Abstract
This study examined experiences with eviction, house foreclosures, and homelessness in a large U.S. city sample of adults with Coronavirus Disease-2019 (COVID-19). A total of 3595 adults with COVID-19 participated in an assessment of health and well-being after completing contact tracing activities. The sample had a 5.7% lifetime prevalence of eviction, 3.7% lifetime prevalence of house foreclosure, and 8.2% lifetime prevalence of homelessness. Relative importance analyses revealed drug use was the most important variable associated with any lifetime eviction, lifetime house foreclosure, lifetime homelessness, and being currently at-risk of eviction or recently evicted. Loneliness was also relatively strongly associated with any lifetime eviction or homelessness, while socioeconomic characteristics were the most importance variables associated with late mortgage payments in the past month. Treatment for addiction problems may be important for in the aftermath of the COVID-19 pandemic and adults with histories of housing instability may be particularly at risk.
Supplementary Information
The online version contains supplementary material available at 10.1007/s10900-022-01166-5.
Keywords: Eviction, Home foreclosure, Homelessness, COVID-19, Drug use disorder
Unstable housing can negatively affect individual and community health. Having a safe, consistent, and secure place to live is important for well-being and everyday functioning [1, 2]. For example, people who experience housing instability are twice as likely to report poor health and to delay medical care due to financial burdens compared to those who have stable housing [3]. However, there are different types of housing instability and many, but not all, types of instability may be associated with health.
One population-based study of working-aged adults in Michigan found that renters behind on rental payments were more likely to have depression, while mortgage-holders behind on their mortgage or in foreclosure were more likely to have poor general health or a recent anxiety attack [4]. The study also found that frequent moves and eviction were not associated with poorer health after adjustment for sociodemographic characteristics. Another study of people living with human immunodeficiency virus (HIV) found the degree of housing instability had a ‘dose–response” association with virologic suppression rates for HIV. Moreover, research has shown that there are multiple pathways to homelessness, which can but not always include events like eviction and house foreclosure [5]. Together, these findings suggest the importance of considering multiple types of housing instability in relation to health.
The Coronavirus Disease-2019 (COVID-19) pandemic was an extraordinary event that affected the health and lives of millions of Americans. As of July 5, 2022, over 87 million cases of COVID-19 have been reported nationwide [6]. In addition to the virus itself and related sequelae, the pandemic has had major social and economic impacts through shelter-in-place orders, social distancing, and closing of non-essential businesses [7–10]. As the world contends with the aftermath of the COVID-19 pandemic, there is considerable concern with long-term negative outcomes from the pandemic, both in terms of symptoms (e.g., “Long COVID”) but also mental health impact. But it is largely unknown how the pandemic affected housing instability or more specifically, how people with histories of housing instability were affected by the pandemic. During the pandemic, empirical studies were published finding that evictions could increase risk for COVID-19 infection and mortality [11, 12]. However, there has been no study that has examined the housing histories of COVID-19 infected individuals and how their housing histories may be associated with current mental health and substance use problems. This information may be important in public health planning during recovery from the pandemic and relevant social determinants of mental health to be considered at a population level.
The current study used a large city-wide sample of residents in San Antonio, Texas (7th largest city in the U.S.) infected with COVID-19 to (1) examine histories of three types of housing instability: eviction, house foreclosures, and homelessness; and (2) examine the relation between histories of housing instability and current mental health and substance use during the COVID-19 pandemic.
Methods
From July 2020 through September 2022, the San Antonio campus of the University of Texas Health Science Center at Houston (UTHealth) School of Public Health partnered with the San Antonio Metropolitan Health District to lead a city-wide contact tracing operation in response to the COVID-19 pandemic in San Antonio, Texas. The UTHealth contact tracing team called lab-confirmed cases of COVID-19 (provided by hospitals or testing centers) to provide isolation instructions, notify contacts of potential exposure, and collect personal and demographic information about the cases.
From February 18, 2021 to March 28, 2022, the UTHealth School of Public Health contact tracing team distributed a survey to all COVID-19 cases after completion of the contact tracing activities. All study procedures and questions were approved by the institutional review board at UTHealth School of Public Health prior to deployment. The survey was sent via text message to the number on file, via a Qualtrics link hosted by the university. The survey contained screening questions at the beginning, only including participants that were (1) over the age of 18, (2) currently live in the city of San Antonio, (3) have a lab-confirmed case of COVID-19, and (4) can read and write in English. Informed consent was obtained after inclusion criteria were met, and the participant was free to complete the survey. Informed consent was obtained and participants were compensated with a $10 gift card for participation. Study procedures were approved by the institutional review board at UTHealth School of Public Health.
A total of 8807 participants initially completed the survey but after cleaning the data and removing incomplete or invalid surveys, a total of 3595 participants were retained and analyzed for the study.
Measures
Sociodemographic information was collected on age, gender, employment status, marital status, highest educational level achieved, income level, and veteran status.
