Abstract
Head and neck cancer is a rare disease and general dental practitioners (GDPs) are at the forefront of head and neck assessment for malignancy in the community. Having an awareness of the signs and symptoms with which head and neck cancers can present promotes earlier diagnosis and increases the potential for better prognosis and quality of life. This article will outline the head and neck cancer pathway from presentation, diagnosis and management planning, to treatment and beyond. This should help to give GDPs insight into the process their patients will experience while under the care of the multidisciplinary team and enable them to give patients returning to primary care the best support. This article is part of a larger series that will explore each facet of care in greater detail to give a significantly greater understanding of the pathway.
Key points
Head and neck cancer includes a range of malignancies and general dental practitioners provide an essential role in early detection to save lives and prevent significant morbidity.
Symptoms of head and neck cancer can be vague but a high index of suspicion should be maintained for patients who have had symptoms for more than a few weeks, with progressive features and without variability.
Standardised pathways exist for diagnosis, staging and multidisciplinary, evidence-based management, all centred around patient preferences.
Introduction
Head and neck cancer (HNC) is a group of epithelial malignancies involving the upper shared respiratory/digestive tract (lips, oral cavity, oropharynx, nasal cavity, nasopharynx, hypopharynx and larynx/upper trachea), the salivary glands and lymphadenopathy associated with these diseases. Cancers of the skin in the head and neck, mucosal melanomas, sarcoma, solid haematologic tumours (lymphoma) and malignancies of the thyroid gland, eye, brain and skull base are usually managed by separate multidisciplinary team (MDT) structures, although the HNC team may be involved in diagnosis and therapy.
Early interventions in primary care
HNC is common and estimated to account for 3% of cancer diagnoses in the UK per year, at approximately 12,500 cases annually or around 34 new diagnoses per day.1 The disease is often detected at late stages of tumour progression, as attribution of HNC symptoms (which are vague and undifferentiated) to transient conditions is common, causing delayed referral to specialist services. Both primary medical and dental practitioners are essential to early diagnosis but the training medical students receive on the subject at undergraduate level is limited. Medical practitioners in the UK, on average, receive 8.5 days of ear, nose and throat (ENT) teaching,2 which includes elements of HNC. This may be the only training they have in their careers without any fixed requirement for further continuing professional development (CPD) in this area. Dental practitioners have more training with greater exposure to HNC in both the preclinical and clinical phases of training, with regular attendance at oral and dental clinics. Additionally, dental practitioners are required to maintain evidence of active CPD in this specific area for revalidation purposes. Dental training unsurprisingly focuses on the oral cavity aspects of HNC, with limited exposure or training in other areas of head and neck malignancy, such as skin cancer. Dentists assess large volumes of the population every year (39.7 million treatments 2018-2019) and, as part of the Make Every Contact Count agenda,3 are ideally placed to encourage preventative behavioural modification (smoking cessation, alcohol reduction) and to identify red flag signs and symptoms that would warrant early specialist review. Dentists make an enormous contribution to the identification and ongoing management of head and neck patients and with further training in the non-oral cavity aspects of HNC, such as ENT and dermatology, could make an even greater contribution to the early diagnosis and treatment of these patients, saving lives and reducing morbidity.
Suspicious signs and symptoms: referral to specialist HNC services
GDPs should be mindful of the possibility of cancers in other head and neck sites besides the oral cavity and oropharynx when carrying out routine examination. Possible signs and symptoms associated with HNC in different subsites are covered in other articles in this themed issue and are briefly listed in Table 1.
Table 1.
