Abstract
Background and Objective
To describe the relative frequency, demographics, comorbidities, and health care utilization of veterans who receive migraine care at the Veteran's Health Administration (VHA) and to evaluate differences by gender.
Methods
This study extracted data from VHA administrative sources. Veterans diagnosed with migraine by a health care provider between fiscal year 2008 and 2019 were included. Demographics and military exposures were extracted at cohort entry. Comorbidities were extracted within 18 months of the first migraine diagnosis. Health care utilization and headache comorbidities were extracted across the study period. Differences between men and women were evaluated using χ2 tests and Student t tests.
Results
More than half a million (n = 567,121) veterans were diagnosed with migraine during the 12-year study period, accounting for 5.3% of the 10.8 million veterans served in the VHA; in the most recent year of the study period (2019), the annual incidence and 1-year period prevalence of medically diagnosed migraine was 2.7% and 13.0% for women and 0.7% and 2.5% for men. In the total cohort diagnosed with migraine, 27.8% were women and 72.2% men. Among those with diagnosed migraine, a higher proportion of men vs women also had a TBI diagnosis (3.9% vs 1.1%; p < 0.001). A higher proportion of women vs men reported military sexual trauma (35.5% vs 3.5%; p < 0.001). Participants with diagnosed migraine had an average of 1.44 (SD 1.73) annual encounters for headache. Primary care was the most common headache care setting (88.1%); almost one-fifth of veterans with diagnosed migraine sought care in the ED at least once during the study period. Common comorbidities were overweight/obesity (80.3%), nonheadache pain disorders (61.7%), and mental health disorders (48.8%).
Discussion
Migraine is commonly treated in the VHA setting, but likely underascertained. Most people treated for migraine in the VHA are men. Pain comorbidities and psychiatric disorders are common. Future research should identify methods to improve diagnosis and treatment and to reduce use of the emergency department.
Migraine is common in adults, with a 1-year period prevalence of 6%–10% in men and 18%–21% in women in the United States.1-3 Migraine is particularly burdensome with a greater prevalence during midlife years when productivity is highest.1,4 Migraine is associated with higher health care utilization and direct medical costs compared with age, gender, and comorbidity-matched controls.5,6 Improving migraine care quality could improve quality of life for a large number of people with migraine.7-9
The Veteran's Health Administration (VHA) is the largest integrated health care system in the United States.10 The VHA serves roughly 9 million veterans annually across 171 medical centers and 1,112 outpatient clinics throughout the United States.
Understanding the characteristics of veterans with migraine presenting to the VHA is the first step toward identifying gaps and improving quality of care.6,11 Most of the patients by the VHA are men (90.4% in 2017)10 providing a unique opportunity to better understand migraine in men.12 Furthermore, the VHA gives us an opportunity to evaluate service-related exposures (for example, traumatic brain injury [TBI], the “signature injury” of the recent conflicts in Iraq and Afghanistan [Operation Enduring Freedom/Operation Iraqi Freedom/Operation New Dawn; OEF/OIF/OND],13 and military sexual trauma14) that could contribute to the development and course of migraine.15-19
The current cohort study describes the annual incidence and 1-year prevalence of medically diagnosed migraine in the VHA, as well as the demographics, comorbidities, and health care utilization of veterans with medically diagnosed migraine by gender.
Methods
Standard Protocol Approvals, Registrations, and Patient Consents
The VHA HCoE Administrative Data Headache Cohort protocol has been approved by the VA Connecticut Healthcare System Institutional Review Board, which approved a waiver of informed consent.
Study Design
This cohort study evaluated differences in demographics, comorbidities, and health care utilization among men and women who presented to any VHA facility with migraine diagnosed by a health care provider during fiscal year (FY) 2008–2019 (corresponding to October 1, 2007—September 30, 2019).
Participants and Procedures
This study used the VHA Headache Centers of Excellence (HCoE) Administrative Data Headache Cohort, which at the time of the data pull included all veterans with at least 1 outpatient visit in the VHA for a headache diagnosis from FY 2008–2019. We selected FY 2008 to coincide with establishment of national TBI screening in VHA. A validated algorithm which was previously used to identify veterans with specific conditions was adapted to identify veterans with headache disorders diagnosed with an International Classification of Diseases Clinical Modification (ICD-CM) code by a VHA health care provider from electronic VHA clinical and administrative data sources.20 The prior algorithm required 2 outpatient visits or 1 inpatient visit within 18 months with identical ICD codes for inclusion in the cohort. In our preliminary data, we found that many patients with at least 1 migraine code received a variety of headache codes, including multiple types of migraine codes and headache not otherwise specified (NOS). For this reason, we adapted the algorithm by reducing the requirement to only a single outpatient encounter with a migraine diagnosis for inclusion into the cohort. We also removed inpatient headache diagnoses from the algorithm as chart review for veterans with only inpatient visits for headache revealed they were time-limited headaches associated with a medical condition, rather than a primary headache disorder such as migraine. Entry into the cohort occurred on the date of the first encounter with a coded headache disorder within the study period (FY 2008–2019).
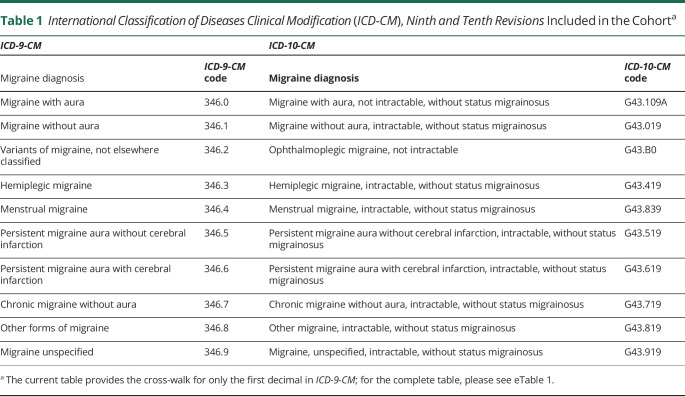
As the sampling time frame included both ICD-CM-9 and ICD-CM-109 and 10, a group of 4 neurologists board-certified in headache medicine independently reviewed a Centers for Medicare and Medicaid Services (CMS) General Equivalence Mapping post-traumatic linking ICD-9-CM headache codes to the ICD-10-CM codes and then reached consensus on all headache diagnoses (Table 1; eTable 1, links.lww.com/WNL/C328). For this study, we included only patients with a health care provider's diagnosis of migraine. In a preliminary chart review study designed to validate migraine diagnostic codes in the VHA electronic health record, 343 charts of veterans with ICD-CM migraine codes in FY 2017 were abstracted by an independent external peer review process team including registered nurses, registered health information administrators, and registered health information technicians.21 In comparing their independent clinical impression to the ICD-CM diagnostic code, the overwhelming majority (330/343, 96.2%) had a definite clinical impression of migraine, and less than 1% (3/343) of the charts with coded migraine had a definite clinical impression of a diagnosis other than migraine, providing evidence for the validity of the use of ICD-CM codes (Table 1) for identifying migraine in the VHA.
