Abstract
Background
Simulator training is an effective way of acquiring laparoscopic skills but there remains a need to optimize teaching methods to accelerate learning. We evaluated the effect of the mental exercise ‘deconstruction into key steps’ (DIKS) on the time required to acquire laparoscopic skills.
Methods
A randomized controlled trial with undergraduate medical students was implemented into a structured curricular laparoscopic training course. The intervention group (IG) was trained using the DIKS approach, while the control group (CG) underwent the standard course. Laparoscopic performance of all participants was video-recorded at baseline (t0), after the first session (t1) and after the second session (t2) nine days later. Two double-blinded raters assessed the videos. The Impact of potential covariates on performance (gender, age, prior laparoscopic experience, self-assessed motivation and self-assessed dexterity) was evaluated with a self-report questionnaire.
Results
Both the IG (n = 58) and the CG (n = 68) improved their performance after each training session (p < 0.001) but with notable differences between sessions. Whereas the CG significantly improved their performance from t0 –t1 (p < 0.05), DIKS shortened practical exercise time by 58% so that the IG outperformed the CG from t1 -t2, (p < 0.05). High self-assessed motivation and dexterity associated with significantly better performance (p < 0.05). Male participants demonstrated significantly higher overall performance (p < 0.05).
Conclusion
Mental exercises like DIKS can improve laparoscopic performance and shorten practice times. Given the limited exposure of surgical residents to simulator training, implementation of mental exercises like DIKS is highly recommended. Gender, self-assessed dexterity, and motivation all appreciably influence performance in laparoscopic training.
Keywords: Laparoscopic skills, Teaching methods, Deconstruction into key steps, Laparoscopic course
Minimally invasive access to the abdominal cavity (laparoscopy) is the standard approach for various procedures in visceral surgery [1, 2], since patients generally experience less postoperative pain, recover faster, and have improved perioperative morbidity and mortality [3–6]. As such, the laparoscopic approach is increasingly employed for more complex surgeries including oncological procedures [7–11].
To support the safe implementation of laparoscopic approaches, early and intensive training is required [12, 13]. However, working-hour restrictions and a high administrative workload severely limit the time young surgeons spend in the operating theatre. Adequate exposure time consequently poses a major challenge to surgical education along with the development of laparoscopic skills [14, 15].
Several studies have demonstrated the efficacy of virtual and non-virtual laparoscopic simulator training for the successful transfer of acquired skills into the clinical setting [16–18]. Structured laparoscopic simulator training not only shortens operating times, but also lowers costs for resources [13, 19]. However, while laparoscopic simulators exist at universities and teaching hospitals, young surgeons usually have limited access to them [20, 21].
For laparoscopic procedures such as cholecystectomy, the risks and complications can be mitigated when adhering to a standardized procedure. The evaluated mental exercise ‘deconstruction into key steps (DIKS)’ is a teaching method which meets these needs when learning basic laparoscopic skills [22]. Here, we implemented a prospective randomized controlled trial into a curricular laparoscopic skill course to investigate whether DIKS results in a similar improvement of performance compared to prolonged time to practice. The desired outcome was to identify a method that reduces the required exposure time to a laparoscopic simulator without impairing performance outcome [15]. Additionally, the impact of various covariates including gender, age, prior laparoscopic experience, self-assessed motivation and self-assessed dexterity on laparoscopic performance was evaluated. The purpose of this covariate analysis was to identify factors that enhance /diminish laparoscopic performance sui generis.
Materials and methods
Study design and course schedule
A structured, two-session laparoscopy course was constructed as an integral part of an obligatory two-week rotation in surgery ( 10th semester students) at the Julius-Maximilians-University of Würzburg, Germany. Informed consent was obtained from all participants. The study was approved by the local ethics committee (20,170,403 01).
At baseline, participants had to complete an online questionnaire (EvaSys®) containing demographic data, previous laparoscopic expertise, self-assessment of dexterity, as well as motivation. Participants were randomly assigned to either the intervention (IG) or the control group (CG).
Performance was measured at baseline (t0), at the end of the first session (t1), and nine days later (t2). Improvement of performance was determined as the difference between t0 -t1, t1 -t2 and t0-t2 using the normalized gain equation R. [23]. where the numerator is the difference between the pre-test and the post-test, and the denominator is the maximum achievable value minus the pre-test [24].
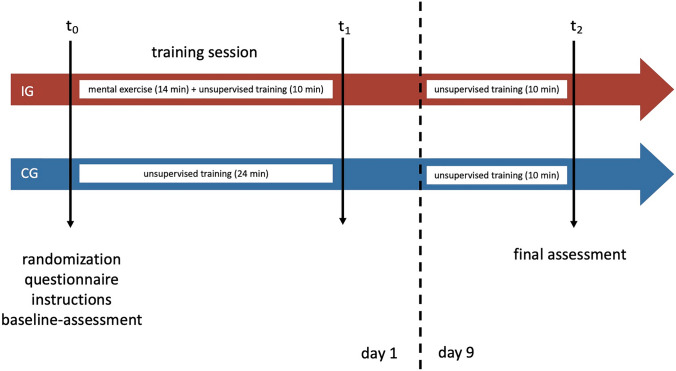
Students were trained in surgeon-camera assistant tandem pairs (Fig. 1) and standard introductory video tutorials were given to both the IG and the CG. Multimedia-based training is a valid method to teach complex motion sequences required for surgical procedures [25].
