Objectives
Although video visits may offer some benefits over the telephone, not all patients may be equipped to access video telemedicine, raising questions surrounding access disparities. The aim of this study is to examine patient characteristics associated with the use of phone versus video-enabled tele-medication for opioid use disorders (MOUD) during COVID-19.
Methods
This study uses data from a nonurban integrated substance use disorder treatment site in New York to examine patient characteristics associated with the modality of tele-MOUD care. The provider did not offer in-person care. Multivariable regression models were used to assess the association between patient’s primary mode of tele-MOUD and patient demographic characteristics. Additional analysis of new patient inductions examined associations between mode of tele-MOUD induction and 30-day follow-up receipt.
Results
Of the 4557 tele-MOUD encounters, 76.92% were video and 23.08% were telephone visits. Older patients had significantly higher odds of primarily using telephone (odds ratio [OR]: 0.580; 95% confidence interval [CI]: 0.045, 1.115). Patients with higher education (OR: –0.791; 95% CI: –1.418, –0.168), recent overdose (OR: –0.40; 95% CI: –0.793, –0.010), and new patients (OR: 0.484; 95% CI: –0.945, 0.023) were significantly less likely to rely on telephone. Of 336 new patient initiations, 31 were conducted by telephone while 305 were conducted through video. The mode of new patient initiation was not associated with a follow-up visit within 30 days of initiation.
Conclusions
Telemedicine may increase access to MOUD, though certain patients may rely on different forms of telemedicine. Attention must be paid to policies that promote equitable access to both video and telephone tele-MOUD visits.
Key Words: buprenorphine, COVID-19, healthcare disparities, opioid-related disorders, telemedicine
The convergence of the COVID-19 pandemic on the opioid crisis has intensified challenges for people struggling with addiction across the U.S. Over 93,000 overdose deaths occurred in 2020, highlighting the need to urgently expand access to substance use disorder (SUD) treatment using an approach that limits in-person interactions.1 In recognition of the public health emergency, the U.S. Drug Enforcement Administration and Department of Health and Human Services relaxed restrictions on use of telemedicine to admit and treat new patients with opioid use disorder (OUD) using controlled substances including buprenorphine early in the pandemic, initially by allowing for telemedicine visits that used audio-visual platforms, and subsequently expanding flexibilities to include audio-only visits.2 As a result, many SUD treatment providers pivoted to telemedicine as their primary means of providing medication for opioid use disorders (MOUD).3,4
Telemedicine is the practice of using technology to deliver medical care at a distance; this includes both video and phone modalities.5,6 The benefits of telemedicine during a respiratory-spread pandemic are many. For patients, telemedicine affords greater flexibility in appointment times and virtual medication management, and lowers traditional barriers such as lack of transportation and physical distance.7–9 SUD treatment providers using telemedicine meanwhile report reductions in no-show rates, improved quality of patient interactions, and comparable treatment outcomes including reduced illicit drug use and patient retention compared to in-person programs.9–14 For both patients and providers, telemedicine provides a means to stay connected while reducing unnecessary contact or exposure.
However, although the potential benefits of telemedicine for OUD are clear, much less is known about the potential disparities arising from its rapid expansion. Patients face multiple barriers to accessing some forms of telemedicine such as video, including absence of technology, digital literacy, and reliable internet coverage.15 These barriers are more commonly experienced by low-income populations that were disproportionately affected by COVID-19. A quarter of adults with incomes below $30,000 a year do not own a smartphone.16 Similarly, a sizable proportion of adults with lower incomes do not have home broadband (43%) or a laptop (41%).16 Studies conducted in broader medical settings found that older, low-income, and less educated patients are less likely to use video-enabled telehealth.15,17,18 These disparities in access are likely to be amplified in SUD treatment settings, given the concentration of the opioid epidemic among lowincome populations.19
Qualitative studies conducted early in the pandemic suggest that equity in treatment access by modality remains a key concern among SUD treatment providers. In 1 study of 18 providers in 10 sites, providers noted many patients of low socioeconomic status lacked access to video-enabled devices.12 Similarly, a study of telemedicine for MOUD found video visits were “almost impossible” for patients with very limited resources.3 These findings suggest that inequities may exist in accessing video-enabled tele-MOUD services. However, very few studies to date have examined this issue using quantitative data in SUD treatment settings.
