Abstract
Purpose of Review
Since 2007, voluntary medical male circumcision (VMMC) programs have been associated with substantially reduced HIV incidence across 15 prioritized countries in Eastern and Southern Africa. Drawing on the programmatic experience of global VMMC leaders, this report reviews progress made in the first 15 years of the program, describes programmatic and research gaps, and presents considerations to maximize the impact of VMMC.
Recent Findings
Overall, key programmatic and research gaps include a lack of robust male circumcision coverage estimates due to limitations to the data and a lack of standardized approaches across programs; challenges enhancing VMMC uptake include difficulties reaching populations at higher risk for HIV infection and men 30 years and older; limitations to program and procedural quality and safety including variations in approaches used by programs; and lastly, sustainability with limited evidence-based practices. Considerations to address these gaps include the need for global guidance on estimating coverage, conducting additional research on specific sub-populations to improve VMMC uptake, implementation of responsive and comprehensive approaches to adverse event surveillance, and diversifying financing streams to progress towards sustainability.
Summary
This report’s findings may help establish a global VMMC research and programmatic agenda to inform policy, research, and capacity-building activities at the national and global levels.
Keywords: HIV prevention, Voluntary medical male circumcision, HIV/AIDS, Sub-Saharan Africa
Introduction
Voluntary medical male circumcision (VMMC) was first formally recommended in 2007 by the World Health Organization (WHO) and the Joint United Nations Programme on HIV/AIDS (UNAIDS) as an effective and essential HIV prevention strategy [1]. Since this recommendation, important advances have been made by VMMC programs in prioritized countries in Eastern and Southern Africa [2, 3]. These advances offer lessons learned, helping to identify opportunities for future programmatic growth. Drawing on the programmatic experience and expertise of global VMMC stakeholders, this report presents the progress made since 2007, programmatic gaps, and potential responses needed for VMMC to maximize its contribution to the 2030 targets to end the AIDS epidemic. The suggestions for considerations represent the shared opinion of authors leading the global VMMC portfolios of major funding agencies and organizations and international implementing agencies. The two questions this report seeks to answer are, first, what are the remaining research and programmatic gaps, and, second, what additional efforts may be considered to address these needs.
Background
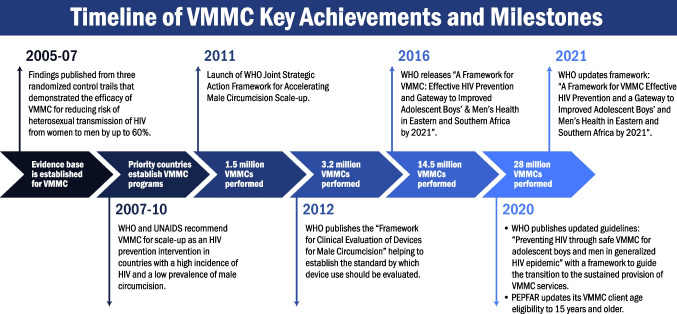
In 2007, WHO and UNAIDS’s recognition of VMMC as an efficacious prevention strategy was prompted by findings from randomized controlled trials (RCTs) conducted in Kenya, Uganda, and South Africa, demonstrating a reduction in the acquisition of HIV in men by up to 60% (Fig. 1) [4–7]. Countries with generalized HIV epidemics and low national or subnational male circumcision prevalence were prioritized following this global guidance. Countries originally prioritized included Botswana, Eswatini, Ethiopia, Kenya, Lesotho, Malawi, Mozambique, Namibia, Rwanda, South Africa, United Republic of Tanzania, Uganda, Zambia, and Zimbabwe, with South Sudan establishing a program in 2018 [8•]. The VMMC programs were country-led and incorporated into national HIV prevention portfolios with funding support primarily provided by the U.S. President’s Emergency Plan for AIDS Relief (PEPFAR) and national governments [2, 9]. It was recommended VMMC be offered as part of a package of services including the surgical removal of the foreskin, voluntary HIV testing, links to HIV care and treatment, HIV risk reduction education, condom provision, and referrals for screenings or treatment when patients are diagnosed with other sexually transmitted infections (STIs) [1, 10].
Fig. 1.
Timeline of VMMC key achievements and milestones
In 2011, WHO and UNAIDS published a framework to guide the development of VMMC programs [11]. The framework described two phases of the program and presented global targets to maximize the impact on HIV incidence. The first phase was initially intended to conclude by 2016 with circumcision coverage of at least 80% among 15–49-year-old males [2]. The expectation was once the first phase was completed; the high coverage achieved among older males would mean high-volume VMMC services would no longer be needed for these clients. However, the initial phase of the program continued beyond the intended timeline largely due to the policy and programmatic challenges of establishing and scaling up an elective surgical public health intervention and changes to the global male circumcision coverage targets based on updated modeling. By the end of 2010, the original 14 prioritized countries had all established national programs, and between 2007 and 2014, over 9 million VMMCs were performed [12]. The program experienced performance decreases of nearly 9% in 2015 and 2016, primarily due to reductions in global funding. However, in 2017, there was an increase to 4.0 million VMMCs performed compared to 2.8 million in 2016 due to an increase in PEPFAR funding [13]. The annual growth continued until 2020 when programs experienced a reduction in the number of VMMCs performed largely due to the COVID-19 pandemic. From 2007 to 2020, 26.8 million VMMCs were performed [14, 15].
From 2007 to 2020, adolescents aged 10–14 years comprised the greatest proportion of VMMC clients. In 2020, there was a shift in the age distribution of VMMC clients due to updated global guidance and changes in PEPFAR’s age eligibility restricting procedures to clients 15 years and older [16••, 17••]. PEPFAR made this policy decision following a data review showing a higher rate of adverse events (AEs) associated with VMMC in clients 10–14 years of age. Thus, despite its success, the scale-up phase did not follow the original projections for the program, given younger adolescents represented a disproportionally greater client volume than was expected in most countries, and uptake was somewhat stagnant among men 30 years and older [18].