Fig. 1.
Study design and training for students in pairs
Intervention from t0-t1
The IG was instructed in using DIKS for 14 min, followed by unsupervised training for 10 min (5 min per participant in each pair). The CG spent the entire 24-min timeslot practicing laparoscopic skills using the simulator (12 min per participant in each pair). Time to practice for the IG was subsequently reduced by 58%. Participants were asked to make handwritten notes using their own words since this seems to aid with memorization [26–29]. Furthermore, the IG recorded their individual difficulties and corresponding solutions when performing the laparoscopic exercise.
Intervention from t1-t2
For IG and CG the second 10-min session (5 min per participant in each pair) was identical to the first session but was unsupervised and the IG was allowed to (re)examine their keysteps.
Performance of attending surgeons (n = 6) and surgical residents (n = 5) from the Department of Visceral Surgery, University Hospital Würzburg, Germany served as an internal validation.
Training setup
For core training, the Berlin OP trainer (BOPT) was used [30]. The video unit comprised a 30° “Autoclave” lens and a “telecam PAL” camera module with a “telepac PAL” screen from Storz (KARL STORZ SE & Co. KG, Tuttlingen, Germany). “Click line overholts" with a length of 2 cm from Storz were used as instruments. Three Trocars (Endopath Xcel (Ethicon 12 mm); Ethicon J&J Medical Devices, Norderstedt, Germany) were used in a standardized way to access the BOPT’s cavity.
Laparoscopic training and performance were assessed using the laparoscopic training module "packing suitcases". This exercise was developed and validated as an integral teaching module of the “Lübecker Toolbox” (LBT) [31]. In order to enable integration of camera assistance and corresponding interactions, dimensions were modified (scale: 25.5 cm × 27.5 cm vs. LTB 12 cm x 12 cm). The aim of the task was to place all cups in two separate cases, depending on its color. For successful completion of the task, all cups had to be placed in the correct case within five minutes and sorted in an upright position.
In order to collect the students’ personal data and their self-assessments, a questionnaire was given using the survey software EvaSys (Copyright © 2021 EvaSys GmbH, Lüneburg, Germany). All participants were video-recorded throughout the three measurement points as surgeon and camera assistant,
Performance rating
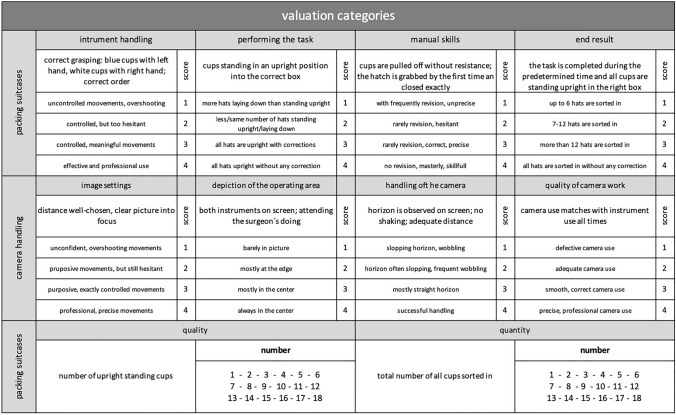
Two blinded raters evaluated the pseudonymized assessment videos using a validated evaluation sheet. The assessment checklist “competency assessment tool” (CAT) was adapted for the purposes of the present study [32] (Fig. 2). The quality of performance was defined as the number of upright cups and the quantity of performance was defined as the total number of cups positioned in the correct case regardless of whether they stand upright.
Fig. 2.
The checklist CAT to assess the laparoscopic performance
Statistics
Statistical analysis was performed using IBM SPSS 25.0, 26.0 and 27.0 (IBM SPSS, Armonk, New York, USA), R 3.6.3 (R: A language and environment for statistical computing, R Foundation for Statistical Computing, Vienna, Austria) and Mplus 7 (www.statmodel.com). Significance was set at p < 0.05. Descriptive analyses consisted of mean (MV), median, minimum (min) and maximum (max) values as well as the standard deviation (SD).
Inter-rater reliability was described by the extended percentage agreement method [33]. An agreement of 100% and a tolerance of one scale point indicated that both examiners differed by a maximum of one point for each item assessed. Reliability was calculated using the Finn coefficient, which varies between 0 and 1 [34]. A value > 0.7 was considered as good [34].
Inferential statistical analysis consisted of four steps:
The performance regardless of group membership was investigated with a repeated measure ANOVA.
Performance depending on group membership was calculated using Welch's test as well as single factor variance and analysis of covariance or as repeated measure ANOVA.
Factor analysis was performed to inspect whether individual questionnaire items could be combined to a scale. Bartletts test and the Kaiser–Meyer–Olkin coefficient (KMO coefficient) were employed to assess whether the data was suited for a factor analysis.
A latent difference model was specified to summarize the interplay of steps 1–3 [35]. A latent difference model is a structural equation modeling technique. It has been developed to conduct latent longitudinal analyses free of measurement error and is mathematically superior to results which are calculated on the manifest level. Usual fit indices (e.g. Comparative Fit Index, threshold = 0.95) were employed to assess the quality of the model.
Results
Sample
One hundred and forty-three students participated in the study. Of these, 17 (11.9%) were excluded from further analysis due to insufficient video footage, missing questionnaire entries, or drop-out.
