Abstract
Background
Gestational diabetes mellitus (GDM) is one of the most common medical complications during pregnancy. eHealth technologies are proving to be successful in supporting the self-management of medical conditions. Digital technologies have the potential to improve GDM self-management.
Objective
The primary objective of this systematic literature review was to identify the views of health professionals (HPs) and women with GDM regarding the use of eHealth for GDM self-management. The secondary objective was to investigate the usability and user satisfaction levels when using these technologies.
Methods
Following the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) approach, the search included primary papers in English on the evaluation of technology to support self-management of GDM from January 2008 to September 2021 using MEDLINE, CINAHL, Embase, ACM, and IEEE databases. The lists of references from previous systematic literature reviews, which were related to technology and GDM, were also examined for primary studies. Papers with qualitative, quantitative, and mixed methodologies were included and evaluated. The selected papers were assessed for quality using the Cochrane Collaboration tool, National Institute for Health and Care Excellence clinical guidelines, Critical Appraisal Skills Programme Qualitative Checklist, and McGill University Mixed Methods Appraisal Tool. NVivo (QSR International) was used to extract qualitative data, which were subjected to thematic analysis. Narrative synthesis was used to analyze the quantitative data.
Results
A total of 26 papers were included in the review. Of these, 19% (5/26) of studies used quantitative research methodologies, 19% (5/26) used qualitative methods, and 62% (16/26) used mixed methods. In all, 4 themes were identified from the qualitative data: the benefits of using technology, engagement with people via technology, the usability of technology, and discouragement factors for the use of technology. The thematic analysis revealed a vast scope of challenges and facilitators in the use of GDM self-management systems. The challenges included usability aspects of the system, technical problems, data privacy, lack of emotional support, the accuracy of reported data, and adoption of the system by HPs. Convenience, improved GDM self-management, peer support, increased motivation, increased independence, and consistent monitoring were facilitators to use these technologies. Quantitative data showed that there is potential for improving the usability of the GDM self-management systems. It also showed that convenience, usefulness, increasing motivation for GDM self-management, helping with GDM self-management, and being monitored by HPs were facilitators to use the GDM self-management systems.
Conclusions
This novel systematic literature review shows that HPs and women with GDM encountered some challenges in using GDM self-management systems. The usability of GDM systems was the primary challenge derived from qualitative and quantitative results, with convenience, consistent monitoring, and optimization of GDM self-management emerging as important facilitators.
Keywords: gestational diabetes mellitus, GDM, gestational diabetes, self-management, eHealth
Introduction
Background
Gestational diabetes mellitus (GDM) is defined as any degree of carbohydrate intolerance with onset or first recognition during pregnancy [1]. GDM is one of the most common medical complications of pregnancy [2], with a significant increase in its prevalence in different ethnic groups and countries over the last several years [3,4]. GDM is most prevalent in the Middle East and North Africa, with an estimated median of 12.9%, and least prevalent in Europe, with an estimated median of 5.8% of all pregnancies [5]. In the United Kingdom, the prevalence of GDM is approximately 4% of all pregnancies [6]. The rate of GDM is likely to rise owing to a growth in GDM risk factors, such as greater prevalence of maternal obesity and advancing age of childbearing [7], leading to an increasing demand for GDM clinical services [8].
GDM is associated with serious maternal [9-11] and fetal complications [12-15]. Mothers who have been affected by GDM are also at risk of developing type 2 diabetes [16] and cardiometabolic disorders later in life [17], and their infants are more at risk of developing adulthood obesity and type 2 diabetes [12,18]. These complications represent significant health problems and cost [19] for health services. The risk of adverse effects of GDM can be minimized by good control over maternal blood glucose (BG), diet, and physical activities [20]. However, there is limited time between diagnosis and delivery to optimize care for women with GDM [21]. Therefore, regular clinic visits [22] to a multidisciplinary team are advised to provide care during pregnancy. Nonetheless, traveling to specialist clinics in central locations [23] is expensive [24], time consuming, and inconvenient for women [25]. Recently, there has been an increase in the use of technology to enable self-management of GDM by women and to shift GDM management away from hospital-based care [26].
In light of increased adoption of technology to access information and communication, a digital GDM self-management system might offer advantages such as reducing patient travel and waiting time [27], saving medical practitioner time [8], reducing costs [28,29] to both the health care system and patients, greater convenience [30], attainment of better pregnancy outcomes [31], and an increased feeling of self-efficacy [32]. This can further lead to better BG control [29,33] and a decrease in GDM complications owing to greater accuracy and more frequent monitoring [34]. Such outcomes are evident in the results of several studies, which have found that health care technology can be beneficial for women with GDM in the improvement of hemoglobin A1c [35-37], mean BG [21,38-40], maternal weight [41], and maternal and fetal outcomes [38,42,43]. Technology could also offer high-quality remote health care in a critical situation such as the COVID-19 pandemic to women with GDM, where travel and in-person contact have been severely restricted [44,45]. Therefore, there is an urgent need to consider computer-based communication technologies for the management of diabetes. This could contribute to better diabetes management by improving patient knowledge, attitudes, skills, lifestyle behavior [46], quality of care, and access to care [29].
Study Aims
Digital GDM self-management systems developed in recent years are available mostly as mobile apps or websites [8,30,34] and offer a wide range of features such as monitoring BG [23], diet, physical activity, blood pressure, and ketonuria [8] for women with GDM. However, a recent study by Kalhori et al [47] suggests that the few GDM apps available in popular app stores are poor in quality, using the Mobile App Rating Scale as a basis for this result [47].
Furthermore, most GDM self-management systems are not widely used [48,49], and some are no longer supported [8,50], one reason for which is obsolete hardware (ML Bartholomew, MD, email communication, 2018). Previous systematic reviews in the scope of technology and GDM management were carried out on available technology for GDM self-management [47,51-53], the impact of technology on clinical and pregnancy outcomes or GDM management [54-56], comparing women’s clinical outcomes using technology with standard care [35], and the psychological aspect of using technology [57]. However, to the best of our knowledge, there is no systematic literature review of the opinions of health care professionals and women with GDM about using technology for GDM self-management.
The primary aim of this systematic literature review was to identify the views of health professionals (HPs) and women with GDM regarding barriers and facilitators of using technology for GDM self-management. The secondary aim was to investigate the usability and user satisfaction of these technologies.
Methods
Approach
The search strategy was developed by following the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) approach [58] with the help of a professional librarian. The PRISMA guidelines lead to standardized reports and enhance the clarity of systematic literature reviews [59].
Criteria of Inclusion and Exclusion
To achieve the aims of this review, the criteria for inclusion and exclusion were developed as presented in Textbox 1.
Inclusion and exclusion criteria.
Inclusion criteria
Views of health care professionals, pregnant women diagnosed with gestational diabetes mellitus (GDM) or postpartum women with a history of GDM about their pregnancy period
Technology (eHealth or telemedicine being used, evaluated, reviewed, or discussed by participants) or usability evaluation or reports of user satisfaction levels
Any primary research studies
Aspects of GDM management (eg, blood glucose control, diet, weight, physical activity, medication adherence, or information)
Exclusion criteria
Published papers written in any language other than English
Women with preexisting type 1 and type 2 diabetes (except papers that provide information about GDM distinct from type 1 and 2 diabetes)
Any nondigital technology
Papers published before 2008
Posters, abstracts, and news items
Systematic literature reviews
Usability results for task performance
Search Strategy and Screening Process
A search was carried out using 3 search terms—“self-management,” “gestational diabetes,” and “technology” (Multimedia Appendix 1). The search terms were identified from papers in eHealth for GDM in the PubMed database.
The search included publications written in English from January 2008 to September 2021 in the MEDLINE, CINAHL, Embase, ACM, and IEEE databases. This date limitation was chosen to represent contemporary technology for GDM self-management.
The screening process was conducted by the first author in line with previous studies [60,61] and with the help of the research team and a professional librarian using the following steps:
Identification: the results of the search from different databases were exported to the EndNote X7 software. Furthermore, the reference lists of previous systematic literature reviews related to technology and GDM were examined in the primary studies. All citations were collated into one group and duplicate records were removed.
Screening: the titles and abstracts of the remaining citations were screened based on the inclusion and exclusion criteria to select potential papers by the first author. At this stage, 2 other members of the research team independently conducted a double screening of the first 10% of the results. Following a discussion phase, this screening process was repeated to ensure reliability based on inclusion and exclusion criteria.
Eligibility: Mendeley software was used to keep electronic copies of the full text of potential papers. The full text of the papers was assessed based on the inclusion and exclusion criteria.
Included: the final papers were selected from the full text based on the inclusion and exclusion criteria by the first author. The papers were discussed with the research team if there was any lack of clarity in their inclusion.
Data Extraction
The study characteristics were extracted from the final 26 included papers. A predefined data extraction table was populated with information, such as study design, sample size, location, analysis method, participants’ ages, inclusion and exclusion criteria, analysis methods, study goals, quantitative and qualitative data collection tools, and key findings (Multimedia Appendix 2 [13, 21, 25, 27, 30, 34, 41, 43, 48, 50, 62-77]).
NVivo 12 was used to extract relevant qualitative data to achieve the primary aim of the review. A predefined table, including the author, measures, scale items, and results, was used to extract relevant quantitative data.
Quality Assessment
Appropriate appraisal tools were chosen based on the methodology and study design. Each of the studies included in this review was critically assessed using an appropriate tool: the Cochrane Collaboration tool for randomized controlled trials (RCTs) [78], National Institute for Health and Care Excellence clinical guidelines for questionnaire studies or surveys [79], the Critical Appraisal Skills Programme Qualitative Checklist for qualitative studies [80], and the McGill University Appraisal Tool for Mixed Methods [81].
To meet the aims of this systematic literature review and not to exclude data relevant to this review, the quality of papers was not assessed with the purpose of excluding them. Instead, limitations of the included studies were considered during the analysis and synthesis of data.
Analysis
The analysis was completed in 2 phases for qualitative and quantitative data. Thematic analysis with an inductive approach [82] was used to develop themes from 73% (19/26) studies that included qualitative data following the 6 steps outlined by Braun and Clarke [82].
Level 1 (reviewing codes of each theme for existence of coherent patterns) and level 2 analyses (reviewing the themes to assess whether they reflect the entire data set) were conducted by the first author and the second coauthor. Interrater reliability was not carried out, in line with the recommended process by Braun and Clarke [83].
Narrative review was used to analyze the quantitative data owing to the heterogeneity of research methods used. A narrative review is flexible and allows different types of evidence to be combined into a coherent summary. The narrative review process [84] included summarizing and explaining the quantitative data presented in 69% (18/26) included papers.
Results
Study Selection and Study Characteristics
The search and screening strategies are shown in Figure 1.
Figure 1.
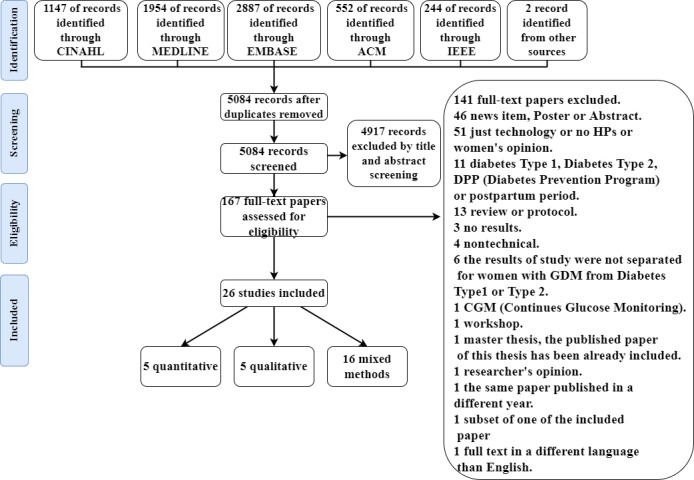
Study identification flowchart. GDM: gestational diabetes mellitus; HP: health professional.
