Abstract
Toxoplasma gondii tachyzoites were transformed with the coding sequence of the circumsporozoite (CS) protein of the primate malaria parasite Plasmodium knowlesi. A single inoculation of live transformed tachyzoites elicited an antibody response directed against the immunodominant repeat epitope (EQPAAGAGG)2 of the P. knowlesi CS protein in rhesus monkeys. Notably, these animals failed to show a positive serum conversion against T. gondii. Antibodies against Toxoplasma antigens were detected only after a second inoculation with a higher number of transformed tachyzoites. This boost induced an increased antibody response against the P. knowlesi CS protein associated with immunoglobulin class switching, thus demonstrating the establishment of immunological memory. These results indicate that the Toxoplasma-derived CS protein is efficiently recognized by the monkey immune system and represents an immunodominant antigen in transformed parasites.
The circumsporozoite (CS) protein uniformly covers the entire surface of the malaria sporozoite in a dense layer (27). Immunity to the CS protein blocks sporozoite invasion of hepatocytes in vitro (21) and exerts a potent antiparasitic effect in rodent malaria models (25, 27, 29). Recently, a recombinant form of Plasmodium falciparum CS protein fused to the hepatitis B surface antigen was reported to induce protective immunity against a sporozoite challenge in the great majority of immunized human volunteers (33). This experiment has shown the feasibility of developing a malaria sporozoite vaccine in humans by using the CS protein formulated together with potent adjuvants. Previous efforts aimed at inducing protection in humans by using different CS protein-based vaccines have failed or resulted in incomplete protection (4, 6, 26, 30). Plasmid DNA (3, 15, 18, 20) and attenuated recombinant poxvirus vectors (2, 23, 35) are also being employed in the effort to generate effective malaria vaccines. The availability of gene transfer technology for the protozoan parasite Toxoplasma gondii may offer an additional opportunity to express and deliver the CS protein in a highly immunogenic form.
T. gondii shares with Plasmodium species the host cell invasion machinery and subcellular organelles. The phylogenetic relationship among these parasites (24) suggests that malaria antigens expressed in Toxoplasma would most likely assume their natural conformation. Transgenic T. gondii tachyzoites also have the potential to induce a long-lasting immunity against malaria antigens. In normal individuals with an intact immune system, T. gondii causes a mild and self-limited flu-like disease that stimulates a potent humoral and cell-mediated immune response (13, 14). Such an immune response efficiently protects exposed individuals from subsequent T. gondii infections for the rest of their lives, although the parasite may persist in the form of tissue cysts. The pathogenicity of Toxoplasma for immunocompromised individuals and nonimmune fetuses (16) currently limits the use of the wild-type parasite as an antigen delivery system. The development of nonvirulent T. gondii strains that have lost the ability to form tissue cysts under normal conditions may ultimately circumvent this problem (8, 9, 11).
To investigate the ability of T. gondii to function as an antigen delivery system for Plasmodium antigens, we have generated tachyzoites expressing the CS protein of the primate malaria parasite Plasmodium knowlesi. We report here on the ability of these transgenic parasites to elicit a specific immune response against the P. knowlesi CS protein in rhesus monkeys, an experimental host for P. knowlesi and a well-defined model for human immune responses.
MATERIALS AND METHODS
Parasite cultures.
T. gondii was propagated by serial passages over a monolayer of human foreskin fibroblasts in Dulbecco’s modified Eagle medium (Gibco) containing 10% NuSerum (Collaborative Biomedical Products). The clonal parasite isolate RH (34), which lacks the ability to form tissue cysts, was used for the genetic manipulation and the immunization procedures.
Transformation vector.
A DNA fragment encompassing the coding sequence of the P. knowlesi CS gene (28) from nucleotide 61 to 1053 was amplified by PCR with P. knowlesi genomic DNA as the template and the primer combination of pk1 (5′-CCG GCC ATG GCT CAC TTC GAA CAT AAT GTA G-3′) and pk2 (5′-CCG GTT AAT TAA TTG AAT AAT GCT AGG AC-3′), containing at their 5′ ends an NcoI and a PacI restriction site, respectively. The amplified P. knowlesi CS sequence was designed to encode the full-length parasite protein with the exception of its signal sequence. The P. knowlesi CS-coding sequence was cloned together with the signal sequence of the T. gondii SAG 1 gene in the plasmid Bluescript between the SAG 1 promoter (32) and a 300-nucleotide untranslated sequence flanking the 3′ end of the SAG 1 gene. The sequence coding for the epitope c-Myc (10) was cloned between the SAG 1 signal sequence and the CS sequence, generating the transformation construct pSPc-myc/PkCS.
Transformation of T. gondii tachyzoites.
