Abstract
Alcohol consumption is associated with a number of diseases and injuries, including cardiovascular diseases, cancers, mental and neurological disorders, as well as transport-related injuries. This article reports the alcohol-attributable burden of diseases and injuries at the regional and national levels in the Middle East and North Africa (MENA) region between 1990 and 2019, by sex, age, underlying cause, and Socio-demographic Index (SDI). The regional deaths and disability-adjusted life-years (DALYs) attributable to alcohol consumption were reported for the MENA region, between 1990 and 2019, using the methodological framework and analytical strategies adopted by the Global Burden of Disease (GBD) study 2019. The estimates were all reported as counts, population-attributable fractions, and age-standardised rates per 100,000 population, along with their corresponding 95% uncertainty intervals (UIs). Also, the average annual percentage changes were used to represent the trends of age-standardised rates. In 2019, there were an estimated 22.0 thousand deaths (95% UI: 16.1–29.4) and 1.1 million DALYs (0.8–1.3) attributable to alcohol consumption in the MENA region. The number of DALYs attributable to alcohol consumption were much higher in men (878.0 thousand, 691.4–1104.8) than among women (181.8, 138.6–232.0). The overall age-standardised death and DALY rates attributable to alcohol consumption decreased by 34.5% (13.2–48.3) and 31.9% (16.9–42.5), respectively, over the study period. Egypt (10.1 [5.7–16.6]) and Kuwait (1.1 [0.8–1.5]) had the highest and lowest age-standardised death rates attributable to alcohol consumption, respectively. In 2019, the number of deaths and DALYs in the MENA region were highest in those aged 60–64 and 50–54 years, respectively. A negative association was observed between a country’s SDI and their corresponding age-standardised DALY rates over the period 1990 to 2019. Digestive diseases were the main contributor to the alcohol-attributable burden. Over 1990–2019, the regional deaths and DALYs of diseases and injuries attributable to alcohol consumption decreased with AAPC of − 1.45 (− 1.78 to − 1.12) and − 1.31 (− 1.46 to − 1.15), respectively. The death and DALY rates attributable to alcohol consumption in the MENA region have decreased over the past three decades. Further decreases can be facilitated by implementing country-level policies and increasing public awareness.
Subject terms: Risk factors, Epidemiology, Epidemiology
Introduction
Alcohol consumption is associated with more than 200 diseases and injuries1, and thus the recommended safe level of alcohol consumption is zero2. Evidence shows that the average volume of alcohol consumption has a causal relationship with a number of cancers, cardiovascular diseases, metabolic disorders, respiratory infections, perinatal complications, mental disorders, and neurological consequences3. Moreover, in 2016 alcohol consumption disorder was reported to be the most common type of substance use disorder4, for which the World Health Organization (WHO) has developed a number of programs5.
Alcohol contributes substantially to the overall global burden of diseases, including 4% of all deaths and 4–5% of all disability-adjusted life-years (DALYs). Moreover, alcohol consumption is considered to be one of the most important preventable risk factors. Younger consumers experience more harmful effects than older consumers, partly due to the fact that the injuries caused by alcohol affect younger individuals’ more than older adults. Furthermore, it has been noted that less wealthy individuals and low income countries are at a higher risk, per unit of alcohol consumed, than those from high income countries6. Previous research at the global level has shown that in 2016 the alcohol attributable disease burden peaked in the 25–29 age group and was negatively related to the human development index (HDI)7. The Middle East and North Africa (MENA) region consists of many low and middle income countries, and in 2016 the age-standardised point prevalence of alcohol consumption was 593.0 (95% uncertainty interval (UI): 507.9–683.0) per 100,000 population. Moreover, alcohol consumption was responsible for 264.6 (204.8 − 342.2) age-standardised DALYs, which comprised 0.8% of the total DALYs in this region4.
Previous research reported the burden of diseases attributable to alcohol and drug use over the period 1990–2016, at the global, regional, and national levels4, while a second study reported the deaths and DALYs attributable to alcohol consumption between 2000 and 20167. However, both of these studies used data from the Global Burden of Disease (GBD) 2016 study, which is now out-of-date, and neither focused solely on the MENA region to investigate the alcohol-attributable burden of diseases.
In this article, we aimed to address these gaps and to provide the most up-to-date estimates of alcohol consumption for the 21 countries and territories located in the MENA region. The present study used data from the Global Burden of Disease (GBD) 2019 study to report the numbers and age-standardised rate of deaths and DALYs for the diseases and injuries attributable to alcohol consumption by sex, age, underlying cause, and Socio-demographic Index (SDI), from 1990 to 2019.
Methods
Overview
The Institute for Health Metrics and Evaluation (IHME) manages the GBD project, which has so far estimated the level and trends associated with 369 diseases and injuries and 87 risk factors, from 1990 to 2019, in 204 countries and territories8,9. The present study reports the disease burden attributable to alcohol consumption in the countries that comprise the MENA region, from 1990 to 2019. The MENA region includes: Afghanistan, Algeria, Bahrain, Egypt, Iran, Iraq, Jordan, Kuwait, Lebanon, Libya, Morocco, Oman, Palestine, Qatar, Saudi Arabia, Sudan, the Syrian Arab Republic, Tunisia, Turkey, the United Arab Emirates and Yemen. The total population of MENA was estimated to be 608.7 million in 201910. The Comparative Risk Assessment approach was used in GBD 2019 to estimate the burden of diseases and injuries attributable to alcohol consumption. Detailed information on each analytical step and the methodology used for estimating the burden of diseases, injuries and risk factors can be found in a previous article8. The data for the fatal and non-fatal estimates are available at https://vizhub.healthdata.org/gbd-compare/ and http://ghdx.healthdata.org/gbd-results-tool.
Definition of alcohol consumption
Alcohol consumption (exposure) was defined as the number of grams of pure alcohol consumed per day by current drinkers. The level of exposure was estimated using the following indicators: (a) the proportion of current drinkers, which were those individuals who consumed one or more alcoholic beverage (or an approximation) in the previous year. (b) alcohol consumption, which was the average number of grams of alcohol consumed each day by current drinkers over a one-year period, and (c) litres of alcohol stock per capita, which was the number of litres of pure alcohol per capita over a one-year period. Furthermore, to account for several types of bias, the following variables were also included: (a) number of tourists, which was the total number who visited a location in the previous year. (b) tourists’ duration of stay, which was the total number of days the tourists stayed in the host country, and (c) unrecorded alcohol stock, which was the estimated proportion of the alcohol stock that was made outside the established markets8.
Data sources
A systematic review of the literature was conducted by IHME to identify and extract data on the primary indicators. Population-level survey data, which contained participant-level information, was searched for using the Global Health Exchange (GHDx) and IHME’s online database of health-related data, in order to create the required alcohol consumption indicators on current drinkers and alcohol consumption. The appropriate information was extracted from the data sources8, but only data from representative samples were included.
The estimated prevalence of current drinkers was split by age and sex. First, a meta-regression tool (MR-BRT) was used to estimate the region-specific sex ratios to separate the prevalence reported by sex. Spatiotemporal Gaussian Process Regression (ST-GPR) was then used to separate the estimates into the standard GBD five-year age groups, in studies that did not report estimates in these groups. MR-BRT was also used to adjust the data for studies that did not use the standard definition of alcohol consumption8.
Since GBD 2017, substantial improvements have been made to the modelling of supply-side-level data. The raw data included the domestic (WHO|Global Information System on Alcohol and Health (GISAH); Food and Agriculture Organization (FAO)) and retail supply (Euromonitor) of pure ethanol consumed (number of litres). Domestic supply was defined as the summation of the production and imports, minus the exports. The WHO and FAO sources were combined, with the FAO data only being used where there was no WHO data available for that location-year, since the WHO figures already consider the FAO values. The outliers, implausible data points or data that created implausible model fluctuations were removed, with a detailed description of this process being previously reported8.
Modelling strategy
Although population-based studies provide accurate estimates regarding the prevalence of current drinkers, they also underestimate real alcohol consumption levels8,11. Therefore, the litres per capita variable was thought to provide a more accurate estimate of the overall volume of alcohol consumption, although this does not produce the age- and sex-specific consumption estimates required to estimate the alcohol attributable burden of diseases and injuries. Therefore, population-based survey data and the total volume of alcohol consumed within a location (sourced from the FAO, GISAH, and Euromonitor) were used to model the patterns of consumption by age and sex8.
The survey data was used by ST-GPR to calculate estimates for each location/year/age/sex, as well as to model the alcohol litres per capita (LPC) and the total number of tourists. The LPC were adjusted to take into account unrecorded consumption and consumption by tourists. Furthermore, ST-GPR was also used to generate sex- and age-specific estimates using the estimated percentage of current drinkers within a location/year/sex/age and the consumption trends previously estimated. All estimates were reported as the number of grams/day8.
Data on the estimated relative risk
The theoretical minimum-risk exposure level (TMREL) to alcohol was calculated, which is the level of exposure that minimises the chances of suffering burden from any alcohol-related cause. IHME conducted a systematic literature review to find all cohort and case–control studies that reported a relative risk, hazard ratio, or odds ratio for any alcohol-disease or alcohol-injury pairs that were covered by GBD 20198. The systematic review only included studies that were representative of their specific population, reported a categorical or continuous dose of alcohol consumption, and reported measures of uncertainty. The studies were then used to compute a dose–response model using the Disease Modelling Ordinary Differential Equation (DisMod ODE) solver to fit non-linear Bayesian meta-regressions. A DisMod ODE model was preferred over the conventional mixed effects meta-regression, as it is able to estimate nonparametric splines over doses (i.e., there is a non-linear dose–response relationship) and to include heterogeneous doses through dose integration (i.e., research normally reports doses categorically in wide ranges and DisMod ODE estimates specific doses when the categories overlap between studies, using an integration step). The results of the meta-regression were then used to estimate a non-parametric curve for all doses between zero and 150 g/day, as well as their corresponding relative risks. The relative risk was considered to be the same for all-ages and for both males and females8.
The systematic review8 found the following diseases and injuries to be associated with alcohol consumption: cardiovascular diseases, diabetes and kidney diseases, digestive diseases, neoplasms, neurological disorders, respiratory infections and tuberculosis, self-harm and interpersonal violence, substance use disorders, transport injuries and unintentional injuries.
Estimation of the proportion of cancers attributable to alcohol consumption
The population-attributable fraction (PAF) was used to estimate the burden of diseases and injuries related to alcohol consumption by country, age, sex, and year, using the following formula:
where: Pc denotes the prevalence of current drinkers, Pa is the prevalence of abstainers, RRC(x) is the relative risk function for current drinkers, and p is the parameters determined by the mean and standard deviation of exposure. This equation was used to produce 1000 draws of the exposure and relative risk models and the PAF was used to calculate the attributable burden8.