One study examined patient characteristics associated with the use of tele-MOUD in the veteran’s administration health system,13 and found that tele-MOUD patients were less likely to be male or Black than patients only receiving in-person care, raising concerns around equity for telemedicine-delivered buprenorphine. However, the study was conducted before COVID-19, among a specific population (veterans), and did not specifically distinguish between telemedicine modalities. More recent studies examining the issue of tele-MOUD access equity following COVID-19 found that patients who were older and had a lower household income were less likely to have a telemedicine buprenorphine induction,20 and that patients who utilized tele buprenorphine were primarily male,21 younger,22 and had Medicaid as their primary source of insurance.22 However, these studies did not distinguish between the use of different modes of tele-MOUD access through phone or video.
Understanding different patient characteristics associated with the modality of tele-MOUD care received during the COVID-19 pandemic is critical given continued discussions regarding the future of telemedicine policy. Broader surveys conducted early in the pandemic found that nearly half (48%) of buprenorphine providers reported initiating buprenorphine by phone, suggesting that telephone plays a critical role in ensuring access.23 Yet proposed policies at this stage of the public health emergency favor video over phone. For example, the recently introduced Telehealth Response for E-prescribing Addiction Therapy Services (TREATS) Act proposes to permanently expand telehealth services for SUD treatment by permitting buprenorphine treatment to be initiated over telehealth.24 (TREATS Act, 2021). However, the proposed legislation mandates the consultation occur using an audiovisual platform. As lawmakers consider permanent changes to telemedicine policies, ongoing research is needed to examine the factors that may affect the adoption of both telephone and video-enabled SUD treatment visits for different patient populations, and the role of phone and video-based tele-MOUD use along access, quality, and equity considerations.
The aim of this study is to examine patient characteristics associated with the use of phone versus video-enabled tele-MOUD during COVID-19. This study uses data from a comprehensive intake assessment and electronic health records (EHR) data from 1 nonurban integrated SUD treatment site in New York to illustrate visit patterns over the course of the pandemic and to examine patient characteristics associated with the modality of tele-MOUD care access. We also examine differences in patient characteristics associated with new MOUD inductions via telephone versus video, and the relationship between video versus telephone inductions and the receipt of follow-up care within 30 days, a standard measure of patient engagement and quality.
METHODS
REACH Medical (Respectful Equitable Access to Compassionate Healthcare) is a low-threshold harm reduction medical practice located in Ithaca, New York\REACH serves several rural and urban communities across 32 counties and offers a variety of clinical services, including MOUD, hepatitis C testing and treatment, primary care, acute care, pre-exposure prophylaxis medication, postexposure prophylaxis medication, human immunodeficiency virus treatment, peer programs, care management, outreach services, naloxone training, and distribution and integrated behavioral health care.25 Over 90% of clients experience SUD.
REACH first implemented telemedicine using telephone and video in March 2020 when the clinic temporarily ceased all in-person encounters as a result of COVID-19, A total of 5494 telemedicine visits were completed by 803 patients between March and December 2020. Of these, approximately 80% were MOUD encounters (n = 4557) that were completed by 795 patients. The analytic sample for the study consists of the 795 patients who completed at least 1 MOUD visit in the timeframe.
We obtained patient information from a comprehensive intake assessment and visit information from EHR. The assessment totaled 110 questions and collected information on patient sociodemographic characteristics, quality of life, stigma, infectious disease history, and substance use history. EHR data included information on all encounters at REACH, including the date, type of visit (primary care, MOUD, other services), the modality of care (telephone vs video), and date of first encounter. MOUD encounters are based on the reason for visit, coded as chief complaint, in the EMR data. If the reason for visit is coded as “Medication Assisted Treatment,” the visit is categorized as MOUD. REACH is not licensed to provider methadone and less than 1% of the tele-MOUD visits between March and December 2020 were for medication other than buprenorphine.
For each patient, we constructed new variables measuring the total number of tele-MOUD visits completed during the study period, the proportion of tele-MOUD visits completed by phone or video, and whether 50% or more of their tele-MOUD encounters were through telephone (majority phone). Although we considered other categorizations (ie, patients who only used telephone vs patients who used video), we decided on “majority phone” categorization because only a small minority of patients relied solely on telephone (n = 19, 2.37%).
In bivariate analyses, we used chi-squared tests to assess the association between a patient’s majority treatment modality (%phone visits = >50%) and patient characteristics obtained from the intake assessment, including measures of race (White or other), age (younger than 50 or 50 and older), sex (male or female), housing status (no permanent housing or permanent housing), education (less than high school, high school, or more than high school), whether the person receives Supplemental Nutrition Assistance Program (SNAP) benefits (receives or does not receive SNAP), problems with mobility (does not have problems or does have problems with mobility), employment (full-time/part-time work or looking for work), patient overdose history (did the patient experience an overdose in the past 6 months), previous incarceration (was the patient incarcerated or detained within the past 6 months), insurance status (no insurance, Medicaid, Medicare, private insurance), and residence in a rural-designated zip code (yes or no).
