005 study where 61% of people surveyed thought that HF patients needed to reduce their physical activity.10 Results obtained in the group of HF patients are especially surprising, where 37% of HF patients, when asked whether they thought they could play sport, responded negatively or indecisively.
This result is a clear indicator of insufficient awareness of the role physical activity plays for HF patients, which is a further testament to inadequate education in this group of patients.
Regarding choice of treatment method in the age groups assessed, we clearly saw a trend towards pharmacotherapy as typical for HF. These results are consistent with a 2006 study where as many as 90% of patients chose this treatment method.12 Physical activity or nutritional interventions were not perceived as primary treatment and prevention methods for HF in this population.
In recent years, internet availability has enabled better access to information. In our study, 80% of young people indicated the internet as their primary source of information on HF and healthy lifestyle (this source was the most frequently indicated one, regardless of age group). A similar trend was shown in a German study, which collected data concerning HF awareness between 2007 and 2015. Here too, 51% of young respondents indicated the internet to be their prime source of information.19
The older the respondents, the more willingly they learn from sources other than the internet. In the middle-aged group of respondents, a frequently chosen option was a consultation with a specialist. Elderly respondents, on the other hand, relied on the internet only in 63% of the cases, and television/radio in 44% of cases. In comparison with the German study, where the majority of elderly respondents indicated newspapers (69%) or information obtained in the doctor’s office (69%), the internet accounted for only 31%.19 These discrepancies may be the result of a difference in the survey format. Our study was an internet-based survey, so the responders were obviously familiar with the internet, whereas in the German study it was a paper-based survey.
An important conclusion drawn from our survey is the fact that almost 78% of respondents declared the need to gain more information on HF. This poses a great educational challenge for healthcare systems.
Conclusions
While the HF morbidity rate is surging, the level of understanding of HF remains low. The general public sees the need for more information and global education seems crucial in bettering the HF situation. It also needs to be clarified that HF cannot be cured. People should be educated about symptoms of HF, even though the majority indicated correct signs and symptoms as most alarming. It is important to encourage positive lifestyle changes, such as a proper diet and physical activity to improve the prognosis, lower re-admission rates and reduce HF care costs. Finally, various sources of information proliferation, particularly the internet, is crucial for every age group.
Acknowledgments
We thank all participants of our study for taking part and for distribution of our survey via the internet, especially Wojewódzki Szpital Zespolony w Lesznie.
Contributor Information
Marta Kałużna-Oleksy, Department of Cardiology I, Poznan University of Medical Sciences, Poznan, Poland.
Michał Wawrzyniak, Email: michalw.47@gmail.com, Department of Cardiology I, Poznan University of Medical Sciences, Poznan, Poland.
Monika Klimkowska, Department of Cardiology I, Poznan University of Medical Sciences, Poznan, Poland.
Magdalena Dudek, Department of Cardiology I, Poznan University of Medical Sciences, Poznan, Poland.
Jacek Migaj, Department of Cardiology I, Poznan University of Medical Sciences, Poznan, Poland.
Ewa Straburzyńska-Migaj, Department of Cardiology I, Poznan University of Medical Sciences, Poznan, Poland.
