Abstract
Humans and animals can become asymptomatic carriers of Listeria monocytogenes and introduce the pathogen into their environment with their feces. In turn, this environmental contamination can become the source of food- and feed-borne illnesses in humans and animals, with the food production chain representing a continuum between the farm environment and human populations that are susceptible to listeriosis. Here, we update a review from 2012 and summarize the current knowledge on the asymptomatic carrier statuses in humans and animals. The data on fecal shedding by species with an impact on the food chain are summarized, and the ways by which asymptomatic carriers contribute to the risk of listeriosis in humans and animals are reviewed.
Keywords: domestic animals, ruminants, wildlife, human, crop, vegetable, environmental contamination, asymptomatic carriers, Listeria monocytogenes
1. Introduction
Food-borne listeriosis caused by Listeria monocytogenes accounted for 1876 human cases in the EU in 2020. It is also the zoonosis with the highest case fatality rate of 10% in the EU [1]. Combined with the often severe neurological symptoms, this makes listeriosis a high priority for food safety efforts worldwide. L. monocytogenes has a broad host range in humans, as well as wild and domestic animals that typically become infected by the ingestion of food or feed that has been contaminated with L. monocytogenes.
Potential sources for L. monocytogenes in feed and food result from the ubiquitous presence of L. monocytogenes in the environment [2], fecal shedding by hosts and the ability of L. monocytogenes to establish itself in suitable niches in the farm or food-processing environment due to its capacity to adapt to a broad range of environmental stresses [3].
The food chain provides a direct link between the farm environment and human hosts. L. monocytogenes gains access to food production facilities through either raw materials of animal origin (meat and milk) via produce that are contaminated with L. monocytogenes from soil or feces or from other sources through a lack in hygiene management. A subset of strains of L. monocytogenes (e.g., clonal complex (CC) 9 or 121) have shown a higher propensity to persist in the food production environment, mainly through increased resistance against disinfectants such as quaternary ammonium compounds [4]. It is not uncommon for L. monocytogenes to persist in niches in food processing facilities for years or even decades [5].
Taken together, food intended for human consumption may become contaminated with L. monocytogenes at any level: (i) during primary production at the farm level, (ii) during processing or (iii) at the retail or (iv) consumer level due to insufficient hygiene measures during food handling. If L. monocytogenes is able to grow in food or feed matrices that are consumed without an inactivation step (e.g., heating), the basic conditions for an outbreak of listeriosis are met.
Infections of human or animal hosts result in clinical presentations that range from asymptomatic carriers to septicemia, encephalitis or abortions [6]. While the pathomechanisms in the host and the bacterial virulence factors in L. monocytogenes are well-understood, it remains largely unclear why some individuals become asymptomatic carriers. In some cases, truncated alleles of the gene inIA encoding surface protein internalin A were found in strains isolated from asymptomatic human carriers [7]. Truncated forms of the inlA gene were associated with a loss of virulence [8], which may lead to asymptomatic carriage, and were also overrepresented in isolates from food compared to clinical isolates [9], suggesting the potential exposure of consumers to these isolates. Additionally, a contribution of viable but nonculturable (VBNC) forms of L. monocytogenes [10] to asymptomatic carriage has been hypothesized [11,12].
Among other bacteria, L. monocytogenes has developed various mechanisms for switching from a vegetative to a metabolically inactive state. However, L. monocytogenes in the VBNC state represent a diagnostic challenge, because the majority of the current tests need at least one cultivation step, thus failing to detect nongrowing VBNC cells. Fortunately, in recent years, a variety of PCR and qPCR applications combined with DNA intercalating dyes have been established for detecting viable and VBNC cells [12].
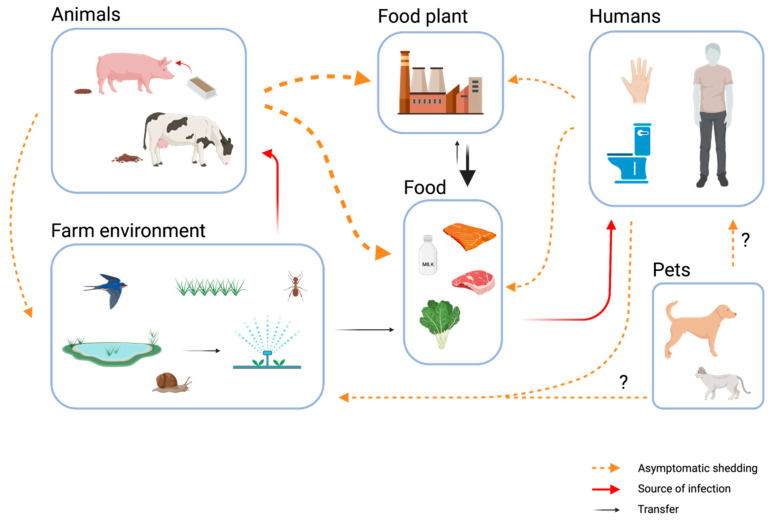
Asymptomatic carriers present a major challenge to food safety (Figure 1). On the other hand, according to a recent study, the gut microbiota itself is a major line of defense against foodborne pathogens [13]. The authors point out that a specific microbiota signature is associated with the asymptomatic shedding of L. monocytogenes. They conclude that fecal carriage of this pathogen is a common phenomenon in healthy individuals and is very much influenced by the gut microbiota [13].
Figure 1.
Role of asymptomatic fecal shedding of L. monocytogenes by humans and animals in the spread between habitats with a focus on food safety. Bold arrows indicate the most relevant contamination pathways in food production chains in Europe today—in particular, along the farm–food plant–food continuum. Figure was created with BioRender.com.
Efficient controls are in place to exclude animals that are obviously ill from milk or meat production. In contrast, the intermittent fecal shedding of asymptomatic carriers often remains invisible in humans and animals. [14]. With regard to farm animals, the fecal shedding of L. monocytogenes can lead to three contamination scenarios with potential implications for food safety: (i) It contributes to a higher load of L. monocytogenes in the immediate barn environment, increasing the risk of additional animals becoming infected. (ii) Manure from these animals may be used to fertilize fields, and runoff from farms may contaminate water sources, both risk factors for the contamination of feed and crops with L. monocytogenes [15,16]. (iii) Unrecognized carrier animals may lead to raw milk and meat contamination due to insufficient hygiene practices during milking or slaughtering. Finally, asymptomatic human colonization with L. monocytogenes may result in the direct contamination of food or the food processing environment due to insufficient hand hygiene.
The aim of this review is to update a 2012 review on the asymptomatic carrier statuses in different species [17] and to summarize the current knowledge on risk factors associated with fecal shedding in different species.
2. Domestic Animals as Asymptomatic Carriers
From studies on Listeria ecology, the asymptomatic carriage of L. monocytogenes seems to be evident worldwide, and most domestic animal species, including dogs and cats, can shed L. monocytogenes intermittently via feces (Table 1). In addition, the prevalence data showed significant counts of L. monocytogenes in tonsil samples from healthy domestic animals (Table 1). The role of household pets in spreading L. monocytogenes is not well-studied. To our knowledge, there is no documented clinical case of the transmission of L. monocytogenes from pets to humans. However, in recent years, it has become increasingly popular for dog and cat owners to feed their pets raw meat-based diets (RMBDs) instead of the more conventional dry or canned pet foods. A Dutch research team demonstrated that RMBDs may be a possible source of L. monocytogenes infection in pet animals and, if transmitted, pose a risk for human beings. They analyzed 35 commercial RMBDs from eight different brands. Alarmingly, L. monocytogenes was present in 54% of all tested samples [18].
Table 1.
Isolation of Listeria monocytogenes from healthy domestic animals.
