ABSTRACT.
Snakebite is a common occurrence in Hangzhou, and identifying bacteria in wounds is very important for snakebite treatment. To define the pattern of wound bacterial flora of venomous snakebites and their susceptibility to common antibiotics, we reviewed the medical charts of patients admitted with snakebite at Hangzhou TCM Hospital from January 2019 to December 2020. A total of 311 patients were enrolled in this study. Among them, bacteria culture was positive in 40 patients, and 80 organisms were isolated. The most frequent pathogens were Morganella morganii and Staphylococcus aureus. According to the results of susceptibility testing, a majority of the isolates were resistant to some common first-line antibiotics, such as ampicillin, ampicillin/sulbactam, amoxicillin/clavulanic acid, cefoxitin, and cephazolin. Quinolones, however, have shown a better antibacterial effect. In conclusion, snakebite wounds involve a wide range of bacteria. Fluoroquinolones, such as levofloxacin and ciprofloxacin, could be an alternative for empirical treatment in patients with snakebite when the effect of other antibiotics is poor.
INTRODUCTION
Snakebite envenomation is an important worldwide health issue and was categorized as a category A neglected tropical disease by the WHO.1 Currently, there are still 5.8 billion people in the world at risk of encountering poisonous snakes, and 81,410 to 137,880 people die of venomous snakebites every year.2 In addition to the expected morbidity and mortality caused by venom alone, cases of severe envenomation are often characterized by subsequent severe local and systemic septic complications.3 Secondary bacterial infection at the site of envenomation is a major cause of infectious complications. Although the use of empirical antibiotics is effective in controlling infection, the types of antibiotics still need to be identified because bacterial compositions vary among snake species and may be influenced by environmental conditions in different geographic regions. Therefore, understanding the microbiology of snakebite wounds is important to help guide empirical antibiotic therapy before the results of antimicrobial susceptibility tests are known. To date, several studies about the bacteriology of snakebite wounds have been conducted in some areas3–7; however, bacteriology data on wound culture following a snakebite remain scarce in mainland China.
Five common venomous snake species are distributed throughout the Hangzhou area, Southeast China, including Gloydius brevicaudus, Deinagkistrodon acutus, Trimeresurus stejnegeri, Naja atra, and Bungarus multicinctus. Snakebite is a common condition and nearly 700 people are bitten by snakes every year in Hangzhou. To understand more fully the bacteriology of venomous snakebite wounds, we analyzed the wound culture data of venomous snakebites from a level A tertiary medical center in Hangzhou.
MATERIALS AND METHODS
Population.
Consecutive patients who presented with venomous snakebite to the Hangzhou TCM Hospital Affiliated to Zhejiang Chinese Medical University between January 2019 to December 2020 were enrolled. The exclusion criteria were as follows: 1) readmission with the same bite accident and 2) wound bacterial culture was not conducted while at the hospital. Data extracted from the hospital medical record system for each patient included gender, age, snake specious, bite site, local complications, and bacteria culture data. Hangzhou TCM Hospital is a level A tertiary medical center with 1,580 beds in northern Zhejiang Province, and it is also a designated hospital for snakebite treatment in the Hangzhou region.
Bacteriology.
The first wound bacterial cultures were all performed before antibiotic treatment, and multiple cultures were performed for some patients when necessary. Wound sampling methods included swabbing from superficial wound fluid and tissue debris, needle aspiration from wound fluid, and deep-tissue during surgical debridement. Both aerobic and anaerobic bacterial culture were performed for all samples. Bacteria were identified using the VITEK-2 Compact microbial identification system (bioMerieux, Marcy l’Etoile, France). The antimicrobial susceptibility test was conducted by the disk diffusion method, and the data were analyzed using WHONET software (Version 5.6).
Definitions.
A wound infection was defined as the presence of one or more of the following criteria: 1) persistent or aggravate redness, swelling, warming, and pain at the bite site; 2) purulence or inflammatory exudation at the bite site; and 3) a wound requiring incision and drainage. Local tissue necrosis was defined as the tissue surrounding bite site becoming blackened and inactivated, with or without infection. Polymicrobial infection was defined as the growth of two or more bacteria from the same wound.8
Statistical analysis.
