Abstract
The current tumour-node-metastasis (TNM) staging system alone cannot provide adequate information for prognosis and adjuvant chemotherapy benefits in patients with gastric cancer (GC). Pathomics, which is based on the development of digital pathology, is an emerging field that might improve clinical management. Herein, we propose a pathomics signature (PSGC) that is derived from multiple pathomics features of haematoxylin and eosin-stained slides. We find that the PSGC is an independent predictor of prognosis. A nomogram incorporating the PSGC and TNM staging system shows significantly improved accuracy in predicting the prognosis compared to the TNM staging system alone. Moreover, in stage II and III GC patients with a low PSGC (but not in those with a high PSGC), satisfactory chemotherapy benefits are observed. Therefore, the PSGC could serve as a prognostic predictor in patients with GC and might be a potential predictive indicator for decision-making regarding adjuvant chemotherapy.
Subject terms: Gastric cancer, Prognostic markers
The current tumour-node-metastasis staging system alone cannot provide adequate information for prognosis and adjuvant chemotherapy benefits in patients with gastric cancer. Herein, the authors propose a pathomics signature that was derived from multiple features of haematoxylin and eosin-stained slides.
Introduction
Despite the remarkably reduced incidence and mortality of gastric cancer (GC), it remains an important contributor to the global burden of cancer1. Currently, the tumour-node-metastasis (TNM) staging system is considered the cornerstone for prognosis prediction and treatment decision-making in GC2. However, prognostic stratification of patients with GC according to the latest TNM staging system is often poor3. Adjuvant chemotherapy is recommended for advanced GC because of the improvement of oncological outcomes, but large variations in survival benefits from adjuvant chemotherapy have been reported even in patients with the same stage of disease and receiving similar treatment regimens3,4. These findings suggest that the present TNM staging system provides inadequate prognostic information and cannot accurately identify patients who are more likely to benefit from adjuvant chemotherapy, which highlights the urgent need for discovering new biomarkers that are associated with prognosis and adjuvant chemotherapy benefits in GC.
To understand the heterogeneous prognoses and adjuvant chemotherapy benefits seen in the clinic, several subtyping algorithms based on gene expression data have been investigated5–7. Although these methods have greatly improved our knowledge regarding GC and the potential of subgroup-specific rational treatment strategies has been enumerated by several studies, the cost and complexity of transcriptomic analyses, including expression microarray and RNA-seq analyses, prevent their active utilization in clinical practice8,9.
Evaluation of haematoxylin and eosin (H&E)-stained slides by experienced pathologists is indispensable for determining the TNM stage and histological classification of GC cases in the clinic. Full digitalization of the stained tissue sections has become feasible because of advances in slide scanning technology and reductions in the cost of digital storage10. Recently, the term “pathomics” has attracted increased attention. Pathomics embodies a wide variety of data that are captured from digital pathology image analyses to generate quantitative features for characterizing diverse phenotypes of tissue samples, and these data are subsequently analysed to determine diagnosis or predict survival outcomes11–13. Therefore, we hypothesized that analyses of the automatic digital pathomics features extracted from H&E-stained slides could predict the prognosis and survival benefits associated with adjuvant chemotherapy in patients with GC.
Integration of multiple features into a single signature, rather than individual analyses, might improve the performance of the prognostic prediction14,15. The least absolute shrinkage and selection operator (LASSO)-Cox regression model is a state-of-the-art machine learning method for regression analysis of the relationships between high-dimensional features and survival16–18. Here, we propose a pathomics signature of GC (PSGC) that was developed with multiple pathomics features extracted from H&E-stained sections using a LASSO-Cox regression model. Thus, in this study, we intended to assess the prognostic value of the PSGC for overall survival (OS) and disease-free survival (DFS) and explore whether the PSGC could identify patients with stage II and III diseases who might benefit from adjuvant chemotherapy.
Results
Participants
Table 1 lists the clinicopathological characteristics of patients in the training (n = 264) and validation (n = 216) cohorts. Of the 480 patients included in this study, 69.4% (333/480) were male, and the median [interquartile range (IQR)] age was 58 (49–65) years. The majority of the patients (76.3%, 366/480) were diagnosed with stage II or III disease. No significant difference in clinicopathological characteristics between the training and validation cohorts was found. The clinicopathological characteristics of patients with and without complete data were similar (Supplementary Table 1). The median (IQR) follow-up duration in the training cohort was 64 (27–72) months, with 5-year OS and DFS rates of 58.7% and 55.3%, respectively (Supplementary Fig. 1a, b). In the validation cohort, the median (IQR) follow-up duration was 55 (22.25–92) months. The 5-year OS and DFS rates were 47.7% and 45.4%, respectively (Supplementary Fig. 1c, d).
Table 1.
Characteristics of patients in the training and validation cohorts
| Variables | Training cohort (n = 264) | Validation cohort (n = 216) | P | ||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Age | 0.417 | ||||
| ≤60 years | 160 | 60.6 | 123 | 56.9 | |
| >60 years | 104 | 39.4 | 93 | 43.1 | |
| Age (years), median (IQR) | 57 (49–65) | 59 (51–65) | 0.443 | ||
| Sex | 0.571 | ||||
| Male | 186 | 70.5 | 147 | 68.1 | |
| Female | 78 | 29.5 | 69 | 31.9 | |
| ECOG PS | 0.840 | ||||
| 0 | 190 | 72.0 | 158 | 73.1 | |
| 1 | 68 | 25.8 | 55 | 25.5 | |
| 2 | 6 | 2.2 | 3 | 1.4 | |
| CEA level | 0.158 | ||||
| Normal | 216 | 81.8 | 187 | 86.6 | |
| Elevated | 48 | 18.2 | 29 | 13.4 | |
| CA 19-9 level | 0.385 | ||||
| Normal | 223 | 84.5 | 176 | 81.5 | |
| Elevated | 41 | 15.5 | 40 | 18.5 | |
| Tumour location | 0.690 | ||||
| Fundus of the stomach | 61 | 23.1 | 43 | 19.9 | |
| Body of the stomach | 49 | 18.6 | 43 | 19.9 | |
| Antrum of the stomach | 154 | 58.3 | 130 | 60.2 | |
| Tumour size | 0.299 | ||||
| ≤4 cm | 147 | 55.7 | 110 | 50.9 | |
| >4 cm | 117 | 44.3 | 106 | 49.1 | |
| Tumour grade | 0.725 | ||||
| Grade 1 | 18 | 6.8 | 12 | 5.6 | |
| Grade 2 | 54 | 20.5 | 44 | 20.4 | |
| Grade 3 | 169 | 64.0 | 135 | 62.5 | |
| Grade 4 | 23 | 8.7 | 25 | 11.5 | |
| Lauren type | 0.530 | ||||
| Intestinal type | 120 | 45.5 | 92 | 42.6 | |
| Diffuse and mixed type | 144 | 54.5 | 124 | 57.4 | |
| Depth of invasion | 0.307 | ||||
| T1 | 48 | 18.2 | 30 | 13.9 | |
| T2 | 24 | 9.1 | 17 | 7.9 | |
| T3 | 29 | 11.0 | 19 | 8.8 | |
| T4a | 143 | 54.2 | 124 | 57.4 | |
| T4b | 20 | 7.5 | 26 | 12.0 | |
| Lymph node metastasis | 0.803 | ||||
| N0 | 112 | 42.4 | 81 | 37.5 | |
| N1 | 50 | 18.9 | 40 | 18.5 | |
| N2 | 42 | 15.9 | 38 | 17.6 | |
| N3a | 37 | 14.0 | 34 | 15.7 | |
| N3b | 23 | 8.8 | 23 | 10.7 | |
| Distant metastasis | 0.999 | ||||
| M0 | 253 | 95.8 | 207 | 95.8 | |
| M1 | 11 | 4.2 | 9 | 4.2 | |
| TNM stage | 0.310 | ||||
| Stage I | 54 | 20.5 | 30 | 13.9 | |
| Stage II | 74 | 28.0 | 66 | 30.5 | |
| Stage III | 125 | 47.3 | 111 | 51.4 | |
| Stage IV | 11 | 4.2 | 9 | 4.2 | |
| Adjuvant chemotherapy | 0.626 | ||||
| Yes | 161 | 61.0 | 127 | 58.8 | |
| No | 103 | 39.0 | 89 | 41.2 | |
The comparisons of continuous age variables between two groups are performed using a two-sided Mann–Whitney U test, and the rest variables are compared using a two-sided χ2 or Fisher’s exact test.
IQR interquartile range, ECOG PS Eastern Cooperative Oncology Group performance status, CEA carcinoembryonic antigen, CA carbohydrate antigen, TNM tumour-node-metastasis.
