1. Introduction
The continuing global spread of COVID-19 has led to a global health crisis(Anon, 2022). The pandemic and efforts to contain it lead to abrupt and unpredictable changes to residents’ daily lives, and could increase the risk of mental health problems (Moreno et al., 2020). Longitudinal analysis showed that more stringent policies and intense pandemics are both associated with worse mental health (Aknin et al., 2022). In late February, 2022, a wave of COVID-19 infection rapidly spread throughout Shanghai, China. To limit the spread of and eliminate COVID-19, from March to May, Shanghai municipal implemented a “dynamic zero-COVID” policy, involving business closures, restrictions on domestic movements, and stay at home orders (Anon, 2022). The stringent and comprehensive pandemic control strategies are essential for China to achieve better outcomes compared to Europe and the America(Tandon, 2021), and exit from the pandemic (Zhang et al., 2022). However, its impact on the mental health of local residents have not been investigated yet.
2. Methods
A cross-sectional study was conducted through an online questionnaire platform called Wenjuanxing (www.wjx.cn) from May 1–15, 2022 in Shanghai. Individuals were eligible to participate if they were resident in Shanghai from March 1st. The Patient Health Questionnaire-2 (PHQ-2) (Kroenke et al., 2003), COVID-19 Exposure and Family Impact Scales (CEFIS) (Kazak et al., 2021) and a self-designed questionnaire to evaluate the impact of COVID-19 on daily life were completed. Categorical variables were subjected to the Pearson χ2 test or Fisher’s exact test. To identify risk and protective factors for depression, multivariable logistic regression was performed.
3. Results
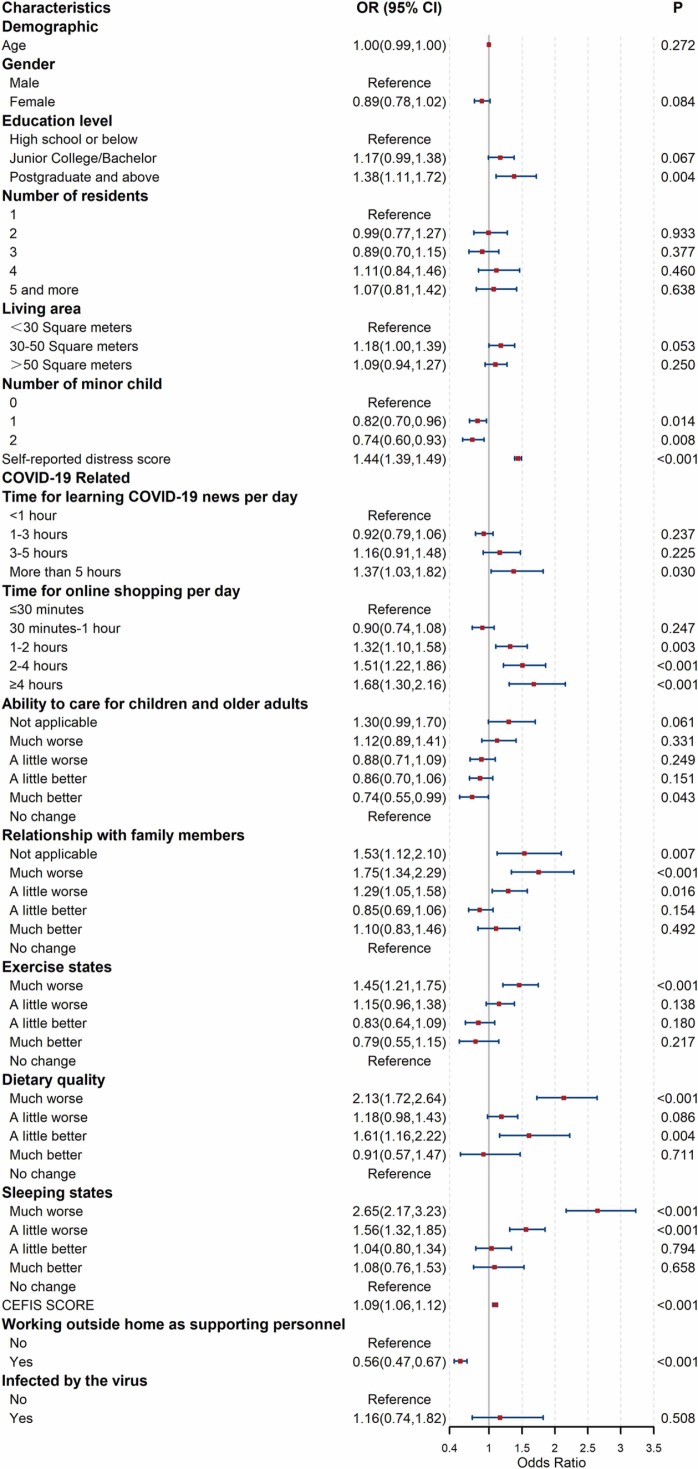
Totally 6154 adults were included in final analysis. The median age of the participants was 40 (33−49) years, and 63.41% were female. In total, 2370 (38.51%) participants had a PHQ-2 score ≥ 3. Multivariate logistic regression showed that high education level (postgraduate and above, aOR: 1.38(1.11,1.72)), more than 5 h for learning COVID-19 news per day (aOR: 1.38(1.11,1.72)), high distress scores (aOR: 1.44(1.39–1.49)), long Time for online shopping per day (≥4 h, aOR: 1.68(1.30,2.16)), poor relationship with family members (much worse, aOR: 1.75(1.34,2.29)), poor exercise (much worse, aOR: 1.45(1.21,1.75)), poor dietary (much worse, aOR: 2.13(1.72,2.64)) and poor sleeping (much worse, aOR: 2.65(2.17,3.23)) were risk factors of depression. In addition, working outside as supporting personnel (aOR: 0.56(0.47,0.67)) and having minor children (2 children, aOR: 0.74(0.60,0.93)) were protective factors of depression development (see Fig. 1).
