Abstract
Anthrax toxin from Bacillus anthracis is a three-component toxin consisting of lethal factor (LF), edema factor (EF), and protective antigen (PA). LF and EF are the catalytic components of the toxin, whereas PA is the receptor-binding component. To identify residues of PA that are involved in interaction with the cellular receptor, two solvent-exposed loops of domain 4 of PA (amino acids [aa] 679 to 693 and 704 to 723) were mutagenized, and the altered proteins purified and tested for toxicity in the presence of LF. In addition to the intended substitutions, novel mutations were introduced by errors that occurred during PCR. Substitutions within the large loop (aa 704 to 723) had no effect on PA activity. A mutated protein, LST-35, with three substitutions in the small loop (aa 679 to 693), bound weakly to the receptor and was nontoxic. A mutated protein, LST-8, with changes in three separate regions did not bind to receptor and was nontoxic. Toxicity was greatly decreased by truncation of the C-terminal 3 to 5 aa, but not by their substitution with nonnative residues or the extension of the terminus with nonnative sequences. Comparison of the 28 mutant proteins described here showed that the large loop (aa 704 to 722) is not involved in receptor binding, whereas residues in and near the small loop (aa 679 to 693) play an important role in receptor interaction. Other regions of domain 4, in particular residues at the extreme C terminus, appear to play a role in stabilizing a conformation needed for receptor-binding activity.
Anthrax toxin, a three-part toxin from Bacillus anthracis, consists of protective antigen (PA), lethal factor (LF), and edema factor (EF) (32). PA, the receptor-binding component of the toxin, binds to an unidentified receptor. PA is cleaved by a furin-like protease (14) and undergoes receptor-mediated endocytosis (8, 10). The PA oligomerizes to form a pore-like heptameric structure (15, 21) and transfers LF and EF into the cytosol, where LF and EF induce cytotoxic events (15, 16). The combination of LF and PA, known as lethal toxin (LT), lyses mouse macrophages within 90 min after addition of the toxin (8, 11). LF is a zinc metalloprotease (13) that is known to cleave at least two targets, mitogen-activated protein kinase kinases 1 and 2 (MAPKK1 and MAPPK2) (4, 35). Cleavage of MAPKK1 by LF inactivates MAPKK1.
Previous research localized the receptor-binding domain of the 735-amino-acid PA to the C terminus, within domain 4 (amino acids [aa] 596 to 735). Comparison of the amino acid sequence of PA with those of iota-b toxin from Clostridium perfringens (23) and the vegetative insecticidal proteins from Bacillus cereus and Bacillus thuringiensis (36) shows that these toxins have a high degree of similarity except in the C-terminal domains (24). Two monoclonal antibodies, 3B6 and 14B7 (17), recognize the region between aa 671 and 721 (18) and block the ability of PA to bind to its receptor, thereby protecting murine macrophage J774A.1 cells from PA-plus-LF challenge. In addition, C-terminal truncations of PA by 3 to 7 aa reduce the toxicity of PA plus LF, due to decreased ability of PA to bind to its receptor (30). Direct evidence that domain 4 contains the receptor recognition site is the demonstration that a CNBr fragment of PA, aa 663 to 735, is able to compete with PA for binding to cells (22).
To produce therapeutic agents, vaccines, and cell biology reagents derived from the anthrax toxin components (9), it would be advantageous to direct PA toward specific types of cell surface receptors. Because the PA receptor is present on most cell types, specificity would be improved if these reagents were derived from a mutant PA protein that is unable to bind to its own receptor. A fusion protein of wild-type PA and the p62c-Myc epitope that is recognized by the antibody produced by the hybridoma cell line 9E10 showed that PA can be redirected to an alternate receptor (34). However, this fusion protein was still able to bind to the PA receptor. To determine which residues in domain 4 are involved in receptor interaction, two solvent-exposed, flexible loops of domain 4 were mutagenized by PCR to introduce alanine (Ala) substitutions. These loops lie between β strands 4β8 and 4β9 (aa 679 to 693) and between β strands 4β9 and 4β10 (aa 704 to 723) and are called the small and large loops, respectively (24). The resulting proteins were tested for PA receptor interaction by cytotoxicity and competitive binding assays. More than 50 mutant proteins were screened, and more than 25 were analyzed in detail. During synthesis of the PCR products, errors in PCR priming and extension produced novel mutations in domain 4, including unique C-terminal truncations. These mutagenized proteins were also tested for receptor interaction. Analysis of the resulting proteins showed that the native amino acids in the large loop and the last eight amino acids of PA are not essential for receptor specificity. C-terminally truncated proteins showed a decrease in toxicity, perhaps due to destabilization of domain 4. Most importantly, we identified several nontoxic mutants which implicate the small loop in receptor recognition.
MATERIALS AND METHODS
Reagents and supplies.
Enzymes for DNA manipulation and modification were purchased from New England Biolabs, Inc. (Beverly, Mass.), Boehringer Mannheim (Indianapolis, Ind.), and Amersham Life Sciences (Arlington Heights, Ill.). Chemicals for protein work were purchased from Sigma (St. Louis, Mo.). Tissue culture products were purchased from Biofluids (Rockville, Md.) or Life Technologies (Grand Island, N.Y.), and the bacterial culture medium was purchased from Difco Laboratories (Detroit, Mich.).
Mutagenesis of PA domain 4 exposed loops.