Transformation experiments were carried out with the construct pSPc-myc/PkCS together with the vector pT/230, which contains the selectable chloramphenicol acetyltransferase marker (22, 31). In brief, 2 × 107 freshly harvested tachyzoites were resuspended in 700 μl of solution (cytomix) containing 100 μg of pSPmyc/CS, 10 μg of pT/230, and 100 U of BamHI (5). The two plasmids were linearized with the restriction enzyme BamHI prior to electroporation (5) and mixed in a 10:1 mass ratio. Electroporated parasites were subjected to chloramphenicol selection as described previously (22). After 7 to 10 days, stable populations of parasites resistant to chloramphenicol emerged, and single clones were isolated by limiting dilution.
Immunoblot analysis.
Protein lysates of extracellular tachyzoites were separated by sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE) and transferred to nitrocellulose filters. Nonspecific absorption of antibodies was prevented by incubating the filters with 1% bovine serum albumin (BSA) in phosphate-buffered saline (PBS) for 2 h at 37°C. The presence of the recombinant CS protein was revealed with monoclonal antibody (MAb) 9E10, directed against the c-Myc epitope (Sigma). Antibody bound to the filter was detected with a goat anti-mouse immunoglobulin conjugated to alkaline phosphatase (Sigma).
To assess the specifity of human immunoglobulin reagents against rhesus monkey antibodies, serum proteins from either macaques, humans, or rats were separated under nonreducing conditions by SDS–8% PAGE or under reducing conditions by SDS–12.5% PAGE and electroblotted onto nitrocellulose filters. Blotted proteins were incubated with either goat anti-human immunoglobulin G heavy plus light chains [IgG(H+L)], goat anti-human IgG (γ-chain specific), or goat anti-human IgM (μ-chain specific) alkaline phosphotase-conjugated immunoglobulins (Sigma). Antibody bound to the filter was detected with a goat anti-mouse immunoglobulin conjugated to alkaline phosphatase (Sigma).
Immunofluorescence.
Extracellular tachyzoites were washed in PBS, air dried on slides, fixed for 10 min in 1% formaldehyde–PBS, and permeabilized in acetone at −20°C for 5 min. The slides were blocked for 30 min in 1% BSA–PBS and then incubated at room temperature with MAb 9E10 for 1 h. Antibodies bound to Toxoplasma cells were revealed with goat anti-mouse fluorescein isothiocyanate-conjugated immunoglobulins (Becton Dickinson). Slides were washed in PBS, mounted with Vectashield (Vector), and analyzed by using a Bio-Rad 600 confocal microscope.
Recombinant bacterial proteins and synthetic peptides.
The recombinant constructs PkCS 1.0 and HRPIIr were amplified by PCR with, as templates, P. knowlesi and P. falciparum genomic DNAs, respectively. PkCS 1.0 encompasses the entire sequence of the P. knowlesi CS with the exception of the signal peptide and the hydrophobic glycosylphosphatidylinositol (GPI) anchor. HRPIIr encompasses the sequence of P. falciparum histidine-rich protein II (HRPII) lacking only its signal peptide. The sequences coding for PkCS 1.0 and HRPIIr were cloned in the vector pDS56/RBSII,6XHis. The expression unit of this vector is under the control of an IPTG (isopropyl-β-d-galactopyranoside)-inducible promoter and yields fusions between a stretch of six histidines and the amino terminus of the inserted sequence (19). The recombinant proteins PkCS 1.0 and HRPIIr containing the histidine tail were purified by nickel chelate chromatography. The synthetic peptide (EQPAAGAGG)2 was purchased from the Imperial College peptide synthesis service. As control, we employed the synthetic peptide Der pI (FGISNYCQIYPPNANKIREALAQPQRYCR), which encompasses an epitope from the house dust mite allergen Der P1.
Selection of animals and immunization.
Sera from 20 rhesus monkeys (Macaca mulatta) were screened by immunoblotting against a T. gondii protein lysate at a 1:50 dilution. Seven of the 20 tested rhesus monkeys showed very strong reactivity with multiple protein bands, suggesting previous exposure to Toxoplasma. Seven animals were completely negative, and the remaining ones reacted only very weakly with one or more protein bands. Ten animals in the same age and weight range were allocated to two groups, with each group consisting of three nonreactive and two weakly reactive (9305 and L167 in group A and L175 and 2BWI in group B) animals. Rhesus monkeys were immunized by intravenous infection with 5 × 106 freshly prepared tachyzoites at day 0. Group A received Tx-PkCS7, and group B received RH strain tachyzoites. Both groups received a booster infection with 30 × 106 Tx-PkCS7 tachyzoites at day 130.
Serum reactivity.