A total of 26 papers were included from the full text based on the inclusion and exclusion criteria. Of the included papers, 19% (5/26) were quantitative, 19% (5/26) were qualitative, and 62% (16/26) used mixed methods (Multimedia Appendix 2). The sample sizes varied among the studies, ranging from 9 [62] to 340 [63] participants. Most of the included studies were from Europe (15/26, 58%), and the rest were from North America (3/26, 11%), Australia (4/26, 15%), Singapore (1/26, 4%), New Zealand (1/26, 4%), and South Korea (1/26, 4%), with 4% (1/26) study of unspecified location. Studies varied in exploring the views of women and HPs. Of these, 96% (25/26) studies included the views of women, with 23% (6/26) including the views of HPs, and only 4% (1/26) including HPs’ views without those of women.
Methodological Quality Assessment
In general, the 26 included studies showed some degree of bias in their research.
Figure 2 [21,25,34,43,50,64] and Figure 3 show the risk of bias summary and graph (specific to an RCT study design), respectively, for the included studies using Review Manager 5.3 (Cochrane Collaboration desktop software).
Figure 2.
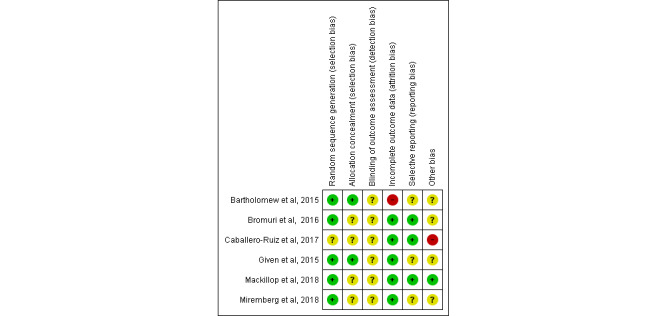
Risk of bias summary—each risk of bias item across included randomized controlled trial studies. Green: Yes (low risk of bias); Red: No (high risk of bias); Yellow: Unclear (bias is not clear or bias cannot be determined) [21,25,34,43,50,64].
Figure 3.
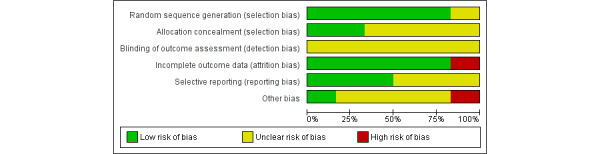
Risk of bias graph—the risk of bias item presented as percentages across included randomized controlled trial studies. Green: Yes (low risk of bias); Red: No (high risk of bias); Yellow=Unclear (bias is not clear or bias cannot be determined).
On the basis of the nature of the included studies that used technology as a core of their research, it was impossible to blind participants and researchers from the knowledge of the intervention participants received [35]. Therefore, performance bias was not included in the risk of bias assessment (Figures 2 and 3) [35]. Of the 23% (6/26) RCT studies, quality assessment showed that 15% (4/26) had a low risk of bias [21,25,43,64]. The other 8% (2/26) studies presented a risk of bias in incomplete outcome data owing to the withdrawal of a large number of participants during the study [50] and an unequal number of participants in the intervention and control groups [34]. Furthermore, the allocation concealment method has been adequately reported in only 8% (2/26) studies [25,50].
Quality appraisal of the remaining studies (Multimedia Appendix 3 [13,21,25,27,30,34,41,43,48,50,62-77]) revealed that 11% (3/26) qualitative studies were of good quality in design, data collection procedure, and data analysis [62,65,66]. The common limitations for the rest of the studies (including quantitative, qualitative, or mixed methods) were bias in sampling [49,67,68], small sample sizes relative to the type of study conducted [67,69,70], lack of information about the validity and reliability of the data collection tools [67,69-71], lack of information about inclusion and exclusion criteria [68], poor qualitative results [64], and unclear recruitment strategy [72]. In addition, there was a lack of information regarding the method of gathering qualitative data [13] and the analysis process [13,72]. In 8% (2/26) mixed methods studies, it was stated that the quantitative data would be collected in the following phase, but there was no clear explanation about how the triangulation of the quantitative and qualitative data would answer the research question [27,48].
Thematic Analysis of Qualitative Data
Overview
Of the included studies, 73% (19/26) contributed qualitative data to the thematic analysis. The views of women and HPs were integrated and reported together throughout the analysis. A total of 4 themes were identified: benefits of using technology, engagement with people via technology, usability of technology, and discouragement factors for the use of technology (definitions of the themes and subthemes are available in Multimedia Appendix 4). Furthermore, 2 subthemes were identified, as outlined in Figure 4.
Figure 4.
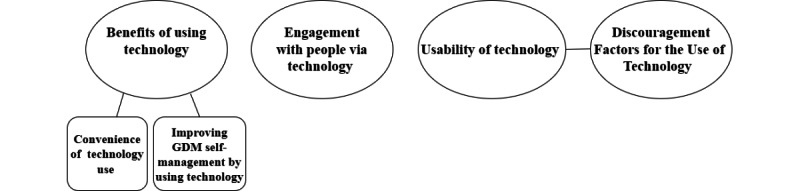
Thematic map showing themes and subthemes. GDM: gestational diabetes mellitus.
Theme 1: Benefits of Using Technology
Overview
Both women and HPs reported their confidence in [27,72] and willingness to use GDM self-management systems because of the benefits of these systems for women with GDM [25,30] and for their babies’ health [65,66,72]. Furthermore, some HPs considered technology to be beneficial for complementing the limited number of health care professionals, while the rate of GDM is increasing [66]. The benefits of using technology themes included 2 subthemes: “convenience of technology use” and “improving self-management by using technology.”
Convenience of Technology Use
Convenience was the predominant benefit of using technology for GDM management. A total of 50% (13/26) papers reported that women with GDM and HPs found the convenience of reduced travel and clinical appointments, as well as the pervasive use of technology, the most beneficial reasons for its use. Women in the studies of Khalil [66] and Edward et al [73] expressed that traveling is “exhausting” [66] particularly toward the end of their pregnancy [73], and especially for women living at a distance [27,30,66]. Women and HPs also indicated that it would lead to a reduction in the need for women to make potentially stressful arrangements for finding childcare and managing absence from work [25,27]. Therefore, technology could be highly advantageous for women with busy lives, especially those who already have children [30]:
I am amazed with the technology and it suited me much better than having to travel in a lot and wait, especially with little ones
Patient 10
Generally, women and HPs lauded the ease and convenience of using technology rather than traditional paper logbooks. This was mainly because of the ability to access technology anytime [74] or anywhere, driven by the growing pervasiveness of mobile devices [62,73]—“you’ve always got your phone haven’t you, so it’s the easiest way to do stuff” (Patient 3).
Women and HPs also recognized constant access to information related to GDM [62,65,73] and being familiar with using similar technology [48,62,72-74] as further elements of ease and convenience.
Saving time is another convenient aspect of technology use for both women [25,27,75] and HPs [64]. In a study by Bromuri et al [64], a telemedicine system helped HPs review BG values quicker than to review them on a paper logbook, owing to alerts that highlighted out-of-range BG values resulting in hyperglycemia and hypoglycemia being recognized quickly. Women and HPs agreed that it takes considerable time to attend clinical appointments [27] just to “be told you’re doing everything right” [25,75]:
They don’t want to spend all of their time trying to get to the hospital and look for parking and spend long periods waiting at hospital.
Clinician 2
Improving GDM Self-management by Using Technology
Improving the ability of women to self-manage GDM is another prominent benefit of using such technology. Increasing awareness of one’s own data has been perceived as an important element of using technology for GDM self-management [25,63,65]. Women in some studies indicated that real-time feedback [63,65,74], visualization of data (eg, graphic nutrient summaries or recommendations) [63,65,74] and the ability to review and track their data [25,63,75] empowered them with “self-awareness” about their own data [63,65,74]. The clarity of the relationship between different attributes, particularly diet and BG levels, was seen as beneficial [63,65,73]. Data relationships also helped women to identify “where it [self-management] was working or where it was going wrong’’ [25] and supported them to change their lifestyle [63,65,74]. However, women and HPs had different opinions about the accuracy of women’s self-reported data. Although some women favored recording data with technology because they were more accurate and precise [74], other women admitted misreporting their data values to get more positive feedback [65]. Some HPs did not want to rely on women’s self-reported data [76] because they did not trust the accuracy of the data; they preferred to enter data into the system themselves [72].
Women also found information related to diet [49,63,68,73,74] and peer support [73,75] useful in improving their lifestyle. Moreover, women felt “automatic messages” [63], rewards, and goal tracking on the system motivated them to change their lifestyle and optimize their GDM self-management.
Both women and HPs perceived increased independence through technology [66,72]. Women and HPs also expressed that using a digital GDM system improved both their self-management skills [27,65,66] and exercise of control on their GDM condition [25,27,63,65,71,73,74,77]:
myDiabby helped patients self-manage their health. [66]
Nurse 2
Technologies help us being more autonomous. We feel more responsible. [66]
Patient 1
Theme 2: Engagement With People via Technology
This theme included 2 main components including engagement with peers and engagement with health care professionals.
Women with GDM indicated that accessing “peer support” by a digital GDM self-management system would be useful [75] as “somebody may know something more” [68]. Although some women had little or no experience with web-based group communication, they were still interested in communicating with other women with GDM via technology [68]. Peer support provided an opportunity for women to access “other people’s experiences” [73] for sharing and exchanging information [68]. As a woman with GDM indicated, peer support provided “a better overview of risks associated with GDM, what could go wrong potentially, and the good stories as well” [73]. Overall, women perceived that peer support empowered them with a broader scope of GDM knowledge than other women who were experiencing the same condition [73]. In addition, peer support reassured women that they were “not alone” [73] and offered them a “constant feeling of support” [73]. Furthermore, it enabled women to talk about their condition and experience in a “safe space” without being judged by other people [73]. Women indicated a lack of peer support in the current care system that might be addressed using technology [75].
Regarding engagement with health care professionals, women appreciated the possibility of receiving additional support using technology. They valued sharing their data and having regular GDM monitoring by HPs via technology [25,66,68,72,73,76], specifically for benefiting both their own health and that of their baby [72]. Women expressed how sharing data with HPs was “reassuring” and gave them a “safety net” [25] owing to a feeling of being monitored more closely by the HPs [73]. Similarly, some HPs believed that sharing data would provide an opportunity to review and monitor the data frequently [64,66], detect any changes or problems at an early stage [25,48] and thereby allow the early application of treatment or interventions for women with GDM [25,64,66].
Although some women and HPs felt comfortable communicating via technology [30,66,71,73,75], others were concerned about a lack of physical and emotional support [27,62,66,75] and a poorer quality of conversation [25,27,66]:
I like the one to one contact so you can ask questions. [25]
Nevertheless, women still felt there was a need to provide more interaction and communication between HPs and women via mobile app technology [76].