Recent and lifetime history of three types of housing instability- eviction, house foreclosure, and homelessness- were assessed using measures used in previous studies [13–15]. Lifetime history of eviction and foreclosure was assessed by asking participants “Have you ever been evicted from an apartment or experienced a home foreclosure? (Please check all that apply)” with three response options; “Been evicted from apartment,” “Experienced foreclosure on a house,” and “Never been evicted or had foreclosure before.” Lifetime history of homelessness was assessed with the question “In your entire adult lifetime, have you ever been homeless (i.e., did not have a stable night-time residence, such as staying on streets, in shelters, cars, etc.)?” with “Yes” or “No” response options. Recent housing instability were assessed in terms of evictions and late mortgage payments. Participants who indicated they rent their home or apartment were asked “Are you currently at risk of being evicted?” with response options of “Yes, I was recently evicted,” “Yes, but I have not yet been evicted,” “No,” and “NA.” Participants who indicated they own a house were asked “Were you late on your mortgage this past month?” with the “Yes” or “No” response options.
To assess levels of social support, the Medical Outcomes Survey: Social Support Survey (MOS-SSS; [16] was used. This measure was developed to assess multiple dimensions of social support among patients with chronic illness, as well as the general adult population. The measure has been found to be valid and reliable [16]. The six items of the measure ask questions like “How often is each of the following kinds of support available to you if you need it?” and then lists scenarios such as “Someone to help with daily chores if you were sick” or “Someone to love and make you feel wanted.” Scores are rated from 1 (“None of the time”) to 5 (“All of the time”). Total scores are calculated by summing responses with total scores ranging from 6 to 30. In this study, the MOS-SSS showed excellent internal consistency (Cronbach’s alpha = 0.92).
To assess loneliness, the short form three-item version of the UCLA Loneliness Scale was used which has been administered in large-scale surveys [17]. This short form version was developed from the original UCLA Loneliness scale [18] and found to be psychometrically sound and strongly correlated with the original scale [17]. The three question ask the participant to rate from 1 (“Hardly ever”) to 3 (“Often”) how often they lack companionship, feel left out, and feel isolated from others. Scores were summed for a total score. In this study, the scale showed good internal consistency (Cronbach’s alpha = 0.82).
Symptoms of major depression and anxiety disorder were assessed with the Patient Health Questionnaire (PHQ-4) which consists of two items that assess depression (PHQ-2; [19] and two items that assess for anxiety (GAD-2; [20] with scores of 3 or greater indicative of a positive screen for each respective disorder [21]. In this study, there was good internal consistency for the depression items (Cronbach’s alpha = 0.82) and anxiety items (Cronbach’s alpha = 0.80).
Symptoms of alcohol use disorder were assessed with the Alcohol Use Disorders Identification Test-Consumption (AUDIT-C) with a score of 4 or greater indicative of a positive screen [22]. In this study, the AUDIT-C showed acceptable internal consistency (Cronbach’s alpha = 0.70).
To assess illicit drug use, the Short Form Patient Reported Outcome Measurement Information System (SF PROMIS) Severity of Substance Use scale was administered which consists of seven items that asked about drug use in reference to the past 30 days. The short-form version was created for research in community and clinical settings, and has shown to be valid and reliable [23]. The scale measures the severity of substance use in four areas: the strong presence/desire to use drugs, the inability to cut back or quit, large amounts of time spent obtaining or using drugs, and continued use despite interference in interpersonal relationships. Items are rated on a scale from 1 (“Never”) to 5 (“Almost always”). In this study, these items showed excellent internal consistency (Cronbach’s alpha = 0.95). Using a score conversation table created for this scale [24], each summed raw score was converted to a T score to produce a standardized normed score with a population mean of 50 and standard deviation of 10.
Analysis
Data analysis was performed using Stata statistical software, version 16.0. Descriptive statics were used to analyze mean and percentages of variables within the study population (n = 3595). Tetrachoric correlations and Pearson’s correlations were used to explore associations between the three primary variables of interest (lifetime eviction, lifetime foreclosure, and lifetime homelessness), demographic characteristics, social support (as measured by the MOS-SSS), loneliness (as measured by the UCLA Three-Item Loneliness Scale), and severity of substance use (as measured by the SF PROMIS Severity of Substance Use survey). Tetrachoric correlations were used for associations between binary variables, and Pearson’s correlation was used between continuous/ordinal and binary variables. Significance was determined by p-values less than 0.05.
Using the total sample, a series of logistic regression analyses were then performed on three binary outcome variables: any lifetime eviction, lifetime foreclosure, and lifetime homelessness. Characteristics that were found to be significantly correlated with these outcome variables in bivariate analyses were included as independent variables in regression analyses. Odds ratios (ORs) were calculated as an effect size measure. In addition to ORs, we conducted relative importance analyses (also called dominance analyses) which is an extension of regression modeling that allows one to model intercorrelations among independent variables to determine the relative importance of each independent variable in explaining variance in the dependent variable [25]. The analysis yields a relative weight (% variance explained) for each independent variable that collectively sums to the total R2 in explaining the dependent variable. These logistic regression and relative importance analyses were then repeated on two binary outcomes for recent housing instability, namely being currently at-risk of eviction/recently evicted and having a late mortgage payment in the past month. Only participants who reported renting an apartment or owning a house were included in each analysis, respectively.