| Country | Animal | Target | Sample (n) | Positive (%) | Ref. |
|---|---|---|---|---|---|
| Austria | Sheep/Goat | L. spp. | Feces (53) | 42.6 | [32] |
| L. monocytogenes | 13 | ||||
| Egypt | Cattle | L. monocytogenes | Feces (660) | 6.8 | [37] |
| Milk (660) | 5.9 | ||||
| Finland | Chicken | L monocytogenes | Cloacal swabs (457) | 1.3 | [36] |
| Germany | Cattle | L. monocytogenes | Feces (138) | 33 | [38] |
| Sheep | (100) | 8 | |||
| Hens | (100) | 8 | |||
| Pigs | (34) | 5.9 | |||
| Horses | (400) | 4.8 | |||
| Dogs | (300) | 1.3 | |||
| Cats | (275) | 0.4 | |||
| Germany | Pigs | L. monocytogenes | Tonsils (430) | 1.6 | [39] |
| L. innocua | 1.2 | ||||
| Italy | Pigs | L. monocytogenes | Salivary gland, lymph nodes, tonsils (189) | 13.2 | [40] |
| Japan | Cattle | L. monocytogenes | Feces (1705) | 1.9 | [41] |
| Pigs | 0.6 | ||||
| Dogs | 0.9 | ||||
| Rats | 6.5 | ||||
| Japan | Cattle | L. monocytogenes | Feces (1738) | 6 | [42] |
| Jordan | Cattle | L. monocytogenes | Feces (610) | 1.5 | [43] |
| Qatar | Camel | L. monocytogenes | Feces (50) | 4 | [44] |
| Slovenia | Cows | L. monocytogenes | Feces (540) | 18.2 | [45] * |
| Calves | (511) | 8.4 | |||
| Spain | Cattle (beef) | L. monocytogenes | Feces (301) | 42.3 | [23] |
| Cattle (dairy) | 46.3 | ||||
| Sheep | 23.5 | ||||
| Spain | Cattle | L. monocytogenes | Feces (953) | 4.3 | [25] |
| Sheep | Feces (483) | 5.8 | |||
| Goat | Feces (333) | 0.3 | |||
| Switzerland | Cattle | Ab to LO | Serum (1652) | 11 | [24] |
| and IA ** | |||||
| Taiwan | Chicken | L. monocytogenes | Carcass rinse (246) | 11.4 | [35] |
| USA | Cattle | L. monocytogenes | Feces (825) | 31 | [14] *** |
| USA | Cattle | L. monocytogenes | Feces (528) | 20.2 | [31] **** |
| USA | Broiler | L. monocytogenes | Feces (555) | 14.9 | [46] |
| USA (Central NY State) | Cattle | L. monocytogenes | Milk (1412) | 13 | [47] |
| Udder swab (1408) | 19 | ||||
| Feces (1414) | 43 |
* Fecal samples were collected from cows and calves on 20 family dairy farms in 2-week intervals for a period of 1 year. ** Antibodies to listeriolysin O and internalin A. *** Twenty-five fecal samples were collected daily for two 2-week periods and one 5-day period. **** A case–control study involving 24 case farms with at least one recent case of listeriosis and 28 matched control farms with no listeriosis cases was conducted to study the transmission and ecology of Listeria monocytogenes on farms.
Pigs can be important reservoirs for L. monocytogenes (Table 1), and in particular, younger animals are at risk for asymptomatic carriage. For example, the prevalence of L. monocytogenes in the tonsils of fattening pigs (22%) was significantly higher than in sows (6%) [19]. Hypervirulent clones of L. monocytogenes such as CC6 [9] were found in pig tonsils, and due to the presence of closely related isolates along the production chain, the cross-contamination or recontamination of meat from a specific source in the slaughterhouse seems to play an important role [20].
Housing conditions significantly influence the risk of L. monocytogenes detection in healthy pigs: According to Hellstrom et al. [21], there is a higher prevalence of L. monocytogenes in animals from organic production compared to conventional farms. The EU regulation on organic production (EU 2018/848) stipulates that pigs in organic production systems must have straw bedding and must have outdoor access. Additionally, pigs in organic production systems are typically housed in larger groups [21], all of which may contribute to a higher exposure of the animals to L. monocytogenes from the environment or from other animals within the same group. On the other hand, it cannot be denied that pigs of intensive indoor farming are often exposed to prolonged social, environmental and metabolic stress [22], which may also enhance the shedding of L. monocytogenes.
A highly variable prevalence has been found in fecal samples of healthy dairy cattle ranging from ±1.9% in individual animals to ≥46% of beef herds [23]. Antibody titers to specific L. monocytogenes virulence proteins, such as listeriolysin O and internalin A, were demonstrated in 11% of 1652 healthy dairy cows in Switzerland, suggesting that contact with L. monocytogenes is relatively frequent in this animal species [24]. A large-scale longitudinal study conducted to monitor Listeria spp. in dairy farms during three consecutive seasons in Spain showed that the prevalence of L. monocytogenes was affected by season and age: a higher prevalence was observed during the winter in cattle, and cows in their second lactation had the highest probability of L. monocytogenes fecal shedding [25].
In all likelihood, the fecal shedding of L. monocytogenes by cattle depends on extraneous factors, including feedstuff contamination and season. Shedding appears to be directly associated with feeding practices. A higher prevalence of L. monocytogenes in feces has occurred in farms with contaminated feed. Generally, Listeria spp. and L. monocytogenes prevalence were higher during the indoor season compared to the pasture season [26,27]. L. monocytogenes shedding by cows on a study farm was (i) dependent on the subtype of L. monocytogenes, (ii) highly associated with silage contamination and (iii) related to animal stress [28]. Poor-quality silage with fermentation defects can have pH values that are permissive to the growth of L. monocytogenes and act as a major risk factor for listeriosis in ruminants [29]. This may also explain the seasonal shedding patterns of L. monocytogenes by ruminants [14,30,31]. Additionally, for sheep and goats, the likelihood of the isolation of L. monocytogenes was three to seven times higher in farms that relied on silage feeding compared to those without [32]. Finally, it is interesting to note that L. monocytogenes clonal complex 1 is the most prevalent clonal group associated with human listeriosis and is strongly associated with cattle and dairy products [33].
Given the general proclivity of L. monocytogenes for most vertebrates, the special association of L. monocytogenes with ruminants may be a specific host adaptation that reflects the unique conditions in the pre-fermentative ruminant fore-stomach. It is the voluminous rumen that may favor the rapid multiplication of L. monocytogenes at a pH between 6.5 and 7.2 and at body temperatures between 38.0 and 40.5 °C before confrontation with the acidic environment of the abomasum. This hypothesis is supported by findings that brief, and the low-level fecal excretion of L. monocytogenes in sheep is concomitant with a transitory asymptomatic infection after translocation from the gastrointestinal tract (GIT), with the rumen digesta serving as a reservoir. In this study, the asymptomatic carriage of L. monocytogenes in sheep was not simply a case of passive passage of the bacteria but was associated with transitory multiplication in the rumen, depending on the dose of L. monocytogenes ingested and the age of the animal [34].
Poultry, turkeys, ducks and geese can asymptomatically carry L. monocytogenes [17]. Recently, carcass rinses and cloacal swabs were reported to be positive at a level of 11 and 1.3%, respectively [35,36]. In addition, there are numerous reports about contamination rates in poultry production establishments and poultry meat and meat products. Stress, such as transport, is plausibly one important factor that exacerbates shedding and thus contributes to the contamination of production lines.
In summary, healthy domestic animals can be asymptomatic carriers of L. monocytogenes. While the prevalence of fecal shedding tends to be low, husbandry practices involving silage feeding, as well as stressors associated with housing conditions, group sizes and transport are risk factors that can increase fecal shedding.
3. Carriage of L. monocytogenes by Wild Animals
Typically, studies on wildlife shedding L. monocytogenes provide no metadata on the health status of the animals, either because it was not evaluated, because animal droppings were sampled in the absence of the animal or because the symptoms of listeriosis were difficult to spot or unknown in a species. Additionally, catch and release studies may be biased towards animals with an impaired health status that may render them more likely to be caught. This makes a classification as “asymptomatic” carriers in wild animals problematic. However, for the purpose of this review, we assume that wild animals that are fecal shedders, symptomatic or not, contribute to the distribution of L. monocytogenes in and between environments and should therefore be considered in food safety risk assessments.
A variety of birds, including pheasants, pigeons, gulls, crows, rooks and sparrows, have been shown to be asymptomatic carriers of L. monocytogenes (Table 2). A comprehensive prevalence study in Japan looked at fecal or intestinal samples from 996 birds across 18 species and found Listeria spp. in 13.4% of all samples, most commonly in samples from crows [48]. Additionally, the fecal presence of L. monocytogenes was shown in 33% of urban rooks [49]. According to Hellstrom et al. [50], feces from wild birds (mostly from gulls, pigeons and sparrows) collected in Finland exhibited an overall L. monocytogenes prevalence of 36%. Pulsotypes obtained from the birds were often similar to those collected from the food chain, suggesting a possible role of birds in the spread of L. monocytogenes strains that are relevant in the context of human infections.
Table 2.
Isolation of Listeria monocytogenes from healthy wild animals.
| Country | Animal | Target | Sample (n) | Positive (%) | Ref. |
|---|---|---|---|---|---|
| Austria/ Germany |
Red deer | L. monocytogenes | samples* (45) | 42 | [52] |
| Wild boar | (49) | 25 | |||
| Bulgaria | Birds (Riparia riparia, Motacilla flava) | L. monocytogenes | Feces (673) | 0.6 | [54] |
| Canada | Geese | L. spp. | Feces (495) | 9.5 | [55] |
| L. monocytogenes | 4.0 | ||||
| Canada | Gulls (Laurus delawarensis) | L. monocytogenes | Cloacal swabs (264) | 9.5 | [56] |
| China | Rodents | L. m | Feces (702) | 0.3 | [57] |
| L. ivanovii | 3.7 | ||||
| L. innocua | 6.7 | ||||
| China | Rodents | L. spp. | Feces (341) | 9 | [58] |
| L. monocytogenes | 3.2 | ||||
| L. innocua | 2.9 | ||||
| Finland | Birds | L. monocytogenes | Feces (212) | 36 | [50] |
| Finland/Norway | Reindeer | L. monocytogenes | Feces (470) | 3.2 | [59] |
| France | Rooks | L. monocytogenes | Feces (112) | 33 | [49] |
| L. innocua | 24 | ||||
| L. seeligeri | 8 | ||||
| Germany | Pigeons | L. monocytogenes | Feces (350) | 0.8 | [60] |
| L. innocua | 2.3 | ||||
| L. seeligeri | 0.6 | ||||
| Japan | Crows | L. monocytogenes | Feces (301) | 1.7 | [48] |
| L. innocua | 43 | ||||
| Kenya | Nile tilapia | L. monocytogenes | Muscle (167) | 1.2 | [61] |
| Poland | Red deer | L. monocytogenes | Feces (120) | 1.75 | [62] |
| Poland | Red fox, beech marten, racoon |
L. monocytogenes | Rectal swab (286) | 3.5 | [53] |
| (65) | 6.1 | ||||
| (70) | 4.3 | ||||
| Switzerland | Wild boars | L. monocytogenes | Tonsils (153) | 17 | [63] |
| Feces (153) | 1 | ||||
| USA (central New York) |
Reptiles | L. monocytogenes | Feces (17) | 12 | [64] |
| Mammals | (64) | 8 | |||
| Birds | (242) | 4.5 |
* Tonsils and content of the rumen or the stomach, liver, intestinal lymph nodes, cecum content and feces.
