Abstract
Background/aims:
To report the incidence and clinical characteristics of pediatric keratitis diagnosed over a 10-year period in a well-defined population. Design: Retrospective, population-based study
Methods:
Setting: Multicenter. Population: Patients (<19 years) diagnosed with keratitis as residents of Olmsted County from January 1, 2000, through December 31, 2009. Main Outcome Measures: Calculated annual age- and gender-specific incidence rates, demographic information, and initial and final visual acuity.
Results:
A total of 294 diagnoses of keratitis occurred in 285 children during the 10-year period, yielding an incidence of 78.0 per 100,000 younger than 19 years (95% CI 69.0–87.1), or approximately 1 in 1282 children. The incidence increased throughout the 10-year study period (p<0.001). The mean age at diagnosis was 15.3 years (range, 0.2–18.9) and 172 (60.4%) were female. The observed forms included keratitis due to contact lens wear in 134 (45.6%), infectious keratitis in 72 (24.5%), keratitis not otherwise specified in 65 (22.1%) and keratitis sicca in 23 (7.8%). The visual acuity was reduced to ≤ 20/40 in 61 (21.4) of the 285 patients at the initial examination and in 24 (8.4%) at the final examination. Children with infectious keratitis had the poorest presenting vision and the best final vision, whereas the reverse was true for those with keratitis sicca.
Conclusions:
Keratitis, regardless of etiology, was observed in approximately 1 in 1300 children by 19 years of age in this population-based cohort. Nearly half were related to contact lens wear and a decrease of vision to ≤ 20/40 occurred in 1 in 12 patients.
Keratitis is an infectious or inflammatory condition of the cornea, generally characterized by corneal edema, inflammation, and ciliary congestion.1 Recent studies have demonstrated that keratitis is more common in adults than children, with the latter comprising from 3 to 13% of cases.2–4 Because children may poorly communicate their symptoms and lack cooperation during physical examination, they may be diagnosed later in the course of their disease and present more severely.5, 6 The etiology of keratitis in children is varied and geography-dependent; most commonly associated with trauma in developing countries and contact lens wear in developed countries.7
Although a number of studies have reported on the clinical characteristics, incidence, and management of pediatric microbial keratitis,4, 8–11 there are no known population-based reports regarding pediatric keratitis. The purpose of this study is to report the incidence and clinical characteristics of keratitis diagnosed during a 10-year period among residents of Olmsted County, Minnesota who were younger than 19 years of age.
Methods
The medical records of all patients < 19 years of age who were diagnosed with any form of keratitis while residing in Olmsted County, Minnesota from January 1, 2000, through December 31, 2009, were reviewed retrospectively. Potential cases were identified using the resources of the Rochester Epidemiology Project (REP), a medical records linkage system designed to capture data on any patient-physician encounter in Olmsted County, Minnesota.12 The population of this county is relatively isolated from other urban areas and virtually all medical care is provided to its residents by Mayo Clinic, Olmsted Medical Group, and their affiliated hospitals. Patients not residing in Olmsted County at the time of their diagnosis were excluded from the study. Institutional Review Board approval was obtained for this study.
Potential cases of keratitis were ascertained by searching the REP linkage system for International Classification of Diseases 9th edition (ICD-9) codes for disorders of the globe, keratitis, cornea opacity, other disorders of the cornea, disorders of the conjunctiva, and other disorders of the eye (ICD-9 codes 360, 370, 371, 372 and 379, respectively). Patients were included if the examining physician made a diagnosis of infectious keratitis, contact lens-associated keratitis, keratitis not otherwise specified, or keratitis sicca. Contact lens-associated keratitis included any patient diagnosed with keratitis related to contact-lens wear. Infectious keratitis included any patient clinically diagnosed with infectious keratitis not related to contact lens wear. Keratitis not otherwise specified included those diagnosed with keratoconjunctivitis, allergic keratitis, keratitis secondary to blepharitis, or any other unspecified form of keratitis. If a patient was diagnosed with more than one type of keratitis, each diagnosis was recorded and included. Patients were excluded if they were diagnosed outside the time period of the study, resided outside of Olmsted County, or refused research authorization. Residency and age verification was ascertained using REP-provided information at the time of record review. The entire ophthalmic record of each case was individually reviewed by the authors to confirm the clinical diagnosis. Demographic data and visual acuity at diagnosis and final examination were also recorded.