The deaths and DALYs attributable to alcohol consumption for each country, age, sex, year, and disease/injury were calculated by multiplying the PAFs with the estimated number of deaths or DALYs for each country, age, sex, year, and disease/injury. The number of deaths were estimated using the Cause of Death Ensemble model (CODEm) in GBD 2019. CODEm generates a number of individual models to identify the best model fit using all obtainable data and covariates. The predictive validity for the different models, or combinations of models, were assessed and the one with the best (out-of-sample) predictive validity was chosen. Furthermore, the DALYs for diseases/injuries were estimated in three stages: (a) the years lived with disability (YLDs) was calculated by multiplying the severity-specific disability weights with the prevalence of each severity category for each disease/injury; (b) the number of deaths in an age group were then multiplied by the remaining life expectancy in that age group, taken from the GBD standard life table, to produce the years of life lost (YLLs) for each disease/injury; (c) the YLLs and YLDs were then summed for each disease/injury to calculate the DALYs. A comprehensive description of the methods used to calculate the total number of deaths and DALYs has been previously reported8. The estimates were all reported as counts, proportions (PAFs) and age-standardised rates per 100,000, along with their corresponding 95% UIs. The UIs were calculated by running 1000 repetitions at each computational step and through the inclusion of uncertainty from multiple sources (i.e., input data, measurement error and estimates of residual non-sampling error). The UIs were defined as the 25th and 975th values of the ordered draws8.
The relationship between the burden of diseases/injuries attributable to alcohol consumption and SDI was also investigated. Smoothing splines models12 were used to determine the shape of the association between the burden attributable to alcohol consumption, in terms of DALYs, and SDI for the 21 countries in MENA. SDI is a multifactorial measure of socio-economic development which contains the lag-distributed income per capita, educational attainment for the population aged > 15, and the total fertility rate < 25 years old. The SDI ranges from the least developed (0) to the most developed (1). The age-standardised death and DALY rates were mapped using R software (version 3.5.2). In addition, annual percentage change (APC) and the average APC (AAPC) were calculated using the joinpoint regression tool13,14.
Ethics approval
The present study was approved by ethics committee of Shahid Beheshti University of Medical Sciences (IR.SBMU.RETECH.REC.1401.070). This study is based on publicly available data and solely reflects the opinion of its authors and not that of the Institute for Health Metrics and Evaluation.
Results
The Middle East and North Africa region
In 2019, there were an estimated 22.0 thousand deaths (95% UI: 16.1 to 29.4) attributable to alcohol consumption in the MENA region, representing 0.7% (0.5 to 0.9) of all deaths (Table 1). Also in 2019, there were 18.7 (13.7 to 25.4) thousand deaths in men and 3.2 (2.1 to 4.8) thousand deaths in women (Table S1). The age-standardised death rate associated with alcohol consumption in 2019 (4.6 [3.4 to 6.3] per 100,000) was 34.5% lower (13.2 to 48.3) than the 1990 level (7.1 [5.3 to 9.1]) (Table S2). During 2019, alcohol consumption caused 1.1 million DALYs (0.8 to 1.3), representing 0.6% (0.5 to 0.8) of all DALYs in both sexes combined, with 878.0 (691.4 to 1104.8) thousand DALYs in men and 181.8 (138.6 to 232.0) thousand DALYs in women (Table S3). Between 1990 and 2019, the age-standardised DALY rate (per 100,000) decreased from 276.6 (218.9 to 339.0) to 188.3 (148.5 to 235.7), a relative decrease of 31.9% (16.9 to 42.5) from the 1990 level (Table S4).
Table 1.
The burden of diseases attributable to alcohol consumption in the Middle East and North Africa region in 2019 and percentage change of age-standardised rates during 1990–2019 (Generated from data available from http://ghdx.healthdata.org/gbd-results-tool).
| Deaths (95% UI) | DALY (95% UI) | |||||||
|---|---|---|---|---|---|---|---|---|
| Counts (2019) | PAF (2019) | ASRs (2019) | % change in ASRs 1990–2019 | Counts (2019) | PAF (2019) | ASRs (2019) | % change in ASRs 1990–2019 | |
| North Africa and Middle East | 21,980 (16,085, 29,408) | 0.7 (0.5, 0.9) | 4.6 (3.4, 6.3) | − 34.5 (− 48.3, − 13.2) | 1,059,791 (842,123, 1,316,847) | 0.6 (0.5, 0.8) | 188.3 (148.5, 235.7) | − 31.9 (− 42.5, − 16.9) |
| Afghanistan | 583 (375, 853) | 0.2 (0.2, 0.3) | 3.8 (2.5, 5.4) | − 23.1 (− 43.9, 4.2) | 35,540 (25,680, 47,682) | 0.2 (0.2, 0.3) | 155.6 (110.4, 208.9) | − 14.3 (− 33.5, 12.8) |
| Algeria | 1285 (766, 1972) | 0.6 (0.4, 1) | 3.3 (1.9, 5.3) | 5.8 (− 36.8, 82.3) | 72,122 (51,488, 96,915) | 0.7 (0.5, 0.9) | 170.2 (119.7, 231.3) | 1.8 (− 28.5, 42.9) |
| Bahrain | 69 (44, 101) | 1.6 (1.1, 2.3) | 5.1 (3, 8) | − 76.2 (− 85.7, − 62.3) | 3859 (2757, 5297) | 1.4 (1, 1.8) | 227.4 (159.7, 320.2) | − 67.5 (− 77.6, − 54.7) |
| Egypt | 6207 (3373, 10,443) | 1.1 (0.6, 1.8) | 10.1 (5.7, 16.6) | − 5.6 (− 46.7, 57.4) | 221,195 (135,795, 354,970) | 0.8 (0.5, 1.3) | 290.3 (177, 457.1) | − 6.3 (− 45.9, 58) |
| Iran (Islamic Republic of) | 2976 (2244, 3996) | 0.8 (0.6, 1) | 3.8 (2.9, 5.2) | 36.7 (2.7, 89.6) | 139,833 (109,766, 175,225) | 0.7 (0.6, 0.9) | 158.9 (124.4, 200.3) | 27 (3.6, 59.5) |
| Iraq | 817 (406, 1418) | 0.5 (0.2, 0.8) | 2.5 (1.1, 4.6) | − 70.6 (− 87.2, − 42.9) | 54,549 (35,290, 82,758) | 0.5 (0.4, 0.8) | 143 (88, 225.5) | − 61.5 (− 76.7, − 37.9) |
| Jordan | 186 (97, 309) | 0.6 (0.3, 0.9) | 2.3 (1.2, 4) | − 16.5 (− 56.6, 65.5) | 12,615 (8213, 17,650) | 0.6 (0.4, 0.8) | 121.4 (77.1, 176.4) | − 12.6 (− 43, 36.8) |
| Kuwait | 32 (23, 45) | 0.3 (0.2, 0.4) | 1.1 (0.8, 1.5) | − 14.5 (− 34.1, 8.9) | 3363 (2394, 4598) | 0.4 (0.3, 0.6) | 68.1 (49.9, 90) | − 10.8 (− 24.5, 4) |
| Lebanon | 262 (147, 419) | 0.8 (0.5, 1.2) | 5 (2.8, 8) | − 64.3 (− 78.3, − 46.1) | 10,835 (7429, 15,522) | 0.8 (0.6, 1.1) | 203.8 (138.8, 291.2) | − 61.9 (− 73.9, − 47.1) |
| Libya | 209 (124, 310) | 0.7 (0.4, 0.9) | 3.6 (2.2, 5.4) | 35.9 (− 15.4, 120.4) | 11,185 (7345, 15,020) | 0.7 (0.5, 0.8) | 158.8 (103.5, 214.5) | 32.1 (− 8.2, 87.4) |
| Morocco | 1108 (638, 1698) | 0.5 (0.3, 0.7) | 3.2 (1.8, 5) | − 58.4 (− 73.8, − 36.7) | 58,610 (40,044, 82,346) | 0.6 (0.4, 0.8) | 157.6 (107.7, 222.5) | − 51.5 (− 65.2, − 32.1) |
| Oman | 67 (33, 108) | 0.5 (0.3, 0.9) | 2.3 (1, 3.9) | − 12.6 (− 47, 62.1) | 6057 (4026, 8578) | 0.7 (0.5, 1) | 125.8 (79.5, 182.1) | − 10.1 (− 34.1, 29.2) |
| Palestine | 219 (155, 298) | 1.3 (1, 1.7) | 8.6 (5.8, 12.2) | 1.9 (− 37.9, 85.6) | 9873 (7511, 12,534) | 1 (0.8, 1.2) | 288.9 (215.2, 375.2) | 2.6 (− 30.4, 61.3) |
| Qatar | 75 (49, 110) | 1.7 (1.2, 2.3) | 6.8 (4.2, 10) | − 26.4 (− 56, 19.7) | 5715 (4097, 7660) | 1.3 (1, 1.6) | 218.1 (152.5, 296.2) | − 37.5 (− 58.5, − 8.7) |
| Saudi Arabia | 722 (352, 1405) | 0.6 (0.3, 1) | 3.4 (1.8, 6.1) | − 61.9 (− 77.7, − 26.4) | 50,542 (30,270, 81,200) | 0.6 (0.4, 0.9) | 141.3 (86.8, 233.6) | − 54 (− 70.6, − 20.9) |
| Sudan | 494 (300, 774) | 0.2 (0.2, 0.4) | 2.6 (1.5, 4) | − 74.4 (− 86.5, − 44.6) | 29,763 (21,608, 39,519) | 0.2 (0.2, 0.3) | 105 (75.4, 144.5) | − 71.8 (− 83.3, − 48.3) |
| Syrian Arab Republic | 567 (306, 938) | 0.7 (0.4, 1) | 4.6 (2.5, 7.7) | − 49.5 (− 70.1, − 22) | 24,012 (15,482, 35,496) | 0.6 (0.4, 0.8) | 172.9 (112.1, 256.6) | − 45.4 (− 62.6, − 24) |
| Tunisia | 723 (446, 1109) | 1.1 (0.7, 1.5) | 5.6 (3.4, 8.6) | 37.1 (− 15.9, 120.2) | 34,614 (24,314, 47,583) | 1.2 (0.9, 1.5) | 271.1 (189.9, 371.3) | 23.4 (− 10.1, 70.9) |
| Turkey | 3941 (2551, 5734) | 0.9 (0.6, 1.2) | 4.3 (2.7, 6.4) | − 35.6 (− 58.8, 1.7) | 194,539 (143,449, 256,399) | 1 (0.8, 1.2) | 208.7 (153.1, 276.7) | − 33.8 (− 50.8, − 11.1) |
| United Arab Emirates | 553 (306, 884) | 1.9 (1.1, 2.8) | 8.4 (4, 13.8) | − 63.1 (− 81.4, − 37.5) | 34,097 (22,366, 49,773) | 1.6 (1.1, 2.2) | 342 (204.3, 523.2) | − 55.9 (− 73.3, − 31.8) |
| Yemen | 861 (492, 1325) | 0.5 (0.3, 0.7) | 5.2 (2.9, 8.1) | − 67.9 (− 80.1, − 50.2) | 45,794 (30,451, 64,918) | 0.4 (0.3, 0.5) | 211.5 (137.3, 303.9) | − 61.9 (− 74.6, − 44.1) |
DALY Disability adjusted life year, GBD Global Burden of Disease, ASRs Age-standardised rates.
