Abstract
Obesity has been recently identified as a predisposing factor for a worse prognosis in viral illnesses such as SARS-CoV-2; however, its role in children with influenza is not yet clarified. The current systematic review and meta-analysis aims to assess whether obesity is a risk factor for either hospitalization or a worse prognosis when hospitalized among children infected by influenza. We systematically searched the following databases using a structured algorithm: MEDLINE, Clinicaltrials.gov, and Cochrane Central Register of Controlled Trials (CENTRAL). Statistical meta-analysis was performed using the “meta” package in R software, and included studies were evaluated using the Newcastle–Ottawa scale. Among children with influenza, obesity increased the odds of hospitalization with a pooled OR of 1.89 (95% CI [1.23, 2.9], I2 = 0, p = 0.003). When hospitalized, children with obesity were also more likely to have a worse outcome than their healthy-weight counterparts, with a pooled OR of 1.24 (95% Cl [1.02; 1.51], I2 = 11, p = 0.03). In an effort to lower heterogeneity, a leave-one-out meta-analysis was conducted. Publication bias was assessed with the visual inspection of funnel plots and the trim-and-fill method. Certainty assessment was evaluated using the GRADE score.
Conclusions: The findings of our meta-analysis suggest that obesity in children with influenza is associated with a worse prognosis, both hospitalization and ICU admission/death.
|
What is Known: • Obesity has been identified as a risk factor for non-communicable as well as communicable diseases. • A previous meta-analysis failed to demonstrate a statistically significant association between obesity and influenza infection severity. | |
|
What is New: • Children with high BMI and influenza infection are more likely to get hospitalized. • Pediatric inpatients with increased BMI and influenza infection may have a worse prognosis. |
Supplementary Information
The online version contains supplementary material available at 10.1007/s00431-022-04689-0.
Keywords: Obesity, Influenza, Risk factor, Hospitalization
Introduction
Rationale
An important finding during the SARS-CoV-2 pandemic is that obesity may be an independent risk factor for severe COVID-19 in children and young people [1, 2]. At the same time, we have learned about the exponential rise in childhood obesity (MMWR 21) due to prolonged quarantine measures that may consequently lead to a vicious circle of severe viral respiratory infections in children [3].
Recent translational research shows the inflammatory nature of excess adipose tissue that secretes cytokines and alters immune regulation in favor of the invading viruses. Maria Smith et al., in an attempt to explain the impact of obesity on influenza and coronavirus pathogenetic mechanisms, highlight, among others, the role of leptin resistance and lipotoxicity as well as the suppression of interferon induction and cytokine production in infected rodents and human hosts which may dampen their innate and adaptive immune responses [4]. In addition to childhood obesity’s pro-inflammatory effects, mechanical as well as functional alterations on lung physiology have been highlighted, most commonly reduced lung compliance and abnormalities in lung volumes such as lower functional residual capacity (FRC) and FEV1/FVC ratios [5, 6].
As influenza infection still remains a major cause of morbidity among pediatric patients in Europe [7] and childhood obesity is reaching epidemic proportions [8], we aimed to revisit the literature concerning children with obesity infected with the influenza virus. In this regard, the most recent meta-analysis performed by Gill et al. [9] did not demonstrate a statistically significant relationship between childhood obesity and influenza-related complications, as opposed to other comorbidities. However, the numbers of patients included in the meta-analysis were considerably low to extract firm conclusions regarding the outcome of interest.
Objectives
In the current systematic review and meta-analysis, we aim to evaluate the association of obesity with influenza infection among pediatric patients.
Methods
Protocols and registration
The protocol of the present study has been registered in PROSPERO on the 6th of April 2022 (CRD42022315121).
Study design (eligibility criteria)
The current systematic review and meta-analysis is written according to the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines [10]. The PRISMA checklist is presented in Supplementary Fig. 1. Every single study reporting data on children with obesity infected by influenza and disease severity was deemed eligible for inclusion. The study selection process was done in three consecutive steps. At first, the titles and abstracts of all search results were investigated and evaluated for relevance. The second step included full-text access to studies potentially suitable for inclusion. Finally, studies meeting our inclusion criteria were included in the systematic review, and studies reporting their results in an appropriate manner (i.e., quantitative) were included in the meta-analysis. Review articles, animal studies, and non-comparative studies (case reports, case series) were excluded. Any disagreement between the authors on the methodological approach, the retrieval of articles, and the statistical analysis was resolved through the consensus of all authors.
Inclusion criteria
Children and adolescents (CYA) less than 18 years old diagnosed with influenza infection or influenza-like illness during a period of known influenza circulation admitted in hospital settings or high dependency unit/intensive care unit (ICU).
Since childhood obesity prevalence is estimated to be 19,3% in the USA and 4 to 20% and 6 to 28% for girls and boys, respectively, in Europe, studies with a low obesity prevalence of less than 1% were excluded from the study [11, 12].