Testing for gender predilection were completed with a simple one-sample test of proportions. The percentage was tested to determine if it was significantly different than 0.5. The overall incidence of keratitis was estimated using age- and sex-specific population figures from Olmsted County. Yearly incidence rates for each sex group were calculated by dividing the number of cases within that group by the estimated total Olmsted County resident population of that group for the given year. Population figures for 2000 and 2010 were derived from U.S. census data, and population figures for inter-census years were estimated by linear interpolation. These incidence rates were age- and/or sex-adjusted to the 2010 census figures for the U.S. white population. Overall trends in incidence were investigated using Poisson regression models.
Results
A total of 294 diagnoses with any form of keratitis occurred among 285 patients during the 10-year period, yielding an overall age and sex adjusted incidence of 78.0 per 100,000 (95% CI 69.0–87.1), or 1 in 1292 for patients aged < 19 years. The historical and clinical characteristics of the 4 principal forms are shown in the Table, and include keratitis due to contact lens wear in 134 (45.6%), infectious keratitis in 72 (24.5%), keratitis not otherwise specified in 65 (22.1%), and keratitis sicca in 23 (7.8%). Using Poisson regression models, incidence of keratitis was found to have significantly increased over the 10-year period (p<0.001) as shown in the Figure, including the subtypes of keratitis due to contact lens wear (p<0.001), infectious keratitis (p<0.001), and keratitis not otherwise specified (p=0.02). There were too few cases of keratitis sicca to assess incidence over time.
Table.
Historical and Clinical Characteristics of 285 patients < 19 years diagnosed with keratitis in Olmsted County, MN, from 2000 to 2009
| Characteristics | Contact-lens associated keratitis | Infectious keratitis | Keratitis not otherwise specified | Keratitis sicca | Total |
|---|---|---|---|---|---|
| N | 134 | 72 | 65 | 23 | 285 |
| Age and sex adjusted Incidence per 100,000 | 36.7 | 19.7 | 17.8 | 6.3 | 78.0 |
| Females: Males | 85:49 | 37:35 | 41:24 | 17:6 | 172:113 |
| Mean age at diagnosis in years (range) | 16.5 (11.0–18.9) | 15.6 (0.2–18.9) | 13.2 (1.5–18.8) | 13.1 (0.4–18.9) | 15.3 (0.2–18.9) |
| Laterality (% unilateral: bilateral) | 56:44 | 92:8 | 52:48 | 30:70 | 62:38 |
| Ocular comorbidity | 1a | 7b | 5c | 5d | 18 |
| Medical comorbidity | 5e | 5f | 7g | 5h | 21 |
| Initial VA ≤ 20/40 in affected eye(s) | 27 (20.1%) | 19 (26.4%) | 16 (24.6%) | 2 (8.7%) | 61 (21.4%) |
| Final VA ≤ 20/40 in affected eye(s) | 9 (6.7%) | 5 (6.9%) | 8 (12.3%) | 5 (21.7%) | 24 (8.4%) |
Strabismus
Strabismus (2), trauma (1), disorders of the adnexa and orbit (3), and uveitis (1).
Amblyopia (1), strabismus (2), nystagmus (1), and disorders of the adnexa and orbit (1).
Amblyopia (2), strabismus (3), nystagmus (1), disorders of the adnexa and orbit (3), and retina and vitreous (2).
Metabolic (1), neurologic (4), and endocrine (1).
Genetic (1), metabolic (1), musculoskeletal (1), urogenital (1), and infectious (1)
Genetic (3), neurocognitive (2), cardiac (1), neurologic (2), and oncologic (1).
Neurocognitive (2), neurologic (2), oncologic (1), and gastrointestinal (1).
Figure.
