Abstract
Background and Objectives
To determine gender differences in headache types diagnosed, sociodemographic characteristics, military campaign and exposures, and health care utilization among US veterans in the Veterans Health Administration (VHA).
Methods
This study used a retrospective cohort design to examine VHA electronic health record (EHR) data. This cohort includes veterans who had at least 1 visit for any headache between fiscal years 2008 and 2019. Headache diagnoses were classified into 8 categories using International Classification of Disease, Clinical Modification codes. Demographics, military-related exposures, comorbidities, and type of provider(s) consulted were extracted from the EHR and compared by gender. Age-adjusted incidence and prevalence rates of medically diagnosed headache disorders were calculated separately for each type of headache.
Results
Of the 1,524,960 veterans with headache diagnoses included in the cohort, 82.8% were men. Compared with women, men were more often White (70.4% vs 56.7%), older (52.0 ± 16.8 vs 41.9 ± 13.0 years), with higher rates of traumatic brain injury (2.9% vs 1.1%) and post-traumatic stress disorder (23.7% vs 21.7%), and lower rates of military sexual trauma (3.2% vs 33.7%; p < 0.001 for all). Age-adjusted incidence rate of headache of any type was higher among women. Migraine and trigeminal autonomic cephalalgia rates were most stable over time. Men were more likely than women to be diagnosed with headache not otherwise specified (77.4% vs 67.7%) and have higher incidence rates of headaches related to trauma (3.4% vs 1.9% [post-traumatic]; 5.5% vs 5.1% [postwhiplash]; p < 0.001 for all). Men also had fewer headache types diagnosed (mean ± SD; 1.3 ± 0.6 vs 1.5 ± 0.7), had fewer encounters for headache/year (0.8 ± 1.2 vs 1.2 ± 1.6), and fewer visits to headache specialists (20.8% vs 27.4% p < 0.001 for all), compared with women. Emergency department utilization for headache care was high for both genders and higher for women compared with men (20.3% vs 22.9%; p < 0.001).
Discussion
Among veterans with headache diagnoses, important gender differences exist for men and women veterans receiving headache care within VHA regarding sociodemographic characteristics, headache diagnoses, military exposure, and headache health care utilization. The findings have potential implications for providers and the health care system caring for veterans living with headache.
Headache is one of the most common and debilitating neurologic conditions encountered by neurologists and other health care providers.1 The worldwide lifetime prevalence of any headache disorder is 66%, with half of all people with a diagnosed headache disorder experiencing headache attacks annually.1,2 Prevalence estimates vary by headache type, age, gender, race, and ethnicity.3 Gender differences have also been reported for headache health care utilization, with women seeking medical care and seeing specialists for headache management more than men.4 Estimates of headache diagnoses and receipt of headache care are built on studies of community-based samples that have consistently demonstrated disparities in care and areas in need of improvement,1,5-8 including diagnosis, coding, treatment, and referral processes related to headache.
Headache disorders are problematic in veterans beyond high rates of primary headache disorders. Traumatic brain injury (TBI) or other injuries sustained during deployment (e.g., whiplash) can lead to headache. Other military-related exposures (e.g., combat or military sexual trauma [MST]-related post-traumatic stress disorder [PTSD], airborne hazards, and burn pit) may increase headache risk.9-12 However, relatively few studies have examined headache disorders in US veterans. Most studies to date generally focused on veterans of the recent military campaigns in Iraq and Afghanistan.13-15
Veterans served by the VHA are predominantly men; however, the number of women has been growing. Attributed partly due to changes in legislation, women have been enlisting into the military at higher rates during more recent military campaigns. Among veterans, women are younger and more likely to be from a minority background compared with men.16 Conducting epidemiologic investigations within the VHA examining gender differences across sociodemographic characteristics, military campaign and exposures, headache diagnoses, and health care utilization is imperative. Such studies would forward our understanding of the population-level burden within the largest integrated health care system in the United States. They would also guide explorations related to patient-level burden of headache, identify patient and health care system factors associated with care quality, and inform policy change should meaningful health care differences and disparities be identified. We report on gender differences in headache diagnoses, sociodemographic characteristics, military campaign and exposures, and health care utilization among veterans receiving care within the VHA.
Methods
Cohort Design and Study Population
The VHA serves more than 9 million veterans annually across 1,293 health care facilities17; all VHA medical centers (VAMCs) and clinics use the same electronic health record (EHR) platform. A total of 9.1 million inpatient records and 2.4 billion outpatient visits from October 1, 2007 (fiscal year [FY] 2008) to September 30, 2019 (FY2019) were searched to gather veterans medically diagnosed with headache disorders. As part of the Congressionally mandated VHA Headache Centers of Excellence (HCoE) program, the VHA HCoE Administrative Data cohort was created to improve our understanding of the epidemiology of headache and headache care within the VHA. In the spirit of the VHA Learning Healthcare System, these data are also intended to be used to improve headache care quality and delivery for veterans living with headache disorders.18
First, International Classification of Diseases 9th version (ICD-9-CM) and 10th version (ICD-10-CM) codes for headache disorders were identified with guidance from the American Academy of Neurology (AAN)19 and the International Headache Society.20 Next, we accessed the Centers for Medicare and Medicaid Services General Equivalence Mapping crosswalk to link the ICD-9-CM headache codes to the ICD-10-CM codes.21 Four United Council for Neurologic Subspecialties [UCNS] Headache Medicine Certified neurologists independently reviewed the crosswalk of headache diagnoses. Using both ICD-9-CM and ICD-10-CM codes, headache diagnoses were then classified into 8 categories: headache, not otherwise specified (NOS), migraine, tension-type headache (TTH), trigeminal autonomic cephalalgias (TACs), other primary headache disorders (e.g., new daily persistent headache), post-traumatic headache (PTHA), postwhiplash headache (PWHA), and other secondary headache disorders (e.g., headache attributed to infection). Given the importance of headache related to head trauma, separate categories for PTHA and PWHA were created (eTable 1, links.lww.com/WNL/C327).
We adapted a validated algorithm to identify veterans with specific (nonheadache) conditions using VHA electronic clinical and administrative data sources.22 We included 1,562,036 veterans who had at least 1 outpatient or inpatient visit with an ICD-CM–coded headache diagnosis between FY 2008 and FY 2019. One single visit was sufficient for cohort entry, given concerns informed by clinical experience and the literature about the underestimation of headache diagnoses within and outside of the VHA.23 However, those veterans who only had inpatient visits and without any outpatient visits during the cohort period were determined to be singular time-limited headaches associated with an acute or exacerbated medical condition leading to hospitalization and hence were excluded from this analysis (n = 37,058). veterans may have multiple specific headache types over the 12-year period. The index date for entry into the cohort was the date of the veteran's first headache diagnosis coded in the EHR during the cohort period FY 2008–2019. We also excluded veterans younger than 18 years during cohort entry (n = 18; likely data entry errors in the year of birth).