Fig. 1.
Multivariate logistic regression analysis of characteristics associated with depression among participants.
4. Discussion
This study examined the prevalence of depression and its risk factors in Shanghai residents during the COVID-19 pandemic and lockdown measures. The prevalence of depression was 38.5%, which is in line with existing literature (Santomauro et al., 2021). The pandemic and subsequent stringent measures taken in Shanghai caused inconvenience in everyday life, such as dietary, exercise, sleep and negatively impacted population mental health. In India and Bangladesh, suicide demographics was also impacted(Kar et al., 2021).
Self-reported distress score, spending a large amount of time on COVID-19 news or shopping online daily, having a considerably poorer relationship with family members, having considerably poorer exercise, dietary quality or sleep and more COVID-19 exposure are risk factors for depressive symptoms. Having minor children and continuously working outside the home during pandemic are protective factors for mental health. The most interesting finding is that individuals who spent more time engaged in online shopping for food and vegetables were inclined to experience depression. Because of the stringent lockdown measures, most adult residents of Shanghai bought supplies online via smartphone apps. 24.36% of the participants spent more than 2 h on online shopping. This behavior was called “Qiang cai” in chinese, which became a buzzword in April and May. These irrational consumer behaviors are known as panic buying(Taylor, 2021). The possible explanation might be that during the early days of this wave of COVID-19, the public experienced fear, panic, anxiety, and uncertainty, in part as a response to a real and/or perceived shortage of basic supplies. Panic buying by an anxious minority of shoppers leads to fear among other shoppers, in a process amplified by widespread dissemination of images and videos of panic buying and empty shelves in stores via social media (Arafat et al., 2021). Populations with limited digital literacy, such as the elderly, experienced increased difficultly sourcing food, medication, and other necessities (Hall et al., 2022).
5. Conclusion
Our findings reveals that a significant proportion of residents in Shanghai experienced depression during the COVID-19 pandemic and highlight the widespread adverse impact of COVID-19 on the public. Efforts should be made to address these issues during the ongoing pandemic. Various methods should be adopted to expand the supply channels for daily necessities for all people, especially vulnerable groups, including planned, centralized government procurement, management and supply of materials from non-governmental organizations. In view of adverse effect of residents’ excessive online shopping and media consumption on mental health, managing individuals’ risk perceptions and establishing healthy social media use are important to prevent mental problems during the COVID-19 lockdown.
Funding/Support
This work was funded by the National Natural Science Foundation of China (grant 71774166 to X.L, 72174204 to L.Z.), the Chinese Defence Research Program of Science and Technology (grant 2019-JCJQ-JJ-065 to X.L.), Military Medical Science and Technology Youth Cultivation Program (grant 19QNP019 to J.W.), Shanghai Sailing Program (grant 20YF1457900 to Y.Q.), , and the Sailing Talents Project of the Naval Military Medical University.
Role of the Funder/Sponsor
The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Conflict of Interest Disclosures
None reported.
Acknowledgements
The authors would like to express their gratitude to EditSprings (https://www.editsprings.cn) for the expert linguistic services provided.