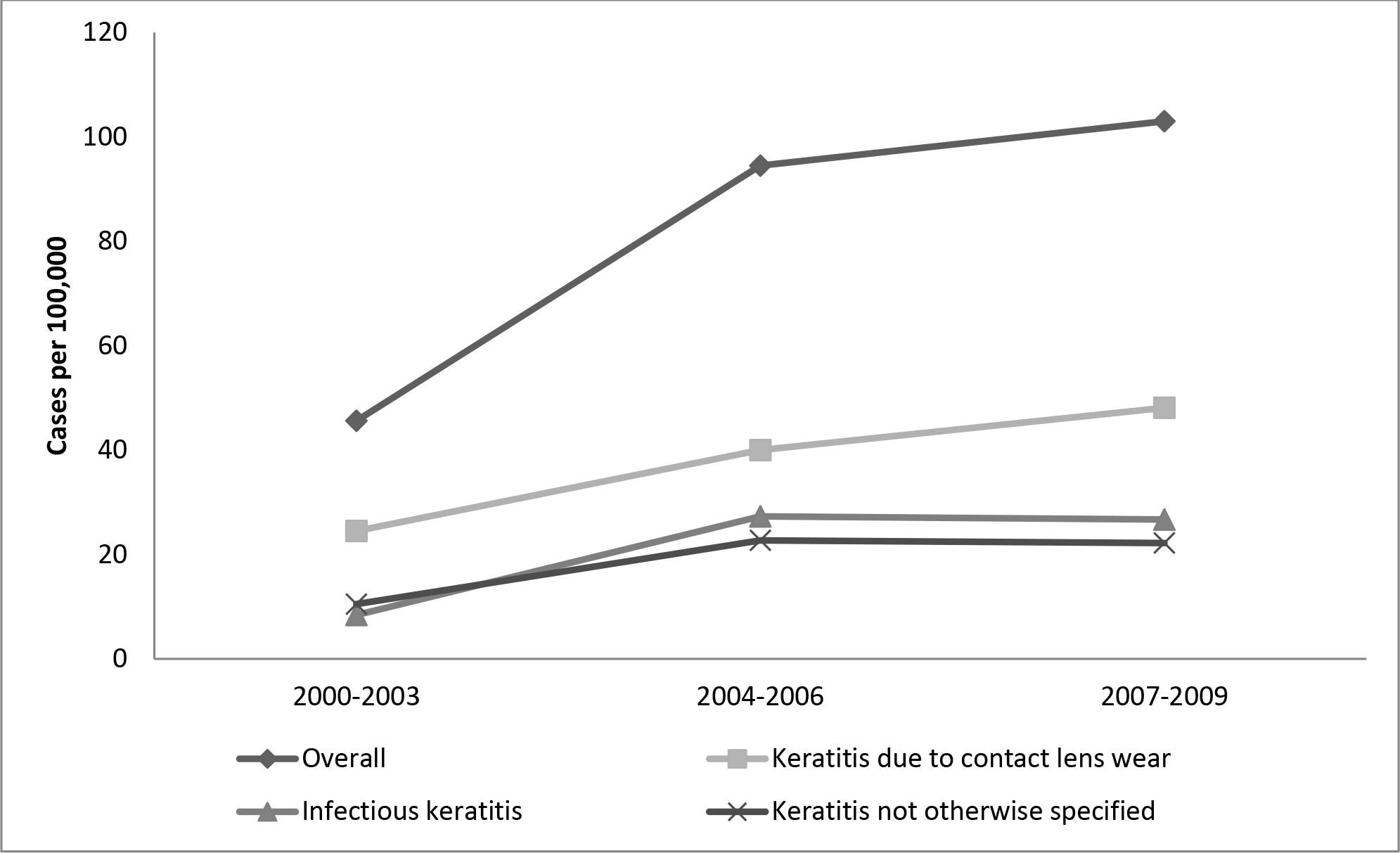
Incidence of keratitis due to contact lens wear, infectious keratitis, and keratitis not otherwise specified from 2000 through 2009 in Olmsted County, Minnesota. All trends statistically significant using Poisson regression models (p<0.05).
The mean age at diagnosis for the 285 patients was 15.3 years (range, 0.2–18.9) and 172 (60.4%) were female. Infectious keratitis showed no gender predilection (p=0.81), while keratitis due to contact lens wear (p=0.002), keratitis not otherwise specified (p=0.04), and keratitis sicca (p=0.02) were significantly more likely to occur in females. Infectious keratitis (91.8%) and keratitis due to contact lens wear (56%) were more likely to occur unilaterally, while keratitis sicca (69.6%) was more likely to occur bilaterally. Eighteen patients (6.3%) had ocular comorbidities, including strabismus in 8 (2.8%) and disorders of the adnexa and orbit in 7 (2.5%), and 21 (7.4%) had medical conditions including neurologic conditions in 8 (2.8%) and genetic conditions in 4 (1.4%). The visual acuity was reduced to ≤ 20/40 in 61 (21.4%) of the 285 patients at the initial examination and in 24 (8.4%) at the final examination. Children with infectious keratitis tended to have the worst presenting vision and the best final vision, whereas those with keratitis sicca had the best presenting vision and the worst final vision.