Categorical variables were expressed as absolute and relative frequencies, and continuous values were reported as mean ± SD (normally distributed) or median with interquartile range (non-normally distributed). All data were analyzed using SPSS software (version 22.0; IBM, Armonk, NY) and R software (version 4.1.0; R Foundation for Statistical Computing, Vienna, Austria).
RESULTS
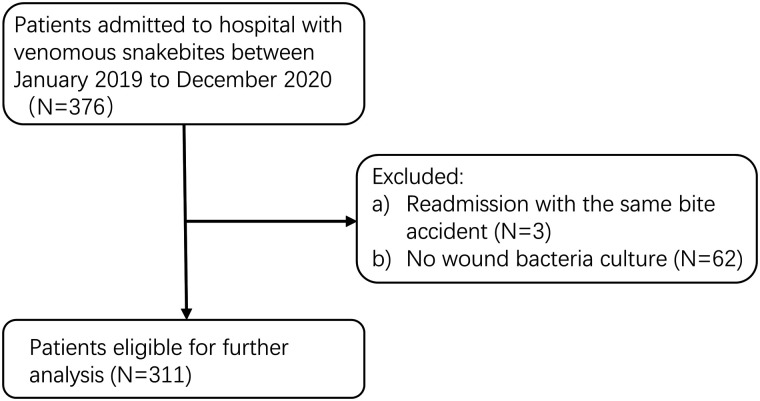
A total of 311 patients with venomous snakebites were included in this study (Figure 1). The mean ± SD age of patients was 56 ± 16 years, and 189 (60.8%) were male. One patient (0.3%) died of antivenom-induced anaphylactic shock. Of the snake species identified, the most common type of snake was G. brevicaudus (166 patients), followed by D. acutus (81 patients), T. stejnegeri (45 patients), N. atra (9 patients), and B. multicinctus (2 patients). The species of snake could not be identified in eight cases. Except for one with head envenomation, all other patients had fang marks in their extremities. The local complications, including wound infection, localized tissue necrosis, lymphangitis, and necrotizing fasciitis developed in 78 (25.1%), 71 (22.8%), 9 (2.9%), and 2 (0.6%) patients, respectively. Thirty-two patients (10.3%) finally received various types of surgery, including debridement, vacuum-sealing drainage, fasciotomy or fasciectomy, flap transplantation, skin grafting, and finger or toe amputation. All patients received empirical antibiotic treatment after admission. The median time between snakebite to the microbiological sampling was 14 hours, and deep cultures accounted for 17%. Forty patients (12.9%) had positive bacterial cultures. Repeated cultures were performed in 8 patients, and multiple organisms were isolated from the cultures of 10 patients (Table 1).
Figure 1.
Flow diagram for patient’s enrollment.
Table 1.
Baseline demographics and clinical characteristics of patients
| Variable | n (%)* |
|---|---|
| Age, years; mean ± SD | 56 ± 16 |
| Gender | |
| Male | 189 (60.8) |
| Female | 122 (39.2) |
| Bite site | |
| Head | 1 (0.3) |
| Upper limb | 158 (50.8) |
| Lower limb | 152 (48.9) |
| Surgery | 32 (10.3) |
| Positive bacterial cultures | 40 (12.9) |
| Polymicrobial | 10 (3.2) |
| Species of snake | |
| Gloydius brevicaudus | 166 (53.4) |
| Deinagkistrodon acutus | 81 (26.0) |
| Trimeresurus stejnegeri | 45 (14.5) |
| Naja atra | 9 (2.9) |
| Bungarus multicinctus | 2 (0.6) |
| Unknow | 8 (2.6) |
| Local complication | |
| Wound infection | 78 (25.1) |
| Local tissue necrosis | 71 (22.8) |
| Lymphangitis | 9 (2.9) |
| Necrotizing fasciitis | 2 (0.6) |
Unless noted otherwise.
Of the 40 positive samples, 23 (57.5%) were from deep tissue. Among the positive bacterial culture patients, 24 presented with wound infection, 20 had local tissue necrosis, 2 developed lymphangitis, and 1 was diagnosed with necrotizing fasciitis. In addition, in these patients, 19 were bitten by D. acutus, 12 by G. brevicaudus, 5 by T. stejnegeri, 2 by N. atra, and 2 by unknown species; 13 of them required surgical treatment.