Table 1.
International Classification of Diseases Clinical Modification (ICD-CM), Ninth and Tenth Revisions Included in the Cohorta
To permit calculation of annual incidence and 1-year period prevalence, age and gender were obtained from administrative data for the entire VHA population during the study period (FY 2008–2019).
Measures
Demographics
Age (evaluated both continuously and as an ordinal variable in 5-year increments), gender (assessed as a dichotomous social construct, men/women) race (American Indian or Alaska Native, Asia, Black or African American, Native Hawaiian or Other Pacific Islander, White, or Unknown), and ethnicity (Spanish, Hispanic, Latino) assessed using self-report on enrollment or update in the health care system, smoking status (never smoker, former smoker, current smoker, unknown), first military campaign (World War II, Korean conflict, Vietnam War era, Gulf War, Operation Enduring Freedom/Operation Iraqi Freedom/Operation New Dawn [OEF/OIF/OND]), marital status (single/never married, married, separated/divorced, widowed), and geographic region (highly rural: < 7 residents per square mile; rural: any other nonurban location; urban: ≥ 50,000 people in the urban nucleus, and an urban core with ≥1,000 residents per square mile)22 were extracted at the date of entry into the cohort. Military exposure factors (traumatic brain injury [TBI] and military sexual trauma [MST]) were extracted from routinely administered patient-reported measures using validated algorithms.15-19 TBI includes TBIs incurred before and after active-duty service. The VHA definition of military sexual trauma includes both sexual harassment and sexual assault.
Comorbid Diagnoses
Body mass index (BMI) was derived from weight extracted from the measurement taken closest to entry in the cohort (range: −12 months to +6 months from date of cohort entry) and height from the median of all readings from the central VHA database. Other headache diagnoses were extracted from the entire study period (FY 2008–2019). Select medical and psychiatric comorbidities were also extracted from VHA administrative data sources using previously validated algorithms,20,23-26 including vascular and cardiovascular diseases, pain disorders, mental health disorders, substance-related/addictive disorders, sleep-wake disorders, neurologic diseases, pulmonary diseases, infection, rheumatologic diseases, and for women only, gynecologic diagnoses. Comorbidities required at least 1 inpatient or 2 outpatient codes within 18 months (12 months before, 6 months after) of date of entry into the cohort. Only comorbidities that represented at least 1.0% of the total population of veterans with diagnosed migraine were displayed in table.
Health Care Utilization
VHA health care utilization was captured for all outpatient headache visits. Commonly used clinics were described alone and in the most common combinations. In the VHA, women commonly received primary care services in women's clinic; therefore, the primary care and women's clinic care settings were collapsed for these analyses.
Analysis
Annual incidence and 1-year period prevalence were calculated in the total sample and in men and women across 5-year age increments. For these analyses, annual incidence is defined as the first migraine diagnosis coded in a clinic during the cohort period. One-year period prevalence is defined as the number of veterans coded with a migraine diagnosis with at least 1 clinic visit for migraine within the specific FY divided by the total VHA population, to be consistent with the 1-year period prevalence definition commonly reported in the migraine literature.1,2 All other study variables were described in all veterans with diagnosed migraine and in men and women with diagnosed migraine. Categorical variables are displayed using frequency and percentage, while continuous variables are displayed using means (standard deviation [SD]). Differences between women and men were evaluated using the χ2 test for categorical variables and the Student t test or the Wilcoxon rank-sum test for continuous variables. All analyses were two-tailed with alpha set at 0.05 and were performed using SAS, version 9.4 (Cary, NC). Consistent with previous cohort studies,24 we consider results clinically relevant reflect at least 2% absolute difference or a 2-fold difference in overall proportions for proportions or follow Cohen conventions of d ≥ 0.20.
Data Availability
Owing to VA regulations and our ethics agreements, the analytic data sets used for this study are not permitted to leave the VA firewall without a Data Use Agreement. However, VA data are made freely available to researchers with an approved VA study protocol. For more information, please visit virec.research.va.gov or contact the VA Information Resources Center at VIReC@va.gov.
Results
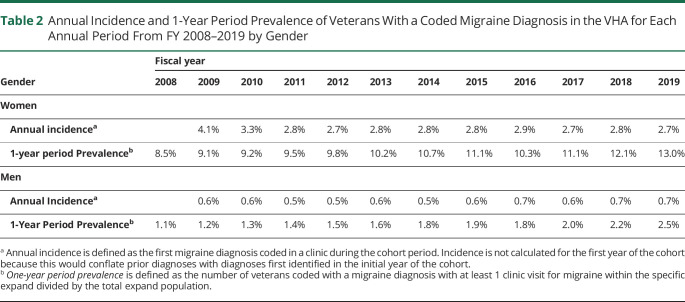
From FY 2008–2019, the VHA served 11.5 million unique veterans, of which 92.6% were men. The annual incidence of medically diagnosed migraine ranged from 2.7% to 4.1% in women and 0.6%–0.7% in men (Table 2). The 1-year period prevalence of medically diagnosed migraine, taking each FY as a distinct period (e.g., not summing prevalence across years), ranged from 8.5% to 13.0% for women and 1.1%–2.5% for men. Across the study period, the 12-year period prevalence of medically diagnosed migraine was 5.3%, including 19.6% of women, and 4.1% of men served in the VHA.
Table 2.