Discussion
In this population-based cohort diagnosed over a 10-year period, keratitis occurred in 1 in 1292 children before 19 years of age, with a significantly increasing incidence over the 10-year period. Females were more commonly affected than males and nearly half were related to contact lens wear. Approximately 1 in 12 experienced vision loss to ≤ 20/40 by their final examination.
There are no known population-based studies of pediatric keratitis with which to compare this study. Prior reports of childhood keratitis are primarily tertiary care, single-institution cohorts describing clinical features and risk factors, and many only include children with infectious forms of keratitis or keratitis sicca.4, 8–11, 13–15 There was a significant increase in the incidence of keratitis over the duration of this 10-year study. Other reports have similarly shown an increase in incidence of keratitis over time, which is thought to be due to the increased use of contact lenses among adolescent children.15 This observation may also be due to the increased use of cosmetic contact lenses in this population. While numbers for the types of contact lenses worn were not included in this study, the vast majority of contact lens use was either daily or extended wear. In this study, there was an increase over time for all types of keratitis, except for keratitis sicca which had too few cases to assess incidence over time.
Keratitis associated with the use of contact lenses in children was the most prevalent etiology in this cohort. Contact lens wear is consistently reported as the most common risk factor for pediatric keratitis in developed countries, whereas trauma is the most common risk factor in developing countries.7 Risk factors for keratitis in pediatric contact lens wearers include storage in water and poor cleaning compliance.3 The average age of keratitis due to contact lens wear in this study was 16.5 years. Previous reports of microbial keratitis in children have shown a bimodal distribution of ages: preschoolers between 1 and 3 years of age and adolescent contact lens wearers.4, 5 Contact lens-associated keratitis occurred bilaterally in 44% of cases. Prior studies of pediatric microbial keratitis have reported lower rates of bilateral disease 2,3. However, relatively higher rates of bilateral keratitis have been reported in studies with higher proportions of contact lens wearers.3 This higher rate in contact lens wearers may be due to poor hygiene practices, including prolonged length of contact lens wear and poor cleaning and storage, leading to contamination or irritation bilaterally.
Infectious keratitis was the second most prevalent etiology of keratitis in this cohort. Green et al. reported the incidence of pediatric microbial keratitis as 0.11 cases per 10,000 patients 16 years or younger, a rate that is much lower than the 19.7 cases per 100,000 < 19 years observed in the current study.4 However, Green et al., who included patients up to 16 years, identified cases of microbial keratitis by positive corneal scrapings from pathology organizations identified through online and local directory searches. They likely underestimated the true incidence due to cases that were not cultured or culture-negative.4 Herpes keratitis is a common cause of keratitis in children. While specific numbers of herpes keratitis cases were not included in this study, it likely accounted for a number of those in the infectious keratitis category. The average age of patients with infectious keratitis in our study was 15.6 years, higher than prior reports, in which average ages ranged from 8.9 to 13.0 years.3, 4, 8, 9, 13 However, many of these studies included only patients under the age of 16 years. Moreover, 1 in 10 children with microbial keratitis in this cohort had an underlying ocular condition and 6.9% had an underlying medical condition. Other studies have shown that underlying ocular surface and systemic diseases, like Stevens-Johnson syndrome, are important predisposing factors for microbial keratitis.11, 14
Keratitis not otherwise specified, which included allergic keratitis, keratoconjunctivitis, and keratitis secondary to blepharitis, occurred in 22.1% of this cohort, yielding an incidence of 17.2 per 100,000 children < 19 years of age. Previous studies have shown that blepharokeratoconjunctivitis, which falls into this category, is responsible for 15–25% of pediatric corneal referrals.16, 17 Prior reports have also shown that blepharokeratoconjunctivitis is most common in Asian and Middle Eastern children.17 In our study, 72% of the children in the “keratitis not otherwise specified” category were white, and only 6% were Asian. This finding may be partially explained by the relatively homogeneous, white population of Olmsted County, Minnesota. Previous reports of pediatric blepharokeratoconjunctivitis have also found a sex predilection with girls diagnosed in 55–80% of cases.17, 18 In this study, 63% of the children in the keratitis not otherwise specified category were girls. Atopic disease is most common in children and adolescents, and people with asthma, eczema, and rhinitis often experience concurrent ocular allergic diseases like allergic keratitis.19 In our study, 7 of the 65 patients with keratitis not otherwise specified were diagnosed with medical comorbidities.
