Abstract
HIV/HCV prevention among people who inject drugs (PWID) is of key public health importance. We aimed to assess the impact of COVID-19 and associated response measures on HIV/HCV prevention services and socio-economic status of PWID in high-HIV-risk sites. Sites with recent (2011–2019) HIV outbreaks among PWID in Europe North America and Israel, that had been previously identified, were contacted early May 2020. Out of 17 sites invited to participate, 13 accepted. Semi-structured qualitative site reports were prepared covering data from March to May 2020, analyzed/coded and confirmed with a structured questionnaire, in which all sites explicitly responded to all 103 issues reported in the qualitative reports. Opioid maintenance treatment, needle/syringe programs and antiretroviral treatment /hepatitis C treatment continued, but with important reductions and operational changes. Increases in overdoses, widespread difficulties with food and hygiene needs, disruptions in drug supply, and increased homelessness were reported. Service programs rapidly reformed long established, and politically entrenched, restrictive service delivery policies. Future epidemic control measures should include mitigation of negative side-effects on service provision and socio-economic determinants in PWID.
Supplementary Information
The online version contains supplementary material available at 10.1007/s10461-022-03851-x.
Keywords: HIV, Hepatitis C, COVID-19, People who inject drugs (PWID), Treatment, Prevention, Services, Epidemiology, Social determinants, Outbreaks, Homelessness, Overdose
Resumen
La prevención del VIH/VHC entre las personas que se inyectan drogas (PWID) es de vital importancia para la salud pública. Nuestro objetivo fue evaluar el impacto de COVID-19 y las medidas de respuesta asociadas en los servicios de prevención del VIH/VHC y el estado socioeconómico de las PWID en sitios de alto riesgo de VIH. Se contactó con sitios con brotes recientes (2011–2019) de VIH entre PWID en Europa, América del Norte e Israel, que habían sido previamente identificados, a principios de mayo de 2020. De los 17 sitios invitados a participar, 13 aceptaron. Se prepararon informes cualitativos semiestructurados del sitio que cubrían los datos de marzo a mayo de 2020, analizados/codificados y confirmados con un cuestionario estructurado, en el que todos los sitios respondieron explícitamente a los 103 asuntos reportados en los informes cualitativos. El tratamiento de mantenimiento con opiáceos, los programas de agujas/jeringas y el tratamiento antirretroviral/tratamiento de la hepatitis C continuaron, pero con importantes reducciones y cambios operativos. Se reportaron aumentos en las sobredosis, dificultades generalizadas con las necesidades alimentarias y de higiene, interrupciones en el suministro de medicamentos y aumento de personas sin hogar. Los programas de servicios reformaron rápidamente las políticas restrictivas de prestación de servicios, establecidas desde hace mucho tiempo y políticamente arraigadas. Las futuras medidas de control de epidemias deben incluir la mitigación de los efectos secundarios negativos en la prestación de servicios y los determinantes socioeconómicos en las PWID.
Introduction
COVID-19 has spread worldwide with over 514 million confirmed cases and over 6 million deaths reported globally as of 8 May 2022 [1]. Furthermore, there were an estimated 13.3–16.6 million excess deaths reported due to the COVID-19 pandemic by end of 2021 [2]. Early in the pandemic, in the absence of effective treatment and an adequate vaccine supply, unprecedented hygienic, social distancing, and rolling ‘lockdown’ measures were implemented to reduce transmission and the associated morbidity and mortality burden. As recognized by the United Nations, COVID-19 is far more than a health crisis, affecting societies and economies at their core [3].
People who inject drugs (PWID) have a disproportionate burden of HIV and hepatitis C virus (HCV) infection as compared to the general population [4]. However, the coverage of HIV and HCV prevention interventions for PWID (mainly needle/syringe programs (NSP) and opioid agonist maintenance treatment (OMT)) is variable and remains insufficient overall [5–7]. In many countries, NSP and OMT operate under restrictive rather than needs-based policies resulting in lower than recommended coverage [4, 6, 8–12].
Many PWID have comorbidities, including cardiovascular disease, pulmonary disease, and diabetes, which greatly increases the chances of severe disease in case of a SARS-CoV-2 infection [13]. COVID-19 patients with substance use disorders have been found to be at increased risk for adverse outcomes (hospitalization, ventilator use, death), which seems to be partially mediated by drug-related respiratory and cardiovascular diseases. In addition, as PWID with HIV infection may have a weakened immune system (e.g. low CD4 count, especially if not on effective antiretroviral treatment), they might be at a particularly increased risk for severe illness following COVID-19 infection [14]. Maintaining HIV/HCV prevention in sites with high risk of HIV/HCV spread is therefore of key importance during the COVID-19 pandemic.
Since 2011, multiple HIV outbreaks occurred among PWID, including in Athens (Greece) and Bucharest (Romania) (both 2011), Tel Aviv (Israel, 2012), Luxembourg (2013), Dublin (Ireland, 2014) and Scott County (Indiana US, 2014), Glasgow (UK, 2014), Southeastern Saskatchewan (Canada, 2016) and Seattle & King County (Washington US, 2018) [15, 16]. Although these outbreaks should be compared with caution and they varied in size, common risk factors included: community-wide economic instability, homelessness and marginalization (including of migrants), a history of incarceration, changes in the drug market and drug injection patterns, low or interrupted coverage of prevention measures (in particular OMT, NSP) as well as possible sexual transmission [15–25]. (Panel I) These outbreaks underline the vulnerability of PWID to changes in the economic, social, and drug market contexts as well as the need to monitor and respond rapidly to increases in HIV/HCV [22, 26, 27].
Panel I.
Impact of COVID-19/response measures on known risk factors for HIV outbreaks in sites with recent HIV outbreaks in people who inject drugs in Europe, North America and Israel
| ● Financial/economic problems: increased |
| ● Homelessness and marginalization: increased |
| ● Low or interrupted coverage of prevention measures: only 3 / 13 sites reported high coverage of both NSP and OMT prior to COVID-19/response measures (2 sites had no coverage data). Following COVID-19/response measures, 9 sites reported reduced access to OMT, 10 sites (temporary) NSP closures, 11 sites reduced hours, reduced services and/or closures of social services, 10 sites reported that outreach was reduced, 9 sites reported that drop-in centers closed, etc. |
| ● A history of incarceration: no data (hypotheses: early releases from prison due to COVID-19 have been generally reported that would have resulted in increased numbers of PWID with a (recent) history of incarceration in the community) |
| ● Sexual transmission: no data (hypotheses: economic hardship may lead to increases in sex work but lockdowns may lead to reduction in opportunity for sexwork and other sexual contacts) |
The COVID-19 pandemic has jeopardized essential services for PWID, such as NSP, OMT or antiretroviral HIV treatment (ART) or HCV treatment programs, and increased the risk of overdose [28–32]. Given that areas with recent HIV outbreaks among PWID may be particularly vulnerable for renewed or increased HIV/HCV transmission, disruptions in prevention services for infectious diseases as a consequence of COVID-19 control measures could have more serious consequences than elsewhere. This high vulnerability is underlined by: (1) the HIV outbreaks themselves, i.e. the occurrence of the outbreaks suggests inadequate coverage of prevention services and other structural risk factors, and high prevalence of risk behaviors and (2) once structural and individual risk factors have increased in a population of PWID they are extremely difficult to reverse, so that these sites are at continued high risk, and (3) HIV outbreaks result in a critical mass of HIV infected persons and this, in turn, facilitates further transmission [33]. Disruptions of services due to the COVID-19 pandemic, e.g. regarding NSP, have been reported among sites with no previous HIV outbreaks [34–40]. However, few studies include reports on the wider socio-economic and drug-related settings affecting PWID [38, 39] or HIV/HCV research and surveillance.
Our aim was to assess the early impact of the COVID-19 pandemic and associated control measures on HIV/HCV prevention services, including research, and socio-economic and health determinants of PWID, in high-HIV-risk sites (sites with recent HIV outbreaks in PWID). Our results are particularly relevant for public health, as these sites are at high risk of newly increased HIV transmission in PWID. Covering a multi-national sample of 13 high-HIV-risk sites in Europe, North America and Israel, our results are likely to be less biased by regional policies and more representative of sites with high risk of HIV transmission in PWID in high-income countries.