After the initial scale-up phase, programs were meant to enter a second phase, the sustainability phase, where the focus would shift to younger adolescents and infants who were not eligible for VMMC during the first phase. Programs were intended to enter this phase once they had achieved at least 80% male circumcision coverage among 15–49-year-old males. Each country established a national program providing VMMC services to all infants up to 2 months old. During the implementation of this second phase, VMMC services were also meant to be integrated into national health systems. In practice, both proposed phases of the program were implemented differently from the original plan.
Although VMMC programs were implemented differently than initially planned, the growth and achievements of the VMMC program to date carry immediate and future benefits [19]. By 2020, the nearly 27 million VMMCs performed were estimated to have averted 340,000 new HIV infections [20]. The impact of medical male circumcision is estimated to be significantly more substantial on HIV incidence than non-medical circumcision. Unlike medical circumcision which is a standardized surgical procedure, the amount of foreskin removed during non-medical circumcision is not uniform, and the protective effects for HIV and STI prevention vary [21, 22]. Although VMMC programs have focused primarily on circumcision to prevent HIV among males, there is evidence demonstrating reductions in STI transmission in both men and women and reductions in cervical cancer in women [23, 24•, 25•]. To ensure VMMC programs continue to contribute to population-level benefits, it is important to understand the research and programmatic gaps hindering the progress of the program and the opportunities to progress.
Programmatic and Research Gaps and Priority Actions
This section outlines relevant VMMC programmatic and research gaps and recommends priority steps to address them (Table 1). Identifying and responding to these challenges is important considering some programs are reaching high VMMC coverage requiring an updated programmatic focus and technical support.
Table 1.
VMMC programmatic and research gaps and recommended priority actions for prioritized countries
| VMMC program area | Programmatic and research gaps | Recommended priority actions |
|---|---|---|
| Estimating male circumcision coverage | National programmatic planning to reach HIV epidemic control benchmarks remains a challenge, particularly in areas with dynamic or limited denominator data | Global guidance for standardized data inputs and statistical processes to measure male circumcision coverage |
| Robust estimates of VMMC coverage, particularly for subnational areas, are limited by the data currently available | Country-level strategies to ensure high-quality data (timely, accurate, and complete) to provide robust data inputs | |
| Standardized male circumcision module for country-level adaption in surveys, particularly to improve reporting of type of circumcision (medical or non-medical) | ||
| When possible, adapt study design and statistical power of household surveys to improve measurement of male circumcision coverage | ||
| Country-level support for establishing programmatic strategies to support long-term and sustainable efforts to estimate high coverage of VMMC | Global guidance and adaptable frameworks for identifying male circumcision coverage gaps among sub-populations with lower coverage | |
| Enhancing uptake | Low uptake among specific groups of men who have lower circumcision coverage and are at higher risk for HIV, particularly among specific occupational groups such as fisherfolk, truck drivers, miners, and seasonal workers | Greater research on behavioral drivers of uptake, including use of compensation or incentives and when programs should use them |
| Investigation of generalizability or consistency of factors that account for segmentation of VMMC clients | ||
| Low uptake among older age groups (≥ 30 years) and lack of specialized approaches to target key groups | Leverage mapping and analytic technology, such as geographic information systems, to optimize use of resources and service provision | |
| Demand creation activities that communicate the benefits of VMMC to individuals and partners to address behavioral and interpersonal barriers | ||
| Examine the cost/benefit of targeting clients 30 years and older | ||
| Innovative technological limits due to gaps in specialized knowledge, infrastructure, and financial resources for demand creation | Digital and social media demand creation packages that can be adapted to meet the needs of each VMMC prioritized country | |
| Gaps in research to better understand the use of device-based male circumcision including ShangRing© compared to conventional surgical approaches | Understand preferences for type of male medical circumcision procedure offered, and the impact of device availability on VMMC uptake | |
| Quality and safety | Lack of a standardized approach to appropriately manage certain severe adverse events | Establish a network to share safety and adverse event experiences across VMMC programs to improve outcomes |
| Develop a responsive, standardized, and comprehensive approach to adverse event surveillance | ||
| Categorization of attributes of clients at higher risk for AEs or with compliance challenges to improve and potentially prevent adverse outcomes | ||
| Lack of standardized communication of benefits and risks of the procedure to aid clients’ decision-making process and lack of specific guidance on how best to assess capacity for informed consent/assent, particularly for younger age bands (≤ 19 years) | Create a comprehensive and easily understandable communication guide on the benefits and risk (i.e., standardize summaries) to strengthen client’s decision-making abilities during the informed consent process | |
| Global guidance to improve assessment of readiness of younger clients (≤ 19 years) and parents/guardian to comprehend benefits and risks of VMMC | ||
| Lack of focus on the quality and safety of program areas beyond the procedure, such as sexual health, HIV testing services, demand creation, education, and communication for the client | Review and improve materials, standard operating procedures, and checklists for client counseling on sexual health, HIV testing services, referrals, etc | |
| Sustainability | Each service delivery and strategic planning component needed to achieve sustainability for VMMC programs remains relatively unknown | Strategic inclusion of WHO health systems six building blocks and components framework for sustainable VMMC services into national planning (Table 2) |
| Limited evidence-based sustainability practices to inform planning for sustainability | Measuring country progression towards sustainability is critical for countries to understand and assess their transition and identify needed support as well as best practices. Compiling country efforts towards sustainability will help to establish an evidence base and provide lessons learned | |
| Limited understanding of long-term workforce needs to sustain VMMC services | Engaging ministries of health and finance, in addition to policymakers, for VMMC integration and long-term workforce planning into national health priorities | |
| Lack of diversified funding and need for commitment to non-donor supported funding | Diversified financing schemes that include both domestic and external funding and greater resource mobilization through engagement of ministries of health and finance |
Estimating Male Circumcision Coverage
Circumcision coverage estimates play a critical role in VMMC program planning, target setting, and monitoring progress towards HIV epidemic control goals. The VMMC programs use a variety of survey and sampling methodologies, statistical tools, and data to estimate coverage. National household surveys, including the Population-based HIV Impact Assessment (PHIA) and the Demographic and Health Surveys (DHS), are commonly used to inform the estimation of VMMC coverage [21, 26, 27••]. However, evidence suggests male circumcision coverage estimates are unreliable with inconsistencies between data sources, coverage continuously exceeding 100% in some areas, and continued high demand in areas with high estimated coverage [28].