Eighty organisms were identified in 40 positive samples, including 24 Gram-positive bacteria, and 56 Gram-negative bacteria. Among Gram-positive bacteria, Staphylococcus aureus (13 isolates, 16.3% of all bacterial growth and 54.2% of Gram-positive isolates) was the most common pathogen, followed by Enterococcus faecalis and coagulase-negative Staphylococcus species. Morganella morganii (13 isolates, 16.3% of all bacterial growth and 23.2% of Gram-negative isolates) was the most frequent Gram-negative isolate. Other important Gram-negative pathogens included Hydrophila/caviae aeromonas, Pseudomonas aeruginosa, Citrobacter braakii, and Escherichia coli (Table 2).
Table 2.
Bacteria isolated from the positive samples
| Organism | n |
|---|---|
| Aerobic and facultative aerobic Gram-positive bacteria | 24 |
| Bacillus species | 1 |
| Staphylococcus warneri | 2 |
| Staphylococcus epidermidis | 1 |
| Staphylococcus haemolyticus | 1 |
| Streptococcus agalactiae (B) | 1 |
| Staphylococcus aureus | 13 |
| Enterococcus faecalis (D) | 5 |
| Aerobic and facultative aerobic Gram-negative bacteria | 55 |
| Citrobacter braakii | 6 |
| Morganella morganii | 13 |
| Escherichia coli | 5 |
| Enterobacter cancerogenus | 2 |
| Pseudomonas aeruginosa | 7 |
| Klebsiella pneumoniae | 1 |
| Klebsiella oxytoca | 1 |
| Enterobacter cloacae | 2 |
| Hydrophila/caviae aeromonas | 9 |
| Acinetobacter baumannii | 3 |
| Proteus mirabilis | 3 |
| Aeromonas salmonicida | 1 |
| Sphlingomonas paucimobilis | 1 |
| Pantoea | 1 |
| Anaerobic bacteria | 1 |
| Clostridium histolyticum | 1 |
B = Lancefield group B; D = Lancefield group D.
The results of antibiotic susceptibility tests are shown in Tables 3 and 4. The levels of resistance of Gram-positive bacteria for most antibiotics were less than Gram-negative bacteria. However, the level of penicillin G resistance was greater in Gram-positive bacteria, which reached 72.7%, but no resistance to vancomycin or linezolid was observed. Among Staphylococcus species, we found 11 beta-lactamase–positive strains, including one Staphylococcus warneri and 10 S. aureus. In addition, 5 methicillin-resistant S. aureus strains were observed in 13 S. aureus samples isolated. In the Gram-negative bacteria, the drug resistance rate to cefoxitin, cephazolin, and amoxicillin/clavulanic acid was higher. In contrast, most of them were susceptible to aminoglycosides, third- or fourth-generation cephalosporins, quinolones, and carbapenems.
Table 3.
Susceptibility to common antibiotics of Gram-positive bacteria isolated from wound of snakebites
| Susceptible strains | Antibiotic, n/N | Beta-lactamase, n | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| AMP | DA | CN | CIP | LZD | P | VA | AMC | OX | LEV | ||
| Bacillus species (N = 1) | – | – | – | – | – | – | – | – | – | – | – |
| Staphylococcus warneri (N = 2) | – | 2/2 | 2/2 | 1/1 | 2/2 | 0/2 | 2/2 | – | 0/2 | 2/2 | 1* |
| Staphylococcus epidermidis (N = 1) | – | – | – | – | – | – | – | – | – | – | – |
| Staphylococcus haemolyticus (N = 1) | – | – | – | – | – | – | – | – | – | – | – |
| Streptococcus agalactiae (N = 1) | 1/1 | 1/1 | – | – | 1/1 | 1/1 | 1/1 | – | – | 1/1 | – |
| Staphylococcus aureus (N = 13) | 0/1 | 8/13 | 12/13 | 11/13 | 13/13 | 0/13 | 13/13 | 1/1 | 8/13 | 11/12 | 10* |
| Enterococcus faecalis (N = 5) | 5/5 | – | 5/5 | 5/5 | 5/5 | 5/5 | 5/5 | – | – | 5/5 | – |
| Clostridium histolyticum (N = 1) | 1/1 | 1/1 | 1/1 | 1/1 | 1/1 | 0/1 | 1/1 | 1/1 | 1/1 | – | – |
AMC = amoxycillin/clavulanic acid; AMP = ampicillin; CIP = ciprofloxacin; CN = gentamicin; DA = clindamycin; LEV = levofloxacin; LZD = linezolid; n/N = the number of sensitive strains/total number of strains; OX = oxacillin; P = penicillin G; VA = vancomycin; – = not tested.