National level
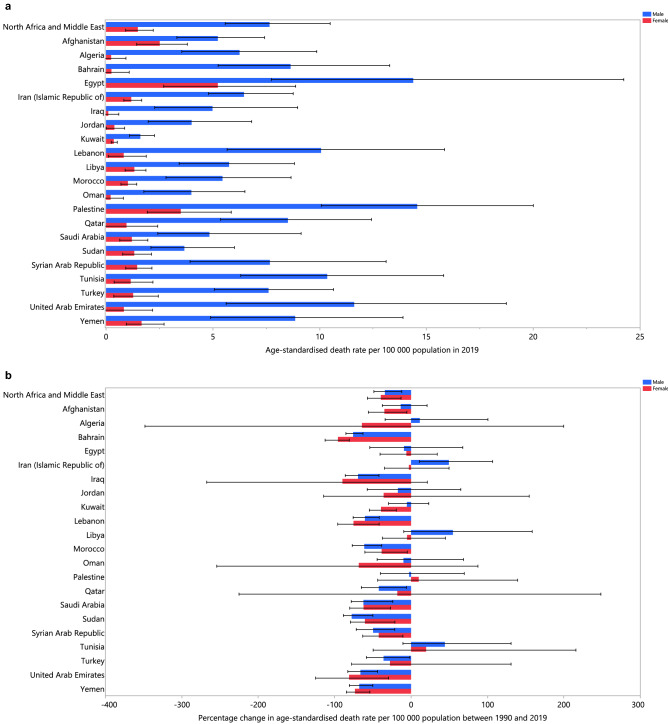
In 2019, the proportion of all deaths attributable to alcohol consumption varied markedly by country (from 0.2% to 1.9%). The United Arab Emirates (1.9% [1.1 to 2.8]), Qatar (1.7% [1.2 to 2.3]) and Bahrain (1.6% [1.1 to 2.3]) had the three highest PAFs. In contrast, the lowest PAFs were found in Afghanistan (0.2% [0.2 to 0.3]), Sudan (0.2% [0.2 to 0.4]) and Kuwait (0.3% [0.2 to 0.4]) (Table 1). The age-standardised death rate attributable to alcohol consumption in 2019 ranged from 1.1 to 10.1 per 100,000. In 2019, Egypt (10.1 [5.7 to 16.6]), Palestine (8.6 [5.8 to 12.2]) and the United Arab Emirates (8.4 [4.0 to 13.8]) had the three highest age-standardised death rates attributable to alcohol consumption (per 100,000). In contrast, the lowest rates were found in Kuwait (1.1 [0.8 to 1.5]), Oman (2.3 [1.0 to 3.9]) and Jordan (2.3 [1.2 to 4.0]) (Table 1). The age-standardised death rates attributable to alcohol consumption in 2019, for males and females, are presented in Fig. 1a. An increase in the age-standardised death rate attributable to alcohol consumption, from 1990 to 2019, was only observed in Iran (36.7% [2.7 to 89.6]). In contrast, the largest decreases over this period were observed in Bahrain (− 76.2% [− 85.7 to − 62.3]), Sudan (− 74.4% [− 86.5 to − 44.6]) and Iraq (− 70.6% [− 87.2 to − 42.9]) (Table S2). The percentage change in the age-standardised death rates, from 1990 to 2019, for males and females, are presented in Fig. 1b.
Figure 1.
Age-standardised death rate (per 100,000 population) in 2019 (a) and percentage change in the age-standardised death rate from 1990 to 2019 (b) of disease and injuries attributable to alcohol consumption in the Middle East and North Africa region, by sex and country. (Generated from data available from http://ghdx.healthdata.org/gbd-results-tool).
The proportion of all DALYs attributable to alcohol consumption in 2019 differed considerably by country (from 0.2% to 1.6%). The United Arab Emirates (1.6% [1.1 to 2.2]), Bahrain (1.4% [1.0 to 1.8]) and Qatar (1.3% [1.0 to 1.6]) had the three highest PAFs. In contrast, the lowest PAFs were found in Afghanistan (0.2% [0.2 to 0.3]), Sudan (0.2% [0.2 to 0.3]) and Yemen (0.4% [0.3 to 0.5]) (Table 1). The age-standardised DALY rate attributable to alcohol consumption in 2019 ranged from 68.1 to 342.0 per 100,000. The United Arab Emirates (342.0 [204.3 to 523.2]), Egypt (290.3 [177.0 to 457.1]) and Palestine (288.9 [215.2 to 375.2]) had the three highest age-standardised DALY rates. In contrast, the lowest rates were found in Kuwait (68.1 [49.9 to 90.0]), Sudan (105.0 [75.4 to 144.5]) and Jordan (121.4 [77.1 to 176.4]) (Table 1). The 2019 age-standardised DALY rates are presented by sex in Fig. S1. Palestine and Egypt had the highest age-standardised DALY rates attributable to alcohol consumption for males and females, respectively, while Kuwait had the lowest DALY rate for both sexes.
An increase in the DALY rate attributable to alcohol consumption, from 1990 to 2019, was only observed in Iran (27.0% [3.6 to 59.5]). In contrast, the largest decreases were observed in Sudan (− 71.8% [− 83.3 to − 48.3]) Bahrain (− 67.5% [− 77.6 to − 54.7]), and Lebanon (− 61.9% [− 73.9 to − 47.1]) (Table 1). The percentage changes in the age-standardised DALY rates, from 1990 to 2019, for males and females are presented in Fig. S2.
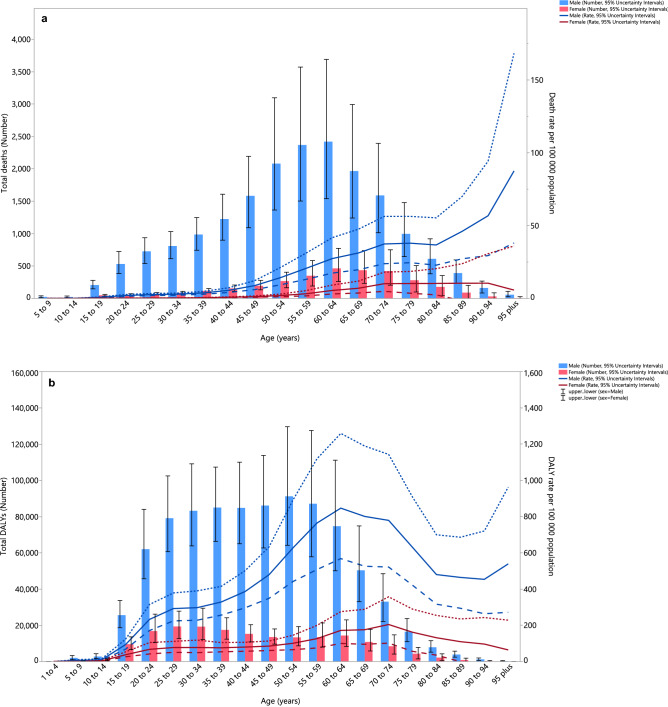
Age and sex patterns
In 2019, the number of deaths attributable to alcohol consumption in the MENA region were highest in the 60–64 age group. The death rate attributable to alcohol consumption started to increase from the 20–24 age group and peaked in the 95+ age group for males, and in the 90–94 age group for females. There were substantial differences between males and females, in terms of the number of deaths and the death rate (Fig. 2a). Furthermore, in 2019 the number of DALYs attributable to alcohol consumption in the MENA region were highest in the 50–54 age group for males and in the 25–29 age group for females. For males, the DALY rate started increasing in the early age groups, peaking in the 60–64 age group and then decreased with age. For females, the DALY rate started to increase during the middle ages, with the highest DALY rate being in the 70–74 age group (Fig. 2b).
Figure 2.
Numbers of deaths and death rate (a) and number of DALYs and DALY rate (b) of disease and injuries attributable to alcohol consumption in the Middle East and North Africa region, by age and sex in 2019. Dotted and dashed lines indicate 95% upper and lower uncertainty intervals, respectively (Generated from data available from http://ghdx.healthdata.org/gbd-results-tool).
Among people aged less than 20 years old, the largest increases in the age-standardised death and DALY rates were observed in Libya. In contrast, the largest decrease in the death rate was found in Sudan, while the largest decrease in the DALY rate was found in Lebanon. Regarding the 20–54 age group, Libya had the largest increases in the age-standardised death and DALY rates, whereas Sudan had the largest decreases in both rates. In addition, the largest increases in the age-standardised death and DALY rates were found among individuals aged over 55 years old in Tunisia, while the largest decreases in these rates were found among the same age group in Bahrain (Figs. S3–S4).
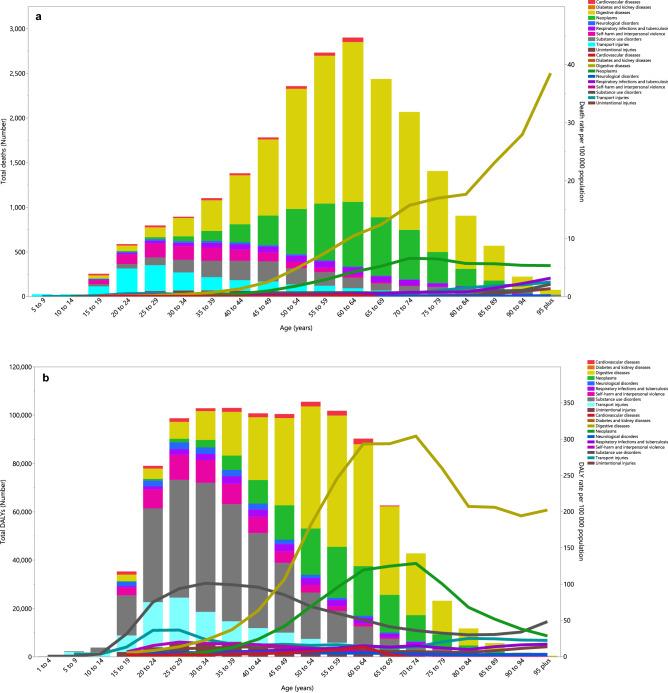
Underlying causes
In 2019, the death rate from alcohol-related digestive diseases was higher in people aged 30 and older than for all other causes. The death rate starting increasing in the 35–39 age group and peaked in the 95+ age group (Fig. 3a). In addition, the death rate attributable to neoplasms accounted for the second largest proportion, which started increasing in the 45–49 age group and peaked in the 70–74 age group, before decreasing in the remaining age groups (Fig. 3a). The DALY rate attributable to digestive diseases started to increase in the 20–24 age group and peaked in the 70–74 age group, then decreased in the last five age groups. In addition, the DALY rate attributable to neoplasms started to increase in the 30–34 age group and peaked in the 70–74 age group, before decreasing in the remaining age groups. Substance use disorders accounted for the third largest proportion and its DALY rate started to increase in the 10–14 age group and reached its highest level in the 30–34 age group (Fig. 3b).
Figure 3.
Numbers of deaths and death rate (a) and number of DALYs and DALY rate (b) of disease and injuries attributable to alcohol consumption in the Middle East and North Africa region, by age and cause in 2019 (Generated from data available from http://ghdx.healthdata.org/gbd-results-tool).