Methods
Seventeen sites with recent HIV outbreaks in PWID were identified using the EMCDDA (European Monitoring Centre for Drugs and Drug Addiction) and CDC (Centers for Disease Control) databases and through additional literature searches covering North America and Europe (including sites described before) [15, 16, 41–43]. A known outbreak in Israel was also included. The CDC/EMCDDA define an HIV outbreak as “increased HIV transmission among a group of people in an area or in a sexual or social network.” [44] A recent outbreak was defined here as a geographic area with a marked increase in HIV transmission among PWID in any years between 2011 and 2019, as identified through HIV diagnoses and/or HIV surveillance (using prevalence/incidence and/or case reporting data) and/or molecular data analysis. Sites were contacted through public health institutions and lead researchers of (published or grey literature) HIV outbreak studies and invited to assign one or more “site correspondents”. The resulting group of site correspondents included multiple public health lead researchers per site, with mostly long-standing experience in dealing with HIV and people who inject drugs (see authors and affiliations) and with complementary expertise per site (mostly HIV /public health expertise and PWID /prevention /social care expertise). Geographic characteristics of sites varied according to the geographic characteristics of their HIV outbreaks, i.e. site sizes and boundaries were defined by the area affected by the HIV outbreak, where case numbers were markedly higher than in surrounding areas.
Out of 17 sites with recent HIV outbreaks in PWID during 2011–2019 in Europe, North America and Israel, 13 accepted participation in the present study. In total, 10 US sites were invited and 4 were not able to contribute, mainly for capacity reasons related to the COVID-19 response efforts in their sites that needed to be prioritized. The participating sites with previous HIV outbreaks were: (1) Canada: Southeastern Saskatchewan, (2) Greece: Athens, (3) Ireland: Dublin, (4) Israel: Tel Aviv, (5) Luxembourg, (6) Romania: Bucharest, (7) UK: Glasgow, (8) US MN: Hennepin and Ramsey Counties, (9) US OR-WA: Four Counties/Municipalities in Oregon including Portland (Multnomah, Washington and Clackamas Counties, Oregon - Portland metro area), (10) US OH: Hamilton County, 11) US PA: Philadelphia, 12) US IN: Scott County and 13) US WA: Seattle & King County. (Table 1)
Table 1.
Study sample characteristics: PWID population size, HIV transmission and HIV-HCV prevention services before the COVID-19 pandemic, COVID-19 mortality and date of full lockdown$, in 13 sites with recent HIV outbreaks in Europe, North America and Israel
| PWID population & harm reduction | HIV among PWID | COVID-19: date of full lockdown$ and mortality | ||||
|---|---|---|---|---|---|---|
| Site (Year HIV outbreak first observed) |
Population size of PWID (Year) | NSP & OMT coverage* (Year) | Cumulative no. of PWID cases since the start of the outbreak (period) | No. of newly diagnosed cases in PWID (2019: 1 Jan − 31 Dec) | Date of full lockdown | Cumulative no. of COVID-19 deaths by May 1st, 2020 (and rate per million) |
|
Canada: Southeastern Saskatchewan (2016) |
7300 [6500–8200] (2016)2 |
Med/Med (2018)1 |
161 |
1332 31 |
20 March2 |
6 deaths (4.9/M)2 |
|
Greece: Athens (2011) |
1487 (2018)1 |
Med/High (2018)1 |
1713 (2011–2019)3 |
723 | 23 March1,3 | 140 deaths (12.9/M)3 |
|
Ireland: Dublin (2014) |
18,988 (2014)3 |
High/High (2018)3 |
139 (2014–2019)3 |
14 (2018); 11 (2019 – provisional)3 | 27 March3 |
1232 deaths (249/M)3 |
|
Israel: Tel Aviv (2012) |
20,000 (2019)3 |
Med/High (2015-present)3 |
340 (2012–2019)3 |
183 | 25 March3 |
222 deaths (25.6/M)3 |
|
Luxembourg (2013) |
800 (2018)1,3 |
High/High (2017)1,3 |
78 (2014–2019)1,3 |
3 (2019)1,3 |
16 March1,3 |
90 deaths (144/M)1,3 |
|
Romania: Bucharest (2011) |
18,316 (2011) - 19,500 (2019)3 |
Low/Low (2018–2019)3** |
17093 | 883 | 16 March3 |
717 deaths (37.3/M)3 |
|
UK: Glasgow (2014) |
8862 (2006)1 |
High/High (2017–2018)1 |
161 (2015–2019)1 |
25 (2019)1 |
23 March (UK)3 |
1515 deaths (512.9/M) (Scotland)3 |
|
US: Hennepin and Ramsey Counties, MN (2019) |
NA1,2 | NA/NA1,2 |
27 (Dec 2018-Dec 2020)1& |
17 (2019) 11 (2018)1& |
27 March2 |
371 deaths (65.0/M)2 |
|
US: Multnomah, Washington and Clackamas Counties, Oregon - Portland metro area, OR-WA (2018) |
28,000–35,400 (2019)1 |
Med/Med (2018)1 |
83 (2018–2019)1 |
48 (2019)1 |
23 March2 |
300 deaths (152/M)1 |
|
US: Hamilton County, OH (2017) # |
NA1,2 | NA/NA1,2 |
166 (2017–2019) |
59 (2019) |
23 March |
96 deaths (117.5/M) |
|
US: Philadelphia, PA (2018) |
25,000 (2018)1 |
Low/Low (2018)1 |
152 (2018–2019)1 |
83 (2018–2019)1 |
23 March1 |
638 deaths (425.3/M)1 |
|
US: Scott County, IN (2014) |
500 (2014)1 |
Med/Med (2019–2020)1 |
235 (2015–2020)1 |
7 (2019)1 |
24 March2 |
1,007 deaths2 (159.8/M)2 |
|
US: Seattle & King County, WA (2018) |
26,500 (2019)1 |
High/Med (2019)1 |
85 (2018–2019)1 |
30 (2019)1 |
23 March2 |
456 deaths (204.8/M)1 |
1 Outbreak area. 2 Whole state/province (US, Canada). 3 National/whole country. $ For full lockdown details see Table SI in the online supplement. * For NSP (syringes / estimated PWID population size / year): 0-100: low, 100–200: medium, 200+: high; for OMT (% of population of problem opioid users that have been in OMT during a calendar year): 0–20%: low, 20–40%: medium, 40%+: high; as per WHO guidance [11] – note syringe ‘high coverage’ has been since increased to 300+. ** Estimate for Bucharest, elsewhere no services exist since 2017 therefore estimates are ‘low/low’ nationally. & Only PWID, excluding PWID/MSM (there were an additional 26 cumulative PWID/MSM cases in December 2018–2020 and 14 such cases in 2019). # Although the cases here described form the bulk of cases in this outbreak, cases also occurred in neighboring Northern Kentucky. Med: medium. NA: not available. /M: per million population.
A cross-sectional survey was conducted using a qualitative questionnaire with open exploratory questions concerning the impact of the COVID-19 pandemic and associated control measures on the following topics of interest: (i) harm reduction programs and other related services, (ii) HIV screening and ART, (iii) social, economic and health problems (including homelessness), (iv) drug market and drug use patterns, (v) COVID-19 testing, and (vi) research. Collaborators from all 13 sites responded to the invitation, and completed the questionnaire, resulting in 13 detailed site reports (summary of data in Tables SI – SIII, the qualitative questionnaire in Table SIV. Full site reports are available from the authors). Data collection was performed between 4 and 25 May 2020 (final site reports were received 15–25 May). Site correspondents consulted with additional local key experts on specific topics if needed.
Once a full overview of all reported issues across the agreed topics was available from each site via site reports, these reports were summarized into one large overview table (Table SIII) by the lead author. This table was reviewed by site correspondents for completeness and correctness. The reported issues as listed in Table SIII were then separated into shorter and more specific items (i.e. manually coded by the lead author) resulting in a list of 103 items across all sites (Table SII part A), which were once again reviewed by the site correspondents for correctly representing their full site report. These items were then considered short and specific enough to be evaluated /confirmed by all sites.
