Abstract
Background
Body mass index (BMI) remains the most used indicator of nutritional status despite the presence of a potentially credible alternative. Mid-upper arm circumference (MUAC) is an anthropometric measure that requires simple equipment and minimal training. The aim of this study was to compare MUAC with BMI and propose a MUAC cut-off point corresponding to a BMI of < 18.5 kg/m2 (underweight) and ≥ 30.0 kg/m2 (obesity) among Sudanese adults.
Methods
A cross-sectional study using multistage cluster sampling was conducted in New-Halfa, eastern Sudan. Participants’ age and sex were recorded and their MUAC, weight and height were measured using the standard procedures. The MUAC (cm) cut-offs corresponding to < 18.5 kg/m2 and ≥ 30.0 kg/m2 were calculated and determined using receiver operating characteristic (ROC) curve analysis
Results
Five hundreds and fifty-two adults were enrolled in the study. The median (interquartile range, IQR) of the participants age was 31.0 (24.0 – 40.0) years and 331 (60.0%) of them were females. The medians (IQR) of BMI and MUAC were 22.4 (19.1 – 26.3) kg/m2 and 25.0 (23.0 – 28.0) cm, respectively.
There was a significant positive correlation between MUAC and BMI (r = 0.673, p < 0.001).
Of the 552 enrolled participants, 104 (18.8%), 282 (51.1%), 89 (16.1%) and 77 (13.9%) were normal weight, underweight, overweight and obese, respectively. Best statistically derived MUAC cut-off corresponding to a BMI < 18.5 kg/m2 (underweight) was ≤ 25.5 cm in both males and females (Youden’s Index, YI = 0.51; sensitivity = 96.0%; specificity = 54.0%), with a good predictive value (AUROCC = 0.82). Best statistically derived MUAC cut-off corresponding to a BMI ≥ 30.0 kg/m2 (obesity) was ≥ 29.5 cm in both males and females (YI = 0.62, sensitivity = 70.3%, specificity = 92.0%), with a good predictive value (AUROCC = 0.86, 95.0% CI = 0.76 – 0.95).
Conclusion
The results suggest that the cut-offs based on MUAC can be used for community-based screening of underweight and obesity
Keywords: Anthropometry, Body mass index, Mid-upper arm circumference, Underweight, Obesity, Sudanese adults
Introduction
Nutrition-related medical problems are common public health issues with high risks of mortality and economic loss, especially in the developing countries [1]. Body weight and height are used to compute body mass index (BMI), which is widely used to assess nutritional status in adults [2, 3]. BMI is an indicator of malnutrition with an individual being considered underweight when BMI is < 18.5 kg/m2 [4]. Undernutrition affects the function and recovery of almost all body organs [5]. On the other hand, BMI is also utilised to diagnose obesity [4]. Obesity (BMI ≥ 30 kg/m2) represents a threat that increases the risk of several non-communicable diseases [4, 6]. It is associated with elements of metabolic syndrome and its complications, cancer, kidney disease, mental/central nervous system diseases, as well as musculoskeletal, respiratory, reproductive and dermatological disorders [7]. The nutritional status problems in adults are neglected or underestimated in developing countries [1]. Data from sub-Saharan Africa, highlight this health problem, as up to half (6.0 – 48.0%) of elderly Africans are underweight, almost a quarter (2.5 – 21.0%) are overweight and 56.0% of older South Africans are obese [8].
BMI may be biased by fluid overload and oedemas, and therefore does not reflect body composition; for example, a high BMI can be seen in fat people and also in very muscular athletes [3, 9, 10]. The simplicity of MUAC measurement means it does not require mathematical derivation [11], frontline professionals or expensive equipment compared to the requirements for measuring BMI [11]. MUAC is a practical tool for screening and grading the severity of nutritional status problems in the general population [12, 13] and it has demonstrated superiority over BMI [6]. Moreover, previous studies have reported a positive correlation between MUAC and BMI [11, 14]. Several studies have identified the MUAC cut-off measurement as an alternative method of detecting underweight [11, 13–15] and obesity [16, 17].
Nutritional health problems are significant in Sudan [18, 19], but there are no published data that evaluate the use of MUAC measurement among adults to detect their nutritional status. Obtaining specific MUAC cut-off for certain areas of the population can be an important method in developing countries in general and particularly in Sudan. The present study was conducted to evaluate the use of MUAC as a reliable alternative to BMI for detecting malnutrition and obesity among adult Sudanese in New Halfa.
Methods
The setting, subjects and data collection
The Strengthening the Reporting of Observational studies in Epidemiology (STROBE) Statement standard checklists were followed [20]. A multistage sampling study was adopted in New Halfa, eastern Sudan. Initially, four sectors (lowest administrative unit) out of the seven sectors were selected by simple random sampling. The total sample size of 552 (please see below) participants was distributed across the four sectors according to the size allocation of the sector. Then, all the agreed adults (18 – 60 years of age) healthy Sudanese participants from the household were then selected using a lottery method. When a selected house was not inhabited or the inhabitants refused to participate or had met one of the exclusion criteria, the next house was chosen. Trained general practitioners interviewed the participants during the period of January to February 2022.