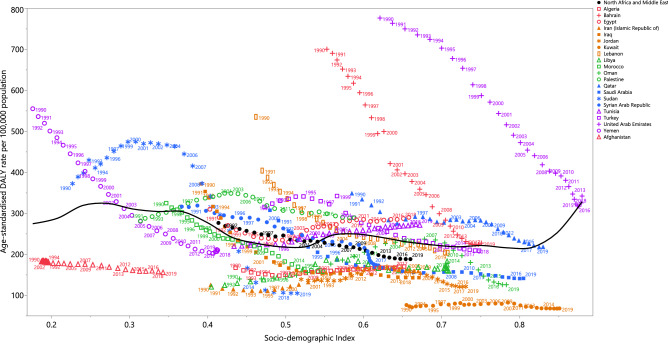
Burden of diseases and injuries attributable to alcohol consumption by Socio-demographic Index (SDI)
There was a generally negative association between a country’s SDI and their corresponding age-standardised DALY rates attributable to alcohol consumption, from 1990 to 2019. Countries higher than the solid black line had a higher than expected burden, while those below the line had a lower than expected burden. Most of the countries showed a decrease in the age-standardised DALY rates from 1990 to 2019. The United Arab Emirates and Bahrain had higher than expected burdens for all years during the measurement period, while lower than expected burdens were found in Kuwait, Iran, Jordan, Libya, Algeria and Afghanistan throughout the measurement period. Qatar, Turkey, Lebanon, Saudi Arabia, Syrian Arabic Republic, Morocco and Yemen had a higher than expected burden at the start of the measurement period, but their burden became lower than expected during the last few years (Fig. 4).
Figure 4.
Age-standardised DALY rates of diseases and injuries attributable to alcohol consumption for 21 countries and territories from 1990 to 2019, by SDI; Each point in a line represents the observed age-standardised DALY rate for each year starting at 1990 and ending at 2019. In all countries, SDI has increased over time, so progress in SDI is associated with points further to the right and later years for a given country. Expected values based on the Socio-demographic Index and disease rates in all locations are shown as the black line. DALY disability-adjusted-life-years. SDI Socio-demographic Index (Generated from data available from http://ghdx.healthdata.org/gbd-results-tool).
Joinpoint trends of diseases and injuries attributable to alcohol consumption
Over 1990–2019, the regional deaths and DALYs of diseases and injuries attributable to alcohol consumption decreased with AAPC of − 1.45% (− 1.78 to − 1.12) and − 1.31% (− 1.46 to − 1.15), respectively (Tables S2 and S4). The AAPC of alcohol-attributable deaths in males and females in 2019 were − 1.43% (− 1.76 to − 1.10) and − 1.72% (− 1.82 to − 1.61), respectively, over the measurement period in MENA (Table S1). Also, the AAPC of regional alcohol-attributable DALYs in males and females over 1990–2019 were − 1.35% (− 1.51 to − 1.19) and − 1.28% (− 1.37 to − 1.19) (Table S3). The AAPC of deaths attributable to alcohol consumption decreased in most countries in MENA and ranged from − 4.96% (− 5.59 to − 4.33) in Bahrain to 1.25% (0.52 to 1.98) in Libya (Table S2). Moreover, the AAPC of DALYs attributable to alcohol consumption in MENA ranged from − 4.35% (− 4.81 to − 3.88) in Sudan to 0.97% (0.41 to 1.54) in Libya over 1990–2019 (Table S4).
Discussion
The present study used pre-existing data from the GBD study 2019 to describe the disease and injury burden due to alcohol consumption in the MENA region. The study found that in 2019 alcohol consumption was responsible for 22.0 thousand deaths and 1.1 million DALYs in this region. Furthermore, we found that there was a 34.5% reduction in the age-standardised death rate with AAPC of − 1.45% and a 31.9% reduction in the DALY rate with AAPC of − 1.31% attributable to alcohol consumption over the period 1990 to 2019. This is in accordance with a 23.3% global reduction in the age-standardised DALY rate due to alcohol consumption8. Considering alcohol consumption is a unique risk factor for several injuries and diseases15,16, measuring the health effects of alcohol consumption and the successful use of control measures could be potentially helpful in preventing or reducing subsequent health problems17.
This study also found that in 2019 0.7% of all deaths and 0.6% of all DALYs were due to alcohol consumption. According to the WHO regions, the proportion of deaths and DALYs caused by alcohol drinking were lowest in the Eastern Mediterranean region6, where 0.7% of all deaths and 0.7% of all DALYs were attributable to alcohol consumption5. Similarly, using the GBD regional classification, MENA had the lowest alcohol-related age-standardised rates for deaths and DALYs in the world7, which is probably due to the fact that MENA also has the lowest alcohol consumption per capita18. Furthermore, many countries located in MENA are Muslim majority countries, where the Islamic laws prohibit alcohol production, consumption, transport and trade services. As a result, the importance of religious beliefs and attitudes, along with religion-based alcohol policies in most of the MENA countries, may explain the low alcohol consumption rate19,20. At the global level, a recent publication using GBD 2016 data reported that alcohol was responsible for 9.0% and 7.6% of all age-standardised deaths and DALYs, respectively16. Furthermore, 5.3% and 5.0% of the global age-standardised deaths and DALYs were reported to be as a result of alcohol consumption, respectively, using data obtained from the WHO Global Health Estimates 20167. The disparities in the reported global PAFs are likely due to variations in the methodologies used in each study.
In 2019, the DALY rate due to alcohol consumption started to rise during adolescence and peaked among older adults. Moreover, the GBD 2019 global risk factor study reported that alcohol consumption was the leading cause of DALYs in the 25–49 age group from 1990 to 20198. Furthermore, alcohol related mortality has been found to occur mainly in young individuals, with more than half (52.4%) of all alcohol-related deaths being found among those younger than 60 years old7. This finding highlights the need for more effective preventive measures in this age group. There were also marked differences between men and women in the MENA region, in terms of the number of deaths and DALYs due to alcohol consumption. In line with this, an analysis of 16 general population surveys from 10 countries noted substantial differences between the drinking behaviors of men and women. The level of alcohol consumption was consistently higher among men (than women) in both frequency and quantity, as well as in rates of heavy drinking episodes. In contrast, women were more likely to be life-time abstainers21. However, it is projected that the ratio of male to female drinkers will reduce in the Eastern Mediterranean region by 0.006 annually, due in part to increased alcohol consumption among females18. In our study, the DALYs attributable to alcohol consumption reduced with AAPC of 1.28% over the last three decades in MENA.
Our study also found that Iran was the only country in the MENA region that showed increases in the age-standardised death and DALY rates attributable to alcohol consumption between 1990 and 2019. Also, Libya and Iran had the highest increase in the AAPC of deaths and DALYs attributable to alcohol consumption in MENA over 1990–2019. A recent systematic review and meta-analysis reported that only one in eight Iranians had ever consumed alcoholic beverages22. However, it has also been noted that substandard and adulterated alcoholic drinks are frequently consumed in Iran, due to policies forbidding legal alcohol marketing and sales23,24. In addition, as a result of the depreciation in the Iranian currency over recent years, people have been driven to buy handmade alcoholic beverages underground, rather than legally imported high quality products, which may have led to increased levels of alcohol poisoning, death and disability across the country19. Although the Iranian Ministry of Health has developed a number of programs aimed at reducing alcohol consumption by 10%, they have not been successfully implemented, due to the low public health service capacity in Iran19.
Generally, a negative relationship was noted between the burden due to alcohol consumption and a country’s SDI level. Although not completely comparable, a similar relationship was reported globally with HDI levels, with low HDI countries having the highest age-standardised DALY rates attributable to alcohol consumption7. Moreover, a negative relationship was found between the burden caused by alcohol consumption and a country’s income level5. Since 1990, alcohol consumption has decreased in most high income countries, particularly in Eastern Europe. During the same time period, alcohol consumption increased markedly in many upper-middle and lower-middle income countries, particularly in China and India5,18. This trend is expected to continue across the globe up to 203018. In Sudan, the alcohol-related age-standardised DALY rates peaked over the period 2000–2005, which may be due to psychological distress from the civil war in South Sudan, which started in 1955 and finished in 200525,26.
In 2019, digestive diseases and neoplasms were the two largest causes of death and DALY rates attributable to alcohol consumption in the MENA region. This finding contrasts with the global GBD 2016 findings, where tuberculosis and road injuries were the two most common alcohol-related causes of death for those aged 15–49 years old, while cancers had the largest burden for individuals 50 or older16. In line with the fact that MENA has the lowest alcohol consumption per capita18, it has also been reported that this region had the lowest death and prevalence rates of cirrhosis and alcohol-related liver disease in the world27,28. Conversely, in MENA the largest proportion of deaths and prevalent cases of cirrhosis were caused by hepatitis B and C27. It is also important to note that alcohol has a synergistic effect with hepatitis B and hepatitis C infections and this combination could lead to a more rapid deterioration of patients with cirrhosis and hepatocellular carcinoma29–32. Interestingly, a recent investigation using GBD 2019 data found that Egypt had the highest incidence of acute viral hepatitis among the MENA countries33. The present study found that Egypt had the highest mortality rate due to alcohol, possibly due to the synergic association between the pathophysiology of viral hepatitis and alcohol consumption. Another important factor, particularly for liver cirrhosis, is the quality of the alcoholic drinks34–36. Counterproductive alcohol bans, which have been applied as a result of religious beliefs, may encourage the consumption of illegally produced and smuggled alcoholic drinks37. This may help to explain the relatively high burden of alcohol attributable digestive diseases in the MENA region.
A causal relationship between alcohol consumption and the development of multiple types of cancer has long been debated. Using the 2020 GLOBOCAN data, it was estimated that globally nearly 4.1% of all new cancer cases were alcohol-related38. Furthermore, given the increased aging of the population, alcohol related disability and death is predicted to rise in the near future, particularly because neoplasms disproportionately affect older adults. Cancers of the esophagus, pharynx, lip and oral cavity had the highest PAFs due to alcohol38. The incidence of these cancers have been linked to direct contact with acetaldehyde, an immediate metabolite of ethanol39. Acetaldehyde is responsible for some of the alcohol related carcinogenicity, via interference with the DNA repair process and damage to the DNA strands within the cells40. Apart from cancers of the upper aerodigestive tract, there have been reports that even a small intake of alcohol could substantially increase the risk of breast cancer among females41, which may be due to impaired regulation of hormones, such as estrogens and androgens42.
It is important to note that most MENA countries have faced population growth and cultural transitions in recent years, so although alcohol consumption was low in MENA, this rate may have increased. Furthermore, there are a number of factors which may increase the consumption of alcoholic drinks among these countries. For instance, by considering alcohol consumption to be a westernized, open-minded, and modern behavior, many young people in developing countries are attracted to drinking alcohol, with little knowledge about the likely health outcomes. Furthermore, extended media coverage over the last few decades has gradually introduced different cultures and attitudes into Islamic countries, which has resulted in the promotion and normalization of alcohol consumption, particularly among the younger age groups. Moreover, alcohol suppliers and distributors have developed new strategies to circumvent the bans, with the aim of advertising well-known alcohol brands and increasing consumption of these alcoholic drinks. Consequently, the problem of alcohol consumption must be addressed in MENA countries as a public health issue, rather than just due to religious concern43.
Public awareness of the causal relationship between alcohol consumption and the risk of several diseases is low. Therefore, adding cancer and digestive disease warnings to alcoholic drink labels, in the same way as on cigarette packages, may help to discourage people from purchasing and consuming alcoholic drinks44 and may also help to increase public cooperation with alcohol control policies45. Due to the substantial burden caused by alcohol consumption, several international initiatives have been proposed. The WHO has endorsed a cost-effective and feasible global strategy of so-called “best buys” to reduce the harmful impact of alcohol consumption at the population level. The program involves policies to increase taxation and ban alcohol advertising46. Reducing the harmful use of alcohol has also been targeted by the Non-Communicable Diseases Global Monitoring Framework and the Sustainable Development Goals programs47. In addition to the implementation of control measures, monitoring and surveillance frameworks are required to track alcohol consumption trends and its related health consequences. With a surveillance system in place, decision makers would be more able to appropriately prioritise and amend policies and interventions, based on the current situation within the community. However, very few countries have well-developed systems which reliably record and monitor the morbidity and mortality attributable to alcohol consumption5.