Blood samples (5 ml) were withdrawn from each monkey 2 weeks before the first inoculation and at monthly intervals thereafter. The detection of specific antibodies to recombinant P. knowlesi CS protein was done on 96-well microtiter plates (Falcon 3912) coated with either purified PkCS 1.0 or HRPIIr (1 μg/ml) at 4°C overnight in 2× PBS, pH 7.3. After blocking for 2 h at 37°C with 1% BSA in 2× PBS, the wells were incubated for 1 h at room temperature with different dilutions of the monkey sera in 2× PBS. Antibodies bound to antigens were revealed by using an anti-human goat immunoglobulin antibody conjugated to alkaline phosphatase (Promega). The IgG and IgM antibody fractions were detected by using goat anti-human IgG (Fc specific) and goat anti-human IgM (μ-chain specific) alkaline phosphotase-conjugated immunoglobulins (Sigma), respectively. The competition experiments were performed by preincubating the monkey sera, diluted 1:50 in 2× PBS, for 30 min either with increasing concentrations (0.16, 0.8, 4, and 20 μg/ml) of the P. knowlesi CS synthetic peptide (EQPAAGAGG)2 or with 20 μg of the peptide Der pI per ml. The reactivity of the monkey sera against Toxoplasma was analyzed by using a diagnostic kit (Radim Diagnostics, Rome, Italy) that has been developed to detect human IgG directed against an extract of parasite proteins.
RESULTS AND DISCUSSION
Expression of P. knowlesi CS protein in T. gondii.
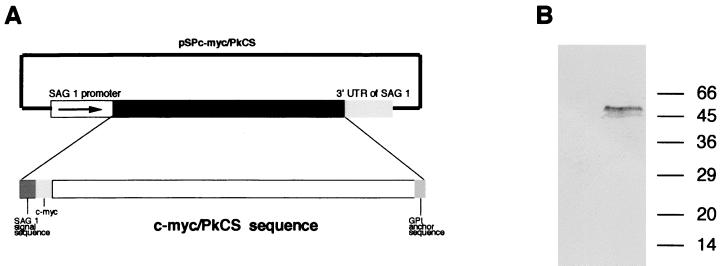
Toxoplasma tachyzoites were transformed with the vector pSPc-myc/PkCS (Fig. 1A), containing (i) the tachyzoite stage-specific promoter of the Toxoplasma major surface antigen SAG 1 (32), (ii) a chimeric P. knowlesi CS protein gene (myc/PkCS), and (iii) a 300-nucleotide untranslated sequence flanking the 3′ end of the SAG 1 gene (7). The myc/PkCS gene encoded a polypeptide encompassing the signal peptide of SAG 1 (7), the c-Myc epitope (10), and the P. knowlesi Nuri strain CS sequence from residue 21 to 351 (28). The malaria protein contained the GPI anchor and lacked its own signal peptide. The promoter and the signal sequence of the SAG 1 gene were inserted in the myc/PkCS expression unit to facilitate correct transcription, translation, and processing of the recombinant malaria protein in Toxoplasma tachyzoites. The c-Myc epitope was inserted between the signal peptide of SAG 1 and the P. knowlesi CS-coding sequence in order to facilitate analysis of expression of the malaria protein.
FIG. 1.
(A) Schematic representation of the construct pSPc-myc/PkCS. (B) Immunoblot analysis of total protein lysates of RH (left lane) and transformed Tx-PkCS7 (right lane) tachyzoites developed by using MAb 9 E10, directed against the c-Myc epitope. The migrations (in kilodaltons) of low-molecular-mass standards from Sigma are indicated on the right.
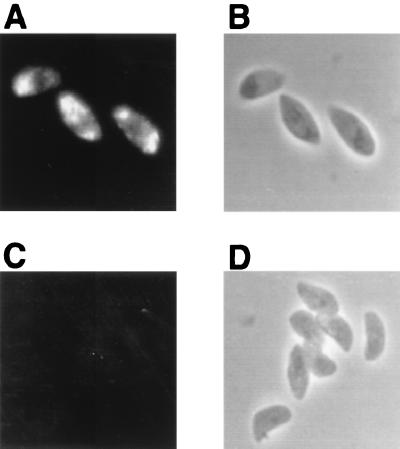
Eight transformed parasite clones were isolated and analyzed in immunoblots with MAb 9E10, directed against the c-Myc epitope (10). One T. gondii clone (Tx-PkCS7) expressed significant amounts of the P. knowlesi CS protein that migrated as two bands with the apparent molecular masses of 44 and 54 kDa (Fig. 1B). This observation is in agreement with a previous report showing that the CS protein from P. knowlesi sporozoites migrated as multiple bands with apparent molecular masses of 42, 50, and 52 kDa (28), with the largest two molecules representing intracellular precursors of the final 42-kDa surface protein. These findings suggest that T. gondii tachyzoites efficiently expressed CS of P. knowlesi. Immunofluorescence of extracellular transformed tachyzoites indicated that the P. knowlesi CS protein was localized in large granules within the cytoplasm of the parasites (Fig. 2). This analysis also revealed the presence of large quantities of P. knowlesi CS protein-reactive material in the parasitophorous vacuoles of intracellular tachyzoites (not shown). The localization of the P. knowlesi CS protein in intra- and extracellular tachyzoites is remarkably similar to the immunofluorescence pattern observed for the Toxoplasma-encoded GRA molecules (1, 12). Accordingly, in transformed tachyzoites the P. knowlesi CS protein may be stored in the dense granules and released after parasite invasion of host cells. On the basis of the structural features of the construct myc/PkCS, we expected a localization of the malaria protein on the surface of the tachyzoites; however, such localization was not observed. Recent reports indicate that a specific signal is not required to target T. gondii protein to the plasma membrane and that the presence of a GPI anchor is sufficient to bring any reporter protein to the plasma membrane. We therefore concluded that the P. knowlesi CS protein GPI anchor sequence may not be efficiently recognized by the tachyzoite-modifying enzymes, resulting in its mistargeting.