The carriage of L. monocytogenes in wildlife is not confined to wild birds. Table 2 shows that Listeria spp., including L. monocytogenes, have been isolated from a broad variety of mammals (e.g., deer, rodents and wild boars) and also other vertebrates such as reptiles. A Japanese study [48] that included fecal or intestinal samples from 623 wild mammals from eleven species identified Listeria spp. in 38 (6.1%) of the tested animals. The highest number of Listeria spp. isolates (16/38) were from monkeys, which resulted in a prevalence of 20.0% (16/80) in the monkey samples. A similar study conducted in Canada analyzed 268 fecal samples from a variety of animals, 112 of which were from wildlife, including deer, moose, otters and raccoons. Among these, 35 samples were positive for L. monocytogenes (29%) [51]. In samples of 45 red deer and 49 wild boars hunted in Austria and Germany during 2011/12, a total of 19 (42.2%) red deer were positive for L. monocytogenes, as were 4 (18.2%) out of 22 pooled feed samples and 12 (24.5%) boars [52]. In several samples, L. monocytogenes was isolated from the tonsils and ruminal or cecal contents without its presence in feces, implying that game can carry L. monocytogenes even if it is not detectable in their feces. The highest counts for L. monocytogenes were found in the rumen of deer and in the tonsils of boars. Pulsed-field gel electrophoresis showed a wide variety of strains, but the serotypes were predominantly 1/2a and 4b. A Polish study examining free-living carnivores as potential sources of infection [53] isolated L. monocytogenes from approximately 5% of animals, which included red foxes, beech martens and raccoons. A full set of intact virulence genes was present in 35% of the isolates; the remainder contained varying numbers and configurations of the genes.
Ready-to-eat fish and seafood products—in particular, cold smoked salmon—are frequent sources of human listeriosis [1]. The majority of cases are likely a consequence of post-harvest contamination by L. monocytogenes strains that persist in food processing facilities [65]. For farmed fish, factors such as water pollution, agricultural runoff and seagull feces are important contributing factors to the presence of L. monocytogenes in the fish and the farm environment [66]. Another alternative is the fish, such as salmon from wild catch. According to a recent Norwegian study, freshly slaughtered salmon contaminated with L. monocytogenes was a likely source for the introduction and subsequent persistence in a salmon processing plant [67]. However, fish themselves do not seem to be very susceptible to L. monocytogenes. After a gavage of L. monocytogenes into the stomachs of live salmon, they were readily cleared without pathologic changes to the animals within three days [66], and rainbow trout held in fish farms where L. monocytogenes was detected in the water were rarely positive for L. monocytogenes [68]. A recent study [61] demonstrated an increase in the L. monocytogenes contamination level in tilapia from capture (1.2%) to the domestic market (5.8%). Taken together, these data suggest that fish may become transient asymptomatic carriers of L. monocytogenes after exposure but are not likely to be long-term spreaders of the pathogen.
Reptiles [64], insects [69] and even protozoa [70] may also harbor L. monocytogenes. The ongoing trend to keep reptiles, such as snakes, turtles and geckos, as exotic pets should not go unmentioned. In Europe alone, it is estimated that more than 11 million reptiles were kept as pets in 2021 [71]. Further studies are required to assess the possible risk of infection for reptile keepers.
Lately, invading Spanish slugs (Arion vulgaris) have been implicated as vectors for L. monocytogenes [72]. Of the pooled samples of 710 slugs, 43% were positive, and 16% of them had mean counts of 405 CFU/g of slug tissue. Of 62 slugs cultured, 11% had a positive surface or mucus. Additionally, when the slugs were fed with L. monocytogenes, they shed viable bacteria in their feces for up to 22 days. Recently, ants were found to harbor L. monocytogenes sporadically, and their potential to transmit pathogenic microorganisms from contaminated environments to food has been demonstrated [69].
Overall, these data show that a wide range of vertebrates, including reptiles, birds and mammals, as well as some invertebrates, can act as carriers of L. monocytogenes and contribute to its spread between habitats through asymptomatic carriage.
4. Asymptomatic Carriage of L. monocytogenes in Humans
The fecal transmission of L. monocytogenes is not only confined to domestic and wild animals. Humans have been shown to shed L. monocytogenes intermittently, with the prevalence of fecal shedding in healthy individuals determined by cultures typically ranging below 5% (Table 3); for older studies, see [73].
Table 3.
Humans as carriers of Listeria spp.
| Country | Target | Sample (n) | Positive (%) | Reference |
|---|---|---|---|---|
| Austria | L. monocytogenes | Feces, healthy people (505) | 0.2 | [74] |
| Brazil | L. monocytogenes | Feces, pregnant women (213) | 2.4 | [79] |
| L. spp. | 7.5 | |||
| Egypt | L. monocytogenes | Hand swabs, farm workers (100) | 16 | [83] |
| L. innocua | 2 | |||
| France | hly gene | Feces (900) | 10 | [13] |
| Germany | L. monocytogenes | Feces, patients with diarrhea (1000) | 0.6 | [84] |
| L. innocua | 1.7 | |||
| Germany | L. monocytogenes | Feces, healthy people (2000) | 0.8 | [84] |
| L. innocua | 2 | |||
| Iran | L. monocytogenes | Feces (80) | 7.5 | [85] |
| Vaginal swabs (80 samples from women with at least two abortions) | 11.3 | |||
| Senegal | L. monocytogenes | Breast milk, mothers of SAM children (120) | 100 | [82] |
| Breast milk, mothers of healthy children (32) | 37.5 | |||
| Turkey | L. monocytogenes | Hand and clothes swabs, abattoir workers (70) | 5.7 | [86] |
| Turkey | L. monocytogenes | Feces (1061) | 0.9 | [87] |
| UK | L. monocytogenes | Feces, patients with gastroenteritis (171) | 1.8 | [78] |
| USA | L. monocytogenes | Feces (827) | 0.12 | [75] |
Interestingly, although low levels of carriage were found in Austria [74] and the USA [75] for healthy people, a later study in Austria compared feces from three individuals sampled over a three-year period. They found that ten (1.2%) out of 868 samples proved positive for L. monocytogenes, all of which were serotypes 1/2a and 1/2b. A closer analysis revealed that there were five independent asymptomatic exposures to the bacterium, corresponding to an average of two exposures per person per year [76]. According to the scientific opinion of the European Food Safety Authority on L. monocytogenes contamination of RTE foods and the risk for human health in the EU, there is an increasing number of clinical cases for the over 75 years of age group and female age group between 25 and 44 years old. Quantitative modeling demonstrated that more than 90% of invasive listeriosis is caused by the ingestion of RTE food containing > 2000 CFU/g and that one-third of cases are due to growth of the organism in the consumer phase [77].
Underlying medical conditions may also be a predisposing factor for the asymptomatic carriage of L. monocytogenes in humans—for instance, in patients on renal dialysis who received the H2 receptor antagonist antacid ranitidine [78]. On the other hand, the fecal prevalence of Listeria spp. or L. monocytogenes was the same between HIV-infected pregnant women receiving antiretrovirals and uninfected controls [79]. Pregnancy itself does not seem to affect the rate of human asymptomatic carriage. It was shown that 51 women in their 10–16th weeks of pregnancy had a fecal carriage rate of only 2% [80]. In comparison, the same fecal carriage was confirmed for 3.4% out of 59 nonpregnant controls. Moreover, when the fecal carriage rates in pregnant women with listeriosis were compared with matched, nonpregnant controls following an outbreak in Los Angeles, similar carriage rates were found [81]. A recent study [82] indicated that dysbiosis of breast milk microbiota may result in an increased relative abundance of L. monocytogenes in the milk of the mothers of children showing severe acute malnutrition (SAM).
A culture-independent approach based on molecular methods detected L. monocytogenes in 173/3338 (5.2%) human microbiome datasets on MG-RAST (16S sequencing) and in 90/900 (10%) stool samples from healthy individuals using PCR [13]. The interpretation of these data should bear in mind that DNA-based detection methods do not differentiate between live and dead organisms. The same study also showed a correlation between specific gut microbiota and the presence of L. monocytogenes. Interestingly, a study in mice indicated that aging may cause significant dysbiosis of the commensal microbiota, resulting in increased L. monocytogenes colonization of the gut [88]. Additionally, occupational groups encountering animals, feces and meat and those who undergo work-related exposure to the bacterium are anticipated to be at an increased risk of asymptomatic infection. For example, the cumulative prevalence of L. monocytogenes in hand swabs from farm workers and hand and clothes swabs from abattoir workers was 16% and 6%, respectively [83,86], which is higher than the average prevalence typically found in fecal samples from healthy people (Table 3).