Literature search and data collection (information sources, search strategy, selection process, data collection process, data items)
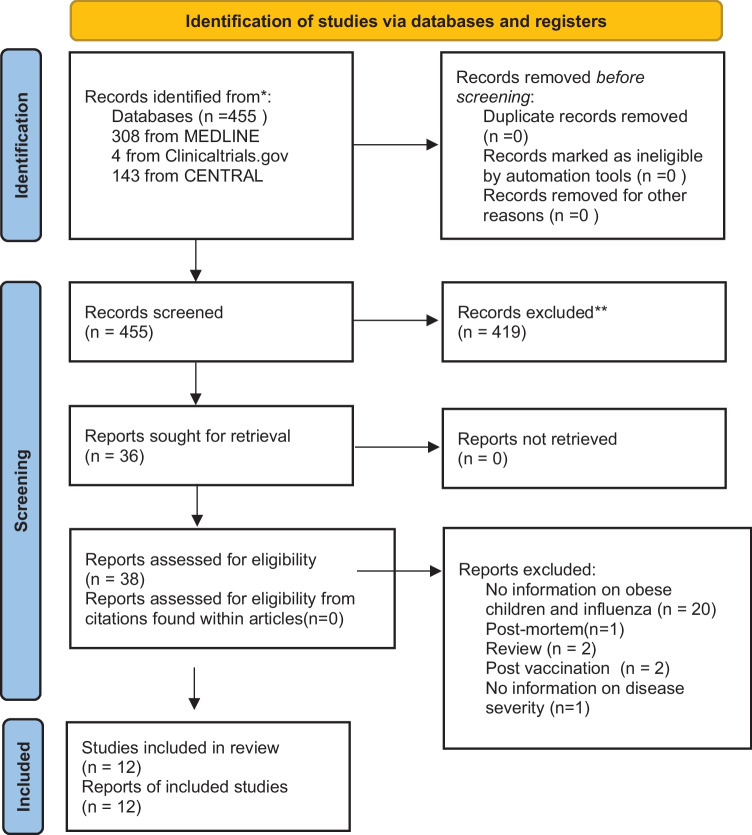
Every single study reporting data on the prognosis of children/adolescents with obesity and influenza infection was eligible for inclusion. Data on obesity was collected for the following two outcomes: (1) hospitalized influenza patients vs. non-hospitalized influenza patients and (2) ward influenza inpatients vs. ICU influenza patients or deceased patients. Two reviewers (G.P.M., D.I.V.) applied the following structured algorithm: (obesity OR BMI OR “metabolic syndrome”) AND (influenza OR “influenza-like illness” OR flu) AND (child* OR adolescent*) in the databases MEDLINE (1966–2022), Clinicaltrials.gov (2008–2022), and Cochrane Central Register of Controlled Trials (CENTRAL) (1999–2022). If necessary, the algorithm was altered and critical search terms were used instead, depending on the database interface. In order to achieve a wider assessment of the literature, in-text citations found within the included articles were manually screened (snowball method). No language or date restrictions were applied. The date of the last search was set at February 17, 2022. The flowchart of the literature is presented in Fig. 1. The extracted data from each study included the following: name of the first author, year of publication, study design, NOS scale evaluation, study population, country of origin, age range of the include population, month/year of enrollment, type of influenza, obesity definition, excluded populations, prevalence of obesity in the studied population, and outcome measured.
Fig. 1.
PRISMA flow diagram 2020
Study risk of bias assessment
Studies suitable for inclusion in our meta-analysis were independently evaluated by three researchers (G.P.M., D.I.V., P.K.) with the use of the Newcastle–Ottawa scale (NOS) [13]. This scale applies to nonrandomized studies and assigns stars (maximum score: 9) according to the selection of the study groups, comparability of the groups and the ascertainment of exposure (case–control) or outcome of interest (cohort studies).
Statistical analysis (effect measures, synthesis methods, reporting bias assessment)
The statistical meta-analysis was performed using the “meta” package in R software [14], and the confidence intervals (CI) were set at 95%. Heterogeneity among the included studies was substantial, according to the Cochrane Handbook [15], and therefore, the Der Simonian-Laird random effect model [16] was utilized to calculate odds ratios (OR) and 95% CI. Most included studies reported odds ratios; however, some did not but presented 2 × 2 tables from which we manually extracted odds ratios regarding our outcome of interest. As odds ratios are not normally distributed [17], we transformed them into logarithm odds ratios (logOR) in order to be able to meta-analyze them and then back-transform the final outcome into odds ratio (OR) for a better interpretation of the results. The influence of each individual study on the overall outcome was explored though leave-one-out meta-analysis; each study was consecutively omitted in order to evaluate its effect on the final estimate. Meta-regression analysis was not performed due to the fact that at least 10 studies are required in order for this analysis to be robust, according to the Cochrane Handbook [18]. Last but not least, publication bias was examined visually through funnel plots that were created together with the aid of the trim-and-fill method [19].
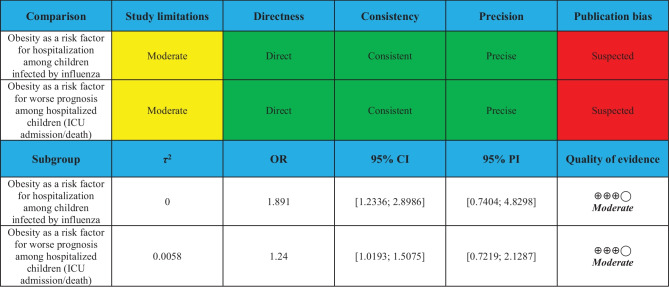
Certainty assessment
The credibility of outcomes was evaluated using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) framework (ranging from very low to high). Examination of the quality of evidence was done through the following domains: study limitations, directness, consistency, precision, and publication bias [20].
Results
Study selection and study characteristics
A total of 455 studies were screened and assessed for inclusion in the current meta-analysis (see Fig. 1). Title and abstract screening led to the exclusion of 419 studies as data for children were not specified in these studies. A total of 26 studies were excluded after the full-text assessment. Two articles were reviews and therefore provided no odds ratio measure for our outcome of interest [21, 22]. One study was performed post-mortem and therefore did not provide any valuable information [23]. Two studies provided information post-vaccination [24, 25]. Another study provided no information regarding disease severity [26]. Last but not least, 20 studies failed to provide information on children with obesity and influenza infection [27–46].
Finally, a total of 7 studies were included in the quantitative analysis [47–53]. Five more studies [54–58] were included in the qualitative analysis. Study characteristics are presented in Table 1.
Table 1.