Theme 3: Usability of Technology
Women and HPs provided various perspectives on the usability of digital GDM systems in this theme. The content of the systems, including the quality of information and format and presentation of patients’ data, was the main usability aspect discussed by women and HPs in the included papers.
When women and HPs found the GDM systems “easy to use” [25,30,66,72,74], “simple” [25,66], “intuitive” [66] and “straightforward” [25,74], these impressions were influenced by the presence of simple language and images [63] and the simplicity of information presentation, such as displaying all data on one screen [62,72,77].
When usability concerns arose, they were also related to the data format and layout. Women and HPs suggested improving the layout and format of the information by changing the size of images or the amount of text [49], using videos [27], improving the data summary presentation [74,77], changing the data format to be similar to that of a paper logbook [25,48,63,74], and distinguishing different degrees of BG severity [48]:
To look back and see is there a blood sugar previous to try and identified yourself which was the pre and which was the post [meal test]. [25]
In the study by Pustozerov and Popova [76], HPs also indicated that improving the data format would help them review the data more easily.
Discussions on usability were also directed at the effectiveness of GDM apps in fulfilling the needs of women. Participants in different studies provided opinions about the lack of functionality in their GDM self-management systems. Some of their diverse suggestions included an option to scan barcodes of food [74], a time-alerting function for entering data [13], an educational or coaching feature [48], the ability to add a note to BG readings, and the ability to record the type of physical activity they have performed [65].
Women were also interested in having pop-up messages [65], informing them about any changes in their data [48], their condition [73], or any new activities in the forum [68] on the system:
To be able to review previous (entered) results and comments, to get an alert notice if results are out of the ideal range... [48]
A final aspect of usability concerned the effectiveness of information content. Women and HPs found the GDM information in both older technology [73] as well as that introduced by the studies [63,65,77] to be insufficient and simplistic [63,65,73,77]. Personalized information was considered vital [63] for diet [48,49] and in-depth information about GDM [65,77]. In addition, some women had issues with the clarity of the content and wanted simple, clear [49,77] and commonly used language [63,77] such as using “tablespoon” or “bowl” as familiar measurement units used by their dietitian rather than imperial measurements that were used to display food quantities on the app [63].
Despite the clear views of some women and HPs that using GDM self-management technology was more efficient in monitoring [48] and recording [68], other women were concerned about the inefficiency of their GDM systems [73,74]. Women with GDM found it was time consuming to use the system, particularly to retrieve information from food databases [74]. Postpartum women who had GDM perceived that the apps they used for GDM were overcomplicated and required too much commitment to complete a task [73]:
For something that was quite simple, it would take actually a long time to find it. [74]
I’ve never managed to do it for a long period, because of the amount of commitment. [65]
Theme 4: Discouragement Factors for the Use of Technology
The apparent disinterest of HPs was a cause of discouragement for women with GDM. Some said HPs lacked interest [63,65,71] and knowledge [65] in using technology. Indeed, their HPs’ preference for a paper logbook discouraged women from using digital GDM self-management tools [65], particularly those who were already unfamiliar with such technology [27]:
I had no interest in writing it two places, and I understood that no one was going to read or use my app…They always asked for my book, so I used that. [79]
Similarly, HPs were concerned about women’s abilities to use technology:
they’re all on their screens but at the end of the day, some of them don’t actually have credit to even look at a website or download a piece of information. [67]
Confirming this, some women reported little or no experience of using “message boards and things of that nature” [68]. Therefore, women themselves believed that some training might be needed to increase their confidence to use such technologies [27,72]. Some women with GDM were also concerned about the privacy of personal health information recorded on the systems [25,77].
In addition, HPs were concerned about the time required to use the systems and thought it would increase their workload [25,48,66,75]. They were also concerned that some women might not be able to afford the technology [75]:
We have some women who have got quite a low socioeconomic status, most of them still have phones...but not all have [mobile] data. [67]
Women with GDM and HPs also experienced technical problems as barriers to the use of GDM self-management technology. Both women and HPs reported some difficulties with data transmission [62,65,71], problems with accessing technology [75], and poor access to the local internet [25,30].
Narrative Review of Quantitative Data
A narrative review was used to analyze the quantitative data, including the usability and user satisfaction results from 50% (13/26) of the included studies. Quantitative data from the remaining 27% (7/26) studies were not included in the analysis, as the results were not related to usability or user satisfaction [27,48,49,63,72,75] or were the result of objective task performance [77].
Usability
Quantitative studies used various measurements to gather data. Of these, only 12% (3/26) included a usability questionnaire to evaluate their systems, as summarized in Table 1.
Table 1.
Included studies that used a usability questionnaire.
| Usability | Type |
| Gianfrancesco et al [74] | SUSa questionnaire |
| Jo and Park [13] | SUS (Korean version) |
| Pustozerov and Popova [76] | Custom usability questionnaire (10-point scale questions on convenience and usefulness + open-ended questions) |
aSUS: system usability scale.
Of the included studies, 8% (2/26) applied the system usability scale (SUS) developed by Brook in 1996 [85], with defined acceptability ranges for SUS scores (0-50 not acceptable, 50-70 marginal and 70-100 acceptable range) [86]. Jo and Park [13] reported a marginal score for their app, just below the acceptable threshold, (69.5 of 100). A similar, but acceptable, score was reported in the study by Gianfrancesco et al [74] for their web-based dietary system (70.9 out of 100) [74]. Pustozerov and Popova [76] included a custom questionnaire wherein women with GDM rated the “usefulness” and “convenience” of their GDM system on a 10-point scale. Usefulness was rated highly (8.7 out of 10), with convenience scoring somewhat lower (7.2 of 10).
In short, although these results suggest that previous GDM systems have usability challenges, it is impossible to draw any reliable conclusions with only 12% (3/26) studies providing results from a usability questionnaire.
User Satisfaction
The included studies used different measurements to evaluate user satisfaction. Given et al [25] used an adapted version of the Telemedicine Satisfaction and Usefulness Questionnaire by Bakken et al [87]. Of the studies that included user satisfaction questionnaires, 4% (1/26) did not make their satisfaction questionnaire available [21], 12% (3/26) used specially developed satisfaction questionnaires [30,34,50], and the rest (4/26, 15%) used satisfaction questionnaires without any information on how they were developed [21,67,69-71]. Studies by Hirst et al [30] and Mackillop et al [43] were the only ones to provide evidence of the validity and reliability of their developed questionnaires.
The included studies reported generally high user satisfaction in their evaluations of GDM systems [21,25,30,34,50,67,69-71]. However, their user satisfaction questionnaires evaluated many different aspects of GDM systems regarding the type of technology and its features, making it difficult to clearly summarize areas for improvement. Table 2 shows the key measures of the user satisfaction questionnaires in the included studies (the complete measures are available in Multimedia Appendix 5). Most questionnaires used a Likert scale rating to assess the degree of participants’ agreement with their statements about the GDM systems. Women in these studies interacted with the technology within the period from GDM diagnosis until childbirth (usually between 8 and 10 weeks). They all used and evaluated the real working prototypes. Miremberg et al [21] were not included in Table 2 because the questions or satisfaction items were not available in their study.
Table 2.
User satisfaction question topics in the included studies.
| Summary of key measures of user satisfaction questionnaires | Study | ||||||||
|
|
Varnfield et al [71] | Johnson and Berry [67] | Mackillop et al [43] | Peleg et al [70] | Caballero-Ruiz et al [34] | Peleg et al [69] | Bartholomew et al [50] | Hirst et al [30] | Given et al [25] |
| Convenient |
|
|
✓a |
|
|
|
|
✓ |
|
| Avoiding displacement |
|
|
|
|
✓ |
|
|
|
|
| Fit in with life or did not complicate it |
|
|
✓ | ✓ | ✓ | ✓ |
|
✓ |
|
| Adapt to daily life and context changes |
|
|
|
✓ |
|
✓ |
|
|
|
| Number of hospital consultations is enough |
|
|
✓ |
|
✓ |
|
|
|
|
| Help to record BGLsb | ✓ |
|
|
|
|
|
|
|
|
| Help to remember to take medication and take BGc |
|
✓ |
|
|
|
|
|
|
|
| Help to eat healthier or become more active |
|
✓ |
|
|
|
|
|
|
|
| Helps to improve GDMd knowledge |
|
|
|
|
✓ |
|
|
|
|
| Increased motivation for self-management |
|
|
|
|
|
|
✓ |
|
|
| Improved diabetes control |
|
|
|
|
|
|
✓ |
|
|
| Help to feel confident in managing GDM | ✓ |
|
|
✓ |
|
✓ |
|
|
|
| Feel confident that health care team checked BGLs | ✓ |
|
|
|
|
|
|
|
|
| Recommending to others |
|
✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
|
|
| Using it again |
|
✓ | ✓ | ✓ |
|
✓ |
|
|
✓ |
| Useful |
|
|
|
✓ | ✓ |
|
|
|
|
| Easy to use |
|
|
|
✓ |
|
|
✓ |
|
✓ |
| Ease to learn how to use |
|
|
|
✓ | ✓ |
|
|
|
|
| Helps data interpretation |
|
|
|
✓ | ✓ |
|
|
|
|
| Clarity or effectiveness of visualization |
|
|
|
✓ | ✓ |
|
|
|
|
| Clarity of activities’ sequence in app |
|
|
|
✓ |
|
|
|
|
|
| Personalized |
|
|
|
|
|
|
✓ |
|
|
| System response time |
|
|
|
✓ |
|
✓ |
|
|
|
| Experiencing error with the system |
|
|
|
✓ |
|
|
|
|
|
| Time consuming |
|
|
|
|
|
|
✓ |
|
|
| Trust is being well controlled |
|
|
|
|
✓ |
|
|
|
|
| Trust it to work |
|
|
|
|
|
|
|
|
✓ |
| Reliable to use |
|
|
✓ |
|
|
|
|
✓ |
|
| Satisfaction regarding diabetes follow-up |
|
|
|
|
✓ |
|
|
|
|
| Satisfied with the system | ✓ |
|
|
|
|
|
|
|
✓ |
| Enjoyable or interesting |
|
|
|
✓ |
|
|
✓ |
|
|
| Paying for the system |
|
|
|
✓ |
|
✓ |
|
|
|
a✓: illustrates where a study included a measure of user satisfaction in its participant questionnaire.
bBGL: blood glucose level.
cBG: blood glucose.
dGDM: gestational diabetes mellitus.
Assessment of the aspects of convenience was common. Caballero-Ruiz et al [34] highlighted the convenience of minimizing travel to centralized clinics as the strongest indicator of satisfaction (approximately, on average, 9.5 out of 10). In other studies, women rated GDM apps highly for factors such as not complicating their lives [34,69,70] and the ability of these apps to fit into their lifestyles [30].
Improvement of GDM self-management was a highly rated aspect of the studied systems, including helping women to record BG levels [71], reminding them to take medication and record BG levels, helping them eat healthier, encouraging them to be more active [67], and helping to improve their GDM knowledge [34]. Moreover, most women found SMS text messages helpful and motivated them to optimize their GDM self-management [50,67]. A total of 2 studies also reported a general increase in women’s confidence in the management of their GDM [34,70].
Confidence or trust in GDM systems was rated well. Women with GDM reported confidence that the health care team checked their BG levels on the GDM system [71]. Many studies reported high ratings of confidence in the GDM systems, with women recommending them to others [34,43,50,67,69] or planning to use them in their next pregnancy [25,43,50,67]. Similarly, a study reported a high degree of trust (average 9 out of 10) in the GDM system [34], while another study reported that the GDM system was reliable [30].