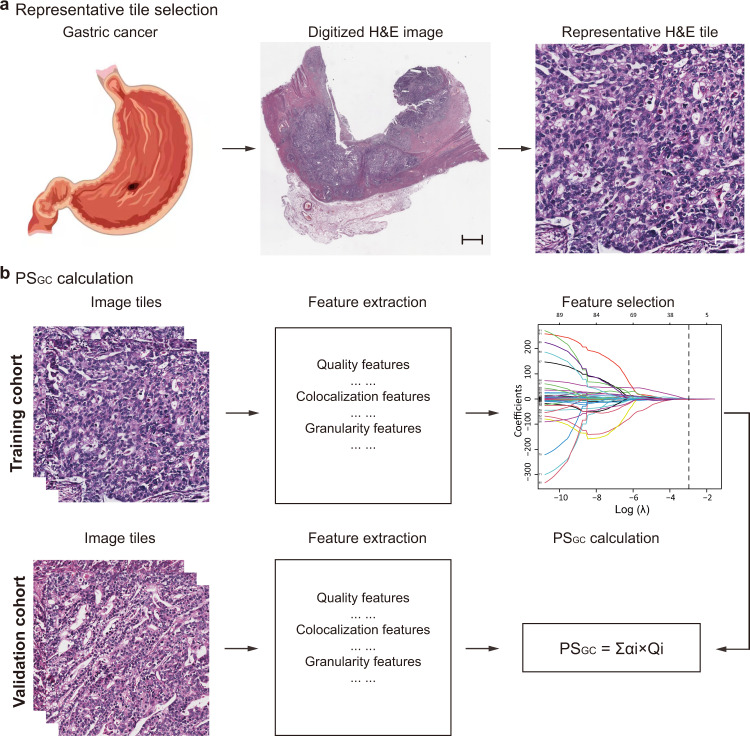
Construction of the PSGC
The framework for constructing the PSGC is presented in Fig. 1. In the training cohort, a LASSO-Cox regression model with 10-fold cross-validation was used to construct the PSGC. The final PSGC included 12 pathomics features (Supplementary Fig. 2). The PSGC calculation formula is presented in the Supplementary Note, from which the PSGC of the validation cohort was acquired directly. No statistically significant difference in the distribution of the PSGC [median (IQR)] was found between the training [1.211 (0.857–1.593)] and validation [1.196 (0.902–1.734)] cohorts [median difference: −0.050; 95% confidence interval (CI): −0.151 to 0.051; P = 0.340]. In particular, compared with the intestinal type, a significantly higher PSGC was detected in diffused and mixed type, with a median difference of 0.376 (95% CI: 0.250–0.497; P < 0.001) in the training cohort and 0.393 (95% CI: 0.258–0.541; P < 0.001) in the validation cohort (Supplementary Fig. 3). In terms of the tumour grade, the PSGC in patients with grade 3 and grade 4 tumours was significantly higher than that in patients with grade 1 and grade 2 tumours in both the training (median difference: 0.415; 95% CI: 0.271–0.553; P < 0.001) and validation (median difference: 0.463; 95% CI: 0.307–0.630; P < 0.001) cohorts (Supplementary Fig. 4). In addition, the distribution of PSGC was similar according to the tumour size subgroups in both the training (median difference: 0.099; 95% CI: −0.036 to 0.235; P = 0.158) and validation (median difference: 0.119; 95% CI: −0.031 to 0.268; P = 0.125) cohorts (Supplementary Fig. 5).
Fig. 1. Schematic illustration of PSGC construction.
a Selection of a representative H&E tile. The H&E-stained images of all included 480 patients are used, and 10 regions of interest with a field of view of 1000 × 1000 pixels per image containing the greatest number of tumour cells are randomly selected for analysis. One pixel is equal to 0.504 μm. Scale bars: 1500 and 50 μm, respectively. b Framework for constructing the PSGC. The pathomics features are extracted from the H&E-stained image tiles, and then the potential predictors are selected using a LASSO-Cox regression model in the training cohort with 264 patients. The PSGC is calculated via a linear combination of the selected features, and the PSGC for the validation cohort with 216 patients is directly calculated from the formula obtained in the training cohort. PSGC pathomics signature of gastric cancer, H&E haematoxylin and eosin, LASSO least absolute shrinkage and selection operator.
Association of the PSGC with prognosis
An optimum cutoff value of 1.16, which provided the highest standardized log-rank statistic, was determined with the training cohort (Supplementary Fig. 6). Accordingly, patients in both the training and validation cohorts were classified into high- and low-PSGC groups. The distribution of the PSGC across survival statuses as well as select pathomics features is shown in Supplementary Fig. 7, which revealed that a higher PSGC was associated with a higher risk of recurrence or death.
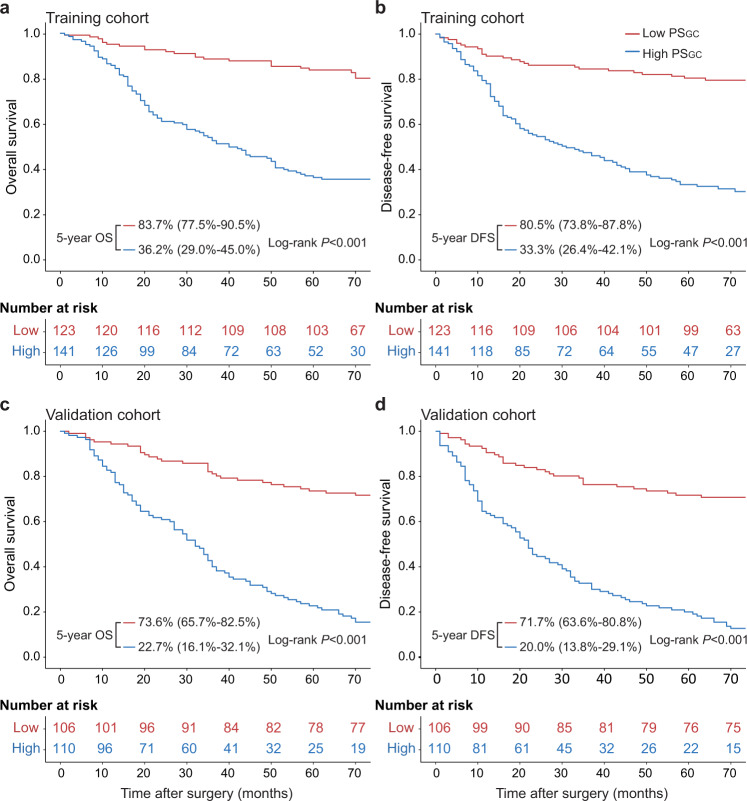
In the training cohort, the 5-year OS and DFS rates were 83.7% and 80.5% in low-PSGC patients, respectively, which were significantly reduced to 36.2% and 33.3% in high-PSGC patients (Fig. 2a, b, both log-rank P < 0.001). We subsequently performed the same analyses in the validation cohort. Among low-PSGC patients, the 5-year OS and DFS rates were 73.6% and 71.7%, respectively, and significantly worse 5-year OS and DFS rates of 22.7% and 20.0% were found in high-PSGC patients (Fig. 2c, d, both log-rank P < 0.001). The PSGC remained a significant prognostic indicator after stratification by clinicopathological variables, indicating the independent association of the PSGC with the prognosis (Supplementary Figs. 8–11).
Fig. 2. Kaplan–Meier survival curves according to the PSGC level.
a The OS rate difference between the high- and low-PSGC patients in the training cohort. b The DFS rate difference between the high- and low-PSGC patients in the training cohort. c The OS rate difference between the high- and low-PSGC patients in the validation cohort. d The DFS rate difference between the high- and low-PSGC patients in the validation cohort. The comparisons of OS and DFS between the two groups are performed using a two-sided log-rank test. OS overall survival, DFS disease-free survival, PSGC pathomics signature of gastric cancer. Source data are provided as a Source data file.
Development and validation of the pathomics nomogram for prognosis
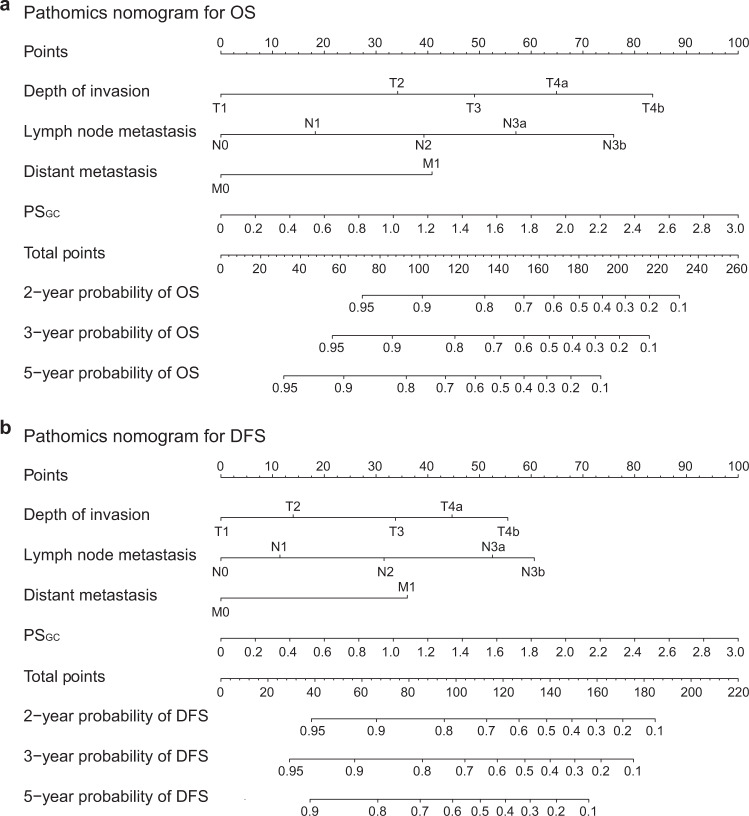
In the univariate Cox regression analysis, the PSGC, carcinoembryonic antigen (CEA) level, carbohydrate antigen (CA) 19-9 level, tumour location, tumour size, Lauren type, depth of invasion (T stage), lymph node metastasis (N stage) and distant metastasis (M stage) were significantly associated with OS in the training cohort (Table 2). The backwards stepwise multivariate Cox regression analysis showed that the PSGC, depth of invasion, lymph node metastasis and distant metastasis were independent predictors of OS. The same results were found in the Cox regression analysis for DFS. The proportional hazards (PH) assumption tests for the Cox regression models were valid (Supplementary Figs. 12 and 13). No interaction effects were observed between PSGC and the TNM staging system for OS and DFS (Supplementary Tables 2–4). Therefore, two pathomics nomograms were developed to predict OS and DFS by incorporating the four independent predictors (Fig. 3). Lymph node metastasis had the most important contribution to the prognostic prediction in the pathomics nomograms, followed by the PSGC (Supplementary Fig. 14).