Inclusion criteria
A multistage sampling method for selection.
Apparently healthy males and females.
Participants who were residents of New Halfa.
Age (≥ 18 years – ≤ 60 years).
Signed consent for participation.
Exclusion criteria
Age below 18 years and above 60 years.
Pregnant women.
Individuals with chronic diseases such as diabetes, thyroid diseases and heart failure.
Critically ill patients with severe acute illness.
Athletes, persons with a mental illness or disability, hormonal or any apparent congenital dysmorphism.
Individuals on chronic medications
Individuals who refused to participate.
Based on our selection criteria, the eligible participants were approached between 9 am and 4 pm from Sunday to Thursday. Age, sex, weight (to the nearest 10.0 g), standing height (to the nearest 1mm) and MUAC (to the nearest 1mm) in sitting or standing posture were measured following standard procedures using calibrated instruments. During weight measurement, each subject was asked to stand after removing their shoes, any heavy clothing and any objects in their pockets. They were then instructed to relax with their arms at the sides and feet positioned close together to evenly distribute their weight across their feet. Height was measured by a stadiometer without shoes and socks, while the feet were positioned together at the heels to ensure the back of the heels, buttocks and shoulder blades touched the back plate/stick. Besides this, the head was adjusted in the Frankfurt horizontal plane. The MUAC was measured using a non-stretchable MUAC measuring tape. The tape was placed at a point equidistant between the acromion process of the left scapula and the olecranon process of the left ulna to measure the MUAC. All anthropometric measurements were performed twice, and the average was recorded. A third measurement was obtained in case of considerable variation between the first two measurements (differences of more than 100.0 g for weight, 0.5 cm for height and 0.2 cm for MUAC). The average of the nearest two measurements was recorded. BMI was calculated using the standard formula: weight in kg/height in m2 [4]. In accordance with the WHO criteria, the BMI cut-off points of < 18.5kg/m 2 and ≥ 30.0 kg/m2 were used to identify adults who were underweight and those with obesity, respectively [4].
Determining sensitivity and specificity
Sensitivity and specificity are of diagnostically equal importance; hence the Youden index (YI) was used to indicate the best performance (the larger the better) at a given cut-off. The Statistical Package for the Social Sciences (SPSS) was used to obtain the receiver operating characteristic (ROC) curve and coordinates of the curve that indicate sensitivity and 1−specificity. Then the J-index was calculated as the YI = sensitivity + specificity - 1 to locate the suitable cut-off points depending on the highest J-index. Then we suggested the best cut-off point based on the highest value of YI to show the best sensitivity and specificity.
Sample size calculation
A sample of 552 participants adults was calculated to have the significant minimum difference in the correlations (r = 0.15) for calculated BMI and measured MUAC, This sample (552 adults) would have an 80% power and a difference of 5% at α = 0.0 5[21]. To ensure state-wide representativeness, respondents were selected from all sectors after New Halfa was divided in to four sectors according to its population.
Statistical analysis
Data were collected and statistical analyses were performed using IBM SPSS v.25. Normality in distribution was tested using Shapiro-Wilk tests. The data were not normally distributed hence Mann-Whitney U was used to test the difference of variables between males and females. Descriptive statistics were generated for demographic variables, all measurements (weight, height and MUAC) and BMI. Scatterplots with fitted linear regression lines were calculated to assess the relationship between MUAC and BMI, and correlation analysis was performed using Spearman’s correlation to obtain correlation coefficients and P value for all females and male participants, Sensitivity and specificity were calculated for all individual measurements in the dataset. Youden’s Index (YI) was calculated as YI = sensitivity + specificity - 1. The MUAC cut-off with the highest YI-value was considered the optimal statistically-derived cut-off [22]. The area under the receiver operating characteristic curve (AUROCC) was calculated for all participants and females and male separately. P value less than 0.05 was adopted for significance.
Results
Five hundreds and fifty-two participants were enrolled in the study. The median (IQR) of the age was 31.0 (24.0 – 40.0) years and 331 (60.0%) of them were females. The medians (IQR) of BMI and MUAC were 22.4 (19.1 – 26.3) kg/m2 and 25.0 (23.0 – 28.0) cm, respectively.