Slightly lower satisfaction scores were reported for other aspects of ease of use: clarity of visualization of changes to treatment was rated approximately 7 out of 10 [34], and Peleg et al [70] reported satisfaction with system response time as approximately 3.5 out of 5, and ability to assist with interpreting self-monitored data approximately 3.8 out of 5.
Overall, based on the usability results (scores just under or above the acceptable threshold), there is much room for improvement in the usability of GDM self-management systems. However, with the limited number of papers providing a quantitative usability evaluation and the heterogeneity of questions assessing satisfaction, more studies are needed to identify where the improvement of usability and user satisfaction should be focused.
Discussion
Principal Findings
Overview
The primary objective of this systematic literature review was to identify the views of HPs, women with GDM, and postpartum women who have had GDM regarding GDM self-management technology. The secondary objective was to investigate the usability and user satisfaction levels of existing technologies and quantitatively evaluate these factors.
Regarding the first objective, thematic analysis of the qualitative data in the selected papers identified four themes: (1) the benefits of using technology, (2) engagement with people via technology, (3) usability of technology, and (4) discouragement factors for the use of technology.
The thematic analysis of qualitative data revealed barriers to usability, including technical problems, data privacy, lack of emotional support, the accuracy of reported data, and adoption of the system by HPs. Convenience, improving GDM self-management, peer support, increasing motivation, increasing independency, and providing consistent monitoring were common facilitators of using this technology.
For the second objective, the narrative review of the quantitative data (usability and user satisfaction) showed that there is room for improvement in the usability of GDM self-management systems.
Benefits of Using Technology
Convenience of Technology Use
The influence of convenience in our analysis, in both the qualitative and quantitative findings, is echoed in other literature on telemedicine. Pérez-Ferre et al [88] reported a 65% reduction in the number of clinical visits for women with GDM who were using telemedicine. The main benefits of doing so are the improvement of HPs' work efficiency and a better quality of life for women with GDM [57].
Although our findings indicated a strong positive desire to reduce in-person clinics through technology, not everyone wanted clinical visits replaced altogether. This was affirmed in a recent systematic review that highlighted the negative impact of losing in-person contact between women with GDM and HPs [57], particularly for women who experience social isolation and anxiety during pregnancy [89]. However, these studies were carried out before the COVID-19 pandemic. Today, patients may be more familiar with remote consultations, and the impact of this would benefit from further investigation.
Improving GDM Self-management by Using Technology
Our results revealed that women appreciated the use of technology to manage various aspects of their condition. These findings are consistent with those of relevant studies outside the scope of this review. Leziak et al [90] explored the experiences of women with GDM and pregnant women with type 2 diabetes using mobile health (mHealth) during pregnancy. Their results showed enhanced self-management through the use of mHealth technology [90]. Similarly, Yee et al [91] explored how pregnant women with GDM or preexisting diabetes perceived an SMS-based intervention during their pregnancy, showing an optimization of GDM self-management and increased motivation for diabetes self-care. In 2007, Homok et al [32] evaluated the feasibility of a web-based telemedicine system that monitored the BG levels of underserved (poor socioeconomic status) women with GDM using the Diabetes Empowerment Scale [92]. Participants experienced increased diabetes management self-efficacy, such as readiness to change their lifestyle behaviors to achieve diabetes goals.
In summary, evidence suggests that technology could help women optimize their GDM self-management abilities, leading to benefits for both themselves and their baby’s health. As a result of good practices initiated through GDM self-management technology, women could also improve control over their health, which could be maintained habitually after giving birth to prevent the development of type 2 diabetes.
Engagement With People via Technology
As mentioned earlier, this theme consists of 2 main components: “engagement with peers” and “engagement with health care professionals.”
The results of the thematic analysis demonstrated the benefits of peer support in digital GDM self-management systems [68,73,75] a finding supported by similar studies outside the scope of this review. Leziak et al [90] explored the experiences of low-income women with GDM and pregnant women with type 2 diabetes, using mHealth technology to support and improve diabetes self-management during pregnancy. Their results highlighted how women valued social interactions with other women and accessed their knowledge and experiences. McMillan et al [93] evaluated mHealth technology to support postpartum women with a history of GDM in maintaining postnatal activity and good dietary habits, finding that a discussion forum was a valuable feature in doing so [93]. As other previous studies have emphasized, such favorable opinions of women toward peer support stem from their ability to share or read stories about other women [91] and receive emotional support [94], which is an important factor in health communication [95,96]. Indeed, some HPs believed that pregnant women valued other women’s experiences more than HPs’ advice during their pregnancy [97]. However, Sherman and Greenfield [94] found that, when examining message boards for pregnant teenagers, some of the medical information posted by pregnant women was misleading because it was suitable for their specific condition and therefore inappropriate for others [94]. Furthermore, validation of posted information is also a major challenge [95], and further work is needed in this area to provide a reliable and validated communication path between women with GDM.
Our thematic analysis described women’s interest in sharing data with their clinicians by remote means, to obtain reassurance and to be monitored more consistently. This is also evident in some previous studies. Dalfra et al [31] found that women with GDM and pregnant women with type 1 diabetes appreciated their telemedicine system for sharing their data with HPs and their ability to communicate with them whenever needed. Similarly, Leziak et al [90] showed that women were also in favor of sharing data with HPs and receiving real-time feedback. However, in the included studies, some HPs found it difficult to trust women’s reported data [72,76]. In contrast, Kruger et al [98] found that HPs were satisfied with the accuracy of the data reported by women with GDM via a telemedicine system. Other studies have found that it is unlikely that women would misreport their records, as they are highly motivated to maintain BG control [31] for the sake of their baby’s health [57]. Further work is needed to examine the means of decreasing the possibility of reporting incorrect data.
Usability of Technology
Although the evidence available regarding the usability of digital GDM self-management systems is limited [99], the findings of our review are in line with those of previous studies on mHealth self-management systems for type 1 and type 2 diabetes. Katz et al [100] assessed 8 current diabetes self-management apps for adults with type 1 diabetes, discovering issues in the interpretability of data and high cognitive load. These results were corroborated by Fu et al [101] in an evaluation of 4 apps for type 2 diabetes management. Further studies have also found usability challenges with data format on mHealth self-management systems [102-104], such as difficulty interpreting or understanding data in its current format [104]. A useful digital self-management system should display data trends and patterns, specifically showing which data are normal or abnormal. Usability issues with data formats thus prevent patients from understanding their data [105,106], thereby limiting their self-management capabilities.
Our review also identified limitations in the functionality of the systems as another usability concern across the included studies. Previous reviews of general diabetes self-management apps have highlighted important missing functionality, including automatic transfer of BG data from a glucometer to a mobile app, personalized diabetes management advice [107], prevention of errors [108], freedom to edit or remove data entries and appointments, and the ability to automate common tasks [109].
The limited functionality of diabetes self-management systems can be considered a usability problem [109] and is likely to result in these systems failing to meet users’ needs [107]. Addressing these functionality limitations would mitigate some of the usability challenges and help users optimize their engagement and interaction with these systems.
Quantitative evaluation of GDM self-management apps in the studies by Jo and Park [13] and Gianfrancesco et al [74] yielded SUS scores just below and above the acceptable threshold, respectively. Unsurprisingly, previous studies that used the SUS questionnaire to evaluate diabetes self-management apps in different domains have received similarly poor ratings [101,110,111]. Similar to this systematic review, these previous studies used guidance from Bangor et al [85] to interpret the SUS scores, with most apps falling below the acceptable range.
Our quantitative analysis identified the need to improve the usability of GDM self-management systems. However, with the limited number of papers providing a quantitative usability evaluation, the heterogeneity of questions assessing satisfaction and the variation in systems being assessed, it is difficult for quantitative studies to identify where the improvement of usability and user satisfaction should be focused. Therefore, it is an aspect that needs further investigation.
Discouragement Factors for the Use of Technology
Despite the perceived benefits of GDM technology, our analysis revealed technical problems as a prevalent barrier across the included studies. Previous studies have reported similar technical problems when using eHealth and self-management systems [102,112-115]. Moreover, a previous systematic literature review by Simblett et al [116] identified technical problems as one of the most significant barriers to using mHealth technologies. The most common technical problems in their review were app disappearance, loss of power, restarting without warning, not receiving notifications, receiving them at the wrong time, and having a difficult connection. Indeed, 2 participants withdrew from one of the included studies because of difficulties with internet connectivity. Parallel to the findings of this review, technical problems were the cause of reducing participants’ motivations [112,113] and even the cause of leaving the study by participants with other health conditions [114,116].
In addition to technical problems, the privacy of personal health information was a concern for some women. Simblett et al [116] also reported privacy concerns in one of the included studies. Although the use of advanced encryption algorithms and pseudoanonymization of personal data should address security and privacy challenges at the system level, it is important for future GDM systems to effectively communicate good security practices to reassure new users [117].
Although most women across all studies were interested in using self-management technology, some suggested that their HPs were disinterested. Similarly, Wake et al [118] recognized the lack of awareness and adoption of technology by HPs as an important barrier to using eHealth for diabetes self-management [118]. HPs’ difficulty to accept technology was experienced in previous studies [119-121], influenced by difficulty integrating it with their workflow [102,121], lack of integration with the medical record system [120], or a lack of technical knowledge [116]. Further work is required to involve HPs in the design and development of GDM technology more effectively to reduce this barrier.
Limitations and Further Work
The strengths of this review were its application of a rigorous process in paper selection and summarizing results that include both qualitative and quantitative data to cover a wide scope of understanding. Although this systematic literature review was conducted by the first author, we mitigated the potential for bias through a double screening of a proportion of papers’ citations (title and abstract) by the entire research team, in line with previous systematic literature reviews published in JMIR. Two of the authors were also involved in theme development and the methods and results were reviewed by all authors.
Thematic analysis was restricted to the qualitative data contained in the papers (19/26, 73%). It is possible that the authors of the included studies did not report significant results. However, it is unlikely that the key findings were not reported in the original papers.
The details of the methods and methodologies applied were limited in some studies. The available evidence is also limited by several factors. First, some studies used small sample sizes. Methodologically robust trials of greater sizes are needed to confirm the findings of our review. Second, the number of quantitative studies that measured usability was limited. Third, most of the evaluations of satisfaction did not address the validity and reliability of the satisfaction questionnaires. Furthermore, some questions in the satisfaction questionnaires were generic. Using standard evaluation tools and valid questionnaires would offer consistent and robust results across different studies.
Overall, further work is required to improve the usability of GDM self-management systems. There is a need to evaluate the systems using various usability approaches [109,122,123] and larger samples to obtain broader usability perceptions and identify problems with the systems. Furthermore, more engaging elements in a GDM self-management system are needed to develop better emotional support for women. Work is needed to improve peer communication to develop more support for women with GDM.
Further work is also needed to assess the design and development process of these GDM self-management technologies that might help identify the source of these usability challenges.
Conclusions
This is the first systematic literature review to carry out a comprehensive review of the perspectives of HPs, women with GDM, and postpartum women who have had GDM about using technology for GDM self-management during pregnancy. Despite the existence of several studies on technology and GDM, information about the perceptions of women with GDM and HPs regarding GDM self-management technology is limited. More rigorous studies are needed to reveal evidence-based barriers to and facilitators of using existing GDM self-management systems.