In order to grasp the extent of L. monocytogenes exposure in the wider human community, a European Union-wide baseline survey was carried out in 2010 and 2011. All in all, 13,088 food samples were examined for the presence of L. monocytogenes. The prevalence across the entire European Union in fish samples was 10.4%, while, for meat and cheese samples, the prevalence were 2.07% and 0.47%, respectively [89].
Wagner et al. [90] sampled ready-to-eat foods in Austria. Out of 946 food samples collected from food retailers in Vienna, 124 (13.1%) and 45 (4.8%) tested positive for Listeria spp. and L. monocytogenes, respectively. Products showing the highest contamination were fish and seafood (19.4%), followed by raw meat sausages (6.3%), soft cheese (5.5%) and cooked meats (4.5%). The samples were also collected from households in the same region, and 5.6% and 1.7% out of 640 foodstuffs tested positive for Listeria spp. and L. monocytogenes, respectively. Alarmingly, the same isolates from the latter products could be detected from pooled fecal samples of household members, suggesting that even low-level contaminated foods (<100 CFU/g) may result in fecal shedding.
5. The Impact of Asymptomatic Carriers on the Presence of L. monocytogenes on Farms and in the Food Processing Environment
As discussed above, asymptomatic fecal shedding of L. monocytogenes by farm animals contributes to an increased presence of the pathogen in the farm environment with an associated risk to food and feed safety. A systems approach to food safety therefore should include a thorough analysis of the ecology of L. monocytogenes in the agricultural environment, and the identification and elimination of farm reservoirs for L. monocytogenes is a prerequisite for the implementation of farm-specific pathogen reduction programs [91]. Table 4 summarizes the recent studies that were performed in this context.
Table 4.
Listeria spp. isolated from the farm and environment.
| Country | Target | Sample (n) | Positive (%) | Ref. |
|---|---|---|---|---|
| Austria | L. spp. | Working Boots (53) | 51 | [32] |
| Floor (53) | 39.3 | |||
| L. monocytogenes | Working Boots (53) | 15.7 | ||
| Floor (53) | 7.9 | |||
| Canada | L. monocytogenes | Irrigation water (223) | 10.3 | [106] |
| Canada (Arctic region) | L. monocytogenes | Wastewater stabilization ponds (109) | 99 | [99] |
| Denmark | L. monocytogenes | Abattoir poultry (3080) | 8.0 | [107] |
| Egypt | L. monocytogenes | Water (36) | 8.3 | [37] |
| Silage (36) | 27.8 | |||
| Manure (36) | 19.4 | |||
| Soil (36) | 8.3 | |||
| Milking equipment (432) | 6.9 | |||
| Germany | L. monocytogenes | Slaughterhouse (environment and equipment, 77) | 0.9 | [20] |
| Iran | L. monocytogenes | Water (180) | 16.7 | [85] |
| Iran | L. monocytogenes | Iranian currency (108) | 0.93 | [108] |
| Jordan | L. monocytogenes | Bulk tank milk (305) | 7.5 | [43] |
| New Zealand | L. monocytogenes | Bulk tank milk (400) | 4.0 | [109] * |
| South Africa | L. monocytogenes | Roof-harvested rainwater (264) | 22 | [110] |
| Taiwan | L. monocytogenes | Abattoir environment (246) | 0 | [35] |
| USA | L. monocytogenes | Soil (555) | 15.3 | [46] |
| USA | L. spp.** | Stream water (196) | 28 | [95] |
| L. monocytogenes | 10 | |||
| USA (Colorado, wilderness area) | L. monocytogenes | Soil, water, sediment, surface soil and wildlife fecal samples (572) | 0.23 | [111] |
| L. spp. | 1.5 | |||
| USA (Idaho) | L. monocytogenes | Dairy wastewater ponds (30) | 6.7 | [112] |
| USA (New York State) | L. monocytogenes | Water (132) | 48 | [113] |
| L. innocua | 10.6 | |||
| L. monocytogenes | Feces (77) | 29 | ||
| L. innocua | 8 | |||
| USA (NYS) | L. spp. | Spinach field soil (1092) | 12 | [96] |
| L. monocytogenes | 7.8 | |||
| USA (NYS) | L. spp. | Pond/river water used for irrigation (9) | 44 | [97] |
| L. monocytogenes | 22 | |||
| USA (Virginia) | L. monocytogenes | irrigation water | [98] | |
| pond (48) | 27.1 | |||
| well (48) | 4.2 |
* Survey from November 2011 to August 2012 during which 25-mL milk samples were collected five times from each of 80 randomly selected dairy farms and tested for the presence of L. monocytogenes. ** Excluding L. monocytogenes.
We can conclude that asymptomatic fecal shedding by farm animals is linked to diet, particularly to silage [92]. The incidence of L. monocytogenes silages was reported to range from 2.5% (clamp silage) to 22.2% (large bales) and to be even higher (44%) in moldy samples [93]. L. monocytogenes is thought to initially access silage from the contamination of raw grass via soil. Insufficient acidification of the silage caused by inadequate fermentation then allows the growth of L. monocytogenes to levels that can cause disease. Surprisingly, L. monocytogenes was rarely detected on grass and vegetables prior to processing [92], which may reflect the low numbers of bacteria needed as an initial contamination. However, once plant material is contaminated, the bacteria can survive for weeks, with implications for feed safety if the grass is contaminated and food safety when the crops are contaminated [94]. Importantly, recent studies in the USA demonstrated that the use of surface water for irrigation could be a major source of contamination [95,96,97]. L. monocytogenes was found in up to 27% of the samples of pond water [98] and in up to up to 99% in the waste water of stabilization ponds in the arctic region of Canada [99]. In addition, the ability of L. monocytogenes to enter the VBNC state may contribute to adaptation, persistence and transmission between different ecological niches [11].
Besides silage, L. monocytogenes was regularly isolated from samples obtained from feed bunks, water troughs and bedding [47,100], which is consistent with its ubiquitous presence in soil and subsequent spread through feed and animals. Most interestingly, recent studies indicated that dairy farms may favor the selection of hypervirulent L. monocytogenes clones, which can then enter the food chain [4,25].
Taken together, the persistence of L. monocytogenes in the ruminant farm environment may be supported by a cycle of ingestion of L. monocytogenes with contaminated feed, multiplication in animal hosts and subsequent fecal contamination of the environment [101].
Although pigs seldom develop clinical listeriosis, pork products have consistently been linked to human infection [1,102,103]. Slaughter and processing environment contaminations have been traced back to healthy carrier pigs [104]. As for in–out or empty and clean finishing pig facilities, when the duration of the empty period prior to the introduction of growing pigs was less than one day in the fattening section, the risk of L. monocytogenes contamination was significantly increased [105]. This same group also proposed that wet feeding is a risk factor for L. monocytogenes colonization of a finishing batch, likely because of feed residue layers and biofilm formation within the pipes and valves. The prevalence of fecal shedding of L. monocytogenes in healthy swine generally increases from the farm to food manufacturing plants [91]. However, the main source for L. monocytogenes contamination in food appears to be at the slaughter and processing steps, where the bacterium can survive for very long periods [104].
Taken together, the asymptomatic shedding of humans and animals, as well as L. monocytogenes persistence in the farm environment, present a risk to animal and human health. Since L. monocytogenes may access food production facilities from these primary sources, preventative strategies at this level of the food production chain should focus on a high standard of feed and animal hygiene, sanitary milk production and good farming practices. Poor hygiene on farms, such as inattention to boot cleaning, hand washing, failure to wear protective clothing and indifference to silage quality, increases the risk of animals becoming colonized with L. monocytogenes, including the downstream risk to the human consumer.
The colonization of food processing equipment and facilities can originate from raw food sources or introduction by poor hygiene practices or fomites [114]. Persistent strains of L. monocytogenes isolated from the food processing environment show enhanced adherence with short contact times, promoting survival and possibly initiating the establishment of a strain as a “house strain” in a food processing plant [115]. Sodium chloride, which is often used in food production, induces autoaggregation and increases L. monocytogenes adhesion to plastic [114]. The same authors found that persistent strains might have a lower virulence potential than clinical strains. Others have also observed that L. monocytogenes strains responsible for persistent contamination differ from sporadic strains, but there does not seem to be any specific evolutional lineage of persistent strains [19]. Disturbingly, this lower virulence may change following exposure to disinfectants [116,117].
Asymptomatic fecal shedding of L. monocytogenes by cows can lead to the entry of L. monocytogenes into dairy processing plants via contaminated raw milk and result in persistence as disinfectant-tolerant biofilms on surfaces and the subsequent contamination of processed products [101]. While L. monocytogenes is killed by short-term, high-temperature pasteurization, it can survive and thrive in post-pasteurization processing environments and thereby recontaminate dairy products [118,119,120]. The unique growth and survival properties of L. monocytogenes and its ability to adhere to surfaces contribute to the difficulty of eliminating it entirely [121].