The IG comprised 58 participants (MV: 25.8 years, female: 63.8%) and the CG 68 participants (MV: 26.0 years, female: 64.7%). The IG and CG did not differ regarding gender, age, prior laparoscopic experience and self-assessed motivation (Table 1).
Table 1.
Characteristics of IG and CG
| IG | CG | |||||
|---|---|---|---|---|---|---|
| total | SD | total | SD | p-value*2 | ||
| Participants (n) | 58 | 68 | ||||
| Gender (f/m) | 37/21 | 44/24 | 0.94*3 | |||
| Age (years) | 25.78 | ± 2.39 | 26.04 | ± 2.79 | 0.31*4 | |
| Prior laparoscopic experience (mean) | 1.72*5 | ± 0.62 | 1.64*5 | ± 0.62 | 0.22*4 | |
| Motivation (mean) | 3.38*5 | ± 1.0 | 3.21*5 | ± 1.03 | 0.10*4 | |
*1standard deviation *2group-differencese, *3chi-quadrat-test with Yates ‘continuity correction, *4 welch-test, *5 mean value of the entry questionnaire
Questionnaire evaluation and factor analysis
Only 7% of participants reported prior laparoscopic experience, e.g. during clerkships. Overall, participants were highly motivated (MV: 3.38, on a five-point-Likert-scale). Barlett’s test (p < 0.001) and KMO (0.82) confirmed suitability of the data for factor analysis and a one factor solution (self-assessed dexterity) was favored. Five items had factor loadings > 0.30 and Cronbach's alpha as a measure of internal consistency exceeded 0.6 including “manual skills”, “fine motor skills”, “steady hand”, “use manual adroitness”, and “eye-hand-coordination”.
Internal validation and inter-rater reliability
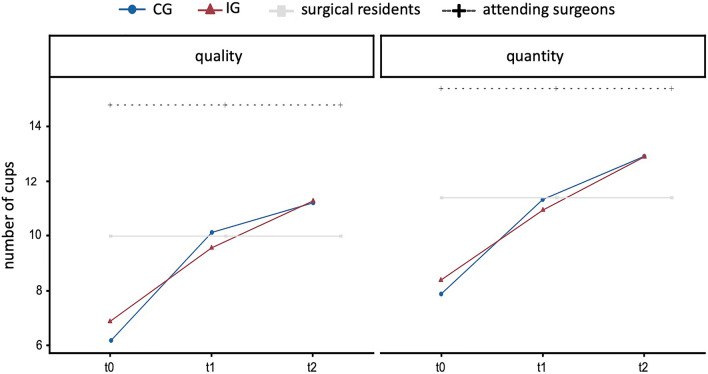
Attending surgeons and surgical residents performed “packing suitcases” solely at one time point. We used their performance as a gold standard for comparison with less experienced users. As expected, attending surgeons outperformed students in all categories (p < 0.05). Similarly, surgical residents showed significantly better performance than students (p < 0.05) in the three assessment categories of the CAT: "instrument handling", "manual skills" and "end result" (data not shown). Throughout the course, participants improved their laparoscopic skills so that their final assessment (t2) was comparable to the surgical residents in “quality” and “quantity” (Fig. 3).
Fig. 3.
Internal validation. Increase in performance of students in the control group (CG) and intervention group (IG) compared to surgical residents and attending surgeons regarding the categories “quality” and “quantity”
Extended percentage agreement was 97.2% with a tolerance of 1 scale point. The Finn coefficient was 0.72 indicating high inter-rater reliability.
Increase in performance independent of group membership
All participants increased their laparoscopic performance (in role of the surgeon and camera-assistant from t0 to the final assessment at the end of the course (t2). The effect was independent of whether participants belonged to the IG or CG (Table 2).
Table 2.
Performance of participants independent of group membership from t0 to t2
| t0 | t2 | |||||
|---|---|---|---|---|---|---|
| MV | SD | MV | SD | p-value | ||
| Packing suitcases | ||||||
| Instrument handling | 1.98 | ± 0.67 | 2.86 | ± 0.74 | < 0.001 | |
| Performing the task | 2.37 | ± 0.86 | 2.51 | ± 0.79 | Not significant (n.s.) | |
| Manual skills | 1.87 | ± 0.69 | 2.53 | ± 0.82 | < 0.001 | |
| End result | 1.85 | ± 0.46 | 2.56 | ± 0.57 | < 0.001 | |
| Camera handling | ||||||
| Image settings | 2.59 | ± 0.60 | 2.79 | ± 0.69 | < 0.05 | |
| Depiction of the operating area | 2.56 | ± 0.93 | 2.63 | ± 0.76 | n.s | |
| Handling of the camera | 2.13 | ± 0.76 | 2.30 | ± 0.68 | < 0.05 | |
| Quality of camera handling | 2.44 | ± 0.75 | 2.75 | ± 0.79 | < 0.001 | |
| Number of cups | ||||||
| Quality | 6.49* | ± 2.76 | 11.26* | ± 3.18 | < 0.001 | |
| Quantity | 8.11* | ± 2.29 | 12.91* | ± 2.63 | < 0.001 | |
*Number of cups; significance (p-value) is defined as the difference between t0 to t2
Increase in performance depending on group membership
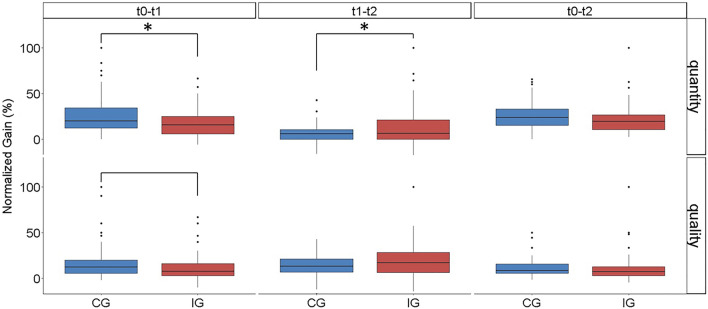
Overall the performance from baseline (t0) to final assessment (t2) did not differ. From t0 to t1, however the CG experienced a significantly higher performance increase (“quantity” and “quality”) compared to the IG, whereas the IG showed a significantly higher increase in performance from t1 to t2 (quantity) (Fig. 4).