Acknowledgments
The authors would like to take this opportunity to thank the Engineering and Physical Sciences Research Council (EPSRC) for the funding support and opportunity to conduct this research project. They also thank Professor Annalu Waller, Dr Rachel Menzies, and Mr Scott McGregor for providing their help and advice during this review.
Abbreviations
- BG
blood glucose
- GDM
gestational diabetes mellitus
- HP
health professional
- mHealth
mobile health
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- RCT
randomized controlled trial
- SUS
system usability scale
Keywords and search strategy.
Study characteristics.
Quality assessment.
Definition of the themes and subthemes.
Satisfaction measurements.
Footnotes
Conflicts of Interest: None declared.
References
- 1.World Health Organization Definition, diagnosis and classification of diabetes mellitus and its complications : report of a WHO consultation. Part 1, Diagnosis and classification of diabetes mellitus. World Health Organization. 1999. [2022-10-21]. https://apps.who.int/iris/handle/10665/66040 .
- 2.Mastrogiannis DS, Igwe E, Homko CJ. The role of telemedicine in the management of the pregnancy complicated by diabetes. Curr Diab Rep. 2013 Feb;13(1):1–5. doi: 10.1007/s11892-012-0352-x. [DOI] [PubMed] [Google Scholar]
- 3.Ferrara A. Increasing prevalence of gestational diabetes mellitus: a public health perspective. Diabetes Care. 2007 Jul;30 Suppl 2:S141–6. doi: 10.2337/dc07-s206.30/Supplement_2/S141 [DOI] [PubMed] [Google Scholar]
- 4.Anna V, van der Ploeg HP, Cheung NW, Huxley RR, Bauman AE. Sociodemographic correlates of the increasing trend in prevalence of gestational diabetes mellitus in a large population of women between 1995 and 2005. Diabetes Care. 2008 Dec;31(12):2288–93. doi: 10.2337/dc08-1038. https://europepmc.org/abstract/MED/18809630 .dc08-1038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhu Y, Zhang C. Prevalence of gestational diabetes and risk of progression to type 2 diabetes: a global perspective. Curr Diab Rep. 2016 Jan;16(1):7. doi: 10.1007/s11892-015-0699-x. https://europepmc.org/abstract/MED/26742932 .10.1007/s11892-015-0699-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.National Collaborating Centre for Women's and Children's Health . The National Institute for Health and Clinical Excellence. London, UK: RCOG Press; 2008. Diabetes in pregnancy: management of diabetes and its complications from preconception to the postnatal period. [PubMed] [Google Scholar]
- 7.Births in Scottish Hospitals. Information Services Division Publication Report. 2017. Nov 28, [2019-06-06]. https://www.isdscotland.org/Health-Topics/Maternity-and-Births/Publications/2017-11-28/2017-11-28-Births-Report.pdf .
- 8.Rigla M, Martínez-Sarriegui I, García-Sáez G, Pons B, Hernando ME. Gestational diabetes management using smart mobile telemedicine. J Diabetes Sci Technol. 2018 Mar;12(2):260–4. doi: 10.1177/1932296817704442. https://europepmc.org/abstract/MED/28420257 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ovesen PG, Jensen DM, Damm P, Rasmussen S, Kesmodel US. Maternal and neonatal outcomes in pregnancies complicated by gestational diabetes. A nation-wide study. J Matern Fetal Neonatal Med. 2015;28(14):1720–4. doi: 10.3109/14767058.2014.966677. [DOI] [PubMed] [Google Scholar]
- 10.Pettitt DJ, Knowler WC, Baird HR, Bennett PH. Gestational diabetes: infant and maternal complications of pregnancy in relation to third-trimester glucose tolerance in the Pima Indians. Diabetes Care. 1980;3(3):458–64. doi: 10.2337/diacare.3.3.458. [DOI] [PubMed] [Google Scholar]
- 11.Xiong X, Saunders LD, Wang FL, Demianczuk NN. Gestational diabetes mellitus: prevalence, risk factors, maternal and infant outcomes. Int J Gynaecol Obstet. 2001 Dec;75(3):221–8. doi: 10.1016/s0020-7292(01)00496-9.S0020-7292(01)00496-9 [DOI] [PubMed] [Google Scholar]
- 12.Carolan M. Women's experiences of gestational diabetes self-management: a qualitative study. Midwifery. 2013 Jun;29(6):637–45. doi: 10.1016/j.midw.2012.05.013.S0266-6138(12)00100-3 [DOI] [PubMed] [Google Scholar]
- 13.Jo S, Park H. Development and evaluation of a smartphone application for managing gestational diabetes mellitus. Healthc Inform Res. 2016 Jan;22(1):11–21. doi: 10.4258/hir.2016.22.1.11. https://www.e-hir.org/DOIx.php?id=10.4258/hir.2016.22.1.11 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Metzger BE, Buchanan TA, Coustan DR, de Leiva A, Dunger DB, Hadden DR, Hod M, Kitzmiller JL, Kjos SL, Oats JN, Pettitt DJ, Sacks DA, Zoupas C. Summary and recommendations of the Fifth International Workshop-Conference on Gestational Diabetes Mellitus. Diabetes Care. 2007 Jul;30 Suppl 2:S251–60. doi: 10.2337/dc07-s225.30/Supplement_2/S251 [DOI] [PubMed] [Google Scholar]
- 15.Schneider S, Hoeft B, Freerksen N, Fischer B, Roehrig S, Yamamoto S, Maul H. Neonatal complications and risk factors among women with gestational diabetes mellitus. Acta Obstet Gynecol Scand. 2011 Mar;90(3):231–7. doi: 10.1111/j.1600-0412.2010.01040.x. doi: 10.1111/j.1600-0412.2010.01040.x. [DOI] [PubMed] [Google Scholar]
- 16.Bellamy L, Casas J, Hingorani AD, Williams D. Type 2 diabetes mellitus after gestational diabetes: a systematic review and meta-analysis. Lancet. 2009 May 23;373(9677):1773–9. doi: 10.1016/S0140-6736(09)60731-5.S0140-6736(09)60731-5 [DOI] [PubMed] [Google Scholar]
- 17.Krishnaveni GV, Hill JC, Veena SR, Geetha S, Jayakumar MN, Karat CL, Fall CH. Gestational diabetes and the incidence of diabetes in the 5 years following the index pregnancy in South Indian women. Diabetes Res Clin Pract. 2007 Dec;78(3):398–404. doi: 10.1016/j.diabres.2007.06.002. https://linkinghub.elsevier.com/retrieve/pii/S0168-8227(07)00311-7 .S0168-8227(07)00311-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.American Diabetes Association Diagnosis and classification of diabetes mellitus. Diabetes Care. 2010 Jan;33 Suppl 1:S62–9. doi: 10.2337/dc10-S062. https://europepmc.org/abstract/MED/20042775 .33/Supplement_1/S62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ohno MS, Sparks TN, Cheng YW, Caughey AB. Treating mild gestational diabetes mellitus: a cost-effectiveness analysis. Am J Obstet Gynecol. 2011 Sep;205(3):282.e1–7. doi: 10.1016/j.ajog.2011.06.051. https://europepmc.org/abstract/MED/22071065 .S0002-9378(11)00786-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Crowther CA, Hiller JE, Moss JR, McPhee AJ, Jeffries WS, Robinson JS, Australian Carbohydrate Intolerance Study in Pregnant Women (ACHOIS) Trial Group Effect of treatment of gestational diabetes mellitus on pregnancy outcomes. N Engl J Med. 2005 Jun 16;352(24):2477–86. doi: 10.1056/NEJMoa042973.NEJMoa042973 [DOI] [PubMed] [Google Scholar]
- 21.Miremberg H, Ben-Ari T, Betzer T, Raphaeli H, Gasnier R, Barda G, Bar J, Weiner E. The impact of a daily smartphone-based feedback system among women with gestational diabetes on compliance, glycemic control, satisfaction, and pregnancy outcome: a randomized controlled trial. Am J Obstet Gynecol. 2018 Apr;218(4):453.e1–.e7. doi: 10.1016/j.ajog.2018.01.044.S0002-9378(18)30133-9 [DOI] [PubMed] [Google Scholar]
- 22.Sheikhi H, Saadatifar B, Dashtban R, Anvari N, Mastaelizadeh H. Self-care in patients with gestational diabetes. J Biochem Technol. 2018;9(2):177–80. [Google Scholar]
- 23.Mackillop L, Loerup L, Bartlett K, Farmer A, Gibson OJ, Hirst JE, Kenworthy Y, Kevat DA, Levy JC, Tarassenko L. Development of a real-time smartphone solution for the management of women with or at high risk of gestational diabetes. J Diabetes Sci Technol. 2014 Nov;8(6):1105–14. doi: 10.1177/1932296814542271. https://europepmc.org/abstract/MED/25004915 .1932296814542271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nam S, Chesla C, Stotts NA, Kroon L, Janson SL. Barriers to diabetes management: patient and provider factors. Diabetes Res Clin Pract. 2011 Jul;93(1):1–9. doi: 10.1016/j.diabres.2011.02.002.S0168-8227(11)00051-9 [DOI] [PubMed] [Google Scholar]
- 25.Given JE, Bunting BP, O'Kane MJ, Dunne F, Coates VE. Tele-Mum: a feasibility study for a randomized controlled trial exploring the potential for telemedicine in the diabetes care of those with gestational diabetes. Diabetes Technol Ther. 2015 Dec;17(12):880–8. doi: 10.1089/dia.2015.0147. [DOI] [PubMed] [Google Scholar]
- 26.van den Heuvel JF, Groenhof K, Veerbeek JH, van Solinge WW, Lely AT, Franx A, Bekker MN. eHealth as the next-generation perinatal care: an overview of the literature. J Med Internet Res. 2018 Jun 05;20(6):e202. doi: 10.2196/jmir.9262. https://www.jmir.org/2018/6/e202/ v20i6e202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Harrison TN, Sacks DA, Parry C, Macias M, Ling Grant DS, Lawrence JM. Acceptability of virtual prenatal visits for women with gestational diabetes. Womens Health Issues. 2017;27(3):351–5. doi: 10.1016/j.whi.2016.12.009.S1049-3867(16)30145-1 [DOI] [PubMed] [Google Scholar]
- 28.Edwards L, Connors C, Whitbread C, Brown A, Oats J, Maple-Brown L, NT Diabetes in Pregnancy Partnership Improving health service delivery for women with diabetes in pregnancy in remote Australia: survey of care in the Northern Territory Diabetes in Pregnancy Partnership. Aust N Z J Obstet Gynaecol. 2014 Dec;54(6):534–40. doi: 10.1111/ajo.12246. [DOI] [PubMed] [Google Scholar]
- 29.Franc S, Daoudi A, Mounier S, Boucherie B, Dardari D, Laroye H, Neraud B, Requeda E, Canipel L, Charpentier G. Telemedicine and diabetes: achievements and prospects. Diabetes Metab. 2011 Dec;37(6):463–76. doi: 10.1016/j.diabet.2011.06.006.S1262-3636(11)00127-3 [DOI] [PubMed] [Google Scholar]
- 30.Hirst JE, Mackillop L, Loerup L, Kevat DA, Bartlett K, Gibson O, Kenworthy Y, Levy JC, Tarassenko L, Farmer A. Acceptability and user satisfaction of a smartphone-based, interactive blood glucose management system in women with gestational diabetes mellitus. J Diabetes Sci Technol. 2015 Jan;9(1):111–5. doi: 10.1177/1932296814556506. https://europepmc.org/abstract/MED/25361643 .1932296814556506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dalfrà MG, Nicolucci A, Lapolla A, TISG The effect of telemedicine on outcome and quality of life in pregnant women with diabetes. J Telemed Telecare. 2009;15(5):238–42. doi: 10.1258/jtt.2009.081213.15/5/238 [DOI] [PubMed] [Google Scholar]