A second structured questionnaire with closed answer options was administered to the site correspondents, listing all 103 items in an expanded “yes /no /unknown /n.a.” answer format (Table SII part B). This permitted each site to respond explicitly on all issues reported by all sites in the first questionnaire and report additional issues as ‘yes’ (for example meaning: ‘we did not think of this in our initial report but seeing this item was reported by other sites we confirm this also happened in our site’) while also permitting to specify if a negative result in the first questionnaire (item not reported, thus an implicit ‘no-or-unknown’) was a real ‘no’ (meaning: ‘we confirm that this issue-item did not happen in our site’) or if it was in fact an ‘unknown/missing’ or a ‘not applicable’ (‘n.a.’). Given the small sample size (n = 13), data analysis was limited to simple counts of affirmative responses on the different items, then sorting the items by frequency and by an assessment whether the item was describing a COVID-19 impact or a response measure (Table 2 and Fig. 1). Both questionnaires were administered by email as MS Word documents, with the results of the second questionnaire (a structured form with input fields) automatically read by and frequencies calculated in a purpose-built MS Excel tool. We adapted an existing framework for qualitative meta-analyses [45] resulting in what could be described as an innovative exploratory sequential mixed methods study, where we first collected qualitative data, which then informed the creation of a quantitative survey.
Table 2.
Summary of reported impact of COVID-19/response measures (March – May 2020) on HIV-HCV prevention services and social determinants in people who inject drugs, in 13 sites with recent HIV outbreaks in Europe, North America and Israel* (number of sites reporting an issue in brackets, ordered by decreasing frequency)
| TOPIC AREA | CHANGES DUE TO LOCKDOWNS** | RESPONSE MEASURES TO ACCOMMODATE CHANGES |
|---|---|---|
| OMT (Opioid Maintenance Treatment) | Social distancing implemented (13), Decreased access (slight to serious) (9), New intakes stopped or strongly reduced (9), Counseling/support groups stopped (8), Urine testing stopped (6), Mobile outreach stopped (6), Adherence problems (5), Clients relapsed, losing clients (5), | Longer duration/take-home prescriptions started (12), Telemedicine implemented (10), New patients who experienced homelessness accepted (6), New low-threshold OMT service opened (5), OMT expanded, waiting lists cleared (2) |
| NSP (Needle/syringe programs) | Seriously affected or closed (10), all of which improved or (partially) reopened after initial problems (10), PPE problems for staff (10), Service provision moved to outside (8), Less outreach (6) | More supplies given /for longer period /needs based (10), Mobile outreach implemented (8), New services started (food, overdose prevention) (8), home delivery (7), More outreach (4) |
| ART (Anti-Retroviral Treatment) and/or hepatitis treatment | Treatment continued but experienced problems (12), Adherence problems (5) | Treatment continued (13), Telemedicine (11), Longer duration prescriptions (9) |
| OMT, NSP, ART declared ‘Essential services’? | Yes (12), not applicable (1 - in Romania availability is ensured by special law) | |
| HIV/HCV screening /testing | Fully or almost fully suspended (13), of which being (partially) reintroduced during the study period (6), Decrease in reported HIV cases (7) | Self-test offered (4) |
| Other services | Social services affected: reduced hours, reduced services and/or closures (11), Outreach reduced (10), Drop-in centers closed (9), Food provision affected (9) Residential programs reduced or closed (8) Counseling in prisons suspended (5), Restricted access to supervised drug consumption rooms, reduced spaces (2), Indigenous outreach center (providing hot lunches, NSP, and counseling) closed (2) | Implementation of hygiene materials (masks, hand sanitizers, wipes, etc.) for staff and/or clients (13), Food distribution initiated (11), Frontline services provided for PWEH (8), Naloxone: limits on refills mostly removed /actively provided (7), Rural harm reduction services mostly by phone/video (4), Hepatitis A vaccination on site, outreach and delivery (4), Installation of public toilets (3) |
| Research | Face-to-face studies halted or significantly reduced or changed to televisits (10), Problems with confidentiality barriers of remote working (4), HIV industry mostly stopped enrolling trials and face-to-face visits (4), OMT data collection continued e.g. mini web-surveys (4), Grant proposals continued (2) | Continued or new initiated including COVID-19 (8) |
| Drugs market | Shortage and lower quality of drugs on streets, higher price, less availability (9), Harder to secure drugs, open air buying/selling scenes mostly deserted (8), Rumors of more cutting (e.g. with concrete) (6), Using any substances they can access (6), Reduction in heroin availability, increase in tablet use, ‘fake’ benzodiazepines, more street cocaine (6), More use of novel/ synthetic drugs (6), Increased drug and/or syringe sharing due to financial challenges (5), Increased violence and acute mental health issues (5), Lower quality heroin /switch to methadone (4), Decreased ED visits for detox/overdose (3), No change noted /same prices and availability (0) | More police present on the streets (6) |
| Financial, social, health problems | Difficulty to access money (empty streets during lockdown affect possibilities to begging or prostitution) (12), Problems with food (and water) (11), Strong economic impact (10), Mental health problems (due to isolation and increased marginalization) (9), Increased drug sharing and infection risks (7), Housing problems, homeless camps growing, many are PWID (7), Increase in overdoses (7), No increase but continued overdoses (5), Fewer arrests thus less opportunity to test in jail (5), Increased aggressiveness, frustration (4), hepatitis A virus outbreak (2), No major economic, social or health issues (1) | (See Homeless) |
| Homeless | Fear for shelters due to COVID-19 (9), Problems with digital /teleaccess to homeless (9), Problems with food provision in homeless PWID (8), Some or all homeless services ceased or interrupted (8), Increased COVID-19 related stigma (5), Encampments closed or at risk of closing (5), Increase in homeless with mental problems on the street (4), Outbreaks of COVID-19 in homeless settings (4) | Existing shelters continued (11), Additional emergency housing provided (e.g. hotels and shelters) (11), of which: “but some left again” (3), Lack of education on COVID-19 prevention being addressed (9), Hand sanitizer and soap given (8), Range of services provided (6), New (or first ever) shelters set up (5), National guidance on homelessness produced (6), Group-specific shelters: e.g. for PWID, People of color, Queer, Indigenous, General population (3) |
| TOPIC AREA | IMPACT OF COVID-19 | RESPONSE MEASURES TO ACCOMMODATE CHANGES |
| COVID-19 | No or few reported cases in PWID (7), Outbreaks of COVID-19 in homeless settings (4), Outbreaks or ‘many cases’ among PWID (0) | Measurement of the body temperature of clients entering the night shelters (9), Special screening of PWEH and/or PWID (7) |
*Participating sites with recent HIV outbreaks: (1) Canada: Southeastern Saskatchewan (2) Greece: Athens (3) Ireland: Dublin (4) Israel: Tel Aviv (5) Luxembourg (6) Romania: Bucharest 7 UK: Glasgow 8) US MN: Hennepin and Ramsey Counties 9) US OR-WA: Four Counties/Municipalities in Oregon including Portland 10) US OH: Hamilton County 11) US PA: Philadelphia 12) US IN: Scott County 13) US WA: Seattle & King County.
** Lockdowns in the 13 sites started between 16 March and 27 March
Fig. 1.
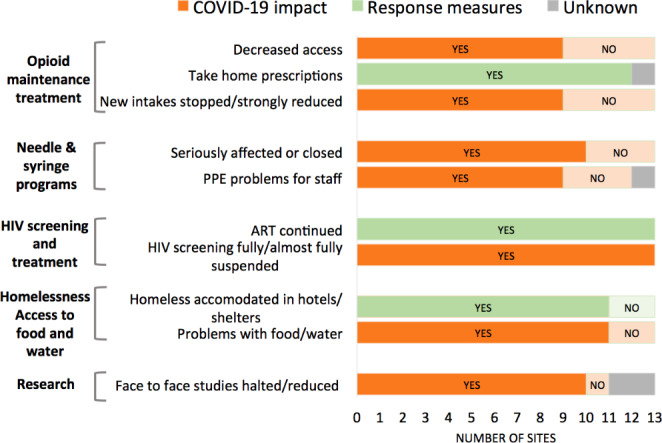
Impact of COVID-19/response measures on HIV-HCV services and social determinants in people who inject drugs, in sites with recent HIV outbreaks in Europe, North America and Israel
Results
Both questionnaires had a 100% response rate, where 77.5% of items in the second questionnaire were other than ‘unknown’ (i.e. specifically reported as a ‘yes’, ‘no’ or ‘n.a.’), with higher rates for selected key items (Fig. 1). Between the first and second questionnaire, the average number of sites reporting ‘yes’ across all items (out of 13, i.e. the maximum possible if all 13 sites would report ‘yes’ on an item), increased over 3-fold (from 1.92 to 6.38, i.e. an increase of 4.46, or 332%; median 4; interquartile range 2.25–6).