Fig. 4.
Increase in performance given as the normalized gain of “quality” and “quantity” *p-value ≤ 0,05
Influence of covariates
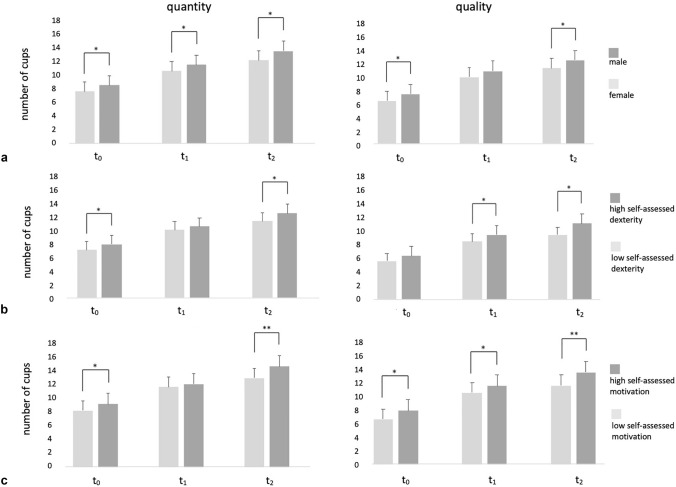
The impact of potential covariates on “quality” and “quantity” was assessed for gender, self-assessed dexterity and self-assessed motivation (Fig. 5).
Fig. 5.
Quantitative and qualitative performance at t0, t1 and t2 by a gender, b self-assessed dexterity and c self-assessed motivation, *p ≤ 0,05; **p ≤ 0,001
Gender
Gender had an impact on performance. Female participants correctly placed significantly (p < 0.05) less cups in the right case (“quantity”). Additionally, female participants showed significantly (p < 0.05) lower quality at two time-points (t0: 6.14 cups and t2: 10.85 cups) compared to their male counterparts (t0: 7.14 cups and t2: 12.00 cups).
Dexterity
Self-assessed dexterity was classified according to the calculated percentiles as "low" (0.00 to 2.60) and as "high" (3.31 to 5.00). Students, who rated themselves with high manual skills, showed better performance regarding quality from time-point t1 to t2. At baseline (t0) and the final assessment (t2), they also achieved higher scores regarding quantity.
Motivation
Self-assessed motivation was subdivided into two groups "low" and "high", based on the results of the question "I am more motivated than average on this course". This partition was made at MV 3.0 since percentile ranges were unequal. At each time point, there was a significant difference between the two groups of students. Participants who were highly motivated achieved higher quality at all time-points as well as a higher quantity at baseline (t0) and final assessment (t2).
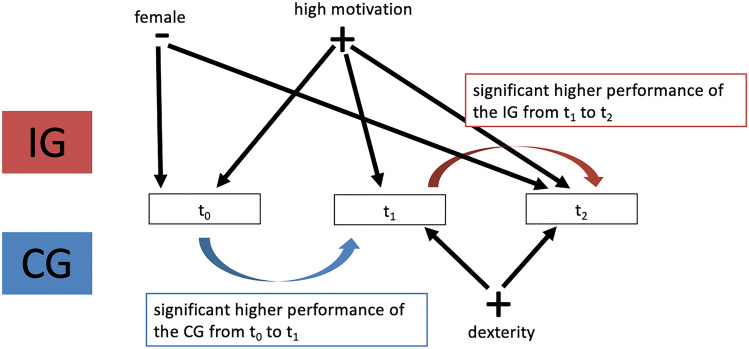
Latent difference model
A latent-difference model was used to demonstrate the relationship of the covariates, the IG and CG on performance at each time-point. The closer Lambda (λ) approaches “1” the higher the dependency between two variables. A simplified version of the latent difference model is shown in Fig. 6. To simplify the presentation, only the influence on quality (upright standing cups) is shown in the figure.
Fig. 6.
Simplified version of a latent difference model
For the covariate gender, the loading λ=0.953 was associated with significantly higher baseline performance (p < 0.05). Self-assessed motivation of the participants had a significant influence on the baseline results with λ = 1.125. Self-assessed motivation also impacted improvements in performance at time point t1 (λ = 0.732) and t2 (λ = 0.855). The CG showed a significantly higher increase in performance from t0 to t1. The IG showed a higher increase in performance from t1 to t2.