Results
In the total sample (n = 3595), 206 (5.73%) reported experiencing eviction in their lifetime, 133 (3.70%) reported experiencing house foreclosure in their lifetime, and 294 (8.18%) reported experiencing homelessness in their lifetime. Additionally, in the total sample, 34 (0.94%) reported experiencing homelessness in the past month, 134 (3.73%) reported they were currently at risk of eviction, 25 (0.70%) reported they had recently been evicted, and 113 (3.14%) reported they were late on their mortgage payments in the past month. These three types of housing instability were moderately to strongly correlated with each other, with tetrachoric correlations between lifetime eviction and lifetime home foreclosure at rt = 0.26, lifetime eviction and lifetime homelessness at rt = 0.67, and lifetime house foreclosure and lifetime homelessness at rt = 0.35.
Table 1 details the sociodemographic and mental health characteristics of the sample. The majority of participants were female, White, in their late 30’s, with at least some college education, employed, with annual income below $60,000, and have no psychiatric history. Bivariate correlations revealed there were similar and different characteristics that were strongly correlated with the three types of housing stability: any lifetime eviction, any lifetime house foreclosure, and any lifetime homelessness. Specifically, being Asian/Pacific Islander was strongly associated with lower lifetime risk of all three types of housing instability while being Native American/Alaskan Native was strongly associated with higher lifetime risk for all three types (correlation coefficients all ≥|.20|). A history of diagnosed schizophrenia-spectrum disorder and alcohol use disorder were both strongly associated with higher lifetime risk for all three types of housing instability. However, there were also characteristics that were more independently correlated with certain types of housing instability. For example, being Black Non-Hispanic and self-employed were strongly associated with both lifetime house foreclosure and homelessness (but not eviction). Being divorced/separated/widowed was only strongly associated with lifetime house foreclosure. Several psychiatric diagnoses were strongly associated with lifetime eviction and lifetime homelessness (but not house foreclosure), including history of diagnosed bipolar disorder, anxiety disorder, posttraumatic stress disorder, and drug use disorder.
Table 1.
Sociodemographic and mental health characteristics of the sample and their association with any lifetime eviction, house foreclosure, or homelessness (n = 3595)
| Sociodemographic characteristics | Mean/count (SD/%) | Correlation with any lifetime eviction | Correlation with any lifetime house foreclosure | Correlation with any lifetime homelessness |
|---|---|---|---|---|
| Age | 37.04 (0.22) | − 0.02 | 0.02 | − 0.05** |
| Gender | ||||
| Male | 1238 (34.44%) | − 0.03 | 0.09 | 0.11** |
| Female | 2344 (65.20%) | 0.0243 | − 0.10 | − 0.12** |
| Other | 13 (0.36%) | 0.05 | 0.12 | 0.31* |
| Race/ethnicity | ||||
| White Non-Hispanic | 951 (26.45%) | − 0.03 | 0.06 | − 0.09* |
| White Hispanic | 2003 (55.72%) | − 0.07 | − 0.24*** | − 0.12** |
| Black Non-Hispanic | 297 (8.26%) | 0.15** | 0.28*** | 0.27*** |
| Black Hispanic | 78 (2.17%) | 0.06 | 0.11 | 0.08 |
| Asian/Pacific Islander | 100 (2.78%) | − 0.29* | − 0.21 | − 0.20 |
| Native American/Alaskan Native | 30 (0.83%) | 0.40*** | 0.26* | 0.43*** |
| Other | 136 (3.78%) | − 0.02 | 0.11 | 0.10 |
