Abstract
Introduction:
The impact of depressed mood in daily life is difficult to investigate using traditional retrospective assessments, given daily or even within-day mood fluctuations in various contexts. This study aimed to use a smartphone-based ambulatory assessment to examine real-time relationships between depressed mood and functional behaviors among individuals with stroke.
Methods:
A total of 202 participants with mild-to-moderate stroke (90% ischemic, 45% female, 44% Black) completed an ecological momentary assessment five times per day for 2 weeks by reporting their depressed mood and functional behaviors regarding where, with whom, and what activity was spent.
Results:
Participants spent 28% of their wake-up time participating in passive leisure activities but spent the least time in physical (4%) and vocational (9%) activities. Depressed mood was concurrently lower when participants engaged in social activities (β = −0.023 ± 0.011) and instrumental activities of daily living (β = −0.061 ± 0.013); spent time with family members (β = −0.061 ± 0.014), spouses (β = −0.043, ± 0.016), friends (β = −0.094, ± 0.021), and coworkers (β = −0.050 ± 0.021); and were located in restaurants (β = −0.068 ± 0.029), and homes of family members (β = −0.039 ± 0.020) or friends (β = −0.069 ± 0.031). Greater depressed mood was associated with worse ratings in satisfaction, performance, and engagement of activities in concurrent (βs = −0.036 ± 0.003, −0.053 ± 0.003, −0.044 ± 0.003) and time-lagged models (β = −0.011 ± 0.004, −0.012 ± 0.004, −0.013 ± 0.004).
Discussion:
Smartphone-based ambulatory assessment can elucidate functional behaviors and associated mood after stroke. Findings support behavioral activation treatments to schedule social and instrumental activities for stroke survivors to reduce their depressed mood.
Keywords: Telemedicine, mobile health, smartphone, ambulatory assessment, ecological momentary assessment, stroke, depression, daily functional behaviors
Introduction
Stroke survivorship and its long-term consequences is a significant public health problem. Stroke is one of the leading causes of long-term disability worldwide.1 Every year approximately 795,000 people in the United States experience a stroke. Of those 795,000 individuals, 610,000 are incident cases, and 185,000 are recurrent strokes. Depressed mood (DM) is the most common neuropsychiatric complication following a stroke, affecting a third of all stroke survivors. DM is associated with higher mortality rates, suicidal ideation, and cognitive deficits. It can persist multiple years after stroke, leading to a higher prevalence of long-term disabilities than those without depression2 including reduced functional status, decreased social participation, and decreased quality of life.3 Despite its high prevalence, the etiology of poststroke DM is poorly understood and complex, involving multiple factors. Neurobiological factors such as a left-hemispheric lesion, cumulative lacunes in deep brain structures, and larger lateral and third ventricle to brain ratio have been associated with an increased likelihood of developing DM.4 As well as older age, female sex, genetics, history of depression, and diabetes mellitus. Psychosocial factors present during stroke recovery may also impact the occurrence of DM. Poor social support, divorce, and living alone increase the likelihood of developing DM.4 Stroke survivors report experiencing social marginalization, decreased self-esteem, and maladaptive psychological changes, such as passive coping and neuroticism.
Detailed insight into factors affecting the course of DM is needed to develop effective treatments. These efforts are impeded by the way depression is commonly measured via one-time psychiatric interviews or questionnaires, such as Hospital Anxiety and Depression Scale,5 and Patient Health Questionnaire, which query depressive symptoms retrospectively (e.g. past 2 weeks) making them more prone to recall bias.6 Bias may be amplified in instances where poststroke cognitive impairment may limit accurate recall. Moreover, traditional measures cannot capture dynamic variations in DM over time. Traditional measures produce a single score capturing the average level of DM in a given period. This single-score approach disregards that poststroke symptoms vary across or within days based on context (e.g. activities a person is engaged in and who they are with). Furthermore, traditional measures are administered in a controlled setting (e.g. lab or clinic), limiting the ability to compare dynamic variations in poststroke symptoms across real-world contexts.7 Thus, clinicians and researchers need more precise measurements to gain a deeper understanding of the variability and influence of DM in day-to-day contexts.
Technology-based ambulatory assessments, such as ecological momentary assessment (EMA) may overcome many limitations of traditional measures. EMA captures real-world data through repeated assessments administered via a smartphone. This method minimizes recall bias by measuring mood and daily behaviors in real time. It captures temporal and contextual variations by assessing study constructs multiple times a day within an individual’s natural context. As such, a strength of EMA is the ability to capture intensive longitudinal data to study within- and between-subject variability of DM in daily life.8 EMA allows us to understand poststroke daily activity patterns which may provide novel insights into the etiology of DM and its impact on functional behaviors after stroke.
Despite these advantages, only a few studies have used EMA to study DM after stroke. One study supported the validity of EMA in measuring DM after stroke.9 Another EMA study showed that fewer social interactions but higher participation in sports and work activities after hospital discharge predicted higher DM at 3 months poststroke.10 Notably, both studies included a small sample (n = 489 and n = 3610) and focused on the first 3 months poststroke, limiting generalizability to the broader poststroke population. In addition, Jean and colleagues10 measured a limited range of daily activities, highlighting a need for research to expand what is known about daily functional behaviors across multiple domains. The present study aimed to investigate DM related to daily functional behaviors during the chronic phase after stroke, i.e., at least 3-month poststroke. We used EMA to assess DM and time spent in and performance appraisals of daily activities. We investigated whether DM was predicted by activity type, locations, and social interactions. We hypothesized that higher DM was reported when participants stayed at home, alone, and did passive, sedentary activities. We also investigated if DM was momentarily related to perceived activity quality. We hypothesized that DM was higher during activities experienced as more difficult, less satisfied and engaged, and more help needed.
Methods
Participants
Participants were recruited between October 2018 and January 2021 using a hospital database. Inclusion criteria for the study included mild-to-moderate stroke defined by a National Institutes of Health Stroke Scale (NIHSS)11 score ≤ 13 at the time of stroke onset, hemorrhagic or ischemic stroke, ≥ 3 months poststroke before enrollment, no or minor disability pre-stroke measured by a modified Rankin Scale (mRS)12 score ≤ 2, 18 + years old, and fluency in English. Exclusion criteria included previous co-morbid neurologic or psychiatric disorders, severe communication difficulty (Frenchay Aphasia Screening Test score <24), severe apraxia (Apraxia Screen of Test for Upper-Limb Apraxia score <6), visual inattention (Star Cancellation Test score <44), and visual acuity worse than 20/100 corrected version on the Lighthouse Near Visual Acuity test
We recruited 234 potential participants. Eight participants did not meet the eligibility criteria, and 14 participants dropped out before completing the study. Figure 1 shows a flow diagram of participant recruitment and completion. Two hundred and two participants completed the entire study protocol and had the EMA completion ≥ 30%. The institutional review board at the study sites approved this study. All participants provided written informed consent.
Figure 1.