Measures and Variables
For included veterans, we obtained demographics from VHA Corporate Data Warehouse (CDW) at initial headache diagnosis including gender (assessed as a dichotomous social construct, men/women), age, race (American Indian or Alaska Native, Asia, Black or African American, Native Hawaiian or Other Pacific Islander, White, or unknown), and ethnicity (Spanish, Hispanic, and Latino) assessed through self-report on enrollment or update in the health care system, marital status, military campaign, and military exposures. Military campaign refers to an era of service rather than combat deployment and was categorized into World War II, Korean Conflict, Vietnam War, first Persian Gulf War, Operation Enduring Freedom/Operation Iraqi Freedom/Operation New Dawn (OEF/OIF/OND), or others/unknown (e.g., current active duty, World War I, and missing). Anthropometric measurements were extracted from the closest measurement within the window of 1 year before and up to 6 months after to headache index date. Height was recorded as the median height from all available measurements. Weights <75 or >700 lbs, or heights <48 or >84 inches were considered biologically implausible24 and therefore excluded. Body mass index (BMI) was calculated as weight in pounds by height in inches squared and multiplying by a conversion factor of 703.
Military exposure factors, physical and mental health comorbidities, and nonheadache painful condition data were obtained from CDW. TBI, PTSD, and MST were of particularly high interest. MST was defined by 38 US Code § 1720D as “physical assault of a sexual nature, battery of a sexual nature, or sexual harassment which occurred while the veteran was serving on active duty or active-duty training.” MST was coded positive if at least one of the MST screens administered to the veteran starting in 2008 was positive. Baseline comorbidity was defined as starting within the year before and up to 6 months after the first diagnosis of headache. We used diagnostic algorithms from other large VHA and non-VHA cohorts: Northeast Program Evaluation Center (NEPEC) for mental health conditions, Kaiser for musculoskeletal and pain conditions, the VHA Musculoskeletal Disorders Cohort, Veterans Aging Cohort Study, and Women Veterans Cohort.22,25,26 The coding of baseline comorbid conditions required at least 1 inpatient visit with a selected ICD-CM diagnostic code or 2 outpatient visits with selected ICD-CM diagnostic codes within 18 months of each other.
To assess clinical provider types and health care unitization, we defined clinics as Primary Care, Women's Health, Emergency Department (ED), Neurology, Physical Medicine and Rehabilitation (PM&R), Pain Management, and Mental Health. Within VHA, clinics and specialties are identified by unique stop codes, making it possible to determine where veterans attended when receiving headache care (eTable 2, links.lww.com/WNL/C327). To compare differences in visits with specialty types between men and women veterans, we further combined Primary Care and Women's Health as “Primary Care Plus.” All provider types were displayed as dichotomous variables. We also investigated the utilization of interdisciplinary care using a combination of different specialty types. For example, whether and when patients were seen or managed by Primary Care Providers and Neurologists.
Additional data gathered to construct the cohort included the following: outpatient prescriptions of headache abortive and conventional preventive medications, Calcitonin gene–related peptide antagonists and opioids; headache procedures such as occipital nerve blocks and neurotoxin injections identified by common procedural terminology (CPT); nonpharmacologic headache interventions such as physical therapy referral and biofeedback, and headache services under the purview of VHA prosthetics (e.g., neuromodulator devices, oxygen). Geographic location of veterans across the United States was also determined from administrative data by mapping veterans to the VAMC assigned by the VHA as their primary location of receiving care. VAMCs are nested within geographic regions known as Veterans Integrated Service Networks (VISNs; eTable 3, links.lww.com/WNL/C327).
Statistical Analysis
Categorical variables were reported as frequencies and percentages and continuous variables as mean values and SDs. Differences between men and women veterans were compared using the χ2 test for categorical variables and independent sample t test for continuous variables. A p value <0.05 was considered statistically significant. We also indicated categorical results that reflected at least 2% absolute difference or a 2-fold difference in overall proportions or followed Cohen conventions of d ≥ 0.20 as a statistical test for clinical significance. All analyses were performed using SAS version 9.4 (Cary, NC).
The crude incidence rates equal the total number of new headaches diagnosed in a specific fiscal year divided by the at-risk population. Period prevalence was defined as the number of veterans with at least 1 outpatient encounter in a specific fiscal year divided by the total VHA population. Incidence and prevalence rates were reported as number of cases per 100,000 people per year. After visualizing the age distributions of men and women veterans, age-adjusted rates were calculated to the 2010 US standard population. The proportions of the 2010 US standard population in each age group serve as weights for calculating age-adjusted rate. In addition, incidence rates at FY 2008 were not reported because veterans could previously be diagnosed with headache disorders before cohort initiation. Then, age-adjusted incidence rate for each specific headache type was calculated separately.
Standard Protocol Approvals, Registrations, and Patient Consents
The VHA HCoE Administrative Data cohort was approved by the Institutional Review Board of the VHA Connecticut Healthcare System and granted a Health Insurance Portability and Accountability Act waiver and waiver of informed consent.
Data Availability
Anonymized data not published within this article will be made available by request from any qualified investigator. As per VA policy, analytic datasets used for this study are not permitted to leave the VA firewall without a Data Use Agreement. Drs. Sico, Fenton, Wang, and Seng affirm that the manuscript is an honest, accurate, and transparent account of the resource and analyses being described; no important aspects have been omitted.