In a poultry processing facility in Northern Ireland, a particular genotype of L. monocytogenes, considered to originate from incoming birds and prevalent in the raw meat processing area, was found to be widespread on food contact surfaces, floors and drains [122]. One year later, the strains isolated from cooked poultry products and the cooked poultry-processing environment contained only that genotype, plus one other, common to both raw and cooked meat areas. This highlights the potential for persistent strains to cross-contaminate processed foods in the same facility.
6. Future Implications
Since it is evident that animals and humans can persistently carry L. monocytogenes and thereby act as a source for the contamination of processed food, control measures must begin on the farm and include humans, animals and the environment in a one-health approach. An awareness of asymptomatic carriage should inform hygiene regulations with respect to the animal and food handlers at all stages of food production. In the farm context, proactive farm hygiene practices to lower the bacterial burden on crops and in animal feed can reduce the root causes of L. monocytogenes access to animal and human hosts. In particular, sewage handling and irrigation techniques for crops should take into account the possibility of spreading L. monocytogenes to growing plants. Attention to feed hygiene and to correct fermentation during silage production helps interrupt the cycle between the shedding of L. monocytogenes from asymptomatic ruminant carriers to grass via manure and the subsequent colonization of more animals from contaminated feed.
Meaningful preventive measures include the adequate compartmentalizing of the raw food processing steps, the critical rethinking of the need for silage feeding, avoiding irrigation close to the harvest, the scrupulous cleanliness of food contact surfaces and equipment, the strict personal hygiene of food handlers and regular monitoring for the persistent colonization of the food processing environment with L. monocytogenes.
Author Contributions
Conceptualization, D.S., E.M. and C.G.; writing—original draft preparation, D.S., E.M. and C.G. and writing—review and editing, D.S., E.M. and C.G. All authors have read and agreed to the published version of the manuscript.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Anonymous. The European Union One Health 2020 Zoonoses Report. EFSA J. 2021;19:e06971. doi: 10.2903/j.efsa.2021.6971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Haase J.K., Didelot X., Lecuit M., Korkeala H., Group L.m.M.S., Achtman M. The ubiquitous nature of Listeria monocytogenes clones: A large-scale Multilocus Sequence Typing study. Environ. Microbiol. 2014;16:405–416. doi: 10.1111/1462-2920.12342. [DOI] [PubMed] [Google Scholar]
- 3.Belias A., Sullivan G., Wiedmann M., Ivanek R. Factors that contribute to persistent Listeria in food processing facilities and relevant interventions: A rapid review. Food Control. 2022;133:108579. doi: 10.1016/j.foodcont.2021.108579. [DOI] [Google Scholar]
- 4.Maury M.M., Bracq-Dieye H., Huang L., Vales G., Lavina M., Thouvenot P., Disson O., Leclercq A., Brisse S., Lecuit M. Hypervirulent Listeria monocytogenes clones’ adaption to mammalian gut accounts for their association with dairy products. Nat. Commun. 2019;10:2488. doi: 10.1038/s41467-019-10380-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Harrand A.S., Jagadeesan B., Baert L., Wiedmann M., Orsi R.H. Evolution of Listeria monocytogenes in a Food Processing Plant Involves Limited Single-Nucleotide Substitutions but Considerable Diversification by Gain and Loss of Prophages. Appl. Environ. Microbiol. 2020;86:e02493-19. doi: 10.1128/AEM.02493-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schlech W.F., Fischetti V.A., Novick R.P., Ferretti J.J., Portnoy D.A., Miriam Braunstein M., Rood J.I. Epidemiology and Clinical Manifestations of Listeria monocytogenes Infection. Microbiol. Spectr. 2019;7:3. doi: 10.1128/microbiolspec.GPP3-0014-2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Olier M., Garmyn D., Rousseaux S., Lemaître J.P., Piveteau P., Guzzo J. Truncated Internalin A and Asymptomatic Listeria monocytogenes Carriage: In Vivo Investigation by Allelic Exchange. Infect. Immun. 2005;73:644–648. doi: 10.1128/IAI.73.1.644-648.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nightingale K.K., Windham K., Martin K.E., Yeung Y., Wiedmann M. Select Listeria monocytogenes Subtypes Commonly Found in Foods Carry Distinct Nonsense Mutations in inlA, Leading to Expression of Truncated and Secreted Internalin A, and Are Associated with a Reduced Invasion Phenotype for Human Intestinal Epithelial Cells. Appl. Environ. Microbiol. 2005;71:8764–8772. doi: 10.1128/AEM.71.12.8764-8772.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Maury M.M., Tsai Y.H., Charlier C., Touchon M., Chenal-Francisque V., Leclercq A., Criscuolo A., Gaultier C., Roussel S., Brisabois A., et al. Uncovering Listeria monocytogenes hypervirulence by harnessing its biodiversity. Nat. Genet. 2016;48:308–313. doi: 10.1038/ng.3501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Besnard V., Federighi M., Declerq E., Jugiau F., Cappelier J.M. Environmental and physico-chemical factors induce VBNC state in Listeria monocytogenes. Vet. Res. 2002;33:359–370. doi: 10.1051/vetres:2002022. [DOI] [PubMed] [Google Scholar]
- 11.Lotoux A., Milohanic E., Bierne H. The Viable But Non-Culturable State of Listeria monocytogenes in the One-Health Continuum. Front. Cell. Infect. Microbiol. 2022;12:849915. doi: 10.3389/fcimb.2022.849915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fleischmann S., Robben C., Alter T., Rossmanith P., Mester P. How to Evaluate Non-Growing Cells—Current Strategies for Determining Antimicrobial Resistance of VBNC Bacteria. Antibiotics. 2021;10:115. doi: 10.3390/antibiotics10020115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hafner L., Pichon M., Burucoa C., Nusser S.H.A., Moura A., Garcia-Garcera M., Lecuit M. Listeria monocytogenes faecal carriage is common and depends on the gut microbiota. Nat. Commun. 2021;12:6826. doi: 10.1038/s41467-021-27069-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ho A.J., Ivanek R., Grohn Y.T., Nightingale K.K., Wiedmann M. Listeria monocytogenes fecal shedding in dairy cattle shows high levels of day-to-day variation and includes outbreaks and sporadic cases of shedding of specific L. monocytogenes subtypes. Prev. Vet. Med. 2007;80:287–305. doi: 10.1016/j.prevetmed.2007.03.005. [DOI] [PubMed] [Google Scholar]
- 15.Wilkes G., Edge T.A., Gannon V.P.J., Jokinen C., Lyautey E., Neumann N.F., Ruecker N., Scott A., Sunohara M., Topp E., et al. Associations among pathogenic bacteria, parasites, and environmental and land use factors in multiple mixed-use watersheds. Water Res. 2011;45:5807–5825. doi: 10.1016/j.watres.2011.06.021. [DOI] [PubMed] [Google Scholar]
- 16.Lyautey E., Lapen D.R., Wilkes G., McCleary K., Pagotto F., Tyler K., Hartmann A., Piveteau P., Rieu A., Robertson W.J., et al. Distribution and characteristics of Listeria monocytogenes isolates from surface waters of the South Nation River watershed, Ontario, Canada. Appl. Environ. Microbiol. 2007;73:5401–5410. doi: 10.1128/AEM.00354-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schoder D., Wagner M. Growing awareness of asymptomatic carriage of Listeria monocytogenes. Wien. Tierarztl. Mon. 2012;99:322–329. [Google Scholar]
- 18.van Bree F.P.J., Bokken G.C.A.M., Mineur R., Franssen F., Opsteegh M., van der Giessen J.W.B., Lipman L.J.A., Overgaauw P.A.M. Zoonotic bacteria and parasites found in raw meat-based diets for cats and dogs. Vet. Rec. 2018;182:50. doi: 10.1136/vr.104535. [DOI] [PubMed] [Google Scholar]
- 19.Autio T., Markkula A., Hellstrom S., Niskanen T., Lunden J., Korkeala H. Prevalence and genetic diversity of Listeria monocytogenes in the tonsils of pigs. J. Food Prot. 2004;67:805–808. doi: 10.4315/0362-028X-67.4.805. [DOI] [PubMed] [Google Scholar]