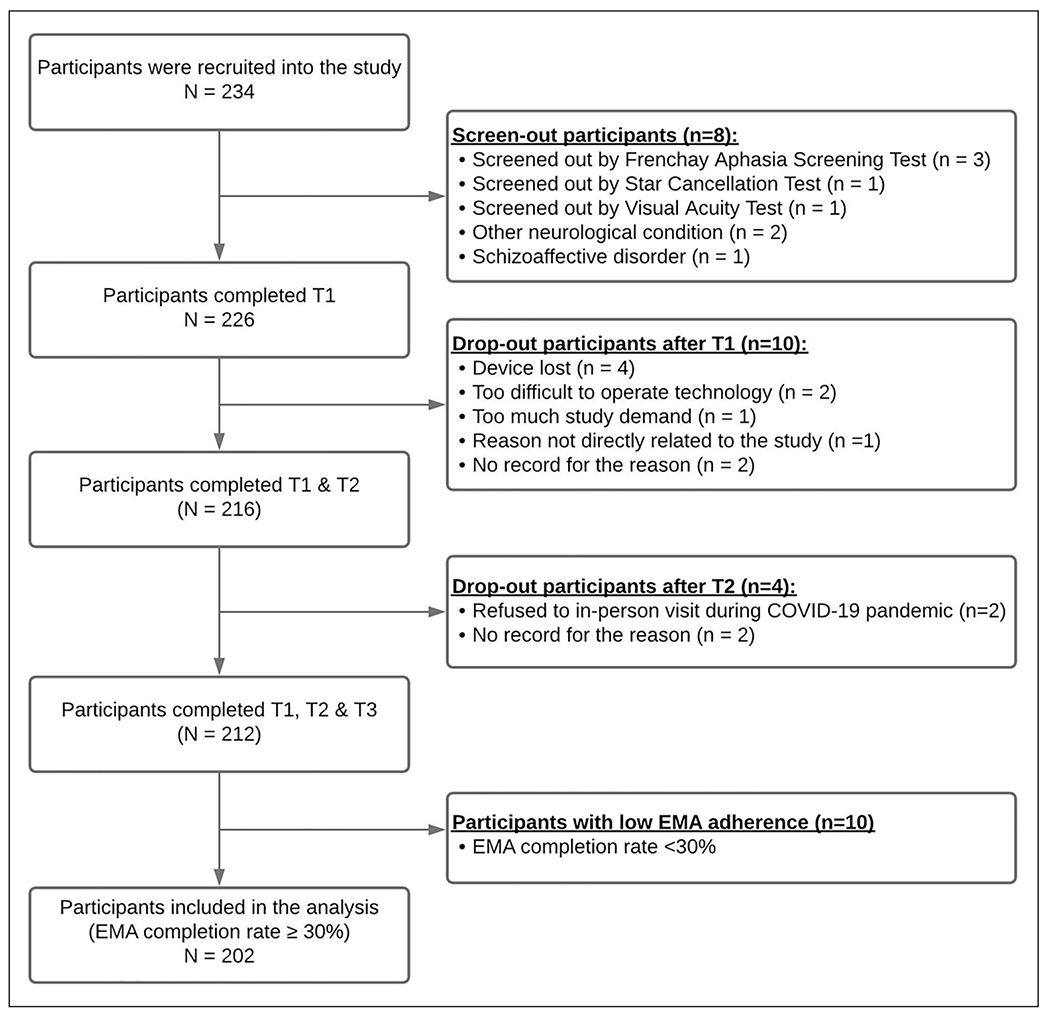
Flow diagram showing participant recruitment and completion. T1: First lab visit, T2: 14 day EMA monitoring, T3: Second lab visit. EMA: ecological momentary assessment.
Procedures
At the initial lab-based visit, participants completed screening to ensure eligibility. Participants completed a 20-min individualized tutorial on how to use Status/Post, an EMA survey mobile application (app) using their iPhone or an iPod Touch device we provided. They completed a practice survey monitored by the examiner to assess any difficulties participants had with using the app or survey and were provided with hotlines to call should questions arise.
The EMA protocol started within 1 week of the initial visit. During the 14-day EMA period, participants completed five surveys per day between the hours of 8 a.m.–10 p.m., 11 a.m.–1 p.m., 2 p.m.–4 p.m., 5 p.m.–7 p.m., and 8 p.m.–10 p.m. On the first 2 days and periodically thereafter, the examiner called the participant to verify any questions completing the surveys at home. After the 14-day period, participants returned to the lab to return the device or delete the app from their iPhones. Participants were compensated up to $125 for baseline and follow-up lab visits and EMA survey completed (maximum of 70 surveys).
EMA functioning survey
We developed an EMA functioning survey tailored to the unique needs of stroke survivors by modifying a validated EMA functioning survey.13 EMA surveys were predominantly checkbox or slider-format questions. Participants first reported their current location (home, workplace, restaurant, etc.). Next, participants reported with whom they were with (alone, family members, coworkers, etc.). The subsequent screens were customized to deliver home versus nonhome queries tapping a range of potential activities. Based on prior classification models,14,15 we categorized activities into domains (e.g. physical, cognitive, social, activities of daily living (ADL), instrumental ADL (IADL), vocational, and passive leisure activities) and further grouped them into “total productive” versus “non-productive, sedentary” activities. After reporting what they were doing, participants rated the activity quality with the following questions: “How much help are you getting from someone else while doing this activity?”, “I am performing this activity well…”, “I am satisfied with doing this activity…”, and “I am engaged in doing this activity…”. Questions were answered on a 7-point scale from “no help/not well/not satisfied/not engaged” to “a lot of help/very well/very satisfied/very engaged”.
Participants also reported current levels of DM with the following question “Right now, I feel depressed…” with five possible response options (“not at all” to “very much”) during each EMA survey.
Statistical analysis
We used descriptive statistics to examine the study sample demographics. Multilevel models were used to investigate concurrent and lagged associations between DM and daily behaviors based on the time of day. EMA observations were thus modeled as level 1 (within-person level) units nested within individuals, who were modeled as level 2 (between-person level). The significance level was set at 0.05. We conducted two sets of models to examine (1) concurrent associations: either activity type, location, the person interacting with, or quality of activity as a predictor of same-survey DM and (2) lagged associations: either activity type, location, persons interacting with, or quality of activity as a predictor of next-survey DM. For time-lag associations, we included each predictor at the previous time point (t − 1) to predict the DM at the time point (t) and adjusted with the DM at a previous time point (t − 1). Activity quality variables were centered on creating person-centered deviation scores. The centered value indicated the momentary change (for moment-to-moment analyses) relative to each person’s own weekly average. Centering allows for examining within-person and between-person variance separately.16 We performed PROC MIXED in SAS version 9.4 to model between-person and within-person variances and account for the autocorrelation between adjacent observations. PROC MIXED is robust in handling missing data. This procedure does not omit the observations listwise, thus analyzing all data and assuming random missingness.17 We generated figures using R software, version 4.0.3.
Results
Sample characteristics
The EMA survey completion rate was 86.3% (14,140 surveys). We excluded 10 participants with low EMA adherence (<30%) from the analyses. The majority of included participants were men (55%), White (55%), married (52%), unemployed (57%), ischemic stroke (90%), and neurologic mild (75%) with the mean age of 59.7 years (SD = 11.7) (Table 1). Compared to the included participants, the excluded participants had lower total household income, higher DM, lower cognition, less mobile device usage experience, and required more mobility device use in the community.
Table 1.