Despite the observed decrease in the burden attributable to alcohol consumption, it is important that government agencies and other health care organisations implement policies to reduce alcohol consumption, in order to decrease the level of alcohol induced harm. Tailoring these interventions to religious countries is crucial, since although the religious-driven policy may restrict alcohol intake to a low level, it is not sufficient on its own. The integration of scientific and evidence-based alcohol control guidelines are needed within the health systems of the MENA countries.
Limitations
The present study has several limitations, which must be taken into account when interpreting the findings. Firstly, the results were not stratified according to the individuals’ level of alcohol intake or according to their drinking status (drinking or abstention). Furthermore, the pattern of alcohol consumption within the last 12 months is an important predictor of risk48, but the estimates assumed a consistent drinking pattern over time, as the currently available information was not detailed enough. Moreover, in addition to the interconnected relationship between alcohol consumption and dependence on tobacco, it is now clear that there is a synergic carcinogenic relationship between the two for most neoplasms of the upper aerodigestive tract49–51. Therefore, it could be hypothesised that some of the alcohol-attributable burden may have been caused by tobacco use. Fourthly, our findings are susceptible to several biases, due to the lack of high quality prospective cohort studies and the possibility that there are a substantial number of unrecorded alcohol related diseases in low and middle income countries. In a number of countries, alcohol consumption may be greatly under-reported, due to sociocultural factors, such as stigma52. Fifthly, the estimates were calculated using alcohol sales data, meaning that the burden due to alcohol consumption may have been underestimated, as some illicit production is likely to have been missed. Finally, data sparseness on the consumption of alcohol among adolescents may introduce further biases, suggesting more investigations are needed to study youth drinking behavior and the harm caused by alcohol consumption in this age group. Taken together, these limitations indicate that the burden attributable to alcohol consumption may have been underestimated.
Conclusions
In summary, alcohol consumption remains a leading risk factor for adverse health outcomes, and its relative importance is increasing. The consumption of alcohol is low in the MENA region and the disease burden attributable to alcohol consumption has decreased over the last three decades. Nevertheless, increasing public awareness about the risk of alcohol consumption, together with country-specific policies for marketing bans and restricting alcohol industry lobbying, particularly in rapidly developing countries, might help reduce alcohol consumption and its attributable burden. Further research is needed to investigate the effects of alcohol consumption patterns on the burden of different diseases, especially among adolescents. Moreover, providing data at the subnational level, and by residential area, may help health policymakers and should be considered in future research.
Supplementary Information
Acknowledgements
We would like to thank the Institute for Health Metrics and Evaluation staff and its collaborators who prepared these publicly available data. We would also like to acknowledge the support of the Shahid Beheshti University of Medical Sciences.
Author contributions
S.S. and A.A.K. designed the study. SS analyzed the data and performed the statistical analyses. S.S., S.A.N., M.N., M.J.M.S., G.S.C., J.S.K., and A.A.K. drafted the initial manuscript. All authors reviewed the drafted the manuscript for critical content. All authors approved the final version of the manuscript.
Funding
The Bill and Melinda Gates Foundation, who were not involved in any way in the preparation of this manuscript, funded the GBD study. The Shahid Beheshti University of Medical Sciences, Tehran, Iran (Grant No. 32448) also supported the present report.
Data availability
The data used for these analyses are all publicly available at http://ghdx.healthdata.org/gbd-results-tool.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Saeid Safiri, Email: safiris@tbzmed.ac.ir.
Ali-Asghar Kolahi, Email: a.kolahi@sbmu.ac.ir.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-022-22901-x.
References
- 1.World Health Organization. Alcohol: Key Facts. https://www.who.int/news-room/fact-sheets/detail/alcohol (2018, 2022).
- 2.Burton R, Sheron N. No level of alcohol consumption improves health. Lancet. 2018;392:987–988. doi: 10.1016/S0140-6736(18)31571-X. [DOI] [PubMed] [Google Scholar]
- 3.Rehm J, Baliunas D, Borges GLG, et al. The relation between different dimensions of alcohol consumption and burden of disease: An overview. Addiction. 2010;105:817–843. doi: 10.1111/j.1360-0443.2010.02899.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Degenhardt L, Charlson F, Ferrari A, et al. The global burden of disease attributable to alcohol and drug use in 195 countries and territories, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Psychiatry. 2018;5:987–1012. doi: 10.1016/S2215-0366(18)30337-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization . Global Status Report on Alcohol and Health 2018. World Health Organization; 2019. [Google Scholar]
- 6.Rehm J, Mathers C, Popova S, et al. Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. Lancet. 2009;373:2223–2233. doi: 10.1016/S0140-6736(09)60746-7. [DOI] [PubMed] [Google Scholar]
- 7.Shield K, Manthey J, Rylett M, et al. National, regional, and global burdens of disease from 2000 to 2016 attributable to alcohol use: A comparative risk assessment study. Lancet Public Health. 2020;5:e51–e61. doi: 10.1016/S2468-2667(19)30231-2. [DOI] [PubMed] [Google Scholar]
- 8.Murray CJ, Aravkin AY, Zheng P, Abbafati C, Abbas KM, Abbasi-Kangevari M, Abd-Allah F, Abdelalim A, Abdollahi M, Abdollahpour I, Abegaz KH. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. The Lancet.396(10258),1223-49 (2020). [DOI] [PMC free article] [PubMed]
- 9.Vos Theo, Lim Stephen S, Abbafati Cristiana, Abbas Kaja M, Abbasi Mohammad, Abbasifard Mitra, Abbasi-Kangevari Mohsen, Abbastabar Hedayat, Abd-Allah Foad, Abdelalim Ahmed, Abdollahi Mohammad, Abdollahpour Ibrahim, Abolhassani Hassan, Aboyans Victor, Abrams Elissa M, Abreu Lucas Guimarães, Abrigo Michael R M, Abu-Raddad Laith Jamal, Abushouk Abdelrahman I, Acebedo Alyssa, Ackerman Ilana N, Adabi Maryam, Adamu Abdu A, Adebayo Oladimeji M, Adekanmbi Victor, Adelson Jaimie D, Adetokunboh Olatunji O, Adham Davoud, Afshari Mahdi, Afshin Ashkan, Agardh Emilie E, Agarwal Gina, Agesa Kareha M, Aghaali Mohammad, Aghamir Seyed Mohammad Kazem, Agrawal Anurag, Ahmad Tauseef, Ahmadi Alireza, Ahmadi Mehdi, Ahmadieh Hamid, Ahmadpour Ehsan, Akalu Temesgen Yihunie, Akinyemi Rufus Olusola, Akinyemiju Tomi, Akombi Blessing, Al-Aly Ziyad, Alam Khurshid, Alam Noore, Alam Samiah, Alam Tahiya, Alanzi Turki M, Albertson Samuel B, Alcalde-Rabanal Jacqueline Elizabeth, Alema Niguse Meles, Ali Muhammad, Ali Saqib, Alicandro Gianfranco, Alijanzadeh Mehran, Alinia Cyrus, Alipour Vahid, Aljunid Syed Mohamed, Alla François, Allebeck Peter, Almasi-Hashiani Amir, Alonso Jordi, Al-Raddadi Rajaa M, Altirkawi Khalid A, Alvis-Guzman Nelson, Alvis-Zakzuk Nelson J, Amini Saeed, Amini-Rarani Mostafa, Aminorroaya Arya, Amiri Fatemeh, Amit Arianna Maever L, Amugsi Dickson A, Amul Gianna Gayle Herrera, Anderlini Deanna, Andrei Catalina Liliana, Andrei Tudorel, Anjomshoa Mina, Ansari Fereshteh, Ansari Iman, Ansari-Moghaddam Alireza, Antonio Carl Abelardo T, Antony Catherine M, Antriyandarti Ernoiz, Anvari Davood, Anwer Razique, Arabloo Jalal, Arab-Zozani Morteza, Aravkin Aleksandr Y, Ariani Filippo, Ärnlöv Johan, Aryal Krishna K, Arzani Afsaneh, Asadi-Aliabadi Mehran, Asadi-Pooya Ali A, Asghari Babak, Ashbaugh Charlie, Atnafu Desta Debalkie, Atre Sachin R, Ausloos Floriane, Ausloos Marcel, Ayala Quintanilla Beatriz Paulina, Ayano Getinet, Ayanore Martin Amogre, Aynalem Yared Asmare, Azari Samad, Azarian Ghasem, Azene Zelalem Nigussie, Babaee Ebrahim, Badawi Alaa, Bagherzadeh Mojtaba, Bakhshaei Mohammad Hossein, Bakhtiari Ahad, Balakrishnan Senthilkumar, Balalla Shivanthi, Balassyano Shelly, Banach Maciej, Banik Palash Chandra, Bannick Marlena S, Bante Agegnehu Bante, Baraki Adhanom Gebreegziabher, Barboza Miguel A, Barker-Collo Suzanne Lyn, Barthelemy Celine M, Barua Lingkan, Barzegar Akbar, Basu Sanjay, Baune Bernhard T, Bayati Mohsen, Bazmandegan Gholamreza, Bedi Neeraj, Beghi Ettore, Béjot Yannick, Bello Aminu K, Bender Rose G, Bennett Derrick A, Bennitt Fiona B, Bensenor Isabela M, Benziger Catherine P, Berhe Kidanemaryam, Bernabe