Results
Description of Veterans With Headache by Gender
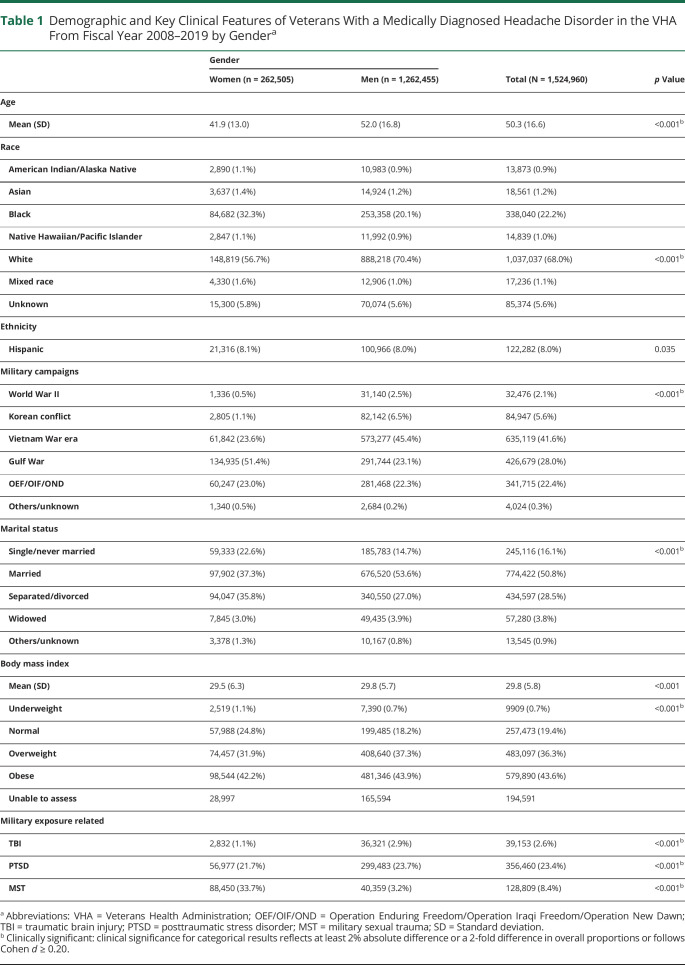
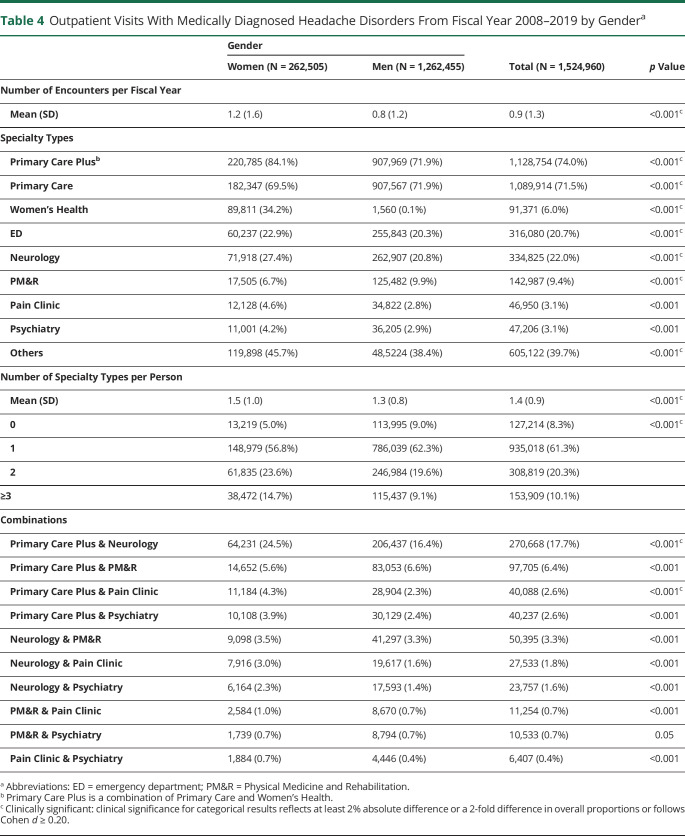
A total of 11.5 million veterans were served by the VHA in the 12 years of observation covered by the headache cohort; 7.4% of them were women. The VHA HCoE Administrative Data Cohort includes 1,524,960 distinct veterans who were medically diagnosed with any type of headache in at least 1 outpatient visit (a total of 8.2 million visits for headache) between FY 2008 and FY 2019 (Table 1). Women made up 17.2% of the cohort and were significantly younger (41.9 vs 52.0 years), more often non-White (43.3% vs 29.6%), and unmarried (62.7% vs 43.4%), compared with men. Women are an increasing proportion of veterans serving in more recent military campaign eras; three-quarters of women veterans served after Vietnam when compared with 45.6% of men veterans. A bimodal age distribution for first headache diagnosis was noted in men, whereas a single peak for women aged 25–29 years was noted (Figure 1). Regarding events/conditions of high interest in the VHA, men with headache had clinically significant higher rates of overweight/obesity (81.0% vs 74.3%), TBI (2.9% vs 1.1%), and PTSD (23.7% vs 21.7%) and lower rates of MST (3.2% vs 33.7%).
Table 1.
Demographic and Key Clinical Features of Veterans With a Medically Diagnosed Headache Disorder in the VHA From Fiscal Year 2008–2019 by Gendera
Figure 1. Baseline Age Distribution of Veterans in the VHA HCoE Administrate Data Cohort by Gender.
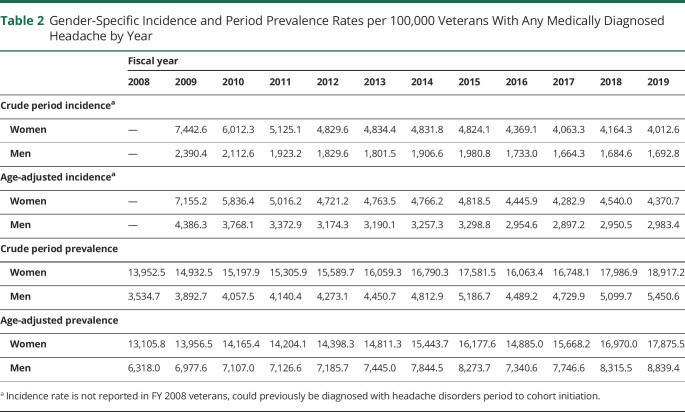
Description of Headache Types and Incidence
Table 2 summarizes the gender-specific incidence and 1-year period prevalence rates of “any headache” diagnosis per 100,000 veterans per fiscal year. Age-adjusted incidence rates of medically diagnosed headache disorders were higher among women veterans in all years observed, with a range of 4,283 to 7,155 per 100,000 compared with a range of 2,897 to 4,386 per 100,000 for men. While age-adjusted incidence rates decreased over time for both genders, we saw an increase in the 1-year period prevalence rates over the same period for men and women. The age-adjusted prevalence rates of headache in women veterans were always higher than men.
Table 2.