- 32.Homko CJ, Santamore WP, Whiteman V, Bower M, Berger P, Geifman-Holtzman O, Bove AA. Use of an internet-based telemedicine system to manage underserved women with gestational diabetes mellitus. Diabetes Technol Ther. 2007 Jun;9(3):297–306. doi: 10.1089/dia.2006.0034. [DOI] [PubMed] [Google Scholar]
- 33.Wojcicki JM, Ladyzynski P, Krzymien J, Jozwicka E, Blachowicz J, Janczewska E, Czajkowski K, Karnafel W. What we can really expect from telemedicine in intensive diabetes treatment: results from 3-year study on type 1 pregnant diabetic women. Diabetes Technol Ther. 2001;3(4):581–9. doi: 10.1089/15209150152811207. [DOI] [PubMed] [Google Scholar]
- 34.Caballero-Ruiz E, García-Sáez G, Rigla M, Villaplana M, Pons B, Hernando ME. A web-based clinical decision support system for gestational diabetes: automatic diet prescription and detection of insulin needs. Int J Med Inform. 2017 Jun;102:35–49. doi: 10.1016/j.ijmedinf.2017.02.014.S1386-5056(17)30053-9 [DOI] [PubMed] [Google Scholar]
- 35.Ming W, Mackillop LH, Farmer AJ, Loerup L, Bartlett K, Levy JC, Tarassenko L, Velardo C, Kenworthy Y, Hirst JE. Telemedicine technologies for diabetes in pregnancy: a systematic review and meta-analysis. J Med Internet Res. 2016 Nov 09;18(11):e290. doi: 10.2196/jmir.6556. https://www.jmir.org/2016/11/e290/ v18i11e290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kim Y, Kim H, Kim Y. Effects of a web-based self-management program on the behavior and blood glucose levels of women with gestational diabetes mellitus. Telemed J E Health. 2019 May;25(5):407–14. doi: 10.1089/tmj.2017.0332. [DOI] [PubMed] [Google Scholar]
- 37.Guo H, Zhang Y, Li P, Zhou P, Chen L, Li S. Evaluating the effects of mobile health intervention on weight management, glycemic control and pregnancy outcomes in patients with gestational diabetes mellitus. J Endocrinol Invest. 2019 Jun;42(6):709–14. doi: 10.1007/s40618-018-0975-0.10.1007/s40618-018-0975-0 [DOI] [PubMed] [Google Scholar]
- 38.Yew TW, Chi C, Chan S, van Dam RM, Whitton C, Lim CS, Foong PS, Fransisca W, Teoh CL, Chen J, Ho-Lim ST, Lim SL, Ong KW, Ong P, Tai BC, Tai ES. A randomized controlled trial to evaluate the effects of a smartphone application-based lifestyle coaching program on gestational weight gain, glycemic control, and maternal and neonatal outcomes in women with gestational diabetes mellitus: the SMART-GDM study. Diabetes Care. 2021 Feb;44(2):456–63. doi: 10.2337/dc20-1216. https://europepmc.org/abstract/MED/33184151 .dc20-1216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Li S, Ouyang Y, Qiao J, Shen Q. Technology-supported lifestyle interventions to improve maternal-fetal outcomes in women with gestational diabetes mellitus: a meta-analysis. Midwifery. 2020 Jun;85:102689. doi: 10.1016/j.midw.2020.102689.S0266-6138(20)30062-0 [DOI] [PubMed] [Google Scholar]
- 40.Seo Y, Kim EM, Choi JS, Park C. Using a mobile-based nutritional intervention application improves glycemic control but reduces the intake of some nutrients in patients with gestational diabetes mellitus: a case series study. Clin Nutr Res. 2020 Jan;9(1):73–9. doi: 10.7762/cnr.2020.9.1.73. https://e-cnr.org/DOIx.php?id=10.7762/cnr.2020.9.1.73 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Carolan-Olah M, Sayakhot P. A randomized controlled trial of a web-based education intervention for women with gestational diabetes mellitus. Midwifery. 2019 Jan;68:39–47. doi: 10.1016/j.midw.2018.08.019.S0266-6138(17)30524-7 [DOI] [PubMed] [Google Scholar]
- 42.Xie W, Dai P, Qin Y, Wu M, Yang B, Yu X. Effectiveness of telemedicine for pregnant women with gestational diabetes mellitus: an updated meta-analysis of 32 randomized controlled trials with trial sequential analysis. BMC Pregnancy Childbirth. 2020 Apr 06;20(1):198. doi: 10.1186/s12884-020-02892-1. https://bmcpregnancychildbirth.biomedcentral.com/articles/10.1186/s12884-020-02892-1 .10.1186/s12884-020-02892-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mackillop L, Hirst JE, Bartlett KJ, Birks JS, Clifton L, Farmer AJ, Gibson O, Kenworthy Y, Levy JC, Loerup L, Rivero-Arias O, Ming W, Velardo C, Tarassenko L. Comparing the efficacy of a mobile phone-based blood glucose management system with standard clinic care in women with gestational diabetes: randomized controlled trial. JMIR Mhealth Uhealth. 2018 Mar 20;6(3):e71. doi: 10.2196/mhealth.9512. https://mhealth.jmir.org/2018/3/e71/ v6i3e71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Albert L, Capel I, García-Sáez G, Martín-Redondo P, Hernando ME, Rigla M. Managing gestational diabetes mellitus using a smartphone application with artificial intelligence (SineDie) during the COVID-19 pandemic: much more than just telemedicine. Diabetes Res Clin Pract. 2020 Nov;169:108396. doi: 10.1016/j.diabres.2020.108396. https://europepmc.org/abstract/MED/32890548 .S0168-8227(20)30649-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Aziz A, Zork N, Aubey JJ, Baptiste CD, D'Alton ME, Emeruwa UN, Fuchs KM, Goffman D, Gyamfi-Bannerman C, Haythe JH, LaSala AP, Madden N, Miller EC, Miller RS, Monk C, Moroz L, Ona S, Ring LE, Sheen J, Spiegel ES, Simpson LL, Yates HS, Friedman AM. Telehealth for high-risk pregnancies in the setting of the COVID-19 pandemic. Am J Perinatol. 2020 Jun;37(8):800–8. doi: 10.1055/s-0040-1712121. https://europepmc.org/abstract/MED/32396948 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Jackson CL, Bolen S, Brancati FL, Batts-Turner ML, Gary TL. A systematic review of interactive computer-assisted technology in diabetes care. Interactive information technology in diabetes care. J Gen Intern Med. 2006 Feb;21(2):105–10. doi: 10.1111/j.1525-1497.2005.00310.x. https://onlinelibrary.wiley.com/resolve/openurl?genre=article&sid=nlm:pubmed&issn=0884-8734&date=2006&volume=21&issue=2&spage=105 .JGI310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kalhori SR, Hemmat M, Noori T, Heydarian S, Katigari MR. Quality evaluation of english mobile applications for gestational diabetes: app review using mobile application rating scale (MARS) Curr Diabetes Rev. 2021;17(2):161–8. doi: 10.2174/1573399816666200703181438.CDR-EPUB-107881 [DOI] [PubMed] [Google Scholar]
- 48.Wickramasinghe N, Gururajan R. Innovation practice using pervasive mobile technology solutions to improve population health management: a pilot study of gestational diabetes patient care in Australia. J Healthc Qual. 2016;38(2):93–105. doi: 10.1097/JHQ.0000000000000033.01445442-201603000-00006 [DOI] [PubMed] [Google Scholar]
- 49.Carolan-Olah M, Steele C, Krenzin G. Development and initial testing of a GDM information website for multi-ethnic women with GDM. BMC Pregnancy Childbirth. 2015 Jul 05;15:145. doi: 10.1186/s12884-015-0578-0. https://bmcpregnancychildbirth.biomedcentral.com/articles/10.1186/s12884-015-0578-0 .10.1186/s12884-015-0578-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bartholomew ML, Soules K, Church K, Shaha S, Burlingame J, Graham G, Sauvage L, Zalud I. Managing diabetes in pregnancy using cell phone/internet technology. Clin Diabetes. 2015 Oct;33(4):169–74. doi: 10.2337/diaclin.33.4.169. https://europepmc.org/abstract/MED/26487790 .169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Balaji B, Halperin I, Mukerji G, Lipscombe L. 1350-P: eHealth technologies for gestational diabetes mellitus: summary of features and effectiveness: scoping review. Diabetes. 2020 Jun 1;69(Supplement_1):1350-P. doi: 10.2337/db20-1350-P. [DOI] [Google Scholar]
- 52.Garg N, Arunan SK, Arora S, Kaur K. Application of mobile technology for disease and treatment monitoring of gestational diabetes mellitus among pregnant women: a systematic review. J Diabetes Sci Technol. 2022 Mar;16(2):491–7. doi: 10.1177/1932296820965577. https://europepmc.org/abstract/MED/33118397 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Nguyen M, Hossain N, Tangri R, Shah J, Agarwal P, Thompson-Hutchison F, Halperin I. Systematic evaluation of Canadian diabetes smartphone applications for people with type 1, type 2 and gestational diabetes. Can J Diabetes. 2021 Mar;45(2):174–8.e1. doi: 10.1016/j.jcjd.2020.07.005.S1499-2671(20)30225-2 [DOI] [PubMed] [Google Scholar]
- 54.Eberle C, Loehnert M, Stichling S. Effectivness of specific mobile health applications (mHealth-apps) in gestational diabtetes mellitus: a systematic review. BMC Pregnancy Childbirth. 2021 Dec 05;21(1):808. doi: 10.1186/s12884-021-04274-7. https://bmcpregnancychildbirth.biomedcentral.com/articles/10.1186/s12884-021-04274-7 .10.1186/s12884-021-04274-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Leblalta B, Kebaili H, Lee S. PDB1 telemedicine use for gestational diabetes: a systematic review and meta-analysis of randomised controlled trials. Value in Health Regional Issues. 2020 Sep;22:S32. doi: 10.1016/j.vhri.2020.07.160. [DOI] [Google Scholar]
- 56.Rasekaba TM, Furler J, Blackberry I, Tacey M, Gray K, Lim K. Telemedicine interventions for gestational diabetes mellitus: a systematic review and meta-analysis. Diabetes Res Clin Pract. 2015 Oct;110(1):1–9. doi: 10.1016/j.diabres.2015.07.007.S0168-8227(15)00329-0 [DOI] [PubMed] [Google Scholar]
- 57.Fantinelli S, Marchetti D, Verrocchio MC, Franzago M, Fulcheri M, Vitacolonna E. Assessment of psychological dimensions in telemedicine care for gestational diabetes mellitus: a systematic review of qualitative and quantitative studies. Front Psychol. 2019;10:153. doi: 10.3389/fpsyg.2019.00153. doi: 10.3389/fpsyg.2019.00153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009 Jul 21;339:b2700. doi: 10.1136/bmj.b2700. https://europepmc.org/abstract/MED/19622552 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Fleming PS, Koletsi D, Pandis N. Blinded by PRISMA: are systematic reviewers focusing on PRISMA and ignoring other guidelines? PLoS One. 2014;9(5):e96407. doi: 10.1371/journal.pone.0096407. https://dx.plos.org/10.1371/journal.pone.0096407 .PONE-D-14-05280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Lumsden J, Edwards EA, Lawrence NS, Coyle D, Munafò MR. Gamification of cognitive assessment and cognitive training: a systematic review of applications and efficacy. JMIR Serious Games. 2016 Jul 15;4(2):e11. doi: 10.2196/games.5888. https://games.jmir.org/2016/2/e11/ v4i2e11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Gaffney H, Mansell W, Tai S. Conversational agents in the treatment of mental health problems: mixed-method systematic review. JMIR Ment Health. 2019 Oct 18;6(10):e14166. doi: 10.2196/14166. https://mental.jmir.org/2019/10/e14166/ v6i10e14166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Garnweidner-Holme L, Hoel Andersen T, Sando MW, Noll J, Lukasse M. Health care professionals' attitudes toward, and experiences of using, a culture-sensitive smartphone app for women with gestational diabetes mellitus: qualitative study. JMIR Mhealth Uhealth. 2018 May 14;6(5):e123. doi: 10.2196/mhealth.9686. https://mhealth.jmir.org/2018/5/e123/ v6i5e123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Surendran S, Lim CS, Koh GC, Yew TW, Tai ES, Foong PS. Women's usage behavior and perceived usefulness with using a mobile health application for gestational diabetes mellitus: mixed-methods study. Int J Environ Res Public Health. 2021 Jun 21;18(12):6670. doi: 10.3390/ijerph18126670. https://www.mdpi.com/resolver?pii=ijerph18126670 .ijerph18126670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Bromuri S, Puricel S, Schumann R, Krampf J, Ruiz J, Schumacher M. An expert personal health system to monitor patients affected by gestational diabetes mellitus: a feasibility study. J Ambient Intelligence Smart Environ. 2016 Mar 15;8(2):219–37. doi: 10.3233/ais-160365. [DOI] [Google Scholar]