Discussion
Laparoscopic skill training
In this prospective randomized study, performance during a standardized laparoscopy course was evaluated with a focus on learning activity and potential influencing factors. In line with other studies [17, 36, 37], all participants showed a significant increase in performance throughout the course [17, 38]. Although not examined in the present study, research has shown the likelihood of laparoscopic skill transfer from training to the clinical setting [16, 39, 40] in particular the LTB technique [31, 41]. Here, a modified version integrating a mental exercise was developed and employed [33, 34]. Although a positive effect of mental exercises on learning efficiency is widely acknowledged [42], little attention has been paid to its implementation in laparoscopic training courses [43, 44].
Different proficiency levels prove internal validity
Validity of the module “packing suitcases” was investigated by analyzing performance of attending surgeons and surgical residents. As expected, attending surgeons outperformed surgical residents, who in turn were superior to laparoscopy-naïve participants at baseline. Similarly, Hassan et al. showed that different levels of competence, from professional to novice, could be differentiated when analyzing performance on a laparoscopic trainer [45]
Deconstruction into key steps
The present study evaluated whether the teaching method DIKS could decrease the required time to practice. A significant and continuous improvement in performance from baseline (t0) to the end of the course (t2) was found, independent of the teaching method. Overall, there were no significant differences between the two groups over the entire study period (t0 t1 t2). However, distinct differences in performance depending on the teaching method (IG or CG) were found to be associated with the time point of training. Increased time to practice led to a more pronounced early increase in performance (t0 to t1, p < 0.05), whereas DIKS exerted its beneficial effect on prolonged learning (t1 to t2), while practical training time was reduced by 58%.
These results confirm that at the beginning of learning a new practical skill, adequate time to practice (manual handling of instruments and cameras) results in an immediate improvement in performance. Additional mental exercises may compensate for significantly reduced time to practice. This finding is in line with previous studies which found that mental exercise in surgical training can have a positive effect on learning success and is a cost- and time-efficient strategy [42, 46–49]. One study even demonstrated that additional mental exercise such as DIKS may lead to superior results compared to practical exercise [42]. This contrasts with the concept of “see one, do one, teach one …”, which is widely used in surgery [50].
Covariates
The participants' self-assessment of dexterity significantly impacted performance. Specifically, those who rated themselves poorly showed significantly worse performance than students who were convinced of their motor skills [51].
A significant positive correlation between high self-assessed motivation and performance was also found throughout this study [52]. The extent to which teaching methods influence self-assessed motivation in medical education requires further research.
Unexpectedly, we found that gender influenced performance with male participants significantly outperforming female participants. This might be because females tend to be more concerned about making mistakes, and subsequently require greater time to complete a given task [53]. In this context, males seem to benefit from their tendency to take risks and be more self-confident [53, 54]. The difference between genders in surgical training is in line with the systematic review of Ali et al. which included 247 studies [55, 56].
Contrary to our hypothesis, camera handling did not impact operative outcomes [57]. This may be due to a methodological artifact: Surgeon and camera-assistant formed a permanent team throughout the course. Future investigations would need to include both weak and strong camera assistance with an experienced as well as an inexperienced surgeon.
Latent difference model
After analyzing all covariates, a latent-difference model was implemented to investigate inter-individual differences on a measurement-free level [58]. This model is mathematically sound in studies that consider changes over a certain period of time [58]. As expected, the latent-difference model prevented distortions and increased the informative value of the data.
Strengths and limitations
The prospective randomized design and sample size are strengths of the study. The high number of participants enabled differentiated subgroup and covariate analysis. Similar studies had significantly less participants [59, 60]. Since the study was conducted during a curricular surgical internship, highly as well as less motivated participants took part avoiding selection bias. Furthermore, the standardized setting of the course with supervision and standardized instructional videos ensured comparable settings. The performance was evaluated using a standardized evaluation sheet and a behaviorally anchored rating scale, which has been described and evaluated earlier [61].
Conclusions
We showed that novices were able to significantly improve their skills during a laparoscopic surgical course. DIKS compensated for shorter practice time and thereby proved to be a valuable tool to optimize performance outcome. Covariates such as gender, self-assessed motivation and self-assessed dexterity significantly influenced training outcome emphasizing the importance of tailored training interventions.
The aim of the study was to emphasize the importance of efficient structured laparoscopic training combined with sound psychological learning techniques. `DIKS` can be easily integrated into the daily work routine. Regardless of the career stage, complex motion sequences require elaborated educational techniques based on learning and instructional psychology. Much more research in the field of medical education needs to explore, validate and disseminate knowledge on learning and teaching professional practical skills.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Declarations
Disclosures
Priv.-Doz. Dr. med. Florian Seyfried´s basic scientific research is founded by the German research foundation DFG SE 2027/5–1. Prof. Dr. med. Armin Wiegering´s basic scientific research is founded by the German research foundation DFG WI-5037/1–4. Dr. rer. nat. Mohamed Hankir´s basic scientific research is founded by the German research foundation DFG HA 8213/3–1. Dr. med. Sven Flemming´s basic scientific research is founded by the German research foundation in DFG FL 870/2–2. Prof. Dr. med. Christoph-Thomas Germer, Prof. Dr. med. Sarah König, Priv.-Doz. Dr. med. Johan Friso Lock, Ilona Hering, Dr. med. Alexander Wierlemann, Joy Backhaus and Anna Widder have no conflicts of interest or financial ties to disclose.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