- 20.Oswaldi V., Luth S., Dzierzon J., Meemken D., Schwarz S., Fessler A.T., Felix B., Langforth S. Distribution and Characteristics of Listeria spp. in Pigs and Pork Production Chains in Germany. Microorganisms. 2022;10:512. doi: 10.3390/microorganisms10030512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hellstrom S., Laukkanen R., Siekkinen K.M., Ranta J., Maijala R., Korkeala H. Listeria monocytogenes contamination in pork can originate from farms. J. Food Prot. 2010;73:641–648. doi: 10.4315/0362-028X-73.4.641. [DOI] [PubMed] [Google Scholar]
- 22.Martínez-Miró S., Tecles F., Ramón M., Escribano D., Hernández F., Madrid J., Orengo J., Martínez-Subiela S. Causes, consequences and biomarkers of stress in swine: An update. BMC Vet. Res. 2016;12:171. doi: 10.1186/s12917-016-0791-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hurtado A., Ocejo M., Oporto B. Salmonella spp. and Listeria monocytogenes shedding in domestic ruminants and characterization of potentially pathogenic strains. Vet. Microbiol. 2017;210:71–76. doi: 10.1016/j.vetmic.2017.09.003. [DOI] [PubMed] [Google Scholar]
- 24.Boerlin P., Boerlin-Petzold F., Jemmi T. Use of listeriolysin O and internalin A in a seroepidemiological study of listeriosis in Swiss dairy cows. J. Clin. Microbiol. 2003;41:1055–1061. doi: 10.1128/JCM.41.3.1055-1061.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Palacios-Gorba C., Moura A., Gomis J., Leclercq A., Gomez-Martin A., Bracq-Dieye H., Moce M.L., Tessaud-Rita N., Jimenez-Trigos E., Vales G., et al. Ruminant-associated Listeria monocytogenes isolates belong preferentially to dairy-associated hypervirulent clones: A longitudinal study in 19 farms. Environ. Microbiol. 2021;23:7617–7631. doi: 10.1111/1462-2920.15860. [DOI] [PubMed] [Google Scholar]
- 26.Husu J.R. Epidemiological studies on the occurrence of Listeria monocytogenes in the feces of dairy cattle. Zent. Vet. B. 1990;37:276–282. doi: 10.1111/j.1439-0450.1990.tb01059.x. [DOI] [PubMed] [Google Scholar]
- 27.Husu J.R., Seppanen J.T., Sivela S.K., Rauramaa A.L. Contamination of raw milk by Listeria monocytogenes on dairy farms. Zent. Vet. B. 1990;37:268–275. doi: 10.1111/j.1439-0450.1990.tb01058.x. [DOI] [PubMed] [Google Scholar]
- 28.Ivaneka R., Grohn Y.T., Ho A.J.J., Wiedmann M. Markov chain approach to analyze the dynamics of pathogen fecal shedding—Example of Listeria monocytogenes shedding in a herd of dairy cattle. J. Theor. Biol. 2007;245:44–58. doi: 10.1016/j.jtbi.2006.09.031. [DOI] [PubMed] [Google Scholar]
- 29.Vilar M.J., Yus E., Sanjuán M.L., Diéguez F.J., Rodríguez-Otero J.L. Prevalence of and Risk Factors for Listeria Species on Dairy Farms. J. Dairy Sci. 2007;90:5083–5088. doi: 10.3168/jds.2007-0213. [DOI] [PubMed] [Google Scholar]
- 30.Nightingale K.K., Fortes E.D., Ho A.J., Schukken Y.H., Grohn Y.T., Wiedmann M. Evaluation of farm management practices as risk factors for clinical listeriosis and fecal shedding of Listeria monocytogenes in ruminants. J. Am. Vet. Med. Assoc. 2005;227:1808–1814. doi: 10.2460/javma.2005.227.1808. [DOI] [PubMed] [Google Scholar]
- 31.Nightingale K.K., Schukken Y.H., Nightingale C.R., Fortes E.D., Ho A.J., Her Z., Grohn Y.T., McDonough P.L., Wiedmann M. Ecology and transmission of Listeria monocytogenes infecting ruminants and in the farm environment. Appl. Environ. Microbiol. 2004;70:4458–4467. doi: 10.1128/AEM.70.8.4458-4467.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schoder D., Melzner D., Schmalwieser A., Zangana A., Winter P., Wagner M. Important vectors for Listeria monocytogenes transmission at farm dairies manufacturing fresh sheep and goat cheese from raw milk. J. Food Prot. 2011;74:919–924. doi: 10.4315/0362-028X.JFP-10-534. [DOI] [PubMed] [Google Scholar]
- 33.Moura A., Lefrancq N., Wirth T., Leclercq A., Borges V., Gilpin B., Dallman T.J., Frey J., Franz E., Nielsen E.M., et al. Emergence and global spread of Listeria monocytogenes main clinical clonal complex. Sci. Adv. 2021;7:eabj9805. doi: 10.1126/sciadv.abj9805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zundel E., Bernard S. Listeria monocytogenes translocates throughout the digestive tract in asymptomatic sheep. J. Med. Microbiol. 2006;55:1717–1723. doi: 10.1099/jmm.0.46709-0. [DOI] [PubMed] [Google Scholar]
- 35.Lin C.H., Adams P.J., Huang J.F., Sun Y.F., Lin J.H., Robertson I.D. Contamination of chicken carcasses and the abattoir environment with Listeria monocytogenes in Taiwan. Br. Poult. Sci. 2021;62:701–709. doi: 10.1080/00071668.2021.1927984. [DOI] [PubMed] [Google Scholar]
- 36.Pohjola L., Nykäsenoja S., Kivistö R., Soveri T., Huovilainen A., Hänninen M.L., Fredriksson-Ahomaa M. Zoonotic Public Health Hazards in Backyard Chickens. Zoonoses Public Health. 2016;63:420–430. doi: 10.1111/zph.12247. [DOI] [PubMed] [Google Scholar]
- 37.Elsayed M.M., Elkenany R.M., Zakaria A.I., Badawy B.M. Epidemiological study on Listeria monocytogenes in Egyptian dairy cattle farms’ insights into genetic diversity of multi-antibiotic-resistant strains by ERIC-PCR. Environ. Sci. Pollut. Res. 2022;29:54359–54377. doi: 10.1007/s11356-022-19495-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Weber A., Potel J., SchaferSchmidt R., Prell A., Datzmann C. Investigations on the occurrence of Listeria monocytogenes in fecal samples of domestic and companion animals. Zent. Hyg. Umw. 1995;198:117–123. [PubMed] [Google Scholar]
- 39.Oswaldi V., Dzierzon J., Thieme S., Merle R., Meemken D. Slaughter pigs as carrier of Listeria monocytogenes in Germany. J. Consum. Prot. Food Saf. 2021;16:109–115. doi: 10.1007/s00003-021-01322-4. [DOI] [Google Scholar]
- 40.Adorisio E., Tassone D.D., Conte A., Annicchiarico L.S. Lysteria monocytogenes in samples of swines sent to the human alimentary chain. Ann. Ig. Med. Prev. Comunita. 2003;15:575–581. [PubMed] [Google Scholar]
- 41.Iida T., Kanzaki M., Maruyama T., Inoue S., Kaneuchi C. Prevalence of Listeria monocytogenes in intestinal contents of healthy animals in japan. J. Vet. Med. Sci. 1991;53:873–875. doi: 10.1292/jvms.53.873. [DOI] [PubMed] [Google Scholar]
- 42.Hasegawa M., Iwabuchi E., Yamamoto S., Muramatsu M., Takashima I., Hirai K. Prevalence and characteristics of Listeria monocytogenes in feces of black beef cattle reared in three geographically distant areas in Japan. Foodborne Pathog. Dis. 2014;11:96–103. doi: 10.1089/fpd.2013.1616. [DOI] [PubMed] [Google Scholar]
- 43.Obaidat M.M., Stringer A.P. Prevalence, molecular characterization, and antimicrobial resistance profiles of Listeria monocytogenes, Salmonella enterica, and Escherichia coli O157:H7 on dairy cattle farms in Jordan. J. Dairy Sci. 2019;102:8710–8720. doi: 10.3168/jds.2019-16461. [DOI] [PubMed] [Google Scholar]
- 44.Stipetic K., Chang Y.C., Peters K., Salem A., Doiphode S.H., McDonough P.L., Chang Y.F., Sultan A., Mohammed H.O. The risk of carriage of Salmonella spp. and Listeria monocytogenes in food animals in dynamic populations. Vet. Med. Sci. 2016;2:246–254. doi: 10.1002/vms3.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bandelj P., Jamnikar-Ciglenecki U., Ocepek M., Blagus R., Vengust M. Risk factors associated with fecal shedding of Listeria monocytogenes by dairy cows and calves. J. Vet. Intern. Med. 2018;32:1773–1779. doi: 10.1111/jvim.15234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Locatelli A., Lewis M.A., Rothrock M.J., Jr. The Distribution of Listeria in Pasture-Raised Broiler Farm Soils Is Potentially Related to University of Vermont Medium Enrichment Bias toward Listeria innocua over Listeria monocytogenes. Front. Vet. Sci. 2017;4:227. doi: 10.3389/fvets.2017.00227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mohammed H.O., Stipetic K., McDonough P.L., Gonzalez R.N., Nydam D.V., Atwill E.R. Identification of potential on-farm sources of Listeria monocytogenes in herds of dairy cattle. Am. J. Vet. Res. 2009;70:383–388. doi: 10.2460/ajvr.70.3.383. [DOI] [PubMed] [Google Scholar]