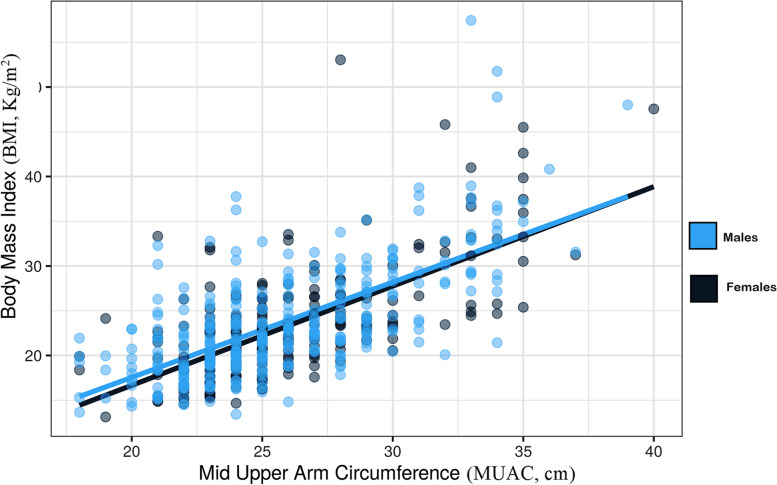
While males were significantly elder and taller, for weight, BMI and MUAC there were no differences between males and females, Table 1. There was a significant positive correlation between MUAC and BMI (r = 0.673, p < 0.001) in both females and males, in females (r = 0.639, p < 0.001) and in males (r = 0.634, p < 0.001), Fig. 1.
Table 1.
Comparison of anthropometric profile between men and women from eastern Sudan
| Total (number =552) | Female (number =331) | Male (number =221) | P | |
|---|---|---|---|---|
| Age, years. | 31.0 (24.0 – 40.0) | 30.0 (24.0 – 39.0) | 33.0 (26.0 – 44.0) | 0.040 |
| Weight, kg | 58.2 (46.0 – 70.0) | 56.0 (45.0 – 70.0) | 59.0 (48.0 – 70.0) | 0.127 |
| Height, cm | 160.0 (150.0 – 170.0) | 160.0 (150.0 – 168.0) | 163.0 (154.0 – 172.0) | <0.001 |
| Body mass index, kg/m2. | 22.4 (19.1 – 26.3) | 22.31 (19.2 – 27.01) | 22.4 (18.8 –25.2) | 0.437 |
| Mid upper arm circumference, cm | 25.0 (23.0 – 28.0) | 25.0 (23.0 – 28.0) | 25.0 (23.0 – 29.0) | 0.439 |
Fig 1.
Curve estimation for assessing linear relationship between mid-upper arm circumference and body mass index in adults in eastern Sudan 2022
Of the 552 enrolled participants, 104 (18.8%), 282 (51.1%), 89 (16.1%) and 77(13.9%) were normal weight, underweight, overweight, and obese, respectively.
The best statistically derived MUAC cut-off corresponding to a BMI < 18.5 kg/m2 (underweight) was ≤ 25.5 cm in both males and females (YI = 0.51; sensitivity = 96.0%; specificity = 54.0%), with a good predictive value (AUROCC = 0.82, 95.0% CI = 0.78 – 0.86), in females (YI = 0.51, sensitivity = 97.0%, specificity = 54.0%), with a good predictive value (AUROCC = 0.83, 95.0% CI = 0.78 – 0.87) and in males (YI = 0.51, sensitivity = 96.0%, specificity = 56.0%), with a good predictive value (AUROCC = 0.83,95.0% CI = 0.77 – 0.88) (Table 2 and Fig. 2).
Table 2.
MUAC cut-off points for the diagnosis of underweight and obesity in adults from eastern Sudan, 2022
| Underweight (body mass index<18.5 kg/m2) | Obese (body mass index≥ 30.0 kg/m2) | |||||
|---|---|---|---|---|---|---|
| All participants | Females | Males | All participants | Females | Males | |
| Mid-upper arm circumference cut-off | ≤ 25.5 cm | ≤ 25.5 cm | ≤ 25.5 cm | ≥ 29.5 cm | ≥ 29.5 cm | ≥ 29.5 cm |
|
Area under the curve (95.0% confidence interval) |
0.82 (0.78–0.86) |
0.83 (0.78–0.87) |
0.83 (0.77–0.88) |
0.84 (0.78–0.90) |
0.84 (0.76–0.91) |
0.86 (0.76–0.95) |
| Youden's index | 0.51 | 0.51 | 0.51 | 0.62 | 0.59 | 0.64 |
| Sensitivity | 96.0 | 97.0 | 96.0 | 70.3 | 68.9 | 72.4 |
| Specificity | 54.0 | 54.0 | 56.0 | 92.0 | 91.0 | 92.2 |
Fig. 2.