The number of beta-lactamase production strains.
Table 4.
Susceptibility to common antibiotics of Gram-negative bacteria isolated from wounds of snakebites to common antibiotics
| Susceptible strains | Antibiotic, n/N | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| AK | AMP | CIP | TZP | CN | FEP | CRO | CAZ | CTT | FOX | KZ | IPM | LEV | AMC | TGC | |
| Citrobacter braakii (N = 6) | 6/6 | – | 6/6 | – | 6/6 | 6/6 | 6/6 | – | – | 0/6 | 0/6 | 4/6 | 6/6 | 0/6 | 6/6 |
| Morganella morganii (N = 13) | 13/13 | 0/13 | 13/13 | 13/13 | 13/13 | 13/13 | 13/13 | 9/9 | 9/9 | 0/3 | 0/13 | – | 13/13 | 0/4 | 0/4 |
| Escherichia coli (N = 5) | 5/5 | 2/5 | 5/5 | 5/5 | 5/5 | 5/5 | 4/5 | 3/3 | 3/3 | 1/2 | – | 5/5 | 5/5 | 0/2 | 2/2 |
| Enterobacter cancerogenus (N = 2) | 2/2 | – | 2/2 | 2/2 | 2/2 | 2/2 | 2/2 | – | – | 0/2 | 0/2 | 2/2 | 2/2 | 0/2 | 2/2 |
| Pseudomonas aeruginosa (N = 7) | 7/7 | 1/6 | 5/7 | 6/7 | 7/7 | 6/7 | 1/6 | 4/4 | 1/3 | 0/3 | 1/7 | 5/6 | 5/7 | 0/3 | 0/3 |
| Klebsiella oxytoca (N = 1) | 1/1 | 0/1 | 1/1 | 1/1 | 1/1 | 1/1 | 1/1 | 1/1 | 1/1 | – | 1/1 | 1/1 | 1/1 | – | – |
| Klebsiella pneumoniae (N = 1) | 1/1 | 0/1 | 1/1 | 1/1 | 1/1 | 1/1 | 1/1 | – | – | 1/1 | – | 1/1 | 1/1 | 1/1 | 1/1 |
| Enterobacter cloacae (N = 2) | 2/2 | – | 1/2 | 2/2 | 2/2 | 2/2 | 2/2 | 1/1 | 1/1 | 0/1 | 0/2 | 2/2 | 2/2 | 0/1 | 1/1 |
| Hydrophila/caviae aeromonas (N = 9) | 8/9 | – | 7/8 | 4/9 | 8/9 | 8/9 | 3/9 | 3/4 | – | 0/5 | 1/9 | 4/9 | 4/9 | 0/5 | 5/5 |
| Acinetobacter baumannii (N = 3) | – | – | 3/3 | – | 3/3 | 3/3 | 1/1 | 2/2 | – | – | 0/3 | 3/3 | 3/3 | – | 1/1 |
| Proteus mirabilis (N = 3) | 3/3 | 0/3 | 3/3 | 3/3 | 3/3 | 3/3 | 3/3 | 3/3 | 3/3 | – | 0/3 | – | 3/3 | – | – |
| Aeromonas salmonicida (N = 1) | 1/1 | – | 1/1 | 1/1 | 1/1 | 1/1 | 1/1 | 1/1 | – | – | 0/1 | 1/1 | 1/1 | – | – |
| Sphlingomonas paucimobilis (N = 1) | 1/1 | – | 1/1 | 1/1 | 1/1 | 1/1 | 1/1 | - | – | – | 1/1 | 1/1 | 1/1 | – | 1/1 |
| Pantoea (N = 1) | – | – | – | 1/1 | – | – | – | 1/1 | – | – | – | 1/1 | 1/1 | – | – |
AK = amikacin; AMC = amoxycillin/clavulanic acid; AMP = ampicillin; CAZ = ceftazidime; CIP = ciprofloxacin; CN = gentamicin; CRO = ceftriaxone; CTT = cefotetan; FEP = cefepime; FOX = cefoxitin; IPM = imipenem; KZ = cephazolin; LEV = levofloxacin; n/N = the number of sensitive strains/total number of strains; TGC = tigecycline; TZP = piperacillin/tazobactam; – = not tested.