Possible signs and symptoms of malignancy at different head and neck cancer subsites
| Site | Possible symptoms/signs |
|---|---|
| Oropharynx | New onset tonsil asymmetry, bleeding tonsil, unexplained blood-stained saliva, otalgia, dysarthria, neck lump |
| Nose/nasopharynx | Progressive nasal obstruction, unilateral hearing loss, unilateral epistaxis, infraorbital numbness without trauma, unexplained maxillary dental pain, malodour, new nasal speech, neck lumps |
| Larynx | Hoarse voice, breathing difficulty, coughing and choking while eating, haemoptysis |
| Hypopharynx/upper oesophagus | Progressive dysphagia to solids, neck lumps |
| Oral cavity | Persistent ulcer, speckled leukoplakia, loss of function, unexplained tooth mobility |
| Salivary glands | Unexplained unilateral swelling, paraesthesia, facial palsy, trismus, rapid increase in size of long-standing swelling |
Oral cavity tumours are typically asymptomatic and may present as persistent ulceration of greater than three weeks' duration, associated with leukoplakia (white patch), erythroplakia (red patch) or speckled leukoplakia (mixed red/white patch). Common sites include the lower lip, lateral border of tongue, floor of the mouth and retromolar region and such findings require a suspected cancer referral to oral and maxillofacial surgery for assessment.
Non-oral cavity types and sites of head and neck malignancy often have vague symptoms and few clear visible signs until late in the disease process, resulting in delayed referral while treatment of other possible diagnoses is explored. It is essential that a high index of suspicion is maintained when symptoms have been present for more than three weeks, are constant and are progressing in severity. If the situation is not typical, it is imperative that the possibility of a malignant process is considered and, if necessary, a specialist referral should be made. Linking features of red flag symptoms of HNC with the more generic red flags for malignancy (duration, consistency and progression) are key to rapid referral to specialist services. In general dental practice, neck examination (including skin) and oral cavity inspection are routinely performed and practitioners are familiar with referral to an oral and maxillofacial or ENT team for assessment via the two-week wait (TWW) pathway for patients presenting in this manner. In some areas of the UK, for those patients presenting with a neck lump alone, service provisions exist for direct referral into an urgent suspected cancer (USC) neck lump scanning service, to further reduce waiting time. If this is not available locally, then the GDP should refer to oral and maxillofacial surgery (OMFS) or ENT teams.
Beyond the oral cavity, directly visible oropharynx and neck lump assessments, the remainder of the combined upper airway digestive tract is not accessible for review by the GDP and therefore it is sometimes a high index of suspicion and awareness of the key red flag symptoms that will highlight to a practitioner the possibility of malignancy. Although there is some overlap in symptoms, especially as the primary tumour enlarges, clinicians can link sites to specific issues (Table 1). On clinical examination, it is important to examine the neck of all patients and on oral examination, assess the oropharynx as asymmetrical tonsil enlargement may be the first sign of a malignant process. Further details on early detection of HNC is provided in another paper in this edition.
The British Association of Head and Neck Oncologists (BAHNO) is a multidisciplinary professional group which includes representation of all core MDT member specialties. The organisation speaks for the interests of HNC clinicians and champions patient groups and charitable organisations dedicated to this disease process in the UK. The 2020 BAHNO standards4 set out standards for the process of HNC care.
In terms of referral, with reference to the BAHNO standards,4 lip and oral cavity cancers should go to OMFS and those suspicious of nasal, nasopharynx, oropharynx, larynx, hypopharynx/upper oesophagus and thyroid cancers should go to ENT. Salivary lumps can be sent for urgent assessment to OMFS or ENT. This is also the case for suspicious cervical lymphadenopathy with unknown primary tumours but in this situation, referral to ENT is preferred due to the availability and expert use of flexible nasendoscopy to assess additional upper respiratory tract sites. Referrals should adhere to national and local guidance via the TWW pathway and should contain sufficient detail to allow for triage into the most appropriate clinic.