Table 2.
Univariate and multivariate Cox regression analyses of the PSGC and clinicopathological characteristics for overall survival and disease-free survival in training cohort
| Variables | Overall survival | Disease-free survival | ||||||
|---|---|---|---|---|---|---|---|---|
| Univariate analysis | Multivariate analysis | Univariate analysis | Multivariate analysis | |||||
| HR (95% CI) | P | HR (95% CI) | P | HR (95% CI) | P | HR (95% CI) | P | |
| Age (years) (>60 years vs. ≤60 years) | 1.153 (0.794–1.675) | 0.454 | 1.107 (0.771–1.590) | 0.583 | ||||
| Sex (female vs. male) | 0.769 (0.504–1.172) | 0.221 | 0.722 (0.478–1.090) | 0.121 | ||||
| ECOG PS | 0.295 | 0.519 | ||||||
| 0 | Reference | – | Reference | – | ||||
| 1 | 1.361 (0.912–2.032) | 0.132 | 1.252 (0.846–1.852) | 0.261 | ||||
| 2 | 1.399 (0.441–4.437) | 0.568 | 1.214 (0.384–3.843) | 0.741 | ||||
| CEA level (Elevated vs. normal) | 1.870 (1.219–2.866) | 0.004 | 1.742 (1.147–2.646) | 0.009 | ||||
| CA 19-9 level (Elevated vs. normal) | 1.658 (1.049–2.622) | 0.031 | 1.942 (1.357–2.780) | 0.041 | ||||
| Tumour location | 0.005 | 0.007 | ||||||
| Cardia of the stomach | Reference | – | Reference | – | ||||
| Body of the stomach | 0.756 (0.449–1.272) | 0.291 | 0.838 (0.509–1.381) | 0.489 | ||||
| Antrum of the stomach | 0.504 (0.331–0.776) | 0.001 | 0.532 (0.353–0.801) | 0.003 | ||||
| Tumour size (>4 cm vs. ≤4 cm) | 2.142 (1.475–3.109) | <0.001 | 2.194 (1.529–3.149) | <0.001 | ||||
| Tumour grade | 0.060 | 0.079 | ||||||
| Grade 1 | Reference | – | Reference | – | ||||
| Grade 2 | 4.529 (1.068–19.215) | 0.040 | 5.176 (1.228–21.812) | 0.025 | ||||
| Grade 3 | 5.344 (1.312–21.764) | 0.019 | 5.433 (1.336–22.103) | 0.018 | ||||
| Grade 4 | 7.291 (1.645–32.324) | 0.009 | 7.176 (1.619–31.819) | 0.009 | ||||
| Lauren type (Diffuse and mixed vs. intestinal) | 1.700(1.159–2.494) | 0.007 | 1.579 (1.092–2.281) | 0.015 | ||||
| Depth of invasion | <0.001 | 0.018 | <0.001 | 0.049 | ||||
| T1 | Reference | – | Reference | – | Reference | – | Reference | – |
| T2 | 3.442 (0.822–14.401) | 0.091 | 2.256 (0.529–9.623) | 0.272 | 2.129 (0.616–7.354) | 0.232 | 1.437 (0.409–5.052) | 0.572 |
| T3 | 7.039 (1.962–25.248) | 0.003 | 3.228 (0.872–11.947) | 0.079 | 4.639 (1.633–13.177) | 0.004 | 2.415 (0.828–7.042) | 0.106 |
| T4a | 12.661 (3.995–40.125) | <0.001 | 4.688 (1.415–15.533) | 0.011 | 8.172 (3.312–20.163) | <0.001 | 3.198 (1.233–8.296) | 0.017 |
| T4b | 24.761 (7.151–85.744) | <0.001 | 7.282 (1.967–26.956) | 0.003 | 14.135 (5.120–39.025) | <0.001 | 4.175 (1.408–12.383) | 0.010 |
| Lymph node metastasis | <0.001 | <0.001 | <0.001 | |||||
| N0 | Reference | – | Reference | – | Reference | – | Reference | – |
| N1 | 2.372 (1.266–4.445) | 0.007 | 1.548 (0.817–2.932) | 0.180 | 2.078 (1.148–3.762) | 0.016 | 1.345 (0.732–2.470) | 0.340 |
| N2 | 4.353 (2.402–7.889) | <0.001 | 2.533 (1.364–4.702) | 0.003 | 3.745 (2.136–6.567) | <0.001 | 2.257 (1.251–4.071) | 0.007 |
| N3a | 8.563 (4.818–15.218) | <0.001 | 3.874 (2.111–7.107) | <0.001 | 8.264 (4.816–14.180) | <0.001 | 3.875 (2.174–6.909) | <0.001 |
| N3b | 12.189 (6.566–22.629) | <0.001 | 5.973 (3.057–11.671) | <0.001 | 10.779 (5.935–19.577) | <0.001 | 4.753 (2.477–9.120) | <0.001 |
| Distant metastasis (M1 vs. M0) | 3.540 (1.887–6.643) | <0.001 | 2.611 (1.350–5.051) | <0.001 | 3.450 (1.840–6.466) | <0.001 | 2.518 (1.306–4.854) | 0.006 |
| PSGC | 4.263 (3.054–5.952) | <0.001 | 2.209 (1.539–3.170) | <0.001 | 4.281 (3.084–5.943) | <0.001 | 2.372 (1.646–3.420) | <0.001 |
Association of all variables with prognosis is analysed using a two-sided Cox proportional hazard regression analysis.
PSGC pathomics signature of gastric cancer, CEA carcinoembryonic antigen, CA carbohydrate antigen, HR hazard ratio, CI confidence interval, ECOG PS Eastern Cooperative Oncology Group performance status.
Fig. 3. Pathomics nomograms for the prediction of OS and DFS.
a Pathomics nomogram for OS. b Pathomics nomogram for DFS. The patient’s T stage on the depth of the invasion axis is first located using the nomogram. Then, a line is drawn straight upward to the Points axis to determine how many points the patient receives from the T stage. This process is repeated for each variable, and the points obtained from each risk factor are summed. Finally, the final sum is located on the Total point axis. A line is drawn straight down to find the patient’s probability of survival. OS overall survival, DFS disease-free survival, PSGC pathomics signature of gastric cancer. Source data are provided as a Source data file.
In the training cohort, the pathomics nomogram yielded a concordance index (C-index) of 0.809 (95% CI: 0.741–0.878) for OS and 0.792 (95% CI: 0.718–0.866) for DFS. In addition, the time-dependent receiver operating characteristic (ROC) curve of the pathomics nomogram at 5 years produced an area under the receiver operating characteristic curve (AUROC) of 0.901 (95% CI: 0.863–0.939) for OS and 0.891 (95% CI: 0.850–0.932) for DFS (Supplementary Fig. 15a, b). Furthermore, the calibration curves showed good agreement between the nomogram-predicted survival and actual survival (Supplementary Fig. 16a, b). The good discrimination with a C-index of 0.784 (95% CI: 0.706–0.862) for OS and 0.794 (95% CI: 0.709–0.873) for DFS was externally validated in the validation cohort. The AUROCs for OS and DFS were 0.887 (95% CI: 0.842–0.931) and 0.888 (95% CI: 0.844–0.933), respectively (Supplementary Fig. 15c, d). The favourable agreement between the nomogram-predicted survival and actual survival of the calibration curves was also confirmed in the validation cohort (Supplementary Fig. 16c, d). Finally, the decision curve analysis indicated that using the pathomics nomograms to predict OS and DFS provided more net benefits than using the treat all scheme or treat none scheme in both the training and validation cohorts (Supplementary Fig. 17), indicating that the pathomics nomograms were clinically applicable.