Study characteristics of the included studies on the impact of obesity on severe influenza infection in children and adolescents
| Author, publication year | Country | Study type | Newcastle–Ottawa score (NOS) | Type of influenza (pandemic, seasonal) | Study population | Age range (in years) | Month/year of enrolment | Obesity definition | Obesity prevalence in the studied population | Excluded populations | Outcome |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Okubo et al. 2017 [47] | Japan | Retrospective | 8 | Seasonal | 27,771 patients hospitalized with bronchitis/pneumonia and influenza | 0–18 | 07/2010–03/2015 | Weight-for-length, weight-for-height and ΒΜΙ according to WHO criteria | 9.9% | Children with congenital diseases, malignancy, or autoimmune disease) | No association between obesity and likelihood of ICU admission [aOR: 1.00 95% CI (0.73–1.37); p:0.99] |
| Garcia et al. 2015 [48] | Texas | Retrospective medical record review | 6 | pH1N1 (2009) | 696 patients with laboratory-confirmed influenza infection (316 non-hospitalized: 263 ICU admitted and 116 hospitalized with ICU admission) | 0–18 | 04/2009–06/2010 | Not mentioned | 1.9% | Patients transferred from other healthcare organizations due to incomplete records | Obesity was associated with hospital admission (± ICU admission) only in the adjusted multivariate analysis [OR: 2.58, 95% Cl (0.87–7.65), p = 0.087; aOR: 3.28, 95%Cl (1.05–10.21) p = 0.04] |
| Plessa et al. 2010 [49] | Greece | Retrospective cohort | 7 | pH1N1 (2009) | 51 hospitalized children with laboratory-confirmed influenza | 0–13 | 10/2009–1/2010 | BMI ≥ 95th percentile for age and sex according to 2000 CDC charts | 16% | Not laboratory-confirmed influenza | No association between obesity and hospital admission |
| Morris et al. 2012 [50] | Canada | Retrospective | 5 | pH1N1 (2009) and seasonal | 176 inpatients with pH1N1 and 200 patients with seasonal influenza. All laboratory-confirmed cases | 0–18 | 2004–2009 | BMI ≥ 95th percentile for age and sex according to 2000 CDC charts for > 2 years old | 5,8% | Any children with influenza-like symptoms on or after the third day of admission | No association between obesity and ICU admission for pandemic [OR: 3.25, 95% CI (0.81–19.69)] [aOR: 4.18, 95% CI (0.76–22.95)] or seasonal influenza [OR: 1.14, 95% CI (0.22–5.99)] [aOR: 1.06, 95% CI (0.20–5.64)] |
| Moser et al. 2018 [51] | Mexico | Observational Cohort | 8 | Seasonal influenza and influenza-like-illness | 1530 patients with laboratory-confirmed influenza or influenza-like illness (ILI) | 0–18 | 04/2010–03/2014 | 2.0 < BMI z-score ≤ 3.0 according to WHO Child Growth standards | 6.4% | Patients in the ER > 24 h and patients with missing information | Obesity was associated with hospital admission [OR: 2.20, 95% Cl (1.32–3.74), p = 0.002] |
| Campbell et al. 2017 [52] | USA | Retrospective case–control | 6 | seasonal | 185 patients with laboratory-confirmed influenza infection and 185 healthy controls | 2–18 | 01/2010–12/2013 | BMI ≥ 95th percentile for age and sex according to 2000 CDC charts | 11.08% | Missing data and no consent | No association between obesity and hospital admission (p = 0.69) |
| Yu et al. 2011 [53] | China | Retrospective | 7 | pH1N1 (2009) | 3,577 patients hospitalized due to laboratory-confirmed influenza infection | 2–17 | 09/2009–02/2010 | BMI 95th–100th percentile in children aged 2–17 years (US criteria) or Chinese criteria | 2% | NA | Obesity was associated with ICU admission [OR: 1.34, 95% Cl (1.10–1.63); p = .004] |
| Wieching et al. 2012 [54] | Germany | Retrospective | - | pH1N1 (2009) | 94 hospitalized patients with laboratory-confirmed influenza | 0–18 | 07/2009–03/2010 | ≥ 99th percentile for age and gender | 12.7% | Hospital infections (starting > 72 h after admission) | No association between obesity and severe influenza |
| Neyer et al. 2018 [55] | USA | Retrospective chart review | - | Influenza or Influenza-like-illness | 188 hospitalized children with severe influenza complications | 2–20 | 08/2010–06/2013 | Severe obesity (BMI) | 8% | Patients with missing anthropometric data | No association between severe obesity and hospitalization or death (p = 0.61) |
| Chen et al. 2012 [56] | Taiwan | Prospective medical record review | - | pH1N1 (2009) | 61 hospitalized patients with laboratory-confirmed influenza | 0–18 | 7/2009–12/2009 | BMI ≥ 25 kg/m2 in children ≥ 2 years of age, or a body weight ≥ 95th | 6% | NA | Obesity was associated with the need for ICU care and/or death (p = 0.008) |
| Charland et al. 2013 [57] | USA | Retrospective | - | Influenza or influenza-like-illness | 3.076.699 (adults and children) | 0–18 | 2002–2008 | Not mentioned | NA | Those meeting ICD code 487 criteria and not meeting ICD 486 | A 5% increase in community childhood obesity was associated with a 25% ↑in hospitalization rate [RR:1.25, 95% CI (1.18–1.32)] |
| Ma et al. 2015 [58] | Taiwan | Retrospective | - | Seasonal | 110 hospitalized patients with laboratory-confirmed influenza infection | Median age: 2.6 (IQR, 1.0–6.3) | 8/2013–5/2014 | Age-corrected normal range of BMI released by Taiwan Health Promotion Administration | 14% | NA | No association between obesity and ICU admission (p = 0.07) |
Risk of bias in studies
NOS scale assessment outcomes are shown in Table 1. Two studies (28,5%) scored 8 stars, two studies (28,5%) scored 7 stars, two studies (28,5%) scored 6 stars, and one study (14,2%) scored 5 stars.