There are limitations to national household surveys when used to estimate coverage. Typically, the subnational circumcision estimates are less robust than national-level estimates when using national household surveys. Less robust estimates at the subnational level are partly because of inaccurate or dynamic denominator data with limited information on internal and external population migration, particularly in countries with older census data, high mobility, or areas with an unstable population with a high proportion of unregistered immigrants, migrant workers, and refugees. This denominator issue is particularly pronounced in countries where granular clinical data are missing at lower administrative levels and in countries with great variation in coverage across geographic regions. The lack of robust subnational-level estimates is partly because national household surveys are not designed statistically for estimating male circumcision coverage.
Additionally, there are limitations to how male circumcision is measured, usually through self-report, with challenges distinguishing medical and non-medical male circumcision. Previous research has found conflicting findings with self-reported circumcision status may be subject to reporting errors in some settings. At the same time, in other areas, there is high concurrence with physical exams [29, 30]. These inconsistencies can lead to over- and underestimating male circumcision coverage and an overall lack of robust and comparable estimates.
According to anecdotal reports, another challenge to estimating accurate coverage is VMMC may be “replacing” non-medical male circumcision in some settings. However, the models and tools used to estimate coverage sometimes assume the proportion of non-medical male circumcision in a national population remains constant. Therefore, additional research is needed to estimate non-medical male circumcision coverage more precisely in various settings.
Robust estimation of male circumcision coverage is important for all aspects of the program but is particularly critical for setting program targets. UNAIDS establishes VMMC targets roughly every 5 years, aligning with goals for ending the AIDS epidemic. Prioritized countries adopt these targets nationally, typically establishing 5-year plans to reach these goals. In addition, PEPFAR supports national governments in establishing program targets annually. However, the accuracy of these targets, particularly at the subnational level, is limited by the reliability of male circumcision coverage estimates discussed above. Overall, there has also been a lack of a standardized approach to establishing coverage estimates and set targets. In 2020, the UNAIDS Reference Group on Estimates, Modeling, and Projections, along with partners, worked with prioritized countries to integrate VMMC into the UNAIDS HIV estimates process to standardize the process [31, 32]. However, official global guidance for standardized estimation of circumcision coverage is needed to enable routine monitoring and more accurate and precise male circumcision coverage estimates.
Defining the types of data collected to supplement national household surveys could help countries determine when additional survey data is needed and which sources are best used in triangulating data. Guidance may be helpful to identify programmatic and service delivery gaps among specific eligible sub-populations with lower male circumcision coverage. Establishing standardized framework countries could easily adapt for estimating coverage at the district or lower administrative level or help identify pockets of low coverage could increase reliability in estimates. Additionally, improvements can be made to national household surveys to improve the accuracy of VMMC reporting. For example, a standardized male circumcision module could be included in national household surveys to more accurately document circumcision status among males through direct observation of circumcision status. As countries reach higher male circumcision coverage, estimating VMMC coverage will become increasingly challenging considering, as coverage rises, estimates become increasingly sensitive to errors in target population estimates.
Enhancing Uptake
Despite the success of the VMMC program, there is an ongoing effort to improve strategies to increase VMMC uptake to reduce HIV incidence to reach epidemic control. Programs currently use a variety of approaches and strategies to tailor the most successful interventions for enhancing uptake [17••, 33–35]. However, key gaps remain in understanding factors accounting for the choice to undergo the procedure, including motivators, barriers, and experiences [31, 36]. Programs have reported challenges reaching specific groups of men, some of whom are at higher risk of HIV infection and hard to reach for services. Hard-to-reach groups commonly include mobile workers, fishermen, truck drivers, miners, and seasonal workers [17••, 37•]. Populations at higher risk such as men diagnosed with STIs, male partners of female sex workers, and serodiscordant partnerships can also pose specific demand creation challenges [38, 39]. Another important programmatic challenge is the limited voluntary uptake of circumcision among males 30 years and older who are more likely to be married or cohabiting, finding it challenging to justify VMMC to their partners [40].
Programs are also facing a digital divide. There is varying capacity to implement technology in social media campaigns across prioritized countries. Only programs with the specialized knowledge, infrastructure, and financial resources to develop the mobile tools have the advantage of utilizing the algorithms social media affords reaching targeted groups with tailored messaging. Programs have experienced recent success in using innovative technology to target specific audiences through social media, particularly to engage older men [41].
A promising strategy for improving uptake of VMMC is psychographic-behavioral segmentation, using human-centered design (HCD). Through segmentation, potential VMMC clients are categorized according to certain characteristics, which allows for specific messaging based on a client’s profile [42]. Initial studies found differing client characteristics in Zimbabwe and Zambia, indicating the importance of tailored interventions [43, 44]. Another important factor for increasing uptake is understanding the stage of change in which the client is in when they are approached for VMMC [45]. Additional evidence is needed to understand how readiness for the procedure relates to the uptake of services. In addition to psychographic approaches, demographic and geographic segmentation are important for developing a strategic approach to demand generation. Demographic segmentation may be useful for increasing uptake among older age groups, because demand creation approaches are specifically tailored to address their needs. Another demographic segmentation factor for consideration is a client’s financial status. Wage loss from time off work for recovery after VMMC, including the perceived time needed, has differential effects on men depending on their financial status. More information is needed to understand situations in which compensation or incentives are most sensible for programs to offer and leverage proven approaches to reach different sub-demands. Geographic segmentation by clustering clients according to their location could benefit demand creation planning. Mapping and analytic technology such as geographic information systems can help programs plan for optimal use of resources and guide services with the greatest potential for VMMC conversion.