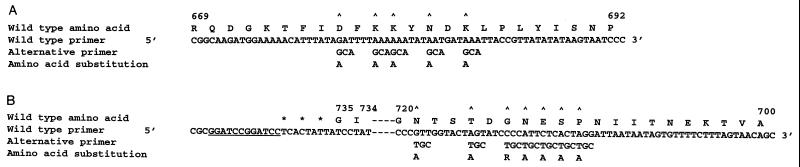
The codon-based mutagenesis protocol (3) used for mutagenesis of residues D677, K679, K680, N682, and K684 in the small loop of domain 4 required PCR amplification of the region R669 to G735 with a 3′ wild-type primer and a mutagenic, degenerate 5′ primer (Fig. 1A). The wild-type 3′ primer 5′-CGCGGATCCGGATCCTCACTATTATCCTATCTCATAGCC-3′ coded for residues G731 to G735 and two stop codons (TAG and TGA) in addition to the one TAA that exists at the 3′ end of PA in pYS5. A double BamHI restriction site and an appropriate clamp region for the BamHI enzyme were added to the primer to allow for eventual cloning of the PCR product. The 5′ degenerate 72-nucleotide (nt) primer (Fig. 1A) was synthesized on an Applied Biosystems (Foster City, Calif.) PCR-Mate 391 DNA synthesizer. During synthesis of the mutagenic primer, at positions where Ala substitutions were to be introduced, half of the resin from the 0.2-μmol DNA synthesis column was removed from the column. The Ala codon sequence, GCA (or the reverse complement, TGC), was synthesized on the remaining resin. The resin that was removed was placed into an empty column, and the wild-type codon sequence was synthesized on this column. The two resins were recombined, and synthesis of the primer continued until another Ala substitution site was reached, at which point the resin was again split. This splitting and mixing of resins created a mutagenic primer having 50% each of wild-type and Ala codons at the selected sites (Fig. 1A). When synthesis was completed, the oligonucleotide was removed from the resin according to standard protocols.
FIG. 1.
PCR mutagenesis of PA. (A and B) Degenerate primers for PCR amplification of pYS5. The wild-type amino acid and nucleotide sequences (37) are shown below the amino acid residue numbers for PA. The nucleotide substitutions encoded by the degenerate primers are shown below the wild-type sequence along with the resulting amino acid substitutions. Carats indicate the sites at which, during the synthesis of the oligonucleotide chain, the synthesis was paused to permit mixing of the resin before synthesis of the next codon. Asterisks indicate stop codons, and the underlined nucleotides are two BamHI restriction sites. (A) 5′ 72-nt degenerate primer used for the first round of PCR to generate substitutions in the small loop of domain 4 of PA; (B) 3′ 131-nt degenerate primer used to generate substitutions in the large loop of domain 4 of PA. The (unaltered) sequence at aa 733 to 721 is not shown so as to decrease the size of the figure.
The wild-type 3′ primer and the degenerate 5′ primer were used to PCR amplify pYS5 (28) with the DNA polymerase Taq (Boehringer Mannheim). The pYS5 plasmid, encoding pag (37), the gene for PA, is an Escherichia coli-Bacillus shuttle vector. The PCR product generated from the pYS5 amplification was gel purified and fused by overlap PCR to a PCR product encoding PA S319 to I676. The DNA fragment encoding PA S319 to I676 was generated by PCR using the 5′ primer 5′-AGTGTATCTGCAGGATTTAG-3 and 3′ primer 5′-TATAAATGTTTTTCCATCTTGCCG-3′. The 5′ primer binds at the unique PstI site in PA, and the 3′ primer binds to the DNA region of PA at R669 to I676. The PCR product of PA R669 to I676 overlaps with the 5′ end of the first PCR product created with the degenerate 5′ and wild-type 3′ primers, thereby permitting overlap PCR. The overlap PCR of the two PCR products was generated by using the PstI primer as the 5′ primer and the wild-type primer with the BamHI recognition sites from the first PCR as the 3′ primer. Thus, the PCR products had a PstI site at the 5′ end and a BamHI site at the other end. A PstI/BamHI digest of the overlap PCR product was cloned between the PstI and BamHI sites of pYS5. The resulting clones were identified with the prefix LST.
A protocol similar to that described above was used for mutagenesis of residues P710, S711, E712, N713, G714, T716, and N719 in the large loop of domain 4 between β strands 4β9 and 4β10 of PA. The region of DNA from P710 to G735 was amplified with a 5′ wild-type primer and degenerate 3′ primer (Fig. 1B). The last step during the synthesis of the degenerate primer also added two stop codons and two BamHI recognition sites at the end of the sequence, similar to the 3′ wild-type primer prepared for the PCR of the small loop described above. The 5′ primer overlapping the PstI site, identical to the PstI primer for the overlap PCR described above, and the degenerate 3′ primer with the BamHI site were used to PCR amplify pYS5. Gel-purified PCR product was digested with PstI and BamHI and ligated into PstI/BamHI-digested pYS5. The clones resulting from this procedure were also identified with the prefix LST. The region of pag between the PstI and BamHI sites of all LST plasmids was sequenced on both strands.
Mutagenesis of the C terminus of PA.