References
- 1.McDonagh TA, Metra M, Adamo M. et al. ESC Scientific Document group. 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: developed by the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) With the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2021;36:3599–3726. [Google Scholar]
- 2.Savarese G, Lund LH. Global public health burden of heart failure. Card Fail Rev. 2017;3(1):7–11 . doi: 10.15420/cfr.2016:25:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McKee PA, Castelli WP, McNamara PM, Kannel WB. The natural history of congestive heart failure: the Framingham study. N Engl J Med. 1971;285(26):1441–1446. doi: 10.1056/NEJM197112232852601. [DOI] [PubMed] [Google Scholar]
- 4.Mosterd A, Hoes AW. Clinical epidemiology of heart failure. Heart. 2007;93(9):1137–1146. doi: 10.1136/hrt.2003.025270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Levy D, Kenchaiah S, Larson MG. et al. Long-term trends in the incidence of and survival with heart failure. N Engl J Med. 2002;347:1397–1402. doi: 10.1056/NEJMoa020265. [DOI] [PubMed] [Google Scholar]
- 6.Cowie MR, Mosterd A, Wood DA. et al. The epidemiology of heart failure. Eur Heart J. 1997;18(2):208–225. doi: 10.1093/oxfordjournals.eurheartj.a015223. [DOI] [PubMed] [Google Scholar]
- 7.Cowie MR, Wood DA, Coats AJ. et al. Incidence and aetiology of heart failure; a population-based study. Eur Heart J. 1999;20(6):421–428. doi: 10.1053/euhj.1998.1280. [DOI] [PubMed] [Google Scholar]
- 8.McMurray JJ, Stewart S. The burden of heart failure. Heart J Suppl. 2002;4(Suppl D):D50–D58. [Google Scholar]
- 9.McMurray JJ, Stewart S. Epidemiology, aetiology, and prognosis of heart failure. Heart. 2000;83(5):596–602. doi: 10.1136/heart.83.5.596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Remme WJ, McMurray JJ, Rauch B. et al. Public awareness of heart failure in Europe: first results from shape. Eur Heart J. 2005;26(22):2413–2421. doi: 10.1093/eurheartj/ehi447. [DOI] [PubMed] [Google Scholar]
- 11.Rogers AE, Addington-Hall JM, Abery AJ. et al. Knowledge and communication difficulties for patients with chronic heart failure: qualitative study. Br Med J. 2000;321(7261):605–607. doi: 10.1136/bmj.321.7261.605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Van der Wal MH, Jaarsma T, Moser DK, Veeger NJ, van Gilst WH, van Veldhuisen DJ. Compliance in heart failure patients: the importance of knowledge and beliefs. Eur Heart J. 2006;27(4):434–440. doi: 10.1093/eurheartj/ehi603. [DOI] [PubMed] [Google Scholar]
- 13.Rogers A, Addington-Hall JM, McCoy AS. et al. A qualitative study of chronic heart failure patients’ understanding of their symptoms and drug therapy. Eur J Heart Fail. 2002;4(3):283–287. doi: 10.1016/s1388-9842(01)00213-6. [DOI] [PubMed] [Google Scholar]
- 14.Nowak K, Stępień K, Furczyńska P. et al. The awareness and knowledge about heart failure in Poland – lessons from the Heart Failure Awareness Day and internet surveys. Folia Med Cracov. 2019;59(2):93–109. [PubMed] [Google Scholar]
- 15.Lainscak M, Letonja M, Kovacic D. et al. General public awareness of heart failure: results of questionnaire survey during Heart Failure Awareness Day 2011. Arch Med Sci. 2014;10:355–360. doi: 10.5114/aoms.2014.42589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stewart S, MacIntyre K, Hole DJ, Capewell S, McMurray JJ. More ‘malignant’ than cancer? Five-year survival following a first admission for heart failure. Eur J Heart Fail. 2001;3(3):315–322. doi: 10.1016/s1388-9842(00)00141-0. [DOI] [PubMed] [Google Scholar]
- 17.Płotka A, Prokop E, Migaj J, Straburzyńska-Migaj E, Grajek S. Patients’ knowledge of heart failure and their perception of the disease. Patient Pref Adherence. 2017;11:1459–1467. doi: 10.2147/PPA.S126133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Störk S, Kavoliuniene A, Vinereanu D. et al. What does the lay public know about heart failure? Findings from the Heart Failure Awareness Day Initiative . J Heart Fail. 2016;18(1):66–70. doi: 10.1002/ejhf.425. [DOI] [PubMed] [Google Scholar]
- 19.Zelenak C, Radenovic S, Musial-Bright L. et al. Heart failure awareness survey in Germany: general knowledge on heart failure remains poor. ESC Heart Fail. 2017;4(3):224–231. doi: 10.1002/ehf2.12144. [DOI] [PMC free article] [PubMed] [Google Scholar]