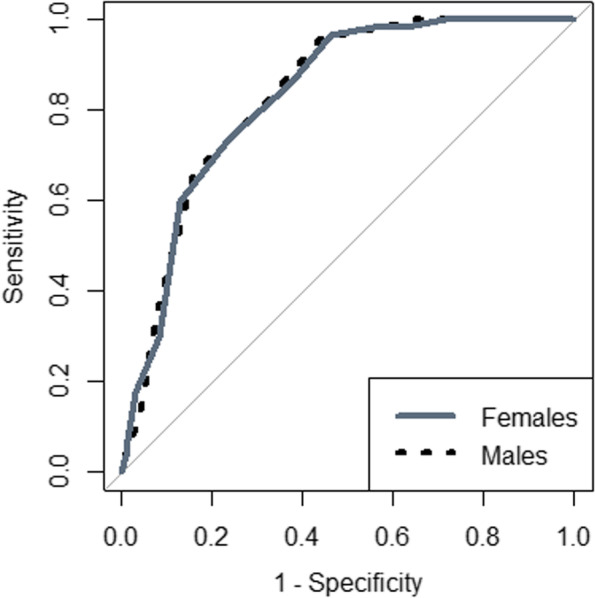
Receiver operating curve of mid-upper-arm-circumference for underweight (body mass index <18.5 kg/m2) for adults in eastern Sudan 2022
The best statistically derived MUAC cut-off corresponding to a BMI ≥ 30.0 kg/m2 (obesity) was ≥ 29.5 cm in both males and females (Y I = 0.62, sensitivity = 70.3%, specificity = 92.0%), with a good predictive value (AUROCC = 0.84, 95.0% CI = 0.78–0.90), in females (YI = 0.59, sensitivity = 68.9%, specificity = 91.0%), with a good predictive value (AUROCC = 0.84, 95.0 % CI = 0.76–0.91) and in males (YI = 0.64, sensitivity = 72.4%, specificity = 92.2%), with a good predictive value (AUROCC = 0.86, 95.0 CI = 0.76 – 0.95) (Table 2 and Fig. 3).
Fig. 3.
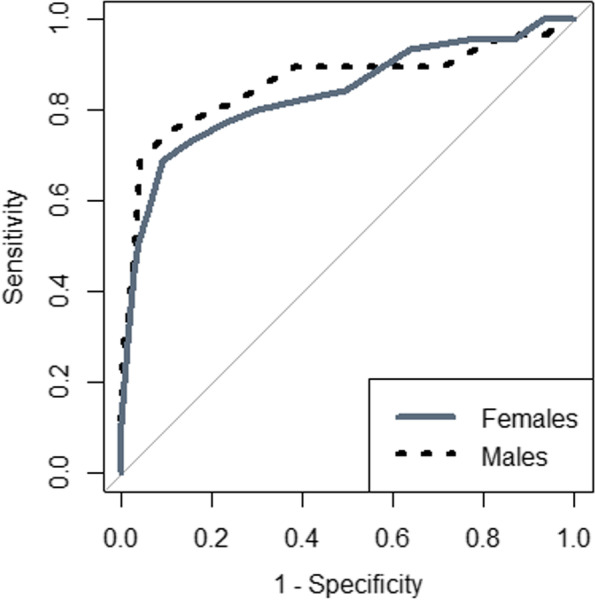
Receiver operating curve of mid-upper-arm-circumference for obesity t (body mass index ≥ 30.0 kg/m2) for adults in eastern Sudan 2022
Discussion
The current study demonstrated a positive correlation between BMI and MUAC in all participants and in male and non-pregnant female adults separately. This was similar to the previous findings in several studies, e.g., in South Sudan [16, 23], Bangladesh (males r = 0.81, versus females r = 0.828,) [11], Nepal (women r = 0.889 and men r = 0.846) [14], Spain (r = 0.78) [24] and in India (r = 0.81) [25].
In the current study a statistically derived MUAC cut-off for an underweight individual was ≤ 25.5 cm, which showed similar results in females and males (YI = 0.51; sensitivity = 96.0%; specificity = 54.0% and AUROCC = 0.82). The MUAC cut-off proposed in our study to detect underweight, was similar to that obtained recently in South Sudan (MUAC ≤ 25.4 cm, sensitivity = 87.0% and specificity = 81.0%) [16] and among adults in Sub-Saharan African countries (≤ 25·5cm, sensitivity = 77.0% and specificity = 79.6%) [26]. Moreover, the same cut-off of MUAC (≤ 25.5 cm) was adopted to assess nutritional risk, three months post-acute stroke, in patients aged over 65 years in South-eastern Norway [27].
Furthermore, MUAC cut-off to detect underweight, in the current study, was slighter higher than that reported in a meta-analysis study, evaluating twenty datasets from Africa (13,835 participants) (≤ 25·0 cm) [15], female and male farmers in Tanzania and Mozambique (≤ 25.0 cm) [13], in Nepal (≤ 24.5 cm, sensitivity = 92.8%, specificity = 82.4% and AUROCC > 0.9) [14] and in Bangladesh (≤25.1 cm, = AUROCC 0.93) [11]. Additionally, MUAC cut-off < 24.0 cm was reported among adults in different studies across the globe such as in South Africa (sensitivity = 89.3% and specificity= 82.9%) [12], in Kolkata, India (male ≤ 24.0 cm) [28, 29], in eastern India (males ≤ 22·7 cm and female ≤ 21·9 cm) [30], in northern Vietnam (≤ 23.5 cm) [17], and in females in Bangladesh (≤ 23.9 cm) [11]. Likewise, a markedly lower MUAC cut -off was reported from another study that recruited 2,421 men and 3,248 women from selected regions of five African countries, India, China and Papua New Guinea: (≤23.0 cm in male and ≤22.0 cm in female) [31] as well as in Spain (22.5 cm) [24]. The summary of the different cut-off points which were reported in several previous studies across the globe are shown in Table 3.