Lockdowns with restrictions on all non-essential movement were introduced 16–27 March 2020 in all sites (Tables 1 and SI). The 13 sites were heterogeneous in terms of PWID population size, size of HIV outbreak and coverage of harm reduction programs before the pandemic, with not all sites meeting WHO-recommended levels of service coverage despite the high-HIV-risk context (Table 1) [11]. In almost all sites (n = 12), OMT, NSP, ART were declared to be essential services (in Ireland NSP were not specified but assumed to be covered by ‘drug services’ being declared essential services), with the exception of Romania, where free ART provision and health services are mandated by law since 2002 (Table 2).
Opioid Maintenance Treatment and Needle/Syringe Programs
OMT programs continued but sites reported disruptions, reductions in services and changes in operation including implementing social distancing. Most (n = 9) sites reported a slight to significant decrease in access to OMT programs, including in-person client visits and counseling. In almost all (n = 12) sites, OMT programs tried to adjust to the new situation by starting longer duration/take-home prescriptions and most (n = 10) sites reported implementing telemedicine. In several (n = 6) sites new patients who experienced homelessness were accepted for OMT and (n = 5) new low-threshold OMT services opened (Table 2).
NSP were seriously affected or closed in most (n = 10) sites, all of which (at least partially) opened again by the end of the study period. Most (n = 10) sites reported having problems with sourcing sufficient PPE for staff, while many (n = 8) moved their services outside or (n = 6) had to reduce outreach activities. Most (n = 10) sites compensated decreased NSP access by providing supplies for longer periods /needs based, implementing mobile outreach (n = 8), adding/increasing other services such as food or overdose prevention (n = 8), providing home delivery (n = 7) or expanding outreach in general (n = 4) (Table 2).
HIV/HCV Treatment and Screening
Antiretroviral treatment continued in all 13 sites, although almost all (n = 12) sites experienced problems in continuing the treatment, with five sites reporting reduced adherence. Significant efforts were made to ensure that clients had access to their medication, mostly by implementing telemedicine (n = 11) or longer duration prescriptions (n = 9). (Table 2)
Screenings for HIV and HCV infections drastically decreased or were fully suspended in all sites although in about half (n = 6) of the sites screening was again (partially) reintroduced during the study period and some (n = 4) sites offered self-testing. About half of the sites (n = 7) reported a decrease in reported HIV cases.
Social, Financial and Health Problems Including Homelessness
Almost all (n = 12) sites reported that PWID appeared to have difficulty getting access to money, while most sites reported problems with access to food and water (n = 10) as well as that COVID-19 / response measures had a strong financial impact on PWID (n = 10). Mental health problems (due to isolation and increased marginalization) were also reported by most (n = 9) sites with some (n = 4) sites reporting increased aggressiveness and frustration among PWID. About half (n = 7) of the sites reported increased drug sharing and infection risks, as well as (n = 9) housing problems and camps for people who experience homelessness (PWEH) growing including with many PWID. An increase in overdoses was reported by about half (n = 7) of the sites (all North American sites), while two sites reported hepatitis A outbreaks. (Table 2)
Services provided to PWEH were affected in multiple ways, including decreased access to drop-in centers offering food, showers, laundry and other services, and clusters of cases being detected in shelters). Most sites (n = 9) reported having difficulties reaching PWEH due to COVID-19 related fear within shelters and difficulties in contacting PWEH digitally /via teleaccess (n = 9). Some or all services for PWEH ceased or were interrupted in most (n = 8) sites, several sites (n = 5) reported increased stigma to PWEH, encampments for PWEH were closed or at risk of closure (n = 5), and an increase was reported of PWEH with apparent mental problems on the street (n = 4).
Almost all sites reported strongly increasing support services for PWEH: eleven sites offered temporary accommodation, both by continuing existing shelters (n = 11) and by setting up additional emergency housing including hotels (n = 11) or new or ‘first ever’ shelters (n = 5), often supplemented (n = 6) with a range of (medical and other) services (Table 2).
Drug Market and Drug Use Patterns
Changes in the drug market were reported although these were heterogeneous across sites. Overall, it seemed harder for PWID to secure drugs, with shortages, lower quality and higher prices in most sites (n = 9). About half (n = 6) of sites reported a reduction in heroin availability (with ‘rumors of more cutting (e.g. with concrete)’), more street cocaine and more ‘fake benzodiazepines’, more novel /synthetic drugs and PWID ‘using any substances they could access’ (n = 6). Sites also reported more police presence on the streets (n = 6), increased violence and mental health issues and increased drug and/or syringe sharing due to financial challenges (n = 5).
Research
Research in the area of substance use was affected in most sites. Existing face-to-face studies were either halted or significantly reduced in 10 sites, with 4 sites reporting problems with the confidentiality barriers of remote working and stopping enrolment in trials and face-to-face visits. Research was continued or new research initiated, including on COVID-19, in 8 sites. (Table 2)
COVID-19
Four sites reported COVID-19 outbreaks including in homeless settings serving PWID (PWEH settings, shelters, jails) although outbreak data did not record PWID status and no outbreaks specific to PWID were noted. Special COVID-19 screening among PWEH or PWID was reported by 7 sites with no or few cases found. Nine sites reported body temperature measurement of clients entering night shelters. (Table 2)
Discussion
To our knowledge, this is the first study to report on the initial impact of the COVID-19 pandemic on HIV/HCV prevention and care services in sites with recent HIV outbreaks among PWID (“high risk sites”). All sites reported important disruptions in multiple services, potentially increasing the risk of adverse outcomes such as HIV or HCV infection, while increases in overdoses were reported in 7 out of 13 sites. Several known risk factors for HIV transmission appear to have increased (Panel I). The different sites showed considerable resilience in modifying existing programs, rapidly adapting to the new situation by implementing telemedicine, low-threshold and longer take-home prescriptions of OMT and ART, and larger needs-based NSP provision, often changing entrenched policies to ensure continuity of care. However, despite the high-HIV-risk context, recommended levels of service coverage appeared to be not always met. (Panel II, Table 1)
Panel II.