Results of individual studies
Qualitative synthesis
In the USA, a study [57] on seasonal influenza using data from 274 US counties showed that a 5% increase in obesity in the pediatric population was associated with a 25% (RR 1·25, 95% CI 1·18, 1·32) increase in influenza-related hospitalization rates. A chart-review study [55] of 188 children hospitalized with seasonal influenza failed to show a significant association (p = 0.61) between severe obesity status (BMI ≥ 99% for age and gender) and influenza hospitalization or death due to influenza complications.
A multicenter study [54] conducted in Germany reported on 94 children hospitalized with H1N1 (2009) pandemic influenza, 6 of which needed ICU admission. In this cohort, 12 children had a BMI greater than the 90th percentile for age and sex, of which only 1 needed ICU admission. In contrast, in Taiwan, data from 61 children hospitalized with H1N1 (2009) pandemic influenza support that obesity is a significant risk factor for a worse prognosis [56]. This was not supported by the study of Ma et al. in Taiwan, where obesity was not associated with a worse prognosis for seasonal influenza pediatric cases [58].
Quantitative synthesis
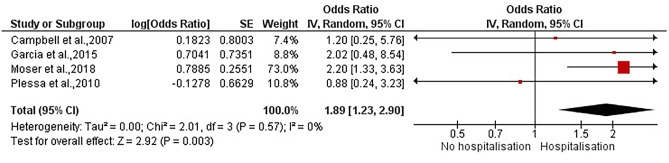
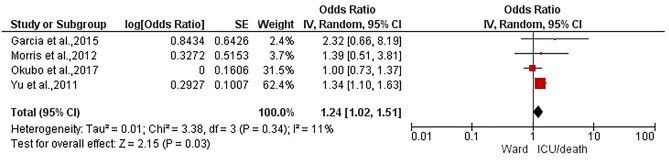
A total of 7 studies were included in the meta-analysis. The analysis regarding obesity as a risk factor for hospitalization of children with influenza infection (see Fig. 2), including 4 studies [48, 49, 51, 52], led to a statistically significant association of children with obesity and hospitalization with a pooled OR 1.89 (95% CI [1.23, 2.9], I2 = 0, p = 0.003). In addition, the analysis regarding obesity as a risk factor for a worse outcome after hospitalization (see Fig. 3), which included 4 studies [47, 48, 50, 53], showed a statistically significant association with a pooled OR equal to 1.24 (95% CI [1.02; 1.51], I2 = 11, p = 0.03).
Fig. 2.
Forest plot of the analysis regarding obesity as a risk factor for hospitalization of children with influenza infection
Fig. 3.
Forest plot of the analysis regarding obesity as a risk factor for poor prognosis after hospitalization
Results of syntheses
Leave-one-out meta-analysis
The leave-one-out meta-analysis is presented in Table 2. Regarding the outcome of poor prognosis among children with obesity already hospitalized, the sequential omission of each study provided estimates that ranged from 1.2254 (95% CI [0.9376; 1.6015] I2 = 40.1%) to 1.0756 (95% CI [0.8029; 1.4407] I2 = 0).
Table 2.
Leave-one-out meta-analysis
| Odds ratio (OR) | 95% CI | p-value | τ2 | τ | I2 | |
|---|---|---|---|---|---|---|
| Obesity as a risk factor for worse prognosis among hospitalized children infected by influenza | ||||||
| Garcia et al., 2015 | 1.2183 | [0.9934; 1.4942] | 0.0579 | 0.0071 | 0.0841 | 17.8% |
| Morris et al., 2012 | 1.2254 | [0.9376; 1.6015] | 0.1366 | 0.0225 | 0.1501 | 40.1% |
| Okubo et al., 2017 | 1.3589 | [1.1221; 1.6456] | 0.0017 | 0.0000 | 0.0000 | 0% |
| Yu et al., 2011 | 1.0756 | [0.8029; 1.4407] | 0.6253 | 0.0000 | 0.0000 | 0% |
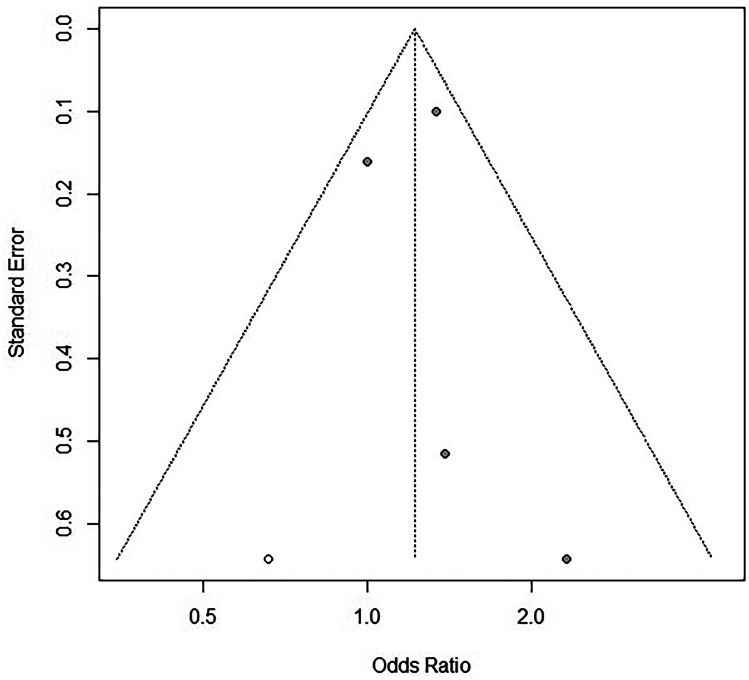
Reporting biases (publication bias)
Publication bias was evaluated with the use of funnel plots together with the aid of the trim-and-fill method. In the group regarding hospitalized and non-hospitalized children affected by Influenza, the visual inspection of the funnel plot raises high suspicion of publication bias due to its asymmetry. High suspicion of publication bias in this group is also confirmed by the trim-and-fill method as 2 missing studies were calculated (see Fig. 4). Furthermore, in the group regarding hospitalized children with influenza and children with influenza admitted to the ICU or with poor prognosis (death), the funnel plot extracted showcases a small asymmetry. Finally, this asymmetry (suspicion of publication bias) is also confirmed by the trim-and-fill method, as one missing study was calculated (see Fig. 5).