Assessment in specialist services
Once a referral has been received by the specialist cancer services, a clinician will assess the merits of the case. The referral should include as much information as possible to prevent an erroneous priority being designated. If accepted, the patient will be seen, as per guidance, in the TWW pathway. The clinician has three other options: 1) downgrade the priority if they feel there is sufficient evidence to remove the suspicion of a malignant process; 2) ask for more information if there isn't enough clinical detail to make an adequate review of the referral; and 3) return the referral if they feel it is inappropriate for their service. If returned, there may be advice/information on the reasons for this and treatment options that should be considered or suggestions of more appropriate referral pathways. Since COVID-19, many specialist services virtually assess USC patient referrals using validated risk assessment tools to prevent overbooking of TWW slots.5
First appointment at a specialist team
When seen in the specialist outpatient clinic, a thorough history and examination will be repeated. Typically, the outpatient examination will include visual assessment of the oral cavity and in ENT clinics, a flexible nasoendoscopic assessment of the nasal cavity, pharynx (naso/oro/laryngo/hypo) and larynx (and oesophagus at centres where transnasal oesophagoscopy facilities are available); this is to assess areas of concern not visible on routine examination. Assessment also excludes synchronous primary tumours6 of the head and neck due to issues such as field cancerisation by carcinogen exposure7 and identifies subclinical primaries usually related to human papillomavirus (HPV)-related cancers.8 Meta-analysis of research into synchronous tumours have suggested rates of 13.2% in HNC.9 After this assessment, several options exist dependent on the clinical scenario:
Primary site identified - if a primary site of malignancy has been identified, imaging to review the extent of the disease would occur before pathological confirmation due to the risks of surgical trauma confounding accurate radiological assessment of the situation (see below). Following radiological evaluation, a surgical biopsy would be performed under local or general anaesthetic to confirm the pathological diagnosis but also to evaluate the potential for surgical excision and what any procedure would entail
No primary site identified but suspicious lymphadenopathy - if no primary site is identified, definitive pathological diagnosis is made from the nodal tissue via ultrasound-guided core biopsy. Synchronously, cross-sectional imaging of the head, neck and chest would be undertaken to evaluate for primary sites
Malignancy found on core biopsy - if the histological specimen from the node is positive for malignancy but a primary site not identified radiologically, positron emission tomography (PET) is used to evaluate for a hidden primary site. Histopathology assessment for HPV using a surrogate marker (p16), is useful to identify whether the oropharynx is the most likely primary site and Epstein-Barr virus for a nasopharyngeal origin. If PET does not reveal the primary site, a panendoscopy including tonsillectomy ± mucosectomy of the tongue base would be considered
Malignancy not found on core biopsy - if the core specimen is negative twice and no primary site can be identified on cross-sectional imaging, definitive diagnosis of the node is required. This requires excision of the node and histological assessment with frozen sections. If frozen sections identify a tumour, a complete neck dissection is undertaken at the same surgical event.
Once a HNC is identified, discussion at the MDT meeting ensues. If not already performed, a thorough radiological workup to assess local and distant extent of disease is commenced. Typically, the primary tumour is assessed with cross-sectional imaging using either an MRI or CT scan, dependent on the need for soft tissue or bony assessment.10,11 The neck is staged with ultrasound scans as this is more specific for malignant disease within the cervical lymph nodes than all other imaging modalities.10,11 The chest, the most common site of distant metastatic head and neck cancer, is typically assessed with a CT scan. An orthopantomogram is essential as surgical or non-surgical cancer treatment may impact the oral cavity. Occasionally, PET scanning will occur at this stage for assessment of - especially when surgical intervention with high morbidity is being considered - the presence of distant metastasis.
Tumour classification: TNM8
Staging of tumours helps to predict prognosis as well as treatment in populations and is based on the TNM system, developed by the American Joint Committee on Cancer and the International Union Against Cancer and includes three parts: T (tumour); N (lymph nodes); and M (distant metastases), followed by a number with increasing value denoting later stage of disease presentation. Staging can be clinical and radiological (cTNM) or pathological (pTNM), with the later most accurate. Increasing T-stage corresponds with tumour size, depth of invasion and extent of involvement of adjacent structures.12 Although pathological staging is considered the gold standard, advances in radiotherapy and chemotherapy for oropharyngeal tumours have led to similar prognostic outcomes as patients treated surgically and staging for these tumours tends to be clinical.
Informing patients and breaking bad news
Prior to the MDT meeting, it is essential that the patient is informed of the cancer diagnosis so that they can fully engage with the decision-making process and the choices they face in relation to management.11 The meeting should be private and involve a clinical member of the MDT, the clinical nurse specialist (CNS) and the patient. The patient will be encouraged to bring a supportive person with them. The meeting allows information about the diagnosis, the likely stage/severity of disease and the potential treatment options to be outlined to the patient, allowing them to better engage in a prepared manner, with the MDT outcomes. The meeting also allows the transfer of patient information and assessment of other needs beyond the cancer diagnosis.