Incremental value of the PSGC added to the TNM stage model
Two TNM stage models for OS and DFS were built based on multivariate Cox regression analyses without the PSGC to elucidate the incremental value of the PSGC added to clinicopathological variables for predicting the prognosis (Supplementary Table 5). In the training cohort, the C-index of the PSGC for the prediction of OS and DFS was 0.727 (95% CI: 0.641–0.813) and 0.712 (95% CI: 0.622–0.802), respectively, and the TNM stage models showed a C-index of 0.782 (95% CI: 0.709–0.855) for OS and 0.770 (95% CI: 0.694–0.846) for DFS. Compared with the TNM stage models, the pathomics nomograms, which were based on the combination of PSGC and the TNM staging system, displayed a significantly improved C-index of 0.809 (95% CI: 0.741–0.878; P = 0.002) for OS and 0.792 (95% CI: 0.718–0.866; P = 0.022), respectively (Supplementary Table 6). Similarly, the AUROCs of the PSGC for OS and DFS were 0.798 (95% CI: 0.744–0.852) and 0.794 (95% CI: 0.739–0.848), respectively, and the TNM stage models yielded an AUROC of 0.868 (95% CI: 0.825–0.910) for OS and 0.859 (95% CI: 0.814–0.904) for DFS. Compared with the TNM stage models, the pathomics nomograms exhibited a significantly higher AUROC of 0.901 (95% CI: 0.863–0.939; P = 0.004) for OS and 0.891 (95% CI: 0.850–0.932; P = 0.005) for DFS (Supplementary Fig. 15a, b). The decision curve analysis indicated that compared with the TNM stage models, the pathomics nomograms showed greater net benefits across most of the range of reasonable threshold probabilities (Supplementary Fig. 17a, b). Moreover, the pathomics nomograms showed a net reclassification improvement (NRI) of 0.177 (95% CI: 0.021–0.319; P = 0.026) for OS and 0.218 (95% CI: 0.048–0.344; P = 0.012) for DFS compared to the TNM stage models (Supplementary Table 7). The abovementioned results were well validated in the validation cohort. In the validation cohort, the PSGC demonstrated a C-index of 0.725 (95% CI: 0.627–0.823) for OS and 0.738 (95% CI: 0.642–0.834) for DFS, respectively, and the TNM stage models presented a C-index of 0.742 (95% CI: 0.656–0.828) for OS and 0.748 (95% CI: 0.660–0.836) for DFS. Compared with the TNM stage models, a significantly increased C-index of 0.784 (95% CI: 0.706–0.862; P < 0.001) for OS and 0.794 (95% CI: 0.709–0.873; P < 0.001) for DFS was observed in the pathomics nomograms (Supplementary Table 6). Meanwhile, the AUROCs of the PSGC for OS and DFS were 0.774 (95% CI: 0.710–0.837) and 0.775 (95% CI: 0.711–0.839), respectively, and the TNM stage models exhibited an AUROC of 0.848 (95% CI: 0.797–0.900) for OS and 0.846 (95% CI: 0.794–0.898) for DFS. Compared with the TNM stage models, a significantly enhanced AUROC of 0.887 (95% CI: 0.842–0.931; P = 0.003) for OS and 0.888 (95% CI: 0.844–0.933; P = 0.003) for DFS was also confirmed in the pathomics nomograms (Supplementary Fig. 15c, d). In addition, higher net benefits across most of the range of reasonable threshold probabilities in the pathomics nomograms compared to the TNM stage models were detected (Supplementary Fig. 17c, d). Finally, an NRI of 0.318 (95% CI: 0.147–0.497; P = 0.010) for OS and 0.380 (95% CI: 0.141–0.556; P = 0.028) for DFS in the pathomics nomograms compared to the TNM stage models was found in the validation cohort (Supplementary Table 7). Herein, the PSGC could provide additional prognostic value to the TNM staging system for GC.
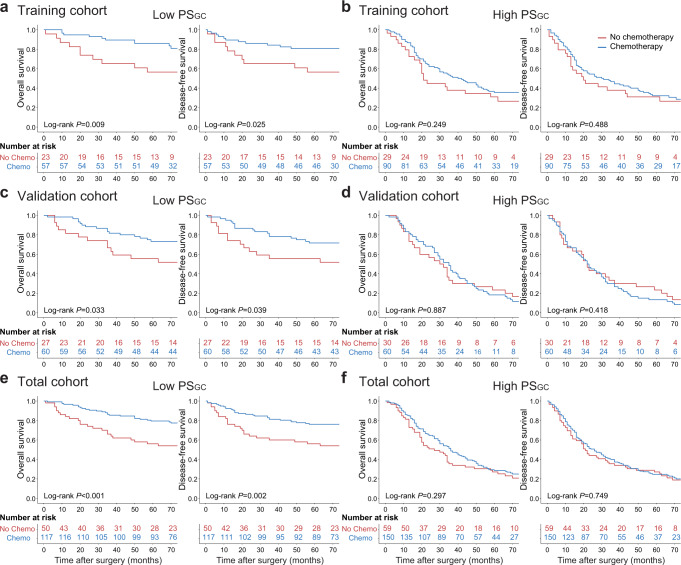
Predictive value of the PSGC for adjuvant chemotherapy response
To assess the predictive value of the PSGC for adjuvant chemotherapy response, we evaluated the association between the PSGC and survival among GC patients with stage II and stage III disease who either received or did not receive postoperative adjuvant chemotherapy. Patient information after stratification according to adjuvant chemotherapy status is listed in Supplementary Table 8. For the low-PSGC patients, adjuvant chemotherapy was significantly associated with improved OS and DFS in the training, validation and total cohorts; however, the improved prognosis was not observed in high-PSGC patients (Fig. 4). Similar results were obtained from the subgroup analyses of patients with stage II and III tumours (Supplementary Figs. 18, 19). No difference in the performance status of patients with a high PSGC to tolerate the full course of chemotherapy was observed (Supplementary Table 9). Subsequently, a test of the interaction between the PSGC and adjuvant chemotherapy indicated that patients with a low PSGC had superior adjuvant chemotherapy benefits compared to patients with a high PSGC, with the P for interaction <0.05 for OS and DFS (Table 3, Supplementary Table 10). Taken together, these results indicated that the PSGC could identify stage II and III GC patients who might obtain survival benefits from adjuvant chemotherapy.
Fig. 4. Association between the PSGC and survival benefits from adjuvant chemotherapy in stage II and stage III GC.
a Survival benefits from adjuvant chemotherapy for the low-PSGC patients in the training cohort. b Survival benefits from adjuvant chemotherapy for the high-PSGC patients in the training cohort. c Survival benefits from adjuvant chemotherapy for the low-PSGC patients in the validation cohort. d Survival benefits from adjuvant chemotherapy for the high-PSGC patients in the validation cohort. e Survival benefits from adjuvant chemotherapy for the low-PSGC patients in the total cohort. f Survival benefits from adjuvant chemotherapy for the high-PSGC patients in the total cohort. The comparisons of OS and DFS between the two groups are performed using a two-sided log-rank test. PSGC pathomics signature of gastric cancer, GC gastric cancer, Chemo chemotherapy. Source data are provided as a Source data file.
Table 3.
Association of the PSGC with overall survival and disease-free survival in stage II and III patients receiving adjuvant chemotherapy
| PSGC level | Adjuvant chemotherapy | Overall survival | Disease-free survival | |||||
|---|---|---|---|---|---|---|---|---|
| No chemo | Chemo | HR (95% CI) | P | Pinteraction | HR (95% CI) | P | Pinteraction | |
| Training cohort (n = 199) | ||||||||
| High PSGC (Chemo vs. No chemo) | 29 | 90 | 0.748 (0.454–1.233) | 0.255 | 0.001 | 0.840 (0.513–1.377) | 0.490 | <0.001 |
| Low PSGC (Chemo vs. No chemo) | 23 | 57 | 0.366 (0.136–0.786) | 0.013 | 0.388 (0.165–0.914) | 0.030 | ||
| Validation cohort (n = 177) | ||||||||
| High PSGC (Chemo vs. No chemo) | 30 | 60 | 1.028 (0.639–1.657) | 0.908 | <0.001 | 1.203 (0.753–1.924) | 0.439 | <0.001 |
| Low PSGC (Chemo vs. No chemo) | 27 | 60 | 0.459 (0.221–0.955) | 0.037 | 0.475 (0.231–0.979) | 0.044 | ||
| Total cohort (n = 376) | ||||||||
| High PSGC (Chemo vs. No chemo) | 59 | 150 | 0.834 (0.591–1.177) | 0.302 | <0.001 | 0.947 (0.675–1.329) | 0.751 | <0.001 |
| Low PSGC (Chemo vs. No chemo) | 50 | 117 | 0.392 (0.224–0.687) | 0.001 | 0.434 (0.250–0.755) | 0.003 | ||
Association of all variables with prognosis is analysed using a two-sided Cox proportional hazard regression analysis.
PSGC pathomics signature of gastric cancer, HR hazard ratio, CI confidence interval, Chemo chemotherapy.
Discussion
Accurate prediction of prognosis and adjuvant chemotherapy benefits is integral to the risk stratification and management of GC patients in the clinic. In this study, we constructed the PSGC to predict the prognosis of patients with GC and found that the PSGC successfully stratified patients into high- and low-PSGC groups with significant differences in terms of OS and DFS. Furthermore, by combining the PSGC and TNM staging systems, we developed and validated two pathomics nomograms with significantly improved prognostic predictions compared with the TNM staging system alone. These results indicate that the PSGC might provide complementary information about the prognosis of GC.
Adjuvant chemotherapy is a standard treatment for nonmetastatic advanced GC3,19. However, the variations in survival outcomes even in patients with the same TNM stage who receive the same regimens indicate that a considerable number of patients do not benefit from adjuvant chemotherapy. Individualized biomarkers that can distinguish patients who are likely to benefit from adjuvant chemotherapy could improve tailored therapy20. Our results revealed that patients with a low PSGC were predicted to benefit from adjuvant chemotherapy, but in patients with a high PSGC, limited benefits were observed. Patient performance status is an important factor that might affect tolerance to adjuvant chemotherapy. In this study, we did not observe a difference in the performance status of patients with a high PSGC to tolerate the full course of chemotherapy, indicating that the predictive value of the PSGC for adjuvant chemotherapy benefits might be also applicable to patients with a poor physical condition. Although patients receiving neoadjuvant therapy were excluded, most patients included in this study were still diagnosed with locally advanced GC, which did not imply that patients with a potentially lower risk were included. To our knowledge, this is the first study to demonstrate the utility of fully quantitative imaging features extracted from H&E-stained slides to predict prognosis and benefits from adjuvant chemotherapy in GC.
Two factors were critical for the construction of the PSGC. The first factor is the use of a convenient image-processing approach to extract quantitative pathomics features. To date, a consensus about the extraction of pathomics features has not been reached12,13. CellProfiler is a free, open-source software that automatically measures phenotypes from biological images and has been used in digital pathology analysis with satisfactory performance21,22. Therefore, CellProfiler is an easy-to-use and reproducible platform that allows clinicians to extract quantitative pathomics features. The second factor is a practical machine learning method for the selection of prognostic features23. For this purpose, the LASSO-Cox regression model was employed because of its ability to deal with high-dimensional data16,17.