Eduardo, Bertolacci Gregory J, Bhageerathy Reshmi, Bhala Neeraj, Bhandari Dinesh, Bhardwaj Pankaj, Bhattacharyya Krittika, Bhutta Zulfiqar A, Bibi Sadia, Biehl Molly H, Bikbov Boris, Bin Sayeed Muhammad Shahdaat, Biondi Antonio, Birihane Binyam Minuye, Bisanzio Donal, Bisignano Catherine, Biswas Raaj Kishore, Bohlouli Somayeh, Bohluli Mehdi, Bolla Srinivasa Rao Rao, Boloor Archith, Boon-Dooley Alexandra S, Borges Guilherme, Borzì Antonio Maria, Bourne Rupert, Brady Oliver J, Brauer Michael, Brayne Carol, Breitborde Nicholas J K, Brenner Hermann, Briant Paul Svitil, Briggs Andrew M, Briko Nikolay Ivanovich, Britton Gabrielle B, Bryazka Dana, Buchbinder Rachelle, Bumgarner Blair R, Busse Reinhard, Butt Zahid A, Caetano dos Santos Florentino Luciano, Cámera Luis LA Alberto, Campos-Nonato Ismael R, Car Josip, Cárdenas Rosario, Carreras Giulia, Carrero Juan J, Carvalho Felix, Castaldelli-Maia Joao Mauricio, Castañeda-Orjuela Carlos A, Castelpietra Giulio, Castle Chris D, Castro Franz, Catalá-López Ferrán, Causey Kate, Cederroth Christopher R, Cercy Kelly M, Cerin Ester, Chandan Joht Singh, Chang Alex R, Charlson Fiona J, Chattu Vijay Kumar, Chaturvedi Sarika, Chimed-Ochir Odgerel, Chin Ken Lee, Cho Daniel Youngwhan, Christensen Hanne, Chu Dinh-Toi, Chung Michael T, Cicuttini Flavia M, Ciobanu Liliana G, Cirillo Massimo, Collins Emma L, Compton Kelly, Conti Sara, Cortesi Paolo Angelo, Costa Vera Marisa, Cousin Ewerton, Cowden Richard G, Cowie Benjamin C, Cromwell Elizabeth A, Cross Di H, Crowe Christopher Stephen, Cruz Jessica A, Cunningham Matthew, Dahlawi Saad M A, Damiani Giovanni, Dandona Lalit, Dandona Rakhi, Darwesh Aso Mohammad, Daryani Ahmad, Das Jai K, Das Gupta Rajat, das Neves José, Dávila-Cervantes Claudio Alberto, Davletov Kairat, De Leo Diego, Dean Frances E, DeCleene Nicole K, Deen Amanda, Degenhardt Louisa, Dellavalle Robert Paul, Demeke Feleke Mekonnen, Demsie Desalegn Getnet, Denova-Gutiérrez Edgar, Dereje Nebiyu Dereje, Dervenis Nikolaos, Desai Rupak, Desalew Assefa, Dessie Getenet Ayalew, Dharmaratne Samath Dhamminda, Dhungana Govinda Prasad, Dianatinasab Mostafa, Diaz Daniel, Dibaji Forooshani Zahra Sadat, Dingels Zachary V, Dirac M Ashworth, Djalalinia Shirin, Do Hoa Thi, Dokova Klara, Dorostkar Fariba, Doshi Chirag P, Doshmangir Leila, Douiri Abdel, Doxey Matthew C, Driscoll Tim Robert, Dunachie Susanna J, Duncan Bruce B, Duraes Andre Rodrigues, Eagan Arielle Wilder, Ebrahimi Kalan Mohammad, Edvardsson David, Ehrlich Joshua R, El Nahas Nevine, El Sayed Iman, El Tantawi Maha, Elbarazi Iffat, Elgendy Islam Y, Elhabashy Hala Rashad, El-Jaafary Shaimaa I, Elyazar Iqbal RF, Emamian Mohammad Hassan, Emmons-Bell Sophia, Erskine Holly E, Eshrati Babak, Eskandarieh Sharareh, Esmaeilnejad Saman, Esmaeilzadeh Firooz, Esteghamati Alireza, Estep Kara, Etemadi Arash, Etisso Atkilt Esaiyas, Farahmand Mohammad, Faraj Anwar, Fareed Mohammad, Faridnia Roghiyeh, Farinha Carla Sofia e Sá, Farioli Andrea, Faro Andre, Faruque Mithila, Farzadfar Farshad, Fattahi Nazir, Fazlzadeh Mehdi, Feigin Valery L, Feldman Rachel, Fereshtehnejad Seyed-Mohammad, Fernandes Eduarda, Ferrari Alize J, Ferreira Manuela L, Filip Irina, Fischer Florian, Fisher James L, Fitzgerald Ryan, Flohr Carsten, Flor Luisa Sorio, Foigt Nataliya A, Folayan Morenike Oluwatoyin, Force Lisa M, Fornari Carla, Foroutan Masoud, Fox Jack T, Freitas Marisa, Fu Weijia, Fukumoto Takeshi, Furtado João M, Gad Mohamed M, Gakidou Emmanuela, Galles Natalie C, Gallus Silvano, Gamkrelidze Amiran, Garcia-Basteiro Alberto L, Gardner William M, Geberemariyam Biniyam Sahiledengle, Gebrehiwot Abiyu Mekonnen, Gebremedhin Ketema Bizuwork, Gebreslassie Assefa Ayalew Ayalew Ayalew, Gershberg Hayoon Anna, Gething Peter W, Ghadimi Maryam, Ghadiri Keyghobad, Ghafourifard Mansour, Ghajar Alireza, Ghamari Farhad, Ghashghaee Ahmad, Ghiasvand Hesam, Ghith Nermin, Gholamian Asadollah, Gilani Syed Amir, Gill Paramjit Singh, Gitimoghaddam Mojgan, Giussani Giorgia, Goli Srinivas, Gomez Ricardo Santiago, Gopalani Sameer Vali, Gorini Giuseppe, Gorman Taren M, Gottlich Harrison Chase, Goudarzi Houman, Goulart Alessandra C, Goulart Bárbara Niegia Garcia, Grada Ayman, Grivna Michal, Grosso Giuseppe, Gubari Mohammed Ibrahim Mohialdeen, Gugnani Harish Chander, Guimaraes Andre Luiz Sena, Guimarães Rafael Alves, Guled Rashid Abdi, Guo Gaorui, Guo Yuming, Gupta Rajeev, Haagsma Juanita A, Haddock Beatrix, Hafezi-Nejad Nima, Hafiz Abdul, Hagins Hailey, Haile Lydia M, Hall Brian J, Halvaei Iman, Hamadeh Randah R, Hamagharib Abdullah Kanaan, Hamilton Erin B, Han Chieh, Han Hannah, Hankey Graeme J, Haro Josep Maria, Harvey James D, Hasaballah Ahmed I, Hasanzadeh Amir, Hashemian Maryam, Hassanipour Soheil, Hassankhani Hadi, Havmoeller Rasmus J, Hay Roderick J, Hay Simon I, Hayat Khezar, Heidari Behnam, Heidari Golnaz, Heidari-Soureshjani Reza, Hendrie Delia, Henrikson Hannah J, Henry Nathaniel J, Herteliu Claudiu, Heydarpour Fatemeh, Hird Thomas R, Hoek Hans W, Hole Michael K, Holla Ramesh, Hoogar Praveen, Hosgood H Dean, Hosseinzadeh Mehdi, Hostiuc Mihaela, Hostiuc Sorin, Househ Mowafa, Hoy Damian G, Hsairi Mohamed, Hsieh Vivian Chia-rong, Hu Guoqing, Huda Tanvir M, Hugo Fernando N, Huynh Chantal K, Hwang Bing-Fang, Iannucci Vincent C, Ibitoye Segun Emmanuel, Ikuta Kevin S, Ilesanmi Olayinka Stephen, Ilic Irena M, Ilic Milena D, Inbaraj Leeberk Raja, Ippolito Helen, Irvani Seyed Sina Naghibi, Islam M Mofizul, Islam MdMohaimenul, Islam Sheikh Mohammed Shariful, Islami Farhad, Iso Hiroyasu, Ivers Rebecca Q, Iwu Chidozie C D, Iyamu Ihoghosa Osamuyi, Jaafari Jalil, Jacobsen Kathryn H, Jadidi-Niaragh Farhad, Jafari Hussain, Jafarinia Morteza, Jahagirdar Deepa, Jahani Mohammad Ali, Jahanmehr Nader, Jakovljevic Mihajlo, Jalali Amir, Jalilian Farzad, James Spencer L, Janjani Hosna, Janodia Manthan Dilipkumar, Jayatilleke Achala Upendra, Jeemon Panniyammakal, Jenabi Ensiyeh, Jha Ravi Prakash, Jha Vivekanand, Ji John S, Jia Peng, John Oommen, John-Akinola Yetunde O, Johnson Catherine Owens, Johnson Sarah Charlotte, Jonas Jost B, Joo Tamas, Joshi Ankur, Jozwiak Jacek Jerzy, Jürisson Mikk, Kabir Ali, Kabir Zubair, Kalani Hamed, Kalani Rizwan, Kalankesh Leila R, Kalhor Rohollah, Kamiab Zahra, Kanchan Tanuj, Karami Matin Behzad, Karch André, Karim Mohd Anisul, Karimi Salah Eddin, Kassa Getachew Mullu, Kassebaum Nicholas J, Katikireddi Srinivasa Vittal, Kawakami Norito, Kayode Gbenga A, Keddie Suzanne H, Keller Cathleen, Kereselidze Maia, Khafaie Morteza Abdullatif, Khalid Nauman, Khan Maseer, Khatab Khaled, Khater Mona M, Khatib Mahalaqua Nazli, Khayamzadeh Maryam, Khodayari Mohammad Taghi, Khundkar Roba, Kianipour Neda, Kieling Christian, Kim Daniel, Kim Young-Eun, Kim Yun Jin, Kimokoti Ruth W, Kisa Adnan, Kisa Sezer, Kissimova-Skarbek Katarzyna, Kivimäki Mika, Kneib Cameron J, Knudsen Ann Kristin Skrindo, Kocarnik Jonathan M, Kolola Tufa, Kopec Jacek A, Kosen Soewarta, Koul Parvaiz A, Koyanagi Ai, Kravchenko Michael A, Krishan Kewal, Krohn Kris J, Kuate Defo Barthelemy, Kucuk Bicer Burcu, Kumar G Anil, Kumar Manasi, Kumar Pushpendra, Kumar Vivek, Kumaresh Girikumar, Kurmi Om P, Kusuma Dian, Kyu Hmwe Hmwe, La Vecchia Carlo, Lacey Ben, Lal Dharmesh Kumar, Lalloo Ratilal, Lam Jennifer O, Lami Faris Hasan, Landires Iván, Lang Justin J, Lansingh Van Charles, Larson Samantha Leigh, Larsson Anders O, Lasrado Savita, Lassi Zohra S, Lau Kathryn Mei-Ming, Lavados Pablo M, Lazarus Jeffrey V, Ledesma Jorge R, Lee Paul H, Lee Shaun Wen Huey, LeGrand Kate E, Leigh James, Leonardi Matilde, Lescinsky Haley, Leung Janni, Levi Miriam, Lewington Sarah, Li Shanshan, Lim Lee-Ling, Lin Christine, Lin Ro-Ting, Linehan Christine, Linn Shai, Liu Hung-Chun, Liu Shiwei, Liu Zichen, Looker Katharine J, Lopez Alan D, Lopukhov Platon D, Lorkowski Stefan, Lotufo Paulo A, Lucas Tim C D, Lugo Alessandra, Lunevicius Raimundas, Lyons Ronan A, Ma Jianing, MacLachlan Jennifer H, Maddison Emilie R, Maddison Ralph, Madotto Fabiana, Mahasha Phetole Walter, Mai Hue Thi, Majeed Azeem, Maled Venkatesh, Maleki Shokofeh, Malekzadeh Reza, Malta Deborah Carvalho, Mamun Abdullah A, Manafi Amir, Manafi Navid, Manguerra Helena, Mansouri Borhan, Mansournia Mohammad Ali, Mantilla Herrera Ana M, Maravilla Joemer C, Marks Ashley, Martins-Melo Francisco Rogerlândio, Martopullo Ira, Masoumi Seyedeh Zahra, Massano João, Massenburg Benjamin Ballard, Mathur Manu Raj, Maulik Pallab K, McAlinden Colm, McGrath John J, McKee Martin, Mehndiratta Man Mohan, Mehri Fereshteh, Mehta Kala M, Meitei Wahengbam Bigyananda, Memiah Peter T N, Mendoza Walter, Menezes Ritesh G, Mengesha Endalkachew Worku, Mengesha Meresa Berwo, Mereke Alibek, Meretoja Atte, Meretoja Tuomo J, Mestrovic Tomislav, Miazgowski Bartosz, Miazgowski Tomasz, Michalek Irmina Maria, Mihretie Kebadnew Mulatu, Miller Ted R, Mills Edward J, Mirica Andreea, Mirrakhimov Erkin M, Mirzaei Hamed, Mirzaei Maryam, Mirzaei-Alavijeh