The mutant PA LST8-min was created by site-directed mutagenesis of the C terminus of pYS5 with a QuickChange site-directed mutagenesis kit (Stratagene, La Jolla, Calif.). PA LST8-MV was created by site-directed mutagenesis of pYS5 by modification of the ExSite PCR-based site-directed mutagenesis protocol (Stratagene). LA Taq (TaKaRa Biochemical Inc., Berkeley, Calif.) was used instead of the supplied polymerase for the ExSite reaction. LST-51L was created by PCR amplification of pPA26 (37), which encodes PA. A 5′ wild-type primer and a 3′ mutagenic primer and Pfu polymerase were used to amplify the regions that overlapped the HindIII/SmaI sites of pPA26. The HindIII site is within and near the 5′ end of the coding region for pag. The SmaI site on pPA26 lies beyond the 3′ coding region of pag. The 3′ mutagenic primer was engineered to encode a BamHI site for future manipulation, which introduced an extra serine at the C terminus of PA. The PCR product was digested with HindIII and SmaI and cloned into the HindIII/SmaI site of pYS5. DNA isolated from the transformations for pLST8-min, pLST8-MV, and LST-51L were sequenced and then used for further experiments.
Expression and purification of protein.
To express the mutagenized proteins, the plasmids were first transformed into the E. coli dcm dam strain GM2163. The unmethylated GM2163 DNA was then transformed into B. anthracis UM23C1-1 (25), from which the secreted protein was isolated as a crude preparation, as described previously (34). Culture supernatants were made to 5 mM EDTA and 35% saturation of ammonium sulfate (200 g added to each liter of supernatant), and 10 ml of phenyl-Sepharose Fast Flow (Pharmacia) was added per liter. After gentle agitation for 60 min, the resin was collected on a filter, washed with 35% saturated ammonium sulfate, and eluted with 10 mM HEPES–1 mM EDTA (pH 7.5). The resulting preparations were more than 50% pure. The LST-8, LST-26, and LST-35 proteins were further purified on a 1-ml MonoQ column (Pharmacia Biotech), using a 30 to 200 mM NaCl gradient in 10 mM CHES (2-[N-cyclohexylamino]ethanesulfonic acid)–0.06% (vol/vol) ethanolamine (pH 9.1). The pooled MonoQ fractions were dialyzed against 10 mM HEPES–1 mM EDTA (pH 8.0), concentrated with a Centricon 50 (Amicon, Beverly, Mass.), and analyzed by native 8 to 25% Phast gel electrophoresis (Pharmacia Biotech).
LST8-MV was isolated from the media of B. anthracis cultures grown in the presence of 3% horse serum to limit proteolysis, using an immunoadsorbent made from monoclonal anti-PA antibody 10G4 (17) as previously described for other PA mutants (30). The 10G4 immunoglobulin G was isolated from ascites fluid by using a MabTrapG kit (Pharmacia Biotech), and the purified 10G4 was then coupled to activated CNBr-Sepharose (Pharmacia Biotech). The 10G4-coupled resin was added to the B. anthracis culture supernatant, and the protein was eluted from the resin with 2 M NaSCN–20 mM HEPES–1 mM EDTA (pH 7.5). After extensive dialysis against 20 mM HEPES–1 mM EDTA (pH 7.5), the protein was concentrated with a Centricon 50 (Amicon) and analyzed by sodium dodecyl sulfate-polyacrylamide gel electrophoresis on 8 to 25% gradient gels (Phast gels; Pharmacia Biotech).
Quantitation of protein.
For crude extracts, the amount of the mutated PA protein was determined with the Mancini radial diffusion assay (20). Briefly, a goat antiserum against PA was added to agarose medium to create antibody-impregnated plates. Holes were punched in the agarose gel, and samples were added. After incubation at 37°C for 1 to 3 days, the concentrations of the mutagenized proteins were determined by comparison of the diameters of the immunoprecipitation rings to a standard curve prepared from purified PA.
Cell culture.
RAW264.7 cells (mouse macrophages) were cultured in Dulbecco’s modified Eagle’s medium with 4,500 mg of d-glucose per liter, 10% (vol/vol) fetal bovine serum, 50 μg of gentamicin per ml, 10 mM HEPES, and 2 mM glutamine.
Cytotoxicity assays.
The macrophage lysis assay was used to measure the toxicity of the mutagenized PA proteins for RAW264.7 macrophages (26). PA, as a control, or the mutagenized proteins were serially diluted in the presence of 100 ng of LF per ml. The protein solution was added to one-third confluent, adherent RAW264.7 cells in a 96-well microtiter plate to a final volume of 200 μl/well. The cells were incubated for 3 h at 37°C in the presence of toxin. Cell viability was assayed by adding MTT (3-[4,5-dimethylthiazol-2-yl]-2,5-diphenyltetrazolium bromide), which is converted by viable cells to an insoluble blue pigment, which was dissolved and measured as described previously (34).
Competitive cytotoxicity assays.
For the competitive cytotoxicity assays, the mutagenized PA proteins at various fixed concentrations and 100 ng of LF per ml were first added to a microtiter dish. Then native PA was added and serially diluted in the wells, holding the concentration of the mutated PA and LF constant. For comparison to the mutant PA proteins, we used PA ΔFF, a nontoxic receptor-binding variant of PA in which residues F313 and F314 are deleted (29). The protein mixture was added to RAW264.7 cells, and the cytotoxicity assay was performed as detailed above. The EC50s (concentrations of toxin required to kill 50% of the cells) from the competition assays were used to construct Schild plots (12).
RESULTS
Mutagenesis of domain 4 exposed loops of PA (LST clones).