Despite its limited performance, the TNM staging system remains the cornerstone for predicting the prognosis of patients with GC. To date, some investigators have explored potential biomarkers that might provide additional prognostic information in GC. Based on the gene expression data, several molecular classifications have been proposed. For example, according to The Cancer Genome Atlas project, GC was divided into four subtypes based on molecular classification, including tumours positive for Epstein-Barr virus, microsatellite unstable tumours, genomically stable tumours and tumours with chromosomal instability, which might aid in patient stratification and tailoring therapy5,7. However, the cost and complexity of gene expression data analyses prevent their clinical application, especially in developing countries. In addition, a radiomics analysis of radiological images has also shown a favourable ability for predicting the prognosis of GC24,25. Other studies have also revealed that the stromal immune cells, such as tumour-associated macrophages, cytotoxic T cells and neutrophils, are indicators of the GC prognosis26,27. Prospective studies and further evaluations are needed to better clarify their impacts on the prognosis of GC. In addition to the pathological diagnosis, the evaluation of H&E-stained sections has provided limited information on patient prognosis and chemotherapy response. Currently, the literature regarding the prognostic information of pathomics analysis in GC has not yet been reported. In this study, we discovered that the PSGC could also contribute to the prediction of prognosis and identify patients who are more likely to benefit from adjuvant chemotherapy in GC. Because the PSGC was derived from the routinely used H&E-stained sections in the clinic, the PSGC might be conveniently applied in clinical practice without additional financial burden and might favour the development of tailored therapy for GC. We expect that these biomarkers, including molecular subtypes, radiomics, stromal immune cells, and pathomics, will be utilized together to improve the prediction of prognosis and chemotherapy response of GC in the future.
In Western countries, patients with locally advanced GC are recommended to receive neoadjuvant chemotherapy because of the prolonged survival28,29; however, radical gastrectomy followed by adjuvant chemotherapy remained the standard of care for these patients in Eastern Asia2,30, and patients with locally advanced GC are treated with this therapeutic strategy in our medical centre31. Patients receiving neoadjuvant chemotherapy were excluded from our study, as neoadjuvant chemotherapy would result in morphological changes in the H&E-stained sections, including tumour regression and fibrosis; thus, the prediction models developed in this study might be inappropriate to be extended to patients with GC who receive neoadjuvant chemotherapy. However, our results revealed that the pathomics analysis reflected tumour heterogeneity, which was a potential indicator of the prognosis and chemotherapy response of patients with GC. Thus, the pathomics analysis might also be suitable for evaluating the response and outcomes of neoadjuvant chemotherapy. Further investigations are required in this specific setting.
Pathomics is a novel method that has been utilized to explore tumour heterogeneity since different degrees of disease progression, clinical outcomes, and treatment responses correspond to a range of histologic features in different tumour cells11. Traditional pathological examination is performed by experienced pathologists at multiple magnifications to evaluate the characteristics of tumour cells; however, pathologists do not and cannot routinely characterize more detailed information for every slide. Thus, pathomics can serve as a useful method to complement traditional pathological evaluation32. Our results revealed significant differences in the Lauren type and tumour grade subgroups, indicating that the local image features would change according to the Lauren type and tumour grade, and the Lauren type and tumour grade might drive the PSGC. Moreover, a similar distribution of PSGC was found between the tumour size subgroups, which implied no bias in the selection of regions of interest due to tumour size.
The PSGC was found to be a potential predictor of prognosis and adjuvant chemotherapy benefits for GC patients. However, it remains unclear whether the predictive value of the PSGC is determined by tumour intrinsic factors or tumour microenvironment effects. Currently, the integrative analysis of pathomics features and genomics data provides a feasible way to explore the underlying mechanisms of PSGC with prognosis and adjuvant chemotherapy benefits33,34. Thus, further investigations should focus on the relationship between pathomics features and genomics data.
The tumour grade is a common term used to diagnose GC in the clinic, which evaluates the progression of tumour cells. Our data showed that the PSGC substantially outperformed the tumour grade in predicting the OS and DFS (Supplementary Table 11 and Supplementary Fig. 20). The prognostic performance of the TNM staging system was not increased when the tumour grade was added; conversely, significantly improved prognostic performance was detected when the PSGC was added to the TNM staging system (Supplementary Table 12 and Supplementary Fig. 21). Thus, the PSGC performed better when it was included in the pathomics nomogram than when it was replaced by the tumour grade.
The improvement in AUROC ranged from 3.2% to 4.2% when the PSGC was added to the TNM staging system, and the corresponding improvement in the C-index ranged from 2.2% to 4.6%, which might seem small. In this study, the pathomics nomograms were developed based on the depth of invasion, lymph node metastasis, distant metastasis and PSGC. In terms of the individual variables, the prognostic value of the PSGC was comparable to that of the lymph node metastasis (Supplementary Tables 13 and 14). However, in the pathomics nomograms, lymph node metastasis had the most important contribution to predict the prognosis, followed by the PSGC. Based on these results, lymph node metastasis exerted more powerful effects on the AUROCs and C-indexes of the pathomics nomograms than the PSGC, although the individual prognostic performance of the two variables was comparable, which explained the small incremental value of adding PSGC to the TNM staging system. Several prognostic biomarkers with statistically different but numerically small incremental values have also been reported previously35–37. Although the incremental value of adding PSGC to the TNM staging system for predicting the prognosis was small, it did provide additional prognostic information. Meanwhile, the ability of the PSGC to predict response to adjuvant chemotherapy was valuable, which might avoid the toxic effects of chemotherapy in those patients least likely to benefit. Thus, from the perspective of clinicians, the PSGC was clinically relevant and worth further investigation.
The AUROCs of the pathomics nomograms were acquired from the multivariate analysis of potential prognostic factors. Currently, a unanimous consensus has not been reached about the calculation of sample size in the multivariate analysis for developing a prediction model. According to the TRIPOD Statement, at least 10 events per variable are needed38. Thus, the minimum sample size of patients with recurrence is 100 according to the 10 events per variable criteria to assess the difference in AUROCs between the pathomics nomograms and TNM stage models. In the training cohort, 122 patients suffered from recurrence. Thus, our sample size in the training cohort was adequate to conduct the multivariate analysis. For the sample size in the validation cohort, Lei et al.39 suggested that the ratio between the training and validation cohorts was 7:3. In our study, the validation cohort contained 216 patients, which was also sufficient.
Considering the survival differences between the training and validation cohorts (OS: 58.7% vs. 47.7%; DFS: 55.3% vs. 45.4%), we speculated that it might be due to the socioeconomic differences despite the similar clinicopathological characteristics between the two cohorts. The training cohort and validation cohort came from Guangdong and Fujian in China, respectively. Guangdong is the most economically advanced province in China, most patients in the training cohort live in urban areas, and the local medical insurance covers more examinations and therapies; conversely, the economic level of Fujian is moderate in China, and considerable numbers of patients in the validation cohorts reside in rural areas, and the local medical insurance covers the costs of fewer examinations and therapies40. Therefore, despite the rigorous follow-up after surgery, early detection and treatment of recurrent diseases are limited for patients in the validation cohort, thus resulting in differences in survival.
According to the Global Burden of Diseases, Injuries, and Risk Factors Study (GBD) 2017 Stomach Cancer Collaborators, the estimated 5-year OS of GC is approximately 20%, with the exceptions of 65% in Japan and 71·5% in South Korea, where population screening has led to the effective diagnosis of tumours at early stages1. In this study, all included GC patients who had received radical gastrectomy; however, the data sources of the GBD 2017 were derived from patients diagnosed with GC, regardless of resectable or unresectable diseases. Thus, the survival outcomes of the included patients are high by global standards. In addition, the 5-year OS of GC patients receiving radical gastrectomy generally ranges from 45% to 60% in China, indicating that the survival outcomes of patients with GC included in this study are similar to those in other parts of China30.
Our results revealed that elevated CEA and CA 19-9 levels were significantly associated with a worse prognosis. In clinical practice, CEA and CA 19-9 levels are the most common tumour markers measured before surgery and during follow-up for GC. CEA and CA 19-9 levels have been used as diagnostic markers and are apt to rise 2–3 months before metastatic lesions become detectable by imaging modalities2. Several studies have also reported that elevated preoperative CEA and CA 19-9 levels are associated with a worse prognosis for patients with resectable GC41,42. Currently, the intrinsic mechanisms of elevated CEA and CA 19-9 levels for worse survival are still unclear. One possible explanation might be that CEA and CA 19-9, which are a ligand of E-selectin and an intercellular adhesion molecule, respectively, play critical roles in the intercellular adhesion of tumour cells to vascular endothelial cells and contribute to tumour invasion and metastasis43,44. Thus, the prognostic values of CEA and CA 19-9 levels for GC need to be further investigated.
In general, there are two main types of artificial intelligence-based computational approaches for pathomics analysis: deep neural network-based approaches and handcrafted feature-based approaches12. The method used in this study is a handcrafted feature-based approach that was developed based on the close collaboration between pathologists and oncological surgeons, and thus could be complex and time-consuming45. Deep neural network-based approaches are developed through unsupervised feature learning, which depends on the existence of learning sets and annotated exemplars from the categories of interest, and the network design usually focuses on fine-tuning the algorithm to maximize accuracy while minimizing processing time46. In addition, deep neural network-based approaches trained on a particular disease subtype could be applied to other subtypes as well12. However, in terms of interpretability, because of being more interpretable than deep neural network-based approaches, handcrafted feature-based approaches might be more likely to be used for high-level decision-making, such as that regarding oncological prognosis or prediction of benefit from therapy; in contrast, deep neural network-based approaches might be more appropriate in situations where the need to “explain the decision” is reduced; such situations could include low-level tasks such as object detection or segmentation12,47,48. Considering the application scene of this study and that oncologists and pathologists are the primary end users, we select the handcrafted feature-based approaches.