Device-based male circumcision may influence men’s perceptions of VMMC and may be a promising approach to increase uptake [17••, 46]. However, gaps still exist on whether device-based male circumcision increases demand among those previously hesitant or merely replaces surgical VMMC among those who eventually would have sought services. Research is also needed on the cost/benefit of targeting older men (≥ 30 years) for VMMC when fewer resources are believed to be required for demand generation targeting younger age groups (≤ 19 years) [47]. Once a program has reached high coverage and shifted towards sustainability, strategies to enhance uptake could focus on males aging into eligibility [48] with ongoing evaluations to ensure strategies continue to be effective on newly eligible clients.
Quality and Safety
Voluntary medical male circumcision is a preventive procedure typically performed on healthy males. Safety has been a critical priority for VMMC programs, and VMMC has demonstrated it is a safe procedure. Adverse events have been monitored since program inception, and overall, < 2% of VMMC clients have been identified through passive reporting as having moderate or severe AEs [49, 50]. In addition, national VMMC programs have made critical adjustments in response to safety signals, such as implementing mitigation measures in response to tetanus cases associated with VMMC, halting the use of forceps-guided circumcisions in clients 10–14 years old, enhancing pre-circumcision screening for bleeding disorders, and raising client age eligibility for conventional surgical VMMC to 15 years and older due to an increase in specific adverse events reported in 10–14-year-old clients [51–53].
Quality assurance and quality improvement activities commonly practiced by VMMC programs include AE surveillance, AE investigations and contributing root cause analyses, external quality assessments, and continuous quality improvement. However, each national program has its approach to quality and safety, which often changes over time and is frequently determined in reaction to an event. Therefore, the lack of a deliberate approach to program quality can lead to inadequate monitoring, missed epidemiologic signals, insufficient AE investigations and analyses, improper corrective actions, and ultimately, missed opportunities to improve safety for clients and staff.
With any surgical intervention, it is impossible to eliminate all complications. When AEs occur, timely diagnosis and optimal management can minimize long-term sequelae. Although tools and guidance have been developed to standardize and improve the management and prevention of commonly reported AEs, there is considerable variation in how national VMMC programs manage certain severe AEs [48, 54, 55]. Some programs have a well-planned AE management system, including designated specialty care providers or centers of excellence. Still, many lack a standardized approach or local capacity to manage these cases appropriately.
Informed consent/assent is a critical component of preoperative counseling. Counseling on risks and benefits can be transparent and delivered in easy-to-understand language with ample opportunities for clients to ask questions. Clients, especially younger adolescents, have a wide range of maturity and capacity to understand the procedure, potentially impacting their ability to give informed consent/assent. Although the general need for client understanding of risks and benefits prior to surgery is well-accepted, there is a potential need for greater assessment and support of adolescents’ capacity for autonomous decision-making in healthcare settings [56].
Improving VMMC safety is a constant priority for VMMC program planners and implementers. Recommended priority steps for improving the quality and safety of VMMC programs include a responsive, standardized, and comprehensive approach to AE surveillance. Through continuous quality improvement, surveillance data for action gives purpose to surveillance by translating safety events to improved outcomes for future clients and overall improved program safety. Continued monitoring of quality and safety activities can remain a critical component of VMMC programs. Standardized summaries of risks and benefits could be developed for VMMC programs to translate and use for eligible clients to improve informed consenting practices. In addition, global guidance is needed on how VMMC counselors can assess the ability of younger clients and their parents or guardians to comprehend and provide consent or assent for VMMC.
Robust networks and coordination across programs are needed to improve the safety and quality of VMMC programs. Establishing a network of shared safety experiences within and across national VMMC programs could amplify best practices and provide a mechanism to share AE management experiences. Additionally, improved coordination within and among countries to optimize the management of serious, complex AEs is needed. Additional research on the categorization of attributes of clients at higher risk for AEs or who missed follow-up appointments could help to identify higher risk clients to prevent adverse outcomes. Additionally, male circumcision devices warrant monitoring to inform programming decisions around safety and sustainability. Finally, another important gap is that the program has primarily concentrated on the quality of the procedure but has not focused as rigorously on the quality of other areas such as HIV testing services, medical record keeping, demand creation, and client education. Additional attention and resources may be needed to ensure all aspects of quality for the VMMC program are rigorously monitored.
Sustainability
Following the first 15 years of program expansion, the sustainability of national VMMC programs is becoming increasingly important. Although sustainability was initially conceived as a distinct phase of program transition, sustainability of VMMC will require a more gradual evolution including measured integration of VMMC services into national health systems. The sustainability of VMMC is particularly important with economic modeling predicting the program will continue to be a cost-effective prevention strategy and, in fact, cost-saving in most countries over a 50-year horizon [57]. In 2020, as part of the updated recommendations for VMMC, WHO published a framework for sustaining VMMC services [17••]. The framework builds upon the WHO’s health system “building blocks” and integrates VMMC-specific information [58]. The sustainability of VMMC is defined in the following ways: (1) the capacity of VMMC services to maintain high male circumcision coverage (≥ 90%); (2) the integration of VMMC services into a country’s health system; (3) strong country ownership and leadership; and (4) resource mobilization may include domestic and external funding. VMMC sustainability is a new area for national programs, and programmatic and research gaps remain, and each strategic planning component for sustainable VMMC services remains relatively unknown. One area which poses a challenge is long-term workforce needs. Although the capacity building of the health workforce, particularly nurses, to perform the surgical procedure has been a major success of VMMC implementers and donors, the long-term resource and policy could sustain this workforce capacity remain unknown.
Priority steps could be taken to progress successfully to fully sustainable VMMC programs. The VMMCs programs have relied largely on donor support, and the need for diversified financing streams is evident, as donor-funded programs alone are not sustainable. Engaging ministries of health and finance will be critical as national health priorities are financed. However, careful evolution of financial responsibility is essential, with most countries lacking the resources to fully support HIV prevention services. Priority components for VMMC sustainability for each of the building blocks are outlined in the WHO framework summarized in Table 2. Key steps for the first building block of finance include estimating country resource needs and inclusion into national health plans. Inclusion of VMMC programs into national health plans could include integration with other health services such as national sexual and reproduction health programs for adolescents and males. For health workforce planning, the establishment of systems to monitor staff retention and integration of the VMMC workforce into national workforce planning can be considered. Recommended initial steps towards workforce sustainability include the incorporation of VMMC into pre-service health care worker training programs [59]. Recommended steps for the strategic information building block include integrating data collection into routine monitoring and evaluation systems and modernizing data collection.