FIG. 2.
Immunolocalization of the P. knowlesi CS protein in Tx-PkCS7 tachyzoites. Confocal immunofluorescence (A and C) and transmission (B and D) photomicrographs of Tx-PkCS7 (A and B) and nontransformed (C and D) tachyzoites stained by MAb 9E10 are shown. Magnification, ×630; zoom factor, 2.6 for image acquisition.
Immunogenicity of transformed T. gondii.
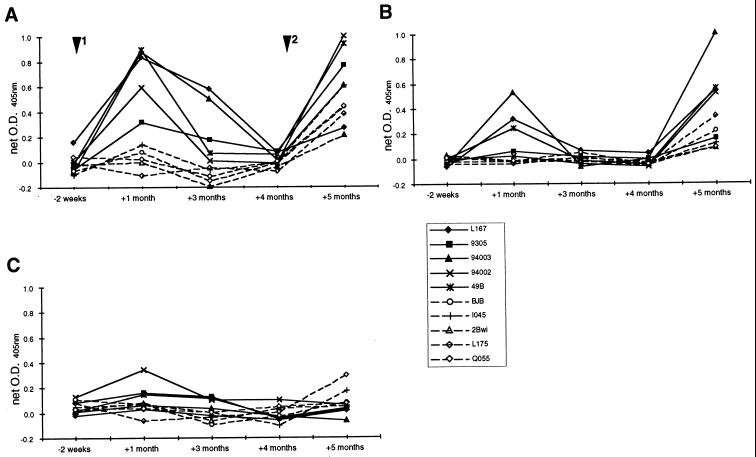
The transformed Toxoplasma clone Tx-PkCS7 was assessed for its ability to induce a specific immune response against the P. knowlesi CS protein in rhesus monkeys (M. mulatta). Two groups of five animals were injected intravenously with 5 × 106 freshly cultured extracellular tachyzoites of either the Tx-PkCS7 clone (group A) or its nontransformed parental strain (group B). Four months after the first inoculation, both groups were injected with 30 × 106 Tx-PkCS7 parasites. Serum samples were collected from each monkey 2 weeks before the first inoculation and thereafter at monthly intervals for 5 months. The antibody responses elicited by the immunization regimens were evaluated by using an enzyme-linked immunosorbent assay (ELISA) developed with the recombinant bacterial construct PkCS 1.0. This construct spans the entire coding sequence of the P. knowlesi CS protein with the exception of the signal peptide and the GPI anchor sequence. As a control, the rhesus monkey sera were also analyzed by ELISA against an unrelated malaria recombinant construct which encompasses the coding sequence of HRPII of P. falciparum. The specific reactivity of each serum against the construct PkCS 1.0 was expressed as net optical density (OD) (ODPkCS 1.0 − ODHRPIIr). One month after the first inoculation, we detected in sera from the monkeys inoculated with live Tx-PkCS7 tachyzoites significant amounts of antibodies directed against the P. knowlesi CS protein (Fig. 3A). At this time point, three of five monkeys (L167, 49b, and 94003) showed a predominant IgG response, whereas high IgM levels were detected in the two remaining animals (94002 and 9305) (Fig. 3A and B). The specific antibody levels in group A monkeys steadily decreased in the following 3 months while still remaining significantly higher (P < 0.02) than those in group B. After boosting with Tx-PkCS7 tachyzoites, all monkeys of group A showed elevated levels of antibodies (exclusively IgG) directed against the P. knowlesi CS protein. Monkeys from group B, which were initially inoculated with the parental nontransformed RH tachyzoites, failed to show any specific reactivity against the malaria antigen during the 4 months following primary immunization (Fig. 3). In this group of animals a subsequent inoculation with Tx-PkCS7 tachyzoites was able to induce specific antibodies directed against the P. knowlesi CS protein, thus indicating that the previous exposure to T. gondii parasites did not impair the ability of the monkeys to respond to the transgenic malaria antigen. The dynamics of the IgM and IgG isotype responses after the first and second inoculations strongly indicated that the Tx-PkCS7 tachyzoites induced immunological memory against the malaria antigen associated with immunoglobulin class switch.