Fig. 4.
Funnel plot of the analysis regarding obesity as a risk factor for hospitalization
Fig. 5.
Funnel plot of the analysis regarding obesity as a risk factor for poor prognosis after hospitalization
Certainty of evidence
The certainty of the evidence was moderate. Publication bias was suspected in both outcomes due to the calculation of missing studies from the trim-and-fill method. Finally, there were no major concerns with the directness, precision, and consistency domains in all outcomes. The GRADE approach is presented in Table 3.
Table 3.
GRADE
Discussion
Childhood obesity has been associated with chronic low-grade systemic inflammation as well as a dysregulated immune response due to alterations caused by adaptive and innate immunity [59, 60]. This dysregulation of the immune system consists of an imbalance of cytokines, adipokines, immune cell subsets, and humoral factors that circulate in the excess adipose tissue [59] and has been linked with vulnerability to a variety of infectious diseases in addition to chronic non-communicable diseases [61]. Moreover, it was during the 2009 (H1N1) influenza A pandemic when obesity was first recognized as an independent risk factor for worse clinical outcomes in adults but evidence in children and young people remained scarce.
In this regard, a previous meta-analysis published in 2015 exploring possible risk factors for influenza-related complications and hospital admission, including 1782 children, reported that obesity was not a risk factor. However, the percentage of children with obesity was strikingly low (93 children) [7].
Another systematic review conducted by Mertz et al. including more than 60,000 adult and pediatric participants reveals that the evidence supporting risk factors for severe outcomes of influenza infection “ranged from being limited to absent.” In particular, data on influenza infection outcome specific for children with obesity have not been provided. In contrast, the risk for children and adults with obesity has been estimated as a cumulative odds ratio as high as 2.77 for mortality (95%CI 1.90, 4.05) for pandemic influenza and 2.04 (95%CI 1.74, 2.39) for seasonal influenza, respectively. Finally, the authors suggest that the level of evidence was low for the specific outcome due to lack of power and lack of adjustment but not very low compared to other risk factors investigated.
Finally, Fezeu and colleagues conducted a systematic review and meta-analysis in order to explore whether obesity is linked to a higher likelihood of ICU admission or death in adult and pediatric patients with the 2009 pandemic influenza A (H1N1). The results of the sole study comprising of (59) pediatric patients [62] showed a 3.5-fold non-significant increase in the likelihood risk of ICU admission (OR: 3.50, 95%CI: 0.66–18.43) when patients had a BMI of more than 30 kg/m2.
In our meta-analysis, obesity was found to be a risk factor for hospitalization as CYA infected with influenza were 89% more likely to be hospitalized (OR:1.89 (95% CI [1.23, 2.9], I2 = 0, p = 0.003), and already hospitalized patients with obesity were 24% (OR:1.24) more likely to have a worse prognosis in a statistically significant manner (95% CI [1.02;1.51], I2 = 11, p = 0.03). Leave-one-out meta-analysis was performed only in the group studying obesity as a risk factor for hospitalization and led to the lowering of I2 to 0%. In addition, concerning both outcomes, there seems to be high suspicion of publication bias using both the visual inspection of funnel plots and the aid of the trim-and-fill method. Finally, the certainty assessment was moderate, mainly due to publication bias suspicion.
Strengths and limitations
This meta-analysis assessed whether obesity is a risk factor for hospitalization and whether it leads to an unfavorable outcome for hospitalized children. All databases were accessed using a structured algorithm, and therefore, strict inclusion criteria were met. Since most of the included studies were cohort studies, selection bias was eliminated. In the outcome regarding hospitalization, heterogeneity was non-existent, and in the outcome regarding worse prognosis, we managed to lower the inter-study heterogeneity with the aid of the leave-one-out meta-analysis. Ultimately, our publication bias evaluation was thorough, and it managed to present a high suspicion of publication bias through the trim-and-fill method.
The main limitation of this meta-analysis is that the results are based mostly upon crude odds ratios, which can lead to an overestimation of the true risk [63]. Moreover, the studies included are observational, implying that data were extracted in a non-standardized manner and underreporting may have occurred, introducing bias in the meta-analysis. Additionally, the quality of studies was not within the strengths of this meta-analysis, and our results describe a high suspicion of publication bias.
Finally, BMI z-scores and percentiles seem to be weakly associated with true adiposity in children [64]; thus, in most studies, BMI categories may not reflect the relevant immune dysfunction caused by obesity. The definition of obesity also varied between studies in the qualitative synthesis, limiting the ability to analyze the data.
Implications for practice and future research
Our meta-analysis shows a higher likelihood of severe influenza infection among children and adolescents with obesity. Policymakers and clinical practitioners may consider obesity among the risk factors for severe influenza when drawing preventive or therapeutic strategies including vaccination and prompt antiviral treatment. Furthermore, given the logarithmic rise of childhood obesity and morbid obesity in the SARS-CoV-2 pandemic era, public health policies should attempt to fight the obesity epidemic in order to counteract the unfavorable outcomes of viral infections in children. We believe our meta-analysis adds important clinical data on the management of obese children with influenza infection.
Conclusion
Our findings suggest that among children with influenza infection, children with obesity are at an increased risk of hospitalization or worse prognosis when hospitalized than their healthy-weight counterparts. For future research, to better evaluate the risk of children with obesity and influenza infection in the community, larger prospective cohort studies with well-defined obese populations are needed.
Registration and protocol
CRD42022315121.
Supplementary Information
Below is the link to the electronic supplementary material.