In multivariable analyses, we used logistic regression to examine the relationship between the patient characteristics and a patient’s majority treatment modality. For ease of interpretation, we used predictive margins to report average adjusted probability and absolute risk differences, with 95% confidence intervals (CIs). For categorical variables, absolute risk difference represents the difference in adjusted probability of having 50% or more visits via telephone between patients with a given characteristic and the reference value. Missingness in the predictor variables ranged from 18% to 31.63%. To reduce bias from missing observations, missing values of predictor variables were imputed using multiple imputation by chained equations. Because visit patterns may differ between patients with more frequent and less frequent visits, we conducted a sub-analysis of patients who had 3 or more MOUD encounters during the study period (n = 680) (see Supplementary Material Table 1, http://links.lww.com/JAM/A338).
We also conducted an additional analysis of new patients to the clinic during the study period. New patients are identified as those whose first encounter date was between March and December 2020. New patients are of particular analytic interest because COVID-19 related policy changes allowed for induction of new patients using telephone and video – modalities that were previously not allowed under the Ryan Haight Act.26 Of the 795 individuals with at least 1 MOUD encounter during the study timeframe, 336 were new patients who initiated MOUD using telemedicine. We used chi-squared test to assess the association between patient’s mode of MOUD induction (telephone vs video) and sociodemographic characteristics. We also assessed bivariate associations between the patient’s mode of MOUD induction and receipt of follow-up care within 30 days of initial visit, a standard measure of patient engagement and quality. Statistical analyses were 2-tailed and conducted using Stata SE 16.1. (Statacorp, College Station, TX) Significance was established throughout at P < 0.05. This study of de-identified patient records was exempt from IRB review.
FINDINGS
A total of 4557 telemedicine visits for MOUD were completed by 795 patients from March 2020 to December 2020. Of these encounters, 76.92% (n = 3463) were video visits and 23.08% (n = 1039) were telephone visits. Figure 1 shows visit counts by modality per month\(March 2020).
FIGURE 1.
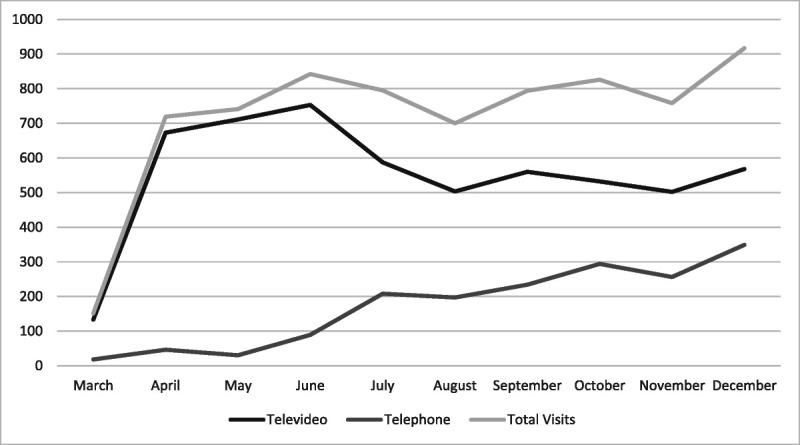
Tele-MOUD visits over time, March 2020-December 2020. MOUD indicates medication for opioid use disorders.
Most patients (80.8%) used video as their primary means of accessing tele-MOUD. However, a sizable minority relied mostly on telephone (19.2%). On average, patient in our sample completed 5.73 visits between March and December 2020, of which 4.35 were conducted over video and 1.3 conducted via phone. Patients were majority male (56.60%), White (94.59%), and had a mean age of 37.60 years, with the majority being younger than 50 (87.17%). Three quarters of patients were permanently housed (74.39%), whereas only one-third had full or part-time employment (34.9%). Most patients had Medicaid as their primary insurance (72.96%). Smaller proportions of patients were rural residents (41.31%), were incarcerated or detained in the past 6 months (19.24%), and had problems with mobility (17.35%). Approximately half of all patients (51%) received SNAP benefits, and a third experienced an overdose in the past 6 months (34%). Level of education varied among patients, with 46.0% having completed high school, 31.5% completing more than high school, and 22.4% not having completed high school. Table 1 shows demographic characteristics of patients who completed a telemedicine visit included in the study.