Keratitis sicca, the least prevalent form of keratitis in this cohort, occurred in only 6.3 per 100,000 children < 19 years of age, similar to the 0.01% of children 2–17 years of age reported by Dana et al,20 but significantly lower than the 2688 per 1 million Indian children reported by Donthineni et al.21 The difference in incidence may be due to environmental and lifestyle differences between the United States and India. In children, keratitis sicca has been associated with congenital, autoimmune, endocrine, and inflammatory disorders and certain environmental and nutritional conditions.22 In this study, 1 in 5 patients with keratitis sicca were also diagnosed with systemic conditions. Other studies have shown that smartphone use in children is associated with pediatric dry eye disease, especially in older-grade school students.23 This may partially explain the average age that was observed in this study.
There are a number of limitations to the findings of this study. Its retrospective design is limited by incomplete data and variable follow-up. Moreover, although the vast majority of patients in Olmsted County are managed by the medical systems within the community, some residents may have sought care outside of the county, thereby underestimating the true incidence in this population. Children with mild or asymptomatic disease may have avoided detection altogether, thereby further underestimating incidence in this population. Also, the study did not sub-classify the etiology of contact lens-associated keratitis into infectious or sterile forms. If a patient had contact lens-associated keratitis due to an infectious etiology, their diagnosis would have been classified as contact lens associated keratitis. This may have resulted in an underrepresentation of the incidence of infectious keratitis. Additionally, due to the retrospective nature of the study and the varying institutions involved, precise documentation of clinical disorders was sometimes inconsistent or incomplete. We were, for example, unable to determine accurate numbers of the individual forms that comprised keratitis NOS or infectious keratitis, including herpes keratitis or staphylococcal lid disease. Finally, the ability to generalize these findings to other populations is limited by the demographics of Olmsted County, a relatively homogeneous, suburban, white population with a higher median family income than the US median.
The findings of this study provide a population-based incidence rate for pediatric keratitis diagnosed over a 10-year period. The observed increasing incidence of pediatric keratitis over this time span may, in part, be due to the increasing use of contact lenses in children. Females were more commonly affected than males and the final visual acuity was reduced to ≤ 20/40 in 1 in 12 children.
Key messages.
What is already known on this topic
There are no known population-based reports regarding the incidence of pediatric keratitis.
What this study adds
This study reports the population-based incidence and clinical characteristics of pediatric keratitis diagnosed over a 10-year period in a well-defined population.
How this study might affect research, practice or policy
The results of this study will help clinicians identify children with clinical characteristics associated with keratitis. It may also help guide recommendations for contact lens usage in children.
Synopsis/ Precis:
Keratitis was observed in approximately 1 in 1300 children < 19 years of age in this population-based cohort. Nearly half were related to contact lens wear.
Funding Statement:
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Footnotes
Competing Interests: There are no competing interests for any author.