Although the crystal structure of PA was recently solved (24), little work has been done to identify residues in domain 4 that are involved in binding to receptor. Therefore, we chose a mutagenesis method that would economically survey many residues simultaneously. We targeted two loops on the domain 4 surface that is predicted from the structure of the heptameric PA63 to face toward the cell surface. These two loops are solvent exposed and differ most from the homologous region of C. perfringens iota toxin. Codon-based mutagenesis (3) permitted the creation of multiple substitutions in different combinations (Fig. 1A). Selection of residues to mutagenize was somewhat arbitrary, although hydrophilic residues that were more likely to be surface exposed were preferred. Because a convenient restriction site was not available between the PstI and BamHI restriction sites, mutagenesis of the 15-aa small loop between β strands 4β8 and 4β9 required overlap PCR with an upstream PCR-amplified product. Only two mutants were obtained from this mutagenesis reaction. The mutagenesis of the 20-aa large loop between β strands 4β9 and 4β10 was simpler, and over 40 mutants were isolated from the mutagenesis of this region. Some plasmids were also found to code for novel mutations not encoded by the primers.
Cytotoxicity of PA domain 4 mutants (LST clones).
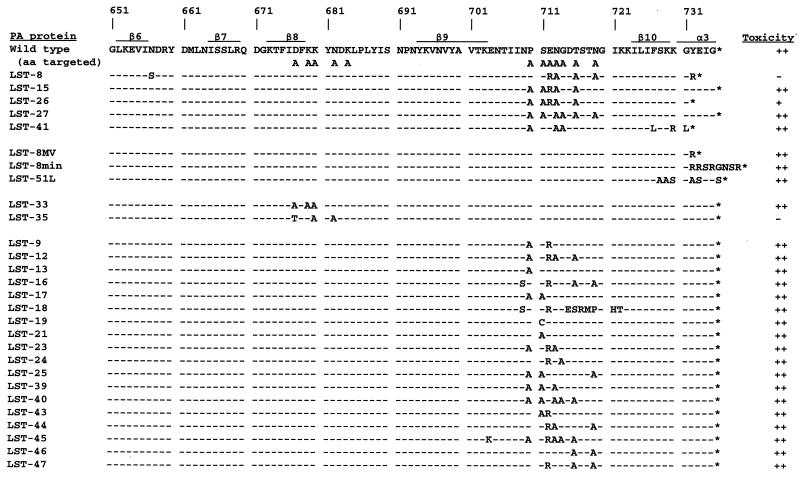
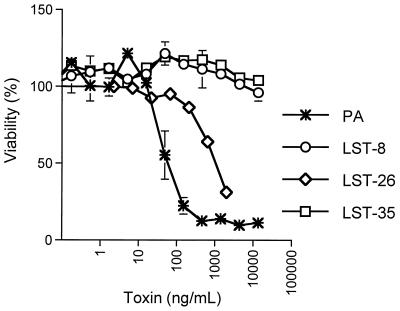
If a mutation in the PA prevents binding of the protein to the PA receptor, then the mutagenized PA (LST proteins) and LF should not be cytotoxic to RAW264.7 cells (mouse macrophages). Most of the mutant PA proteins were toxic when tested in the presence of LF (Fig. 2). All of the PA proteins with substitutions restricted to the large loop were fully toxic. For example, LST-18 had eight substitutions in the large loop (aa 709, 712, 715 to 719, and 721 to 722) and remained fully toxic. Only two of the LST clones, LST-35 and LST-8, were nontoxic (Fig. 3). LST-26 was partially toxic, with an EC50 of 1,000 ng/ml, compared to 60 ng/ml for PA (Fig. 3).
FIG. 2.
Mutated PA protein sequences. Shown are the C-terminal amino acid sequences of mutated PA proteins from residue 651 to the end of the protein sequence (indicated by *). The β-strand (β) and α-helical (α) motifs of PA are indicated above the wild-type PA sequence (37) as determined from the PDB file of the crystal structure of PA (PDB ID code 1ACC) (24). The motifs are numbered according to their sequential appearance in domain 4 of PA. Regions targeted for mutagenesis included the small loop, aa 678 to 693, and the large loop, aa 704 to 723. The substituted amino acids are indicated in the sequence. Toxicities of the proteins as determined from RAW264.7 cell cytotoxicity assays are indicated at the column right as ++ (10 to 100% as toxic as wild type), + (2 to 10% as toxic as wild type), or − (<0.1% as toxic as wild type).
FIG. 3.
Cytotoxicity assays. PA or the LST proteins were serially diluted into a 96-well plate containing RAW264.7 cells in the presence of LF (100 ng/ml). After 3 h of toxin challenge, MTT was added to determine cell viability. Data points are the mean ± standard deviation of triplicate wells, and the experiment shown is representative of the three performed.
Role of C-terminal residues of PA.
PCR amplification with Taq polymerase introduced novel mutations into the PA proteins (5, 31). The proteins LST-8, LST-26, and LST-41 were found to have C-terminal truncations. Analysis of these proteins showed that LST-8 was nontoxic, LST-26 was partially toxic, and LST-41 was fully toxic in the presence of LF (Fig. 2). LST-26 has the same internal amino acid substitutions as the fully toxic mutant LST-15, suggesting that the truncation was responsible for the decreased activity of LST-26. However, LST-41 was similarly truncated and was fully toxic. Also, LST-8, which was nontoxic, has a novel mutation at the C terminus not present in LST-26, namely, a Y732R substitution. However, LST-8 also has an N657S substitution not found in any other protein.