Abbreviations
- MMWR
Morbidity and mortality weekly report
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- CYA
Children and adolescents
- ICU
Intensive care unit
- NOS
Newcastle-Ottawa scale
- CI
Confidence intervals
- OR
Odds ratio
- GRADE
Grading of Recommendations Assessment, Development and Evaluation
- RR
Risk ratio
- BMI
Body mass index
Author contribution
Dimitra-Irinna Vitoratou: study design, data curation, formal analysis, investigation, visualization, writing – original draft, writing – review and editing. Gerasimos-Panagiotis Milas: data curation, formal analysis, investigation, methodology, software, validation, visualization, writing – original draft, writing – review and editing. Paraskevi Korovessi: writing – review and editing, supervision. Stavroula Kostaridou: writing – review and editing, supervision. Patra Koletsi: conceptualization, study design, supervision, validation, writing – original draft, writing – review and editing.
Availability of data and material
Not applicable.
Code availability
Not applicable.
Declarations
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Tsankov BK, Allaire JM, Irvine MA, et al. Severe COVID-19 infection and pediatric comorbidities: a systematic review and meta-analysis. Int J Infect Dis. 2021;103:246–256. doi: 10.1016/J.IJID.2020.11.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kompaniyets L, Goodman AB, Belay B et al (2021) Body mass index and risk for COVID-19-related hospitalization, intensive care unit admission, invasive mechanical ventilation, and death - United States, March-December 2020. MMWR Morb Mortal Wkly Rep 70:355–361. 10.15585/MMWR.MM7010E4 [DOI] [PMC free article] [PubMed]
- 3.Lange SJ, Kompaniyets L, Freedman DS et al (2021) Longitudinal trends in body mass index before and during the COVID-19 pandemic among persons aged 2–19 years — United States, 2018–2020. MMWR Morb Mortal Wkly Rep 70:1278–1283. 10.15585/MMWR.MM7037A3 [DOI] [PMC free article] [PubMed]
- 4.Smith M, Honce R, Schultz-Cherry S (2020) Metabolic syndrome and viral pathogenesis: lessons from influenza and coronaviruses. J Virol 94:. 10.1128/JVI.00665-20/ASSET/0A33F693-06C6-4157-9A4A-FAAB4DABB07D/ASSETS/GRAPHIC/JVI.00665-20-F0001.JPEG [DOI] [PMC free article] [PubMed]
- 5.Robinson PD. Obesity and its impact on the respiratory system. Paediatr Respir Rev. 2014;15:219–226. doi: 10.1016/J.PRRV.2014.06.003. [DOI] [PubMed] [Google Scholar]
- 6.Bhammar DM, Babb TG (2021) Effects of obesity on the oxygen cost of breathing in children. Respir Physiol Neurobiol 285:. 10.1016/J.RESP.2020.103591 [DOI] [PMC free article] [PubMed]
- 7.Villani L, D’Ambrosio F, Ricciardi R et al (2022) Seasonal influenza in children: costs for the health system and society in Europe. Influenza Other Respi Viruses. 10.1111/IRV.12991 [DOI] [PMC free article] [PubMed]
- 8.Obesity and overweight. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight. Accessed 6 June 2022
- 9.Gill PJ, Ashdown HF, Wang K, et al. Identification of children at risk of influenza-related complications in primary and ambulatory care: a systematic review and meta-analysis. Lancet Respir Med. 2015;3:139–149. doi: 10.1016/S2213-2600(14)70252-8. [DOI] [PubMed] [Google Scholar]
- 10.Page MJ, McKenzie JE, Bossuyt PM et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372. 10.1136/BMJ.N71 [DOI] [PMC free article] [PubMed]
- 11.Products - Health E Stats - Prevalence of overweight, obesity, and severe obesity among children and adolescents aged 2–19 years: United States, 1963–1965 Through 2017–2018. https://www.cdc.gov/nchs/data/hestat/obesity-child-17-18/obesity-child.htm. Accessed 6 June 2022
- 12.WHO/Europe | Nutrition - WHO European Childhood Obesity Surveillance Initiative (COSI) report on the fourth round of data collection, 2015–2017 (2021). https://www.euro.who.int/en/health-topics/disease-prevention/nutrition/activities/who-european-childhood-obesity-surveillance-initiative-cosi/cosi-publications/who-european-childhood-obesity-surveillance-initiative-cosi-report-on-the-fourth-round-of-data-collection,-20152017-2021. Accessed 6 June 2022
- 13.Ottawa Hospital Research Institute. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 6 June 2022
- 14.Schwarzer G, Carpenter JR, Rücker G (2015) Meta-analysis with R. 10.1007/978-3-319-21416-0
- 15.Cochrane Handbook for Systematic Reviews of Interventions | Cochrane Training. https://training.cochrane.org/handbook/current. Accessed 6 June 2022
- 16.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 17.Bland JM, Altman DG. Statistics notes. The odds ratio. BMJ. 2000;320:1468. doi: 10.1136/BMJ.320.7247.1468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.9.6.4 Meta-regression. https://handbook-5-1.cochrane.org/chapter_9/9_6_4_meta_regression.htm. Accessed 6 June 2022
- 19.Shi L, Lin L, Omboni S (2019) The trim-and-fill method for publication bias: practical guidelines and recommendations based on a large database of meta-analyses. Med (United States) 98. 10.1097/MD.0000000000015987 [DOI] [PMC free article] [PubMed]
- 20.Balshem H, Helfand M, Schünemann HJ, et al. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol. 2011;64:401–406. doi: 10.1016/j.jclinepi.2010.07.015. [DOI] [PubMed] [Google Scholar]
- 21.Honce R, Schultz-Cherry S (2019) Influenza in obese travellers: increased risk and complications, decreased vaccine effectiveness. J Travel Med 26. 10.1093/JTM/TAZ020 [DOI] [PMC free article] [PubMed]