Gender-Specific Incidence and Period Prevalence Rates per 100,000 Veterans With Any Medically Diagnosed Headache by Year
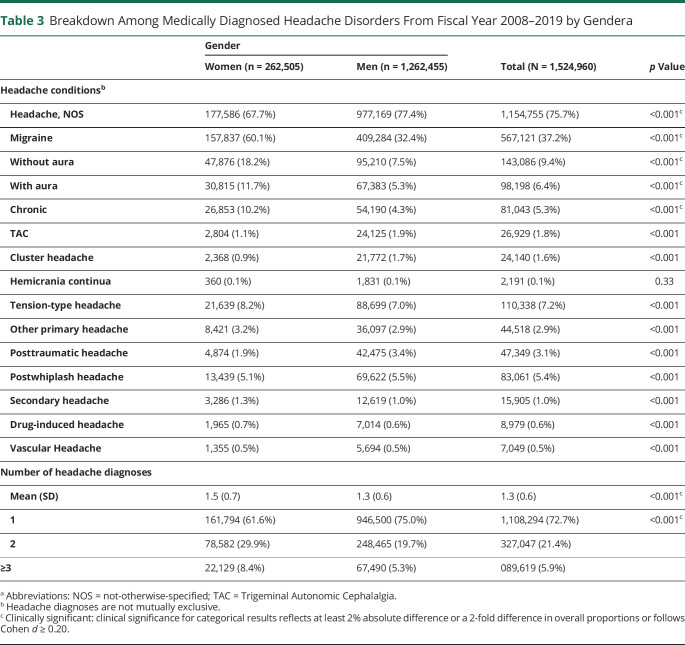
Table 3 lists the number of veterans who were given each headache diagnosis stratified by gender; individual patients may be listed more than 1 time in this Table. More than three-quarters of veterans within the VHA HCoE Administrative Data Cohort dataset received a diagnosis of headache NOS, with migraine being the next most common headache diagnosis. There were significant differences between men and women in the cohort on headache NOS, migraine and migraine subtypes, and statistically significant differences on all other headache types, except for hemicrania continua (p = 0.33). A higher proportion of men in the VHA HCoE Administrative Data cohort had diagnoses of headache NOS (77.4% vs 67.7%), post-traumatic headache (3.4% vs 1.9%), postwhiplash headache (5.5% vs 5.1%), and cluster headache (1.7% vs 0.9%) than women. A higher proportion of women were diagnosed with migraine (60.1% vs 32.4%, including all migraine subtypes), tension-type headache (8.2% vs 7.0%), other primary (3.2% vs 2.9%), and other secondary headaches (1.3% vs 1.0%). More men than women had only a single headache type documented (75.0% vs 61.6%).
Table 3.
Breakdown Among Medically Diagnosed Headache Disorders From Fiscal Year 2008–2019 by Gendera
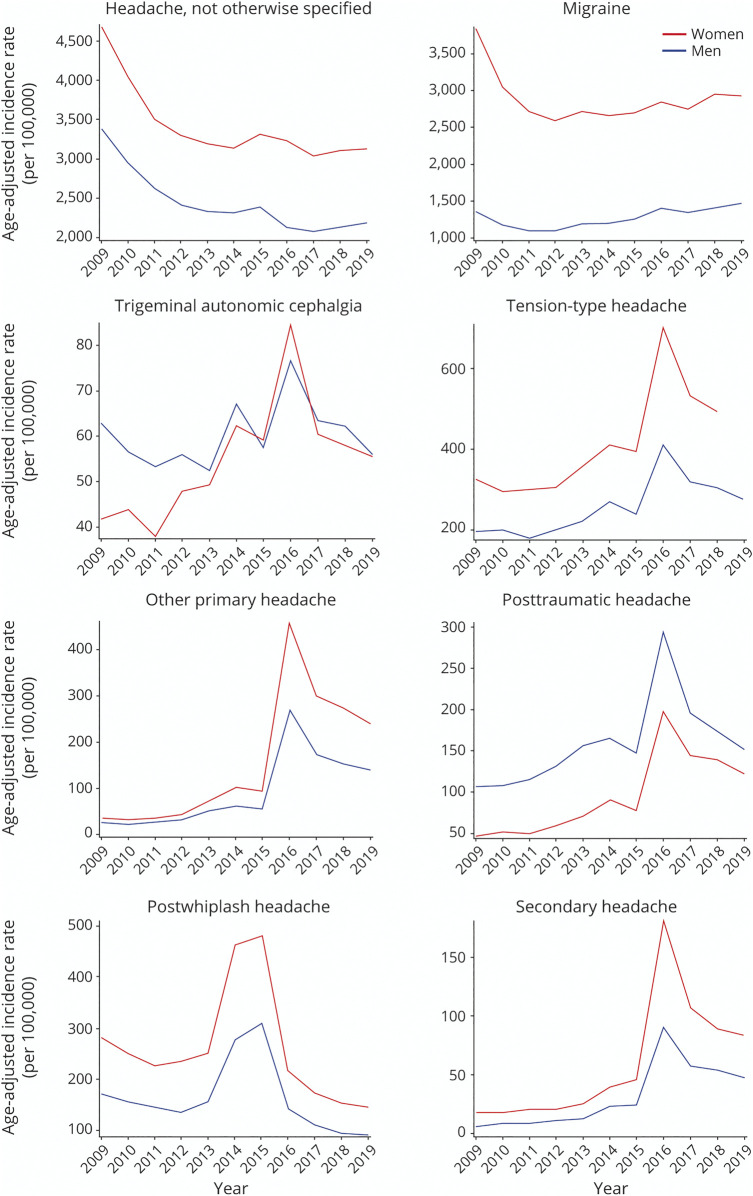
Figure 2 shows the age-adjusted gender-specific incidence rates for each distinct headache type per 100,000 veterans per fiscal year. Of note, the VHA transitioned from ICD-9-CM to ICD-10-CM at the beginning of FY 2016 (on October 1, 2015). We observed that the incidence curves for the specific headache types were quite different over time. Whereas the incidence rate of migraine remained stable from FY 2009 onward, TAC, tension-type headache, other primary headache, PTHA, and other secondary headache showed sharp increases after the establishment of the ICD-10-CM. The incidence rate for PWHA had a surge in FY 2014 and FY 2015 and then dropped back to their baseline rates after the transition to ICD-10-CM. Men and women had incidence profiles that were similar in shape, with women veterans having higher rates for all headaches but PTHA and TACs.
Figure 2. Age-Adjusted Headache Incidence of Distinct Headache Types Encountered Within the Veterans Health Administration, Stratified by Gender and Standardized to the US Population (2010), Fiscal Year 2009–2019.