Table 3.
MUAC cut-off points for the identification of underweight and obesity in various populations around the world
| Author | Year | Country | Total number | Males (N) | Females (N) | MUAC cut -off, cm | Youden’s index | sensitivity | specificity | AUROCC | r |
|---|---|---|---|---|---|---|---|---|---|---|---|
| underweight | |||||||||||
| Tang et al. | 2020 | Different countries | 13835 | 4860 | 8993 | 24 | -- | 84 % | 83 % | -- | -- |
| Thorup et al. | 2020 | Nepal | 302 | 105 | 197 | 24.5 | 0.75 | 92.86 % | 82.48 % | > 0.9 |
F;.889 M;.846. |
| Sultana et al. | 2015 | Bangladesh | 650 | 260 | 390 |
F <24 M <25 |
F; 0.69 M; 0.72 |
F; 92.6 % M;92.6 % |
F;76.46 % M;79.6 % |
F;0.93 M; 0.93 |
F;.828 M = 0.8 |
| Eleraky et al. | 2021 | Tanzania and Mozambique | 2106 | 689 | 1417 | <25 | 0.67 | 77.8 % | 87.2 % | -- | 0.837 |
| Chakraborty et al. | 2011 | India | 205 | 205 | 24 | 0.45 | 74.8 % | 70.3 % | 0.79 | 0.45 | |
| Chakraborty et al. | 2009 | India | 474 | 474 | 24 | -- | 0.84 | ||||
| Amegovu et al. | 2020 | South Sudan | 251 | 214 | 37 | < 25.4 | -- | 87 % | 81 % | 90% | 0.8621 |
| Nguyen et al. | 2014 | Vietnam | 4,981 | 4,981 | 23.5 | -- | 89.1 % | 71 % | 0.905 | 0.84 | |
| Tonder et al. | 2019 | multi-centre | 266 | 138 | 128 | 23.7 | -- | 89.3 % | 82.9 % | 0.92 | 0.93, |
| Das et al. | 2020 | India | 618 | -- | 618 | 23.2 | -- | 89 % | 82 % | 0.923 | 0.81 |
| Das et al. | 2018 | India | 955 | 467 | 488 |
M;22·7 F;21·9 |
M;0·605 F; 0·72 |
M;85.71 % F;91.67 % |
M;74·80 % F;79.89 % |
M;0·85 F;0·93 |
0·71 |
| Philpott et al. | 2021 | sub-Saharan | 11 917 | 11 917 | -- | 25·5 | --- | 77 % | 79·6 % % | 0·87 | -- |
| Benítez Brito et al | 2016 | Spain | 1373 | 778 | 595 | ≤22.5 | -- | 67.7 % | 94.5 % | 0.92 | 0.78 |
| Obesity | |||||||||||
| Amegovu et al. | 2020 | South Sudan | 251 | 214 | 37 | >31.1 | -- | 100 % | 96 % | .99 | 0.8621 |
| Das et al. | 2020 | India | 618 | 618 | 30.5 | -- | 99 % | 83 % | 0.876 | 0.81 | |
| Tonder et al. | 2019 | South Africa | 266 | 138 | 128 | 29.4 | -- | 100 % | 87.2 % | 0.97 | -- |
| Eleraky et al.. | 2021 | Tanzania and Mozambique | 2106 | 689 | 1417 | > 31.5 | 0.88 | 95.8 | 92.1 | -- | 0.837 |
| Shifraw T et al. | 2021 | Ethiopia | 4914 | - | 4914 | >30.0 | 0.7 | 87.0 | 83.0 | 0.93 | |
MUAC Mid upper arm circumference, AUROCC Area Under the Receiver Operating Characteristics Curve, r; Correlation coefficient
In the current study, a statistically derived MUAC cut-off for underweight was ≥ 29.5 cm, which was similar in females and males (YI = 0.60; sensitivity = 69.0% and specificity = 92.0%). A similar MUAC cut-off (> 29.4 cm, sensitivity = 100% and specificity = 87.2%) was proposed and obtained in South Africa [12]. On the other hand, slightly higher MUAC cut-offs were demonstrated in the neighbouring country, South Sudan (31.1cm, sensitivity = 100% and specificity = 96.0%) [16], in Ethiopia (≥ 30.0 cm, sensitivity = 87.0 % and specificity = 83.0%) [32], among female and male farmers in Tanzania and Mozambique (≥ 31.5 cm ) [13], in northern Vietnam (≥ 31cm) [17] and among Chinese males (≥ 30.9 cm) [33].
While one study questioned the diagnostic accuracy of BMI when diagnosing obesity and found it to be limited, particularly for individuals in the intermediate BMI ranges [9]. Another study recommended using BMI to detect only overweight related problems [10]. Furthermore, another study concluded that BMI was not a reliable measurement of body composition in individuals, in particular older and younger individuals [34].