The MDT role and representatives
All patients diagnosed with HNC are managed within an MDT framework and work according to National Institute for Health and Care Excellence guidance10,13 and BAHNO standards.4 The MDT includes many specialist representatives to allow a holistic review of the patient and their needs before and during treatment and recovery (Table 2). The MDT meets weekly and new patients, as well as those who have recently completed treatment, are discussed. For every new patient, the lesion is defined and staged based on pathological and radiological findings. Using this information, the team will discuss and agree on the answers to basic questions: what is the best method of treating the disease in relation to the general health of this patient and is the proposed treatment curative or palliative? What additional physical, nutritional, psychological or social therapy/management will the patient require before treatment and as a consequence of the disease and its management? What options are present to restore appearance and function and reduce morbidity following treatment?
Table 2.
The multidisciplinary team4
| Specialist | Role |
|---|---|
| MDT coordinator/data manager | The coordinator organises the MDT meeting and collates all the information required for each of the patients presented is available to allow the MDT to make treatment decisions. They take a record of the outcome and plans made and upload these to the central HNC dataset. Some aspects of the data will be audited as part of quality performance indicating programmes run by local cancer networks, as well as being held on National Cancer registries and audits |
| Clinical nurse specialist (CNS) | The CNS plays an essential role in coordinating care and psychosocial support for the patient and are often the first to identify the non-clinical needs of patients. The CNS is the first contact for the patient in the head and neck team. The CNS requires excellent communication and support skills, often clarifying situations and outlining care to patients and their families. In the MDT meeting, the CNS outlines patient and family preferences and concerns |
| Speech and language therapist (SLT) | The SLT plays an essential role in the voice, speech and swallowing issues associated with HNC and the consequences of its treatment. In the MDT meeting the SLT highlights likely voice and swallowing outcomes and potential impacts of proposed therapies. Following treatment, the SLT works with patients to recover as much function as possible to return to normal diet and normal voice |
| Dietitian | The dietitian has an essential role ensuring patients are nourished before and during treatment and that weight (and dietary requirements) are maintained in the follow-up setting. In the MDT, meeting the dietitian, in association with SLT, may advocate adjuvant feeding therapies (nasogastric tubes/percutaneous endoscopic gastrostomy tubes) dependent on treatment plans |
| Specialist restorative dentist | The consultant in restorative dentistry plays an essential role in evaluating and managing the impact of cancer treatment on the patient's oral and dental appearance and function. This will include planning for primary implants to be placed at the same time as cancer resection where indicated and carrying out oral prehabilitation, including dental extractions, where indicated, for those receiving radiotherapy where osteoradionecrosis is a risk. Following treatment, the restorative dentistry consultant may carry out any specialist prosthodontic rehabilitation needed, including complex implants beyond the scope of primary dental care services. The restorative dentist should have contact with the primary care dental team |
| Pathologist | The pathologist in the pre-treatment process will give the diagnosis along with grade of tumour and may be able to describe potential adverse features. Following a surgical resection, the pathologist will give tumour dimensions and margins (described below) and describe adverse features (including neural and vascular invasion) that may indicate the need for additional therapy |
| Radiologist | The radiologist provides information on the size and stage of the primary site, nodal disease and evidence of metastatic spread to enable assessment of viable treatment options. Post treatment, the radiologist evaluates for residual disease or recurrence to allow further planning if necessary |
| Head and neck surgeon | The head and neck surgeon is from an ENT or OMFS background and will present the patient to the MDT. They will review the information provided and give their impression of the options available in terms of treatment and the nature of that treatment. This will be agreed by the MDT. The surgeon will discuss what surgical intervention would entail so that the allied specialties and restorative dentists can assess what additional therapy/intervention is needed |