Table 2.
WHO health systems six building blocks and components framework for suitable VMMC services
| Building block | Component |
|---|---|
| Finance |
• Resource allocation and mobilization • Purchasing of services • Financial risk protection |
| Health workforce |
• Health workforce planning • Pre-service and continuing education • Management, supply, and supervision |
| Strategic information |
• Data collection and management • Data quality • Data analysis and use • Safety monitoring |
| Supplies and equipment |
• Norms and standards • Procurement, supply, and distribution • Quality of VMMC supplies and equipment |
| Leadership and governance |
• Program leadership and coordination • Accountability, oversight, and regulation • Inter-sectoral coordination • Health sector plans and policies |
| Service delivery |
• Access (strategic planning of health services) • Reorienting service delivery models • Empowering and engaging people • Safety and quality |
Note: Adapted from WHO Preventing HIV Through Safe Voluntary Medical Male Circumcision for Adolescent Boys and Men in Generalized HIV Epidemics. 2020. Available at: https://www.who.int/publications/i/item/978-92-4-000854-0
For the supplies and equipment building block, integration of procurement and distribution of supplies into national procurement systems are recommended. This area may be easier to transition, with several ministries of health already procuring supplies for other health services. Although the scale-up phase of the program primarily relied on single-use instruments, more recent guidance has prioritized reusable instruments, not only for the sustainability of services but also to reduce costs and environmental impact. Considerations for the leadership and governance building block focus on integration with local governance. Leadership and governance for VMMC have been country-led since the program’s inception and maintaining this momentum will be critical for the program’s sustainability. Lastly, key actions for the service delivery building block focus on strategic planning of health services and promotion of VMMC as part of a comprehensive package of care.
Measuring a country’s progress towards sustainability is critical for countries to understand and assess their transition. A 2022 landscape analysis conducted by WHO and UNAIDS applied the above-referenced framework and summarized the status of each country’s VMMC program in relation to the sustainability of services. The overwhelming majority of the WHO building block designations were either at an early or intermediate phase with minimal or only a few sustainable features present. A full report on the analysis is expected to be published in mid-2022.
Many countries have taken steps towards sustainability. Actions range from developing national plans for sustainability to piloting the transition of service delivery from donor-funded community organizations to government services [60, 61]. For example, several countries have tried to incorporate early infant male circumcision (EIMC) as part of their sustainability plan, but no national EIMC programs are currently active. In 2019, PEPFAR support for all EIMC activities was ceased after a careful review of impact and safety data. In 2020, WHO further cautioned countries to carefully consider the risks and benefits, human rights, and resources to safely deliver EIMC services for HIV prevention [17••].
Conclusions
The issues presented in this report contribute to policy and research agenda-setting and action at the global and national levels. Continuing the progress VMMC programs have made during the first 15 years of the program is important to reduce HIV incidence and achieve the UNAIDS 2025 AIDS Targets for 90% of males 15 years and older to have access to VMMC in prioritized countries [62–64]. However, important VMMC programmatic challenges remain requiring budgetary commitments, leadership, and commitment across governments and global partners. Programs have demonstrated their ability to grow and adapt and will continue to do so as they work towards addressing programmatic and research gaps.
Declarations
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the funding agency.
Footnotes
This article is part of the Topical Collection on Voluntary Medical Male Circumcision: Progress and Challenges
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
PEPFAR Attribution
This publication has been supported by the President’s Emergency Plan for AIDS Relief (PEPFAR) through the Centers for Disease Control and Prevention (CDC).
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.World Health Organization, Joint United Nations Programme on HIV/AIDS. WHO/UNAIDS Technical Consultation on Male Circumcision and HIV Prevention: Research Implications for Policy and Programming. 2007. http://www.unaids.org/sites/default/files/media_asset/mc_recommendations_en_1.pdf. Accessed 15 February 2022.
- 2.Reed JB, Njeuhmeli E, Thomas AG, Bacon MC, Bailey R, Cherutich P, et al. Voluntary medical male circumcision: an HIV prevention priority for PEPFAR. JAIDS. 2012;60:S88. doi: 10.1097/QAI.0b013e31825cac4e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Davis SM, Hines JZ, Habel M, Grund JM, Ridzon R, Baack B, et al. Progress in voluntary medical male circumcision for HIV prevention supported by the US President’s Emergency Plan for AIDS Relief through 2017: longitudinal and recent cross-sectional programme data. BMJ Open. 2018;8:e021835. doi: 10.1136/bmjopen-2018-021835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bailey RC, Moses S, Parker CB, Agot K, Maclean I, Krieger JN, et al. Male circumcision for HIV prevention in young men in Kisumu, Kenya: a randomised controlled trial. Lancet. 2007;369:643–656. doi: 10.1016/S0140-6736(07)60312-2. [DOI] [PubMed] [Google Scholar]
- 5.Gray RH, Kigozi G, Serwadda D, Makumbi F, Watya S, Nalugoda F, et al. Male circumcision for HIV prevention in men in Rakai, Uganda: a randomised trial. Lancet. 2007;369:657–666. doi: 10.1016/S0140-6736(07)60313-4. [DOI] [PubMed] [Google Scholar]
- 6.Auvert B, Taljaard D, Lagarde E, Sobngwi-Tambekou J, Sitta R, Puren A. Randomized, controlled intervention trial of male circumcision for reduction of HIV infection risk: the ANRS 1265 trial. PLoS Med. 2005;2:e298. doi: 10.1371/journal.pmed.0020298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Weiss HA, Quigley MA, Hayes RJ. Male circumcision and risk of HIV infection in sub-Saharan Africa: a systematic review and meta-analysis. AIDS. 2000;14:2361–2370. doi: 10.1097/00002030-200010200-00018. [DOI] [PubMed] [Google Scholar]
- 8.• World Health Organization, Joint United Nations Programme on HIV/AIDS. Voluntary medical male circumcision. Remarkable progress in the scale up of VMMC as an HIV prevention intervention in 15 ESA countries. 2019. https://apps.who.int/iris/bitstream/handle/10665/330010/WHO-CDS-HIV-19.50-eng.pdf?ua=1. Accessed 15 February 2022. This joint WHO and UNAIDS report is important because it describes the most up to date VMMC program performance by country since the start of the program and progress towards UNAIDS global targets.