Annual Incidence and 1-Year Period Prevalence of Veterans With a Coded Migraine Diagnosis in the VHA for Each Annual Period From FY 2008–2019 by Gender
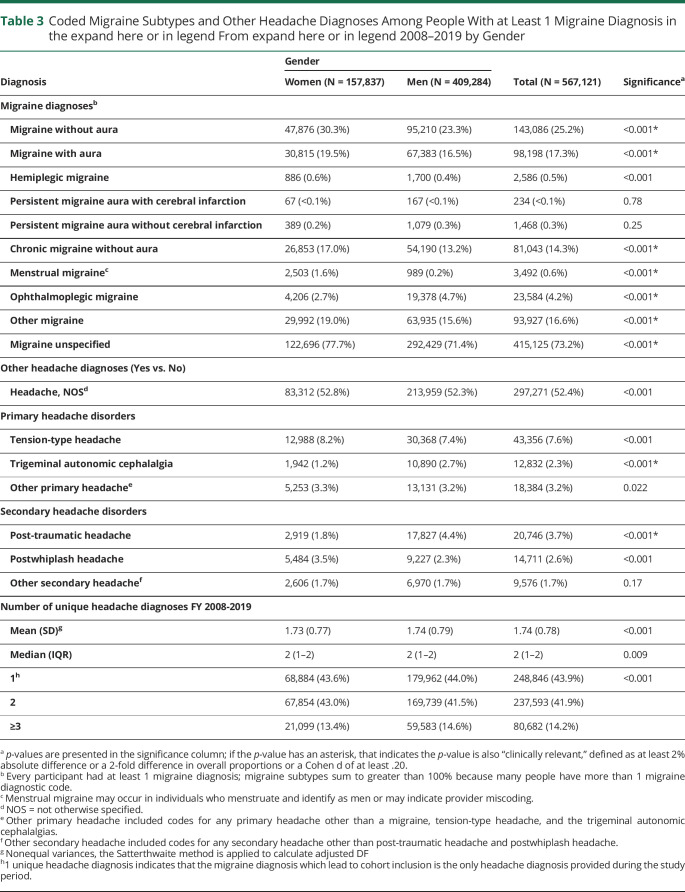
The remainder of the results will focus on the sample with medically diagnosed migraine during the study period. More than half (56.1%) of veterans with diagnosed migraine received more than 1 coded headache diagnosis within the study period (Table 3). After “migraine, unspecified,” (73.2%) the next most frequently assigned headache diagnosis among veterans with diagnosed migraine was headache NOS (52.4%; Table 3). Almost three-quarters of veterans with diagnosed migraine were coded as “migraine, unspecified” at least once during the study period; a higher proportion of women with diagnosed migraine received “migraine, unspecified” compared with men (77.7% vs 71.4%, p < 0.001; Table 3). Among those with any migraine diagnosis, higher proportions of women (vs. men) were coded as migraine without aura (30.3% vs 23.3%, p < 0.001), migraine with aura (19.5% vs 16.5%, p < 0.001), and chronic migraine without aura (17.0% vs 13.2%, p < 0.001; Table 3). Compared with men, smaller proportions of women with diagnosed migraine had a coded diagnosis of sleep-related headache during the study period (1.8% vs 4.4%, p < 0.001; Table 3).
Table 3.
Coded Migraine Subtypes and Other Headache Diagnoses Among People With at Least 1 Migraine Diagnosis in the expand here or in legend From expand here or in legend 2008–2019 by Gender
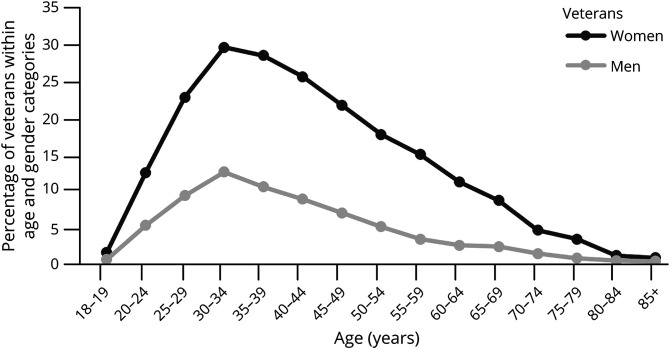
Demographics
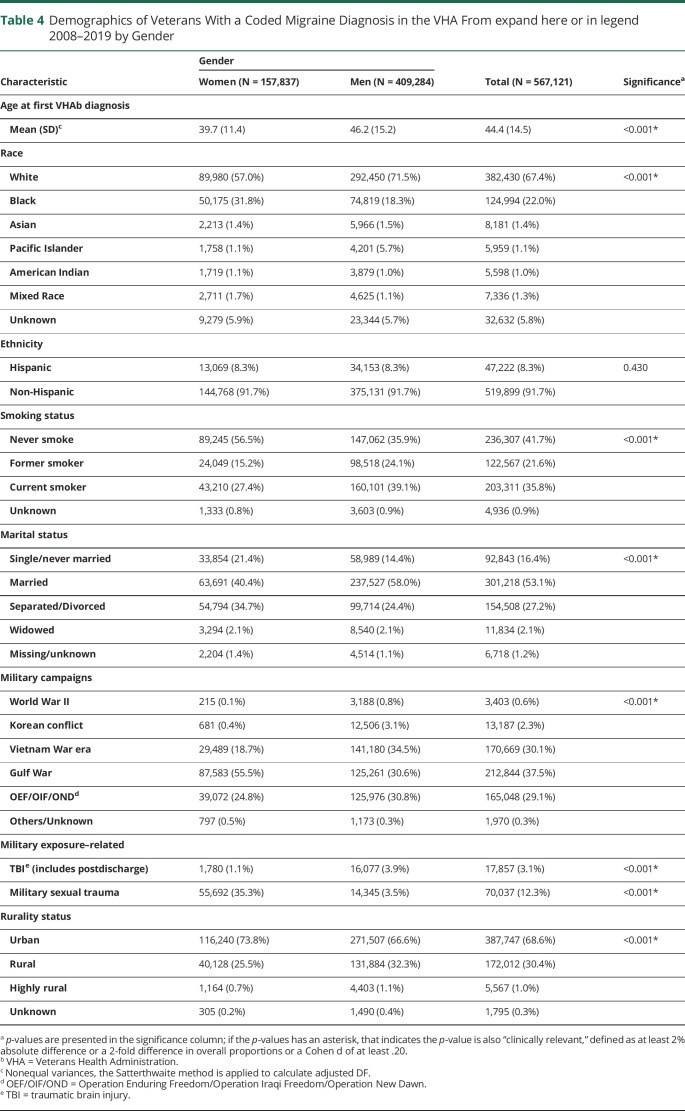
Both women and men have a steady increase in coded migraine between the ages of 20 and 34 years and a steady decline through the 60s (Figure 1). The incline is steeper for women, rising from 12.6% in the 20–24 age bracket and peaking at 29.8% in the 30–34 age bracket, whereas men rise from a prevalence of 5.4% in the 20–24 age bracket to 12.7% in the 30–34 age bracket. Among all veterans diagnosed with migraine, women were younger than men (Table 4). For both women and men with diagnosed migraine, more than half did not identify as Hispanic ethnicity; however, a larger proportion of women (vs men) with diagnosed migraine identified as Black (31.8% vs 18.3%, p < 0.001), whereas a smaller proportion of women (vs. men) with diagnosed migraine identified as White (57.0% vs 71.5%, p < 0.001; Table 4). Among veterans with diagnosed migraine, a lower proportion of women were married relative to men (40.4% vs 58.0% p < 0.001; Table 4).