DISCUSSION
In this study, both males and females were at risk of being bitten by a snake, and males were at greater risk. This ties in with the results of other studies done in other parts of China.9,10 The main reason is that males in China are usually in charge of field activity and they are more likely to encounter snakes. Significantly, among 40 patients with a positive bacterial culture, those bitten with D. acutus accounted for nearly half. Deinagkistrodon acutus can inject a large amount of venom at each envenomation, and their venom is rich in C-type lectin, metalloproteinase, phospholipase A2s, and serine protease, which can lead to tissue necrosis at the site of the bite.11–14 Thus, the risk of secondary infection of the dead tissue may be increased.
Regarding the bacteriology of snakebite wounds, although there are some differences in bacterial flora of snakebite wounds, a great resemblance exists between different snake species as well as different geographic regions. Two studies of wound bacteriology of snakebite in Taiwan found Gram-positive bacteria were identified more frequently than Gram-negative bacteria. Enterococcus faecalis and M. morganii were the main pathogens identified in the culture report.5,15 A study from India showed that S. aureus was the most frequent isolate, followed by E. coli, showing similar numbers of Gram-positive and Gram-negative bacteria.16 Our study revealed that Gram-negative pathogens were more frequent than Gram-positive pathological bacteria in culture reports; Morganella morganii and S. aureus were the predominant organisms, respectively. Furthermore, H./caviae aeromonas, P. aeruginosa, and E. faecalis were also seen more frequently in our study. It is not surprising that these results are somewhat different. The microbes recovered from the bitten wound are reflective of the oral flora of the biting snake. However, the oral flora of the biting snake not only involves the oral normal flora, but also is influenced by the microbiome of their habitat environment and prey.6,17,18 Notably, one isolate of Clostridium histolyticum was recovered in this study. There has been no recorded case of clostridial infection caused by snakebite, and cases of anaerobe-inducing snakebite wound infections are unusual (probably because anaerobic cultures are not often conducted).17,19 However, Clostridium species have always been isolated in the venom and oral cavity of snakes.6,20–23 Clostridium histolyticum is characterized by its specifically pronounced ability to attack soft tissue; it can undermine tissue and cause gas gangrene.24 Therefore, we suggest that anaerobic cultures be performed routinely, even in for those patients who do not have characteristics of anaerobic infection. In addition, all snakebites with massive tissue necrosis should be treated with antibiotics effective against clostridia.22 Polymicrobial infections are generally observed in patients with infected wounds secondary to snake envenomation.4,5,15,25 In our study, we noticed that polymicrobial infection cases accounted for 25% (10 of 40) of all positive bacterial cultures. Previous studies showed that polymicrobial infections presented enhanced causative agent persistence and disease severity, as well as heightened antimicrobial agent resistance.26 Therefore, more attention should be paid to snakebite wounds with polymicrobial infections.
The antibiotics to be used in the treatment of snakebite is still controversial. Some scholars recommend the routine use of antibiotics to prevent or control infection after snake bite,6,20 whereas others opine that microbiotic use should be initiated only after clinical proof of infection, such as local soft tissue necrosis, abscess formation, or gangrene.7,19 Moreover, the sensitivity of the pathogens and regional antibiotic resistance patterns should guide the choice of antibiotics.27 In our study, 78 patients (25.1%) progressed to clinically evident infection; this proportion is similar to two recent studies and is less than earlier research.4,5,15,16 A plausible explanation is that empirical antibiotics used in every hospitalized snakebite patient in our ward reduced infection rates. To our knowledge, there is still no consensus on the choice of antibiotic types for empirical treatments in Hangzhou. Clinicians often make choices based on their personal experience, common types include ampicillin, amoxicillin/clavulanic acid, azlocillin, and levofloxacin. In other areas, a study in Taiwan suggested that first-line agents such as amoxicillin/clavulanic acid, ampicillin/sulbactam, oxacillin, and cefazolin could be used empirically in patients with cellulitis secondary to snakebite.15 Scholars from India recommended that amoxicillin/clavulanic acid, levofloxacin, azithromycin, and imipenem can effectively contain the risk of secondary bacterial infections.28 However, in our study, isolated bacteria from snakebites showed 73.0% resistance to ampicillin, 91.3% resistance to cefoxitin, 91.7% resistance to cephazolin, and 88.5% resistance to amoxicillin/clavulanic. In addition, we observed 11 beta-lactamase production strains and 5 methicillin-resistant S. aureus strains among staphylococci. These findings all suggest that some first-line antibiotics recommended by clinicians to prevent infections after snakebite may not be effective in Hangzhou. Almost all isolated bacteria in our study were sensitive to fluoroquinolones such as levofloxacin and ciprofloxacin. Although this result is encouraging, we still need to be conservative about the use of fluoroquinolones as first-line empirical antibiotics to treat snakebite infection, because overuse of fluoroquinolones is particularly prone to fluoroquinolone resistance. Accordingly, we propose that fluoroquinolones be an alternative for treating snakebites when other first-line antibacterials are less effective.