Clinico-demographic information of participants.
| Variable | Overall, n = 212a | Excluded participants, n = 10a | Included participants, n = 202a | P-valueb |
|---|---|---|---|---|
| Stroke diagnosis | 0.603 | |||
| Hemorrhagic | 20 (9.4%) | 0 (0%) | 20 (9.9%) | |
| Ischemic | 192 (91%) | 10 (100%) | 182 (90%) | |
| Stroke side | 0.278 | |||
| Bilateral | 9 (4.3%) | 0 (0%) | 9 (4.5%) | |
| Left | 84 (40%) | 3 (30%) | 81 (40%) | |
| Right | 83 (39%) | 3 (30%) | 80 (40%) | |
| Unknown | 35 (17%) | 4 (40%) | 31 (15%) | |
| Handedness | 0.181 | |||
| Both | 1 (0.5%) | 0 (0%) | 1 (0.5%) | |
| Left | 28 (14%) | 3 (30%) | 25 (13%) | |
| Right | 178 (86%) | 7 (70%) | 171 (87%) | |
| Premorbid disability (mRS) | 0.188 | |||
| 0 | 177 (84%) | 8 (80%) | 169 (84%) | |
| 1 | 20 (9.5%) | 0 (0%) | 20 (10.0%) | |
| 2 | 14 (6.6%) | 2 (20%) | 12 (6.0%) | |
| Stroke severity (NIHSS) | 3.23 (3.55) | 3.50 (3.17) | 3.21 (3.57) | 0.549 |
| Mean momentary depressed mood (DM) | 0.24 (0.63) | 0.46 (0.77) | 0.24 (0.63) | <0.001 |
| Time since stroke (days) | 1449.33 (1025.35) | 1639.00 (1378.75) | 1439.95 (1008.29) | 0.839 |
| Age | 59.85 (11.69) | 62.10 (11.45) | 59.74 (11.72) | 0.459 |
| Gender | 0.518 | |||
| Female | 93 (44%) | 3 (30%) | 90 (45%) | |
| Male | 119 (56%) | 7 (70%) | 112 (55%) | |
| Race | 0.091 | |||
| Asian | 1 (0.5%) | 0 (0%) | 1 (0.5%) | |
| Black | 97 (46%) | 8 (80%) | 89 (44%) | |
| White | 114 (54%) | 2 (20%) | 112 (55%) | |
| Marital status | 0.079 | |||
| Married/Cohabitating | 107 (50%) | 2 (20%) | 105 (52%) | |
| Separated/Divorced/Widowed | 66 (31%) | 6 (60%) | 60 (30%) | |
| Single | 39 (18%) | 2 (20%) | 37 (18%) | |
| Residential status | 0.063 | |||
| Alone | 51 (24%) | 5 (50%) | 46 (23%) | |
| With others | 161 (76%) | 5 (50%) | 156 (77%) | |
| Education years | 14.13 (2.63) | 12.80 (2.97) | 14.20 (2.60) | 0.069 |
| Number of previous stroke | 1.65 (1.76) | 1.78 (1.09) | 1.65 (1.78) | 0.227 |
| Employment status | 0.195 | |||
| Full time | 57 (27%) | 0 (0%) | 57 (28%) | |
| Not employed | 125 (59%) | 9 (90%) | 116 (57%) | |
| Part time | 27 (13%) | 1 (10%) | 26 (13%) | |
| Volunteer | 3 (1.4%) | 0 (0%) | 3 (1.5%) | |
| Total personal income | 0.093 | |||
| $0–$14,999 | 60 (28%) | 6 (60%) | 54 (27%) | |
| $15,000–$34,999 | 59 (28%) | 1 (10%) | 58 (29%) | |
| $35,000–$54,999 | 40 (19%) | 3 (30%) | 37 (18%) | |
| $55,000–$74,999 | 11 (5.2%) | 0 (0%) | 11 (5.4%) | |
| $75,000 or more | 42 (20%) | 0 (0%) | 42 (21%) | |
| Total household income | 0.030 | |||
| $0–$14,999 | 40 (19%) | 5 (50%) | 35 (17%) | |
| $15,000–$34,999 | 37 (17%) | 2 (20%) | 35 (17%) | |
| $35,000–$54,999 | 52 (25%) | 3 (30%) | 49 (24%) | |
| $55,000–$74,999 | 20 (9.4%) | 0 (0%) | 20 (9.9%) | |
| $75,000 or more | 63 (30%) | 0 (0%) | 63 (31%) | |
| Financial responsibilities | >0.999 | |||
| Dependent, and living in residential treatment facility | 7 (3.3%) | 0 (0%) | 7 (3.5%) | |
| Primary and partial responsibility | 205 (97%) | 10 (100%) | 195 (97%) | |
| Social benefits | 0.126 | |||
| Commercial/Private Insurance | 33 (16%) | 0 (0%) | 33 (16%) | |
| No benefit | 30 (14%) | 0 (0%) | 30 (15%) | |
| SSB/Medicare/Medicaid | 149 (70%) | 10 (100%) | 139 (69%) | |
| Mobility device use at home | 0.149 | |||
| Cane/Crutches/Walker | 29 (14%) | 4 (40%) | 25 (12%) | |
| Manual wheelchair | 4 (1.9%) | 0 (0%) | 4 (2.0%) | |
| None | 176 (83%) | 6 (60%) | 170 (85%) | |
| Other | 1 (0.5%) | 0 (0%) | 1 (0.5%) | |
| Power wheelchair | 1 (0.5%) | 0 (0%) | 1 (0.5%) | |
| Mobility device use in community | 0.011 | |||
| Cane/Crutches/Walker | 35 (17%) | 3 (30%) | 32 (16%) | |
| Manual wheelchair | 4 (1.9%) | 0 (0%) | 4 (2.0%) | |
| None | 168 (79%) | 5 (50%) | 163 (81%) | |
| Others | 4 (1.9%) | 2 (20%) | 2 (1.0%) | |
| Power wheelchair | 1 (0.5%) | 0 (0%) | 1 (0.5%) | |
| Global cognition function | 25.86 (3.26) | 22.10 (5.32) | 26.04 (3.02) | 0.017 |
| Comorbidity | 4.56 (2.87) | 5.11 (2.26) | 4.53 (2.90) | 0.312 |
| Mobile device use experience | 0.023 | |||
| No | 6 (2.9%) | 2 (22%) | 4 (2.0%) | |
| Yes | 203 (97%) | 7 (78%) | 196 (98%) |
n (%); Mean (SD).
Fisher’s exact test; Wilcoxon rank-sum test.
mRS: modified Rankin Scale; NIHSS: National Institutes of Health Stroke Scale.
Daily functional behaviors
Table 2 shows participants’ daily functional behaviors. Participants mainly participated in passive leisure sedentary activities (28%), such as watching television and resting. Participants engaged in physical activities (3.6%) least, followed by vocational activities (8.6%). Participants spent most of their time at home (71%) and were primarily alone (27%) or with family members (17%). Regarding activity quality self-appraisal, participants rated their performance very well (mean = 5.19 [SD = 1.37]) and did not need much help (mean = 1.12 [SD = 2.04]). They were highly satisfied (mean = 5.16 [SD = 1.39]) and engaged (mean = 5.11 [SD = 1.45]) while doing activities.
Table 2.