References
- 1.Singh P, Gupta A, Tripathy K. Keratitis. Treasure Island (FL): StatPearls Publishing, 2020. [Google Scholar]
- 2.Hsiao CH, Yeung L, Ma DH, et al. Pediatric microbial keratitis in Taiwanese children: a review of hospital cases. Arch Ophthalmol 2007;125(5):603–9. [DOI] [PubMed] [Google Scholar]
- 3.Hepschke JL, Ung L, Cabrera-Aguas M, et al. Pediatric Microbial Keratitis: Experience From Tertiary Referral Centers in New South Wales, Australia. Pediatr Infect Dis J 2020;39(10):883–8. [DOI] [PubMed] [Google Scholar]
- 4.Green M, Apel A, Stapleton F. Pediatric Microbial Keratitis in Queensland, Australia (2005 to 2015). Cornea 2019;38(12):1519–23. [DOI] [PubMed] [Google Scholar]
- 5.Zaidman GW. The pediatric corneal infiltrate. Curr Opin Ophthalmol 2011;22(4):261–6. [DOI] [PubMed] [Google Scholar]
- 6.Al-Otaibi AG. Non-viral microbial keratitis in children. Saudi J Ophthalmol 2012;26(2):191–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Di Zazzo A, Antonini M, Fernandes M, et al. A global perspective of pediatric non-viral keratitis: literature review. Int Ophthalmol 2020;40(10):2771–88. [DOI] [PubMed] [Google Scholar]
- 8.Young AL, Leung KS, Tsim N, et al. Risk factors, microbiological profile, and treatment outcomes of pediatric microbial keratitis in a tertiary care hospital in Hong Kong. Am J Ophthalmol 2013;156(5):1040–4.e2. [DOI] [PubMed] [Google Scholar]
- 9.Song X, Xu L, Sun S, et al. Pediatric microbial keratitis: a tertiary hospital study. Eur J Ophthalmol 2012;22(2):136–41. [DOI] [PubMed] [Google Scholar]
- 10.Soleimani M, Tabatabaei SA, Mohammadi SS, et al. A ten-year report of microbial keratitis in pediatric population under five years in a tertiary eye center. J Ophthalmic Inflamm Infect 2020;10(1):35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kunimoto DY, Sharma S, Reddy MK, et al. Microbial keratitis in children. Ophthalmology 1998;105(2):252–7. [DOI] [PubMed] [Google Scholar]
- 12.Melton LJ. History of the Rochester Epidemiology Project. Mayo Clin Proc 1996;71(3):266–74. [DOI] [PubMed] [Google Scholar]
- 13.Rossetto JD, Cavuoto KM, Osigian CJ, et al. Paediatric infectious keratitis: a case series of 107 children presenting to a tertiary referral centre. Br J Ophthalmol 2017;101(11):1488–92. [DOI] [PubMed] [Google Scholar]
- 14.Noureddin GS, Sasaki S, Butler AL, et al. Paediatric infectious keratitis at tertiary referral centres in Vancouver, Canada. Br J Ophthalmol 2016;100(12):1714–8. [DOI] [PubMed] [Google Scholar]
- 15.Lee YS, Tan HY, Yeh LK, et al. Pediatric microbial keratitis in Taiwan: clinical and microbiological profiles, 1998–2002 versus 2008–2012. Am J Ophthalmol 2014;157(5):1090–6. [DOI] [PubMed] [Google Scholar]
- 16.Hammersmith KM, Cohen EJ, Blake TD, et al. Blepharokeratoconjunctivitis in children. Arch Ophthalmol 2005;123(12):1667–70. [DOI] [PubMed] [Google Scholar]
- 17.Hammersmith KM. Blepharokeratoconjunctivitis in children. Curr Opin Ophthalmol 2015;26(4):301–5. [DOI] [PubMed] [Google Scholar]
- 18.Viswalingam M, Rauz S, Morlet N, Dart JK. Blepharokeratoconjunctivitis in children: diagnosis and treatment. Br J Ophthalmol 2005;89(4):400–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Patel DS, Arunakirinathan M, Stuart A, Angunawela R. Allergic eye disease. BMJ 2017;359:j4706. [DOI] [PubMed] [Google Scholar]
- 20.Dana R, Bradley JL, Guerin A, et al. Estimated Prevalence and Incidence of Dry Eye Disease Based on Coding Analysis of a Large, All-age United States Health Care System. Am J Ophthalmol 2019;202:47–54. [DOI] [PubMed] [Google Scholar]
- 21.Donthineni PR, Kammari P, Shanbhag SS, et al. Incidence, demographics, types and risk factors of dry eye disease in India: Electronic medical records driven big data analytics report I. Ocul Surf 2019;17(2):250–6. [DOI] [PubMed] [Google Scholar]
- 22.Alves M, Dias AC, Rocha EM. Dry eye in childhood: epidemiological and clinical aspects. Ocul Surf 2008;6(1):44–51. [DOI] [PubMed] [Google Scholar]
- 23.Moon JH, Kim KW, Moon NJ. Smartphone use is a risk factor for pediatric dry eye disease according to region and age: a case control study. BMC Ophthalmol 2016;16(1):188. [DOI] [PMC free article] [PubMed] [Google Scholar]