- 48.Yoshida T., Sugimoto T., Sato M., Hirai K. Incidence of Listeria monocytogenes in wild animals in Japan. J. Vet. Med. Sci. 2000;62:673–675. doi: 10.1292/jvms.62.673. [DOI] [PubMed] [Google Scholar]
- 49.Bouttefroy A., Lemaitre J.P., Rousset A. Prevalence of Listeria sp. in droppings from urban rooks (Corvus frugilegus) J. Appl. Microbiol. 1997;82:641–647. doi: 10.1111/j.1365-2672.1997.tb02874.x. [DOI] [PubMed] [Google Scholar]
- 50.Hellstrom S., Kiviniemi K., Autio T., Korkeala H. Listeria monocytogenes is common in wild birds in Helsinki region and genotypes are frequently similar with those found along the food chain. J. Appl. Microbiol. 2008;104:883–888. doi: 10.1111/j.1365-2672.2007.03604.x. [DOI] [PubMed] [Google Scholar]
- 51.Lyautey E., Hartmann A., Pagotto F., Tyler K., Lapen D.R., Wilkes G., Piveteau P., Rieu A., Robertson W.J., Medeiros D.T., et al. Characteristics and frequency of detection of fecal Listeria monocytogenes shed by livestock, wildlife, and humans. Can. J. Microbiol. 2007;53:1158–1167. doi: 10.1139/W07-084. [DOI] [PubMed] [Google Scholar]
- 52.Weindl L., Frank E., Ullrich U., Heurich M., Kleta S., Ellerbroek L., Gareis M. Listeria monocytogenes in Different Specimens from Healthy Red Deer and Wild Boars. Foodborne Pathog. Dis. 2016;13:391–397. doi: 10.1089/fpd.2015.2061. [DOI] [PubMed] [Google Scholar]
- 53.Nowakiewicz A., Zieba P., Ziolkowska G., Gnat S., Muszynska M., Tomczuk K., Dziedzic B.M., Ulbrych L., Troscianczyk A. Free-Living Species of Carnivorous Mammals in Poland: Red Fox, Beech Marten, and Raccoon as a Potential Reservoir of Salmonella, Yersinia, Listeria spp. and Coagulase-Positive Staphylococcus. PLoS ONE. 2016;11:e0155533. doi: 10.1371/journal.pone.0155533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Najdenski H., Dimova T., Zaharieva M.M., Nikolov B., Petrova-Dinkova G., Dalakchieva S., Popov K., Hristova-Nikolova I., Zehtindjiev P., Peev S., et al. Migratory birds along the Mediterranean–Black Sea Flyway as carriers of zoonotic pathogens. Can. J. Microbiol. 2018;64:915–924. doi: 10.1139/cjm-2017-0763. [DOI] [PubMed] [Google Scholar]
- 55.Gorham T.J., Lee J. Pathogen Loading From Canada Geese Faeces in Freshwater: Potential Risks to Human Health Through Recreational Water Exposure. Zoonoses Public Health. 2016;63:177–190. doi: 10.1111/zph.12227. [DOI] [PubMed] [Google Scholar]
- 56.Quessy S., Messier S. Prevalence of Salmonella spp., Campylobacter spp. and Listeria spp. in ring-billed gulls (Larus delawarensis) J. Wildl. Dis. 1992;28:526–531. doi: 10.7589/0090-3558-28.4.526. [DOI] [PubMed] [Google Scholar]
- 57.Cao X., Wang Y., Wang Y., Li H., Luo L., Wang P., Zhang L., Li H., Liu J., Lu L., et al. Prevalence and Characteristics of Listeria ivanovii Strains in Wild Rodents in China. Vector-Borne Zoonotic Dis. 2019;19:8–15. doi: 10.1089/vbz.2018.2317. [DOI] [PubMed] [Google Scholar]
- 58.Wang Y., Lu L., Lan R., Salazar J.K., Liu J., Xu J., Ye C. Isolation and characterization of Listeria species from rodents in natural environments in China. Emerg. Microbes Infect. 2017;6:e44. doi: 10.1038/emi.2017.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Laaksonen S., Oksanen A., Julmi J., Zweifel C., Fredriksson-Ahomaa M., Stephan R. Presence of foodborne pathogens, extended-spectrum beta-lactamase -producing Enterobacteriaceae, and methicillin-resistant Staphylococcus aureus in slaughtered reindeer in northern Finland and Norway. Acta Vet. Scand. 2017;59:2. doi: 10.1186/s13028-016-0272-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Weber A., Potel J., Schafer-Schmidt R. The occurrence of Listeria monocytogenes in fecal samples of pigeons. Berl. Und Muenchener Tieraerztliche Wochenschr. 1995;108:26–27. [PubMed] [Google Scholar]
- 61.Onjong H.A., Ngayo M.O., Mwaniki M., Wambui J., Njage P.M.K. Microbiological Safety of Fresh Tilapia (Oreochromis niloticus) from Kenyan Fresh Water Fish Value Chains. J. Food Prot. 2018;81:1973–1981. doi: 10.4315/0362-028X.JFP-18-078. [DOI] [PubMed] [Google Scholar]
- 62.Gnat S., Troscianczyk A., Nowakiewicz A., Majer-Dziedzic B., Ziolkowska G., Dziedzic R., Zieba P., Teodorowski O. Experimental studies of microbial populations and incidence of zoonotic pathogens in the faeces of red deer (Cervus elaphus) Lett. Appl. Microbiol. 2015;61:446–452. doi: 10.1111/lam.12471. [DOI] [PubMed] [Google Scholar]
- 63.Wacheck S., Fredriksson-Ahomaa M., Konig M., Stolle A., Stephan R. Wild boars as an important reservoir for foodborne pathogens. Foodborne Pathog. Dis. 2010;7:307–312. doi: 10.1089/fpd.2009.0367. [DOI] [PubMed] [Google Scholar]
- 64.Chen T., Orsi R.H., Chen R., Gunderson M., Roof S., Wiedmann M., Childs-Sanford S.E., Cummings K.J. Characterization of Listeria monocytogenes isolated from wildlife in central New York. Vet. Med. Sci. 2022;8:1319–1329. doi: 10.1002/vms3.758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Ferreira V., Wiedmann M., Teixeira P., Stasiewicz M.J. Listeria monocytogenes persistence in food-associated environments: Epidemiology, strain characteristics, and implications for public health. J. Food Prot. 2014;77:150–170. doi: 10.4315/0362-028X.JFP-13-150. [DOI] [PubMed] [Google Scholar]
- 66.Hsu J.-L., Opitz H.M., Bayer R.C., Kling L.J., Halteman W.A., Martin R.E., Slabyj B.M. Listeria monocytogenes in an Atlantic Salmon (Salmo salar) Processing Environment. J. Food Prot. 2005;68:1635–1640. doi: 10.4315/0362-028X-68.8.1635. [DOI] [PubMed] [Google Scholar]
- 67.Fagerlund A., Wagner E., Møretrø T., Heir E., Moen B., Rychli K., Langsrud S. Pervasive Listeria monocytogenes Is Common in the Norwegian Food System and Is Associated with Increased Prevalence of Stress Survival and Resistance Determinants. Appl. Environ. Microbiol. 2022;88:e0086122. doi: 10.1128/aem.00861-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Miettinen H., Wirtanen G. Ecology of Listeria spp. in a fish farm and molecular typing of Listeria monocytogenes from fish farming and processing companies. Int. J. Food Microbiol. 2006;112:138–146. doi: 10.1016/j.ijfoodmicro.2006.06.016. [DOI] [PubMed] [Google Scholar]
- 69.Simothy L., Mahomoodally F., Neetoo H. A study on the potential of ants to act as vectors of foodborne pathogens. AIMS Microbiol. 2018;4:319–333. doi: 10.3934/microbiol.2018.2.319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Pushkareva V.I., Ermolaeva S.A. Listeria monocytogenes virulence factor Listeriolysin O favors bacterial growth in co-culture with the ciliate Tetrahymena pyriformis, causes protozoan encystment and promotes bacterial survival inside cysts. BMC Microbiol. 2010;10:26. doi: 10.1186/1471-2180-10-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Statista GmbH Anzahl der Reptilien in Europa Nach Ländern im Jahr 2021. [(accessed on 7 October 2022)]. Available online: https://de.statista.com/statistik/daten/studie/454104/umfrage/reptilien-in-europa-nach-laendern/
- 72.Gismervik K., Aspholm M., Rorvik L.M., Bruheim T., Andersen A., Skaar I. Invading slugs (Arion vulgaris) can be vectors for Listeria monocytogenes. J. Appl. Microbiol. 2015;118:809–816. doi: 10.1111/jam.12750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Schuchat A., Swaminathan B., Broome C.V. Epidemiology of human listeriosis. Clin. Microbiol. Rev. 1991;4:169–183. doi: 10.1128/CMR.4.2.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Grif K., Hein I., Wagner M., Brandl E., Mpamugo O., McLauchlin J., Dierich M.P., Allerberger F. Prevalence and characterization of Listeria monocytogenes in the feces of healthy Austrians. Wien. Klin. Wochenschr. 2001;113:737–742. [PubMed] [Google Scholar]
- 75.Sauders B.D., Pettit D., Currie B., Suits P., Evans A., Stellrecht K., Dryja D.M., Slate D., Wiedmann M. Low prevalence of Listeria monocytogenes in human stool. J. Food Prot. 2005;68:178–181. doi: 10.4315/0362-028X-68.1.178. [DOI] [PubMed] [Google Scholar]
- 76.Grif K., Patscheider G., Dierich M.P., Allerberger F. Incidence of fecal carriage of Listeria monocytogenes in three healthy volunteers: A one-year prospective stool survey. Eur. J. Clin. Microbiol. Infect. Dis. 2003;22:16–20. doi: 10.1007/s10096-002-0835-9. [DOI] [PubMed] [Google Scholar]