| Oncologist | The head and neck oncologist will review the information and give their impression of the options available in terms of treatment and the nature of that treatment. The oncologist will discuss what non-surgical therapy would entail so that the allied specialties can assess what additional therapy/intervention is needed |
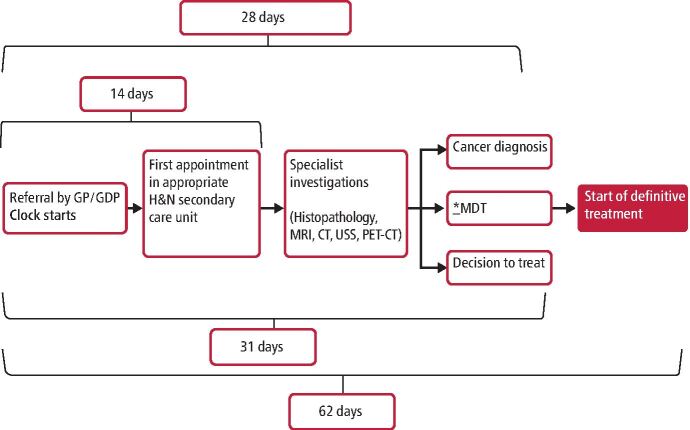
At the end of a new patient discussion, the MDT will formulate a treatment plan for the disease (surgical, non-surgical, combined modality or supportive care), the intent of that treatment (curative or palliative), the additional therapies required initially and long term (for example, percutaneous endoscopic gastrostomy feeding, nutritional support, speech and/or voice restoration, swallow therapy) and the need for a restorative dentistry plan to consider any future issues for long-term oral and dental care (for example, dental implants, oral prosthesis, dental extractions). A surgical/oncology member of the MDT will then discuss the preferred treatment options with the patient, clarifying any areas of uncertainty. The outcome of the MDT discussion is presented to the patient with further information relating to the benefits and risks, associated morbidity and the relative chance of success. Shared decision-making allows the patient to evaluate the proposed 'best option' and explore alternative treatment options if they are uncertain. Treatment must commence within 62 days from the date of referral (Fig. 1).
Fig. 1.
Key timeline targets following fast track (TWW) referral (note: MDT = multidisciplinary team), reproduced with permission from Peter Glen and Etienne Botha
Post-treatment MDT review
Following cancer treatment, the initial post-treatment review assesses the effect of treatment. In surgical cases this requires a pathological evaluation of the surgical specimen to define prognosis and the need for adjuvant treatment. Prognostic information in pathology reports include: site and subsite, type and grade of carcinoma, growth pattern, maximum diameter, depth of invasion, presence of vascular and perineural invasion, involvement of bone (mandible/maxilla) or cartilage (larynx) and status of surgical margins. For oral cavity cancers, resection margins >5 mm from the surgical margin are considered clear, those 1-5 mm close, and <1 mm as involved. This varies in other parts of the head and neck where 1 mm for transoral laser microsurgical resection of vocal cord cancers and 3 mm for transoral robotic resections of tonsil cancers could be considered appropriate. Neck dissection reports include the total number of nodes per level, number of positive nodes per level, size of largest metastasis and the presence or absence of extranodal spread (where tumour breaches the node and invades adjacent tissue of the neck). Pathology findings in combination with clinical and radiological features are used to determine the need for adjuvant therapy.
When patients have been treated non-surgically, initial post-treatment assessment involves clinical examination and one post treatment scan, usually at 12 weeks after the final radiotherapy fraction. If residual tumour or unexplained tissue remains, further clinical assessment and biopsy may be required for treatment planning.
Follow-up
Follow up of patients with HNC is essential to firstly identify the presence of residual or recurrent disease early where, potentially, treatment options may exist but also to assess, manage and improve the early and late onset morbidity associated with the treatment of these cancers. Follow-up regimes follow National guidelines14and typically require face-to-face assessments for the first 3-5 years. Early in the follow-up pathway, appointments are more frequent and 1-2 months apart, as the risk of recurrence is higher. Later in the pathway, the appointment interval becomes longer due to reducing risk of recurrent disease and the reduction in morbidity evolution. Although it is common for patients to be discharged from HNC clinics following cessation of the follow-up pathway, there is a growing trend to allow patients access to specialist care at its end via patient-initiated follow-up pathways (PIFU).15 PIFU, in this context, gives patients confidence that, if required, they can get seen rapidly by the head and neck team rather than trouble primary care teams. From a primary care standpoint, regular check-ups to identify areas suspicious of recurrence or identify treatment related morbidity amenable to intervention is an essential part of lifelong care.