- 22.Mertz D, Kim TH, Johnstone J et al (2013) Populations at risk for severe or complicated influenza illness: systematic review and meta-analysis. BMJ 347. 10.1136/BMJ.F5061 [DOI] [PMC free article] [PubMed]
- 23.Gill JR, Sheng ZM, Ely SF, et al. Pulmonary pathologic findings of fatal 2009 pandemic influenza A/H1N1 viral infections. Arch Pathol Lab Med. 2010;134:235–243. doi: 10.5858/134.2.235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kainth MK, Fishbein JS, Aydillo T et al (2022) Obesity and metabolic dysregulation in children provide protective influenza vaccine responses. Viruses 14. 10.3390/V14010124 [DOI] [PMC free article] [PubMed]
- 25.Smit MA, Wang HL, Kim E, et al. Influenza vaccine is protective against laboratory-confirmed influenza in obese children. Pediatr Infect Dis J. 2016;35:440–445. doi: 10.1097/INF.0000000000001029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kim CO, Nam CM, Lee DC, et al. Is abdominal obesity associated with the 2009 influenza A (H1N1) pandemic in Korean school-aged children? Influenza Other Respi Viruses. 2012;6:313–317. doi: 10.1111/J.1750-2659.2011.00318.X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tramuto F, Restivo V, Costantino C, et al. Surveillance data for eight consecutive influenza seasons in Sicily, Italy. Am J Trop Med Hyg. 2019;101:1232–1239. doi: 10.4269/AJTMH.19-0059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tempia S, Walaza S, Moyes J et al (2017) Risk factors for influenza-associated severe acute respiratory illness hospitalization in South Africa, 2012-2015. Open forum Infect Dis 4. 10.1093/OFID/OFW262 [DOI] [PMC free article] [PubMed]
- 29.Risk Factors for Complicated Influenza A (H1N1) 2009 disease in children - PubMed. https://pubmed.ncbi.nlm.nih.gov/23771110/. Accessed 7 June 2022 [PubMed]
- 30.Gilca R, de Serres G, Boulianne N, et al. Risk factors for hospitalization and severe outcomes of 2009 pandemic H1N1 influenza in Quebec, Canada. Influenza Other Respi Viruses. 2011;5:247–255. doi: 10.1111/J.1750-2659.2011.00204.X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Guerrisi C, Ecollan M, Souty C et al (2019) Factors associated with influenza-like-illness: a crowdsourced cohort study from 2012/13 to 2017/18. BMC Public Health 19. 10.1186/S12889-019-7174-6 [DOI] [PMC free article] [PubMed]
- 32.Jain S, Kamimoto L, Bramley AM, et al. Hospitalized patients with 2009 H1N1 influenza in the United States, April-June 2009. N Engl J Med. 2009;361:1935–1944. doi: 10.1056/NEJMOA0906695. [DOI] [PubMed] [Google Scholar]
- 33.Louie JK, Acosta M, Winter K, et al. Factors associated with death or hospitalization due to pandemic 2009 influenza A(H1N1) infection in California. JAMA. 2009;302:1896–1902. doi: 10.1001/JAMA.2009.1583. [DOI] [PubMed] [Google Scholar]
- 34.Poeppl W, Hell M, Herkner H, et al. Clinical aspects of 2009 pandemic influenza A (H1N1) virus infection in Austria. Infection. 2011;39:341–352. doi: 10.1007/S15010-011-0121-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Poulakou G, Souto J, Balcells J, et al. First influenza season after the 2009 pandemic influenza: characteristics of intensive care unit admissions in adults and children in Vall d’Hebron Hospital. Clin Microbiol Infect. 2012;18:374–380. doi: 10.1111/J.1469-0691.2011.03617.X. [DOI] [PubMed] [Google Scholar]
- 36.Muscatello DJ, Barr M, Thackway SV, Raina Macintyre C. Epidemiology of influenza-like illness during pandemic (H1N1) 2009, New South Wales, Australia. Emerg Infect Dis. 2011;17:1240–1247. doi: 10.3201/EID1707.101173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Metabolic syndrome as an independent risk factor of hypoxaemia in influenza A (H1N1) 2009 pandemic - PubMed. https://pubmed.ncbi.nlm.nih.gov/27367322/. Accessed 7 June 2022 [PubMed]
- 38.Halvorson EE, Peters TR, Skelton JA, et al. Is weight associated with severity of acute respiratory illness? Int J Obes (Lond) 2018;42:1582–1589. doi: 10.1038/S41366-018-0044-Y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Suryaprasad A, Redd JT, Hancock K, et al. Severe acute respiratory infections caused by 2009 pandemic influenza A (H1N1) among American Indians–southwestern United States, May 1-July 21, 2009. Influenza Other Respi Viruses. 2013;7:1361–1369. doi: 10.1111/IRV.12123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ribeiro AF, Pellini ACG, Kitagawa BY et al (2015) Risk factors for death from Influenza A(H1N1)pdm09, State of São Paulo, Brazil, 2009. PLoS One 10. 10.1371/JOURNAL.PONE.0118772 [DOI] [PMC free article] [PubMed]
- 41.Nordstrand SEH, Juvodden HT, Viste R et al (2020) Obesity and other medical comorbidities among NT1 patients after the Norwegian H1N1 influenza epidemic and vaccination campaign. Sleep 43. 10.1093/SLEEP/ZSZ277 [DOI] [PubMed]
- 42.Murphy R, Fragaszy EB, Hayward AC, Warren-Gash C. Investigating obesity as a risk factor for influenza-like illness during the 2009 H1N1 influenza pandemic using the Health Survey for England. Influenza Other Respi Viruses. 2017;11:66–73. doi: 10.1111/IRV.12420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kool JL, Pavlin BI, Musto J, Dawainavesi A (2013) Influenza surveillance in the Pacific Island countries and territories during the 2009 pandemic: an observational study. BMC Infect Dis 13. 10.1186/1471-2334-13-6 [DOI] [PMC free article] [PubMed]