- 65.Skar JB, Garnweidner-Holme LM, Lukasse M, Terragni L. Women's experiences with using a smartphone app (the Pregnant+ app) to manage gestational diabetes mellitus in a randomised controlled trial. Midwifery. 2018 Mar;58:102–8. doi: 10.1016/j.midw.2017.12.021.S0266-6138(17)30546-6 [DOI] [PubMed] [Google Scholar]
- 66.Khalil C. Understanding the adoption and diffusion of a telemonitoring solution in gestational diabetes mellitus: qualitative study. JMIR Diabetes. 2019 Nov 28;4(4):e13661. doi: 10.2196/13661. https://diabetes.jmir.org/2019/4/e13661/ v4i4e13661 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Johnson QB, Berry DC. Impacting diabetes self-management in women with gestational diabetes mellitus using short messaging reminders. J Am Assoc Nurse Pract. 2018 Jun;30(6):320–6. doi: 10.1097/JXX.0000000000000059.01741002-201806000-00005 [DOI] [PubMed] [Google Scholar]
- 68.Nicholson WK, Beckham AJ, Hatley K, Diamond M, Johnson L, Green SL, Tate D. The Gestational Diabetes Management System (GooDMomS): development, feasibility and lessons learned from a patient-informed, web-based pregnancy and postpartum lifestyle intervention. BMC Pregnancy Childbirth. 2016 Sep 21;16(1):277. doi: 10.1186/s12884-016-1064-z. https://bmcpregnancychildbirth.biomedcentral.com/articles/10.1186/s12884-016-1064-z .10.1186/s12884-016-1064-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Peleg M, Shahar Y, Quaglini S, Broens T, Budasu R, Fung N, Fux A, García-Sáez G, Goldstein A, González-Ferrer A, Hermens H, Hernando ME, Jones V, Klebanov G, Klimov D, Knoppel D, Larburu N, Marcos C, Martínez-Sarriegui I, Napolitano C, Pallàs A, Palomares A, Parimbelli E, Pons B, Rigla M, Sacchi L, Shalom E, Soffer P, van Schooten B. Assessment of a personalized and distributed patient guidance system. Int J Med Inform. 2017 May;101:108–30. doi: 10.1016/j.ijmedinf.2017.02.010.S1386-5056(17)30049-7 [DOI] [PubMed] [Google Scholar]
- 70.Peleg M, Shahar Y, Quaglini S, Fux A, García-Sáez G, Goldstein A, Hernando ME, Klimov D, Martínez-Sarriegui I, Napolitano C, Parimbelli E, Rigla M, Sacchi L, Shalom E, Soffer P. MobiGuide: a personalized and patient-centric decision-support system and its evaluation in the atrial fibrillation and gestational diabetes domains. User Model User-Adap Inter. 2017 Mar 11;27(2):159–213. doi: 10.1007/s11257-017-9190-5. [DOI] [Google Scholar]
- 71.Varnfield M, Redd C, Stoney RM, Higgins L, Scolari N, Warwick R, Iedema J, Rundle J, Dutton W. M♡THer, an mHealth system to support women with gestational diabetes mellitus: feasibility and acceptability study. Diabetes Technol Ther. 2021 May;23(5):358–66. doi: 10.1089/dia.2020.0509. https://europepmc.org/abstract/MED/33210954 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Pais S, Parry D, Petrova K, Rowan J. Acceptance of using an ecosystem of mobile apps for use in diabetes clinic for self-management of gestational diabetes mellitus. Stud Health Technol Inform. 2017;245:188–92. [PubMed] [Google Scholar]
- 73.Edwards KJ, Bradwell HL, Jones RB, Andrade J, Shawe JA. How do women with a history of gestational diabetes mellitus use mHealth during and after pregnancy? Qualitative exploration of women's views and experiences. Midwifery. 2021 Jul;98:102995. doi: 10.1016/j.midw.2021.102995.S0266-6138(21)00074-7 [DOI] [PubMed] [Google Scholar]
- 74.Gianfrancesco C, Darwin Z, McGowan L, Smith DM, Haddrill R, Carter M, Scott EM, Alwan NA, Morris MA, Albar SA, Cade JE. Exploring the feasibility of use of an online dietary assessment tool (myfood24) in women with gestational d.iabetes. Nutrients. 2018 Aug 23;10(9):1147. doi: 10.3390/nu10091147. https://www.mdpi.com/resolver?pii=nu10091147 .nu10091147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Rasekaba T, Nightingale H, Furler J, Lim WK, Triay J, Blackberry I. Women, clinician and IT staff perspectives on telehealth for enhanced gestational diabetes mellitus management in an Australian rural/regional setting. Rural Remote Health. 2021 Jan;21(1):5983. doi: 10.22605/RRH5983. https://www.rrh.org.au/articles/subviewnew.asp?ArticleID=5983 .5983 [DOI] [PubMed] [Google Scholar]
- 76.Pustozerov E, Popova P. Mobile-based decision support system for gestational diabetes mellitus. Proceedings of the 2018 Ural Symposium on Biomedical Engineering, Radioelectronics and Information Technology (USBEREIT); 2018 Ural Symposium on Biomedical Engineering, Radioelectronics and Information Technology (USBEREIT); May 07-08, 2018; Yekaterinburg, Russia. 2018. [DOI] [Google Scholar]
- 77.Garnweidner-Holme LM, Borgen I, Garitano I, Noll J, Lukasse M. Designing and developing a mobile smartphone application for women with gestational diabetes mellitus followed-up at diabetes outpatient clinics in Norway. Healthcare (Basel) 2015 May 21;3(2):310–23. doi: 10.3390/healthcare3020310. https://www.mdpi.com/resolver?pii=healthcare3020310 .healthcare3020310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA, Cochrane Bias Methods Group. Cochrane Statistical Methods Group The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011 Oct 18;343:d5928. doi: 10.1136/bmj.d5928. https://europepmc.org/abstract/MED/22008217 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Appendix E Evidence tables. National Institute for Health and Care Excellence. [2021-08-12]. https://www.nice.org.uk/guidance/cg143/evidence/appendix-e-evidence-tables-pdf-186634335 .
- 80.CASP checklists. CASP. [2021-08-15]. https://casp-uk.net/casp-tools-checklists/
- 81.Mixed Methods Appraisal Tool (MMAT) – Version 2011. McGill University. 2011. [2021-08-20]. https://tinyurl.com/mr3wjpd9 .
- 82.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006 Jan;3(2):77–101. doi: 10.1191/1478088706qp063oa. [DOI] [Google Scholar]
- 83.Tigwell G, Menzies R, Flatla D. Designing for situational visual impairments: supporting early-career designers of mobile content. Proceedings of the 2018 Designing Interactive Systems Conference; DIS '18: Designing Interactive Systems Conference 2018; Jun 9 - 13, 2018; Hong Kong China. 2018. [DOI] [Google Scholar]
- 84.Mays N, Pope C, Popay J. Systematically reviewing qualitative and quantitative evidence to inform management and policy-making in the health field. J Health Serv Res Policy. 2005 Jul;10 Suppl 1:6–20. doi: 10.1258/1355819054308576. [DOI] [PubMed] [Google Scholar]
- 85.Brooke J. Usability Evaluation In Industry. Boca Raton, Florida, United States: CRC Press; 1996. SUS: a quick and dirty usability scale. [Google Scholar]
- 86.Bangor A, Kortum PT, Miller JT. An empirical evaluation of the system usability scale. Int J Human Comput Interact. 2008 Jul 30;24(6):574–94. doi: 10.1080/10447310802205776. [DOI] [Google Scholar]
- 87.Bakken S, Grullon-Figueroa L, Izquierdo R, Lee N, Morin P, Palmas W, Teresi J, Weinstock RS, Shea S, Starren J, IDEATel Consortium Development, validation, and use of English and Spanish versions of the telemedicine satisfaction and usefulness questionnaire. J Am Med Inform Assoc. 2006;13(6):660–7. doi: 10.1197/jamia.M2146. https://europepmc.org/abstract/MED/16929036 .M2146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Pérez-Ferre N, Galindo M, Fernández MD, Velasco V, Runkle I, de la Cruz MJ, Martín Rojas-Marcos P, Del Valle L, Calle-Pascual AL. The outcomes of gestational diabetes mellitus after a telecare approach are not inferior to traditional outpatient clinic visits. Int J Endocrinol. 2010;2010:386941. doi: 10.1155/2010/386941. doi: 10.1155/2010/386941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Yee LM, McGuire JM, Taylor SM, Niznik CM, Simon MA. "I was tired of all the sticking and poking": identifying barriers to diabetes self-care among low-income pregnant women. J Health Care Poor Underserved. 2015 Aug;26(3):926–40. doi: 10.1353/hpu.2015.0073.S1548686915300267 [DOI] [PubMed] [Google Scholar]
- 90.Leziak K, Birch E, Jackson J, Strohbach A, Niznik C, Yee LM. Identifying mobile health technology experiences and preferences of low-income pregnant women with diabetes. J Diabetes Sci Technol. 2021 Sep;15(5):1018–26. doi: 10.1177/1932296821993175. https://europepmc.org/abstract/MED/33605158 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Yee L, Taylor S, Young M, Williams M, Niznik C, Simon M. Evaluation of a text messaging intervention to support self-management of diabetes during pregnancy among low-income, minority women: qualitative study. JMIR Diabetes. 2020 Aug 10;5(3):e17794. doi: 10.2196/17794. https://diabetes.jmir.org/2020/3/e17794/ v5i3e17794 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Anderson RM, Funnell MM, Fitzgerald JT, Marrero DG. The Diabetes Empowerment Scale: a measure of psychosocial self-efficacy. Diabetes Care. 2000 Jun;23(6):739–43. doi: 10.2337/diacare.23.6.739. [DOI] [PubMed] [Google Scholar]
- 93.Mcmillan B, Easton K, Delaney B, Mitchell C. Reducing the risk of progression from gestational diabetes to type 2 diabetes mellitus: women’s perspectives on the content, research development and evaluation of a mobile health technology lifestyle intervention to support postnatal dietary and activity lifestyle change. Reducing the risk of type 2 diabetes mellitus in primary care after gestational diabetes. 2017. Jan, [2022-10-21]. https://tinyurl.com/23rw8yke .