- 9.World Health Organization. WHO progress brief on voluntary medical male circumcision for HIV prevention in 14 priority countries in eastern and southern Africa, July 2018. 2018. https://www.malecircumcision.org/resource/who-progress-brief-voluntary-medical-male-circumcision-hiv-prevention-july-2018. Accessed 15 February 2022.
- 10.World Health Organization, Joint United Nations Programme on HIV/AIDS (WHO/UNAIDS). New data on male circumcision and HIV prevention: policy and program implications. 2007. Available at: http://libdoc.who.int/publications/2007/9789241595988_eng.pdf. Accessed 15 February 2022.
- 11.World Health Organization, Joint United Nations Programme on HIV/AIDS. WHO/UNAIDS joint strategic action framework to accelerate the scale-up of voluntary medical male circumcision for HIV prevention in Eastern and Southern Africa, 2012–2016. WHO/UNAIDS; 2011. JC251_circumcision.indd (unaids.org). Accessed 19 March 2022.
- 12.World Health Organization. WHO Progress Brief. VMMC for HIV prevention in 14 priority countries in East and Southern Africa. WHO; 2015. http://apps.who.int/iris/bitstream/handle/10665/179933/WHO_HIV_2015.21_eng.pdf;jsessionid=B63988A95850E2093462CEA6A237AB2B?sequence=1. Accessed 20 February 2022.
- 13.World Health Organization. WHO progress brief. VMMC for HIV Prevention. WHO; 2018. https://www.afro.who.int/sites/default/files/2018-10/29%20Oct_18145_Progress%20Brief_VMMC%202018.pdf?ua=1. Accessed 15 February 2022.
- 14.Joint United Nations Programme on HIV/AIDS. AIDS at 30: nations at a crossroads. UNAIDS; 2011. https://www.unaids.org/en/resources/documents/2011/20110531_JC2095E_aids_at_30. Accessed 15 February 2022.
- 15.Joint United Nations Programme on HIV/AIDS. Voluntary medical male circumcision. UNAIDS; 2021. https://www.unaids.org/sites/default/files/media_asset/JC3022_VMMC_en.pdf. Accessed 15 February 2022.
- 16.•• U.S. President’s emergency plan for aids relief. PEPFAR 2020 Country Operational Guidance for all PEPFAR Countries. PEFPAR; 2020. https://www.state.gov/wp-content/uploads/2020/01/COP20-Guidance.pdf. Accessed 15 February 2022. This PEPFAR guidance document is important because it presents an update in age eligibility for PEPFAR-supported VMMC programs to only support VMMC in clients 15 years and older with the exception of ShangRing©.
- 17.•• World Health Organization. Preventing HIV through safe voluntary medical male circumcision for adolescent boys and men in generalized HIV epidemics. Recommendations and key considerations. WHO; 2020. https://www.who.int/publications/i/item/978-92-4-000854-0. Accessed 15 February 2022. This WHO guidance is important because it provides an update framework for VMMC program with a focus on sustainability. [PubMed]
- 18.Hankins C, Warren M, Njeuhmeli E. Correction: Voluntary medical male circumcision for HIV prevention: new mathematical models for strategic demand creation prioritizing subpopulations by age and geography. PLoS ONE. 2016;11:e0169499. doi: 10.1371/journal.pone.0169499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kripke K, Reed J, Hankins C, Smiley G, Laube C, Njeuhmeli E. Impact and cost of scaling up voluntary medical male circumcision for HIV prevention in the context of the new 90–90-90 HIV treatment targets. PLoS ONE. 2016;11:e0155734. doi: 10.1371/journal.pone.0155734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Joint United Nations Programme on HIV/AIDS. Voluntary medical male circumcision. Progress Brief. 2021. UNAIDS; 2021. Available at: https://hivpreventioncoalition.unaids.org/wp-content/uploads/2021/04/JC3022_VMMC_4-pager_En_v3.pdf. Accessed 15 February 2022.