Distribution of EMA-measured functional behaviors and depressed mood (DM).
| EMA surveysa | |
|---|---|
| Type of activity (14,140 EMA surveys) | |
| ADL | 1419 (12%) |
| Cognitive stimulating activity | 1467 (13%) |
| IADL | 2505 (22%) |
| Passive leisure, sedentary activity | 3258 (28%) |
| Physical activity | 415 (3.6%) |
| Social activity | 1523 (13%) |
| Vocational Activity | 993 (8.6%) |
| Location (14,140 EMA surveys) | |
| At community center | 93 (0.8%) |
| At my home | 8298 (71%) |
| At outpatient medical visit | 103 (0.9%) |
| At restaurant | 186 (1.6%) |
| At the home of family member(s) | 552 (4.7%) |
| At the home of friend(s) | 181 (1.6%) |
| At work | 1002 (8.6%) |
| In a vehicle | 439 (3.8%) |
| In class/school setting | 18 (0.2%) |
| In hospital | 57 (0.5%) |
| In public business/store (e.g. post office, grocery store) | 293 (2.5%) |
| Inside, other | 187 (1.6%) |
| Outside, other | 177 (1.5%) |
| Outside, walking | 56 (0.5%) |
| Person interacting with (11,390 EMA surveys) b | |
| Alone | 3118 (27.4%) |
| Coworkers | 581 (5.1%) |
| Family members | 1940 (17.0%) |
| Friends | 441 (3.9%) |
| Healthcare provider | 118 (1.0%) |
| Pets | 861 (7.6%) |
| Spouse or partners | 1518 (13.3%) |
| Other known people | 128 (1.1%) |
| Unknown people | 91 (0.9%) |
| People you are socializing with electronically | 64 (0.6%) |
| Help scorec, mean (SD) | 1.12 (2.04) |
| Performance scorec, mean (SD) | 5.19 (1.37) |
| Satisfaction scorec, mean (SD) | 5.16 (1.39) |
| Engagementc, mean (SD) | 5.11 (1.45) |
| Depressed moodd, mean (SD) | 0.24 (0.63) |
Number of EMA surveys (%) unless otherwise specified.
In the “Who is with you right now” question, participants could respond with more than one response. As participants might experience different depressive feelings across persons, we selected observations with a single response for data analysis.
In the “How much help are you getting from someone else while doing this activity” question, participants rated on a 1 (no help) to 7 (a lot of help) scale. To match the semantic meaning, we converted it into the 0 (no help) to 6 (a lot of help) scale. In the “I am performing this activity well” question, participants rated on a 1 (not well) to 7 (very well) scale. To match the semantic meaning, we converted it into the 0 (not well) to 6 (very well) scale. In the “I am satisfied with doing this activity” question, participants rated on a 1 (not satisfied) to 7 (very satisfied) scale. To match the semantic meaning, we converted it into the 0 (not satisfied) to 6 (very satisfied) scale. In the “I am engaged in doing this activity” question, participants rated on a 1 (not engaged) to 7 (very engaged) scale. To match the semantic meaning, we converted it into the 0 (not engaged) to 6 (very engaged) scale.
In the “Right now, I feel depressed” question, participants rated on a scale with 1: not at all; 2: a little bit; 3: somewhat; 4: quite a bit; and 5: very much. To match the semantic meaning, we converted it into a new scale with 0: not at all; 1: a little bit; 2: somewhat; 3: quite a bit; and 4: very much.
ADL: activities of daily living; EMA: ecological momentary assessment; IADL: instrumental activities of daily living.
Momentary DM
The average momentary DM was 0.24 (± 0.63). Participants experienced some DM in 16% of all observations (i.e. endorsed “A little bit” or higher in 1859 responded surveys).
DM and daily functional behaviors
Concurrent relationships between DM and daily functional behaviors.
Figure 2 shows relationships of DM with activity type, location, and the person interacting with. DM was reduced while doing productive activities (β = −0.027 ± 0.009, p-value = 0.003), being in a location other than home (β = −0.020 ± 0.009, p-value = 0.025), and being with others (β = −0.050 ± 0.010, p-value < 0.0001).
Figure 2.
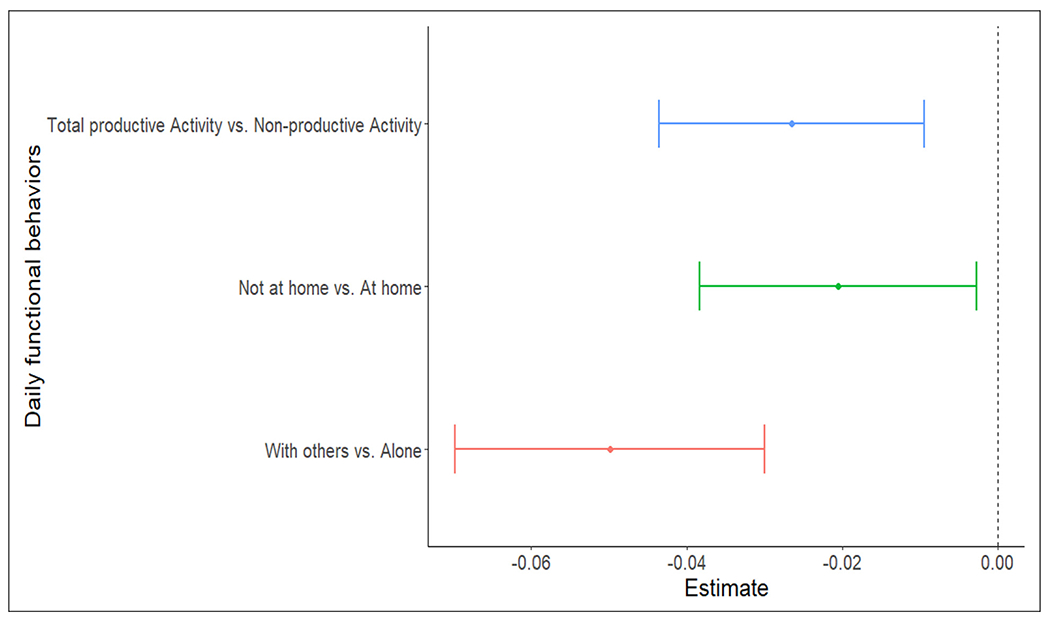
Concurrent relationships of DM with dichotomized functional behaviors: type of activity (total productive activity vs. nonproductive activity), location (not at home vs. at home), and the person interacting with (with others vs. alone). The x-axis showed the estimated DM score. Dots represent the average DM scores, and whiskers represent 95% confidence intervals.
DM: depressed mood.
Table 3 shows seven concurrent models, assessing granular relationships between each functional predictor and DM. For activity type (Figures 3a to 3c), DM was highest while doing passive leisure activity, mean DM = 0.266 ± 0.036 (p < 0.0001). Compared to the passive leisure, performing IADL and social activity had significantly lower mean DM scores (β = −0.023 ± 0.011 (p = 0.041) and −0.061 ± 0.013 (p < 0.0001), respectively).
Table 3.
Multilevel models examining concurrent relationships between depressed mood (DM) and daily functional behaviors.