Headache-Related Care Utilization
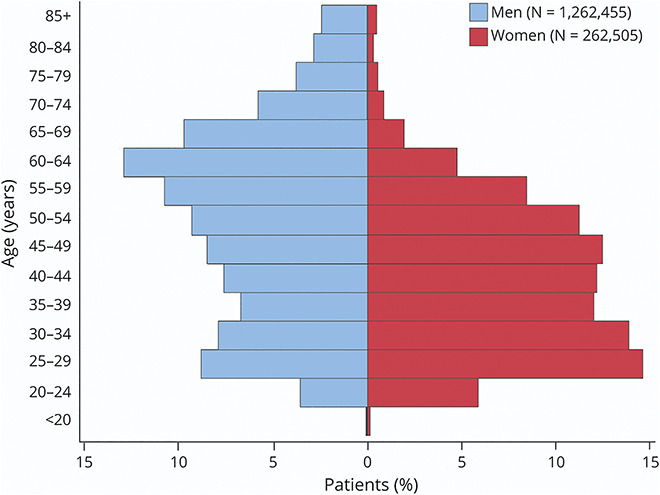
Women veterans with at least 1 headache diagnosis had a significant larger average number of annual encounters for headaches (1.2 vs 0.8) and were evaluated by more provider types (1.5 vs 1.3) for their headaches than men (Table 4). Seventy four percent of veterans receive their headache care from primary care providers, with less than a quarter of all veterans with headache seeing a neurologist. A significant greater proportion of women had Primary Care Plus visits (84.1% vs 71.9%), ED visits (22.9% vs 20.3%), Neurology visits (27.4% vs 20.8%), and other specialty visits (45.7% vs 38.4%). Meanwhile, significantly more men had PM&R visits (9.9% vs 6.7%) and were less likely to be evaluated by Pain Clinic Specialists (2.8% vs 4.6%) and Psychiatrists (2.9% vs 4.2%). For interdisciplinary headache care, significantly more women received their headache-related care from Primary Care Provider and Neurologist (24.5% vs 16.4%) and Primary Care Provider and Pain Clinic Specialist (4.3% vs 2.3%). Geographically, veterans with headache are served by VAMCs distributed across the country. However, distribution of headache cases overall and by gender varied across the VISNs (eTable 3, links.lww.com/WNL/C327).
Table 4.
Outpatient Visits With Medically Diagnosed Headache Disorders From Fiscal Year 2008–2019 by Gendera
Discussion
The VHA HCoE Administrative Data Cohort is the world's largest administrative dataset of patients with headache and was created to increase the understanding of headache among veterans. We reported data for more than 1.5 million veterans with headache across more than 8.2 million headache-related visits over a 12-year period in the largest integrated health care system in the United States, examining gender differences in headache types diagnosed, sociodemographic characteristics, military campaign and exposures, and health care utilization gender differences in age, race, ethnicity, military campaign era and military exposures, geography, diagnoses, and health care utilization. We found important gender differences in veterans with headache, which have potential implications for veterans, health care providers, and policy makers.
Men comprise both most of US veterans (90.6%)27 and of the VHA HCoE Administrative Data cohort (82.8%). When diagnosed with a headache disorder, men are more often classified as headache NOS, have a lower number of headache-related visits, and generally see providers other than their Primary Care providers (e.g., headache specialists) less frequently than women for headache care. Among all US veterans, men are significantly older than women.27 Similarly, within the VHA HCoE Administrative Data cohort, men were on average a decade older than women and had a bimodal distribution of age of first headache diagnosis; both men and women experienced peaks in headache diagnoses between 25 and 29 years of age, whereas men experienced a second peak between 60 and 64 years of age. The relatively low numbers of women veterans from conflicts before the Gulf War may at least partially explain both the gender difference in average age and the lack of bimodality in women. In addition, we found the incidence and prevalence rates of medically diagnosed headache disorders almost doubled when adjusted with 2010 US Standardized population among men. The age distribution shifts between veterans and the US population highlights the unique composition in headaches diagnosed and treated in the VHA. The earlier peak for rates of headache among younger veterans is not surprising because headache commonly affects people during their most productive years and preferentially so among women.3,28 Reports on the 1-year period prevalence of medically diagnosed migraine show an increase for both men and women up until ages 30–39 years, with prevalence higher for women than for men (24.4% vs 7.4%). Among patients 60 years and older, the prevalence of migraine for women and men decreases substantially (5.0% vs 1.6%).29 VHA-based studies examining headache among veterans serving in the most recent military campaigns in Iraq and Afghanistan find comparable mean ages between men and women with migraine and that most with headache occur in persons younger than 50 years.14,23
The overall proportion of Black veterans with headache (22.2%) is elevated in comparison with their representation in the VHA (overall 12%; men: 10.0%, women 18.9%).27 This trend may be partially explained by the fact that Black veterans are more likely to be women and younger, groups at a higher risk for headache disorders. Data from the 2014 National Health Interview Survey reported that 15.0% of Black persons or persons of African American ancestry experienced migraine and severe headache.3
In considering conditions associated with military service, TBI is a signature injury of modern military conflicts.30 Headache is the most common persistent symptom after TBI, with an incidence reaching 90%; approximately 15%–53% of these patients going on to develop persistent PTHA.31 The literature on veterans suggests that women are less likely to sustain a TBI, but more likely to report headache after TBI than men.32 In our study, men had higher rates of PTHA, which may be accounted for by the higher rate of TBI among men. PTSD and TBI are more common among veterans with headache compared with those without headache, and PTSD itself may also exacerbate headache.13,33 Among veterans, military sexual trauma occurs in 8.4% overall, in 33%–41% of women and in 1%–4% of men; headache is one of the many physical symptoms associated with this form of trauma.34,35
Our current work confirms gender differences in headache diagnoses; women are more frequently diagnosed with migraine and tension-type headache than men. Men are more frequently diagnosed with cluster headache, other TACs, and headaches associated with trauma, specifically post-trauma headache and postwhiplash headache.36,37 A large percentage of veterans with headache were diagnosed with headache NOS, an ICD-CM symptom code that typically represents a failure to accurately diagnose an ICHD-defined primary or secondary headache disorder or disorders. Two studies reported the proportions of headache NOS diagnosed in the Emergency Department were 26% and 42%, respectively.38,39 Reasons why men may have had higher rates of being diagnosed with headache NOS in VHA administrative data likely are less related to the underlying biology of headache. Rather, this phenomenon may reflect a combination of men seeing fewer headache specialists invested in making specific diagnoses, possible underreporting of or experiencing headache and headache-associated symptoms, which would support a more specific diagnosis, a lower number of follow-up visits, and hence opportunities to make a more specific diagnosis, for men compared with women, deficiencies in diagnosis and coding by health care providers, and implicit bias providers may have toward headache in men.