| Education level | − 0.08*** | − 0.02 | − 0.11*** | |
| Below high school | 103 (2.87%) | |||
| High school or equivalent | 907 (25.23%) | |||
| Some college | 1100 (30.60%) | |||
| Associates/Bachelor’s | 1116 (31.04%) | |||
| Master’s degree | 305 (8.48%) | |||
| Doctoral degree | 64 (1.78%) | |||
| Marital status | ||||
| Single | 1558 (43.34%) | 0.02 | − 0.09 | 0.07 |
| Married/living with partner | 1607 (44.70%) | − 0.09* | − 0.07 | − 0.14*** |
| Divorced/separated/widowed | 430 (11.96%) | 0.12* | 0.25*** | 0.12** |
| Employment status | ||||
| Employed full/half-time | 2593 (72.13%) | − 0.11** | − 0.01 | − 0.23*** |
| Unemployed/other | 573 (15.94%) | 0.09 | − 0.19** | 0.16*** |
| Disabled/retired | 214 (5.95%) | 0.01 | 0.06 | 0.02 |
| Self-employed | 215 (5.98%) | 0.12* | 0.22*** | 0.24*** |
| Personal annual income | − 0.08*** | 0.01 | − 0.11*** | |
| No income | 329 (9.15%) | |||
| $1–$19,999 | 814 (22.64%) | |||
| $20,000–$39,999 | 964 (26.82%) | |||
| $40,000–$59,999 | 728 (20.25%) | |||
| $60,000–$79,999 | 349 (9.71%) | |||
| $80,000–$99,999 | 175 (4.87%) | |||
| $100,000+ | 236 (6.56%) | |||
| Psychosocial status | ||||
| History of psychiatric diagnoses | ||||
| No mental disorders | 2704 (75.22%) | − 0.28*** | − 0.22*** | − 0.37*** |
| Schizophrenia-spectrum disorder | 12 (0.33%) | 0.39** | 0.28 | 0.24*** |
| Bipolar disorder | 139 (3.87%) | 0.25*** | 0.18* | 0.39*** |
| Major depressive disorder | 263 (7.32%) | 0.27*** | 0.13* | 0.18*** |
| Anxiety disorder | 590 (16.41%) | 0.22*** | 0.15** | 0.28*** |
| Posttraumatic stress disorder | 196 (5.45%) | 0.35*** | 0.19** | 0.43*** |
| Alcohol use disorder | 64 (1.78%) | 0.36*** | 0.34*** | 0.45*** |
| Drug use disorder | 41 (1.14%) | 0.38*** | 0.13 | 0.56*** |
| Current PHQ-2 score | 1.26 (0.03) | 0.15*** | 0.09*** | 0.18*** |
| Current GAD-2 score | 1.31 (0.03) | 0.14*** | 0.09*** | 0.15*** |
| Current AUDIT-C score | 2.27 (0.04) | 0.08*** | 0.09*** | 0.07*** |
| MOS social support survey | 22.16 (0.13) | − 0.11*** | − 0.05** | − 0.16*** |
| UCLA loneliness scale | 4.66 (0.03) | 0.16*** | 0.09*** | 0.17*** |
| PROMIS severity of substance use T-scores | 42.15 (0.06) | 0.18*** | 0.18*** | 0.18*** |
Bolded values indicate correlation coefficients ≥|.20|
*p < 0.05, **p < 0.01, ***p < 0.001
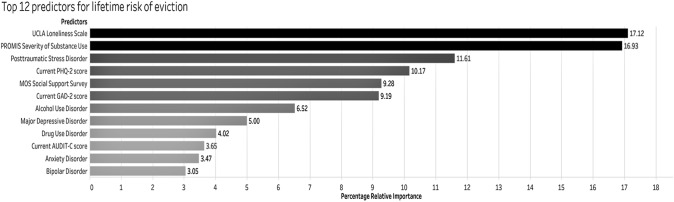
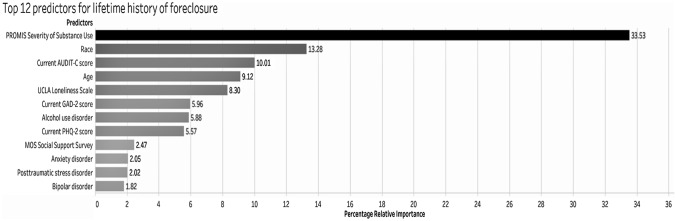
Multivariable analyses were then conducted to identify characteristics independently associated with lifetime risk of three types of housing instability (see Table 2). The most notable associations (ORs ≥ 2.0 or ≤ 0.50) revealed Native American/Alaskan Native adults were at highest risk for any lifetime eviction, house foreclosure, and homelessness while Asian/Pacific Islander adults were at lowest risk. A history of diagnosed schizophrenia/spectrum disorder was associated with any lifetime eviction and house foreclosure, while a history of diagnosed posttraumatic stress disorder, alcohol use disorder, or drug use disorder were each associated with any lifetime homelessness. Being unemployed/other was associated with lower likelihood of any lifetime home foreclosure while being self-employed was associated with higher likelihood of any lifetime homelessness. Relative importance analysis provided further information by showing the measures of loneliness and drug use were the most important variables associated with any lifetime eviction (Fig. 1) and lifetime homelessness (Supplementary Fig. 1). Drug use was also the most important variable associated with any lifetime house foreclosure (Fig. 2).
Table 2.