Examples of the impact of COVID-19/response measures on HIV-HCV services and social determinants in people who inject drugs, in sites with recent HIV outbreaks in Europe, North America and Israel
| OMT |
| ● In particular sites, new homeless patients were accepted (Israel) and a new low-threshold OMT program and medical care service opened for marginalized adult clients currently not (yet) enrolled in a program, independent of having valid health insurance or not (Luxembourg). |
| ● In Dublin (Ireland) OMT continued and expanded, waiting lists were cleared and take-home as well as home delivery were implemented. |
| ● In Tel Aviv (Israel), the demand for in-patient detox treatment increased among homeless female sex-workers due to financial difficulties as a result of brothel closures, concern about potential COVID-19 infection and reduction of drugs distribution. |
| NSP |
| ● In Athens (Greece), NGOs distributed additional syringes via street work. Home delivery was provided in Ireland and in three US sites. |
| ● Some sites introduced new services or expanded existing ones within NSP, such as food (Israel, US PA) and overdose prevention (US PA). |
| ● Novel solutions were implemented such as providing syringes and other materials through windows (Luxembourg). |
| ● NSP have began a needs-based distribution, or a negotiated distribution rather than one-to-one exchange (Seattle & King County, WA) |
| ● Hamilton County Public Health SSP moved to a hybrid needs based model utilizing pre packaged safe use kits. The safe use kits contain: 70 syringes, alcohol wipes, small cottons, tourniquets, cookers, condoms, and small first aid kit. HCPH will continue to this hybrid needs approach model of care/distribution (Hamilton County, OH). |
| HIV and HCV treatment |
| ● Southeastern Saskatchewan (Canada) reported problems in obtaining serology and ART being linked to OMT visits that were moved to telemedicine |
| ● HCV treatment was continued in Dublin (Ireland) and Luxembourg, although new initiations of HCV treatment in this population were suspended. |
| ● Telemedicine was introduced/scaled up to replace physical visits in Southeastern Saskatchewan (Canada), Dublin (Ireland) [67], Tel Aviv (Israel), Luxembourg and three sites in the US (Philadelphia PA, Oregon OR, Seattle & King County WA). |
| ● Five sites reported adherence problems and further sites reported fears for poor adherence, due to e.g. reluctance of PWID to attend appointments or difficulty in reaching PWID who do not have a mobile phone |
| Other services |
| ● The operation of supervised drug consumption rooms was reduced in Luxembourg by limiting the consumption places available at both the supervised injection facility and the ‘blow room’ (non-injected drug consumption room) at the main harm reduction center in Luxembourg city. |
| ● Similarly, drop-in centers were partially or fully suspended in Southeastern Saskatchewan (Canada), Dublin (Ireland), Luxembourg, Athens (Greece) and the sites in Oregon (US OR). |
| ● Counseling services provided in prisons from drug treatment programs were suspended in Athens (Greece), and partially in Luxembourg. |
| ● In Scott County (US IN), large quantities of naloxone were provided for overdose reversals to NSP participants. |
| ● NGOs distributed food from private donations in Luxembourg and Athens (Greece), and PWID received food from NSP centers in Tel Aviv (Israel) and weekly distribution of food boxes was initiated in Philadelphia (US PA). |
| ● A shelter for homeless PWID was set up for the first time in Athens (Greece) offering a wide range of services in collaboration with drug treatment programs; a response team for homeless PWID offered a range of services including accommodation and food in Dublin (Ireland); three shelters were established in Oregon (US OR) (one for Black and Indigenous people of Color, one for individuals identifying themselves as Queer, and one for the general population); accommodation was offered in hotels in Hamilton County (US OH), Glasgow (UK) and Luxembourg; NGOs provided shelter for a number of homeless people in Bucharest (Romania); temporary housing in City-rented hotel space was offered for COVID-19 cases with a range of services (OMT, medical care) in Philadelphia (US PA). |
| COVID-19 screening and research |
| ● Screening for COVID-19 was provided for homeless individuals and/or PWID in five sites: Athens (Greece), Dublin (Ireland), and the US: Hennepin and Ramsey Counties MN, Philadelphia PA [where this was conducted with various successes: few cases were identified among people living unsheltered on the street while cases were largely identified in shelter settings], Seattle & King County WA. |
| ● New research on PWID and COVID-19 was initiated in Athens (Greece), Tel Aviv (Israel) and Luxembourg. |
Several drivers of HIV outbreaks among PWID, i.e. low or interrupted coverage of drug services - in particular of OMT and NSP -, homelessness, economic recession and unemployment, changes in the drug market [15] were strongly exacerbated in most sites. We cannot assess if the quantity and quality of the modified HIV prevention and care services was sufficient to prevent resurgences of HIV or HCV among PWID in these sites, however, resurgences have already been reported in other areas.[46, 47] Also, the short data collection period and the disruption of HIV/HCV screening did not allow for assessing trends in HIV/HCV transmission. However, the increase in overdoses reported in the seven North-American sites (as reported elsewhere, [48–52]), but not in Europe/Israel, suggests that risk factors that may be common for overdoses and HIV outbreaks (e.g. injecting frequency, substance(s) injected, economic instability, homelessness, marginalization, incarceration, low OMT population coverage) may have increased, and possibly more so in North America than in Europe/Israel (possibly in part due to more widespread use - and sudden supply problems - of fentanyl and lower population coverage /individual continuation of OMT) [12, 53–56]. Moreover, increases in drug and/or syringe sharing among PWID as well as multiple other drug market related risks were reported (e.g. shortage and lower quality drugs leading to changes in habitual use potentially increasing risks). (Panel III) However, social distancing measures may have compensated for increases in risk behaviors, while increases in overdose deaths may partly also result from different risk factors (e.g. using alone) than HIV (sharing syringes with others). Some sites were unable to report service coverage, suggesting that they are not sufficiently informed to prevent HIV transmission despite having experienced recent HIV outbreaks.
Panel III.
Examples of changes in the drugs market due to COVID-19/response measures in sites with recent HIV outbreaks in people who inject drugs in Europe, North America and Israel
| Various sites reported changes in the drugs market although these were heterogeneous across those sites. A common characteristic was that it seemed harder for PWID to secure drugs. In Ireland, there was a reduction in heroin availability combined with an increase in tablet use (‘fake’ benzodiazepines) and more street cocaine. In Tel Aviv (Israel), there was a switch back to synthetic drugs, including ‘nice guy’, a synthetic cannabis product that contributed to the HIV outbreak of 2012. In Luxembourg, anecdotal evidence suggested a shortage as well as a lower quality and higher prices of drugs, while the availability was also slightly affected temporarily. Also, less dealers were present on the streets, mainly due to mobility restrictions (including border closures) and more law enforcement, to control violations against confinement measures. An increase in prices was also recorded in Glasgow (UK). In Bucharest (Romania), prices and availability remained stable but heroin was of lower quality, cocaine disappeared and there was a switch to methadone. In Hennepin and Ramsey Counties MN (US), prices were higher and there was increased use of novel substances. In Oregon OR (US), due to changes in availability, PWID reportedly used the substances they could access and increased sharing due to financial challenges. In Philadelphia PA (US), supply was more limited and moved to one area, while the quality of drugs reduced and there were changes in use patterns, as well as a shift in non-opioid drug supplies (cocaine, PCP, methamphetamines) being tainted with fentanyl. In Seattle & King County WA (US), it became harder to secure drugs as open air buying/selling scenes were mostly deserted. |
The serious disruptions and closures of HIV testing and research in the initial phase of the pandemic warrant attention. These disruptions resulted in limiting attention and access to HIV services precisely at the time of a health and social emergency. HIV surveillance (case surveillance, bio-behavioral surveys) and partner services/contact tracing for new HIV diagnoses are core public health functions that contribute to identifying and responding to HIV outbreaks. They were seriously impacted by the COVID-19 pandemic e.g. through decreased HIV testing, reduction in face-to-face encounters, staff having been assigned additional responsibilities for COVID-19 or redeployed to other front line services. Other large, recent outbreaks in the US have occurred that could not be included in this study [16]. It is crucial that research studies and regular HIV testing among PWID be maintained and safe-guarded against future similar interruptions, to be able to rapidly detect new HIV outbreaks and implement actions to contain any outbreaks (including rapid ART initiation).
Mental health problems and violence were reported in several sites, possibly associated with increased marginalization and social exclusion, as reported by other studies [28, 57] This may suggest that additional strategies may be warranted by service providers, such as remaining in contact with PWID by actively approaching them (outreach, including on the streets) or providing more mental health/psychological (dual diagnosis) services, which are challenging tasks when social distancing is required.
Although we did not find direct evidence of enhanced COVID-19 transmission among PWID, four sites (all in the US) reported COVID-19 outbreaks in homeless settings potentially serving PWID, and SARS-CoV-2 testing data in those sites did not include PWID status. These COVID-19 outbreaks may in fact have been facilitated by bringing PWEH together in shelters [58]. This result, coupled with homelessness as a key driver of HIV outbreaks in PWID [15, 16], suggests a need for permanent, individual, housing solutions for PWEH to prevent increases in HIV transmission and improve the social conditions of PWEH and PWID [59]. Moreover, problems with securing sufficient personal protection equipment were widely reported. Thus, particular attention might be given to specific settings where larger numbers of people have prolonged exposure to others, such as shelters for PWEH and jails. It is critical to ensure that PWID are included in vaccination programs despite the often-marginalized status of PWID, including lack of fixed address, identifying documents or lack of mobile phone. Adhering to ART is associated with a much-improved COVID-19 illness course among HIV positive patients [60, 61] suggesting that the high level of ART continuation in our study, despite the often-serious problems in maintaining treatment, may remain important beyond HIV-related outcomes.
Changes in the drug market in the EU have been described, finding higher prices for some drugs, localized shortages of heroin and increases in the use of replacement drugs and alcohol [37–39]. Thus, the unequal economic and social impacts of the pandemic (job and income loss, homelessness) [62] combined with reduced access to services and changes in drug use suggest that the risk of increases in HIV transmission among PWID remains high.