Figure 1. Percentage of Veterans With Migraine of the Total expand Population Stratified by Gender and 5-Year Age Intervals.
Table 4.
Demographics of Veterans With a Coded Migraine Diagnosis in the VHA From expand here or in legend 2008–2019 by Gender
A smaller proportion of women (vs. men) with diagnosed migraine were current smokers (27.4% vs 39.1%; p < 0.001) or former smokers (15.2% vs 24.1%; p < 0.001; Table 4). A larger proportion of women (vs men) with diagnosed migraine had served during the Gulf War era (55.5% vs 30.6%; p < 0.001), whereas a smaller proportion of women (vs. men) had served during OEF/OIF/OND (24.8% vs 30.8%; p < 0.001; Table 4). A larger proportion of men (vs. women) with diagnosed migraine had TBI (3.9% vs 1.1%, p < 0.001; Table 4). More than a third of women with diagnosed migraine reported military sexual trauma (35.5%) compared with 3.5% of men (p < 0.001; Table 4). Most veterans with diagnosed migraine live in urban regions; a greater proportion of women than men live in urban regions (73.8% vs 66.6%, p < 0.001; Table 4).
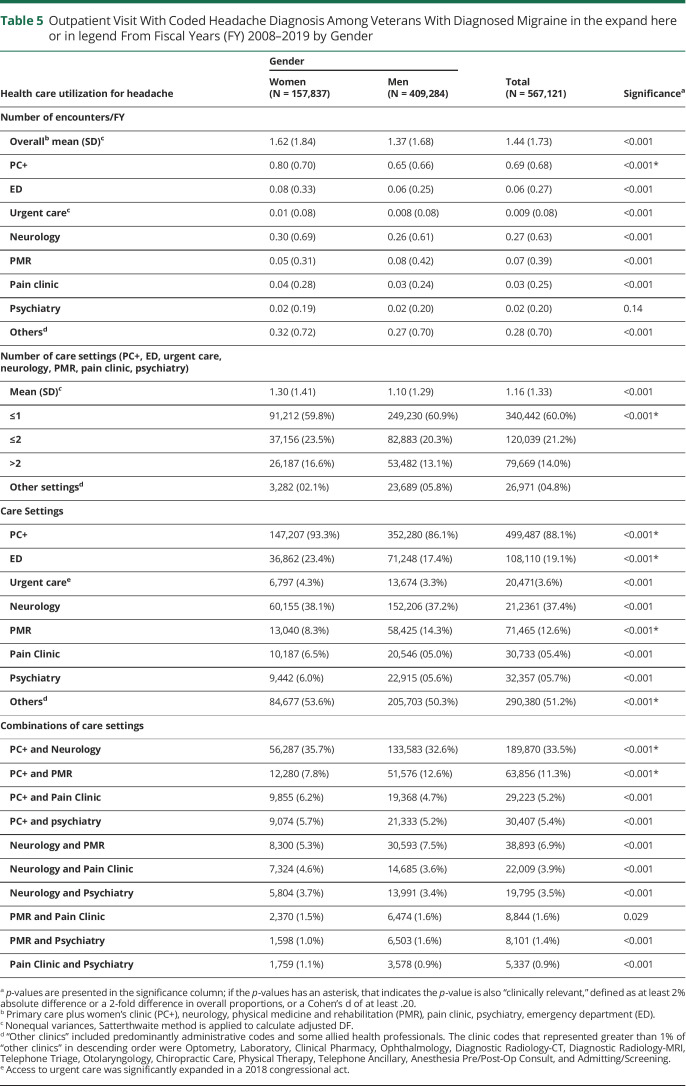
Patterns of Health Care Use for Migraine
On average, veterans with diagnosed migraine had 1.44 encounters for headache annually (standard deviation [SD] = 1.73; Table 5). Veterans with diagnosed migraine were seen in specialty care clinics (neurology, physical medicine and rehabilitation [PMR], pain clinic, physiatry) for headache infrequently and primary care more frequently (Table 5). Roughly 60% of veterans with medically diagnosed migraine were seen in only 1 care setting for headache, whereas a substantial minority (19.8%) were seen in 2 or more care settings. By far, primary care was the most common headache care setting for veterans with migraine; 93.3% of women and 86.1% of men veterans with migraine were treated for headache in primary care at least once (Table 5). Neurology was the next most common headache care setting (37.4%). Primary care + neurology was the most common care combination among both men (32.6%) and women (35.7%; p < 0.001) with diagnosed migraine, followed by primary care + PMR (12.6% of men and 7.8% of women, p < 0.001; Table 5). One-fifth of veterans with diagnosed migraine sought headache care in the ED at least once during the study period, with a higher proportion of women (23.4%) compared with men (17.4%, p < 0.001; Table 5).
Table 5.
Outpatient Visit With Coded Headache Diagnosis Among Veterans With Diagnosed Migraine in the expand here or in legend From Fiscal Years (FY) 2008–2019 by Gender
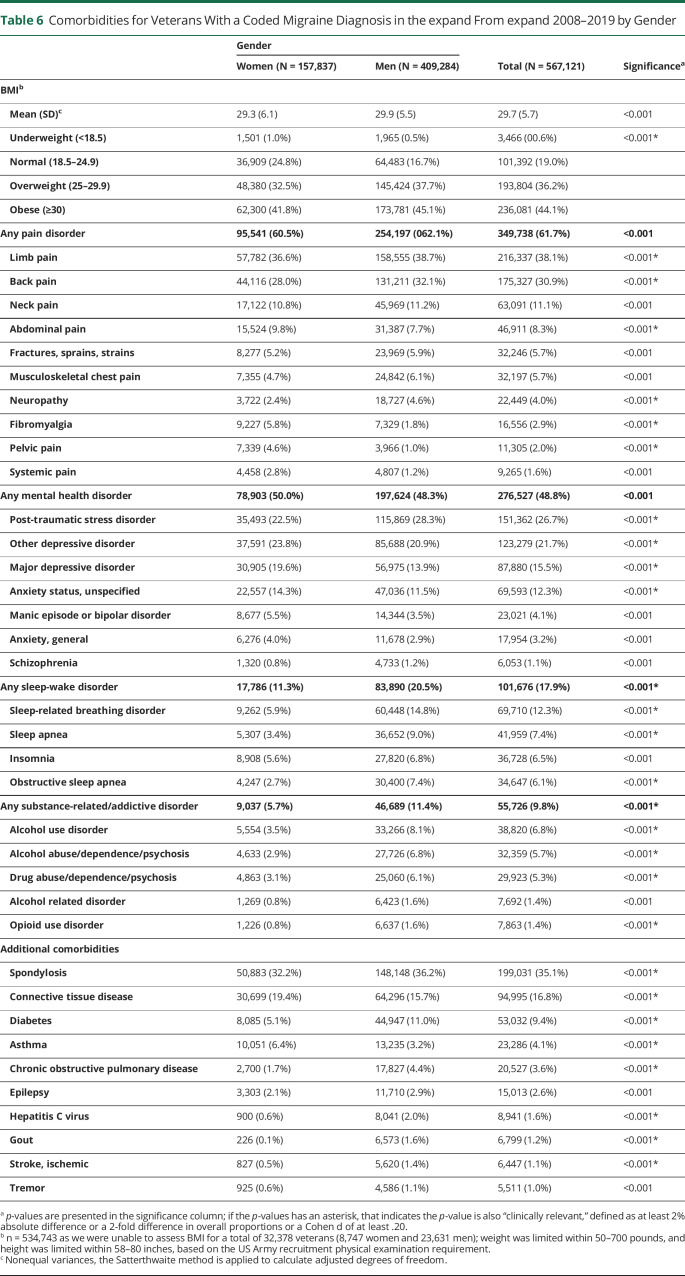
Concomitant Disorders
Most veterans with diagnosed migraine were either overweight or obese based on BMI (80.3%); on average, women had lower BMI than men (p < 0.001, Table 6).