| Models | Estimation | 95% CI | p value | |
|---|---|---|---|---|
| TYPE OF ACTIVITY | ||||
| Fixed effect | ||||
| Intercept | 0.266 | 0.194 | 0.337 | <0.0001 |
| ADL | −0.015 | −0.041 | 0.010 | 0.241 |
| Cognitive stimulating activity | −0.012 | −0.037 | 0.014 | 0.3693 |
| IADL | −0.023* | −0.045 | −0.001 | 0.0403 |
| Physical activity | −0.022 | −0.063 | 0.019 | 0.2903 |
| Social activity | −0.061** | −0.086 | −0.036 | <0.0001 |
| Vocational activity | −0.016 | −0.048 | 0.016 | 0.3256 |
| Random effect | ||||
| Intercept | 0.254 | 0.203 | 0.306 | <0.0001 |
| Residual | 0.151 | 0.147 | 0.155 | <0.0001 |
| LOCATION | ||||
| Fixed effect | ||||
| Intercept | 0.252** | 0.182 | 0.323 | <0.0001 |
| At community center | −0.021 | −0.103 | 0.061 | 0.6108 |
| At outpatient medical visit | −0.004 | −0.081 | 0.073 | 0.9204 |
| At restaurant | −0.068* | −0.125 | −0.010 | 0.0216 |
| At the home of family member(s) | −0.039* | −0.078 | −0.001 | 0.0467 |
| At the home of friend(s) | −0.069* | −0.129 | −0.008 | 0.026 |
| At work | 0.003 | −0.027 | 0.033 | 0.826 |
| In a vehicle | −0.001 | −0.040 | 0.038 | 0.9607 |
| In class/school setting | −0.161 | −0.343 | 0.022 | 0.084 |
| In hospital | 0.310** | 0.202 | 0.418 | <0.0001 |
| In public business/store (e.g. post office, grocery store) | −0.038 | −0.085 | 0.008 | 0.1061 |
| Inside, other | −0.015 | −0.074 | 0.044 | 0.6251 |
| Outside, other | −0.076* | −0.136 | −0.016 | 0.0127 |
| Outside, walking | −0.084 | −0.189 | 0.021 | 0.1188 |
| Random effect | ||||
| Intercept | 0.255 | 0.196 | 0.314 | <0.0001 |
| Residual | 0.151 | 0.147 | 0.155 | <0.0001 |
| PERSON INTERACTING WITH | ||||
| Fixed effect | ||||
| Intercept | 0.279 | 0.207 | 0.352 | <0.0001 |
| Coworkers | −0.050* | −0.092 | −0.009 | 0.0184 |
| Family members | −0.061** | −0.088 | −0.033 | <0.0001 |
| Friends | −0.094** | −0.135 | −0.052 | <0.0001 |
| Healthcare provider | 0.002 | −0.076 | 0.080 | 0.9575 |
| Other known people | −0.096* | −0.170 | −0.023 | 0.0102 |
| People you are socializing with electronically | 0.174* | 0.071 | 0.276 | 0.0009 |
| Pets | 0.002 | −0.041 | 0.045 | 0.9293 |
| Spouse or partners | −0.043* | −0.075 | −0.012 | 0.0069 |
| Unknown people | 0.065 | −0.017 | 0.147 | 0.1193 |
| Random effect | ||||
| Intercept | 0.258 | 0.207 | 0.309 | <0.0001 |
| Residual | 0.152 | 0.148 | 0.156 | <0.0001 |
| HELP FROM SOMEONE WHILE DOING ACTIVITIES | ||||
| Fixed effect | ||||
| Intercept | 0.265 | 0.170 | 0.360 | <0.0001 |
| Help score (between-person) | −0.022 | −0.077 | 0.032 | 0.422 |
| Help score (within-person) | −0.002 | −0.006 | 0.002 | 0.378 |
| Random effect | ||||
| Intercept | 0.244 | 0.195 | 0.292 | <0.0001 |
| Residual | 0.131 | 0.127 | 0.135 | <0.0001 |
| PERFORMANCE OF ACTIVITIES | ||||
| Fixed effect | ||||
| Intercept | 1.471 | 1.140 | 1.802 | <0.0001 |
| Performance score (between-person) | −0.240** | −0.303 | −0.177 | <0.0001 |
| Performance score (within-person) | −0.036** | −0.042 | −0.029 | <0.0001 |
| Random effect | ||||
| Intercept | 0.190 | 0.153 | 0.228 | <0.0001 |
| Residual | 0.130 | 0.126 | 0.133 | <0.0001 |
| SATISFACTION WITH DOING ACTIVITIES | ||||
| Fixed effect | ||||
| Intercept | 1.571 | 1.261 | 1.880 | <0.0001 |
| Satisfaction score (between-person) | −0.262** | −0.321 | −0.202 | <0.0001 |
| Satisfaction score (within-person) | −0.053** | −0.059 | −0.046 | <0.0001 |
| Random effect | ||||
| Intercept | 0.177 | 0.142 | 0.213 | <0.0001 |
| Residual | 0.128 | 0.125 | 0.132 | <0.0001 |
| ENGAGEMENT of ACTIVITIES | ||||
| Fixed effect | ||||
| Intercept | 1.363 | 1.066 | 1.661 | <0.0001 |
| Engagement score (between-person) | −0.223** | −0.281 | −0.166 | <0.0001 |
| Engagement score (within-person) | −0.044** | −0.050 | −0.037 | <0.0001 |
| Random effect | ||||
| Intercept | 0.189 | 0.151 | 0.227 | <0.0001 |
| Residual | 0.129 | 0.125 | 0.133 | <0.0001 |
p-value < 0.0001,
p-value < 0.05.
ADL: activities of daily living; IADL: instrumental activities of daily living
Figure 3.
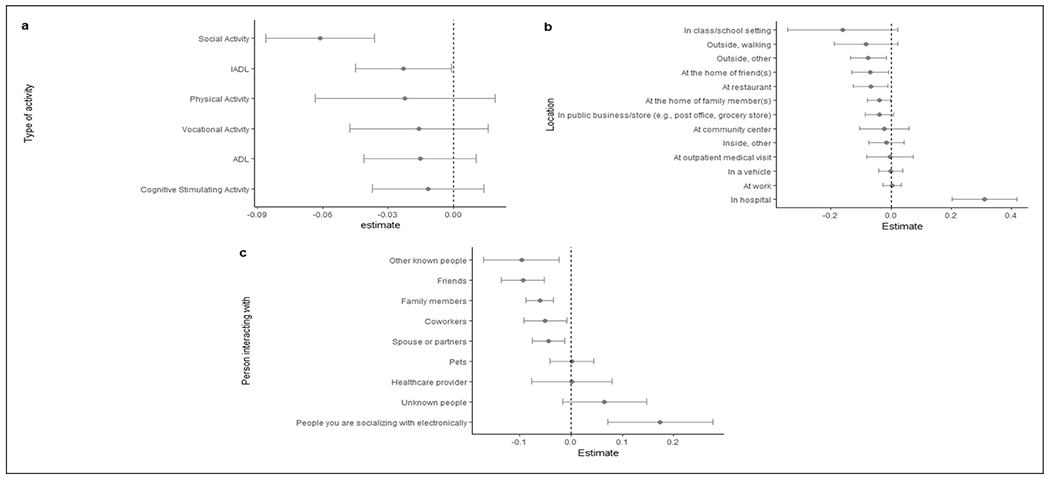
Concurrent relationships of DM with granular functional behaviors: (a) type of activity (reference: passive leisure, sedentary activity), (b) location (reference: home), and (c) the person interacting with (reference: alone). Dots represent the average DM scores, and whiskers represent 95% confidence intervals.
DM: depressed mood.
For the location, “at my home” was used as a reference with mean DM score = 0.252 ± 0.036 (p < 0.0001). When participants were “at the restaurant” (β = −0.068 ± 0.029, p = 0.022), “at home of family member” (β = −0.039 ± 0.020, p = 0.047), “at home of friends” (β = −0.069 ± 0.031, p = 0.026), and “outside, other” (β = −0.076, ± 0.031, p = 0.013), their mean DM score was significantly lower compared to “at my home”. Mean DM score was significantly higher when patients were in the hospital (β = 0.310 ± 0.055, p < 0.0001).
We used being alone as a reference with mean DM score = 0.279±0.037 (p < 0.0001). Participants had significantly lower mean DM scores with “coworkers” (β = −0.050 ± 0.021, p = 0.019), “family member” (β = −0.061 ± 0.014, p < 0.0001), “friends” (β = −0.094, ± 0.021, p < 0.0001), “other known people” (β = −0.096, ± 0.037, p = 0.010), and “spouse or partner” (β = −0.043, ± 0.016, p = 0.007). However, mean DM score was significantly higher while socializing electronically (β = 0.174, ± 0.052, p = 0.001) compared to being alone.