We also observed dramatic increase in the incidence rates of TAC, TTH, other primary headache, PTHA, and other secondary headache after the transition from ICD-9-CM to ICD-10-CM coding. One VHA study revealed a 75% consistency of headache ICD-CM codes assigned to the same patients before and after the transition.40 Although ICD-9-CM and ICD-10-CM share similar hierarchy on disease classification, ICD-10-CM is more granular and contains 7-fold more diagnostic codes, which allows for greater diagnostic specificity. A good example is the coding of other secondary headache attributed to cranial or cervical vascular disorder. In ICD-10-CM, vascular headache was coded as G44.1 and was included with 784.0, a nonspecific symptom code in ICD-9-CM. This cross-sectional difference due to coding transition was also observed in subarachnoid hemorrhage, intracerebral hemorrhage, ischemic stroke, and Parkinson disease.41 Without sudden changes in the rate of exposure or health care access, incidence of a chronic disease should remain constant over time. The incidence of headaches in recent fiscal years returns to similar rates before the ICD-9/10-CM transition; thus, the distinct headache incidences examined in this national veteran cohort are relatively accurate. While it remains unclear why there was a surge in PWHA incidence in FYs 2014 and 2015, we hypothesize that this phenomenon is linked to the Polytrauma Blast-Related Injury Quality Enhancement Research Initiative on OEF/OIF/OND Veterans with TBI sequelae in 2013.42 Exactly how the coding of discrete headache diagnoses may have been affected by the coding transition needs to be addressed in future work.
Women on average had more visits for headache than did men, were more likely to see a health care professional other than a primary care provider for their headache, and to see multiple specialists, with the exception that men were more likely to see physiatrists as part of their headache management. In VHA, physiatrists are more often responsible for polytrauma centers than neurologists, and there was more medically diagnosed TBI in men than women with headache. Women with migraine were more likely than men with migraine to report having consulted any doctor for headache management. In a study of a single VHA Polytrauma Center, men veterans with a positive mTBI screen and persistent headaches refused Neurology clinic referrals more often than women. Still, for those who accepted a Neurology Clinic referral, nearly 70% appeared for the initial Neurology Clinic appointment and 29.2% appeared for at least 1 follow-up appointment.31
Gender differences in health care use may reflect differences in rates of various headache disorders, severity, and patterns of consultation for those disorders among veterans. For example, in both the American Migraine Study and VHA Polytrauma Center study, patients were more likely to accept a referral outside of primary care if they were having more severe headache pain.31,43 In our cohort, headache care was delivered to 20.7% of veterans with headache in the VHA ED, more frequently for women than men. Headache is one of the most common reasons for patients to go to EDs for patient ages 15–64 years, being the 6th and 19th most common diagnosis seen in women and men, respectively.3 The lifetime prevalence of ED use for headache management differs between women and men with migraine (19.5% vs 13.4%).44 Among the limitations, our cohort comprised US military veterans served by the VHA, a predominantly male population. While these results may be less generalizable to other populations, the VHA HCoE Administrative Data Cohort allows for an unparalleled opportunity to study headache among men and examine rarer headache diagnoses in men and women (e.g., hemicrania continua). Regarding gender, the VHA recorded self-reported binary gender in the EHR during the study period. As EHR data capture extends beyond these binary categories, future headache studies should include transgender and nonbinary gender identities. While we examined military campaign and exposures, VHA data do not routinely have the branch of the military veterans served in. Noting that military exposures may vary by service branch suggest that headache may differ across service branches. Our administrative data cohort relies on ICD-CM codes entered by providers working within a nonfee for service health care system. Patients reported here have been medically diagnosed with headache by various VHA providers; as such, universal use of validated instruments to diagnose specific headache diagnoses did not occur nor would be feasible. In addition, while this cohort has a sizable number of cases, undercoding of specific headache diagnoses likely occurs. Similar to claims data, VHA administrative data do not routinely capture pain severity, frequency, disability, or other measures of the burden headache imposes on patients. Furthermore, while men are less likely to see neurologists and other headache specialists in our cohort, we cannot determine whether this is due to unobserved patient and/or provider factors such as differences in real and reported headache severity and frequency between men and women, whether men are less apt to seek medical assistance in the form of a referral45 or be given a referral, or other reasons that may determine referral patterns. Finally, we do not currently report headache treatment or a comprehensive list of chronic pain and mental health comorbidities. The decision was made to not include that data here, given the heterogeneity of headaches and noting that some treatments are more applicable to specific headache types.
Our current findings have important headache management implications for providers and health care systems. Recognizing the large number of older veterans with headache, providers should consider tailoring treatment regimens to this age group and undertake evaluation for secondary causes of headache as appropriate.46,47 Understanding the racial and ethnic composition is imperative to delivering high-quality guideline concordant care. Migraine attacks have been found to be more severe and frequent among Black patients compared with White patients with migraine, perhaps due to stresses related to minority status and observed underutilization of headache services.48 Evaluation and treatment strategies should be sensitive to these racial/ethnic differences. Clinicians providing headache care for veterans with TBI, PTSD, and MST should be aware of potential treatment implications, both holistically and for headache management, in the presence of these conditions. From a health care systems perspective, specific areas that warrant attention include the high rates of both ED utilization for headache care and headache NOS diagnoses. Veterans with headache are going to the ED at roughly the same proportion as going to a neurologist or a higher rate than to other headache specialists. One likely predictor of higher ED use for headache may be limited access to providers with expertise in headache care. Reduced access is likely contributing to the observed rates of headache NOS. It would be impossible for the more than 1 million veterans living with a headache NOS diagnosis to see a headache specialist. Large-scale educational interventions focusing on accurate and specific headache diagnoses and coding, alone or in combination with EHR/informatics-based approaches, could begin addressing this important and previously underappreciated issue among veterans.
Acknowledgment
The authors thank Drs. Christopher Gottschalk MD, FAHS, Chief of the Division of General Neurology at Yale School of Medicine who assisted in the review of ICD-CM headache codes for the creation of the VHA HCoE Administrative Data Cohort. The views expressed in this article are those of the authors and do not necessarily represent the view of the Department of Veterans Affairs.