Table 6.
Comorbidities for Veterans With a Coded Migraine Diagnosis in the expand From expand 2008–2019 by Gender
Most veterans with diagnosed migraine were also diagnosed with another, nonheadache pain disorder (61.7%; Table 6). Limb (38.1%) and back pain (30.9%) were the most common pain comorbidities and were more common in men than women (Table 6). Neuropathy was also more commonly diagnosed in men with migraine 4.6% than women (2.4%, p < 0.001; Table 6). Among women with diagnosed migraine, fibromyalgia (5.8% vs 1.8%), pelvic pain (4.6% vs 1.0%), and abdominal pain (9.8% vs 7.7%) were more common than among men (Table 6).
Approximately half of veterans with diagnosed migraine were also diagnosed with a mental health disorder (48.8%, Table 6). More than a quarter of veterans with diagnosed migraine were also diagnosed with sleep-related stress disorder (with a higher proportion of men [28.3%] vs women [22.5%], p < 0.001; Table 6). More than a fifth were diagnosed with a depressive disorder (with a higher proportion of women than men across depressive disorder diagnoses; Table 6). Bipolar disorder was diagnosed in 5.5% of women with diagnosed migraine and 3.5% of men (p < 0.001, Table 6).
One-fifth of men veterans with diagnosed migraine also had a sleep-wake disorder diagnosis, a rate almost double that of women (20.5% vs 11.3%, p < 0.001; Table 6). Sleep-related breathing disorder, sleep apnea, and obstructive sleep apnea accounted for most of these diagnoses in men (Table 6). Men with diagnosed migraine also had double the rate of substance-related/addictive disorders compared with women (11.4% vs 5.7%, p < 0.001; Table 6). Alcohol disorders accounted for most of these diagnoses. A small proportion of both men and women veterans with migraine had a diagnosis of opioid use disorder (1.6% vs 0.8%, p < 0.001; Table 6).
Among the additional comorbidities commonly diagnosed in veterans with diagnosed migraine, the most common were spondylosis (35.1%) and connective tissue disease (16.8%; Table 6). Other neurologic conditions (epilepsy, ischemic stroke, and tremor) were codiagnosed in a larger proportion of men than women veterans with migraine (Table 6). Among the 157,837 women veterans (vs. the 409,284 men) with diagnosed migraine, the most common gynecologic diagnoses during the study period were menstrual disorder (n = 1,783, 6.1%), menopausal disorder (n = 4.845, 3.1%), fibroids (n = 2,564, 1.6%), endometriosis (n = 1,827, 1.2%), ovarian cyst (n = 1,783, 1.1%), and polycystic ovarian syndrome (n = 1,426, 0.9%); among the 409,284 men, less than 0.1% were also diagnosed with gynecologic disorders (menstrual disorder n = 24; menopausal disorder n = 25; fibroids n = 7; endometriosis n = 4; ovarian cyst = 12; polycystic ovarian syndrome n = 7).
Discussion
This article describes the prevalence, characteristics, health care utilization patterns, and concomitant conditions in the 567,121 veterans diagnosed with migraine in the VHA from FY 2008–2019, which represents 5.3% of veterans served by the VHA during that period. Veterans receiving care for migraine in the VHA have high levels of concomitant conditions, particularly nonheadache pain disorders, mental health disorders, and sleep disorders, all of which have been previously associated with migraine.27,28 This system-wide approach identified important patterns in diagnosis and treatment that can guide the VHA in improving care quality.
Although more than half a million people in the VHA had medically diagnosed migraine, underascertainment of migraine is almost certainly an issue. In 2019, only 13.0% of women and 2.5% of men received a medical diagnosis of migraine in the VHA, which is lower than the rates we would expect simply based on 1-year period prevalence of migraine in the general United States population (17.1% in women and 5.6% in men).1 This is consistent with underascertainment of migraine in other systems29; for example, in the Henry Ford Health System in 2001, only half of patients who reported current migraine on a validated computer-assisted telephone diagnostic interview had a diagnosis of migraine in their chart.30 In this study, annual incidence of medically diagnosed migraine was stable across years evaluated, suggesting that migraine underascertainment is a persistent systems-level challenge. One-year period prevalence slightly improved over time, which may indicate increased access to care corresponding to the roll-out of the congressionally mandated VHA Headache Centers of Excellence initiative.