Higher perceived performance (β = −0.036 ± 0.003, p < 0.0001), satisfaction (β = −0.053 ± 0.003, p < 0.0001) and engagement (β = −0.044 ± 0.003, p < 0.0001) were associated with lower DM (Figure 4a to 4d).
Figure 4.
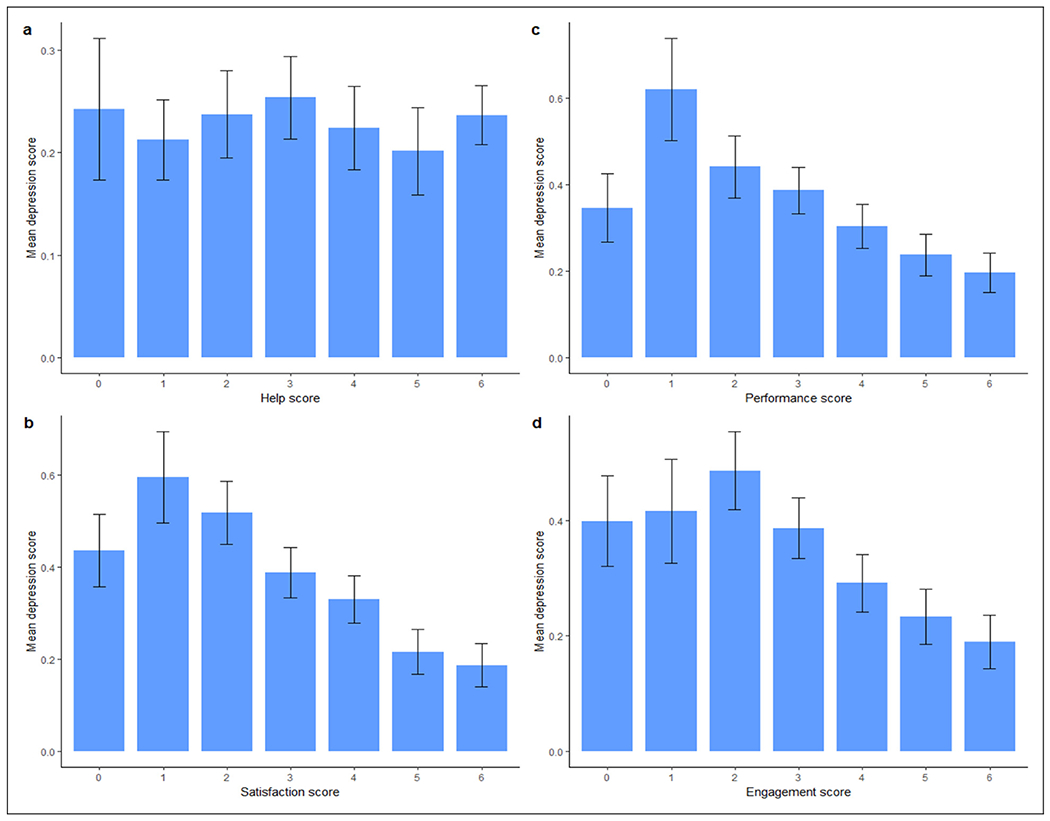
Average depression as a function of (a) help from someone while doing activities, (b) performance of activities, (c) satisfaction with doing activities, and (d) engagement of activities.
Time-lagged relationships between DM and daily functional behaviors
After controlling for DM at the previous time point, current DM was significantly lower when participants were in a store (β = −0.055 ± 0.024, p = 0.019) and socialized with people electronically (β = −0.196 ± 0.055, p = 0.0004) at the previous time point (Table 4). Current DM was lower when participants had higher ratings in perceived performance, satisfaction, engagement, and help at the earlier time point.
Table 4.
Multilevel models examining lagged relationships between depressed mood (DM) and daily functional behaviors.
| Models | Estimation | 95% CI | P-value | |
|---|---|---|---|---|
| TYPE OF ACTIVITY | ||||
| Fixed effect | ||||
| Intercept | 0.181 | 0.127 | 0.234 | <0.0001 |
| ADL | 0.001 | −0.026 | 0.027 | 0.952 |
| Cognitive Stimulating Activity | 0.003 | −0.023 | 0.030 | 0.798 |
| IADL | −0.011 | −0.033 | 0.012 | 0.357 |
| Physical Activity | −0.010 | −0.052 | 0.032 | 0.635 |
| Social Activity | 0.002 | −0.024 | 0.027 | 0.894 |
| Vocational Activity | 0.011 | −0.021 | 0.043 | 0.506 |
| Depression (previous time point) | 0.275** | 0.256 | 0.294 | <0.0001 |
| Random effect | ||||
| Intercept | 0.135 | 0.107 | 0.163 | <0.0001 |
| Residual | 0.137 | 0.133 | 0.141 | <0.0001 |
| LOCATION | ||||
| Fixed effect | ||||
| Intercept | 0.182 | 0.130 | 0.234 | <0.0001 |
| At community center | −0.003 | −0.085 | 0.080 | 0.952 |
| At outpatient medical visit | −0.035 | −0.114 | 0.044 | 0.386 |
| At restaurant | 0.027 | −0.032 | 0.087 | 0.370 |
| At the home of family member(s) | −0.006 | −0.045 | 0.034 | 0.784 |
| At the home of friend(s) | −0.003 | −0.065 | 0.059 | 0.928 |
| At work | −0.006 | −0.037 | 0.025 | 0.712 |
| In a vehicle | −0.020 | −0.060 | 0.020 | 0.317 |
| In class/school setting | −0.120 | −0.323 | 0.083 | 0.248 |
| In hospital | 0.111 | −0.008 | 0.230 | 0.068 |
| In public business/store (e.g. post office, grocery store) | −0.055* | −0.102 | −0.009 | 0.019 |
| Inside, other | 0.017 | −0.044 | 0.078 | 0.580 |
| Outside, other | 0.007 | −0.056 | 0.070 | 0.826 |
| Outside, walking | −0.024 | −0.130 | 0.082 | 0.654 |
| Depression (previous time point) | 0.274** | −0.130 | 0.082 | <0.0001 |
| Random effect | ||||
| Intercept | 0.135 | 0.107 | 0.163 | <0.0001 |
| Residual | 0.136 | 0.132 | 0.140 | <0.0001 |
| PERSON INTERACTING WITH | ||||
| Fixed effect | ||||
| Intercept | 0.177 | 0.122 | 0.233 | <0.0001 |
| Coworkers | 0.017 | −0.026 | 0.061 | 0.434 |
| Family members | 0.007 | −0.021 | 0.035 | 0.614 |
| Friends | 0.000 | −0.043 | 0.043 | 0.984 |
| Healthcare provider | −0.035 | −0.116 | 0.046 | 0.400 |
| Other known people | 0.003 | −0.073 | 0.079 | 0.943 |
| People you are socializing with electronically | −0.196* | −0.304 | −0.088 | 0.0004 |
| Pets | 0.041 | −0.003 | 0.085 | 0.068 |
| Spouse or partners | −0.004 | −0.037 | 0.028 | 0.793 |
| Unknown people | 0.047 | −0.039 | 0.133 | 0.281 |
| Depression (previous time point) | 0.282** | 0.260 | 0.304 | <0.0001 |
| Random effect | ||||
| Intercept | 0.139 | 0.109 | 0.169 | <0.0001 |
| Residual | 0.136 | 0.132 | 0.140 | <0.0001 |
| HELP FROM SOMEONE WHILE DOING ACTIVITIES | ||||
| Fixed effect | ||||
| Intercept | 0.182 | 0.118 | 0.245 | <0.0001 |
| Help score (between-person) | 0.002 | −0.028 | 0.031 | 0.918 |
| Help score (within-person) | −0.005* | −0.009 | 0.000 | 0.034 |
| Depression (previous time point) | 0.245** | 0.225 | 0.265 | <0.0001 |
| Random effect | ||||
| Intercept | 0.141 | 0.112 | 0.170 | <0.0001 |
| Residual | 0.126 | 0.122 | 0.129 | <0.0001 |
| PERFORMANCE OF ACTIVITIES | ||||
| Fixed effect | ||||
| Intercept | 0.565 | 0.364 | 0.765 | <.0001 |
| Performance score (between-person) | −0.074* | −0.112 | −0.037 | 0.0001 |
| Performance score (within-person) | −0.011* | −0.019 | −0.004 | 0.003 |
| Depression (previous time point) | 0.241** | 0.221 | 0.261 | <0.0001 |
| Random effect | ||||
| Intercept | 0.123 | 0.096 | 0.150 | <0.0001 |
| Residual | 0.126 | 0.122 | 0.129 | <0.0001 |
| SATISFACTION WITH DOING ACTIVITIES | ||||
| Fixed effect | ||||
| Intercept | 0.642 | 0.448 | 0.836 | <0.0001 |
| Satisfaction score (between-person) | −0.090** | −0.126 | −0.053 | <0.0001 |
| Satisfaction score (within-person) | −0.012* | −0.019 | −0.004 | 0.002 |
| Depression (previous time point) | 0.240** | 0.219 | 0.260 | <0.0001 |
| Random effect | ||||
| Intercept | 0.117 | 0.091 | 0.142 | <0.0001 |
| Residual | 0.126 | 0.122 | 0.129 | <0.0001 |
| ENGAGEMENT of ACTIVITIES | ||||
| Fixed effect | ||||
| Intercept | 0.582 | 0.397 | 0.766 | <0.0001 |
| Engagement score (between-person) | −0.079** | −0.114 | −0.044 | <0.0001 |
| Engagement score (within-person) | −0.013* | −0.020 | −0.006 | 0.0004 |
| Depression (previous time point) | 0.239** | 0.219 | 0.260 | <0.0001 |
| Random effect | ||||
| Intercept | 0.121 | 0.094 | 0.147 | <0.0001 |
| Residual | 0.126 | 0.122 | 0.129 | <0.0001 |
p-value < 0.0001,
p-value < 0.05.
ADL: activities of daily living; IADL: instrumental activities of daily living.
Discussion