TABLE 1.
Descriptive Statistics and Bivariate Analyses
| Variable | All Patients (n = 795) |
Telephone Visits >=50 (n = 153) |
Video Visits >50 (n = 642) |
[P] |
|---|---|---|---|---|
| Number of MOUD encounters (n) | ||||
| Total number | 5.73 | 5.57 | 5.76 | |
| Video | 4.35 | 1.95 | 4.86 | |
| Phone | 1.30 | 3.59 | 0.75 | |
| Race | [0.066] | |||
| White | 94.59% | 91.27% | 95.39% | |
| Non-White | 5.41% | 8.73% | 4.61% | |
| Age | [0.012]** | |||
| Age < 50 | 87.17% | 81.05% | 88.62% | |
| Age > =50 | 12.83% | 18.95% | 11.38% | |
| Gender | [0.676] | |||
| Male | 43.60% | 58.17% | 56.31% | |
| Female | 56.60% | 41.83% | 43.69% | |
| Housing status | [0.064] | |||
| Have permanent housing | 25.61% | 67.97% | 75.95% | |
| No housing/unstably housed | 74.39% | 32.03% | 24.05% | |
| Education | [0.020]* | |||
| Less than high school | 22.45% | 29.27% | 20.79% | |
| High school | 46.02% | 48.78% | 45.35% | |
| More than high school | 31.53% | 21.95% | 33.86% | |
| SNAP benefits | [0.406] | |||
| No | 49% | 45.45% | 49.89% | |
| Yes | 51% | 54.55% | 50.11% | |
| Problems with mobility | [0.067] | |||
| No | 82.65% | 76.92%% | 84.09% | |
| Yes | 17.35% | 23.08% | 15.91% | |
| Employment status | [0.050]* | |||
| Full-time or part time work | 34.93% | 27.52% | 36.78% | |
| Unemployed/looking for work | 65.07% | 72.58% | 63.22% | |
| Overdose in past 6 months | [0.152] | |||
| No | 37.98% | 58.77% | 51.29% | |
| Yes | 34.00% | 41.23% | 48.71% | |
| Incarcerated in past 6 months | [0.931] | |||
| No | 80.76% | 80.49% | 80.83% | |
| Yes | 19.24% | 19.51% | 19.17% | |
| Insurance Status | [0.345] | |||
| Uninsured | 4.40% | 3.27% | 4.62% | |
| Medicaid | 72.96% | 78.43%% | 71.85% | |
| Medicare | 5.03% | 5.23% | 5.08% | |
| Privately Insured | 17.61% | 13.07% | 18.46 | |
| Rural Resident | [0.156]** | |||
| No | 58.69% | 64.05% | 57.85 | |
| Yes | 41.31% | 35.95% | 42.15 | |
| New patient | [0.000] | |||
| No | 55.04% | 62.75% | 53.23% | |
| Yes | 44.96% | 37.25% | 46.77% |
*P < 0.05.
**P < 0.01.
For bivariate analyses, we grouped patients based on their main tele-MOUD modality (phone vs video). Majority phone patients (n = 153) had slightly fewer total visits (5.57 visits) compared to patients who used mostly video (5.76 visits). Majority phone patients had an average of 3.59 phone visits and 1.95 video visits. In comparison, majority video patients had an average of 0.75 phone visits and 4.86 video visits from March to December 2020. Several socio-demographic characteristics were associated with reliance on telephone-enabled buprenorphine visits. Specifically, patients who were older than 50, unstably housed, had less education, had problems with mobility, and unemployed or looking for work were significantly more likely to rely on telephone as their primary means of tele-MOUD. New patients were significantly less likely to use telephone as their main modality of tele-MOUD access. Associations between patient sociodemographic characteristics and the primary modality used to access tele-MOUD are presented in Table 1. A sensitivity analysis of a subgroup of patients with 3 or more visits (n = 680) found similar results (see Supplementary Material Table 1, http://links.lww.com/JAM/A338).
In multivariable analysis several socio-demographic characteristics remained significant. Specifically, older patients had significantly higher odds of relying on telephone as their primary means to tele-MOUD (odds ratio [OR]: 0.580; 95% CI: 0.045, 1.115), whereas patients with more than a high school education (OR: –0.791; 95% CI: –1.418, –0.168), patients who experienced an overdose in the past 6 months (OR: –0.40; 95% CI: –0.793, –0.010), and new patients (OR: 0.484; 95% CI: –0.945, 0.023) were significantly less likely to rely on telephone as their primary means to tele-MOUD. The results of the multivariable analysis are presented in Table 2.