- 21.Maffioli EM. Is traditional male circumcision effective as an HIV prevention strategy? Evidence from Lesotho. PloS one. 2017;12(5):e0177076. doi: 10.1371/journal.pone.0177076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kigozi G, Wawer M, Ssettuba A, et al. Foreskin surface area and HIV acquisition in Rakai, Uganda (size matters) AIDS. 2009;23:2209–2213. doi: 10.1097/QAD.0b013e328330eda8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McGillen JB, Stover J, Klein DJ, Xaba S, Ncube G, Mhangara M, et al. The emerging health impact of voluntary medical male circumcision in Zimbabwe: An evaluation using three epidemiological models. PLoS ONE. 2018;13(7):e0199453. doi: 10.1371/journal.pone.0199453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Davis SM, Habel MA, Pretorius C, Yu T, Toledo C, Farley T, et al. Brief report: Modeling the impact of voluntary medical male circumcision on cervical cancer in Uganda. JAIDS. 2021;86(3):323–328. doi: 10.1097/QAI.0000000000002552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.• Hall MT, Smith MA, Simms KT, Barnabas RV, Canfell K, Murray JM. The past, present and future impact of HIV prevention and control on HPV and cervical disease in Tanzania: A modelling study. PLoS ONE. 2020:15(5):e0231388. 10.1371/journal.pone.0231388. This study is important because it describes the potential impact of VMMC in Tanzania on cervical cancer and predicts that by 2070, VMMC will have lowered cervical cancer incidence and mortality rates by 28% and 26%. [DOI] [PMC free article] [PubMed]
- 26.Cork MA, Wilson KF, Perkins S, Collison ML, Deshpande A, Eaton JW, et al. Mapping male circumcision for HIV prevention efforts in sub-Saharan Africa. BMC Med. 2020;18:189. doi: 10.1186/s12916-020-01635-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stegman P, Stirling B, Corner B, Schnure M, Mali D, Shihepo E, et al. Voluntary medical male circumcision to prevent HIV: modelling age prioritization in Namibia. AIDS Behav. 2019;23(2):195–205. doi: 10.1007/s10461-019-02556-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kripke K, Opuni M, Odoyo-June E, Onyango M, Young P, Serrem K, et al. Data triangulation to estimate age-specific coverage of voluntary medical male circumcision for HIV prevention in four Kenyan counties. PLoS ONE. 2018;13(12):e0209385. doi: 10.1371/journal.pone.0209385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hewett PC, Haberland N, Apicella L, Mensch BS. The (mis)reporting of male circumcision status among men and women in Zambia and Swaziland: a randomized evaluation of interview methods. PLoS ONE. 2012;7(5):e36251. doi: 10.1371/journal.pone.0036251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Odoyo-June E, Agot K, Mboya E, Grund J, Musingila P, Emusu D, et al. Agreement between self-reported and physically verified male circumcision status in Nyanza region, Kenya: evidence from the TASCO study. PLoS ONE. 2018;13(2):e0192823. doi: 10.1371/journal.pone.0192823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Joint United Nations Programme on HIV/AIDS reference group on estimates, modeling and projections. UNAIDS; 2021. https://www.epidem.org/. Accessed 15 February 2022.
- 32.Stover J, Brown T, Marston M. Updates to the Spectrum/Estimation and Projection Package (EPP) model to estimate HIV trends for adults and children. Sex Transm Infect. 2012;88(2):11–16. doi: 10.1136/sextrans-2012-050640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Atkins K, Yeh PT, Kennedy CE, Fonner VA, Sweat MD, O’Reilly KR, et al. Service delivery interventions to increase uptake of voluntary medical male circumcision for HIV prevention: a systematic review. PLoS ONE. 2020;15:e0227755. doi: 10.1371/journal.pone.0227755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Thirumurthy H, Masters SH, Rao S, Bronson MA, Lanham M, Omanga E, et al. Effect of providing conditional economic compensation on uptake of voluntary medical male circumcision in Kenya: a randomized clinical trial. JAMA. 2014;312(7):703–711. doi: 10.1001/jama.2014.9087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kripke K, Opuni M, Schnure M, Sgaier S, Castor D, Reed J, et al. Age targeting of voluntary medical male circumcision programs using the decision makers’ program planning toolkit (DMPPT) 2.0. PLoS One. 2016;11(7):e0156909. doi: 10.1371/journal.pone.0156909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Carrasco MA, Wilkinson J, Kasdan B, Fleming P. Systematic review of barriers and facilitators to voluntary medical male circumcision in priority countries and programmatic implications for service uptake. Glob Public Health. 2019;14(1):91–111. doi: 10.1080/17441692.2018.1465108. [DOI] [PubMed] [Google Scholar]
- 37.• World Health Organization. Web Annex 5.2. Case studies on enhancing uptake of voluntary medical male circumcision services. WHO; 2020. https://apps.who.int/iris/bitstream/handle/10665/333826/9789240009332-eng.pdf. Accessed 15 February 2022. This report is important because it presents case studies describing interventions that have successfully increased uptake of VMMC. Successful approaches included programs that tried multiple interventions to reach their target audience and strategies that addressed key barriers.
- 38.Carrasco MA, Nguyen TQ, Kaufman MR. Low uptake of voluntary medical male circumcision among high risk men in Malawi. AIDS Behav. 2018;22:447–453. doi: 10.1007/s10461-016-1633-1. [DOI] [PubMed] [Google Scholar]
- 39.Baisley K, Chimbindi N, Mthiyane N, Floyd S, McGrath N, Pillay D, et al. High HIV incidence and low uptake of HIV prevention services: the context of risk for young male adults prior to DREAMS in rural KwaZulu-Natal, South Africa. PLoS ONE. 2018;13(12):e0208689. doi: 10.1371/journal.pone.0208689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hatzold K, Mavhu W, Jasi P, Chatora K, Cowan FM, Taruberekera N, et al. Barriers and motivators to voluntary medical male circumcision uptake among different age groups of men in Zimbabwe: results from a mixed methods study. PLoS ONE. 2014;9(5):e85051. doi: 10.1371/journal.pone.0085051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sgaier SK, Baer J, Rutz DC, Njeuhmeli E, Seifert-Ahanda K, Basinga P, et al. Toward a systematic approach to generating demand for voluntary medical male circumcision: insights and results from field studies. Glob Health Sci Pract. 2015;3(2):209–229. doi: 10.9745/GHSP-D-15-00020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gomez A, Loar R, Kramer AE, Garnett GP. Reaching and targeting more effectively: the application of market segmentation to improve HIV prevention programmes. JAIDS. 2019;22(4):e25318. doi: 10.1002/jia2.25318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sgaier SK, Baer J, Rutz DC, Njeuhmeli E, Seifert-Ahanda K, Basinga P, et al. Toward a systematic approach to generating demand for voluntary medical male circumcision: insights and results from field studies. Glob Health Sci Pract. 2015;3(2):209–229. doi: 10.9745/GHSP-D-15-00020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sgaier SK, Eletskaya M, Engl E, Mugurungi O, Tambatamba B, Ncube G, et al. A case study for a psychographic-behavioral segmentation approach for targeted demand generation in voluntary medical male circumcision. Elife 2017:6. [DOI] [PMC free article] [PubMed]
- 45.Redding CA, Jones D, Zulu R, Chitalu N, Cook R, Weiss SM. Stages of change for voluntary medical male circumcision and sexual risk behavior in uncircumcised Zambian men: the spear and shield project. Int J Behav Med. 2015;22(6):799–806. doi: 10.1007/s12529-015-9485-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Nxumalo CT, Mchunu GG. Circumcised men’s perceptions, understanding and experiences of voluntary medical male circumcision in KwaZulu-Natal, South Africa. S Afr Fam Pract. 2020;62(1):1–8. doi: 10.4102/safp.v62i1.5083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Torres-Rueda S, Wambura M, Weiss H, Plotkin M, Kripke K, Chilongani J, et al. Cost and cost-effectiveness of a demand creation intervention to increase uptake of voluntary medical male circumcision in Tanzania: spending more to spend less. JAIDS. 2018;78:291–299. doi: 10.1097/QAI.0000000000001682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Njeuhmeli E, Hatzold K, Gold E, Mahler H, Kripke K, Seifert-Ahanda K, et al. Lessons learned from scale-up of voluntary medical male circumcision focusing on adolescents. JAIDS. 2014;66:S193–S199. doi: 10.1097/QAI.0000000000000179. [DOI] [PubMed] [Google Scholar]
- 49.World Health Organization. WHO technical advisory group on innovations in male circumcision: evaluation of two adult devices: Meeting report. Geneva. WHO; 2015. https://apps.who.int/iris/bitstream/handle/10665/171780/9789241508803_eng.pdf. Accessed 15 February 2022.