Summary
HNC is a rare disease and GDPs are at the forefront of assessment for malignancy in the community. Being aware of the signs and symptoms, the red flags associated with these and by maintaining a high index of suspicion, patients with early stage HNC can be treated rapidly with better prognosis. This article has outlined the HNC pathway from presentation, diagnosis and management planning to treatment and beyond. This should offer GDPs a deeper understanding of the process their patients experience while under the care of the MDT and enable them to give their patients returning to primary care the best support. This article is part of a larger series that will explore each facet of care in greater detail to give a significantly greater understanding of the situation.
Author contributions
Vinidh Paleri, Adam V. Jones and David Owens all made contributions to the initial manuscript and literature search and were also involved in the review and amendment process.
Ethics declaration
The authors declare no conflicts of interest.
References
- 1.Cancer Research UK. Head and neck cancers statistics. Available at https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/head-and-neck-cancers#heading-Zero (accessed June 2022).
- 2.Powell J, Cooles F A H, Carrie S, Paleri V. Is undergraduate medical education working for ENT surgery? A survey of UK medical school graduates. J Laryngol Otol 2011; 125: 896-905. [DOI] [PubMed]
- 3.Public Health England. Making Every Contact Count (MECC): Consensus statement. 2016. Available at https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/769486/Making_Every_Contact_Count_Consensus_Statement.pdf (accessed October 2022).
- 4.British Association of Head and Neck Oncologists. Publications: BAHNO standards 2020. 2020. Available at https://bahno.org.uk/clinicians_area/publications.aspx (accessed June 2022).
- 5.Hardman J C, Tikka T, Paleri V, ENT UK, BAHNO and INTEGRATE (The UK ENT Trainee Research Network). Remote triage incorporating symptom-based risk stratification for suspected head and neck cancer referrals: A prospective population-based study. Cancer 2021; 127: 4177-4189. [DOI] [PMC free article] [PubMed]
- 6.Jain K S, Sikora A G, Baxi S S, Morris L G T. Synchronous cancers in patients with head and neck cancer: risks in the era of human papillomavirus-associated oropharyngeal cancer. Cancer 2013; 119: 1832-1837. [DOI] [PubMed]
- 7.Waridel F, Estreicher A, Bron L et al. Field cancerisation and polyclonal p53 mutation in the upper aero-digestive tract. Oncogene 1997 14: 163-169. [DOI] [PubMed]
- 8.Olivero C, Lanfredini S, Borgogna C, Gariglio M, Patel G K. HPV-Induced Field Cancerisation: Transformation of Adult Tissue Stem Cell Into Cancer Stem Cell. Front Microbiol 2018; 9: 546. [DOI] [PMC free article] [PubMed]
- 9.Coca-Pelaz A, Rodrigo J P, Suárez C et al. The risk of second primary tumours in head and neck cancer: A systematic review. Head Neck 2020; 42: 456-466. [DOI] [PubMed]
- 10.National Institute for Health and Care Excellence. Improving outcomes in head and neck cancers. 2004. Available at https://www.nice.org.uk/guidance/csg6 (accessed October 2022).
- 11.Paleri V, Roland N. Introduction to the United Kingdom National Multidisciplinary Guidelines for Head and Neck Cancer. J Laryngol Otol 2016; DOI: 10.1017/S0022215116000359. [DOI] [PMC free article] [PubMed]
- 12.Brierley J D, Gospodarowicz M K, Wittekind C. TNM Classification of Malignant Tumours. 8th ed. New Jersey: Wiley-Blackwell, 2018.
- 13.National Institute for Health and Care Excellence. Cancer of the upper aerodigestive tract: assessment and management in people aged 16 and over. 2016. Available at https://www.nice.org.uk/guidance/ng36 (accessed October 2022). [PubMed]
- 14.Kawecki A, Krajewski R. Follow-up in patients treated for head and neck cancer. Memo 2014; 7: 87-91. [DOI] [PMC free article] [PubMed]
- 15.Lorenc A, Wells M, Fulton-Lieuw T et al. Clinicians' Views of Patient-initiated Follow-up in Head and Neck Cancer: a Qualitative Study to Inform the PETNECK2 Trial. Clin Oncol (R Coll Radiol) 2022; 34: 230-240. [DOI] [PMC free article] [PubMed]