Mehdi, Misganaw Awoke Temesgen, Mithra Prasanna, Moazen Babak, Moghadaszadeh Masoud, Mohamadi Efat, Mohammad Dara K, Mohammad Yousef, Mohammad Gholi Mezerji Naser, Mohammadian-Hafshejani Abdollah, Mohammadifard Noushin, Mohammadpourhodki Reza, Mohammed Shafiu, Mokdad Ali H, Molokhia Mariam, Momen Natalie C, Monasta Lorenzo, Mondello Stefania, Mooney Meghan D, Moosazadeh Mahmood, Moradi Ghobad, Moradi Masoud, Moradi-Lakeh Maziar, Moradzadeh Rahmatollah, Moraga Paula, Morales Linda, Morawska Lidia, Moreno Velásquez Ilais, Morgado-da-Costa Joana, Morrison Shane Douglas, Mosser Jonathan F, Mouodi Simin, Mousavi Seyyed Meysam, Mousavi Khaneghah Amin, Mueller Ulrich Otto, Munro Sandra B, Muriithi Moses K, Musa Kamarul Imran, Muthupandian Saravanan, Naderi Mehdi, Nagarajan Ahamarshan Jayaraman, Nagel Gabriele, Naghshtabrizi Behshad, Nair Sanjeev, Nandi Anita K, Nangia Vinay, Nansseu Jobert Richie, Nayak Vinod C, Nazari Javad, Negoi Ionut, Negoi Ruxandra Irina, Netsere Henok Biresaw Netsere, Ngunjiri Josephine W, Nguyen Cuong Tat, Nguyen Jason, Nguyen Michele, Nguyen Minh, Nichols Emma, Nigatu Dabere, Nigatu Yeshambel T, Nikbakhsh Rajan, Nixon Molly R, Nnaji Chukwudi A, Nomura Shuhei, Norrving Bo, Noubiap Jean Jacques, Nowak Christoph, Nunez-Samudio Virginia, Oţoiu Adrian, Oancea Bogdan, Odell Christopher M, Ogbo Felix Akpojene, Oh In-Hwan, Okunga Emmanuel Wandera, Oladnabi Morteza, Olagunju Andrew T, Olusanya Bolajoko Olubukunola, Olusanya Jacob Olusegun, Oluwasanu Mojisola Morenike, Omar Bali Ahmed, Omer Muktar Omer, Ong Kanyin L, Onwujekwe Obinna E, Orji Aislyn U, Orpana Heather M, Ortiz Alberto, Ostroff Samuel M, Otstavnov Nikita, Otstavnov Stanislav S, Øverland Simon, Owolabi Mayowa O, P A Mahesh, Padubidri Jagadish Rao, Pakhare Abhijit P, Palladino Raffaele, Pana Adrian, Panda-Jonas Songhomitra, Pandey Anamika, Park Eun-Kee, Parmar Priya G Kumari, Pasupula Deepak Kumar, Patel Sangram Kishor, Paternina-Caicedo Angel J, Pathak Ashish, Pathak Mona, Patten Scott B, Patton George C, Paudel Deepak, Pazoki Toroudi Hamidreza, Peden Amy E, Pennini Alyssa, Pepito Veincent Christian Filipino, Peprah Emmanuel K, Pereira Alexandre, Pereira David M, Perico Norberto, Pham Hai Quang, Phillips Michael R, Pigott David M, Pilgrim Thomas, Pilz Tessa M, Pirsaheb Meghdad, Plana-Ripoll Oleguer, Plass Dietrich, Pokhrel Khem Narayan, Polibin Roman V, Polinder Suzanne, Polkinghorne Kevan R, Postma Maarten J, Pourjafar Hadi, Pourmalek Farshad, Pourmirza Kalhori Reza, Pourshams Akram, Poznańska Anna, Prada Sergio I, Prakash V, Pribadi Dimas Ria Angga, Pupillo Elisabetta, Quazi Syed Zahiruddin, Rabiee Mohammad, Rabiee Navid, Radfar Amir, Rafiee Ata, Rafiei Alireza, Raggi Alberto, Rahimi-Movaghar Afarin, Rahman Muhammad Aziz, Rajabpour-Sanati Ali, Rajati Fatemeh, Ramezanzadeh Kiana, Ranabhat Chhabi Lal, Rao Puja C, Rao Sowmya J, Rasella Davide, Rastogi Prateek, Rathi Priya, Rawaf David Laith, Rawaf Salman, Rawal Lal, Razo Christian, Redford Sofia Boston, Reiner Robert C, Reinig Nickolas, Reitsma Marissa Bettay, Remuzzi Giuseppe, Renjith Vishnu, Renzaho Andre M N, Resnikoff Serge, Rezaei Nima, Rezai Mohammad sadegh, Rezapour Aziz, Rhinehart Phoebe-Anne, Riahi Seyed Mohammad, Ribeiro Antonio Luiz P, Ribeiro Daniel Cury, Ribeiro Daniela, Rickard Jennifer, Roberts Nicholas L S, Roberts Shaun, Robinson Stephen R, Roever Leonardo, Rolfe Sam, Ronfani Luca, Roshandel Gholamreza, Roth Gregory A, Rubagotti Enrico, Rumisha Susan Fred, Sabour Siamak, Sachdev Perminder S, Saddik Basema, Sadeghi Ehsan, Sadeghi Masoumeh, Saeidi Shahram, Safi Sare, Safiri Saeid, Sagar Rajesh, Sahebkar Amirhossein, Sahraian Mohammad Ali, Sajadi S Mohammad, Salahshoor Mohammad Reza, Salamati Payman, Salehi Zahabi Saleh, Salem Hosni, Salem Marwa R Rashad, Salimzadeh Hamideh, Salomon Joshua A, Salz Inbal, Samad Zainab, Samy Abdallah M, Sanabria Juan, Santomauro Damian Francesco, Santos Itamar S, Santos João Vasco, Santric-Milicevic Milena M, Saraswathy Sivan Yegnanarayana Iyer, Sarmiento-Suárez Rodrigo, Sarrafzadegan Nizal, Sartorius Benn, Sarveazad Arash, Sathian Brijesh, Sathish Thirunavukkarasu, Sattin Davide, Sbarra Alyssa N, Schaeffer Lauren E, Schiavolin Silvia, Schmidt Maria Inês, Schutte Aletta Elisabeth, Schwebel David C, Schwendicke Falk, Senbeta Anbissa Muleta, Senthilkumaran Subramanian, Sepanlou Sadaf G, Shackelford Katya Anne, Shadid Jamileh, Shahabi Saeed, Shaheen Amira A, Shaikh Masood Ali, Shalash Ali S, Shams-Beyranvand Mehran, Shamsizadeh Morteza, Shannawaz Mohammed, Sharafi Kiomars, Sharara Fablina, Sheena Brittney S, Sheikhtaheri Abbas, Shetty Ranjitha S, Shibuya Kenji, Shiferaw Wondimeneh Shibabaw, Shigematsu Mika, Shin Jae Il, Shiri Rahman, Shirkoohi Reza, Shrime Mark G, Shuval Kerem, Siabani Soraya, Sigfusdottir Inga Dora, Sigurvinsdottir Rannveig, Silva João Pedro, Simpson Kyle E, Singh Ambrish, Singh Jasvinder A, Skiadaresi Eirini, Skou Søren T Skou, Skryabin Valentin Yurievich, Sobngwi Eugene, Sokhan Anton, Soltani Shahin, Sorensen Reed J D, Soriano Joan B, Sorrie Muluken Bekele, Soyiri Ireneous N, Sreeramareddy Chandrashekhar T, Stanaway Jeffrey D, Stark Benjamin A, Ştefan Simona Cătălina, Stein Caroline, Steiner Caitlyn, Steiner Timothy J, Stokes Mark A, Stovner Lars Jacob, Stubbs Jacob L, Sudaryanto Agus, Sufiyan Mu'awiyyah Babale, Sulo Gerhard, Sultan Iyad, Sykes Bryan L, Sylte Dillon O, Szócska Miklós, Tabarés-Seisdedos Rafael, Tabb Karen M, Tadakamadla Santosh Kumar, Taherkhani Amir, Tajdini Masih, Takahashi Ken, Taveira Nuno, Teagle Whitney L, Teame Hirut, Tehrani-Banihashemi Arash, Teklehaimanot Berhane Fseha, Terrason Sonyah, Tessema Zemenu Tadesse, Thankappan Kavumpurathu Raman, Thomson Azalea M, Tohidinik Hamid Reza, Tonelli Marcello, Topor-Madry Roman, Torre Anna E, Touvier Mathilde, Tovani-Palone Marcos Roberto Roberto, Tran Bach Xuan, Travillian Ravensara, Troeger Christopher E, Truelsen Thomas Clement, Tsai Alexander C, Tsatsakis Aristidis, Tudor Car Lorainne, Tyrovolas Stefanos, Uddin Riaz, Ullah Saif, Undurraga Eduardo A, Unnikrishnan Bhaskaran, Vacante Marco, Vakilian Alireza, Valdez Pascual R, Varughese Santosh, Vasankari Tommi Juhani, Vasseghian Yasser, Venketasubramanian Narayanaswamy, Violante Francesco S, Vlassov Vasily, Vollset Stein Emil, Vongpradith Avina, Vukovic Ana, Vukovic Rade, Waheed Yasir, Walters Madgalene K, Wang Jiayu, Wang Yafeng, Wang Yuan-Pang, Ward Joseph L, Watson Alexandrea, Wei Jingkai, Weintraub Robert G, Weiss Daniel J, Weiss Jordan, Westerman Ronny, Whisnant Joanna L, Whiteford Harvey A, Wiangkham Taweewat, Wiens Kirsten E, Wijeratne Tissa, Wilner Lauren B, Wilson Shadrach, Wojtyniak Bogdan, Wolfe Charles D A, Wool Eve E, Wu Ai-Min, Wulf Hanson Sarah, Wunrow Han Yong, Xu Gelin, Xu Rixing, Yadgir Simon, Yahyazadeh Jabbari Seyed Hossein, Yamagishi Kazumasa, Yaminfirooz Mousa, Yano Yuichiro, Yaya Sanni, Yazdi-Feyzabadi Vahid, Yearwood Jamal A, Yeheyis Tomas Y, Yeshitila Yordanos Gizachew, Yip Paul, Yonemoto Naohiro, Yoon Seok-Jun, Yoosefi Lebni Javad, Younis Mustafa Z, Younker Theodore Patrick, Yousefi Zabihollah, Yousefifard Mahmoud, Yousefinezhadi Taraneh, Yousuf Abdilahi Yousuf, Yu Chuanhua, Yusefzadeh Hasan, Zahirian Moghadam Telma, Zaki Leila, Zaman Sojib Bin, Zamani Mohammad, Zamanian Maryam, Zandian Hamed, Zangeneh Alireza, Zastrozhin Mikhail Sergeevich, Zewdie Kaleab Alemayehu, Zhang Yunquan, Zhang Zhi-Jiang, Zhao Jeff T, Zhao Yingxi, Zheng Peng, Zhou Maigeng, Ziapour Arash, Zimsen Stephanie R M, Naghavi Mohsen, Murray Christopher J L. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. The Lancet. 2020;396(10258):1204–1222. doi: 10.1016/S0140-6736(20)30925-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang H, Abbas KM, Abbasifard M, et al. Global age-sex-specific fertility, mortality, healthy life expectancy (HALE), and population estimates in 204 countries and territories, 1950–2019: A comprehensive demographic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1160–1203. doi: 10.1016/S0140-6736(20)30977-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bell NS, Amoroso PJ, Yore MM, et al. Self-reported risk-taking behaviors and hospitalization for motor vehicle injury among active duty army personnel. Am. J. Prev. Med. 2000;18:85–95. doi: 10.1016/S0749-3797(99)00168-3. [DOI] [PubMed] [Google Scholar]
- 12.Wang Y. Smoothing Splines: Methods and Applications. Chapman and Hall/CRC; 2011. [Google Scholar]
- 13.Program JR. Version 4.7. 0.0-February 2019; Statistical Methodology and Applications Branch, Surveillance Research Program. National Cancer Institute; 2019. [Google Scholar]
- 14.Kim H-J, Fay MP, Feuer EJ, et al. Permutation tests for joinpoint regression with applications to cancer rates. Stat. Med. 2000;19:335–351. doi: 10.1002/(SICI)1097-0258(20000215)19:3<335::AID-SIM336>3.0.CO;2-Z. [DOI] [PubMed] [Google Scholar]