References
- Aknin L.B., Andretti B., Goldszmidt R., Helliwell J.F., Petherick A., De Neve J., Dunn E.W., Fancourt D., Goldberg E., Jones S.P., Karadag O., Karam E., Layard R., Saxena S., Thornton E., Whillans A., Zaki J. Policy stringency and mental health during the COVID-19 pandemic: a longitudinal analysis of data from 15 countries. Lancet Public Health. 2022;7:e417–e426. doi: 10.1016/S2468-2667(22)00060-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO COVID-19 Dashboard. Geneva: World Health Organization, 2020. Available online: https://covid19.who.int/.
- Arafat S.M.Y., Ahmad A.R., Murad H.R., Kakashekh H.M. Perceived impact of social media on panic buying: an online cross-sectional survey in Iraqi Kurdistan. Front. Public Health. 2021:9. doi: 10.3389/fpubh.2021.668153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall B.J., Li G., Rafiq M.Y., Lu J., Li C. Digital determinants of public mental health and wellbeing in Shanghai during the 2022 lockdown. Asian J. Psychiatry. 2022;76 doi: 10.1016/j.ajp.2022.103155. [DOI] [PubMed] [Google Scholar]
- Kar S.K., Menon V., Arafat S.M.Y., Rai S., Kaliamoorthy C., Akter H., Shukla S., Sharma N., Roy D., Sridhar V.K. Impact of COVID-19 pandemic related lockdown on Suicide: Analysis of newspaper reports during pre-lockdown and lockdown period in Bangladesh and India. Asian J. Psychiatry. 2021;60 doi: 10.1016/j.ajp.2021.102649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kazak A.E., Alderfer M., Enlow P.T., Lewis A.M., Vega G., Barakat L., Kassam-Adams N., Pai A., Canter K.S., Hildenbrand A.K., McDonnell G.A., Price J., Schultz C., Sood E., Phan T. COVID-19 exposure and family impact scales: factor structure and initial psychometrics. J. Pedia Psychol. 2021;46:504–513. doi: 10.1093/jpepsy/jsab026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B.W. The patient health questionnaire-2. Med. Care. 2003;41:1284–1292. doi: 10.1097/01.MLR.0000093487.78664.3C. [DOI] [PubMed] [Google Scholar]
- Moreno C., Wykes T., Galderisi S., Nordentoft M., Crossley N., Jones N., Cannon M., Correll C.U., Byrne L., Carr S., Chen E.Y.H., Gorwood P., Johnson S., Kärkkäinen H., Krystal J.H., Lee J., Lieberman J., López-Jaramillo C., Männikkö M., Phillips M.R., Uchida H., Vieta E., Vita A., Arango C. How mental health care should change as a consequence of the COVID-19 pandemic. Lancet Psychiatry. 2020;7:813–824. doi: 10.1016/S2215-0366(20)30307-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santomauro D.F., Mantilla Herrera A.M., Shadid J., Zheng P., Ashbaugh C., Pigott D.M., Abbafati C., Adolph C., Amlag J.O., Aravkin A.Y., Bang-Jensen B.L., Bertolacci G.J., Bloom S.S., Castellano R., Castro E., Chakrabarti S., Chattopadhyay J., Cogen R.M., Collins J.K., Dai X., Dangel W.J., Dapper C., Deen A., Erickson M., Ewald S.B., Flaxman A.D., Frostad J.J., Fullman N., Giles J.R., Giref A.Z., Guo G., He J., Helak M., Hulland E.N., Idrisov B., Lindstrom A., Linebarger E., Lotufo P.A., Lozano R., Magistro B., Malta D.C., Månsson J.C., Marinho F., Mokdad A.H., Monasta L., Naik P., Nomura S., O'Halloran J.K., Ostroff S.M., Pasovic M., Penberthy L., Reiner Jr R.C., Reinke G., Ribeiro A.L.P., Sholokhov A., Sorensen R.J.D., Varavikova E., Vo A.T., Walcott R., Watson S., Wiysonge C.S., Zigler B., Hay S.I., Vos T., Murray C.J.L., Whiteford H.A., Ferrari A.J. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. 2021;398:1700–1712. doi: 10.1016/S0140-6736(21)02143-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tandon R. The bitter lessons of COVID-19: acknowledging and working through many points of tension. Asian J. Psychiatry. 2021;55 doi: 10.1016/j.ajp.2021.102545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor S. Understanding and managing pandemic-related panic buying. J. Anxiety Disord. 2021;78 doi: 10.1016/j.janxdis.2021.102364. [DOI] [PubMed] [Google Scholar]
- Zhang X., Zhang W., Chen S. Shanghai's life-saving efforts against the current omicron wave of the COVID-19 pandemic. Lancet. 2022;399:2011–2012. doi: 10.1016/S0140-6736(22)00838-8. [DOI] [PMC free article] [PubMed] [Google Scholar]