This study investigated the relationships of DM with daily functional behaviors among individuals with chronic stroke. Examining temporal associations between functional behaviors and DM using mobile health (mHealth) technology is a novel approach to understand mental health problems in stroke survivors. Our findings provide a framework for understanding DM in daily contexts after stroke, which enables progress toward developing effective treatments for DM and functional disability. We found that DM in daily life differed by activity type. Participants had the highest level of DM when engaged in passive leisure activities. Mentally passive sedentary behaviors, such as watching television, may contribute to an increased risk of depression.18 Yet, time-lagged analyses revealed that participation in passive leisure activities did not predict significantly higher DM at a later time when compared to other activities. This result suggests that passive leisure activities are a response to DM, rather than a contributor to DM.
We found that, compared with being alone, participants experienced lower concurrent DM while socializing with others, including their partner, family members, friends, and other known people. These significant associations between spending time with others and DM provide preliminary evidence to support clinical interventions promoting social activity for alleviating DM poststroke. An earlier EMA study supports this notion; increased perceived satisfaction, confidence, and success of social interactions were momentarily associated with reduced DM among mild stroke survivors.19 Similarly, we found that participants reporting lower DM were more likely to be in common locations for social gatherings, like restaurants, and homes of family members and friends. Interventions promoting in-person social interactions in poststroke life may warrant further investigation. Conversely, participants who socialized with people electronically experienced higher DM at the same survey but lower DM at the next survey. We cannot determine the reasons for this opposing relationship but a previous study of non-stroke populations found that participants engaging in online social media over more prolonged periods were at an increased risk of depression and other mental health problems.20
Participating in IADLs was associated with lower DM, supporting previously published results that depression was associated with dependence on IADLs among stroke survivors.21 IADLs are complex activities needed to continue living in the community.22 It is possible that dependence on IADLs may induce feelings of helplessness, reduce self-esteem, and ultimately lead to depression.
Our results showed that reduced DM was associated with increased ratings in perceived satisfaction, performance, and engagement with daily functional behaviors among stroke survivors in both concurrent and lagged models. These results align with the behavioral activation (BA) approach.23 According to BA, behaviors and feelings influence each other. When people are depressed, they become less active. Likewise, when people do not engage in valued activities, they experience more depressed feelings. Our findings support that future intervention should focus on purposefully scheduling activities that stroke survivors perceive as satisfying, thereby reducing their DM. Interestingly, increased help needed for an activity predicted a decrease in DM at the next time point. The unexpected direction of this result warrants further investigation.
Prior literature has shown promising support for the application of telemedicine and mHealth technology in stroke care and management.24–26 This study adds to the literature by employing smartphone-based EMA to characterize the real-time relationships between DM and functional behaviors after stroke. To date, we use EMA as a research tool; however, it has potential clinical utility for monitoring poststroke functioning. Our findings support future interventions targeting structured social or community activities that evoke satisfaction from stroke survivors to reduce their DM.
Strengths and weakness
The use of real-time data in natural contexts, and the large and diverse sample are strengths of this study. However, there are several limitations. Most participants were community-dwelling and neurologically mild, which may not represent the general stroke population. Acute or severely impaired stroke survivors may show poorer functioning. Our sample was not diagnosed with poststroke depression but experienced a range of DM. Further research may include only patients diagnosed with mood disorders due to stroke as they may experience different daily life patterns. Sampling five surveys each day may miss activity episodes between consecutive surveys. Future research may consider using mobile sensing technologies to characterize daily functioning. Most current sensing research in stroke focuses on daily activity monitoring at home;27 future studies integrating EMA with global positioning systems and accelerometers might expand this work to characterize activities in community settings. Assessing real-time associations between functional behaviors and mental health lays the groundwork for developing potential real-time interventions for improving DM and everyday functioning.
Conclusion
This study supports the use of smartphone assessment to examine DM and functional outcomes in real time among individuals after stroke. Our findings demonstrate the complexity of DM in daily life after stroke. Daily, repeated, and self-reported DM measured by smartphones may be clinically beneficial in detecting changes across day-to-day contexts. Future steps may integrate EMA with sensing technologies and behavioral strategies to deliver ecological momentary interventions to improve mental well-being and functional independence.28
Acknowledgements
The contents do not necessarily represent the policy of the funding agencies. We certify that all financial and material support for this research and work are clearly identified in the manuscript. We thank all personnel at Washington University for their assistance in recruitment and data collection.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the American Occupational Therapy Foundation, Center for Smart Use of Technologies to Assess Real-world Outcomes (C-STAR), National Center for Medical Rehabilitation Research (grant numbers AOTFIRG20 Wong, P2CHD101899, and K01HD095388).