- 44.Hedberg P, Karlsson Valik J, Van Der Werff S, et al. Clinical phenotypes and outcomes of SARS-CoV-2, influenza, RSV and seven other respiratory viruses: a retrospective study using complete hospital data. Thorax. 2022;77:1–10. doi: 10.1136/THORAXJNL-2021-216949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Grgić S, Čeljuska-Tošev E, Nikolić J et al (2019) Pandemic influenza A (H1N1) 2009 presenting as a mild disease in children in a Croatian clinical centre. Acta Clin Croat 58:421–429. 10.20471/ACC.2019.58.03.04 [DOI] [PMC free article] [PubMed]
- 46.Pawlińska-Chmara R, Wronka I (2007) Assessment of the effect of socioeconomic factors on the prevalence of respiratory disorders in children. J Physiol Pharmacol.58 Suppl 5(Pt 2):523–529. https://pubmed.ncbi.nlm.nih.gov/18204166/. Accessed 7 June 2022 [PubMed]
- 47.Okubo Y, Michihata N, Uda K, et al. Dose-response relationship between weight status and clinical outcomes in pediatric influenza-related respiratory infections. Pediatr Pulmonol. 2018;53:218–223. doi: 10.1002/PPUL.23927. [DOI] [PubMed] [Google Scholar]
- 48.Garcia MN, Philpott DC, Murray KO, et al. Clinical predictors of disease severity during the 2009–2010 A(HIN1) influenza virus pandemic in a paediatric population. Epidemiol Infect. 2015;143:2939–2949. doi: 10.1017/S0950268815000114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Plessa E, Diakakis P, Gardelis J, et al. Clinical features, risk factors, and complications among pediatric patients with pandemic influenza A (H1N1) Clin Pediatr (Phila) 2010;49:777–781. doi: 10.1177/0009922810368558. [DOI] [PubMed] [Google Scholar]
- 50.Morris SK, Parkin P, Science M et al (2012) A retrospective cross-sectional study of risk factors and clinical spectrum of children admitted to hospital with pandemic H1N1 influenza as compared to influenza A. BMJ Open 2. 10.1136/BMJOPEN-2011-000310 [DOI] [PMC free article] [PubMed]
- 51.Moser JAS, Galindo-Fraga A, Ortiz-Hernández AA, et al. Underweight, overweight, and obesity as independent risk factors for hospitalization in adults and children from influenza and other respiratory viruses. Influenza Other Respi Viruses. 2019;13:3–9. doi: 10.1111/IRV.12618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Campbell MS, Gregory SW, Weaver AL, Mara KC, Kumar S, Boyce TG (2017) Impact of Asthma on the Association between Childhood Obesity and Influenza. JSM Allergy Asthma 2(2). https://pubmed.ncbi.nlm.nih.gov/34396052/. Accessed 7 June 2022 [PMC free article] [PubMed]
- 53.Yu H, Feng Z, Uyeki TM, et al. Risk factors for severe illness with 2009 pandemic influenza A (H1N1) virus infection in China. Clin Infect Dis. 2011;52:457–465. doi: 10.1093/CID/CIQ144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wieching A, Benser J, Kohlhauser-Vollmuth C et al (2012) Clinical characteristics of pediatric hospitalizations associated with 2009 pandemic influenza A (H1N1) in Northern Bavaria, Germany. BMC Res Notes 5. 10.1186/1756-0500-5-304 [DOI] [PMC free article] [PubMed]
- 55.Neyer VL, Woo JG, Siegel RM. Severe obesity in children may not pose independent risk for influenza complications. J Pediatr Nurs. 2018;42:21–24. doi: 10.1016/J.PEDN.2018.05.009. [DOI] [PubMed] [Google Scholar]
- 56.Chen WH, Lu CY, Shao PL, et al. Risk factors of severe novel influenza A (H1N1) infections in hospitalized children. J Formos Med Assoc. 2012;111:421–426. doi: 10.1016/J.JFMA.2011.06.015. [DOI] [PubMed] [Google Scholar]
- 57.Charland KM, Buckeridge DL, Hoen AG, et al. Relationship between community prevalence of obesity and associated behavioral factors and community rates of influenza-related hospitalizations in the United States. Influenza Other Respi Viruses. 2013;7:718–728. doi: 10.1111/IRV.12019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ma HY, Wu JL, Lu CY, et al. Risk factors associated with severe influenza virus infections in hospitalized children during the 2013 to 2014 season. J Microbiol Immunol Infect. 2016;49:387–393. doi: 10.1016/J.JMII.2015.05.015. [DOI] [PubMed] [Google Scholar]
- 59.Fang X, Henao-Mejia J, Henrickson SE. Obesity and immune status in children. Curr Opin Pediatr. 2020;32:805–815. doi: 10.1097/MOP.0000000000000953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Magrone T, Jirillo E (2015) Childhood obesity: immune response and nutritional approaches. Front Immunol 6. 10.3389/FIMMU.2015.00076 [DOI] [PMC free article] [PubMed]
- 61.Pugliese G, Liccardi A, Graziadio C, et al. Obesity and infectious diseases: pathophysiology and epidemiology of a double pandemic condition. Int J Obes (Lond) 2022;46:449–465. doi: 10.1038/S41366-021-01035-6. [DOI] [PubMed] [Google Scholar]
- 62.O’Riordan S, Barton M, Yau Y, et al. Risk factors and outcomes among children admitted to hospital with pandemic H1N1 influenza. CMAJ. 2010;182:39–44. doi: 10.1503/CMAJ.091724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Knol MJ, Le Cessie S, Algra A, et al. Overestimation of risk ratios by odds ratios in trials and cohort studies: alternatives to logistic regression. CMAJ. 2012;184:895–899. doi: 10.1503/CMAJ.101715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Freedman DS, Butte NF, Taveras EM, et al. BMI z-scores are a poor indicator of adiposity among 2- to 19-year-olds with very high BMIs, NHANES 1999–2000 to 2013–2014. Obesity (Silver Spring) 2017;25:739–746. doi: 10.1002/OBY.21782. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Not applicable.
Not applicable.