To more closely examine the role of truncations and of the Y732R substitution, site-specific mutagenesis was used to construct two additional mutants, LST-8MV and LST-8min. Both LST-8MV and LST-8min have the Y732R substitution at the C terminus, similar to LST-8 (Fig. 2). LST-8MV has the same truncation as LST-8, whereas LST-8min has an extension of seven nonnative amino acids beyond the Y732R terminus of LST-8MV and LST-8. Both LST-8MV and LST-8min were found to be fully toxic. Then to test whether mutagenesis of the C-terminal residues to neutral residues would affect the toxicity and ability of PA to bind to its receptor, LST-51L was created. This protein, like LST-8MV and LST-8min, was fully toxic (Fig. 2).
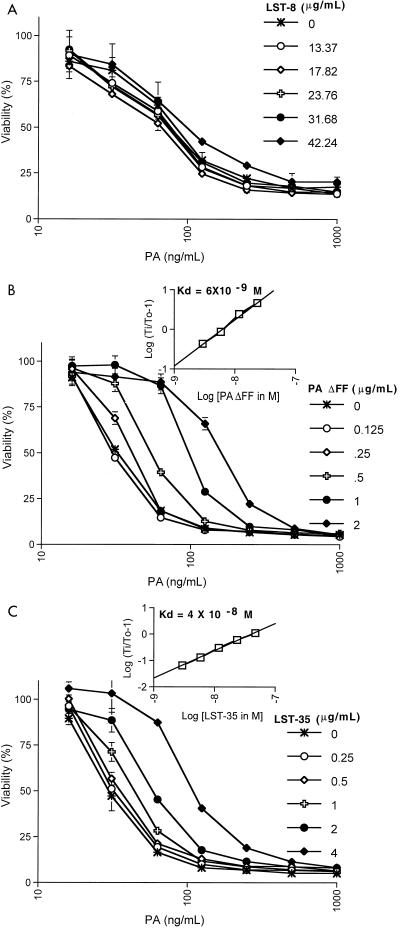
Because LST-8 was nontoxic, competitive cytotoxicity assays were performed to determine if LST-8 bound to the PA receptor (Fig. 4A). If the LST protein does not compete with PA, then the LST protein is nontoxic because the protein is unable to bind to the receptor. In the presence of competitor, competition is shown by shifts of the cytotoxicity dose-response curve to the right. The nontoxic variant of PA, PA ΔFF, was used as a control (Fig. 4B). PA ΔFF is a variant of PA that binds to the receptor but is nontoxic because of a mutation that affects membrane channel formation and translocation (29). The data show that PA ΔFF protected the cells from PA (Fig. 4B) but that LST-8 did not (Fig. 4A). In fact, LST-8 was tested at concentrations up to 42 μg/ml and still failed to protect the cells from PA.
FIG. 4.
Assay of mutated PA proteins for competitive inhibition of cytotoxicity. For the assay, LST-8 (A), PA ΔFF (B), or LST-35 (C) at various concentrations, in the presence of LF (100 ng/ml), was added to 96-well plates containing RAW264.7 cells. PA was serially diluted into the wells; after 3 h of toxin challenge, MTT was added to determine cell viability. Viability was normalized to wells lacking PA. The insets in panels B and C show the Schild plots and derived Kds constructed from the EC50 values plotted on the graphs. The EC50s for PA in the absence and presence of competitor are indicated as To and Ti, respectively. Data points are the mean ± standard deviation of triplicate wells, and the experiments shown are representative of the two to four that were performed for each mutant PA.
Role of small loop residues.
Due to the complex nature of the PCR mutagenesis of the small loop (Fig. 1A), only two clones LST-33 and LST-35, were recovered from the mutagenesis of this region (Fig. 2). LST-33 was fully toxic, whereas LST-35 was nontoxic. LST-33 and LST-35 both contained substitutions at residues D677 and K680. N682 was the only residue of LST-35 not substituted in LST-33, suggesting that it may play a major role in receptor recognition. Competition assays were performed with LST-35 in the same way as for LST-8 (Fig. 4). The EC50 of each curve was then used in a Schild plot to calculate the Kd (dissociation constant). LST-35, which was at least 100-fold less toxic than wild native PA (Fig. 3), did bind to the PA receptor (Fig. 4C), although the Kd was only 4 × 10−8 M, compared with 6 × 10−9 M for PA ΔFF.
DISCUSSION
The intent of this research was to mutagenize the small and large solvent-exposed loops of domain 4 of PA (amino acids 679 to 693 and 704 to 723, respectively) to determine which residues in this region are involved in receptor interaction. Substitutions within the large loop had little or no effect on the ability of PA to kill RAW264.7 cells in the presence of LF (Fig. 2). These data show that the large loop probably does not interact directly with the receptor, and if it participates less directly in receptor interaction, this function is tolerant of many amino acid substitutions. Too few proteins mutated in the small loop were obtained to fully characterize the role of this loop in receptor interaction. However, the two proteins mutated in this region were informative because they differed substantially in activity, with LST-33 having normal activity and LST-35 being nontoxic. LST-35, even though nontoxic, was still capable of binding to the receptor, but with about 10-fold less affinity than PA (discussed below). The other nontoxic mutant obtained in this study, LST-8, has four substitutions in the large loop, but its lack of activity must be due to other mutations, as discussed below.