FIG. 3.
Development of humoral immunity against the P. knowlesi CS protein. Monkeys in groups A (solid lines) and B (dashed lines) were inoculated (day 0, arrowhead 1) either with Tx-PkCS7 tachyzoites or with the nontransformed parental RH line, respectively. Both groups of monkeys were inoculated 4 months later (day 130, arrowhead 2) with Tx-PkCS7 tachyzoites. Specific antibodies against the P. knowlesi CS protein were revealed by comparing the reactivities of each monkey serum against the recombinant constructs PkCS 1.0 and HRPIIr. The net OD at 405 nm was calculated by subtracting the OD values in the HRPIIr ELISA from those in the P. knowlesi CS ELISA. The assays were carried out by using labelled secondary antibodies recognizing IgG(H+L) (A), IgG (B), or IgM (C) human isotypes. Each serum was tested in four replicates at a 1/200 dilution. Letter-and-number codes refer to individual monkeys. The standard error for each determination was less than 10%.
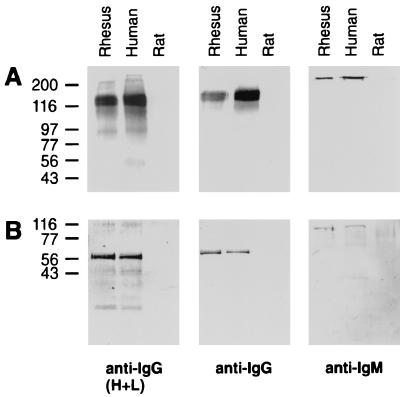
The kinetics of the antibody response in rhesus monkeys was analyzed by using secondary antibodies directed against human immunoglobulins. The specificities of these reagents were investigated by immunoblotting against human, rhesus monkey, and rat serum proteins (Fig. 4). This analysis revealed that the antibodies directed against IgG(H+L) recognize heavy and light chains of both human and monkey immunoglobulins. The IgG and IgM secondary antibodies were shown to selectively recognize, in both human and monkey sera, bands which migrate with the molecular sizes of IgG and IgM, respectively (Fig. 4). These findings rule out the possibility that the use of these reagents has introduced a bias in the analysis of the monkey immune response.
FIG. 4.
Specificity analysis of anti-human immunoglobulin antibodies against human, rhesus monkey, and rat serum proteins under nonreducing (A) and reducing (B) conditions by immunoblotting with anti-IgG(H+L), anti-IgG, or anti-IgM secondary antibodies. The migrations (in kilodaltons) of high-molecular-mass standards from Sigma are indicated on the left.
Previous experiments have shown that the immunodominant region of the P. knowlesi CS protein is contained within the tandem repeat peptide (17), although additional conformational epitopes have also been described (36). To investigate the specificity of the antibody response induced by Tx-PkCS7 tachyzoites, we have assessed the reactivities of the monkey sera against the P. knowlesi CS protein in the presence of an excess of the synthetic peptide (EQPAAGAGG)2, encompassing the repeat epitope (Fig. 5). Our results indicated that a relevant fraction of the P. knowlesi CS antibodies elicited by Tx-PkCS7 were directed against this repeat epitope. In all sera analyzed, the peptide (EQPAAGAGG)2 significantly inhibited, in a dose-dependent manner, antibody binding to the PkCS 1.0 recombinant protein (Fig. 5). However, the serum reactivity was never completely abolished, even in the presence of the highest concentration (20 μg/ml) of peptide, indicating that additional epitopes are also recognized by the immunized monkeys. The unrelated peptide Der pI did not show a significant inhibitory effect (P < 0.001) when compared to the highest concentration of the peptide (EQPAAGAGG)2.
FIG. 5.
Fine specificity of serum reactivity against the P. knowlesi CS protein. Monkey sera collected at 5 months were assessed by ELISA (1/50 dilution) against the recombinant construct PkCS 1.0 in the presence of increasing concentrations of the synthetic peptide (EQPAAGAGG)2 (□). The unrelated peptide Der pI (■) was employed as a specifity control and used at a concentration of 20 μg/ml. The results are the averages of four determinations normalized to control binding in the absence of synthetic peptide.