- 50.Lucas T, Cooney C, Prainito A, Godfrey C, Kiggundu V, Thomas A, et al. Consolidated overview of notifiable adverse events in the U.S. President’s emergency plan for AIDS relief’s voluntary medical male circumcision program through 2020. 2022. In press. [DOI] [PMC free article] [PubMed]
- 51.Grund JM, Toledo C, Davis SM, Ridzon R, Moturi E, Scobie H, et al. Notes from the field: Tetanus cases after voluntary medical male circumcision for HIV prevention—Eastern and Southern Africa, 2012–2015. MMWR. 2016;65:36–37. 10.15585/mmwr.mm6502a5. [DOI] [PubMed]
- 52.Population Services International (PSI). Adverse event action guide for voluntary medical male circumcision (VMMC) by surgery or device 2nd edition. PSI; 2020. https://www.malecircumcision.org/sites/default/files/document_library/Adverse-Event-Action-Guide-for-VMMC-2nd-edition-December-2020.pdf. Accessed 15 February 2022.
- 53.Hinkle LE, Toledo C, Grund JM, Byams VR, Bock N, Ridzon R, et al. Bleeding and blood disorders in clients of voluntary medical male circumcision for HIV prevention — Eastern and Southern Africa, 2015–2016. MMWR. 2018;67:337–339. doi: 10.15585/mmwr.mm6711a6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.World Health Organization. Improving surgical male circumcision practice – urethral fistula: diagnosis, first management and prevention. WHO; 2021. https://www.who.int/publications/i/item/9789240019768. Accessed 15 February 2022.
- 55.World Health Organization. Improving surgical male circumcision practice through experience: preventing urethral fistula. WHO; 2019. https://www.who.int/publications/i/item/WHO-CDS-HIV-19.1. Accessed 15 February 2022.
- 56.World Health Organization. Assessing and supporting adolescents’ capacity for autonomous decision-making in health-care settings. WHO; 2021.9 789240039568-eng.pdf (who.int). Accessed 15 February 2022. [DOI] [PMC free article] [PubMed]
- 57.Bansi-Matharu A, Mudimu E, Martin-Huges R, Hamilton M, Johnson L, ten-Brink M, et al. Cost-effectiveness of voluntary male medical circumcision (VMMC) for HIV prevention across sub-Saharan Africa: results from five independent models. 2022. In press. [DOI] [PMC free article] [PubMed]
- 58.World Health Organization. Everybody’s business - strengthening health systems to improve health outcomes: WHO's framework for action. WHO; 2007. http://www.who.int/healthsystems/strategy/everybodys_business.pdf. Accessed 15 February 2022.
- 59.Davis SM, Baker H, Gross JM, Leslie SL, Chasokela CMZ, Samuelson J, et al. The role of nurses and midwives in expanding and sustaining voluntary medical male circumcision services for HIV prevention: a systematic and policy review. JANAC. 2021;32(1):3–28. doi: 10.1097/JNC.0000000000000222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.The Zimbabwe Smart-LynAges Project. Preventing HIV through safe voluntary medical male circumcision for adolescent boys and men in generalized HIV epidemics: recommendations and key considerations. Geneva: World Health Organization; 2020. WEB ANNEX 6.1, Sustaining Voluntary Medical Male Circumcision Services and Linkages with Adolescent Sexual and Reproductive Health: The Zimbabwe Smart-Lyncages Project. 2020. Available at: https://www.ncbi.nlm.nih.gov/books/NBK562469/. Accessed 15 February 2022.
- 61.Davis SM, Owuor N, Odoyo-June E, Wambua J, Omanga E, Lukobo M, et al. Making voluntary medical male circumcision services sustainable: findings from Kenya’s pilot models, baseline and year 1. PLoS ONE. 2021;16(6):e0252725. doi: 10.1371/journal.pone.0252725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Joint United Nations Programme on HIV/AIDS (UNAIDS). Prevailing against pandemics by putting people at the centre. World AIDS Day Report. 2020. 2025 AIDS TARGETS - UNAIDS.
- 63.Blaizot S, Maman D, Riche B, Mukui I, Kirubi B, Ecochard R, et al. Potential impact of multiple interventions on HIV incidence in a hyperendemic region in Western Kenya: a modelling study. BMC Infect Dis. 2016;16:189. doi: 10.1186/s12879-016-1520-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Loevinsohn G, Kigozi G, Kagaayi J, Wawer MJ, Nalugoda F, Chang LW, et al. Effectiveness of voluntary medical male circumcision for human immunodeficiency virus prevention in Rakai, Uganda. Clin Infect Dis. 2021;73(7):e1946–e1953. doi: 10.1093/cid/ciaa1533. [DOI] [PMC free article] [PubMed] [Google Scholar]