Logistic regression of sociodemographic and mental health characteristics associated with any lifetime eviction, house foreclosure, and homelessness
| Any lifetime eviction (n = 1240) |
Any lifetime house foreclosure (n = 1190) |
Any lifetime homelessness (n = 3595) |
||||
|---|---|---|---|---|---|---|
| Odds ratio | p value | Odds ratio | p value | Odds ratio | p value | |
| Age | 1.02 | 0.02* | 1.02 | 0.03* | 1.02 | 0.04* |
| Gender | ||||||
| Male | Ref | Ref | Ref | Ref | Ref | Ref |
| Female | 1.26 | 0.21 | 0.96 | 0.86 | 0.73 | 0.07 |
| Other | 0.84 | 0.89 | 0.64 | 0.75 | 1.45 | 0.67 |
| Race/ethnicity | ||||||
| White Non-Hispanic | Ref | Ref | Ref | Ref | Ref | Ref |
| White Hispanic | 0.86 | 0.43 | 0.63 | 0.05* | 0.97 | 0.89 |
| Black Non-Hispanic | 1.12 | 0.68 | 1.98 | 0.02* | 1.99 | 0.01** |
| Black Hispanic | 1.13 | 0.80 | 1.67 | 0.35 | 1.75 | 0.22 |
| Asian/Pacific Islander | 0.23 | 0.15 | 0.39 | 0.36 | 0.38 | 0.23 |
| Native American/Alaskan Native | 5.10 | 0.00*** | 2.55 | 0.13 | 10.63 | 0.00*** |
| Other | 0.84 | 0.69 | 2.14 | 0.08 | 1.52 | 0.30 |
| Education | 0.68 | 0.00*** | 0.73 | 0.00*** | 0.68 | 0.00*** |
| Marital status | ||||||
| Single | Ref | Ref | Ref | Ref | Ref | Ref |
| Married/living with partner | 1.16 | 0.43 | 1.36 | 0.20 | 1.24 | 0.24 |
| Divorced/separated/widowed | 1.17 | 0.53 | 2.75 | 0.00*** | 1.15 | 0.58 |
| Employment status | ||||||
| Employed full/half-time | Ref | Ref | Ref | Ref | Ref | Ref |
| Unemployed/other | 0.79 | 0.30 | 0.36 | 0.01** | 1.17 | 0.48 |
| Disabled/retired | 0.68 | 0.29 | 0.77 | 0.54 | 0.57 | 0.16 |
| Self-employed | 1.33 | 0.33 | 1.56 | 0.14 | 2.15 | 0.00*** |
| Personal annual income | 0.93 | 0.03* | 1.03 | 0.48 | 0.96 | 0.23 |
| Psychosocial status | ||||||
| No mental disorders | 0.71 | 0.23 | 0.51 | 0.05* | 0.80 | 0.43 |
| Schizophrenia-spectrum disorder | 2.71 | 0.18 | 4.22 | 0.14 | 1.03 | 0.98 |
| Bipolar disorder | 0.97 | 0.92 | 0.94 | 0.90 | 1.56 | 0.15 |
| Major depressive disorder | 1.35 | 0.27 | 1.00 | 1.00 | 0.59 | 0.07 |
| Anxiety disorder | 0.86 | 0.59 | 0.74 | 0.37 | 1.19 | 0.54 |
| Posttraumatic stress disorder | 1.94 | 0.01** | 0.90 | 0.76 | 2.85 | 0.00*** |
| Alcohol use disorder | 1.71 | 0.19 | 1.52 | 0.37 | 2.10 | 0.07 |
| Drug use disorder | 1.23 | 0.67 | 0.21 | 0.03* | 2.89 | 0.02* |
| Current PHQ-2 score | 1.04 | 0.53 | 1.02 | 0.78 | 1.11 | 0.11 |
| Current GAD-2 score | 1.07 | 0.30 | 1.09 | 0.28 | 1.03 | 0.66 |
| Current AUDIT-C score | 1.06 | 0.08 | 1.07 | 0.10 | 1.02 | 0.56 |
| MOS social support survey | 0.98 | 0.06 | 0.99 | 0.51 | 0.95 | 0.00*** |
| UCLA loneliness scale | 1.14 | 0.01** | 1.10 | 0.12 | 1.11 | 0.04* |
| PROMIS severity of substance use T-scores | 1.06 | 0.00*** | 1.10 | 0.00*** | 1.06 | 0.00*** |
Bolded values indicate odds ratio ≥ 2.0 or ≤ .50
*p < 0.05, **p < 0.01, ***p < 0.001
Fig. 1.
Relative importance analysis of variables predicting any lifetime eviction (n = 1240)
Fig. 2.
Relative importance analysis of variables predicting any lifetime house foreclosure (n = 1190)
Multivariable analyses conducted to identify characteristics associated with recent housing instability (see Table 3) revealed that again among race/ethnic groups, Native American/Alaskan Native adults were most likely to be currently at risk of eviction or were recently evicted and Asian/Pacific Islander adults were least likely (ORs ≥ 2.0 or ≤ 0.50). There was a limited sample size of racial/ethnic minority participants who owned a house, but it appears White Hispanic adults were at greater risk of late mortgage payments at least compared to White non-Hispanic adults. In addition, being divorced/separated/widowed and having a history of bipolar disorder were associated with being late on mortgage payments in the past month, while having history of major depressive disorder was associated with lower likelihood of being at-risk of eviction/recently evicted. As shown in Supplementary Figs. 2 and 3, relative importance analysis revealed drug use was the most important variable (explaining 35% of the variance) associated with being currently at-risk of eviction/recently evicted, while education level and personal income were the most important variables (explaining 40% of the variance) associated with having late mortgage payments in the past month.
Table 3.