Declaration of conflicting interests
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Dr Lenze reported research support from the National Institutes of Health (NIH), Patient-Centered Outcomes Research Institute, and Mercatus Center Emergent Ventures outside the submitted work. He also received grant support (loaned equipment for research) from MagStim. He has served as a consultant for Prodeo, Janssen Pharmaceuticals, and Boehringer Ingelheim. Dr Lee reported research support from the NIH, Barnes-Jewish Foundation, Biogen and consulting fees from Regenera outside the submitted work. Dr Mohr reported research support from the NIH, personal fees from Apple and other support from Actualize Therapy and Otsuka Pharmaceuticals. Dr Mohr has an ownership interest in Adaptive Health and had a patent to US Patent 15/654,245, 2018 pending. Dr Metts has an ownership interest in Infinite Arms. Dr Wong reported research support from the NIH, National Institute on Disability, Independence, and Rehabilitation Research, American Occupational Therapy Foundation, and Craig H. Neilsen Foundation. No other disclosures were reported.
Footnotes
Ethics approval
The study was approved by an Institutional Review Board (IRB) at the study sites. Informed consent was obtained from all individual participants included in the study.
Data availability
Data are available upon reasonable request. The data used as part of this study that support the reported findings are available from the corresponding author upon reasonable request.
References
- 1.Katan M and Luft A. Global burden of stroke. Semin Neurol 2018; 38: 208–211. [DOI] [PubMed] [Google Scholar]
- 2.Paolucci S, Iosa M, Coiro P, et al. Post-stroke depression increases disability more than 15% in ischemic stroke survivors: a case-control study. Front Neurol 2019; 10: 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kapoor A, Lanctôt KL, Bayley M, et al. “Good outcome” isn’t good enough: cognitive impairment, depressive symptoms, and social restrictions in physically recovered stroke patients. Stroke 2017; 48: 1688–1690. [DOI] [PubMed] [Google Scholar]
- 4.Sarkar A, Sarmah D, Datta A, et al. Post-stroke depression: chaos to exposition. Brain Res Bull 2021; 168: 74–88. [DOI] [PubMed] [Google Scholar]
- 5.Sagen U, Vik TG, Moum T, et al. Screening for anxiety and depression after stroke: comparison of the hospital anxiety and depression scale and the Montgomery and Åsberg depression rating scale. J Psychosom Res 2009; 67: 325–332. [DOI] [PubMed] [Google Scholar]
- 6.Mikami K, Sudo T, Orihashi Y, et al. Effective tools to predict depression in acute and subacute phase of ischemic stroke. J Neuropsychiatry Clin Neurosci 2021; 33: 43–48. [DOI] [PubMed] [Google Scholar]
- 7.Moskowitz DS and Young SN. Ecological momentary assessment: what it is and why it is a method of the future in clinical psychopharmacology. J Psychiatry Neurosci 2006; 31: 13–20. [PMC free article] [PubMed] [Google Scholar]
- 8.Shiffman S, Stone AA and Hufford MR Ecological momentary assessment. Annu Rev Clin Psychol 2008; 4: 1–32. [DOI] [PubMed] [Google Scholar]
- 9.Sibon I, Lassalle-Lagadec S, Renou P, et al. Evolution of depression symptoms following stroke: a prospective study using computerized ambulatory monitoring. Cerebrovasc Dis 2012; 33: 280–285. [DOI] [PubMed] [Google Scholar]
- 10.Jean FA, Swendsen JD, Sibon I, et al. Daily life behaviors and depression risk following stroke: a preliminary study using ecological momentary assessment. J Geriatr Psychiatry Neurol 2013; 26: 138–143. [DOI] [PubMed] [Google Scholar]
- 11.Brott T, Adams HP Jr., Olinger CP, et al. Measurements of acute cerebral infarction: a clinical examination scale. Stroke 1989; 20: 864–870. [DOI] [PubMed] [Google Scholar]
- 12.Bruno A, Shah N, Lin C, et al. Improving modified Rankin Scale assessment with a simplified questionnaire. Stroke 2010; 41: 1048–1050. [DOI] [PubMed] [Google Scholar]
- 13.Moore RC, Kaufmann CN, Rooney AS, et al. Feasibility and acceptability of ecological momentary assessment of daily functioning among older adults with HIV. Am J Geriatr Psychiatry 2017; 25: 829–840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Campbell LM, Paolillo EW, Heaton A, et al. Daily activities related to mobile cognitive performance in middle-aged and older adults: an ecological momentary cognitive assessment study. JMIR Mhealth Uhealth 2020; 8: e19579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Granholm E, Holden JL, Mikhael T, et al. What do people with schizophrenia do all day? Ecological momentary assessment of real-world functioning in schizophrenia. Schizophr Bull 2020; 46: 242–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Enders CK and Tofighi D. Centering predictor variables in cross-sectional multilevel models: a new look at an old issue. Psychol Methods 2007; 12: 121–138. [DOI] [PubMed] [Google Scholar]
- 17.Suryawanshi M. Mixed Model Repeated Measures (MMRM). In: SAS Conference Proceedings: Pharmaceutical Users Software Exchange (PHUSE) US 2019. Amsterdam, The Netherlands, 10–13 November 2019. https://www.lexjansen.com/phuse/2019/as/AS06.pdf [Google Scholar]
- 18.Huang Y, Li L, Gan Y, et al. Sedentary behaviors and risk of depression: a meta-analysis of prospective studies. Transl Psychiatry 2020; 10: 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Neff AJ, Lee Y, Metts CL, et al. Ecological momentary assessment of social interactions: associations with depression, anxiety, pain, and fatigue in individuals with mild stroke. Arch Phys Med Rehabil 2021; 102: 395–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Keles B, McCrae N and Grealish A. A systematic review: the influence of social media on depression, anxiety and psychological distress in adolescents. Int J Adolesc Youth 2020; 25: 79–93. [Google Scholar]
- 21.Blomgren C, Samuelsson H, Blomstrand C, et al. Long-term performance of instrumental activities of daily living in young and middle-aged stroke survivors-impact of cognitive dysfunction, emotional problems and fatigue. PLoS One 2019; 14: e0216822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Carod-Artal FJ, González-Gutiérrez JL, Herrero JA, et al. Functional recovery and instrumental activities of daily living: follow-up 1-year after treatment in a stroke unit. Brain Inj 2002; 16: 207–216. [DOI] [PubMed] [Google Scholar]
- 23.Kanter JW, Manos RC, Bowe WM, et al. What is behavioral activation? A review of the empirical literature. Clin Psychol Rev 2010; 30: 608–620. [DOI] [PubMed] [Google Scholar]
- 24.English SW, Barrett KM, Freeman WD, et al. Telemedicine-enabled ambulances and mobile stroke units for prehospital stroke management. J Telemed Telecare 2021: 1357633 × 211047744. DOI: 10.1177/1357633x211047744. [DOI] [PubMed] [Google Scholar]
- 25.Kim DK, Yoo SK, Park IC, et al. A mobile telemedicine system for remote consultation in cases of acute stroke. J Telemed Telecare 2009; 15: 102–107. [DOI] [PubMed] [Google Scholar]
- 26.Salazar AJ, Useche N, Granja M, et al. Reliability and accuracy of individual alberta stroke program early CT score regions using a medical and a smartphone reading system in a telestroke network. J Telemed Telecare 2021; 27: 436–443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chen PW, Baune NA, Zwir I, et al. Measuring activities of daily living in stroke patients with motion machine learning algorithms: a pilot study. Int J Environ Res Public Health 2021; 18 20210209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Demers M and Winstein CJ. A perspective on the use of ecological momentary assessment and intervention to promote stroke recovery and rehabilitation. Top Stroke Rehabil 2021; 28: 594–605. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available upon reasonable request. The data used as part of this study that support the reported findings are available from the corresponding author upon reasonable request.