Some of the mutagenized plasmids obtained in this work were found to contain novel, unintended mutations, apparently introduced either by PCR or by the extensive manipulations of the PCR primers. Fortunately, several of these mutations helped to elucidate the function of the extreme C-terminal region of PA. One protein, LST-26, had an unexpected 4-aa C-terminal truncation and was partially toxic (Fig. 2 and 3). Comparison of LST-26 with LST-15 showed that the truncation in LST-26 was responsible for its decreased toxicity. The decreased activity of LST-26 is consistent with previous research which had shown that truncation of three, five, or seven residues from the C terminus reduces toxicity, while larger truncations of 12 or 14 aa abolishes toxicity of PA (30). However, LST-41 and LST8-MV were also truncated, and both were fully toxic (Fig. 2). These two proteins have additional mutations at the extreme C terminus that are not present in LST-26. These data indicate that while simple truncations of the C terminus generally reduce toxicity, extensive substitutions do not necessarily reduce toxicity. Substitution of native C-terminal residues with alternate residues may stabilize the structure of the protein compared to truncation of those residues. In particular, it appears that the Y732R substitution present in LST-8MV (and LST-8) may compensate for truncation of the proximal three amino acid residues. The crystal structure data show that the C terminus of PA is an α helix (24). This helix is the region that is truncated in LST-26, LST-41, and LST8-MV (Fig. 2). However, protein prediction programs such as PredictProtein (27) do not predict the helical motif observed by X-ray diffraction and cannot accurately predict whether substitutions in this region disrupt the helix.
Further evidence that the extreme C terminus is not critical to receptor binding is the somewhat surprising retention of activity in LST8-min and LST-51L, which have multiple substitutions at the extreme C terminus. Both of these proteins were fully toxic in the presence of LF. In fact, addition of an extra 16 aa to the C terminus of wild-type PA does not affect toxicity (34). This supports the view that the native residues at the C terminus of PA do not confer receptor specificity but instead stabilize the PA structure in a way that permits the protein to interact with the receptor.
For the two proteins found to be nontoxic, LST-8 and LST-35 (Fig. 3), competition assays showed that LST-8 does not bind to PA receptor, while LST-35 binds to the receptor with a decreased affinity (Kd of 4 × 10−8 M) (Fig. 4A and C). For comparison, PA ΔFF, a nontoxic but receptor-binding variant of PA, had a Kd of 6 × 10−9 M (Fig. 4B). The Kd of PA is 1 × 10−9 to 5 × 10−9 M (6, 30). Thus, LST-35 has 10- to 40-fold-lower affinity for the PA receptor. Because PA must form a heptamer as part of the intoxication process (15, 21), a 10-fold-lower affinity for receptor could cause a decrease in toxicity that is much greater than 10-fold, theoretically even approaching 107-fold. This may explain the lack of toxicity of LST-35.
The most informative and potentially useful mutants obtained in this study are LST-8 and LST-35. The nontoxic LST-8 protein has alterations in three regions. Comparison to the toxic mutant proteins discussed above shows that the substitutions in the large loop and at the C terminus of LST-8 are probably not responsible for its lack of toxicity, indicating that the N657S substitution may be the critical change. Comparison of the residues mutated in LST-35 with those in LST-33 suggests that the N682A substitution in LST-35 may be responsible for its lack of toxicity. It should be added that this type of argument does not consider the possibility that several substitutions or truncations which individually have no effect on toxicity can interact to disable the protein. This type of effect, if present, will probably become evident once a thorough analysis of individual local regions is completed.
The PA crystal structure (24) provides a possible explanation as to how the two critical residues identified by analysis of LST-8 and LST-35, namely, N657 and N682, might both be involved in receptor interaction. Although not adjacent in the primary sequence, the two residues are only 8 Å apart in the crystal structure. N657 is a partially buried residue, whereas N682 is surface exposed. The proximity of N657 and N682 suggests that Ala or possibly other substitutions at these positions alter the structure of the surface-exposed small loop area so as to decrease the affinity of PA for its receptor. This indicates that the essential receptor-binding residues may lie within or near the small loop. Consistent with this proposal, the X-ray crystal structure shows that the large loop and the C-terminal α helix of domain 4 lie on the opposite face of the protein from the small loop, consistent with their limited role in receptor binding as revealed by the large loop mutants.
Despite the fact that the majority of the clones isolated from the mutagenesis of PA were still toxic, the two nontoxic proteins, LST-35 and LST-8, and the truncation data indicate that domain 4 of PA is the receptor-binding domain. Domain 4 appears to be a separate domain and shows limited contact with the other three domains (24). Molecular modeling of the heptamer formed by PA during the intoxication process suggests that domain 4 swings out of the way during membrane insertion. Also, fusion of a p62c-Myc epitope to the C terminus of wild-type PA permits this fusion toxin to use antibody directed against the epitope as a receptor (34). Fusion of novel epitopes to LST-8, which does not bind PA receptor, should permit the creation of new anthrax toxins directed to specific cell types. An alternative strategy for redirecting PA would be to delete domain 4 and replace it with other receptor-binding domains. Other modular toxins, such as diphtheria toxin (1, 2, 7, 19) and Pseudomonas exotoxin (2, 33), have been modified to target new receptors. In fact, fusion of the Fc-binding domain of protein A to diphtheria toxin created a toxin that was more potent than the intact diphtheria toxin (19).
In conclusion, mutagenesis of the large loop (aa 704 to 722) in domain 4 of PA did not affect the ability of PA to bind receptor. Truncation of the C terminus, even of only 3 aa, reduced the ability of PA to bind to its receptor. In contrast, substitution of the last 8 aa had no effect on the toxicity of PA in conjunction with LF. This work has established that the native amino acid residues in the large loop of domain 4 and at the C terminus of PA are not essential for receptor binding, but instead an intact C-terminal structural motif seems necessary for toxicity and receptor interaction. The receptor binding residues of PA lie within domain 4, probably in the small loop between β strands 4β8 and 4β9. Analysis of the large number of mutants described here has succeeded in localizing a small region involved in receptor binding. Further work is in progress to delineate the roles of the individual residues in this region.