- 15.Rehm J, Room R, Monteiro M, et al. Alcohol as a risk factor for global burden of disease. Eur. Addict. Res. 2003;9:157–164. doi: 10.1159/000072222. [DOI] [PubMed] [Google Scholar]
- 16.Griswold MG, Fullman N, Hawley C, et al. Alcohol use and burden for 195 countries and territories, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2018;392:1015–1035. doi: 10.1016/S0140-6736(18)31310-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Flor LS, Gakidou E. The burden of alcohol use: Better data and strong policies towards a sustainable development. Lancet Public Health. 2020;5:e10–e11. doi: 10.1016/S2468-2667(19)30254-3. [DOI] [PubMed] [Google Scholar]
- 18.Manthey J, Shield KD, Rylett M, et al. Global alcohol exposure between 1990 and 2017 and forecasts until 2030: A modelling study. Lancet. 2019;393:2493–2502. doi: 10.1016/S0140-6736(18)32744-2. [DOI] [PubMed] [Google Scholar]
- 19.Shokoohi M, Rahimi-Movaghar A, Noroozi A, et al. A public health approach to alcohol use and its related harms in Iran. Lancet Public Health. 2019;4:e175–e176. doi: 10.1016/S2468-2667(19)30038-6. [DOI] [PubMed] [Google Scholar]
- 20.Probst C, Manthey J, Rehm J. Understanding the prevalence of lifetime abstinence from alcohol: An ecological study. Drug. Alcohol Depend. 2017;178:126–129. doi: 10.1016/j.drugalcdep.2017.05.008. [DOI] [PubMed] [Google Scholar]
- 21.Wilsnack RW, Vogeltanz ND, Wilsnack SC, et al. Gender differences in alcohol consumption and adverse drinking consequences: Cross-cultural patterns. Addiction. 2000;95:251–265. doi: 10.1046/j.1360-0443.2000.95225112.x. [DOI] [PubMed] [Google Scholar]
- 22.Chegeni M, Kamel Khodabandeh A, Karamouzian M, et al. Alcohol consumption in Iran: A systematic review and meta-analysis of the literature. Drug Alcohol Rev. 2020;39:525–538. doi: 10.1111/dar.13093. [DOI] [PubMed] [Google Scholar]
- 23.Hassanian-Moghaddam H, Nikfarjam A, Mirafzal A, et al. Methanol mass poisoning in Iran: Role of case finding in outbreak management. J. Public Health. 2015;37:354–359. doi: 10.1093/pubmed/fdu038. [DOI] [PubMed] [Google Scholar]
- 24.Lankarani KB, Afshari R. Alcohol consumption in Iran. Lancet. 2014;384:1927–1928. doi: 10.1016/S0140-6736(14)62279-0. [DOI] [PubMed] [Google Scholar]
- 25.Lien L, Hauff E, Martinez P, et al. Alcohol use in South Sudan in relation to social factors, mental distress and traumatic events. BMC Public Health. 2016;16:937. doi: 10.1186/s12889-016-3605-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wakabi W. South Sudan faces grim health and humanitarian situation. Lancet. 2011;377:2167–2168. doi: 10.1016/S0140-6736(11)60946-X. [DOI] [PubMed] [Google Scholar]
- 27.Sepanlou SG, Safiri S, Bisignano C, et al. The global, regional, and national burden of cirrhosis by cause in 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol. Hepatol. 2020;5:245–266. doi: 10.1016/S2468-1253(19)30349-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rehm J, Shield KD. Global burden of alcohol use disorders and alcohol liver disease. Biomedicines. 2019;7:99. doi: 10.3390/biomedicines7040099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schwarzinger M, Baillot S, Yazdanpanah Y, et al. Contribution of alcohol use disorders on the burden of chronic hepatitis C in France, 2008–2013: A nationwide retrospective cohort study. J. Hepatol. 2017;67:454–461. doi: 10.1016/j.jhep.2017.03.031. [DOI] [PubMed] [Google Scholar]
- 30.Alavi M, Janjua NZ, Chong M, et al. The contribution of alcohol use disorder to decompensated cirrhosis among people with hepatitis C: An international study. J. Hepatol. 2018;68:393–401. doi: 10.1016/j.jhep.2017.10.019. [DOI] [PubMed] [Google Scholar]
- 31.Hassan MM, Hwang L-Y, Hatten CJ, et al. Risk factors for hepatocellular carcinoma: Synergism of alcohol with viral hepatitis and diabetes mellitus. Hepatology. 2002;36:1206–1213. doi: 10.1053/jhep.2002.36780. [DOI] [PubMed] [Google Scholar]
- 32.Donato F. Alcohol and hepatocellular carcinoma: The effect of lifetime intake and hepatitis virus infections in men and women. Am. J. Epidemiol. 2002;155:323–331. doi: 10.1093/aje/155.4.323. [DOI] [PubMed] [Google Scholar]
- 33.Zeng D-Y, Li J-M, Lin S, et al. Global burden of acute viral hepatitis and its association with socioeconomic development status, 1990–2019. J. Hepatol. 2021;75:547–556. doi: 10.1016/j.jhep.2021.04.035. [DOI] [PubMed] [Google Scholar]
- 34.Lachenmeier DW, Monakhova YB, Rehm J. Influence of unrecorded alcohol consumption on liver cirrhosis mortality. World J. Gastroenterol. 2014;20:7217. doi: 10.3748/wjg.v20.i23.7217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rehm J, Kanteres F, Lachenmeier DW. Unrecorded consumption, quality of alcohol and health consequences. Drug Alcohol Rev. 2010;29:426–436. doi: 10.1111/j.1465-3362.2009.00140.x. [DOI] [PubMed] [Google Scholar]
- 36.Rehm J, Gmel GE, Sr, Gmel G, et al. The relationship between different dimensions of alcohol use and the burden of disease: An update. Addiction. 2017;112:968–1001. doi: 10.1111/add.13757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Massoumi G, Saberi K, Eizadi-Mood N, et al. Methanol poisoning in Iran, from 2000 to 2009. Drug Chem. Toxicol. 2012;35(330–333):20120131. doi: 10.3109/01480545.2011.619193. [DOI] [PubMed] [Google Scholar]
- 38.Rumgay H, Shield K, Charvat H, et al. Global burden of cancer in 2020 attributable to alcohol consumption: A population-based study. Lancet Oncol. 2021;22:1071–1080. doi: 10.1016/S1470-2045(21)00279-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Seitz HK, Becker P. Alcohol metabolism and cancer risk. Alcohol Res. Health. 2007;30:38–47. [PMC free article] [PubMed] [Google Scholar]
- 40.Brooks PJ, Theruvathu JA. DNA adducts from acetaldehyde: Implications for alcohol-related carcinogenesis. Alcohol. 2005;35:187–193. doi: 10.1016/j.alcohol.2005.03.009. [DOI] [PubMed] [Google Scholar]
- 41.Bagnardi V, Rota M, Botteri E, et al. Alcohol consumption and site-specific cancer risk: A comprehensive dose-response meta-analysis. Br. J. Cancer. 2015;112:580–593. doi: 10.1038/bjc.2014.579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Singletary KW, Gapstur SM. Alcohol and breast cancer: Review of epidemiologic and experimental evidence and potential mechanisms. JAMA. 2001;286:2143–2151. doi: 10.1001/jama.286.17.2143. [DOI] [PubMed] [Google Scholar]
- 43.Al-Ansari B, Thow AM, Day CA, et al. Extent of alcohol prohibition in civil policy in Muslim majority countries: The impact of globalization. Addiction. 2016;111:1703–1713. doi: 10.1111/add.13159. [DOI] [PubMed] [Google Scholar]
- 44.Zhao J, Stockwell T, Vallance K, et al. The effects of alcohol warning labels on population alcohol consumption: An interrupted time series analysis of alcohol sales in Yukon, Canada. J. Stud. Alcohol Drugs. 2020;81:225–237. doi: 10.15288/jsad.2020.81.225. [DOI] [PubMed] [Google Scholar]
- 45.Weerasinghe A, Schoueri-Mychasiw N, Vallance K, et al. Improving knowledge that alcohol can cause cancer is associated with consumer support for alcohol policies: Findings from a real-world alcohol labelling study. Int. J. Environ. Res. Public Health. 2020;17:398. doi: 10.3390/ijerph17020398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.World Health Organization. ‘Best Buys’ and Other Recommended Interventions for the Prevention and Control of Noncommunicable Diseases. https://apps.who.int/iris/bitstream/handle/10665/259232/WHO-NMH-NVI-17.9-eng.pdf (2022).
- 47.World Health Organization. Global Strategy to Reduce the Harmful Use of Alcohol. https://www.who.int/substance_abuse/alcstratenglishfinal.pdf (2022). [DOI] [PMC free article] [PubMed]
- 48.Wetterling T, Veltrup C, Driessen M, et al. Drinking pattern and alcohol-related medical disorders. Alcohol Alcohol. 1999;34:330–336. doi: 10.1093/alcalc/34.3.330. [DOI] [PubMed] [Google Scholar]
- 49.Salaspuro M, Salaspuro V, Seitz HK. Interaction of Alcohol and Tobacco in Upper Aerodigestive Tract and Stomach Cancer. Alcohol, tobacco and cancer. Karger Publishers; 2006. pp. 48–62. [Google Scholar]
- 50.Prabhu A, Obi KO, Rubenstein JH. The synergistic effects of alcohol and tobacco consumption on the risk of esophageal squamous cell carcinoma: A meta-analysis. J. Am. Coll. Gastroenterol. 2014;109:822–827. doi: 10.1038/ajg.2014.71. [DOI] [PubMed] [Google Scholar]
- 51.Mello FW, Melo G, Pasetto JJ, et al. The synergistic effect of tobacco and alcohol consumption on oral squamous cell carcinoma: A systematic review and meta-analysis. Clin. Oral Invest. 2019;23:2849–2859. doi: 10.1007/s00784-019-02958-1. [DOI] [PubMed] [Google Scholar]
- 52.Schomerus G, Lucht M, Holzinger A, et al. The stigma of alcohol dependence compared with other mental disorders: A review of population studies. Alcohol Alcohol. 2011;46:105–112. doi: 10.1093/alcalc/agq089. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data used for these analyses are all publicly available at http://ghdx.healthdata.org/gbd-results-tool.