Our study has several limitations. The situation in most sites was dynamic, starting with service disruptions and arcing towards service restoration. Thus, the findings in our short study period, while likely capturing well the initial impact of the pandemic, may no longer apply to more recent time periods. However, there have been repeated waves of resurgence of COVID-19 in many parts of the world by 2022, with re-imposition of various forms of lockdowns potentially resulting in resurgence or continuation of the problems here described. Moreover, our data are primarily qualitative, which limits comparisons of the severity of the problems reported. Also, information was not obtained directly from the clients of the services and we do not have PWID represented in our study group. Clients could have provided valuable insight into the effects of service reductions, but this would have required a different research approach. Including PWID representatives in research and service provision for PWID can be instrumental in reducing barriers to engage and reach PWID in services [63, 64]. Furthermore, our study constitutes a convenience sample (although spanning three continents) of experts from sites with experience with pre-COVID-19 HIV outbreaks, likely to be specifically engaged in avoiding any resurgence of HIV transmission among PWID, which may limit generalisability to other, lower-risk sites. Although we followed a modified framework for qualitative meta-analyses, as we did not perform a systematic literature review we did not register our study in PROSPERO, thus our results should be considered exploratory.
Specific strengths of our study include our ability to include the large majority (14 out 17) sites with identified HIV outbreaks in PWID in Europe, North America and Israel, during 2011–2019. Covering a multi-national sample of 13 high-HIV-risk sites in Europe, North America and Israel, our results are likely to be less biased by regional policies and more representative of PWID sites in high-income countries, especially sites at high risk of HIV outbreaks in PWID. By asking highly qualified site researchers to compile our initial qualitative open questionnaire we covered a broad range of topics in service provision and social context that might not have been captured with a structured questionnaire. These reports were subsequently standardized and confirmed in a quantitative format using a second structured questionnaire, resulting in a more than three-fold increase in the number of confirmed items between the first and second questionnaire. Thus, using an innovative approach, starting with a broad qualitative approach in the 13 sites, then confirming the data in a structured questionnaire with 100% response, we (a) strongly increased the sensitivity, consistency and precision of the data in our study while (b) having been likely more able to capture possible unexpected consequences of the pandemic and related control measures.
This study reveals the implementation of innovations such as rapid service developments, remote care, new harm reduction techniques, and lower threshold access to care, while underlining the challenge of sustaining these COVID-19 prompted improvements in a possible future post-pandemic era [65]. Similar innovations have been reported elsewhere in Europe and are being considered to be maintained [37] - even independently of COVID-19, as they simply represent better/best-practice care and treatment responses for PWID. Services for PWID might benefit in the future from the pandemic-induced experiences of dispensing OMT from a wider array of locations and with extended intervals and with needs-based provision and low-threshold access, while ensuring high population-level coverage remains key [11, 66].
Conclusion
Initial response measures to the COVID-19 pandemic have severely impacted HIV/HCV prevention services and PWID in sites with recent HIV outbreaks. This has potentially resulted in an increased risk for HIV/HCV transmission in these already high-HIV-risk sites. Additional problems included treatment relapses, overdoses, mental health challenges, and shortages of food and shelter for PWEH. Services providers have responded in innovative ways, often reforming entrenched policies. However, despite the high-HIV-risk context, recommended levels of service coverage appear to be not always met. We cannot tell how these high-risk sites might generalize to other areas with similar populations globally. However, it is likely that similar patterns can and will emerge in areas where PWID were affected by lockdowns in access to health and social services. NSP, OMT and ART and other PWID services should maintain their status as essential services and be included in continuity and community recovery plans, expanding where possible (e.g. with mobile outreach) to prevent possible future HIV/HCV increases. As a marginalized socially vulnerable group, PWID’s full participation in COVID-19 vaccination programs should be ensured through special outreach measures with advocacy and support to access the vaccines. Research and surveillance on HIV, HCV and COVID-19 among PWID will be key to detecting and responding to potential HIV, hepatitis or COVID-19 outbreaks in this vulnerable population, including by continued monitoring of service provision and socio-economic situation of PWID. Future epidemic response measures should include mitigation of negative side effects on service provision and socio-economic determinants in PWID.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Acknowledgements
D. Broz and S. Lyss, Centers for Disease Control, Atlanta, US; D. Carlson, Hamilton County Public Health, OH, US; J. Hannink Attal, Department of TB and AIDS, MoH, Jerusalem Israel; D. Liddell, Scottish Drug Forum, Glasgow, UK.
Authors’ Contributions
Lucas Wiessing, Vana Sypsa, Don Des Jarlais: Conceptualization, Methodology, Supervision, Writing - original draft; All authors: Data procurement and curation, Investigation, Writing - review & editing, Approved final manuscript; Lucas Wiessing: Data analysis & Validation, Project management; Vana Sypsa, Don Des Jarlais, Lucas Wiessing: Visualization.
Funding
Don Des Jarlais and Jonathan Feelemyer were supported by NIDA grants R01DA003574 and P30DA001041.
Data Availability (data transparency)
See Appendix in the supplementary file.
Code Availability
Not applicable.
Conflicts of Interest/Competing Interests
None declared.
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Change history
1/7/2023
Space has been included between the Spanish abstract and English abstract. In panels 1 and 2 the lines are updated and in Table 2, a header “TOPIC AREA” has been included before COVID-19 data.
References
- 1.WHO. Weekly epidemiological update on COVID-19 - 11 May 2022. Geneva; 2022. Available from: https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19---11-may-2022
- 2.WHO. 14.9 million excess deaths associated with the COVID-19 pandemic in 2020 and 2021. Geneva; 2022. Available from: https://www.who.int/news/item/05-05-2022-14.9-million-excess-deaths-were-associated-with-the-covid-19-pandemic-in-2020-and-2021
- 3.United Nations. A UN framework for the immediate socio-economic response to COVID-19. April 2020. New York; 2020. Available from: https://unsdg.un.org/sites/default/files/2020-04/UN-framework-for-the-immediate-socio-economic-response-to-COVID-19.pdf
- 4.Degenhardt L, Peacock A, Colledge S, Leung J, Grebely J, Vickerman P, et al. Global prevalence of injecting drug use and sociodemographic characteristics and prevalence of HIV, HBV, and HCV in people who inject drugs: a multistage systematic review. Lancet Glob Health. 2017;5(12):e1192-e207. doi: 10.1016/S2214-109X(17)30375-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mathers BM, Degenhardt L, Ali H, Wiessing L, Hickman M, Mattick RP, et al. HIV prevention, treatment, and care services for people who inject drugs: a systematic review of global, regional, and national coverage. Lancet. 2010;375(9719):1014–28. doi: 10.1016/S0140-6736(10)60232-2. [DOI] [PubMed] [Google Scholar]