There are some limitations in our study. First, given the retrospective design, our study was not free from inherent biases. Second, all enroled participants came from two medical centres in China. Thus, further validation in prospective randomized trials incorporating diverse populations is warranted to test the clinical utility of the PSGC for individualized decision-making.
In conclusion, our study constructed the PSGC and found that the PSGC was significantly associated with the prognosis of patients with GC. By integrating the PSGC with the TNM staging system, we developed and validated two pathomics nomograms, which improved the prediction of the GC prognosis compared to the TNM staging system alone. Moreover, the PSGC could distinguish patients with stage II and III diseases who were likely to derive benefits from adjuvant chemotherapy.
Methods
This study was approved by the Institutional Review Boards of Nanfang Hospital of Southern Medical University and the Fujian Cancer Hospital of Fujian Medical University. Written informed consent was obtained from all patients before surgery, which contained a statement on the formalin-fixed, paraffin-embedded samples and clinicopathological data for scientific research. All procedures involving human participants were in accordance with the Declaration of Helsinki.
Participants
A retrospective cohort study was conducted based on consecutive patients who underwent radical gastrectomy for GC from two medical centres. A training cohort including 264 consecutive patients from March 2012 to December 2013 at Nanfang Hospital of Southern Medical University was built. The inclusion criteria were as follows: (i) histologically diagnosed GC and treated with curative surgery, (ii) at least 15 lymph nodes were harvested, (iii) no history of other malignancies, and (iv) complete clinicopathological and follow-up information were available. Patients receiving neoadjuvant chemotherapy, radiotherapy or chemoradiotherapy were excluded because neoadjuvant anticancer therapy not only results in microscopic morphological changes in the H&E-stained sections, including tumour regression and fibrosis but also affects the prognosis of patients with GC. A total of 216 consecutive patients were included from Fujian Provincial Cancer Hospital of Fujian Medical University between August 2010 and September 2012 using the same inclusion and exclusion criteria.
Patient baseline information, including age, sex, Eastern Cooperative Oncology Group performance status (ECOG PS), CEA level, CA 19-9 level, tumour location, tumour size, tumour grade, Lauren type, depth of invasion, lymph node metastasis, distant metastasis, TNM stage, postoperative adjuvant chemotherapy and follow-up data (follow-up duration and survival status), was collected. The TNM stage was reclassified according to the eighth version of the AJCC Cancer Staging Manual of the American Joint Committee on Cancer. Patients were followed up once every 3 months in the first 2 years after surgery, every 6 months in the next 3 years, and annually thereafter. The follow-up duration was measured from the time of surgery to the last follow-up date, and the survival status at the last follow-up was recorded. OS was defined as the interval between surgery and death or the last date of follow-up. DFS was defined as the time from surgery to recurrence at any site or all-cause death, whichever came first.
Sample preparation and region of interest selection
The H&E-stained slides of all included patients were prepared using formalin-fixed paraffin-embedded samples. Then, sections most representative of the depth of invasion in each case were selected by the director of the Department of Pathology, Fujian Cancer Hospital (G.C.), who had 25 years of experience in the pathological diagnosis of GC. Subsequently, all selected slides were scanned by using the Aperio ScanScope Scanner system (Leica Biosystems) with the ×20 objective, and images were digitized as svs. format files, which were managed with the Aperio ImageScope software (version 12.4.6). Under the quality control of the director of the Department of Pathology, Fujian Cancer Hospital (G.C.), the tumour areas in each section were determined. Ten nonoverlapping representative tiles of each case containing the greatest number of tumour cells with a field of view of 1000 × 1000 pixels (one pixel is equal to 0.504 μm) were selected by a pathologist and then confirmed by the other pathologist (L.L. and J.L.), who had 9 and 13 years of experience in the pathological diagnosis of GC, respectively, to reduce the computational time. The regions of tissue folds were excluded and the selected tiles were saved as.tif format files. If the abovementioned two pathologists differed in their opinions, they consulted with the third pathologist (G.C.) to make a decision.
Extraction of pathomics features from images
The quantitative pathomics features of the selected tiles were extracted by using CellProfiler (version 4.0.7), an open-source image analysis software developed by the Broad Institute (Cambridge, MA)21,22. The H&E-stained images were split into haematoxylin-stained and eosin-stained greyscale images using the “UnmixColors” module49. The H&E-stained images were also converted to greyscale images using the “ColorToGray” module based on the “Combine” method for further analysis. First, the features that indicated the image quality of the greyscale H&E, haematoxylin and eosin images were assessed by using the “MeasureImageQuality” and “MeasureImageIntensity” modules with three types of features, including blurred features, intensity features and threshold features50–53. The threshold features were extracted by automatically calculating the threshold for each image to identify the tissue foreground from the unstained background with the Otsu algorithm54. Subsequently, the colocalization and correlation between intensities in each haematoxylin-stained image and eosin-stained image were calculated on a pixel-by-pixel basis across an entire image by using the “MeasureColocalization” module55. In addition, the granularity features of each image were assessed using the “MeasureGranularity” module, which outputted spectra of size measurements of the textures in the image, with a granular spectrum range of 1656,57. Further description of the pipeline for feature extraction is described in the Supplementary Methods. A summary of the pathomics features is presented in Supplementary Table 15.
Construction of the PSGC
The LASSO-Cox regression model uses an L1 penalty to shrink the coefficients of each feature to zero, and this model has been broadly applied in the regression analysis of high-dimensional data for survival analysis16,17. The penalty parameter λ, also called the tuning constant, controls the strength of the penalty. If λ is reduced and the penalty is relaxed, then more predictors can enter the model. In this study, 10-fold cross-validation with minimum criteria was used to determine the optimum value of λ by measuring partial likelihood deviance in the training cohort. The PSGC was constructed via a linear combination of the selected features, and the PSGC for the validation cohort was directly calculated from the formula obtained in the training cohort.
Association of the PSGC with prognosis
Based on the individual PSGC, an optimum cutoff value was identified via the maximally selected rank statistics to classify patients into high- and low-PSGC groups in the training cohort, and then the same cutoff value was applied to the validation cohort58. Potential associations of the PSGC with OS and DFS were first assessed in the training cohort and then validated in the validation cohort. The differences in the survival curves of the high- and low-PSGC groups were evaluated.
Development and validation of the pathomics nomogram for prognosis
In the training cohort, the PSGC and clinicopathological characteristics were incorporated into the univariate Cox regression analyses for OS and DFS. Variables with P < 0.05 were selected for the multivariate Cox regression analyses. The backwards stepwise regression was utilized to detect the independent predictors. Two pathomics nomograms including the independent predictors were developed to predict OS and DFS, respectively.
To quantify the discrimination performance, the C-index and 5-year AUROC were calculated59. To compare the agreement between predicted survival probabilities and the actual probabilities, calibration curves were generated60. To evaluate the clinical usefulness of the pathomics nomograms, decision curve analysis was used to assess the net benefits of the prediction model at different threshold probabilities61,62. The context for decision curve analysis is a situation where individuals’ risks for an undesirable outcome will be evaluated, and individuals with sufficiently high risk will be recommended for some intervention or treatment. The pathomics nomograms were then applied in the validation cohort to validate the discrimination, calibration, and clinical usefulness38.
Incremental value of the PSGC for prognosis prediction
Two clinicopathological models incorporating independent clinicopathological risk factors for the prediction of OS and DFS were developed in the training cohort, respectively, and then applied to the validation cohort to determine the incremental value of the PSGC for the individualized prediction of the prognosis when added to the clinicopathological risk factors. The incremental value of the PSGC to the clinicopathological models was assessed with respect to the C-index, time-independent AUROC, NRI, and decision curve analysis38. The C-indexes and time-independent AUROCs at 5 years between the two models were compared by using the z-score test and DeLong test, respectively63,64. The NRI of the pathomics nomogram to the clinicopathological model was assessed by using the Z test65.
Statistical analysis
Continuous variables were compared using the independent samples, unpaired t-test if they were normally distributed or using the Mann–Whitney U test if they were nonnormally distributed. When comparing a categorical variable, if at least one expected cell count was <5 in the 2 × C contingency table, Fisher’s exact test was used; otherwise, the χ2 test was performed. Survival curves were generated using the Kaplan–Meier method and compared using the log-rank test. Cox regression analysis was used for univariate and multivariate analyses, and the hazard ratio (HR) with 95% CI was calculated. The PH assumption was checked for the Cox regression models by constructing test statistics based on asymptotically mean-zero processes66. If the global P < 0.05, the PH assumption was violated; otherwise, the assumption was valid66. The relative importance of each variable in the multivariable model to predict the prognosis was assessed by using the χ2 statistic minus the corresponding degree of freedom67. Interactions between the PSGC and adjuvant chemotherapy were detected by means of Cox regression analysis. Assessment of the effects of PSGC on adjuvant chemotherapy benefits in stage II and III GC patients was prespecified. All statistical analyses were performed using SPSS (version 19.0) and R (version 4.0.5) software. The LASSO-Cox regression method was performed using the “glmnet” package. The PH assumption was checked using the “CoxPhLb” package. The development, validation and performance assessment of the prognostic nomograms were conducted using the “rms” package. Comparisons of C-indexes between different models were performed using the “compareC” package. The time-dependent ROC curves were plotted using “riskRegression” package. Decision curve analysis was performed with the function of “stdca.R”. The “survminer” package was used for computing survival analyses. Tests were 2-sided, and P < 0.05 was considered to indicate statistical significance.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Supplementary information
Acknowledgements
This work was supported by grant 2019YFE0113700 (S.Z.) from the State’s Key Project of Research and Development Plan; grants 82103041 (D.C.), 82102693 (M.F.), 82273360 (J.Y.), and 81773117 (J.Y.) from the National Natural Science Foundation of China; grant 2019JC05Y361 (G.L.) from the Guangdong Provincial Major Talents Project; grant 202206010085 (J.Y.) from the Science and Technology Planning Project of Guangzhou City; grant 2021B0101420005 (G.L.) from the Key-Area Research and Development Programme of Guangdong Province; grant 2020B121201004 (G.L.) from the Guangdong Provincial Key Laboratory of Precision Medicine for Gastrointestinal Cancer; grant 2021J006 (D.C.) from the Outstanding Youths Development Scheme of Nanfang Hospital, Southern Medical University; grants 2018Y2003 (G.C.), 2019L3018 (G.C.), and 2019YZ016006 (G.C.) from the Science and Technology Programme of Fujian Province; grant 2019Z023 (J.Y.) from the President Foundation of Nanfang Hospital, Southern Medical University; grants 2020CR001 (D.C.) and 2018CR034 (J.Y.) from the Clinical Research Project of Nanfang Hospital, Southern Medical University; and grants 202212121011 (D.C.), S202212121092 (J.Y.) and S202212121104 (J.Y.) from the Training Programme for Undergraduate Innovation and Entrepreneurship.