Glossary
- AAN
American Academy of Neurology
- CPT
common procedural terminology
- CDW
Corporate Data Warehouse
- ED
Emergency Department
- EHR
Electronic Health Record
- FY
Fiscal Year
- HCoE
Headache Centers of Excellence
- MST
military sexual trauma
- NOS
not otherwise specified
- PTHA
post-traumatic headache
- PWHA
postwhiplash headache
- TBI
Traumatic brain injury
- PTSD
post-traumatic stress disorder
- TTH
tension-type headache
- TACs
trigeminal autonomic cephalalgias
- UCNS
United Council for Neurologic Subspecialties
- VHA
Veterans Health Administration
Appendix. Authors
Footnotes
Editorial, page 779
Study Funding
This study was funded by Veterans Health Administration Headache Centers of Excellence.
Disclosure
D. Kuruvilla serves as a consultant, advisory board member, or had received honoraria or research support from Theranica, Allergan/Abbvie, Eli Lilly and Company, Amgen/Novartis, Biohaven, Alphasites consulting, Cefaly, Neurolief, Nowwhat media, and KX advisors. R. Shapiro serves as a consultant for Eli Lilly and Company, and Lundbeck. E.K. Seng has consulted for GlaxoSmithKline and Click Therapeutics and received research funding from the NINDS (NS096107 PI: Seng). R.B. Lipton has received research support from the National Institutes of Health, the FDA, and the National Headache Foundation. He serves as consultant, advisory board member, or has received honoraria or research support from AbbVie/Allergan, Amgen, Biohaven, Dr. Reddy's Laboratories (Promius), electroCore, Eli Lilly, GlaxoSmithKline, Eli Lilly and Company, Lundbeck, Merck, Novartis, Teva, Vector, and Vedanta Research. He receives royalties from Wolff's Headache, 8th edition (Oxford University Press, 2009), and Informa. He holds stock/options in Biohaven and CntrlM. The other authors report no relevant disclosures. Go to Neurology.org/N for full disclosures.
References
- 1.Saylor D, Steiner TJ. The global burden of headache. Semin Neurol. 2018;38:182-190. [DOI] [PubMed] [Google Scholar]
- 2.Stovner L, Hagen K, Jensen R, et al. The global burden of headache: a documentation of headache prevalence and disability worldwide. Cephalalgia. 2007;27:193-210. [DOI] [PubMed] [Google Scholar]
- 3.Burch R, Rizzoli P, Loder E. The prevalence and impact of migraine and severe headache in the United States: updated age, sex, and socioeconomic‐specific estimates from government health surveys. Headache. J Head Face Pain. 2021;61:60-68. [DOI] [PubMed] [Google Scholar]
- 4.Lipton R, Scher A, Steiner T, et al. Patterns of health care utilization for migraine in England and in the United States. Neurology. 2003;60:441-448. [DOI] [PubMed] [Google Scholar]
- 5.Lipton RB, Manack Adams A, Buse DC, Fanning KM, Reed ML. A comparison of the chronic migraine epidemiology and outcomes (CaMEO) study and American migraine prevalence and prevention (AMPP) study: demographics and headache-related disability. Headache. 2016;56:1280-1289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lipton RB, Buse DC, Serrano D, Holland S, Reed ML. Examination of unmet treatment needs among persons with episodic migraine: results of the American Migraine Prevalence and Prevention (AMPP) Study. Headache. 2013;53:1300-1311. [DOI] [PubMed] [Google Scholar]
- 7.Callaghan BC, Burke JF, Kerber KA, et al. The association of neurologists with headache health care utilization and costs. Neurology. 2018;90:e525–e533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Smitherman TA, Burch R, Sheikh H, Loder E. The prevalence, impact, and treatment of migraine and severe headaches in the United States: a review of statistics from national surveillance studies. Headache. 2013;53:427-436. [DOI] [PubMed] [Google Scholar]
- 9.Chalela JA. New onset migraine associated with a civilian burn pit. Mil Med. 2017;182:e1812–e1813. [DOI] [PubMed] [Google Scholar]
- 10.Turner AP, Harding KA, Brier MJ, Anderson DR, Williams RM. Military sexual trauma and chronic pain in veterans. Am J Phys Med Rehabil. 2020;99:1020-1025. [DOI] [PubMed] [Google Scholar]
- 11.Afari N, Harder LH, Madra NJ, et al. PTSD, combat injury, and headache in Veterans Returning from Iraq/Afghanistan. Headache. 2009;49:1267-1276. [DOI] [PubMed] [Google Scholar]
- 12.Department of Veterans Affairs. Report on Data from the Airborne Hazards and Open Burn Pit (AH&OBP) Registry. Veterans Health Administration. Office of Public Health; 2015. [Google Scholar]
- 13.Carlson KF, Taylor BC, Hagel EM, Cutting A, Kerns R, Sayer NA. Headache diagnoses among Iraq and Afghanistan war veterans enrolled in VA: a gender comparison. Headache. 2013;53(10):1573-1582. [DOI] [PubMed] [Google Scholar]
- 14.Jaramillo CA, Eapen BC, McGeary CA, et al. A cohort study examining headaches among Veterans of Iraq and Afghanistan wars: associations with traumatic brain injury, PTSD, and depression. Headache. 2016;56:528-539. [DOI] [PubMed] [Google Scholar]
- 15.Ruff RL, Ruff SS, Wang XF. Headaches among Operation Iraqi Freedom/Operation Enduring Freedom Veterans with mild traumatic brain injury associated with exposures to explosions. J Rehabil Res Dev. 2008;45:941-952. [DOI] [PubMed] [Google Scholar]
- 16.Frayne S, Phibbs C, Saechao F, et al. Sourcebook: Women Veterans in the Veterans Health Administration. Volume 4: Longitudinal Trends in Sociodemographics, Utilization, Health Profile, and Geographic Distribution. Women's Health Services, Veterans Health Administration. Department of Veterans Affairs; 2018:1-132. [Google Scholar]
- 17.Department of Veterans Affairs. Veterans Health Administration [online]. Available at: va.gov/health/. Accessed December 13, 2021.