- 6.Larney S, Peacock A, Leung J, Colledge S, Hickman M, Vickerman P, et al. Global, regional, and country-level coverage of interventions to prevent and manage HIV and hepatitis C among people who inject drugs: a systematic review. Lancet Glob Health. 2017;5(12):e1208-e20. doi: 10.1016/S2214-109X(17)30373-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wiessing L, Ferri M, Belackova V, Carrieri P, Friedman SR, Folch C, et al. Monitoring quality and coverage of harm reduction services for people who use drugs: a consensus study. Harm Reduct J. 2017;14(1):19. doi: 10.1186/s12954-017-0141-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Des Jarlais DC, McKnight C, Goldblatt C, Purchase D. Doing harm reduction better: syringe exchange in the United States. Addiction. 2009;104(9):1441–6. doi: 10.1111/j.1360-0443.2008.02465.x. [DOI] [PubMed] [Google Scholar]
- 9.Maher L, Iversen J. Syringe exchange in the United States: doing the simple things better? Addiction. 2009;104(9):1448–50. doi: 10.1111/j.1360-0443.2009.02602.x. [DOI] [PubMed] [Google Scholar]
- 10.Friedmann PD, Schwartz RP. Just call it “treatment". Addict Sci Clin Pract. 2012;7(1):10. doi: 10.1186/1940-0640-7-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.WHO, UNODC, UNAIDS. WHO, UNODC, UNAIDS Technical Guide For Countries To Set Targets For Universal Access To HIV Prevention, Treatment And Care For Injecting Drug Users – 2012 Revision. Geneva; 2012. Available from: http://apps.who.int/iris/bitstream/10665/77969/1/9789241504379_eng.pdf?ua=1
- 12.Sordo L, Barrio G, Bravo MJ, Indave BI, Degenhardt L, Wiessing L, et al. Mortality risk during and after opioid substitution treatment: systematic review and meta-analysis of cohort studies. BMJ. 2017;357:j1550. doi: 10.1136/bmj.j1550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vasylyeva TI, Smyrnov P, Strathdee S, Friedman SR. Challenges posed by COVID-19 to people who inject drugs and lessons from other outbreaks. J Int AIDS Soc. 2020;23(7):e25583. doi: 10.1002/jia2.25583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Baillargeon J, Polychronopoulou E, Kuo YF, Raji MA. The Impact of Substance Use Disorder on COVID-19 Outcomes. Psychiatric services (Washington, DC). 2021;72(5):578–81. [DOI] [PMC free article] [PubMed]
- 15.Des Jarlais DC, Sypsa V, Feelemyer J, Abagiu AO, Arendt V, Broz D, et al. HIV outbreaks among people who inject drugs in Europe, North America, and Israel. Lancet HIV. 2020;7(6):e434-e42. doi: 10.1016/S2352-3018(20)30082-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lyss SB, Buchacz K, McClung RP, Asher A, Oster AM. Responding to Outbreaks of Human Immunodeficiency Virus Among Persons Who Inject Drugs-United States, 2016–2019: Perspectives on Recent Experience and Lessons Learned. J Infect Dis. 2020;222(Suppl 5):239-s49. doi: 10.1093/infdis/jiaa112. [DOI] [PubMed] [Google Scholar]
- 17.Giese C, Igoe D, Gibbons Z, Hurley C, Stokes S, McNamara S, et al. Injection of new psychoactive substance snow blow associated with recently acquired HIV infections among homeless people who inject drugs in Dublin, Ireland, 2015. Euro Surveill. 2015;20(40):pii = 30036. doi: 10.2807/1560-7917.ES.2015.20.40.30036. [DOI] [PubMed] [Google Scholar]
- 18.Paraskevis D, Nikolopoulos G, Tsiara C, Paraskeva D, Antoniadou A, Lazanas M, et al. HIV-1 outbreak among injecting drug users in Greece, 2011: a preliminary report. Euro Surveill. 2011;16(36):pii = 19962. doi: 10.2807/ese.16.36.19962-en. [DOI] [PubMed] [Google Scholar]
- 19.Paraskevis D, Nikolopoulos G, Fotiou A, Tsiara C, Paraskeva D, Sypsa V, et al. Economic recession and emergence of an HIV-1 outbreak among drug injectors in athens metropolitan area: a longitudinal study. PLoS ONE. 2013;8(11):e78941. doi: 10.1371/journal.pone.0078941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hatzakis A, Sypsa V, Paraskevis D, Nikolopoulos G, Tsiara C, Micha K, et al. Design and baseline findings of a large-scale rapid response to an HIV outbreak in people who inject drugs in Athens, Greece: the ARISTOTLE programme. Addiction. 2015;110(9):1453–67. doi: 10.1111/add.12999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sypsa V, Paraskevis D, Malliori M, Nikolopoulos GK, Panopoulos A, Kantzanou M, et al. Homelessness and Other Risk Factors for HIV Infection in the Current Outbreak Among Injection Drug Users in Athens, Greece. Am J Public Health. 2015;105(1):196–204. doi: 10.2105/AJPH.2013.301656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sypsa V, Psichogiou M, Paraskevis D, Nikolopoulos G, Tsiara C, Paraskeva D, et al. Rapid Decline in HIV Incidence Among Persons Who Inject Drugs During a Fast-Track Combination Prevention Program After an HIV Outbreak in Athens. J Infect Dis. 2017;215(10):1496–505. doi: 10.1093/infdis/jix100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Arendt V, Guillorit L, Origer A, Sauvageot N, Vaillant M, Fischer A, et al. Injection of cocaine is associated with a recent HIV outbreak in people who inject drugs in Luxembourg. PLoS ONE. 2019;14(5):e0215570. doi: 10.1371/journal.pone.0215570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Golden MR, Lechtenberg R, Glick SN, Dombrowski J, Duchin J, Reuer JR, et al. Outbreak of Human Immunodeficiency Virus Infection Among Heterosexual Persons Who Are Living Homeless and Inject Drugs - Seattle, Washington, 2018. MMWR Morbidity and mortality weekly report. 2019;68(15):344–9. [DOI] [PMC free article] [PubMed]
- 25.McAuley A, Palmateer NE, Goldberg DJ, Trayner KMA, Shepherd SJ, Gunson RN, et al. Re-emergence of HIV related to injecting drug use despite a comprehensive harm reduction environment: a cross-sectional analysis. The Lancet HIV. 2019;6(5):e315-e24. doi: 10.1016/S2352-3018(19)30036-0. [DOI] [PubMed] [Google Scholar]
- 26.Sypsa V. Why do HIV outbreaks re-emerge among people who inject drugs? Lancet HIV. 2019;6(5):e274-e5. doi: 10.1016/S2352-3018(19)30079-7. [DOI] [PubMed] [Google Scholar]
- 27.Wiessing L, Likatavicius G, Hedrich D, Guarita B, van de Laar MJ, Vicente J. Trends in HIV and hepatitis C virus infections among injecting drug users in Europe, 2005 to 2010. Euro Surveill. 2011;16(48):pii = 20031. doi: 10.2807/ese.16.48.20031-en. [DOI] [PubMed] [Google Scholar]
- 28.Bolinski RS, Walters S, Salisbury-Afshar E, Ouellet LJ, Jenkins WD, Almirol E, et al. The Impact of the COVID-19 Pandemic on Drug Use Behaviors, Fentanyl Exposure, and Harm Reduction Service Support among People Who Use Drugs in Rural Settings. Int J Environ Res Public Health. 2022;19(4):2230. doi: 10.3390/ijerph19042230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Trayner KMA, McAuley A, Palmateer NE, Yeung A, Goldberg DJ, Glancy M, et al. Examining the impact of the first wave of COVID-19 and associated control measures on interventions to prevent blood-borne viruses among people who inject drugs in Scotland: an interrupted time series study. Drug Alcohol Depend. 2022;232:109263. doi: 10.1016/j.drugalcdep.2021.109263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Aponte-Melendez Y, Mateu-Gelabert P, Fong C, Eckhardt B, Kapadia S, Marks K. The impact of COVID-19 on people who inject drugs in New York City: increased risk and decreased access to services. Harm Reduct J. 2021;18(1):118. doi: 10.1186/s12954-021-00568-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mistler CB, Curley CM, Rosen AO, El-Krab R, Wickersham JA, Copenhaver MM, et al. The Impact of COVID-19 on Access to HIV Prevention Services Among Opioid-Dependent Individuals. J Community Health. 2021;46(5):960–6. doi: 10.1007/s10900-021-00979-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Public Health England, Health Protection Scotland, Public Health Wales, Public Health Agency Northern Ireland. Shooting Up: infections and other injecting-related harms among people who inject drugs in the UK, 2020 - an update December 2021. London; 2022 11/2016. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1053202/Shooting_Up_2021_report_final.pdf
- 33.Roussos S, Paraskevis D, Psichogiou M, Kostaki EG, Flountzi E, Angelopoulos T, et al. Ongoing HIV transmission following a large outbreak among people who inject drugs in Athens, Greece (2014-2020). Addiction. 2021. [DOI] [PubMed]