We compare our results with others’ findings with caution because we (and some others) determined the cut-off levels for MUAC using the equation YI. It is believed that optimal cut-off should not be determined strictly based on YI, but instead by judging and considering the balance between high sensitivity and high specificity. Moreover, many contributing factors may explain the variation in MUAC cut-off for nutritional status in different studies and populations: the previously documented racial/ethnic issues creating variable cut-offs [12, 28, 35]. Hence, ethno-specific cut-offs for MUAC are proposed to assess the nutritional status for certain populations. While the current study recorded no gender variation regarding MUAC cut off, several previous studies reported MUAC cut-off variation for nutritional status [33, 36]. This could be explained by sex fat distribution during aging, as males tend to have more visceral fat in the abdomen (apple shape), and females tend to have more subcutaneous fat in the hip and thighs (pear shape) before menopause [37]. The main advantages of MUAC method compared to BMI method are the simplicity of MUAC measurement, which does not require mathematical derivation [11], frontline professionals (medical or paramedical staff) [12] and requires relativity low -cost equipment [11, 25], besides being an effective measure of screening for poor nutritional status in adults [38] and during famine and emergencies [23, 39]. MUAC emerges as a useful, applicable and alterative measure of nutritional status in nearly all acutely ill patients whom measurements of weight and height may be inappropriate or impossible [40] and among those who have medical conditions affecting the BMI: the localized accumulation of excess fluid (oedema, ascites) [41]. Hence, measurement of MUAC, is a simple non-invasive method, can be used to assess nutritional status in adult in remote area or alternative method for BMI especially in setting where BMI cannot be used (oedema and immobile patients).
One limitation of the cut-off proposed in the present study is that the data collected from one source location which may not totally represent the entire population in Sudan. Moreover, it was a relatively small sample size. As procedure like BMI, for estimating nutritional status, always has its limitations in specific populations e.g., athletes. A higher sample size might have increased the prevalence of the outcome, which again could increase the strength of the analysis.
Conclusion
Our study proposes the cut-offs based on MUAC (≤ 25.5 cm and ≥ 29.5 cm) as alternative for BMI for community-based screening of underweight and obesity, respectively.
Acknowledgments
The authors would like to thank all the participants who participated in this study.
Abbreviations
- kg
kilogram
- m
meter
- cm
centimeter
- BMI
Body mass index
- CI
Confidence interval
- ROC
receiver operating characteristic curve
- AUROCC
Area Under the Receiver Operating Characteristics Curve
- YI
Youden’s Index
- SPSS
Statistical Package for the Social Sciences
- IQR
Interquartile range
- STROBE
The Strengthening the Reporting of Observational studies in Epidemiology
Authors’ contributions
IRM and SMO conceived the study; IA supervised the work, guided the analysis and critically reviewed the manuscript; IRM and IA prepared the analysis plan, performed the data analysis and wrote the first draft of the paper; IRM and SMO supervised data collection. All authors reviewed and approved the final manuscript
Funding
None received.
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available (because the manuscript is still under the peer review process) but are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
This study complies with the Declaration of Helsinki. Ethics approval was obtained from the Ethics Committee of the Faculty of Medicine of Gadarif University, Sudan (Reference number #2022.03). Written informed consent was collected from each participant.
Consent for publication
Not applicable.
Competing interests
The correspondence author (Ishag Adam) is one of the editorial board in this Journal. The other authors have nothing to declare.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Imad R. Musa, Email: irthesudanese@hotmail.com
Saeed M. Omar, Email: drsaeedomar@yahoo.com
Ishag Adam, Email: ishagadam@hotmail.com.