- 94.Sherman LE, Greenfield PM. Forging friendship, soliciting support: a mixed-method examination of message boards for pregnant teens and teen mothers. Comput Human Behav. 2013 Jan;29(1):75–85. doi: 10.1016/j.chb.2012.07.018. [DOI] [Google Scholar]
- 95.Moorhead SA, Hazlett DE, Harrison L, Carroll JK, Irwin A, Hoving C. A new dimension of health care: systematic review of the uses, benefits, and limitations of social media for health communication. J Med Internet Res. 2013 Apr 23;15(4):e85. doi: 10.2196/jmir.1933. https://www.jmir.org/2013/4/e85/ v15i4e85 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Dasgupta K, Da Costa D, Pillay S, De Civita M, Gougeon R, Leong A, Bacon S, Stotland S, Chetty VT, Garfield N, Majdan A, Meltzer S. Strategies to optimize participation in diabetes prevention programs following gestational diabetes: a focus group study. PLoS One. 2013;8(7):e67878. doi: 10.1371/journal.pone.0067878. https://dx.plos.org/10.1371/journal.pone.0067878 .PONE-D-13-03729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Vickery M, van Teijlingen E, Hundley V, Smith G, Way S, Westwood G. Midwives' views towards women using mHealth and eHealth to self-monitor their pregnancy: a systematic review of the literature. Eur J Midwifery. 2020;4:36. doi: 10.18332/ejm/126625. https://europepmc.org/abstract/MED/33537637 .36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Kruger DF, White K, Galpern A, Mann K, Massirio A, McLellan M, Stevenson J. Effect of modem transmission of blood glucose data on telephone consultation time, clinic work flow, and patient satisfaction for patients with gestational diabetes mellitus. J Am Acad Nurse Pract. 2003 Aug;15(8):371–5. doi: 10.1111/j.1745-7599.2003.tb00410.x. [DOI] [PubMed] [Google Scholar]
- 99.Overdijkink SB, Velu AV, Rosman AN, van Beukering MD, Kok M, Steegers-Theunissen RP. The usability and effectiveness of mobile health technology-based lifestyle and medical intervention apps supporting health care during pregnancy: systematic review. JMIR Mhealth Uhealth. 2018 Apr 24;6(4):e109. doi: 10.2196/mhealth.8834. https://mhealth.jmir.org/2018/4/e109/ v6i4e109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Katz D, Price B, Holland S, Dalton N. Data, data everywhere,still too hard to link: ionsights from user interactions with diabetes apps. Proceedings of the 2018 CHI Conference on Human Factors in Computing Systems; CHI '18: CHI Conference on Human Factors in Computing Systems; Apr 21 - 26, 2018; Montreal QC Canada. 2018. [DOI] [Google Scholar]
- 101.Fu HN, Rizvi RF, Wyman JF, Adam TJ. Usability evaluation of four top-rated commercially available diabetes apps for adults with type 2 diabetes. Comput Inform Nurs. 2020 Jun;38(6):274–80. doi: 10.1097/CIN.0000000000000596. https://europepmc.org/abstract/MED/31904594 .00024665-202006000-00003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Zhu H, Colgan J, Reddy M, Choe EK. Sharing patient-generated data in clinical practices: an interview study. AMIA Annu Symp Proc. 2016;2016:1303–12. https://europepmc.org/abstract/MED/28269928 . [PMC free article] [PubMed] [Google Scholar]
- 103.Georgsson M, Staggers N. An evaluation of patients' experienced usability of a diabetes mHealth system using a multi-method approach. J Biomed Inform. 2016 Feb;59:115–29. doi: 10.1016/j.jbi.2015.11.008. https://linkinghub.elsevier.com/retrieve/pii/S1532-0464(15)00276-2 .S1532-0464(15)00276-2 [DOI] [PubMed] [Google Scholar]
- 104.Hallberg I, Ranerup A, Kjellgren K. Supporting the self-management of hypertension: patients' experiences of using a mobile phone-based system. J Hum Hypertens. 2016 Feb;30(2):141–6. doi: 10.1038/jhh.2015.37. https://europepmc.org/abstract/MED/25903164 .jhh201537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Jalil S, Myers T, Atkinson I. Design implications from the preliminary results of a telemedicine patient-technology interaction study. Proceedings of the 7th International Symposium on Visual Information Communication and Interaction; VINCI '14: The 7th International Symposium on Visual Information Communication and Interaction; Aug 5 - 8, 2014; Sydney NSW Australia. 2014. [DOI] [Google Scholar]
- 106.Freitas CM, Luzzardi PR, Cava RA, Winckler MA, Pimenta MS, Nedel LP. Evaluating usability of information visualization techniques. CNPq, FAPERGS, and CAPES. [2022-10-06]. https://dl.acm.org/doi/abs/10.1145/1556262.1556326 .
- 107.Arnhold M, Quade M, Kirch W. Mobile applications for diabetics: a systematic review and expert-based usability evaluation considering the special requirements of diabetes patients age 50 years or older. J Med Internet Res. 2014 Apr 09;16(4):e104. doi: 10.2196/jmir.2968. https://www.jmir.org/2014/4/e104/ v16i4e104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Fu H, McMahon SK, Gross CR, Adam TJ, Wyman JF. Usability and clinical efficacy of diabetes mobile applications for adults with type 2 diabetes: a systematic review. Diabetes Res Clin Pract. 2017 Sep;131:70–81. doi: 10.1016/j.diabres.2017.06.016.S0168-8227(17)30032-3 [DOI] [PubMed] [Google Scholar]
- 109.Fontecha J, González I, Bravo J. A usability study of a mHealth system for diabetes self-management based on framework analysis and usability problem taxonomy methods. J Ambient Intell Human Comput. 2019 Jun 24;:1. doi: 10.1007/s12652-019-01369-0. [DOI] [Google Scholar]
- 110.Kontio E, Hyrkkänen U, Saarenpää T. Safe and Secure Cities. Cham: Springer; 2014. Experiences on telemedicine solutions for diabetes care – Case eMedic project. [Google Scholar]
- 111.Veazie S, Winchell K, Gilbert J, Paynter R, Ivlev I, Eden KB, Nussbaum K, Weiskopf N, Guise J, Helfand M. Rapid evidence review of mobile applications for self-management of diabetes. J Gen Intern Med. 2018 Jul;33(7):1167–76. doi: 10.1007/s11606-018-4410-1. https://europepmc.org/abstract/MED/29740786 .10.1007/s11606-018-4410-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Verwey R, van der Weegen S, Spreeuwenberg M, Tange H, van der Weijden T, de Witte L. A pilot study of a tool to stimulate physical activity in patients with COPD or type 2 diabetes in primary care. J Telemed Telecare. 2014 Jan;20(1):29–34. doi: 10.1177/1357633X13519057.1357633X13519057 [DOI] [PubMed] [Google Scholar]
- 113.Nes AA, van Dulmen S, Eide E, Finset A, Kristjánsdóttir OB, Steen IS, Eide H. The development and feasibility of a web-based intervention with diaries and situational feedback via smartphone to support self-management in patients with diabetes type 2. Diabetes Res Clin Pract. 2012 Sep;97(3):385–93. doi: 10.1016/j.diabres.2012.04.019.S0168-8227(12)00153-2 [DOI] [PubMed] [Google Scholar]
- 114.Burns MN, Begale M, Duffecy J, Gergle D, Karr CJ, Giangrande E, Mohr DC. Harnessing context sensing to develop a mobile intervention for depression. J Med Internet Res. 2011 Aug 12;13(3):e55. doi: 10.2196/jmir.1838. https://www.jmir.org/2011/3/e55/ v13i3e55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.McCloud RF, Okechukwu CA, Sorensen G, Viswanath K. Beyond access: barriers to internet health information seeking among the urban poor. J Am Med Inform Assoc. 2016 Nov;23(6):1053–9. doi: 10.1093/jamia/ocv204. https://europepmc.org/abstract/MED/27206459 .ocv204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Simblett S, Greer B, Matcham F, Curtis H, Polhemus A, Ferrão J, Gamble P, Wykes T. Barriers to and facilitators of engagement with remote measurement technology for managing health: systematic review and content analysis of findings. J Med Internet Res. 2018 Jul 12;20(7):e10480. doi: 10.2196/10480. https://www.jmir.org/2018/7/e10480/ v20i7e10480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Ristevski B, Chen M. Big data analytics in medicine and healthcare. J Integr Bioinform. 2018 May 10;15(3):42–6. doi: 10.1515/jib-2017-0030. https://europepmc.org/abstract/MED/29746254 ./j/jib.ahead-of-print/jib-2017-0030/jib-2017-0030.xml [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Wake DJ, He J, Czesak AM, Mughal F, Cunningham SG. MyDiabetesMyWay: an evolving national data driven diabetes self-management platform. J Diabetes Sci Technol. 2016 Sep;10(5):1050–8. doi: 10.1177/1932296816648168. https://europepmc.org/abstract/MED/27162192 .1932296816648168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Lapointe L, Rivard S. Getting physicians to accept new information technology: insights from case studies. CMAJ. 2006 May 23;174(11):1573–8. doi: 10.1503/cmaj.050281. http://www.cmaj.ca/cgi/pmidlookup?view=long&pmid=16717265 .174/11/1573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Goodrich DE, Buis LR, Janney AW, Ditty MD, Krause CW, Zheng K, Sen A, Strecher VJ, Hess ML, Piette JD, Richardson CR. Integrating an internet-mediated walking program into family medicine clinical practice: a pilot feasibility study. BMC Med Inform Decis Mak. 2011 Jun 24;11:47. doi: 10.1186/1472-6947-11-47. https://bmcmedinformdecismak.biomedcentral.com/articles/10.1186/1472-6947-11-47 .1472-6947-11-47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Kujala S, Ammenwerth E, Kolanen H, Ervast M. Applying and extending the FITT framework to identify the challenges and opportunities of successful eHealth services for patient self-management: qualitative interview study. J Med Internet Res. 2020 Aug 12;22(8):e17696. doi: 10.2196/17696. https://www.jmir.org/2020/8/e17696/ v22i8e17696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Klaassen B, van Beijnum BJ, Hermens HJ. Usability in telemedicine systems-A literature survey. Int J Med Inform. 2016 Sep;93:57–69. doi: 10.1016/j.ijmedinf.2016.06.004.S1386-5056(16)30130-7 [DOI] [PubMed] [Google Scholar]
- 123.Zapata BC, Fernández-Alemán JL, Idri A, Toval A. Empirical studies on usability of mHealth apps: a systematic literature review. J Med Syst. 2015 Feb;39(2):1. doi: 10.1007/s10916-014-0182-2. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Keywords and search strategy.
Study characteristics.
Quality assessment.
Definition of the themes and subthemes.
Satisfaction measurements.