Source data
Author contributions
S.Z., S.L., G.L., G.C., and J.Y. conceived, designed and supervised the study; D.C., M.F., L.C., L.L., J.C., W.X., C.L. W.J., X.D., J.S., D.L., and J.L. collected and assembled the data; D.C, M.F., L.C., S.Z., G.L., G.C., and J.Y. were responsible for data analysis and interpretation; and D.C., M.F., and J.Y. wrote the manuscript with contributions from all other authors.
Peer review
Peer review information
Nature Communications thanks Yisheng Li and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Data availability
The H&E images and clinical information analysed during the current study are not publicly available for patient privacy purposes. Data access can be obtained through a reasonable request to J.Y. (yanjunfudan@163.com). Access to the data will be restricted to non-commercial research which removes patient-sensitive information. All requests will be answered within 10 working days. The source data underlying Figs. 2–4 and Supplementary Figs. 1–21 is provided as a Source data file. Source data are provided with this paper.
Code availability
The codes used for the slide image process and feature extraction are publicly available at https://github.com/CellProfiler/CellProfiler22. The codes used to develop and evaluate the prediction model are publicly available at https://github.com/Dexin-Chen/Pathomics-analysis and are also placed on the Zenodo platform68.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Dexin Chen, Meiting Fu, Liangjie Chi, Liyan Lin.
Contributor Information
Shuangmu Zhuo, Email: shuangmuzhuo@gmail.com.
Side Liu, Email: liuside2011@163.com.
Guoxin Li, Email: gzliguoxin@163.com.
Gang Chen, Email: naichengang@126.com.
Jun Yan, Email: yanjunfudan@163.com.
Supplementary information
The online version contains supplementary material available at 10.1038/s41467-022-34703-w.
References
- 1.GBD. 2017 Stomach Cancer Collaborators. The global, regional, and national burden of stomach cancer in 195 countries, 1990–2017: a systematic analysis for the Global Burden of Disease study 2017. Lancet Gastroenterol. Hepatol. 2020;5:42–54. doi: 10.1016/S2468-1253(19)30328-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2018 (5th edition) Gastric Cancer. 2020;24:1–21. doi: 10.1007/s10120-020-01042-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jiang Y, et al. Association of adjuvant chemotherapy with survival in patients with stage II or III gastric cancer. JAMA Surg. 2017;152:e171087. doi: 10.1001/jamasurg.2017.1087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gambardella V, Cervantes A. Precision medicine in the adjuvant treatment of gastric cancer. Lancet Oncol. 2018;19:583–584. doi: 10.1016/S1470-2045(18)30131-1. [DOI] [PubMed] [Google Scholar]
- 5.Cristescu R, et al. Molecular analysis of gastric cancer identifies subtypes associated with distinct clinical outcomes. Nat. Med. 2015;21:449–456. doi: 10.1038/nm.3850. [DOI] [PubMed] [Google Scholar]
- 6.Lei Z, et al. Identification of molecular subtypes of gastric cancer with different responses to PI3-kinase inhibitors and 5-fluorouracil. Gastroenterology. 2013;145:554–565. doi: 10.1053/j.gastro.2013.05.010. [DOI] [PubMed] [Google Scholar]
- 7.Cancer Genome Atlas Research Network. Comprehensive molecular characterization of gastric adenocarcinoma. Nature. 2014;513:202–209. doi: 10.1038/nature13480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chia NY, Tan P. Molecular classification of gastric cancer. Ann. Oncol. 2016;27:763–769. doi: 10.1093/annonc/mdw040. [DOI] [PubMed] [Google Scholar]
- 9.Yoo S, et al. Whole-slide image analysis reveals quantitative landscape of tumor–immune microenvironment in colorectal cancers. Clin. Cancer Res. 2020;26:870–881. doi: 10.1158/1078-0432.CCR-19-1159. [DOI] [PubMed] [Google Scholar]
- 10.Ehteshami BB, et al. Diagnostic assessment of deep learning algorithms for detection of lymph node metastases in women with breast cancer. JAMA. 2017;318:2199–2210. doi: 10.1001/jama.2017.14585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gupta R, Kurc T, Sharma A, Almeida JS, Saltz J. The emergence of pathomics. Curr. Pathobiol. Rep. 2019;7:73–84. [Google Scholar]
- 12.Bera K, Schalper KA, Rimm DL, Velcheti V, Madabhushi A. Artificial intelligence in digital pathology—new tools for diagnosis and precision oncology. Nat. Rev. Clin. Oncol. 2019;16:703–715. doi: 10.1038/s41571-019-0252-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Niazi M, Parwani AV, Gurcan MN. Digital pathology and artificial intelligence. Lancet Oncol. 2019;20:e253–e261. doi: 10.1016/S1470-2045(19)30154-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jiang Y, et al. ImmunoScore signature: a prognostic and predictive tool in gastric cancer. Ann. Surg. 2018;267:504–513. doi: 10.1097/SLA.0000000000002116. [DOI] [PubMed] [Google Scholar]
- 15.Chen D, et al. Association of the collagen signature in the tumor microenvironment with lymph node metastasis in early gastric cancer. JAMA Surg. 2019;154:e185249. doi: 10.1001/jamasurg.2018.5249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tibshirani R. Regression shrinkage and selection via the lasso: a retrospective. J. R. Stat. Soc. B. 2011;73:273–282. [Google Scholar]
- 17.Tibshirani R. The lasso method for variable selection in the Cox model. Stat. Med. 1997;16:385–395. doi: 10.1002/(sici)1097-0258(19970228)16:4<385::aid-sim380>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- 18.Chen D, et al. Association of tumor-associated collagen signature with prognosis and adjuvant chemotherapy benefits in patients with gastric cancer. JAMA Netw. Open. 2021;4:e2136388. doi: 10.1001/jamanetworkopen.2021.36388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Noh SH, et al. Adjuvant capecitabine plus oxaliplatin for gastric cancer after D2 gastrectomy (CLASSIC): 5-year follow-up of an open-label, randomised phase 3 trial. Lancet Oncol. 2014;15:1389–1396. doi: 10.1016/S1470-2045(14)70473-5. [DOI] [PubMed] [Google Scholar]
- 20.Cheong JH, et al. Predictive test for chemotherapy response in resectable gastric cancer: a multi-cohort, retrospective analysis. Lancet Oncol. 2018;19:629–638. doi: 10.1016/S1470-2045(18)30108-6. [DOI] [PubMed] [Google Scholar]
- 21.Carpenter AE, et al. CellProfiler: image analysis software for identifying and quantifying cell phenotypes. Genome Biol. 2006;7:R100. doi: 10.1186/gb-2006-7-10-r100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stirling DR, et al. CellProfiler 4: improvements in speed, utility and usability. BMC Bioinforma. 2021;22:433. doi: 10.1186/s12859-021-04344-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Komura D, Ishikawa S. Machine learning methods for histopathological image analysis. Comput. Struct. Biotechnol. J. 2018;16:34–42. doi: 10.1016/j.csbj.2018.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jiang Y, et al. Development and validation of a deep learning CT signature to predict survival and chemotherapy benefit in gastric cancer: a multicenter, retrospective study. Ann. Surg. 2021;274:e1153–e1161. doi: 10.1097/SLA.0000000000003778. [DOI] [PubMed] [Google Scholar]
- 25.Zhang L, et al. A deep learning risk prediction model for overall survival in patients with gastric cancer: a multicenter study. Radiother. Oncol. 2020;150:73–80. doi: 10.1016/j.radonc.2020.06.010. [DOI] [PubMed] [Google Scholar]
- 26.Gambardella V, et al. The role of tumor-associated macrophages in gastric cancer development and their potential as a therapeutic target. Cancer Treat. Rev. 2020;86:102015. doi: 10.1016/j.ctrv.2020.102015. [DOI] [PubMed] [Google Scholar]
- 27.Jiang Y, et al. Tumor immune microenvironment and chemosensitivity signature for predicting response to chemotherapy in gastric cancer. Cancer Immunol. Res. 2019;7:2065–2073. doi: 10.1158/2326-6066.CIR-19-0311. [DOI] [PubMed] [Google Scholar]
- 28.Al-Batran SE, et al. Perioperative chemotherapy with fluorouracil plus leucovorin, oxaliplatin, and docetaxel versus fluorouracil or capecitabine plus cisplatin and epirubicin for locally advanced, resectable gastric or gastro-oesophageal junction adenocarcinoma (FLOT4): a randomised, phase 2/3 trial. Lancet. 2019;393:1948–1957. doi: 10.1016/S0140-6736(18)32557-1. [DOI] [PubMed] [Google Scholar]
- 29.Cunningham D, et al. Perioperative chemotherapy versus surgery alone for resectable gastroesophageal cancer. N. Engl. J. Med. 2006;355:11–20. doi: 10.1056/NEJMoa055531. [DOI] [PubMed] [Google Scholar]