- 18.Atkins D, Kilbourne AM, Shulkin D. Moving from discovery to system-wide change: the role of research in a learning health care system: experience from three decades of health systems research in the veterans health administration. Annu Rev Public Health. 2017;38:467-487. [DOI] [PubMed] [Google Scholar]
- 19.Bever C, Dubinsky R, Tonn S, Swain-Eng R. For the Quality Measures and Reporting Subcommittee, 2010 edition. Quality measure development process manual; 2013. [Google Scholar]
- 20.Headache Classification Committee of the International Headache Society (IHS). The international classification of headache disorders, 3rd ed. Cephalalgia. 2018;38:1-211. [DOI] [PubMed] [Google Scholar]
- 21.The Centers for Medicare, Medicaid Services. ICD-10-CM and GEMs. Available at: cms.gov/Medicare/Coding/ICD10/2018-ICD-10-CM-and-GEMs. [PubMed] [Google Scholar]
- 22.Justice AC, Dombrowski E, Conigliaro J, et al. Veterans aging cohort study (VACS): overview and description. Med Care. 2006;44:S13-S24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Altalib HH, Fenton BT, Sico J, et al. Increase in migraine diagnoses and guideline-concordant treatment in Veterans, 2004-2012. Cephalalgia. 2017;37:3-10. [DOI] [PubMed] [Google Scholar]
- 24.Noël PH, Copeland LA, Perrin RA, et al. VHA Corporate Data Warehouse height and weight data: opportunities and challenges for health services research. J Rehabil Res Dev. 2010;47:739-750. [DOI] [PubMed] [Google Scholar]
- 25.Goulet JL, Kerns RD, Bair M, et al. The musculoskeletal diagnosis cohort: examining pain and pain care among Veterans. Pain. 2016;157:1696-1703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mayhew M, DeBar LL, Deyo RA, et al. Development and assessment of a crosswalk between ICD-9-CM and ICD-10-CM to identify patients with common pain conditions. J Pain. 2019;20:1429-1445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Department of Veterans Affairs. Profile of Veterans: 2017. National Center for Veterans Analysis and Statistics. wwwvagov/vetdata/reportasp 2020.
- 28.Lipton RB, Stewart WF, Diamond S, Diamond ML, Reed M. Prevalence and burden of migraine in the United States: data from the American Migraine Study II. Headache. 2001;41:646-657. [DOI] [PubMed] [Google Scholar]
- 29.Lipton RB, Bigal ME, Diamond M, Freitag F, Reed ML, Stewart WF. Migraine prevalence, disease burden, and the need for preventive therapy. Neurology. 2007;68:343-349. [DOI] [PubMed] [Google Scholar]
- 30.Hayward P. Traumatic brain injury: the signature of modern conflicts. Lancet Neurol. 2008;7:200-201. [DOI] [PubMed] [Google Scholar]
- 31.Patil VK, Andre StJR, Crisan E, et al. Prevalence and treatment of headaches in veterans with mild traumatic brain injury. Headache. 2011;51:1112-1121. [DOI] [PubMed] [Google Scholar]
- 32.Resnick EM, Mallampalli M, Carter CL. Current challenges in female Veterans' health. J Womens Health (Larchmt). 2012;21:895-900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Theeler B, Lucas S, Riechers Ii RG, Ruff RL. Post-traumatic headaches in civilians and military personnel: a comparative, clinical review. Headache. J Head Face Pain. 2013;53:881-900. [DOI] [PubMed] [Google Scholar]
- 34.Barth SK, Kimerling RE, Pavao J, et al. Military sexual trauma among recent veterans: correlates of sexual assault and sexual harassment. Am J Prev Med. 2016;50:77-86. [DOI] [PubMed] [Google Scholar]
- 35.Suris A, Lind L. Military sexual trauma: a review of prevalence and associated health consequences in Veterans. Trauma Violence Abuse. 2008;9:250-269. [DOI] [PubMed] [Google Scholar]
- 36.Lyngberg AC, Rasmussen BK, Jørgensen T, Jensen R. Has the prevalence of migraine and tension-type headache changed over a 12-year period? A Danish population survey. Eur J Epidemiol. 2005;20:243-249. [DOI] [PubMed] [Google Scholar]
- 37.Fischera M, Marziniak M, Gralow Ia, Evers S. The incidence and prevalence of cluster headache: a meta-analysis of population-based studies. Cephalalgia. 2008;28:614-618. [DOI] [PubMed] [Google Scholar]
- 38.Dermitzakis EV, Georgiadis G, Rudolf J, et al. Headache patients in the emergency department of a Greek tertiary care hospital. J Headache Pain. 2010;11:123-128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sahai‐Srivastava S, Desai P, Zheng L. Analysis of headache management in a busy emergency room in the United States. Headache. J Head Face Pain. 2008;48:931-938. [DOI] [PubMed] [Google Scholar]
- 40.Yoon J, Chow A. Comparing chronic condition rates using ICD-9 and ICD-10 in VA patients FY2014-2016. BMC Health Serv Res. 2017;17:572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hamedani AG, Blank L, Thibault DP, Willis AW. Impact of ICD-9 to ICD-10 coding transition on prevalence trends in Neurology. Neurol Clin Pract. 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cifu DX, Taylor BC, Carne WF, et al. Traumatic brain injury, posttraumatic stresss disorder, and pain diagnoses in OIF/OEF/OND veterans. Ethnicity. 2013;137:22. [DOI] [PubMed] [Google Scholar]
- 43.Lipton RB, Stewart WF, Simon D. Medical consultation for migraine: results from the American migraine study. Headache: J Head Face Pain. 1998;38:87-96. [DOI] [PubMed] [Google Scholar]
- 44.Friedman BW, Serrano D, Reed M, Diamond M, Lipton RB. Use of the emergency department for severe headache. A population-based study. Headache. 2009;49:21-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Addis ME, Mahalik JR. Men, masculinity, and the contexts of help seeking. Am Psychol. 2003;58:5-14. [DOI] [PubMed] [Google Scholar]
- 46.VA/DoD Clinical Practice Guidelines - the Primary Care Management of Headache; 2020. [Google Scholar]
- 47.Goldstein J, Camargo C, Pelletier A, Edlow J. Headache in United States emergency departments:demographics, work-up and frequency of pathological diagnoses. Cephalalgia. 2006;26:684-690. [DOI] [PubMed] [Google Scholar]
- 48.Nicholson RA, Rooney M, Vo K, O'Laughlin E, Gordon M. Migraine care among different ethnicities: do disparities exist? Headache. J Head Face Pain. 2006;46:754-765. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Anonymized data not published within this article will be made available by request from any qualified investigator. As per VA policy, analytic datasets used for this study are not permitted to leave the VA firewall without a Data Use Agreement. Drs. Sico, Fenton, Wang, and Seng affirm that the manuscript is an honest, accurate, and transparent account of the resource and analyses being described; no important aspects have been omitted.