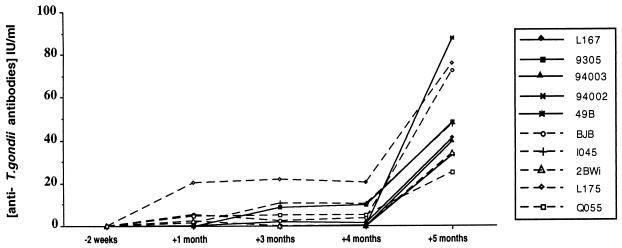
We have also analyzed the monkey sera by using a commercially available ELISA kit that detects human IgG against Toxoplasma antigens. Notably, after the first inoculation, all five monkeys injected with Tx-PkCS7 and four of five animals that received nontransformed parasites failed to react against Toxoplasma antigens in the ELISA kit (Fig. 6). Antibodies directed against Toxoplasma antigens were detected only after injection of a much higher number of tachyzoites, thus ruling out the possibility that the lack of reactivity was due to limitations in the ELISA kit employed. This pattern of reactivity was also confirmed by immunoblot analysis of the rhesus monkey sera against Toxoplasma protein lysates (not shown). It is most likely that the first inoculation of tachyzoites did not result in a sustained and autonomous infection of T. gondii in the monkeys and stimulated a weak immune response against Toxoplasma antigens. This conclusion was supported by the observation that none of the blood samples collected from the monkeys at days 3, 6, and 10 induced toxoplasmosis in susceptible BALB/c mice.
FIG. 6.
Development of humoral immunity against Toxoplasma antigens in immunized rhesus monkeys. Solid and dashed lines indicate group A and B monkeys, respectively. Serum reactivity was analyzed by using a Toxoplasma ELISA kit developed for the diagnosis of human toxoplasmosis. Toxoplasma antibody levels represent the means of duplicate determinations at a 1/200 dilution.
For group A monkeys, the comparison of the antibody responses against the P. knowlesi CS protein and T. gondii antigens is striking. The inoculation of Tx-PkCS7 tachyzoites elicited a significant humoral response to the P. knowlesi CS protein; however, all monkey sera had T. gondii antibody levels lower than the World Health Organization standard positive level for humans of 15 IU per ml (37). This finding strongly indicated that the malaria protein is efficiently recognized by the monkey immune system and represents the major immunodominant antigen in transformed T. gondii parasites. Toxoplasma-derived Plasmodium antigen preparations and/or attenuated live T. gondii-transformed parasite strains may represent invaluable sources of highly immunogenic malaria antigens.
ACKNOWLEDGMENTS
Manlio Di Cristina and Firman Ghouze contributed equally to this work.
This work was supported by a grant from the INCO Programme of the European Commission.
REFERENCES
- 1.Achbarou A, Mercereau Puijalon O, Sadak A, Fortier B, Leriche M A, Camus D, Dubremetz J F. Differential targeting of dense granule proteins in the parasitophorous vacuole of Toxoplasma gondii. Parasitology. 1991;3:321–329. doi: 10.1017/s0031182000059837. [DOI] [PubMed] [Google Scholar]
- 2.Aidoo M, Lalvani A, Whittle H C, Hill A V, Robson K J. Recombinant vaccinia viruses for the characterization of Plasmodium falciparum-specific cytotoxic T lymphocytes: recognition of processed antigen despite limited re-stimulation efficacy. Int Immunol. 1997;9:731–737. doi: 10.1093/intimm/9.5.731. [DOI] [PubMed] [Google Scholar]
- 3.Allsopp C E, Plebanski M, Gilbert S, Sinden R E, Harris S, Frankel G, Dougan G, Hioe C, Nixon D, Paoletti E, Layton G, Hill A V. Comparison of numerous delivery systems for the induction of cytotoxic T lymphocytes by immunization. Eur J Immunol. 1996;26:1951–1959. doi: 10.1002/eji.1830260841. [DOI] [PubMed] [Google Scholar]
- 4.Ballou W R, Hoffman S L, Sherwood J A, Hollingdale M R, Neva F A, Hockmeyer W T, Gordon D M, Schneider I, Wirtz R A, Young J F, et al. Safety and efficacy of a recombinant DNA Plasmodium falciparum sporozoite vaccine. Lancet. 1987;1:1277–1281. doi: 10.1016/s0140-6736(87)90540-x. [DOI] [PubMed] [Google Scholar]
- 5.Black M, Seeber F, Soldati D, Kim K, Boothroyd J C. Restriction enzyme-mediated integration elevates transformation frequency and enables co-transfection of Toxoplasma gondii. Mol Biochem Parasitol. 1995;74:55–63. doi: 10.1016/0166-6851(95)02483-2. [DOI] [PubMed] [Google Scholar]