TABLE 2.
Adjusted Logistic Regression Estimating Association Between Patient Characteristics and Use of Telephone for 50% or More of Total MOUD Visits (n = 795)
| Variable | Odds Ratio (95% Confidence Interval) | P |
|---|---|---|
| Race | –0.206 (–1.023, 0.611) | 0.620 |
| Age | 0.580 (0.045, 1.115) | 0.034* |
| Gender | –0.010 (–0.400, 0.379) | 0.958 |
| Housing Status | –0.412 (–.908, 0.082) | 0.102 |
| Education status (ref = less than high school) | ||
| High school | –0.327 (–0.913, 0.257) | 0.267 |
| More than high school | –0.791 (–1.418, –0.168) | 0.013* |
| SNAP | –0.117 (–0.639, 0.405) | 0.655 |
| Problems with mobility | 0.366 (–0.155, 0.889) | 0.168 |
| Employment status | –0.209 (–0.700, 0.280) | 0.400 |
| Overdose in past 6 months | –0.484 (–0.945, 0.023) | 0.040* |
| Incarcerated or detained in past 6 months | –0.121 (–0.664, 0.422) | 0.661 |
| Insurance (ref = Medicaid) | ||
| Medicare | –0.228 (–1.079, 0.621) | 0.598 |
| No insurance | –0.632 (–1.649 0.384) | 0.223 |
| Privately Insured | –0.445 (–0.990, 0.099) | 0.109 |
| Rural | –0.274 (–0.674, 0.124) | 0.178 |
| New patient | –0.401 (–0.793, –0.010) | 0.044* |
| Number of MOUD encounters | –0.025 (–0.097, 0.045) | 0.475 |
*P < 0.05.
The analysis of new patients at the clinic (Table 3) found that\about 10% (n = 31) of new patient initiations were conducted via phone. Results from chi-squared tests assessing the association between the patient’s mode of MOUD induction and socio-demographic characteristics found that patients who had a first encounter via telephone were significantly less likely to have experienced an overdose in the past 6 months. Other socio-demographic characteristics were not statistically significant. A larger percentage of patients who initiated a telephone visit had a follow-up visit within 30 days of initiation, however, the different was not statistically significant.
TABLE 3.
Sub Analysis of Associations Between Patient Characteristics and Telemedicine Visit Modality by First Visit Modality
| Variable | Outcome: First Encounter Telephone (n = 31) | Outcome: First Encounter Video (n = 305) | P |
|---|---|---|---|
| Race | 1.00 | ||
| White | 95.65% | 95.65% | |
| Non-White | 4.35% | 4.35% | |
| Age | 0.087 | ||
| Age < 50 | 77.42% | 88.20% | |
| Age > =50 | 22.58% | 11.80% | |
| Gender | 0.700 | ||
| Male | 61.29% | 57.70% | |
| Female | 38.71% | 42.30% | |
| Housing status | 0.384 | ||
| Have permanent housing | 76.92% | 68.61% | |
| No housing/unstably housed | 23.08% | 31.39% | |
| Education | 0.136 | ||
| Less than high school | 30.77% | 23.53% | |
| High school | 53.85% | 41.63% | |
| More than high school | 25.38% | 34.84% | |
| SNAP benefits | 0.210 | ||
| No | 64.00% | 50.74% | |
| Yes | 36.00% | 49.26% | |
| Problems with mobility | 0.304 | ||
| No | 75.00% | 83.41% | |
| Yes | 25.00% | 16.59% | |
| Employment status | 0.624 | ||
| Full-time or part time work | 38.46% | 33.64% | |
| Unemployed or looking for work | 61.54% | 66.36% | |
| Overdose in past 6 months | 0.009* | ||
| No | 73.33% | 48.48% | |
| Yes | 26.67% | 51.52% | |
| Incarcerated or detained in past 6 months | 0.753 | ||
| No | 80.77% | 78.08% | |
| Yes | 19.23% | 21.92% | |
| Insurance status | 0.631 | ||
| Uninsured | 6.45% | 5.57% | |
| Medicaid | 64.52% | 73.77% | |
| Medicare | 3.23% | 3.93% | |
| Privately Insured | 25.81% | 16.72% | |
| Rural resident | 0.795 | ||
| No | 48.39% | 50.82% | |
| Yes | 51.61% | 49.18% | |
| 30-day follow-up visit | 0.218 | ||
| No | 6.45% | 14.43% | |
| Yes | 93.55% | 85.57% |
*P < 0.05.