Logistic regression of sociodemographic and mental health characteristics associated with recent types of housing instability
| Currently at-risk of eviction/recently evicted (n = 1240) |
Late on mortgage payments in past month (n = 1190) |
|||
|---|---|---|---|---|
| Odds ratio | p value | Odds ratio | p value | |
| Age | 1.01 | 0.54 | 0.97 | 0.01** |
| Gender | ||||
| Male | Ref | Ref | Ref | Ref |
| Female | 0.55 | 0.01** | 1.21 | 0.48 |
| Other | 0.51 | 0.61 | – | – |
| Race/ethnicity | ||||
| White Non-Hispanic | Ref | Ref | Ref | Ref |
| White Hispanic | 0.54 | 0.01** | 3.16 | 0.00*** |
| Black Non-Hispanic | 1.29 | 0.42 | 1.00 | 1.00 |
| Black Hispanic | 1.43 | 0.51 | – | – |
| Asian/Pacific Islander | 0.21 | 0.15 | 1.90 | 0.36 |
| Native American/Alaskan Native | 6.52 | 0.00*** | – | – |
| Other | 0.47 | 0.20 | 4.18 | 0.02* |
| Education | 0.77 | 0.02* | 0.83 | 0.11 |
| Marital status | ||||
| Single | Ref | Ref | Ref | Ref |
| Married/living with partner | 0.97 | 0.89 | 1.87 | 0.05* |
| Divorced/separated/widowed | 0.80 | 0.51 | 3.84 | 0.00*** |
| Employment status | ||||
| Employed full/half-time | Ref | Ref | Ref | Ref |
| Unemployed/other | 1.26 | 0.43 | 1.78 | 0.07 |
| Disabled/retired | 1.40 | 0.53 | 0.55 | 0.31 |
| Self-employed | 1.43 | 0.28 | 1.72 | 0.22 |
| Personal annual income | 0.88 | 0.01** | 0.97 | 0.39 |
| Psychosocial status | ||||
| No mental disorders | 0.54 | 0.10 | 0.87 | 0.78 |
| Schizophrenia-spectrum disorder | 0.57 | 0.68 | – | – |
| Bipolar disorder | 1.39 | 0.43 | 2.55 | 0.09 |
| Major depressive disorder | 0.49 | 0.06 | 1.30 | 0.56 |
| Anxiety disorder | 0.59 | 0.14 | 1.46 | 0.43 |
| Posttraumatic stress disorder | 1.64 | 0.19 | 0.73 | 0.55 |
| Alcohol use disorder | 1.74 | 0.29 | – | – |
| Drug use disorder | 0.66 | 0.57 | – | – |
| Current PHQ-2 score | 1.00 | 0.97 | 0.97 | 0.77 |
| Current GAD-2 score | 1.33 | 0.00*** | 1.17 | 0.11 |
| Current AUDIT-C score | 0.99 | 0.82 | 0.99 | 0.84 |
| MOS social support survey | 0.98 | 0.13 | 0.94 | 0.00*** |
| UCLA loneliness scale | 1.04 | 0.49 | 0.89 | 0.12 |
| PROMIS severity of substance use T-scores | 1.10 | 0.00*** | 1.06 | 0.04* |
Bolded values indicate odds ratio ≥ 2.0 or ≤ .50
*p < 0.05, **p < 0.01, ***p < 0.001
Discussion
In a city-wide sample of U.S. adults with confirmed cases of COVID-19 infection, we found the lifetime prevalence rates of eviction at 5.7%, lifetime prevalence of house foreclosure at 3.7%, and lifetime prevalence of homelessness at 8.2%. The sample’s prevalence rates of eviction and house foreclosure were comparable, or perhaps lower than estimated U.S. population estimates [5, 26, 27], Tsai & Hooshyar (in press) but the sample’s prevalence rate of homelessness was double that found in the general adult population of 4.2% [19]. However, further study is needed using matched samples with the same measures to confirm that adults with histories of homelessness were in fact more likely to have been infected with COVID-19. Importantly, only small proportions of the sample reported recently experiencing eviction, late mortgage payments, or homelessness which may be due to moratoria on evictions and house foreclosures [15, 20, 28], the economic impact payments [28, 29], and other financial assistance available during the COVID-19 pandemic. But many of these protections and programs have ended as the COVID-19 pandemic winds down and there may be rises in housing instability in the aftermath [10]. For example, 2 years after the pandemic began, more than 4000 households in San Antonio are at risk of losing their homes due to accumulated rent [30].
There were social, economic, and mental health factors associated with different forms of housing instability. Education and income levels were strongly associated with late mortgage payments and loneliness was associated with any lifetime eviction or lifetime homelessness. But perhaps, the most striking finding was how strong and consistent recent drug use was associated with distant and recent experiences of housing instability. While we cannot infer causality, we did examine different time frames and types of housing instability; we also used relative importance analyses which helped determine which were the most important variables out of an array of other psychosocial and clinical variables. Nonetheless, with some reports that mental health and substance use problems have dramatically increased during the COVID-19 pandemic [31, 32] the findings suggest adults with histories of housing instability may be at particularly high risk for substance use problems during this time. Population-level efforts to help communities recover from COVID-19 should consider providing easy access to addiction treatment and targeting those with histories of housing instability to not only treat their addiction but prevent further housing instability.