A. Widder and J. Backhaus were contributed equally to this work and share first authorship.
Contributor Information
A. Widder, Email: widder_a@ukw.de
J. Backhaus, Email: backhaus_j@ukw.de
References
- 1.Jayne D, et al. Five-year follow-up of the medical research council CLASICC trial of laparoscopically assisted versus open surgery for colorectal cancer. J British Surg. 2010;97(11):1638–1645. doi: 10.1002/bjs.7160. [DOI] [PubMed] [Google Scholar]
- 2.Fürst A, et al. Evidenzlage der laparoskopischen Chirurgie beim Rektumkarzinom. Coloproctology. 2015;37(2):97–102. [Google Scholar]
- 3.Seidelmann, Lisa Marie-Anne Martha Nena. 2016. Perioperativer Vergleich der minimalinvasiven Operationsmethoden TEP (Total Extraperitoneale Patchplastik) und TAPP (Transabdominelle Präperitoneale Patchplastik) zur Behandlung der primären einseitigen Leistenhernie: Eine Datenanalyse des Herniamed-Registers mit 17.587 Patienten
- 4.Kitano S, et al. A randomized controlled trial comparing open vs laparoscopy-assisted distal gastrectomy for the treatment of early gastric cancer: an interim report. Surgery. 2002;131(1):S306–S311. doi: 10.1067/msy.2002.120115. [DOI] [PubMed] [Google Scholar]
- 5.Hosono S, et al. Meta-analysis of short-term outcomes after laparoscopy-assisted distal gastrectomy. World J Gastroenterol. 2006;12(47):7676. doi: 10.3748/wjg.v12.i47.7676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sakuramoto S, et al. Laparoscopy versus open distal gastrectomy by expert surgeons for early gastric cancer in Japanese patients: short-term clinical outcomes of a randomized clinical trial. Surg Endosc. 2013;27(5):1695–1705. doi: 10.1007/s00464-012-2658-9. [DOI] [PubMed] [Google Scholar]
- 7.Lee H-J, et al. Short-term outcomes of a multicenter randomized controlled trial comparing laparoscopic distal gastrectomy with D2 lymphadenectomy to open distal gastrectomy for locally advanced gastric cancer (KLASS-02-RCT) Ann Surg. 2019;270(6):983–991. doi: 10.1097/SLA.0000000000003217. [DOI] [PubMed] [Google Scholar]
- 8.Korrel M, et al. Minimally invasive versus open distal pancreatectomy: an individual patient data meta-analysis of two randomized controlled trials. Pancreatology. 2020 doi: 10.1016/j.pan.2020.07.365. [DOI] [PubMed] [Google Scholar]
- 9.Masoomi H, et al. Overview of outcomes of laparoscopic and open Roux-en-Y gastric bypass in the United States. Surg Technol Inter. 2012;22:72–76. [PubMed] [Google Scholar]
- 10.Elgazwi KEZ, et al. Laparoscopic sigmoidectomy for diverticulitis: a prospective study. JSLS. 2010 doi: 10.4293/108680810X12924466008088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Biere SS, et al. Minimally invasive versus open oesophagectomy for patients with oesophageal cancer: a multicentre, open-label, randomised controlled trial. The Lancet. 2012;379(9829):1887–1892. doi: 10.1016/S0140-6736(12)60516-9. [DOI] [PubMed] [Google Scholar]
- 12.Shebrain S, et al. The role of manual dexterity and cognitive functioning in enhancing resident operative autonomy. J Surg Educ. 2019;76(6):e66–e76. doi: 10.1016/j.jsurg.2019.06.002. [DOI] [PubMed] [Google Scholar]
- 13.Aggarwal R, Moorthy K, Darzi A. Laparoscopic skills training and assessment. Br J Surg. 2004;91(12):1549–1558. doi: 10.1002/bjs.4816. [DOI] [PubMed] [Google Scholar]
- 14.Sroka G, et al. Fundamentals of laparoscopic surgery simulator training to proficiency improves laparoscopic performance in the operating room—a randomized controlled trial. Am J Surgery. 2010;199(1):115–120. doi: 10.1016/j.amjsurg.2009.07.035. [DOI] [PubMed] [Google Scholar]
- 15.Grantcharov TP, Reznick RK. Teaching procedural skills. BMJ. 2008;336(7653):1129–1131. doi: 10.1136/bmj.39517.686956.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Buckley CE, et al. Is the skillset obtained in surgical simulation transferable to the operating theatre? Am J Sur. 2014;207(1):146–157. doi: 10.1016/j.amjsurg.2013.06.017. [DOI] [PubMed] [Google Scholar]
- 17.Zendejas B, et al. State of the evidence on simulation-based training for laparoscopic surgery: a systematic review. Ann Surg. 2013;257(4):586–593. doi: 10.1097/SLA.0b013e318288c40b. [DOI] [PubMed] [Google Scholar]
- 18.Korndorffer JR, Jr, et al. Simulator training for laparoscopic suturing using performance goals translates to the operating room. J Am Coll Surg. 2005;201(1):23–29. doi: 10.1016/j.jamcollsurg.2005.02.021. [DOI] [PubMed] [Google Scholar]
- 19.Stefanidis D, et al. Initial laparoscopic basic skills training shortens the learning curve of laparoscopic suturing and is cost-effective. J Am Coll Surg. 2010;210(4):436–440. doi: 10.1016/j.jamcollsurg.2009.12.015. [DOI] [PubMed] [Google Scholar]