SNAP indicates Supplemental Nutrition Assistance Program.
DISCUSSION
In this study of 1 integrated SUD treatment setting in New York State, we found that most tele-MOUD visits were conducted over video and the vast majority of patients used video as their primary means of accessing tele-MOUD. The relatively high proportion of video visits may be attributable to REACH’s model of tele-MOUD delivery, which utilized a team-based telemedicine model in which a team of administrative staff members, nurses, and providers work collaboratively to offer scheduled and routine visits to patients using phones, tablets, or laptops. Although the clinic offered phonebased visits, the clinic’s workflow attempted to first set up patients with video before moving to telephone. Therefore, although phone visits were provided, the majority of REACH patients defaulted to video. REACH’s telemedicine model has been highlighted in the evidence-based guide series for delivering telehealth for the treatment of SUDs by the Substance Abuse and Mental Health Services Administration.27
Yet, despite the efforts to move patients to video-based care, a sizable minority (19.05%) used telephone as their primary means to access care. Not surprisingly, we found that several patient socio-demographic characteristics were significantly associated with reliance on the telephone rather than video as their main mode of tele-MOUD access. In particular, older and less educated patients – those who also disproportionately experience a digital divide – were significantly more likely to rely on telephone, even after controlling for other socio-demographic characteristics. These findings echo results from broader medical settings15,28,29 and corroborate anecdotal evidence found in qualitative studies of buprenorphine providers during the COVID-19 pandemic who noted challenges of delivering video-enabled tele-MOUD to patients who had limited access to smartphones or internet coverage.3,12
Interestingly, patients who experienced an overdose in the past 6 months were significantly less likely to rely on telephone as their primary means of accessing tele-MOUD, and were less likely to initiate MOUD treatment through telephone. Given that patients with a recent history of overdose are more likely to be younger in age,30 this association may be attributable in part to the patient’s age. Similarly, new patients were significantly less likely to use telephone as their primary means of access, and almost 90% of tele-MOUD initiations were through video. It is possible that new patients entering treatment may be more motivated to comply with the clinic’s preference for audio-visual visits while more established patients use a modality that is most convenient for them.
There were no significant differences in one measure of OUD treatment quality – follow up within 30 days of initiation, suggesting that telephone does not necessarily result in lower quality care. This finding is important given the continuing policy discussions around the role both telephone and video in delivering tele-MOUD. Early in the pandemic, both Substance Abuse and Mental Health Services Administration and the Drug Enforcement Administration updated their guidelines in response to the COVID-19 public health emergency by allowing medication initiation through both video and phone. However, policy discussions at this stage of the public health emergency largely favor video over phone.25 (TREATS Act, 2021). In our study, we found that despite concerted effort to shift patients to video-based care, a sizable minority of patients used phone as their primary means of accessing care, and that these patients were more likely to share a disproportionate burden of social determinants of health. To ensure equitable access to treatment, any long-term changes to policy should consider an audio-only amendment that allows remote evaluations using audio-only and video-enabled technologies.
There are several limitations to our study. First, this study was conducted in a single nonurban low-threshold office-based setting in New York State serving a predominantly young and White population. Findings from our study may not be representable or broadly generalizable to other patient populations or settings. Similarly, the clinic temporarily ceased in-person visits during the time of our study, and as a result, most visits were conducted over the phone or video. Although many SUD providers also reduced or eliminated in-person visits during the initial surge of the pandemic the findings may not be generalizable to those clinics that continued in-person care. The clinic also utilized a distinct approach that prioritized video over phone in their workflow and actively sought to ensure patients had access to video-enabled devices. This effort is reflected in the relatively low proportion of patients (10%) who initiated tele-MOUD over phone. Although REACH’s model has been highlighted by policymakers as an example of effectively delivering telehealth to treat SUD, the clinic’s experience may not be generalizable to clinics taking a different approach to tele-MOUD delivery.27
Second, data were collected using a comprehensive intake assessment administered before the pandemic. Some variables such as housing stability or employment may have changed during the pandemic. Third, registration data was used to determine whether each visit was conducted over phone or video. Although REACH developed systems for accurate documentation of visit modality (ie, double-checking registration data against billing codes and documenting visits that switched modalities mid-visit), the registration data may undercount phone visits. Finally, our study of visit patterns does not provide an explanation for why certain patient populations used 1 telemedicine modality over another, and whether the patterns were due to a lack of access to technology or driven by patient choice. Future qualitative studies of patient perspectives are needed to better understand the factors driving the patterns found in our analysis.