Our study has two main strengths. First, the study included a good number of participants with venomous snakebite, which may add significant power to the results. Second, the data in our study is high quality and convincing, because it came from a hospital that specializes in snakebite treatments.
This study also has several limitations. First, it was a retrospective study with some potential bias, such as information bias and selection bias. Second, this is a single-center study and the flora of the snakebite wound varies from region to region. Our results may not be generalizable to other regions of the world. The use of antibiotics should be based on the local culture data. In addition, the presentation of wound infection related to snakebite might also be affected by secondary environmental contamination (e.g., wound cleansing, application of topical medicines, surgical debridement, antimicrobial therapy).
In conclusion, snakebite wounds are comprised of a wide range of bacteria. In our study, M. morganii and S. aureus were the predominant organisms. Most of the pathogenic bacteria presented resistance to some common first-line antibiotics, but were sensitive to levofloxacin and ciprofloxacin. Therefore, in the Hangzhou region, fluoroquinolones could be an appropriate alternative for empirical treatment in patients with snakebite when the effect of other antibiotics is poor.
REFERENCES
- 1. Chippaux J , 2017. Snakebite envenomation turns again into a neglected tropical disease! J Venom Anim Toxins Incl Trop Dis 23: 38. doi: 10.1186/s40409-017-0127-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Gutiérrez J Calvete J Habib A Harrison R Williams D Warrell D , 2017. Snakebite envenoming. Nat Rev Dis Primers 3: 17079. doi: 10.1038/nrdp.2017.63. [DOI] [PubMed] [Google Scholar]
- 3. Wagener M, Naidoo M, Aldous C, 2017. Wound infection secondary to snakebite. South Afr Med J 107: 315–319. [DOI] [PubMed] [Google Scholar]
- 4. Mao Y Liu P Hung D Lai W Huang S Hung Y Yang C , 2016. Bacteriology of Naja atra snakebite wound and its implications for antibiotic therapy. Am J Trop Med Hyg 94: 1129–1135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Yeh H Gao S Lin C , 2021. Naja atra wound infections from Taiwan cobra bites: determining bacteriology, antibiotic susceptibility, and the use of antibiotics: a cobra bite study. Toxins (Basel) 13: 183. doi: 10.3390/toxins13030183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Goldstein E Citron D Gonzalez H Russell F Finegold S , 1979. Bacteriology of rattlesnake venom and implications for therapy. J Infect Dis 140: 818–821. [DOI] [PubMed] [Google Scholar]
- 7. Nishioka SA Silveira P , 1992. Bacteriology of abscesses complicating bites of lance-headed vipers. Ann Trop Med Parasitol 86: 89–91. [DOI] [PubMed] [Google Scholar]
- 8. Lipsky B et al. 2012. 2012 Infectious Diseases Society of America clinical practice guideline for the diagnosis and treatment of diabetic foot infections. Nephrol Dial Transplant 54: e132–e173. [DOI] [PubMed] [Google Scholar]
- 9. Li W Chen F Wu S , 2016. The related risk factors analysis of snake-bite induced acute kidney injury. Med Sci Monit 22: 2335–2339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Chen X He H Cai H , 2019. Clinical and epidemiologic profile of venomous snakebites in Chongqing Wuling mountainous area, western China. Trans R Soc Trop Med Hyg 113: 587–589. [DOI] [PubMed] [Google Scholar]
- 11. Liu C Lin C Hsiao Y Wang P Yu J , 2018. Proteomic characterization of six Taiwanese snake venoms: identification of species-specific proteins and development of a SISCAPA-MRM assay for cobra venom factors. J Proteomics 187: 59–68. [DOI] [PubMed] [Google Scholar]