- 6.Brown A E, Singharaj P, Webster H K, Pipithkul J, Gordon D M, Boslego J W, Krinchai K, Suarchawaratana P, Wongsrichanalai C, Ballou W R, et al. Safety, immunogenicity and limited efficacy study of a recombinant Plasmodium falciparum circumsporozoite vaccine in Thai soldiers. Vaccine. 1994;12:102–108. doi: 10.1016/0264-410x(94)90046-9. [DOI] [PubMed] [Google Scholar]
- 7.Burg J L, Perelman D, Kasper L H, Ware P L, Boothroyd J C. Molecular analysis of the gene encoding the major surface antigen of Toxoplasma gondii. J Immunol. 1988;141:3584–3591. [PubMed] [Google Scholar]
- 8.Buxton D, Innes E A. A commercial vaccine for ovine toxoplasmosis. Parasitology. 1995;110:S11–S16. doi: 10.1017/s003118200000144x. [DOI] [PubMed] [Google Scholar]
- 9.Buxton D, Thomson K M, Maley S, Wright S, Bos H J. Experimental challenge of sheep 18 months after vaccination with a live (S48) Toxoplasma gondii vaccine. Vet Rec. 1993;133:310–312. doi: 10.1136/vr.133.13.310. [DOI] [PubMed] [Google Scholar]
- 10.Chan S, Gabra H, Hill F, Evan G, Sikora K. A novel tumour marker related to the c-myc oncogene product. Mol Cell Probes. 1987;1:73–82. doi: 10.1016/0890-8508(87)90008-9. [DOI] [PubMed] [Google Scholar]
- 11.Dubey J P. Strategies to reduce transmission of Toxoplasma gondii to animals and humans. Vet Parasitol. 1996;64:65–70. doi: 10.1016/0304-4017(96)00961-2. [DOI] [PubMed] [Google Scholar]
- 12.Dubremetz J F, Achbarou A, Bermudes D, Joiner K A. Kinetics and pattern of organelle exocytosis during Toxoplasma gondii/host-cell interaction. Parasitol Res. 1993;79:402–408. doi: 10.1007/BF00931830. [DOI] [PubMed] [Google Scholar]
- 13.Frenkler J K. Pathophysiology of toxoplasmosis. Parasitol Today. 1988;4:273. doi: 10.1016/0169-4758(88)90018-x. [DOI] [PubMed] [Google Scholar]
- 14.Gazzinelli R T, Denkers E Y, Sher A. Host resistance to Toxoplasma gondii: model for studying the selective induction of cell-mediated immunity by intracellular parasites. Infect Agents Dis. 1993;2:139–149. [PubMed] [Google Scholar]
- 15.Gerloni M, Baliou W R, Billetta R, Zanetti M. Immunity to Plasmodium falciparum malaria sporozoites by somatic transgene immunization. Nat Biotechnol. 1997;15:876–881. doi: 10.1038/nbt0997-876. [DOI] [PubMed] [Google Scholar]
- 16.Girdwood R W. ‘Protozoan’ infections in the immunocompromised patient—the parasites and their diagnosis. J Med Microbiol. 1989;30:3–16. doi: 10.1099/00222615-30-1-3. [DOI] [PubMed] [Google Scholar]
- 17.Godson G N, Ellis J, Svec P, Schlesinger D H, Nussenzweig V. Identification and chemical synthesis of a tandemly repeated immunogenic region of Plasmodium knowlesi circumsporozoite protein. Nature. 1983;305:29–33. doi: 10.1038/305029a0. [DOI] [PubMed] [Google Scholar]
- 18.Gramzinski R A, Maris D C, Doolan D, Charoenvit Y, Obaldia N, Rossan R, Sedegah M, Wang R, Hobart P, Margalith M, Hoffman S. Malaria DNA vaccines in Aotus monkeys. Vaccine. 1997;15:913–915. doi: 10.1016/s0264-410x(96)00270-8. [DOI] [PubMed] [Google Scholar]
- 19.Hochuli E, Bannwarth W, Döbeli H, Gentz R, Stüber D. Genetic approach to facilitate purification of recombinant proteins with a novel metal chelate adsorbent. Bio/Technology. 1988;6:1321–1325. [Google Scholar]
- 20.Hoffman S L, Doolan D L, Sedegah M, Aguiar J C, Wang R, Malik A, Gramzinski R A, Weiss W R, Hobart P, Norman J A, Margalith M, Hedstrom R C. Strategy for development of a pre-erythrocytic Plasmodium falciparum DNA vaccine for human use. Vaccine. 1997;15:842–845. doi: 10.1016/s0264-410x(96)00273-3. [DOI] [PubMed] [Google Scholar]
- 21.Hollingdale M R, Nardin E H, Tharavanij S, Schwartz A L, Nussenzweig R S. Inhibition of entry of Plasmodium falciparum and P. vivax sporozoites into cultured cells; an in vitro assay of protective antibodies. J Immunol. 1984;132:909–913. [PubMed] [Google Scholar]
- 22.Kim K, Soldati D, Boothroyd J C. Gene replacement in Toxoplasma gondii with chloramphenicol acetyltransferase as selectable marker. Science. 1993;262:911–914. doi: 10.1126/science.8235614. [DOI] [PubMed] [Google Scholar]