A specific diagnosis is the first step to effective care. A striking 73.2% of veterans with diagnosed migraine received a code of “migraine, unspecified”, and more than half received a code of headache not otherwise specified, at least once during the study period. Lack of diagnostic specificity extended beyond headache disorders: We also observed higher rates nonspecific vs specific psychiatric diagnoses (i.e., “other depressive disorder” vs “major depressive disorder”). Electronic health record systems create subtle disincentives to high specificity coding by inadvertently requiring greater time, effort, and knowledge to assign a specific diagnosis compared with unspecified diagnoses.31 Healthcare provider time is a limited resource. VHA clinicians, who carry most of the burden in coding visits, are generally not reimbursed on the basis of relative value units, and their compensation is not affected by diagnostic complexity, so expediency in ICD coding likely takes precedence over providing the most accurate ICD code. Among veterans with migraine, women received specific diagnoses (e.g., migraine with aura, migraine without aura, chronic migraine) more commonly than men. Higher diagnostic rates may reflect a gender difference in pain processing or communication about headache features or a higher propensity to diagnose headache in women than men among providers.32
Women veterans with diagnosed migraine sought/received more headache-related care than men with migraine, presenting more frequently than men in every clinic type except physical medicine and rehabilitation (which handles most of the TBI screening in the VHA, potentially explaining this finding). Overall, ED utilization was high among veterans with diagnosed migraine, with more than one-fifth of veterans presenting for migraine care in the ED at least once during the study period, compared with estimates outside the VHA where approximately 6% of people with migraine use the ED for headache.33
We observed a rate of TBI among veterans with migraine greater than the overall rates seen in the VHA. Between 2000 and 2019, approximating 1.6% of veterans using VHA services had a TBI.34 The relative risk of TBI for men:women is approximately 2:1 in veterans screened for TBI,35 which is less than the >3:1 ratio depicted in our study. Among the 1 million service members screened for TBI after deployment to OIF/OEF from 2007 to 2015, the rate of TBI was 8.4%, reflecting a higher risk overall in this combat-exposed population than the overall VA population.36 The TBI rates in each of these studies are highly dependent on the population of interest. In a population inclusive of all veterans in VHA regardless of combat exposure, the rate of TBI would be expected to be lower than in a cohort of persons exposed to combat with a high risk of trauma. That our rates are higher than predicted if migraine and TBI sorted independently suggests that migraine and TBI are at least associated conditions, possibly more so in male participants with greater exposure to combat conditions.
More than one-third of women veterans with diagnosed migraine had a history of military sexual trauma (including both harassment and assault), which is comparable with the VHA population.37 Although this number is 10 times higher than men veterans with diagnosed migraine, it is notable that more than 14000 men also reported experiencing military sexual trauma. In fact, this is almost twice the rate of military sexual trauma reported by men veterans seeking care in the VHA in other studies.37 Given the stigmatized nature of military sexual trauma, these figures are likely underestimates; self-report and interview methodology consistently find higher rates of military sexual trauma than administrative data sources.37 Previous research has shown that childhood adverse events, including sexual abuse, are common in migraine and associated with higher migraine symptoms.18,19 VHA providers should be aware of the likelihood many of their patients with migraine experienced military sexual trauma and develop proactive strategies to cultivate a safe environment to optimize migraine care for both women and men with a history of military sexual trauma.
The profiles of concomitant diagnoses in veterans with diagnosed migraine in the VHA provided ample opportunities for improving migraine disease severity and quality of life through cotreatment. Eighty percent of veterans with diagnosed migraine were overweight or obese, which is slightly higher than the rates reported in the VHA primary care population.38 Overweight and obesity are associated with higher migraine symptom severity, disability, and risk of progression.39 More than 60% of veterans with diagnosed migraine also had at least 1 nonheadache pain disorder diagnosis, consistent with the high rates of musculoskeletal pain disorders in the VHA24 and the known migraine comorbidities of low back pain and fibromyalgia.40 Co-occurring pain disorders (particularly multiple pain disorders) and their treatments (especially opioids) may exacerbate and make migraine symptoms more treatment-refractory.41 Almost half of veterans with diagnosed migraine also had at least 1 diagnosed mental health disorder, which is higher than rates observed in VHA primary care.42 Differences between genders were small in magnitude, indicating that a large proportion of both men and women veterans are managing migraine while at the same time managing at least 1 mental health disorder. Sleep disorders, most commonly sleep-related breathing disorders and apnea, were diagnosed in almost one-fifth of veterans with diagnosed migraine and more commonly in men. The association between migraine and sleep disorders outside the VHA has been well-documented.43 Interestingly, sleep disorders are somewhat higher in the VHA than in the general US population, and rates observed among veterans with migraine were consistent with overall trends in the VHA.44
These results are limited to veterans presenting for care in the US VHA and may not generalize to other health systems, particularly because men are over-represented in the VHA. However, this also provides us with a unique opportunity to evaluate gender differences in migraine and to characterize migraine diagnosis and treatment patterns in men, who are typically underrepresented in migraine research.
This study used administrative data; therefore, questions were limited to those that can be answered by using structured data routinely gathered in the treatment of people with migraine in the VHA. Administrative data have greater risk of errors and lack of specificity compared with data collected specifically for research. For example, we described rates of comorbidities in veterans with diagnosed migraine; however, these rates are likely higher than those we would observe in the entire population of veterans with both diagnosed and undiagnosed migraine because they reflect care-seeking in addition to a migraine diagnosis. Similarly, gender is coded with 2 categories, rather than the broader array of categories that more accurately capture the social construct of gender. In addition, incidence is defined as the first diagnosis of migraine within the study period, rather than the first occurrence of the disease in each veteran. Prior research has demonstrated that a diagnosis of migraine is frequently delayed by more than 5 years.45 Furthermore, the VHA only cares for veterans after they have concluded their military service, limiting our ability to capture migraine onset that occurred earlier in life. However, administrative data are ideal to evaluate patterns, such as underascertainment or lack of specificity in diagnosis, crucial to help health systems improve care quality, and to help future researchers understand the limitations of these administrative data.
These data demonstrate promise of the VHA Headache Cohort and other VHA data sources to evaluate migraine in men, a traditionally underrepresented group in migraine research.
Future research should attempt to quantify underascertainment of migraine in the VHA and identify patient characteristics (such as gender and comorbidities) and systems-level characteristics (such as care setting and provider type) associated with nondiagnosis of migraine to inform system-level interventions to improve diagnosis, particularly for those in need of medical care.6,11 Rurality in particular should be evaluated as a potential determinant of underascertainment of migraine because challenges with accessing care in rural geographic settings may limit the opportunity for a patient to bring up migraine symptoms and receive a diagnosis. Natural language processing and machine learning techniques could further mine the electronic health record for clinical information included in unstructured data including diagnostic codes, migraine symptom severity, and migraine-related disability. Provider education and informatics solutions should be developed to encourage specificity of migraine diagnosis in the VHA.
Future research should use a control group of veterans receiving care in the VHA without a headache disorder diagnosis matched on age, gender, race, and treatment location, specifically to evaluate migraine risk factors this study suggests the VHA is well-positioned to answer, such as diagnoses that occur commonly in men (e.g., obstructive sleep apnea) and among individuals who serve in the armed forces (e.g., TBI). A matched control could also permit evaluation of questions related to the burden of migraine, such as by evaluating differences in overall health care utilization between people with and without migraine.
Deep phenotyping among veterans with TBI who present with and without headache and migraine symptoms, particularly from the OEF/OIF/OND era, should be used to understand how TBI-related headache presents over the long term and to untangle diagnostic issues related to post-traumatic headache and migraine. Future research should identify characteristics associated with ED utilization for migraine in the VHA and develop strategies to streamline effective care in other primary and tertiary care ambulatory clinics within the VHA.