- 34.Glick SN, Prohaska SM, LaKosky PA, Juarez AM, Corcorran MA, Des Jarlais DC. The Impact of COVID-19 on Syringe Services Programs in the United States. AIDS Behav. 2020;24(9):2466–8. doi: 10.1007/s10461-020-02886-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Whitfield M, Reed H, Webster J, Hope V. The impact of COVID-19 restrictions on needle and syringe programme provision and coverage in England. Int J Drug Policy. 2020;83:102851. doi: 10.1016/j.drugpo.2020.102851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bartholomew TS, Nakamura N, Metsch LR, Tookes HE. Syringe services program (SSP) operational changes during the COVID-19 global outbreak. Int J Drug Policy. 2020;83:102821. doi: 10.1016/j.drugpo.2020.102821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.EMCDDA. EMCDDA trendspotter briefing. May 2020. Impact of COVID-19 on drug services and help-seeking in Europe. Luxembourg; 2020. Available from: https://www.emcdda.europa.eu/system/files/publications/13073/EMCDDA-Trendspotter-Covid-19_Wave-1-2.pdf
- 38.EMCDDA & Europol. EU Drug Markets: Impact of COVID-19. Luxembourg; 2020. Available from: https://www.emcdda.europa.eu/publications/joint-publications/eu-drug-markets-impact-of-covid-19_en
- 39.EMCDDA & Europol. Impact of COVID-19 on drug markets, use, harms and drug services in the community and prisons. Luxembourg; 2021. Available from: https://www.emcdda.europa.eu/system/files/publications/13745/TD0321143ENN_002.pdf
- 40.WHO. The impact of COVID-19 on mental, neurological and substance use services: results of a rapid assessment. Geneva; 2020. Available from: https://www.who.int/publications/i/item/978924012455
- 41.Slemp C. WV Health Alert Network - Health Advisory #162 - Human Immunodeficiency Virus (HIV) Infections Among People Who Inject Drugs - Additional Area Seeing Increase, Others Vulnerable. West Virginia Department of Health and Human Resources, Bureau for Public Health; 2019. Available from: https://oeps.wv.gov/healthalerts/documents/wv/WVHAN_162.pdf
- 42.Minnesota Department of Health. Health Advisory: HIV Outbreak in Persons Who Inject Drugs (PWID). Minnesota Department of Health; 2020. Available from: https://www.health.state.mn.us/communities/ep/han/2020/feb3hiv.pdf
- 43.Madoff L, Brown CM, Lo JJ, Sánchez S. Increase in newly diagnosed HIV infections among persons who inject drugs in Boston. Massachusetts Department of Public Health, Boston Public Health Commission; 2021. Available from: https://view.officeapps.live.com/op/view.aspx?src=https%3A%2F%2Fwww.mass.gov%2Fdoc%2Fjoint-mdph-and-bphc-clinical-advisory-hiv-transmission-through-injection-drug-use-in-boston-march-15-2021%2Fdownload
- 44.CDC. HIV Cluster and Outbreak Detection and Response 2022. Available from: https://www.cdc.gov/hiv/programresources/guidance/cluster-outbreak/index.html
- 45.Levitt HM. How to conduct a qualitative meta-analysis: Tailoring methods to enhance methodological integrity. Psychother research: J Soc Psychother Res. 2018;28(3):367–78. doi: 10.1080/10503307.2018.1447708. [DOI] [PubMed] [Google Scholar]
- 46.Hershow RB, Wilson S, Bonacci RA, Deutsch-Feldman M, Russell OO, Young S, et al. Notes from the Field: HIV Outbreak During the COVID-19 Pandemic Among Persons Who Inject Drugs—Kanawha County, West Virginia, 2019–2021. Morb Mortal Wkly Rep. 2022;71(2):66. doi: 10.15585/mmwr.mm7102a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sypsa V, Tsirogianni E, Trafali D, Tsiagka D, Gavalaki A, Papanikolaou Z, et al. Estimated HIV prevalence and incidence among people who inject drugs in Thessaloniki, Greece (ALEXANDROS program). 11th IAS Conference on HIV Science, 18–21 July 2021 (virtual); 2021.
- 48.Glober N, Mohler G, Huynh P, Arkins T, O’Donnell D, Carter J, et al. Impact of COVID-19 Pandemic on Drug Overdoses in Indianapolis. J urban health: Bull New York Acad Med. 2020;97(6):802–7. doi: 10.1007/s11524-020-00484-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Slavova S, Rock P, Bush HM, Quesinberry D, Walsh SL. Signal of increased opioid overdose during COVID-19 from emergency medical services data. Drug Alcohol Depend. 2020;214:108176. doi: 10.1016/j.drugalcdep.2020.108176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Rodda LN, West KL, LeSaint KT. Opioid Overdose-Related Emergency Department Visits and Accidental Deaths during the COVID-19 Pandemic. J urban health: Bull New York Acad Med. 2020;97(6):808–13. doi: 10.1007/s11524-020-00486-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Friedman J, Akre S. COVID-19 and the Drug Overdose Crisis: Uncovering the Deadliest Months in the United States, January–July 2020. Am J Public Health. 2021:e1-e8. [DOI] [PMC free article] [PubMed]
- 52.Ochalek TA, Cumpston KL, Wills BK, Gal TS, Moeller FG. Nonfatal Opioid Overdoses at an Urban Emergency Department During the COVID-19 Pandemic. JAMA. 2020;324(16):1673–4. doi: 10.1001/jama.2020.17477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Uuskula A, Raag M, Vorobjov S, Rüütel K, Lyubimova A, Levina OS, et al. Non-fatal overdoses and related risk factors among people who inject drugs in St. Petersburg, Russia and Kohtla-Jarve, Estonia. BMC Public Health. 2015;15:1255. doi: 10.1186/s12889-015-2604-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.O’Donnell J, Tanz LJ, Gladden RM, Davis NL, Bitting J. Trends in and Characteristics of Drug Overdose Deaths Involving Illicitly Manufactured Fentanyls - United States, 2019–2020. MMWR Morbidity and mortality weekly report. 2021;70(50):1740–6. [DOI] [PMC free article] [PubMed]
- 55.Wiessing L, Likatavicius G, Klempova D, Hedrich D, Nardone A, Griffiths P. Associations between availability and coverage of HIV-prevention measures and subsequent incidence of diagnosed HIV infection among injection drug users. Am J Public Health. 2009;99(6):1049–52. doi: 10.2105/AJPH.2008.141846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Chang JS, Behar E, Coffin PO. Narratives of people who inject drugs on factors contributing to opioid overdose. Int J Drug Policy. 2019;74:26–32. doi: 10.1016/j.drugpo.2019.07.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Stack E, Leichtling G, Larsen JE, Gray M, Pope J, Leahy JM, et al. The Impacts of COVID-19 on Mental Health, Substance Use, and Overdose Concerns of People Who Use Drugs in Rural Communities. Journal of Addiction Medicine. 2020. [DOI] [PMC free article] [PubMed]
- 58.Tang JW, Marr LC, Li Y, Dancer SJ. Covid-19 has redefined airborne transmission. BMJ. 2021;373:n913. doi: 10.1136/bmj.n913. [DOI] [PubMed] [Google Scholar]
- 59.Wiessing L, Seguin-Devaux C, Merendeiro CS. Could the COVID-19 Crisis Help Eradicate Chronic Homelessness? Am J Public Health. 2021;111(1):25–6. doi: 10.2105/AJPH.2020.306015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Del Amo J, Polo R, Moreno S, Díaz A, Martínez E, Arribas JR, et al. Incidence and Severity of COVID-19 in HIV-Positive Persons Receiving Antiretroviral Therapy: A Cohort Study. Ann Intern Med. 2020;173(7):536–41. doi: 10.7326/M20-3689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hadi YB, Naqvi SFZ, Kupec JT, Sarwari AR. Characteristics and outcomes of COVID-19 in patients with HIV: a multicentre research network study. Aids. 2020;34(13):F3-f8. doi: 10.1097/QAD.0000000000002666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Bambra C, Riordan R, Ford J, Matthews F. The COVID-19 pandemic and health inequalities. J Epidemiol Commun Health. 2020;74(11):964–8. doi: 10.1136/jech-2020-214401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Friedman SR, Maslow C, Bolyard M, Sandoval M, Mateu-Gelabert P, Neaigus A. Urging others to be healthy: “intravention” by injection drug users as a community prevention goal. AIDS Educ prevention: official publication Int Soc AIDS Educ. 2004;16(3):250–63. doi: 10.1521/aeap.16.3.250.35439. [DOI] [PubMed] [Google Scholar]
- 64.Small W, Wood E, Tobin D, Rikley J, Lapushinsky D, Kerr T. The Injection Support Team: a peer-driven program to address unsafe injecting in a Canadian setting. Subst Use Misuse. 2012;47(5):491–501. doi: 10.3109/10826084.2012.644107. [DOI] [PubMed] [Google Scholar]
- 65.Grebely J, Cerdá M, Rhodes T. COVID-19 and the health of people who use drugs: What is and what could be? Int J Drug Policy. 2020;83:102958. doi: 10.1016/j.drugpo.2020.102958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Del Pozo B, Rich JD. Revising our attitudes towards agonist medications and their diversion in a time of pandemic. J Subst Abuse Treat. 2020;119:108139. doi: 10.1016/j.jsat.2020.108139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Crowley D, Homeniuk R, Delargy I. Scoping review protocol: the use of telemedicine in providing opioid agonist treatment and related psychosocial supports. BMJ Open. 2020;10(12):e040556. doi: 10.1136/bmjopen-2020-040556. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
See Appendix in the supplementary file.
Not applicable.