- 23.Lanar D E, Tine J A, de Taisne C, Seguin M C, Cox W I, Winslow J P, Ware L A, Kauffman E B, Gordon D, Ballou W R, Paoletti E, Sadoff J C. Attenuated vaccinia virus-circumsporozoite protein recombinants confer protection against rodent malaria. Infect Immun. 1996;64:1666–1671. doi: 10.1128/iai.64.5.1666-1671.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Levine N D. Progress in taxonomy of the apicomplexan protozoa. J Protozool. 1988;35:518–520. doi: 10.1111/j.1550-7408.1988.tb04141.x. [DOI] [PubMed] [Google Scholar]
- 25.McGregor I A. Towards a vaccine against malaria. Br J Biomed Sci. 1993;50:35–42. [PubMed] [Google Scholar]
- 26.Nussenzweig R S, Nussenzweig V. Antisporozoite vaccine for malaria: experimental basis and current status. Rev Infect Dis. 1989;11:S579–S585. doi: 10.1093/clinids/11.supplement_3.s579. [DOI] [PubMed] [Google Scholar]
- 27.Nussenzweig V, Nussenzweig R S. Rationale for the development of an engineered sporozoite malaria vaccine. Adv Immunol. 1989;45:283–334. doi: 10.1016/s0065-2776(08)60695-1. [DOI] [PubMed] [Google Scholar]
- 28.Ozaki L S, Svec P, Nussenzweig R S, Nussenzweig V, Godson G N. Structure of the Plasmodium knowlesi gene coding for the circumsporozoite protein. Cell. 1983;34:815–822. doi: 10.1016/0092-8674(83)90538-x. [DOI] [PubMed] [Google Scholar]
- 29.Reed R C, Louis Wileman V, Wells R L, Verheul A F, Hunter R L, Lal A A. Re-investigation of the circumsporozoite protein-based induction of sterile immunity against Plasmodium berghei infection. Vaccine. 1996;14:828–836. doi: 10.1016/0264-410x(95)00175-z. [DOI] [PubMed] [Google Scholar]
- 30.Sherwood J A, Copeland R S, Taylor K A, Abok K, Oloo A J, Were J B, Strickland G T, Gordon D M, Ballou W R, Bales J D, Jr, Wirtz R A, Wittes J, Gross M, Que J U, Cryz S J, Oster C N, Roberts C R, Sadoff J C. Plasmodium falciparum circumsporozoite vaccine immunogenicity and efficacy trial with natural challenge quantitation in an area of endemic human malaria of Kenya. Vaccine. 1996;14:817–827. doi: 10.1016/0264-410x(95)00221-l. [DOI] [PubMed] [Google Scholar]
- 31.Soldati D, Boothroyd J C. Transient transfection and expression in the obligate intracellular parasite Toxoplasma gondii. Science. 1993;260:349–352. doi: 10.1126/science.8469986. [DOI] [PubMed] [Google Scholar]
- 32.Soldati D, Boothroyd J C. A selector of transcription initiation in the protozoan parasite Toxoplasma gondii. Mol Cell Biol. 1995;15:87–93. doi: 10.1128/mcb.15.1.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Stoute J A, Ballou W R, Kolodny N, Deal C D, Wirtz R A, Lindler L E. Induction of humoral immune response against Plasmodium falciparum sporozoites by immunization with a synthetic peptide mimotope whose sequence was derived from screening a filamentous phage epitope library. Infect Immun. 1995;63:934–939. doi: 10.1128/iai.63.3.934-939.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Suresh K, Mak J W, Yong H S. Long term maintenance of Toxoplasma gondii (Rh strain) in Vero cell line and use of harvested antigens for immunodiagnosis. S E Asian J Trop Med Pub Health. 1991;22:124–128. [PubMed] [Google Scholar]
- 35.Tine J A, Lanar D E, Smith D M, Wellde B T, Schultheiss P, Ware L A, Kauffman E B, Wirtz R A, De Taisne C, Hui G S, Chang S P, Church P, Hollingdale M R, Kaslow D C, Hoffman S, Guito K P, Ballou W R, Sadoff J C, Paoletti E. NYVAC-Pf7: a poxvirus-vectored, multiantigen, multistage vaccine candidate for Plasmodium falciparum malaria. Infect Immun. 1996;64:3833–3844. doi: 10.1128/iai.64.9.3833-3844.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Vergara U, Gwadz R, Schlesinger D, Nussenzweig V, Ferreira A. Multiple non-repeated epitopes on the circumsporozoite protein of Plasmodium knowlesi. Mol Biochem Parasitol. 1985;14:283–292. doi: 10.1016/0166-6851(85)90056-8. [DOI] [PubMed] [Google Scholar]
- 37.World Health Organization. Biological substances. International standards, reference preparations, and reference reagents. Geneva, Switzerland: World Health Organization; 1977. pp. 20–21. [Google Scholar]