There were several study limitations to note. The data were based on a cross-sectional survey and we did not used structured diagnostic interviews for mental health or substance use disorders so the findings need to be confirmed with other data sources. Participants were from one U.S. city with a large Hispanic population and the results may not be generalizable to all cities. These limitations were counterbalanced by the strengths of the study which included a large city-wide sample of confirmed COVID-19 cases; assessment of multiple types of housing instability with varying time frames; use of different multivariable analytic procedures; and findings that contribute to the depth of knowledge about social determinants of health and the psychosocial needs of adults with COVID-19 to inform recovery efforts.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
The authors thank the San Antonio Metropolitan Health District, UTHealth contact tracers, and the City of San Antonio for their support of this work.
Author Contributions
JT designed the study and wrote the paper. AG helped collect and analyze the data. MV helped collect the data and write the paper. All authors read and approved the final manuscript.
Funding
There was no specific funding for this work, but the work was supported by a contract tracing operation with the San Antonio Metropolitan Health District and with some supplemental university funds by the first author.
Data Availability
Data generated for this project are not publicly available because they are part of ongoing research but are available from the corresponding author on reasonable request with proper approval by the institutional review board.
Code Availability
Not applicable.
Declarations
Conflict of interest
None of the authors reports any conflicts of interest with this work.
Ethical Approval
The institutional review board at the University of Texas Health Science Center at Houston approved all study procedures (HSC-SPH-20-0931).
Consent to Participate
All participants provided informed consent to participate in this study.
Consent for Publication
Not applicable.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bassuk EL, DeCandia CJ, Tsertsvadze A, Richard MK. The effectiveness of housing interventions and housing and service interventions on ending family homelessness: A systematic review. American Journal of Orthopsychiatry. 2014;84(5):457–474. doi: 10.1037/ort0000020. [DOI] [PubMed] [Google Scholar]
- 2.Bratt RG. Housing and family well-being. Housing Studies. 2002;17(1):13–26. doi: 10.1080/02673030120105857. [DOI] [Google Scholar]
- 3.Stahre M, VanEenwyk J, Siegel P, Njai R. Peer reviewed: Housing insecurity and the association with health outcomes and unhealthy behaviors, Washington State, 2011. Preventing Chronic Disease. 2015;12:E109. doi: 10.5888/pcd12.140511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Burgard SA, Seefeldt KS, Zelner S. Housing instability and health: Findings from the Michigan Recession and Recovery Study. Social science & medicine. 2012;75(12):2215–2224. doi: 10.1016/j.socscimed.2012.08.020. [DOI] [PubMed] [Google Scholar]
- 5.Tsai, J., & Hooshyar, D. (in press). Prevalence of eviction, home foreclosure, and homelessness among low-income U.S. veterans: The National Veteran Homeless and Other Poverty Experiences (NV-HOPE) study. [DOI] [PubMed]
- 6.Centers for Disease Control Prevention. (2022, July 5, 2022). COVID Data Tracker. U.S. Department of Health & Human Services. Retrieved July 5 from https://covid.cdc.gov/covid-data-tracker/#datatracker-home
- 7.Li K, Foutz NZ, Cai Y, Liang Y, Gao S. Impacts of COVID-19 lockdowns and stimulus payments on low-income population’s spending in the United States. PLoS ONE. 2021;16(9):e0256407. doi: 10.1371/journal.pone.0256407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McKee M, Stuckler D. If the world fails to protect the economy, COVID-19 will damage health not just now but also in the future. Nature Medicine. 2020;26(5):640–642. doi: 10.1038/s41591-020-0863-y. [DOI] [PubMed] [Google Scholar]
- 9.Tsai J, Wilson M. COVID-19: A potential public health problem for homeless populations. The Lancet Public Health. 2020;5(4):e186–e187. doi: 10.1016/S2468-2667(20)30053-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wilson JM, Lee J, Fitzgerald HN, Oosterhoff B, Sevi B, Shook NJ. Job insecurity and financial concern during the COVID-19 pandemic are associated with worse mental health. Journal of Occupational and Environmental Medicine. 2020;62(9):686–691. doi: 10.1097/JOM.0000000000001962. [DOI] [PubMed] [Google Scholar]
- 11.Leifheit KM, Linton SL, Raifman J, Schwartz GL, Benfer EA, Zimmerman FJ, Pollack CE. Expiring eviction moratoriums and COVID-19 incidence and mortality. American Journal of Epidemiology. 2021;190(12):2503–2510. doi: 10.1093/aje/kwab196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nande A, Sheen J, Walters EL, Klein B, Chinazzi M, Gheorghe AH, Adlam B, Shinnick J, Tejeda MF, Scarpino SV. The effect of eviction moratoria on the transmission of SARS-CoV-2. Nature Communications. 2021;12(1):1–13. doi: 10.1038/s41467-021-22521-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tsai J. Lifetime and 1-year prevalence of homelessness in the U.S. population: Results from the National Epidemiologic Survey on Alcohol and Related Conditions-III. Journal of Public Health. 2018;40(1):65–74. doi: 10.1093/pubmed/fdx034. [DOI] [PubMed] [Google Scholar]