ACKNOWLEDGMENTS
We thank Carlo Petosa for helpful advice on targeted mutagenesis and Marian Betz and Ryan Miyamoto for technical assistance.
REFERENCES
- 1.Aullo P, Alcami J, Popoff M R, Klatzmann D R, Murphy J R, Boquet P. A recombinant diphtheria toxin related human CD4 fusion protein specifically kills HIV infected cells which express gp120 but selects fusion toxin resistant cells which carry HIV. EMBO J. 1992;11:575–583. doi: 10.1002/j.1460-2075.1992.tb05089.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Batra J K, FitzGerald D J, Chaudhary V K, Pastan I. Single-chain immunotoxins directed at the human transferrin receptor containing Pseudomonas exotoxin A or diphtheria toxin: anti-TFR(Fv)-PE40 and DT388-anti-TFR(Fv) Mol Cell Biol. 1991;11:2200–2205. doi: 10.1128/mcb.11.4.2200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cormack B P, Struhl K. Regional codon randomization: defining a TATA-binding protein surface required for RNA polymerase III transcription. Science. 1993;262:244–248. doi: 10.1126/science.8211143. [DOI] [PubMed] [Google Scholar]
- 4.Duesbery N S, Webb C P, Leppla S H, Gordon V M, Klimpel K R, Copeland T D, Ahn N G, Oskarsson M K, Fukasawa K, Paull K D, Vande Woude G F. Proteolytic inactivation of MAP-kinase-kinase by anthrax lethal factor. Science. 1998;280:734–737. doi: 10.1126/science.280.5364.734. [DOI] [PubMed] [Google Scholar]
- 5.Eckert K A, Kunkel T A. DNA polymerase fidelity and the polymerase chain reaction. PCR Methods Appl. 1991;1:17–24. doi: 10.1101/gr.1.1.17. [DOI] [PubMed] [Google Scholar]
- 6.Escuyer V, Collier R J. Anthrax protective antigen interacts with a specific receptor on the surface of CHO-K1 cells. Infect Immun. 1991;59:3381–3386. doi: 10.1128/iai.59.10.3381-3386.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Finberg R W, Wahl S M, Allen J B, Soman G, Strom T B, Murphy J R, Nichols J C. Selective elimination of HIV-1-infected cells with an interleukin-2 receptor-specific cytotoxin. Science. 1991;252:1703–1705. doi: 10.1126/science.1904628. [DOI] [PubMed] [Google Scholar]
- 8.Friedlander A M. Macrophages are sensitive to anthrax lethal toxin through an acid-dependent process. J Biol Chem. 1986;261:7123–7126. [PubMed] [Google Scholar]
- 9.Goletz T J, Klimpel K R, Arora N, Leppla S H, Keith J M, Berzofsky J A. Targeting HIV proteins to the major histocompatibility complex class I processing pathway with a novel gp120-anthrax toxin fusion protein. Proc Natl Acad Sci USA. 1997;94:12059–12064. doi: 10.1073/pnas.94.22.12059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gordon V M, Leppla S H, Hewlett E L. Inhibitors of receptor-mediated endocytosis block the entry of Bacillus anthracis adenylate cyclase toxin but not that of Bordetella pertussis adenylate cyclase toxin. Infect Immun. 1988;56:1066–1069. doi: 10.1128/iai.56.5.1066-1069.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hanna P C, Kouchi S, Collier R J. Biochemical and physiological changes induced by anthrax lethal toxin in J774 macrophage-like cells. Mol Biol Cell. 1992;3:1269–1277. doi: 10.1091/mbc.3.11.1269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ittelson T R, Gill D M. Diphtheria toxin: specific competition for cell receptors. Nature. 1973;242:330–332. doi: 10.1038/242330b0. [DOI] [PubMed] [Google Scholar]
- 13.Klimpel K R, Arora N, Leppla S H. Anthrax toxin lethal factor contains a zinc metalloprotease consensus sequence which is required for lethal toxin activity. Mol Microbiol. 1994;13:1093–1100. doi: 10.1111/j.1365-2958.1994.tb00500.x. [DOI] [PubMed] [Google Scholar]
- 14.Klimpel K R, Molloy S S, Thomas G, Leppla S H. Anthrax toxin protective antigen is activated by a cell-surface protease with the sequence specificity and catalytic properties of furin. Proc Natl Acad Sci USA. 1992;89:10277–10281. doi: 10.1073/pnas.89.21.10277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Leppla S H. The anthrax toxin complex. In: Alouf J E, Freer J H, editors. Sourcebook of bacterial protein toxins. London, England: Academic Press; 1991. pp. 277–302. [Google Scholar]
- 16.Leppla S H. Anthrax toxins. In: Moss J, Iglewski B, Vaughan M, Tu A, editors. Handbook of natural toxins. 8. Bacterial toxins and virulence factors in disease. New York, N.Y: Marcel Dekker, Inc.; 1995. pp. 543–572. [Google Scholar]
- 17.Little S F, Leppla S H, Cora E. Production and characterization of monoclonal antibodies to the protective antigen component of Bacillus anthracis toxin. Infect Immun. 1988;56:1807–1813. doi: 10.1128/iai.56.7.1807-1813.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Little S F, Novak J M, Lowe J R, Leppla S H, Singh Y, Klimpel K R, Lidgerding B C, Friedlander A M. Characterization of lethal factor binding and cell receptor binding domains of protective antigen of Bacillus anthracis using monoclonal antibodies. Microbiology. 1996;142:707–715. doi: 10.1099/13500872-142-3-707. [DOI] [PubMed] [Google Scholar]