Future studies should capitalize on the large integrated care setting of the VHA to evaluate stepped care and cotreatment strategies to manage migraine and its comorbidities. Effective weight loss interventions and physical activity interventions may reduce migraine symptom severity and disability.46 Because migraine and chronic nonmigraine pain conditions may have shared mechanisms of pain sensitization and altered psychological processing of pain,47 combined treatment of migraine and concurrent pain conditions is advisable. Effective migraine treatment can improve psychiatric symptoms,48 but likely the most effective approach is to address symptoms concomitantly. Sleep in particular may have an important relationship with migraine,42,43,49 interventions to improve both sleep and migraine show promise,50 and the VHA demonstrated a commitment to system-wide implementation of evidence-based sleep interventions.44
Acknowledgment
The views expressed in this article are those of the authors and do not necessarily represent the view of the Department of Veterans Affairs. We would like to acknowledge the contributions of the staff of the Headache Centers of Excellence Research and Evaluation Center, including Nancy Lorenze, Robin Einbinder, Hayley Lindsey, and Addison Kimber.
Glossary
- VHA
Veteran's Health Administration
Appendix. Authors
Footnotes
Editorial, page 779
Study Funding
This study was funded by Veterans Health Administration Headache Centers of Excellence. Dr. Seng is a career-award recipient of NINDS (NS096107 PI: Seng).
Disclosure
E.K. Seng has consulted for GlaxoSmithKline and Click Therapeutics and received research funding from the NINDS (NS096107 PI: Seng) and NCCIH (AT011005 mPI: Seng). R.B. Lipton has received research support from the National Institutes of Health, the FDA, and the National Headache Foundation; he serves as consultant, advisory board member, or has received honoraria or research support from AbbVie/Allergan, Amgen, Biohaven, Dr. Reddy's Laboratories (Promius), electroCore, Eli Lilly, GlaxoSmithKline, Lilly, Lundbeck, Merck, Novartis, Teva, Vector, and Vedanta Research; he receives royalties from Wolff's Headache, 8th edition (Oxford University Press, 2009), and Informa; he holds stock/options in Biohaven and CntrlM. The other authors report no relevant disclosures. Go to Neurology.org/N for full disclosures.
References
- 1.Lipton R, Bigal M, Diamond M, Freitag F, Reed M, Stewart W. Migraine prevalence, disease burden, and the need for preventive therapy. Neurology. 2007;68:343-349. [DOI] [PubMed] [Google Scholar]
- 2.Burch R, Rizzoli P, Loder E. The prevalence and impact of migraine and severe headache in the United States: updated age, sex, and socioeconomic-specific estimates from government health surveys. Headache. 2021;61(1):60-68. [DOI] [PubMed] [Google Scholar]
- 3.Vetvik KG, MacGregor EA. Sex differences in the epidemiology, clinical features, and pathophysiology of migraine. Lancet Neurol. 2017;16:76-87. [DOI] [PubMed] [Google Scholar]
- 4.Global Burden of Disease 2016 Neurology Collaborators. Global, regional, and national burden of neurological disorders, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019;18:459-480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Polson M, Williams TD, Speicher LC, Mwamburi M, Staats PS, Tenaglia AT. Concomitant medical conditions and total cost of care in patients with migraine: a real-world claims analysis. Am J Manag Care. 2020;26:S3–s7. [DOI] [PubMed] [Google Scholar]
- 6.Ashina M, Katsarava Z, Do TP, et al. Migraine: epidemiology and systems of care. Lancet. 2021;397(10283):1485-1495. [DOI] [PubMed] [Google Scholar]
- 7.Lipton RB, Cohen JM, Gandhi SK, Yang R, Yeung PP, Buse DC. Effect of fremanezumab on quality of life and productivity in patients with chronic migraine. Neurology. 2020;95:e878–e888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lombard L, Farrar M, Ye W, et al. A global real-world assessment of the impact on health-related quality of life and work productivity of migraine in patients with insufficient versus good response to triptan medication. J Headache Pain. 2020;21:41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Talbot J, Stuckey R, Crawford L, Weatherby S, Mullin S. Improvements in pain, medication use and quality of life in onabotulinumtoxinA-resistant chronic migraine patients following erenumab treatment - real world outcomes. J Headache Pain 2021;22:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Veterans Health Administration [online]. Available at: va.gov/health/. Accessed December 21, 2021.
- 11.Buse DC, Armand CE, Charleston4th L, et al. Barriers to care in episodic and chronic migraine: results from the chronic migraine epidemiology and outcomes study. Headache. 2021;61(4):628-641. [DOI] [PubMed] [Google Scholar]
- 12.Lipton RB, Serrano D, Holland S, Fanning KM, Reed ML, Buse DC. Barriers to the diagnosis and treatment of migraine: effects of sex, income, and headache features. Headache. 2013;53:81-92. [DOI] [PubMed] [Google Scholar]
- 13.DePalma RG, Hoffman SW. Combat blast related traumatic brain injury (TBI): decade of recognition; promise of progress. Behav Brain Res. 2018;340:102-105. [DOI] [PubMed] [Google Scholar]
- 14.Lofgreen AM, Carroll KK, Dugan SA, Karnik NS. An overview of sexual trauma in the U.S. Military. Focus (Am Psychiatr Publ). 2017;15:411-419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ashina H, Iljazi A, Amin FM, Ashina M, Lipton RB, Schytz HW. Interrelations between migraine-like headache and persistent post-traumatic headache attributed to mild traumatic brain injury: a prospective diary study. J Headache Pain. 2020;21:134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Scher AI, McGinley JS, Wirth RJ, et al. Headache complexity (number of symptom features) differentiates post-traumatic from non-traumatic headaches. Cephalalgia. 2021;41(5):582-592. [DOI] [PubMed] [Google Scholar]
- 17.Bailie JM, Kennedy JE, French LM, et al. Profile Analysis of the neurobehavioral and psychiatric symptoms following combat-related mild traumatic brain injury: identification of subtypes. J Head Trauma Rehabil. 2016;31(1):2-12. [DOI] [PubMed] [Google Scholar]
- 18.Tietjen GE, Peterlin BL. Childhood abuse and migraine: epidemiology, sex differences, and potential mechanisms. Headache. 2011;51:869-879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tietjen GE, Buse DC, Fanning KM, Serrano D, Reed ML, Lipton RB. Recalled maltreatment, migraine, and tension-type headache: results of the AMPP study. Neurology. 2015;84:132-140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Justice AC, Dombrowski E, Conigliaro J. Veterans aging cohort study (VACS): overview and description. Med Care. 2006;44:S13-24k. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sico JJ, Kuruvilla D, Sites A, et al. Electronic health record documentation of headache presentation: argument for improvement in an integrated healthcare system in order to better treatment. Headache. 2020;60(S1):66. [Google Scholar]