Despite the limitations, our study adds to the sparse evidence base surrounding the use of telemedicine for buprenorphine, and the potential disparities arising from an abrupt transition to telemedicine in SUD treatment settings. Although telemedicine has been available long before COVID-19, regulatory barriers and low reimbursement rates stymied its use in SUD treatment settings.31 As a result, telemedicine for SUD treatment has been particularly underused and understudied. To our knowledge, our study is the first to use EHR data to examine the use of different tele-MOUD modalities among patients with OUD. Furthermore, by linking EHR data to a comprehensive intake assessment, our study examines associations between tele-MOUD modality and a range of socio-economic patient characteristics that are unavailable in clinical records alone, such as housing and employment status.
CONCLUSIONS
The COVID-19 pandemic has exacerbated the opioid epidemic, with every state reporting a spike in overdoses deaths in the previous year. For individuals with OUD, telemedicine has the potential to increase access to MOUD during a time in which in-person visits may be infeasible. However, not all patients rely on the same form of telemedicine, raising questions around disparities in access. Permanent changes to SUD treatment telemedicine policies should proactively address potential disparities by allowing and reimbursing both video and phone tele-MOUD visits.
Footnotes
This work was supported by the Center for Drug Use and HIV Research (CDUHR).
The authors report no conflicts of interest.
Supplemental digital content is available for this article. Direct URL citation appears in the printed text and is provided in the HTML and PDF versions of this article on the journal's Web site (www.journaladdictionmedicine.com).
REFERENCES
- 1.Ahmad FB, Rossen LM, Sutton P. Provisional Drug Overdose Death Counts. National Center for Health Statistics. 2021. Available at: https://www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm. Accessed August 12, 2021. [Google Scholar]
- 2.U.S Drug Enforcement Agency (DEA) . DEA SAMHSA Buprenorphine Telemedicine (Final). (DEA-DC-022) (DEA068). 2020. Mar 31. Available at: https://www.deadiversion.usdoj.gov/GDP/(DEA-DC-022)(DEA068)%20DEA%20SAMHSA%20buprenorphine%20telemedicine%20%20(Final)%20+Esign.pdf. Accessed July 15, 2021. [Google Scholar]
- 3.Wang L Weiss J Ryan EB, et al. Telemedicine increases access to buprenorphine initiation during the COVID-19 pandemic. J Subst Abuse Treat. 2021;124:108272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Buchheit BM Wheelock H Lee A, et al. Low-barrier buprenorphine during the COVID-19 pandemic: a rapid transition to on-demand telemedicine with wide-ranging effects. J Subst Abuse Treat. 2021;131:108444. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Flodgren G Rachas A Farmer AJ, et al. Interactive telemedicine: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2015;2015(9):CD002098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Weinstein RS Lopez AM Joseph BA, et al. Telemedicine, telehealth, and mobile health applications that work: opportunities and barriers. Am J Med. 2014;127(3):183–187. [DOI] [PubMed] [Google Scholar]
- 7.Scorsone KL Haozous EA Hayes L, et al. Overcoming barriers: individual experiences obtaining medication-assisted treatment for opioid use disorder. Qual Health Res. 2020;30(13):2103–2117. [DOI] [PubMed] [Google Scholar]
- 8.Bunting AM Oser CB Staton M, et al. Clinician identified barriers to treatment for individuals in Appalachia with opioid use disorder following release from prison: a social ecological approach. Addict Sci Clin Pract. 2018;13(1):23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fiacco L, Pearson BL, Jordan R. Telemedicine works for treating substance use disorder: the STAR clinic experience during COVID-19. J Subst Abuse Treat. 2021;125:108312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Eibl JK Gauthier G Pellegrini D, et al. The effectiveness of telemedicine- delivered opioid agonist therapy in a supervised clinical setting. Drug Alcohol Depend. 2017;176:133–138. [DOI] [PubMed] [Google Scholar]
- 11.Huskamp HA Busch AB Souza J, et al. How is telemedicine being used in opioid and other substance use disorder treatment? Health Aff. 2018;37(12):1940–1947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Uscher-Pines L Sousa J Raja P, et al. Treatment of opioid use disorder during COVID-19: experiences of clinicians transitioning to telemedicine. J Subst Abuse Treat. 2020;118:108124. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lin LA Casteel D Shigekawa E, et al. Telemedicine-delivered treatment interventions for substance use disorders: a systematic review. J Subst Abuse Treat. 2019;101:38–49. [DOI] [PubMed] [Google Scholar]