References
- 1.Abdu AO, Yimamu ID, Kahsay AA. Predictors of malnutrition among older adults aged above 65 years in eastern Ethiopia: neglected public health concern. BMC Geriatr. 2020;20:497. doi: 10.1186/s12877-020-01911-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Physical status: the use of and interpretation of anthropometry, report of a WHO expert committee. https://apps.who.int/iris/handle/10665/37003. Accessed 29 Sept 2022. [PubMed]
- 3.Reber E, Gomes F, Vasiloglou MF, Schuetz P, Stanga Z. Nutritional risk screening and assessment. J Clin Med. 2019;8:1065. doi: 10.3390/jcm8071065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Obesity : preventing and managing the global epidemic : report of a WHO consultation. https://apps.who.int/iris/handle/10665/42330. Accessed 25 May 2022. [PubMed]
- 5.Saunders J, Smith T. Malnutrition: causes and consequences. Clin Med (Northfield Il) 2010;10:624. doi: 10.7861/clinmedicine.10-6-624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bhattacharya A, Pal B, Mukherjee S, Roy SK. Assessment of nutritional status using anthropometric variables by multivariate analysis. BMC Public Health. 2019;19:1045. doi: 10.1186/s12889-019-7372-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Egger G, Dixon J. Beyond obesity and lifestyle: a review of 21st century chronic disease determinants. Biomed Res Int. 2014;2014:731685. doi: 10.1155/2014/731685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kimokoti RW, Hamer DH. Nutrition, health, and aging in sub-Saharan Africa. Nutr Rev. 2008;66:611–623. doi: 10.1111/j.1753-4887.2008.00113.x. [DOI] [PubMed] [Google Scholar]
- 9.Romero-Corral A, Somers VK, Sierra-Johnson J, Thomas RJ, Collazo-Clavell ML, Korinek J, et al. Accuracy of body mass index in diagnosing obesity in the adult general population. Int J Obes (Lond) 2008;32:959–966. doi: 10.1038/ijo.2008.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vanderwall C, Randall Clark R, Eickhoff J, Carrel AL. BMI is a poor predictor of adiposity in young overweight and obese children. BMC Pediatr. 2017;17:135. doi: 10.1186/s12887-017-0891-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sultana T, Karim MN, Ahmed T, Hossain MI. Assessment of under nutrition of Bangladeshi adults using anthropometry: Can body mass index be replaced by mid-upper-arm-circumference? PLoS One. 2015;10:e0121456. doi: 10.1371/journal.pone.0121456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Van Tonder E, Mace L, Steenkamp L, Tydeman-Edwards R, Gerber K, Friskin D. Mid-upper arm circumference (MUAC) as a feasible tool in detecting adult malnutrition. South African J Clin Nutr. 2019;32:93–98. doi: 10.1080/16070658.2018.1484622. [DOI] [Google Scholar]
- 13.Eleraky L, Issa R, Maciel S, Mbwana H, Rybak C, Frank J, et al. High Prevalence of Overweight and Its Association with Mid-Upper Arm Circumference among Female and Male Farmers in Tanzania and Mozambique. Int J Environ Res Public Health. 2021;18:9128. doi: 10.3390/ijerph18179128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Thorup L, Hamann SA, Kallestrup P, Hjortdal VE, Tripathee A, Neupane D, et al. Mid-upper arm circumference as an indicator of underweight in adults: a cross-sectional study from Nepal. BMC Public Health. 2020;20:1187. doi: 10.1186/s12889-020-09294-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tang AM, Chung M, Dong KR, Bahwere P, Bose K, Chakraborty R, et al. Determining a global mid-upper arm circumference cut-off to assess underweight in adults (men and non-pregnant women) Public Health Nutr. 2020;23:3104–3113. doi: 10.1017/S1368980020000397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Amegovu AK, Chewere T, Mawadri M. Mid-upper arm circumference ( MUAC ) cut-offs to diagnose overweight and obesity among adults. J Clin Community Med. 2020:184–90.
- 17.Nguyen P, Ramakrishnan U, Katz B, Gonzalez-Casanova I, Lowe AE, Nguyen H, et al. Mid-upper-arm and calf circumferences are useful predictors of underweight in women of reproductive age in northern Vietnam. Food Nutr Bull. 2014;35:301–311. doi: 10.1177/156482651403500303. [DOI] [PubMed] [Google Scholar]
- 18.Ahmed MH, Ali YA, Awadalla H, Elmadhoun WM, Noor SK, Almobarak AO. Prevalence and trends of obesity among adult Sudanese individuals: Population based study. Diabetes Metab Syndr Clin Res Rev. 2017;11:S963–S967. doi: 10.1016/j.dsx.2017.07.023. [DOI] [PubMed] [Google Scholar]
- 19.Abdelbagi OM, Musa IR, Altigani SA, Osman A, Adam I. Prevalence of diabetic foot amongst adults with diabetes mellitus in northern Sudan: A cross-sectional study. Int J Clin Pract. 2021;75:e14892. doi: 10.1111/ijcp.14892. [DOI] [PubMed] [Google Scholar]
- 20.Cuschieri S. The STROBE guidelines. Saudi J Anaesth. 2019;13(Suppl 1):S31. doi: 10.4103/sja.SJA_543_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bujang MA, Baharum N. Sample Size Guideline for Correlation Analysis. World J Soc Sci Res. 2016;3:37. doi: 10.22158/wjssr.v3n1p37. [DOI] [Google Scholar]
- 22.Youden WJ. Index for rating diagnostic tests. Cancer. 1950;3:32–35. doi: 10.1002/1097-0142(1950)3:1<32::AID-CNCR2820030106>3.0.CO;2-3. [DOI] [PubMed] [Google Scholar]