- 22.US Department of Veterans Affairs Office of Health Equity. National Veteran Health Equity Report—Fy2013: US Department of Veterans Affairs; 2016. [Google Scholar]
- 23.Fultz SL, Skanderson M, Mole LA, et al. Development and verification of a "virtual" cohort using the national VA health information system. Med Care. 2006;44:S25-S30. [DOI] [PubMed] [Google Scholar]
- 24.Goulet JL, Kerns RD, Bair M, et al. The musculoskeletal diagnosis cohort: examining pain and pain care among veterans. Pain. 2016;157:1696-1703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mayhew M, DeBar LL, Deyo RA, et al. Development and assessment of a crosswalk between ICD-9-CM and ICD-10-CM to identify patients with common pain conditions. J Pain. 2019;20:1429-1445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Haskell SG, Brandt CA, Krebs EE, Skanderson M, Kerns RD, Goulet JL. Pain among veterans of operations enduring freedom and Iraqi freedom: do women and men differ? Pain Med. 2009;10:1167-1173. [DOI] [PubMed] [Google Scholar]
- 27.Buse DC, Reed ML, Fanning KM, Bostic RC, Lipton RB. Demographics, headache features, and comorbidity profiles in relation to headache frequency in people with migraine: results of the american migraine prevalence and prevention (AMPP) Study. Headache; 2020. doi: 10.111/head.13966. [DOI] [PubMed] [Google Scholar]
- 28.Lipton RB, Fanning KM, Buse DC, et al. Identifying natural subgroups of migraine based on comorbidity and concomitant condition profiles: results of the chronic migraine epidemiology and outcomes (CaMEO) study. Headache. 2018;58(7):933-947. [DOI] [PubMed] [Google Scholar]
- 29.Pressman AR, Buse DC, Jacobson AS, et al. The migraine signature study: methods and baseline results. Headache. 2021;61:462-484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kolodner K, Lipton RB, Lafata JE, et al. Pharmacy and medical claims data identified migraine sufferers with high specificity but modest sensitivity. J Clin Epidemiol. 2004;57:962-972. [DOI] [PubMed] [Google Scholar]
- 31.Graber ML, Byrne C, Johnston D. The impact of electronic health records on diagnosis. Diagnosis (Berl). 2017;4:211-223. [DOI] [PubMed] [Google Scholar]
- 32.Mogil JS. Qualitative sex differences in pain processing: emerging evidence of a biased literature. Nat Rev Neurosci. 2020;21(7):353-365. [DOI] [PubMed] [Google Scholar]
- 33.Friedman BW, Serrano D, Reed M, Diamond M, Lipton RB. Use of the emergency department for severe headache. A population-based study. Headache. 2009;49:21-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Veterans Health Administration Office of Research, Development. VA Research on Traumatic Brain Injury (TBI); 2022. [online]. research.va.gov/topics/tbi.cfm. [Google Scholar]
- 35.Whiteneck GG, Cuthbert JP, Mellick DC. VA traumatic brain injury veterans health registry report. 2015. [online]. publichealth.va.gov/docs/epidemiology/TBI-report-fy2013-qtr4.pdf.
- 36.Twamley EW, Baker DG, Norman SB, Pittman JO, Lohr JB, Resnick SG. Veterans health administration vocational services for operation Iraqi freedom/operation enduring freedom veterans with mental health conditions. J Rehabil Res Dev. 2013;50(5):663-670. [DOI] [PubMed] [Google Scholar]
- 37.Wilson LC. The prevalence of military sexual trauma: a meta-analysis. Trauma Violence Abuse. 2018;19:584-597. [DOI] [PubMed] [Google Scholar]
- 38.Breland JY, Phibbs CS, Hoggatt KJ, et al. The obesity epidemic in the veterans health administration: prevalence among key populations of women and men veterans. J Gen Intern Med. 2017;32:11-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bigal ME, Liberman JN, Lipton RB. Obesity and migraine: a population study. Neurology. 2006;66:545-550. [DOI] [PubMed] [Google Scholar]
- 40.Vivekanantham A, Edwin C, Pincus T, Matharu M, Parsons H, Underwood M. The association between headache and low back pain: a systematic review. J Headache Pain. 2019;20:82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Scher AI, Buse DC, Fanning KM, et al. Comorbid pain and migraine chronicity: the chronic migraine epidemiology and outcomes study. Neurology. 2017;89:461-468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Trivedi RB, Post EP, Sun H, et al. Prevalence, comorbidity, and prognosis of mental health among US veterans. Am J Public Health 2015;105:2564-2569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Buse DC, Rains JC, Pavlovic JM, et al. Sleep disorders among people with migraine: results from the chronic migraine epidemiology and outcomes (CaMEO) study. Headache. 2019;59:32-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Folmer RL, Smith CJ, Boudreau EA, et al. Prevalence and management of sleep disorders in the veterans health administration. Sleep Med Rev. 2020;54:101358. [DOI] [PubMed] [Google Scholar]
- 45.Viticchi G, Silvestrini M, Falsetti L, et al. Time delay from onset to diagnosis of migraine. Headache. 2011;51(2):232-236. [DOI] [PubMed] [Google Scholar]
- 46.La Touche R, Fernández Pérez JJ, Proy Acosta A, et al. Is aerobic exercise helpful in patients with migraine? A systematic review and meta-analysis. Scand J Med Sci Sports. 2020;30:965-982. [DOI] [PubMed] [Google Scholar]
- 47.Simons LE, Elman I, Borsook D. Psychological processing in chronic pain: a neural systems approach. Neurosci Biobehav Rev. 2014;39:61-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Seng EK, Holroyd KA. Psychiatric comorbidity and response to preventative therapy in the treatment of severe migraine trial. Cephalalgia. 2012;32:390-400. [DOI] [PubMed] [Google Scholar]
- 49.Bertisch SM, Li W, Buettner C, et al. Nightly sleep duration, fragmentation, and quality and daily risk of migraine. Neurology. 2020;94(5):e489–e496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Smitherman TA, Kuka AJ, Calhoun AH, et al. Cognitive-behavioral therapy for insomnia to reduce chronic migraine: a sequential bayesian analysis. Headache. 2018;58(7):1052-1059. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Owing to VA regulations and our ethics agreements, the analytic data sets used for this study are not permitted to leave the VA firewall without a Data Use Agreement. However, VA data are made freely available to researchers with an approved VA study protocol. For more information, please visit virec.research.va.gov or contact the VA Information Resources Center at VIReC@va.gov.