- 14.Zheng W Nickasch M Lander L, et al. Treatment outcome comparison between telepsychiatry and face-to-face buprenorphine medication-assisted treatment (MAT) for opioid use disorder: a 2-year retrospective data analysis. J Addict Med. 2017;11(2):138–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Velasquez D, Mehrotra A. Ensuring the growth of telehealth during COVID-19 does not exacerbate disparities in care. Health Affairs Blog. 2020. doi: 10.1377/hblog20200505.591306. Accessed August 1, 2021. [DOI] [Google Scholar]
- 16.Vogels E. Digital Divide Persists Even as Americans with Lower Incomes Make Gains in Tech Adoption. Pew Research Center. Jun 22, 2021. Available at: https://www.pewresearch.org/fact-tank/2021/06/22/digital-divide-persists-even-as-americans-with-lower-incomes-make-gains-intech-adoption/. Accessed August 8, 2021. [Google Scholar]
- 17.Ye S Kronish I Fleck E, et al. Telemedicine Expansion During the COVID-19 Pandemic and the Potential for Technology-Driven Disparities. J Gen Intern Med. 2021;36(1):256–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dorsey ER, Topol EJ. State of telehealth. N Engl J Med. 2016;375(2):154–161. [DOI] [PubMed] [Google Scholar]
- 19.Song Z. Mortality quadrupled among opioid-driven hospitalizations, notably within lower-income and disabled white populations. Health Aff (Millwood). 2017;36(12):2054–2061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Barsky BA Busch AB Patel SY, et al. Use of telemedicine for buprenorphine inductions in patients with commercial insurance or medicare advantage. JAMA Netw Open. 2022;5(1):e2142531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Castillo M Conte B Hinkes S, et al. Implementation of a medical student-run telemedicine program for medications for opioid use disorder during the COVID-19 pandemic. Harm Reduct J. 2020;17(1):1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tofighi B McNeely J Walzer D, et al. A telemedicine buprenorphine clinic to serve New York City: initial evaluation of the NYC public hospital system’s initiative to expand treatment access during the COVID-19 pandemic. J Addict Med. 2021;16(1):e40–e43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.American Academy of Addiction Psychiatry . First glance: COVID-19 Buprenorphine Provider Survey Report. 2020. Available at: https://www.aaap.org/first-glance-covid-19-buprenorphineprovider-surveyreport/. Accessed August 6, 2021.
- 24.Telehealth Response for E-prescribing Addiction Therapy Services Act” or “TREATS Act” . 3.40, 117th Cong. 2021. Available at: https://www.congress.gov/bill/117th-congress/senate-bill/340/text. Accessed July 21, 2021. [Google Scholar]
- 25.Kapadia SN Griffin JL Waldman J, et al. A harm reduction approach to treating opioid use disorder in an independent primary care practice: a qualitative study. J Gen Intern Med. 2021;36(7):1898–1905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.U.S Department of Justice Drug Enforcement Administration (DEA) . COVID-19 Information Page. 2022. Available at: https://www.deadiversion. usdoj.gov/coronavirus.html. Accessed July 28, 2021.
- 27.Substance Abuse and Mental Health Services Administration (SAMHSA). Telehealth for the Treatment of Serious Mental Illness and Substance Use Disorders . SAMHSA Publication No. PEP21-06-02-001. Rockville, MD: National Mental Health and Substance Use Policy Laboratory, Substance Abuse and Mental Health Services Administration; 2021. [Google Scholar]
- 28.Darrat I Tam S Boulis M, et al. Socioeconomic disparities in patient use of telehealth during the coronavirus disease 2019 surge. JAMA Otolaryngol Head Neck Surg. 2021;147(3):287–295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Eberly LA Kallan MJ Julien HM, et al. Patient characteristics associated with telemedicine access for primary and specialty ambulatory care during the COVID-19 pandemic. JAMA Netw Open. 2020;3(12):e2031640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Au VY Rosic T Sanger N, et al. Factors associated with opioid overdose during medication-assisted treatment: How can we identify individuals at risk? Harm Reduct J. 2021;18(1):71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Busch AB Sugarman DE Horvitz LE, et al. Telemedicine for treating mental health and substance use disorders: reflections since the pandemic. Neuropsychopharmacology. 2021;46(6):1068–1070. [DOI] [PMC free article] [PubMed] [Google Scholar]