- 20.VanLehn K, Jones RM, Chi MT. A model of the self-explanation effect. J Learn Sci. 1992;2(1):1–59. [Google Scholar]
- 21.MacKenzie L, et al. Hierarchical decomposition of laparoscopic surgery: a human factors approach to investigating the operating room environment. Minim Invasive Ther Allied Technol. 2001;10(3):121–127. doi: 10.1080/136457001753192222. [DOI] [PubMed] [Google Scholar]
- 22.Niwa U, et al. Die laparoskopische Cholezystektomie als standardisierter Lehreingriff zur Behandlung der symptomatischen Cholezystolithiasis. Zentralblatt für Chirurgie-Zeitschrift für Allgemeine, Viszeral-, Thorax-und Gefäßchirurgie. 2013;138(02):141–142. doi: 10.1055/s-0032-1328396. [DOI] [PubMed] [Google Scholar]
- 23.Hake RR. Interactive-engagement versus traditional methods: a six-thousand-student survey of mechanics test data for introductory physics courses. Am J Phys. 1998;66(1):64–74. [Google Scholar]
- 24.Westphale S, Backhaus J, Koenig S. Quantifying teaching quality in medical education: the impact of learning gain calculation. Med Edu. 2021 doi: 10.1111/medu.14694. [DOI] [PubMed] [Google Scholar]
- 25.Pape-Koehler C, et al. Multimedia-based training on Internet platforms improves surgical performance: a randomized controlled trial. Surg Endosc. 2013;27(5):1737–1747. doi: 10.1007/s00464-012-2672-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ito R, et al. Comparison of the remembering ability by the difference between handwriting and typeface. In: Stephanidis C, Antona M, et al., editors. International Conference on Human-Computer Interaction. Cham: Springer; 2020. [Google Scholar]
- 27.Widjaja C, Sumali SS. Short-term memory comparison of students of faculty of medicine pelita harapan university batch 2015 between the handwriting and typing method. Medicinus. 2020;7(4):108–111. [Google Scholar]
- 28.Frangou S-M, et al. Can you put your finger on it? the effects of writing modality on finnish students’ recollection. Writ Syst Res. 2018;10(2):82–94. [Google Scholar]
- 29.Salame II, Thompson A. Students’ views on strategic note-taking and its impact on performance, achievement, and learning. Int J Instr. 2020;13(2):1–16. [Google Scholar]
- 30.Lauscher JC, et al. A new surgical trainer (BOPT) improves skill transfer for anastomotic techniques in gastrointestinal surgery into the operating room: a prospective randomized trial. World J Surg. 2010;34(9):2017–2025. doi: 10.1007/s00268-010-0642-x. [DOI] [PubMed] [Google Scholar]
- 31.Laubert T, et al. Conception of the Lübeck toolbox curriculum for basic minimally invasive surgery skills. Langenbecks Arch Surg. 2018;403(2):271–278. doi: 10.1007/s00423-017-1642-1. [DOI] [PubMed] [Google Scholar]
- 32.Miskovic, D. 2012 Proficiency gain and competency assessment in laparoscopic colorectal surgery. [DOI] [PubMed]
- 33.Auerswald, P.G., Das Lübecker Toolbox-‐Curriculum-‐Konzeption und Validierung eines standardisierten Trainingsprogramms für die Basisfertigkeiten der minimal-‐invasiven Chirurgie.
- 34.Spaun GO, et al. A comparison of early learning curves for complex bimanual coordination with open, laparoscopic, and flexible endoscopic instrumentation. Surg Endosc. 2010;24(9):2145–2155. doi: 10.1007/s00464-010-0913-5. [DOI] [PubMed] [Google Scholar]
- 35.Proust-Lima C, et al. Are latent variable models preferable to composite score approaches when assessing risk factors of change? Evaluation of type-I error and statistical power in longitudinal cognitive studies. Stat Methods Med Res. 2019;28(7):1942–1957. doi: 10.1177/0962280217739658. [DOI] [PubMed] [Google Scholar]
- 36.Botden SM, de Hingh IH, Jakimowicz JJ. Suturing training in augmented reality: gaining proficiency in suturing skills faster. Surg Endosc. 2009;23(9):2131–2137. doi: 10.1007/s00464-008-0240-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nagendran M, et al. Laparoscopic surgical box model training for surgical trainees with no prior laparoscopic experience. Cochrane Database of Syst Rev. 2014 doi: 10.1002/14651858.CD010479.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Thijssen AS, Schijven MP. Contemporary virtual reality laparoscopy simulators: quicksand or solid grounds for assessing surgical trainees? Am J Surg. 2010;199(4):529–541. doi: 10.1016/j.amjsurg.2009.04.015. [DOI] [PubMed] [Google Scholar]
- 39.Hyltander A, et al. The transfer of basic skills learned in a laparoscopic simulator to the operating room. Surg Endosc Other Interv Tech. 2002;16(9):1324–1328. doi: 10.1007/s00464-001-9184-5. [DOI] [PubMed] [Google Scholar]