- 30.Wang FH, et al. The Chinese Society of Clinical Oncology (CSCO): clinical guidelines for the diagnosis and treatment of gastric cancer, 2021. Cancer Commun. 2021;41:747–795. doi: 10.1002/cac2.12193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yu J, et al. Effect of laparoscopic vs open distal gastrectomy on 3-year disease-free survival in patients with locally advanced gastric cancer: the CLASS-01 randomized clinical trial. JAMA. 2019;321:1983–1992. doi: 10.1001/jama.2019.5359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yu KH, et al. Predicting non-small cell lung cancer prognosis by fully automated microscopic pathology image features. Nat. Commun. 2016;7:12474. doi: 10.1038/ncomms12474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cheng J, et al. Integrative analysis of histopathological images and genomic data predicts clear cell renal cell carcinoma prognosis. Cancer Res. 2017;77:e91–e100. doi: 10.1158/0008-5472.CAN-17-0313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fu Y, et al. Pan-cancer computational histopathology reveals mutations, tumor composition and prognosis. Nat. Cancer. 2020;1:800–810. doi: 10.1038/s43018-020-0085-8. [DOI] [PubMed] [Google Scholar]
- 35.Pagès F, et al. International validation of the consensus Immunoscore for the classification of colon cancer: a prognostic and accuracy study. Lancet. 2018;391:2128–2139. doi: 10.1016/S0140-6736(18)30789-X. [DOI] [PubMed] [Google Scholar]
- 36.Huang Y, et al. Radiomics signature: a potential biomarker for the prediction of disease-free survival in early-stage (I or II) non-small cell lung cancer. Radiology. 2016;281:947–957. doi: 10.1148/radiol.2016152234. [DOI] [PubMed] [Google Scholar]
- 37.Tang XR, et al. Development and validation of a gene expression-based signature to predict distant metastasis in locoregionally advanced nasopharyngeal carcinoma: a retrospective, multicentre, cohort study. Lancet Oncol. 2018;19:382–393. doi: 10.1016/S1470-2045(18)30080-9. [DOI] [PubMed] [Google Scholar]
- 38.Collins GS, Reitsma JB, Altman DG, Moons KG. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): the TRIPOD statement. BMJ. 2015;350:g7594. doi: 10.1136/bmj.g7594. [DOI] [PubMed] [Google Scholar]
- 39.Lei Z, et al. Nomogram for preoperative estimation of microvascular invasion risk in hepatitis B virus-related hepatocellular carcinoma within the Milan criteria. JAMA Surg. 2016;151:356–363. doi: 10.1001/jamasurg.2015.4257. [DOI] [PubMed] [Google Scholar]
- 40.Yuan S, Xie SH. Urban-rural disparity in cancer incidence in China, 2008-2012: a cross-sectional analysis of data from 36 cancer registers. BMJ Open. 2021;11:e42762. doi: 10.1136/bmjopen-2020-042762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Slagter AE, et al. Prognostic value of tumor markers and ctDNA in patients with resectable gastric cancer receiving perioperative treatment: results from the CRITICS trial. Gastric Cancer. 2022;25:401–410. doi: 10.1007/s10120-021-01258-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lin JP, et al. Prognostic significance of pre- and post-operative tumour markers for patients with gastric cancer. Br. J. Cancer. 2020;123:418–425. doi: 10.1038/s41416-020-0901-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Thomas SN, Zhu F, Schnaar RL, Alves CS, Konstantopoulos K. Carcinoembryonic antigen and CD44 variant isoforms cooperate to mediate colon carcinoma cell adhesion to E- and L-selectin in shear flow. J. Biol. Chem. 2008;283:15647–15655. doi: 10.1074/jbc.M800543200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Berg EL, Robinson MK, Mansson O, Butcher EC, Magnani JL. A carbohydrate domain common to both sialyl Le(a) and sialyl Le(X) is recognized by the endothelial cell leukocyte adhesion molecule ELAM-1. J. Biol. Chem. 1991;266:14869–14872. [PubMed] [Google Scholar]
- 45.Barisoni L, Lafata KJ, Hewitt SM, Madabhushi A, Balis U. Digital pathology and computational image analysis in nephropathology. Nat. Rev. Nephrol. 2020;16:669–685. doi: 10.1038/s41581-020-0321-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.LeCun Y, Bengio Y, Hinton G. Deep learning. Nature. 2015;521:436–444. doi: 10.1038/nature14539. [DOI] [PubMed] [Google Scholar]
- 47.Madabhushi A, Lee G. Image analysis and machine learning in digital pathology: challenges and opportunities. Med. Image Anal. 2016;33:170–175. doi: 10.1016/j.media.2016.06.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rudin C. Stop explaining black box machine learning models for high stakes decisions and use interpretable models instead. Nat. Mach. Intell. 2019;1:206–215. doi: 10.1038/s42256-019-0048-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ruifrok AC, Johnston DA. Quantification of histochemical staining by color deconvolution. Anal. Quant. Cytol. Histol. 2001;23:291–299. [PubMed] [Google Scholar]
- 50.Bray MA, Fraser AN, Hasaka TP, Carpenter AE. Workflow and metrics for image quality control in large-scale high-content screens. J. Biomol. Screen. 2012;17:266–274. doi: 10.1177/1087057111420292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Field DJ. Relations between the statistics of natural images and the response properties of cortical cells. J. Opt. Soc. Am. A. 1987;4:2379–2394. doi: 10.1364/josaa.4.002379. [DOI] [PubMed] [Google Scholar]
- 52.Haralick RM. Statistical and structural approaches to texture. Proc. IEEE. 1979;67:786–804. [Google Scholar]
- 53.Sun Y, Duthaler S, Nelson BJ. Autofocusing in computer microscopy: selecting the optimal focus algorithm. Microsc. Res. Tech. 2004;65:139–149. doi: 10.1002/jemt.20118. [DOI] [PubMed] [Google Scholar]
- 54.Otsu N. A thresholding selection method from gray-level histogram. IEEE Trans. Syst. Man Cybern. 1979;9:62–66. [Google Scholar]
- 55.Aaron JS, Taylor AB, Chew TL. Image co-localization–co-occurrence versus correlation. J. Cell Sci. 2018;131:s211847. doi: 10.1242/jcs.211847. [DOI] [PubMed] [Google Scholar]
- 56.Vincent L. Granulometries and opening trees. Fund. Inf. 2000;41:57–90. [Google Scholar]
- 57.Maragos P. Pattern spectrum and multiscale shape representation. IEEE Trans. Pattern Anal. Mach. Intell. 1989;11:701–716. [Google Scholar]
- 58.Hothorn T, Zeileis A. Generalized maximally selected statistics. Biometrics. 2008;64:1263–1269. doi: 10.1111/j.1541-0420.2008.00995.x. [DOI] [PubMed] [Google Scholar]
- 59.Gerds TA, Kattan MW, Schumacher M, Yu C. Estimating a time-dependent concordance index for survival prediction models with covariate dependent censoring. Stat. Med. 2013;32:2173–2184. doi: 10.1002/sim.5681. [DOI] [PubMed] [Google Scholar]
- 60.Kattan MW. Judging new markers by their ability to improve predictive accuracy. J. Natl Cancer Inst. 2003;95:634–635. doi: 10.1093/jnci/95.9.634. [DOI] [PubMed] [Google Scholar]
- 61.Vickers AJ, Elkin EB. Decision curve analysis: a novel method for evaluating prediction models. Med. Decis. Mak. 2006;26:565–574. doi: 10.1177/0272989X06295361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Vickers AJ, Cronin AM, Elkin EB, Gonen M. Extensions to decision curve analysis, a novel method for evaluating diagnostic tests, prediction models and molecular markers. BMC Med. Inform. Decis. Mak. 2008;8:53. doi: 10.1186/1472-6947-8-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kang L, Chen W, Petrick NA, Gallas BD. Comparing two correlated C indices with right-censored survival outcome: a one-shot nonparametric approach. Stat. Med. 2015;34:685–703. doi: 10.1002/sim.6370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988;44:837–845. [PubMed] [Google Scholar]
- 65.Pencina MJ, D’Agostino RS, Steyerberg EW. Extensions of net reclassification improvement calculations to measure usefulness of new biomarkers. Stat. Med. 2011;30:11–21. doi: 10.1002/sim.4085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Lee CH, Ning J, Shen Y. Model diagnostics for the proportional hazards model with length-biased data. Lifetime Data Anal. 2019;25:79–96. doi: 10.1007/s10985-018-9422-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Bajaj NS, et al. Coronary microvascular dysfunction and cardiovascular risk in obese patients. J. Am. Coll. Cardiol. 2018;72:707–717. doi: 10.1016/j.jacc.2018.05.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Chen, D. Prognostic and predictive value of a pathomics signature in gastric cancer. 10.5281/zenodo.7274306 (2022). [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The H&E images and clinical information analysed during the current study are not publicly available for patient privacy purposes. Data access can be obtained through a reasonable request to J.Y. (yanjunfudan@163.com). Access to the data will be restricted to non-commercial research which removes patient-sensitive information. All requests will be answered within 10 working days. The source data underlying Figs. 2–4 and Supplementary Figs. 1–21 is provided as a Source data file. Source data are provided with this paper.
The codes used for the slide image process and feature extraction are publicly available at https://github.com/CellProfiler/CellProfiler22. The codes used to develop and evaluate the prediction model are publicly available at https://github.com/Dexin-Chen/Pathomics-analysis and are also placed on the Zenodo platform68.