- 19.Madshus I H, Stenmark H, Sandvig K, Olsnes S. Entry of diphtheria toxin-protein A chimeras into cells. J Biol Chem. 1991;266:17446–17453. [PubMed] [Google Scholar]
- 20.Mancini G, Carbonara A O, Heremans J F. Immunochemical quantitation of antigens by single radial immunodiffusion. Immunochemistry. 1965;2:235–254. doi: 10.1016/0019-2791(65)90004-2. [DOI] [PubMed] [Google Scholar]
- 21.Milne J C, Furlong D, Hanna P C, Wall J S, Collier R J. Anthrax protective antigen forms oligomers during intoxication of mammalian cells. J Biol Chem. 1994;269:20607–20612. [PubMed] [Google Scholar]
- 22.Noskov A N, Kravchenko T B, Noskova V P. Detection of the functionally active domains in the molecule of protective antigen of the anthrax exotoxin. Mol Gen Mikrobiol Virusol. 1996;1996:16–20. . (In Russian.) [PubMed] [Google Scholar]
- 23.Perelle S, Gibert M, Boquet P, Popoff M R. Characterization of Clostridium perfringens iota-toxin genes and expression in Escherichia coli. Infect Immun. 1993;61:5147–5156. doi: 10.1128/iai.61.12.5147-5156.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Petosa C, Collier R J, Klimpel K R, Leppla S H, Liddington R C. Crystal structure of the anthrax toxin protective antigen. Nature. 1997;385:833–838. doi: 10.1038/385833a0. [DOI] [PubMed] [Google Scholar]
- 25.Quinn C P, Dancer B N. Transformation of vegetative cells of Bacillus anthracis with plasmid DNA. J Gen Microbiol. 1990;136:1211–1215. doi: 10.1099/00221287-136-7-1211. [DOI] [PubMed] [Google Scholar]
- 26.Quinn C P, Singh Y, Klimpel K R, Leppla S H. Functional mapping of anthrax toxin lethal factor by in-frame insertion mutagenesis. J Biol Chem. 1991;266:20124–20130. [PubMed] [Google Scholar]
- 27.Rost, B. PredictProtein. http://www.embl-heidelberg.de/Services/sander/predictprotein. [Online.] [29 January 1999, last date accessed.]
- 28.Singh Y, Chaudhary V K, Leppla S H. A deleted variant of Bacillus anthracis protective antigen is non-toxic and blocks anthrax toxin action in vivo. J Biol Chem. 1989;264:19103–19107. [PubMed] [Google Scholar]
- 29.Singh Y, Klimpel K R, Arora N, Sharma M, Leppla S H. the chymotrypsin-sensitive site, FFD315, in anthrax toxin protective antigen is required for translocation of lethal factor. J Biol Chem. 1994;269:29039–29046. [PubMed] [Google Scholar]
- 30.Singh Y, Klimpel K R, Quinn C P, Chaudhary V K, Leppla S H. The carboxyl-terminal end of protective antigen is required for receptor binding and anthrax toxin activity. J Biol Chem. 1991;266:15493–15497. [PubMed] [Google Scholar]
- 31.Smedley D P, Ellar D J. Mutagenesis of three surface-exposed loops of a Bacillus thuringiensis insecticidal toxin reveals residues important for toxicity, receptor recognition and possibly membrane insertion. Microbiology. 1996;142:1617–1624. doi: 10.1099/13500872-142-7-1617. [DOI] [PubMed] [Google Scholar]
- 32.Stanley J L, Smith H. Purification of factor I and recognition of a third factor of anthrax toxin. J Gen Microbiol. 1961;26:49–66. doi: 10.1099/00221287-26-1-49. [DOI] [PubMed] [Google Scholar]
- 33.Theuer C P, FitzGerald D, Pastan I. A recombinant form of Pseudomonas exotoxin directed at the epidermal growth factor receptor that is cytotoxic without requiring proteolytic processing. J Biol Chem. 1992;267:16872–16877. [PubMed] [Google Scholar]
- 34.Varughese M, Chi A, Teixeira A V, Nicholls P J, Keith J M, Leppla S H. Internalization of a Bacillus anthracis protective antigen c-Myc fusion protein mediated by cell surface anti-c-Myc antibodies. Mol Med. 1998;4:87–95. [PMC free article] [PubMed] [Google Scholar]
- 35.Vitale G, Pellizzari R, Recchi C, Napolitani G, Mock M, Montecucco C. Anthrax lethal factor cleaves the N-terminus of MAPKKs and induces tyrosine/threonine phosphorylation of MAPKs in cultured macrophages. Biochem Biophys Res Commun. 1998;248:706–711. doi: 10.1006/bbrc.1998.9040. [DOI] [PubMed] [Google Scholar]
- 36.Warren G W, Koziel M G, Mullins M A, Nye G J, Carr B, Desai N, Kostischka K, Duck N B, Estruch J J. Novel pesticidal proteins and strains. Patent application WO 96/10083 (1996). World Intellectual Patent Organization; 1996. [Google Scholar]
- 37.Welkos S L, Lowe J R, Eden-McCutchan F, Vodkin M, Leppla S H, Schmidt J J. Sequence and analysis of the DNA encoding protective antigen of Bacillus anthracis. Gene. 1988;69:287–300. doi: 10.1016/0378-1119(88)90439-8. [DOI] [PubMed] [Google Scholar]