- 40.Seymour NE, et al. Virtual reality training improves operating room performance: results of a randomized, double-blinded study. Ann Surg. 2002;236(4):458. doi: 10.1097/00000658-200210000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Esnaashari H, et al. Lübecker toolbox–ein standardisiertes trainingscurriculum für die minimalinvasive Chirurgie. Z Gastroenterol. 2011;49(08):V54. [Google Scholar]
- 42.Immenroth M, et al. Mental training in surgical education: a randomized controlled trial. Ann Surg. 2007;245(3):385. doi: 10.1097/01.sla.0000251575.95171.b3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mulla M, et al. Learning basic laparoscopic skills: a randomized controlled study comparing box trainer, virtual reality simulator, and mental training. J Surg Educ. 2012;69(2):190–195. doi: 10.1016/j.jsurg.2011.07.011. [DOI] [PubMed] [Google Scholar]
- 44.Eldred-Evans D, et al. Using the mind as a simulator: a randomized controlled trial of mental training. J Surg Educ. 2013;70(4):544–551. doi: 10.1016/j.jsurg.2013.04.003. [DOI] [PubMed] [Google Scholar]
- 45.Hassan I, et al. A virtual reality simulator for objective assessment of surgeons' laparoscopic skill Der Chirurg. Zeitschrift fur Alle Gebiete der Operativen Medizen. 2005;76(2):151–156. doi: 10.1007/s00104-004-0936-3. [DOI] [PubMed] [Google Scholar]
- 46.Arora S, et al. Development and validation of mental practice as a training strategy for laparoscopic surgery. Surg Endosc. 2010;24(1):179–187. doi: 10.1007/s00464-009-0624-y. [DOI] [PubMed] [Google Scholar]
- 47.Germanyuk A, et al. Itʼs all in your head! Einfluss des Mentalen Trainings auf den Kompetenzerwerb praktischer Fertigkeiten in der chirurgischen Lehre. Zentralblatt für Chirurgie-Zeitschrift für Allgemeine, Viszeral-, Thorax-und Gefäßchirurgie. 2019;144(06):597–605. doi: 10.1055/a-1031-9711. [DOI] [PubMed] [Google Scholar]
- 48.Rao A, Tait I, Alijani A. Systematic review and meta-analysis of the role of mental training in the acquisition of technical skills in surgery. Am J Surg. 2015;210(3):545–553. doi: 10.1016/j.amjsurg.2015.01.028. [DOI] [PubMed] [Google Scholar]
- 49.Nickel F, et al. Virtual reality training versus blended learning of laparoscopic cholecystectomy: a randomized controlled trial with laparoscopic novices. Medicine. 2015 doi: 10.1097/MD.0000000000000764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kotsis SV, Chung KC. Application of see one, do one, teach one concept in surgical training. Plast Reconstr Surg. 2013;131(5):1194. doi: 10.1097/PRS.0b013e318287a0b3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Park J, et al. Improving the intraoperative educational experience: understanding the role of confidence in the resident-attending relationship. J Surg Educ. 2019;76(5):1187–1199. doi: 10.1016/j.jsurg.2019.02.012. [DOI] [PubMed] [Google Scholar]
- 52.Kusurkar R, et al. Motivation as an independent and a dependent variable in medical education: a review of the literature. Med Teach. 2011;33(5):e242–e262. doi: 10.3109/0142159X.2011.558539. [DOI] [PubMed] [Google Scholar]
- 53.Schueneman A, Pickleman J, Freeark R. Age, gender, lateral dominance, and prediction of operative skill among general surgery residents. Surgery. 1985;98(3):506–515. [PubMed] [Google Scholar]
- 54.Konge L, et al. Gender differences among medical students in the approach to simulation. Ugeskr Laeger. 2011;173(49):3170–3173. [PubMed] [Google Scholar]
- 55.Ali A, et al. Gender differences in the acquisition of surgical skills: a systematic review. Surg Endosc. 2015;29(11):3065–3073. doi: 10.1007/s00464-015-4092-2. [DOI] [PubMed] [Google Scholar]
- 56.Grantcharov T, et al. Impact of hand dominance, gender, and experience with computer games on performance in virtual reality laparoscopy. Surg Endosc Other Interv Tech. 2003;17(7):1082–1085. doi: 10.1007/s00464-002-9176-0. [DOI] [PubMed] [Google Scholar]
- 57.Huettl F, et al. Higher quality camera navigation improves the surgeon's performance: evidence from a pre-clinical study. J M Access Surg. 2020;16(4):355. doi: 10.4103/jmas.JMAS_143_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Geiser C. Datenanalyse mit Mplus. Wiesbaden: Springer; 2011. [Google Scholar]
- 59.Teber D, et al. The Heilbronn laparoscopic training program for laparoscopic suturing: concept and validation. J Endourol. 2005;19(2):230–238. doi: 10.1089/end.2005.19.230. [DOI] [PubMed] [Google Scholar]
- 60.Laubert T, et al. Conception of the lubeck toolbox curriculum for basic minimally invasive surgery skills. Langenbecks Arch Surg. 2018;403(2):271–278. doi: 10.1007/s00423-017-1642-1. [DOI] [PubMed] [Google Scholar]
- 61.Debnath, S.C., B.B. Lee, and S. Tandon. 2015 Fifty years and going Strong: what makes behaviorally anchored rating scales so perennial as an appraisal method? International Journal of Business and Social Science. 6(2).