- 12. Su H Huang S Mao Y Liu M Lee K Lai P Tsai M , 2018. Deinagkistrodon acutus clinical and laboratory features distinguishing between and envenomation. J Venom Anim Toxins Incl Trop Dis 24: 43. doi: 10.1186/s40409-018-0179-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Chen P Huang M Chang J Liu C Chen C Hsieh C , 2019. Snake venom proteome and immuno-profiling of the hundred-pace viper, Deinagkistrodon acutus, in Taiwan. Acta Trop 189: 137–144. [DOI] [PubMed] [Google Scholar]
- 14. Huang F Zhao S Tong F Liang Y Le Grange J Kuang W Zhou Y , 2021. Unexpected death in a young man associated with a unilateral swollen leg: pathological and toxicological findings in a fatal snakebite from Deinagkistrodon acutus (Chinese moccasin). J Forensic Sci 66: 786–792. [DOI] [PubMed] [Google Scholar]
- 15. Lin C Chen Y Goh Z Seak C Seak J Shi-Ying G Seak C , Spot Investigators , 2020. Wound infections of snakebites from the venomous protobothrops mucrosquamatus and viridovipera stejnegeri in Taiwan: bacteriology, antibiotic susceptibility, and predicting the need for antibiotics—a BITE study. Toxins (Basel) 12: 575. doi: 10.3390/toxins12090575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Garg A Sujatha S Garg J Acharya N Chandra Parija S , 2009. Wound infections secondary to snakebite. J Infect Dev Countries 3: 221–223. [DOI] [PubMed] [Google Scholar]
- 17. Kerrigan K , 1992. Bacteriology of snakebite abscess. Trop Doct 22: 158–160. [DOI] [PubMed] [Google Scholar]
- 18. Abrahamian F Goldstein E , 2011. Microbiology of animal bite wound infections. Clin Microbiol Rev 24: 231–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Blaylock RS , 1999. Antibiotic use and infection in snakebite victims. South Afr Med J 89: 874–876. [PubMed] [Google Scholar]
- 20. Theakston RD Phillips RE Looareesuwan S Echeverria P Makin T Warrell DA , 1990. Bacteriological studies of the venom and mouth cavities of wild Malayan pit vipers (Calloselasma rhodostoma) in southern Thailand. Trans R Soc Trop Med Hyg 84: 875–879. [DOI] [PubMed] [Google Scholar]
- 21. Arroyo O Bolaños R Muñoz G , 1980. The bacterial flora of venoms and mouth cavities of Costa Rican snakes. Bull Pan Am Health Organ 14: 280–285. [PubMed] [Google Scholar]
- 22. Ledbetter EO Kutscher AE , 1969. The aerobic and anaerobic flora of rattlesnake fangs and venom: therapeutic implications. Arch Environ Health 19: 770–778. [DOI] [PubMed] [Google Scholar]
- 23. Lam KK et al. 2011. A cross-sectional survey of snake oral bacterial flora from Hong Kong, SAR, China. Emerg Med J 28: 107–114. [DOI] [PubMed] [Google Scholar]
- 24. Hoogerheide JC , 1937. Variability in morphological and biochemical properties of Clostridium histolyticum (Weinberg and Seguin). J Bacteriol 34: 387–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Jorge M, Ribeiro L, da Silva M, Kusano E, de Mendonça J, 1994. Microbiological studies of abscesses complicating Bothrops snakebite in humans: a prospective study. Toxicon 32: 743–748. [DOI] [PubMed] [Google Scholar]
- 26. Murray J Connell J Stacy A Turner K Whiteley M , 2014. Mechanisms of synergy in polymicrobial infections. J Microbiol 52: 188–199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Palappallil D , 2015. Pattern of use of antibiotics following snake bite in a tertiary care hospital. J Clin Diagn Res 9: OC05–OC09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Padhi L Panda S Mohapatra P Sahoo G , 2020. Antibiotic susceptibility of cultivable aerobic microbiota from the oral cavity of Echis carinatus from Odisha (India). Microb Pathog 143: 104121. doi: 10.1016/j.micpath.2020.104121. [DOI] [PubMed] [Google Scholar]