- 23.Collins S. Using middle upper arm circumference to assess severe adult malnutrition during famine. JAMA. 1996;276:391–395. doi: 10.1001/jama.1996.03540050051023. [DOI] [PubMed] [Google Scholar]
- 24.Benítez Brito N, Suárez Llanos JP, Fuentes Ferrer M, Oliva García JG, Delgado Brito I, Pereyra-García Castro F, et al. Relationship between Mid-Upper Arm Circumference and Body Mass Index in Inpatients. PLoS One. 2016;11:e0160480. doi: 10.1371/journal.pone.0160480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Das A, Saimala G, Reddy N, Mishra P, Giri R, Kumar A, et al. Mid-upper arm circumference as a substitute of the body mass index for assessment of nutritional status among adult and adolescent females: learning from an impoverished Indian state. Public Health. 2020;179:68–75. doi: 10.1016/j.puhe.2019.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Philpott DCE, Belchior-Bellino V, Ververs M. Use of mid-upper arm circumference to screen for thinness among sub-Saharan African male detainees. Public Health Nutr. 2021;24:4777–4785. doi: 10.1017/S1368980021002913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ha L, Hauge T, Iversen PO. Body composition in older acute stroke patients after treatment with individualized, nutritional supplementation while in hospital. BMC Geriatr. 2010;10:75. doi: 10.1186/1471-2318-10-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chakraborty R, Bose K, Bisai S. Mid-upper arm circumference as a measure of nutritional status among adult Bengalee male slum dwellers of Kolkata, India: relationship with self reported morbidity. Anthropol Anz. 2009;67:129–137. doi: 10.1127/0003-5548/2009/0017. [DOI] [PubMed] [Google Scholar]
- 29.Chakraborty R, Bose K, Koziel S. Use of mid-upper arm circumference in determining undernutrition and illness in rural adult Oraon men of Gumla District, Jharkhand, India. Rural Remote Health. 2011;11:1754. [PubMed] [Google Scholar]
- 30.Das P, Khatun A, Bose K, Chakraborty R. The validity of mid-upper arm circumference as an indicator of low BMI in population screening for undernutrition: a study among adult slum dwellers in eastern India. Public Health Nutr. 2018;21:2575–2583. doi: 10.1017/S1368980018001301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.James WPT, Mascie-Taylor GCN, Norgan NG, Bistrian BR, Shetty PS, Ferro-Luzzi A. The value of arm circumference measurements in assessing chronic energy deficiency in Third World adults. Eur J Clin Nutr. 1994;48:883–894. [PubMed] [Google Scholar]
- 32.Shifraw T, Selling K, Worku A, Berhane HY, Ekström EC, Berhane Y. Mid-upper arm circumference for identifying adult overweight in large-scale population-based surveys: Empirical evaluation using data of the EAT Addis study, Ethiopia. BMJ Open. 2021;11:e049602. doi: 10.1136/bmjopen-2021-049602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhu Y, Lin Q, Zhang Y, Deng H, Hu X, Yang X, et al. Mid-upper arm circumference as a simple tool for identifying central obesity and insulin resistance in type 2 diabetes. PLoS One. 2020;15:e0231308. doi: 10.1371/journal.pone.0231308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kok P, Seidell JC, Meinders AE. The value and limitations of the body mass index (BMI) in the assessment of the health risks of overweight and obesity. Ned Tijdschr Geneeskd. 2004;148:2379–2382. [PubMed] [Google Scholar]
- 35.Deurenberg P, Yap M, Van Staveren WA. Body mass index and percent body fat: a meta analysis among different ethnic groups. Int J Obes Relat Metab Disord. 1998;22:1164–1171. doi: 10.1038/sj.ijo.0800741. [DOI] [PubMed] [Google Scholar]
- 36.Zheng HY, Zhang M, Yang CX, Zhang N, Wang XC, Yang XP, et al. Elevated exhaustion levels and reduced functional diversity of T cells in peripheral blood may predict severe progression in COVID-19 patients. Cell Mol Immunol. 2020;17:541–543. doi: 10.1038/s41423-020-0401-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Karastergiou K, Smith SR, Greenberg AS, Fried SK. Sex differences in human adipose tissues - the biology of pear shape. Biol Sex Differ. 2012;3:13. doi: 10.1186/2042-6410-3-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bose K, Ganguly S, Mamtaz H, Mukhopadhyay A, Bhadra M. High prevalence of undernutrition among adult Kora Mudi tribals of Bankura District, West Bengal, India. Anthropol Sci. 2006;114:65–68. doi: 10.1537/ase.050306. [DOI] [Google Scholar]
- 39.Leiter LA, Marliss EB. Survival During Fasting May Depend on Fat as Well as Protein Stores. JAMA. 1982;248:2306–2307. doi: 10.1001/jama.1982.03330180066037. [DOI] [PubMed] [Google Scholar]
- 40.Powell-Tuck J, Hennessy EM. A comparison of mid upper arm circumference, body mass index and weight loss as indices of undernutrition in acutely hospitalized patients. Clin Nutr. 2003;22:307–312. doi: 10.1016/S0261-5614(03)00009-8. [DOI] [PubMed] [Google Scholar]
- 41.Fakier A, ChB M, Petro G, Fawcus S. Mid-upper arm circumference: A surrogate for body mass index in pregnant women. S Afr Med J. 2017;107:606–610. doi: 10.7196/SAMJ.2017.v107i7.12255. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and/or analyzed during the current study are not publicly available (because the manuscript is still under the peer review process) but are available from the corresponding author on reasonable request.