- 14.Tsai J, Huang M, Blosnich JR, Elbogen EB. Evictions and tenant-landlord relationships during the 2020–2021 eviction moratorium in the US. American Journal of Community Psychology. 2022;70:117–126. doi: 10.1002/ajcp.12581. [DOI] [PubMed] [Google Scholar]
- 15.Tsai J, Link BG, Rosenheck RA, Pietrzak RH. Homelessness among a nationally representative sample of U.S. veterans: Prevalence, service utilization, and correlates. Social Psychiatry and Psychiatric Epidemiology. 2016;51(6):907–916. doi: 10.1007/s00127-016-1210-y. [DOI] [PubMed] [Google Scholar]
- 16.Sherbourne CD, Stewart AL. The MOS social support survey. Social Science and Medicine. 1991;32(6):705–714. doi: 10.1016/0277-9536(91)90150-B. [DOI] [PubMed] [Google Scholar]
- 17.Hughes ME, Waite LJ, Hawkley LC, Cacioppo JT. A short scale for measuring loneliness in large surveys: Results from two population-based studies. Research on Aging. 2004;26(6):655–672. doi: 10.1177/0164027504268574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Russell DW. UCLA Loneliness Scale (Version 3): Reliability, validity, and factor structure. Journal of Personality Assessment. 1996;66(1):20–40. doi: 10.1207/s15327752jpa6601_2. [DOI] [PubMed] [Google Scholar]
- 19.Kroenke K, Spitzer RL, Williams JBW. The Patient Health Questionnaire-2: Validity of a two-item depression screener. Medical Care. 2003;41(11):1284–1292. doi: 10.1097/01.MLR.0000093487.78664.3C. [DOI] [PubMed] [Google Scholar]
- 20.Kroenke K, Spitzer RL, Williams JBW, Monahan PO, Löwe B. Anxiety disorders in primary care: Prevalence, impairment, comorbidity, and detection. Annals of Internal Medicine. 2007;146(5):317–325. doi: 10.7326/0003-4819-146-5-200703060-00004. [DOI] [PubMed] [Google Scholar]
- 21.Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bush K, Kivlahan DR, McDonnell MB. The AUDIT alcohol consumption questions (AUDIT-C): An effective brief screening test for problem drinking. JAMA Internal Medicine. 1998;158(16):1789–1795. doi: 10.1001/archinte.158.16.1789. [DOI] [PubMed] [Google Scholar]
- 23.Pilkonis PA, Yu L, Dodds NE, Johnston KL, Lawrence SM, Hilton TF, Daley DC, Patkar AA, McCarty D. Item banks for substance use from the Patient-Reported Outcomes Measurement Information System (PROMIS®): Severity of use and positive appeal of use. Drug and Alcohol Dependence. 2015;156:184–192. doi: 10.1016/j.drugalcdep.2015.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.HealthMeasures. (2018). Patient-Reported Outcomes Measurement Information System. Dynamic Tools to Measure Health Outcomes from the Patient Perspective: Substance Use. HealthMeasures.
- 25.Tonidandel S, LeBreton JM. Relative importance analysis: A useful supplement to regression analysis. Journal of Business and Psychology. 2011;26(1):1–9. doi: 10.1007/s10869-010-9204-3. [DOI] [Google Scholar]
- 26.ATTOM Data Solutions. (2020). U.S. foreclosure activity drops to 15-Year low in 2019. ATTOM Data Solutions. Retrieved January 15 from https://www.attomdata.com/news/market-trends/foreclosures/attom-data-solutions-2019-year-end-u-s-foreclosure-market-report/
- 27.Gromis A, Desmond M. Estimating the prevalence of eviction in the United States. Cityscape. 2021;23(2):279–290. [Google Scholar]
- 28.Tsai J, Huang M, Montgomery AE, Elbogen EB. Receipt, spending, and clinical correlates of the economic impact payment among middle-and low-income US adults. Psychiatric Services. 2021;72(12):1377–1384. doi: 10.1176/appi.ps.202100001. [DOI] [PubMed] [Google Scholar]
- 29.Internal Revenue Service. (2020, December 30, 2020). Economic Impact Payments. U.S. Department of the Treasury. Retrieved December 24 from https://www.irs.gov/coronavirus/economic-impact-payments
- 30.San Antonio Housing Authority. (2022). More than 4000 families have past due rent as eviction moratorium deadline looms. San Antonio Housing Authority. Retrieved July 5 from https://saha.org/press_release/pastduerent/
- 31.Czeisler MÉ, Lane RI, Petrosky E, Wiley JF, Christensen A, Njai R, Weaver MD, Robbins R, Facer-Childs ER, Barger LK. Mental health, substance use, and suicidal ideation during the COVID-19 pandemic—United States, June 24–30, 2020. Morbidity and Mortality Weekly Report. 2020;69(32):1049–1057. doi: 10.15585/mmwr.mm6932a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wei Y, Shah R. Substance use disorder in the COVID-19 pandemic: A systematic review of vulnerabilities and complications. Pharmaceuticals. 2020;13(7):155. doi: 10.3390/ph13070155. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data generated for this project are not publicly available because they are part of ongoing research but are available from the corresponding author on reasonable request with proper approval by the institutional review board.
Not applicable.