- 77.EFSA Panelon Biological Hazards (BIOHAZ) Ricci A., Allende A., Bolton D., Chemaly M., Davies R., Fernández Escámez P.S., Girones R., Herman L., Koutsoumanis K., et al. Listeria monocytogenes contamination of ready-to-eat foods and the risk for human health in the EU. EFSA J. 2018;16:e05134. doi: 10.2903/j.efsa.2018.5134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.MacGowan A.P., Marshall R.J., MacKay I.M., Reeves D.S. Listeria faecal carriage by renal transplant recipients, haemodialysis patients and patients in general practice: Its relation to season, drug therapy, foreign travel, animal exposure and diet. Epidemiol. Infect. 1991;106:157–166. doi: 10.1017/S0950268800056521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Freitag I.G.R., de Castro Lisboa Pereira R., Machado E.S., Hofer E., Vallim D.C., Hofer C.B. Prevalence of Listeria monocytogenes fecal carriers in HIV-infected and -uninfected pregnant women from Brazil. Braz. J. Microbiol. 2021;52:2081–2084. doi: 10.1007/s42770-021-00583-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Lamont R.J., Postlethwaite R. Carriage of Listeria monocytogenes and related species in pregnant and non-pregnant women in Aberdeen, Scotland. J. Infect. 1986;13:187–193. doi: 10.1016/S0163-4453(86)93121-X. [DOI] [PubMed] [Google Scholar]
- 81.Mascola L., Ewert D.P., Eller A. Listeriosis: A previously unreported medical complication in women with multiple gestations. Am. J. Obstet. Gynecol. 1994;170:1328–1332. doi: 10.1016/S0002-9378(94)70151-2. [DOI] [PubMed] [Google Scholar]
- 82.Sarr M., Alou M.T., Delerce J., Khelaifia S., Diagne N., Diallo A., Bassene H., Bréchard L., Bossi V., Mbaye B., et al. A Listeria monocytogenes clone in human breast milk associated with severe acute malnutrition in West Africa: A multicentric case-controlled study. PLoS Negl. Trop. Dis. 2021;15:e0009555. doi: 10.1371/journal.pntd.0009555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Tahoun A., Abou Elez R.M.M., Abdelfatah E.N., Elsohaby I., El-Gedawy A.A., Elmoslemany A.M. Listeria monocytogenes in raw milk, milking equipment and dairy workers: Molecular characterization and antimicrobial resistance patterns. J. Glob. Antimicrob. Resist. 2017;10:264–270. doi: 10.1016/j.jgar.2017.07.008. [DOI] [PubMed] [Google Scholar]
- 84.Muller H.E. Listeria isolations from feces of patients with diarrhea and from healthy food handlers. Infection. 1990;18:97–99. doi: 10.1007/BF01641423. [DOI] [PubMed] [Google Scholar]
- 85.Meghdadi H., Khosravi A.D., Sheikh A.F., Alami A., Nassirabady N. Isolation and characterization of Listeria monocytogenes from environmental and clinical sources by culture and PCR-RFLP methods. Iran. J. Microbiol. 2019;11:7–12. doi: 10.18502/ijm.v11i1.697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Akkaya L., Alisarli M., Cetinkaya Z., Kara R., Telli R. Occurrence of Escherichia coli O157: H7/O157, Listeria monocytogenes and Salmonella spp. in beef slaughterhouse environments, equipment and workers. J. Muscle. Foods. 2008;19:261–274. doi: 10.1111/j.1745-4573.2008.00108.x. [DOI] [Google Scholar]
- 87.Pala K., Oezakin C., Akis N., Sinirtas M., Gedikoglu S., Aytekin H. Asymptomatic carriage of bacteria in food workers in Nilufer district, Bursa, Turkey. Turk. J. Med. Sci. 2010;40:133–139. doi: 10.3906/sag-0811-12. [DOI] [Google Scholar]
- 88.Alam M.S., Gangiredla J., Hasan N.A., Barnaba T., Tartera C. Aging-Induced Dysbiosis of Gut Microbiota as a Risk Factor for Increased Listeria monocytogenes Infection. Front. Immunol. 2021;12:672353. doi: 10.3389/fimmu.2021.672353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.European Food Safety Authority Analysis of the baseline survey on the prevalence of Listeria monocytogenes in certain ready-to-eat (RTE) foods in the EU, 2010-2011 Part A: Listeria monocytogenes prevalence estimates. EFSA J. 2013;11:3241. doi: 10.2903/j.efsa.2013.3241. [DOI] [Google Scholar]
- 90.Wagner M., Auer B., Trittremmel C., Hein I., Schoder D. Survey on the Listeria contamination of ready-to-eat food products and household environments in Vienna, Austria. Zoonoses Public Health. 2007;54:16–22. doi: 10.1111/j.1863-2378.2007.00982.x. [DOI] [PubMed] [Google Scholar]
- 91.Esteban J.I., Oporto B., Aduriz G., Juste R.A., Hurtado A. Faecal shedding and strain diversity of Listeria monocytogenes in healthy ruminants and swine in Northern Spain. BMC Vet. Res. 2009;5:2. doi: 10.1186/1746-6148-5-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Fenlon D.R., Wilson J., Donachie W. The incidence and level of Listeria monocytogenes contamination of food sources at primary production and initial processing. J. Appl. Bacteriol. 1996;81:641–650. doi: 10.1111/j.1365-2672.1996.tb03559.x. [DOI] [PubMed] [Google Scholar]
- 93.Fenlon D.R. Wild birds and silage as reservoirs of Listeria in the agricultural environment. J. Appl. Bacteriol. 1985;59:537–543. doi: 10.1111/j.1365-2672.1985.tb03357.x. [DOI] [PubMed] [Google Scholar]
- 94.Honjoh K., Iwazako Y., Lin Y., Kijima N., Miyamoto T. Possibilities for Contamination of Tomato Fruit by Listeria monocytogenes during Cultivation. Food Sci. Technol. Res. 2016;22:349–357. doi: 10.3136/fstr.22.349. [DOI] [Google Scholar]
- 95.Weller D., Belias A., Green H., Roof S., Wiedmann M. Landscape, Water Quality, and Weather Factors Associated With an Increased Likelihood of Foodborne Pathogen Contamination of New York Streams Used to Source Water for Produce Production. Front. Sustain. Food Syst. 2020;3:124. doi: 10.3389/fsufs.2019.00124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Weller D., Wiedmann M., Strawn L.K. Spatial and Temporal Factors Associated with an Increased Prevalence of Listeria monocytogenes in Spinach Fields in New York State. Appl. Environ. Microbiol. 2015;81:6059–6069. doi: 10.1128/AEM.01286-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Weller D., Wiedmann M., Strawn L.K. Irrigation Is Significantly Associated with an Increased Prevalence of Listeria monocytogenes in Produce Production Environments in New York State. J. Food Prot. 2015;78:1132–1141. doi: 10.4315/0362-028X.JFP-14-584. [DOI] [PubMed] [Google Scholar]
- 98.Gu G., Strawn L.K., Ottesen A.R., Ramachandran P., Reed E.A., Zheng J., Boyer R.R., Rideout S.L. Correlation of Salmonella enterica and Listeria monocytogenes in Irrigation Water to Environmental Factors, Fecal Indicators, and Bacterial Communities. Front. Microbiol. 2020;11:557289. doi: 10.3389/fmicb.2020.557289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Huang Y., Hansen L.T., Ragush C.M., Jamieson R.C. Disinfection and removal of human pathogenic bacteria in arctic waste stabilization ponds. Environ. Sci. Pollut. Res. Int. 2018;25:32881–32893. doi: 10.1007/s11356-017-8816-9. [DOI] [PubMed] [Google Scholar]
- 100.Walland J., Lauper J., Frey J., Imhof R., Stephan R., Seuberlich T., Oevermann A. Listeria monocytogenes infection in ruminants: Is there a link to the environment, food and human health? A review. Schweiz Arch. Tierheilkd. 2015;157:319–328. doi: 10.17236/sat00022. [DOI] [PubMed] [Google Scholar]
- 101.Oliver S.P., Jayarao B.M., Almeida R.A. Foodborne pathogens in milk and the dairy farm environment: Food safety and public health implications. Foodborne Pathog. Dis. 2005;2:115–129. doi: 10.1089/fpd.2005.2.115. [DOI] [PubMed] [Google Scholar]
- 102.de Valk H., Vaillant V., Jacquet C., Rocourt J., Le Querrec F., Stainer F., Quelquejeu N., Pierre O., Pierre V., Desenclos J.C., et al. Two consecutive nationwide outbreaks of Listeriosis in France, October 1999-February 2000. Am. J. Epidemiol. 2001;154:944–950. doi: 10.1093/aje/154.10.944. [DOI] [PubMed] [Google Scholar]
- 103.McLauchlin J., Hall S.M., Velani S.K., Gilbert R.J. Human listeriosis and pate: A possible association. BMJ. 1991;303:773–775. doi: 10.1136/bmj.303.6805.773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Giovannacci I., Ragimbeau C., Queguiner S., Salvat G., Vendeuvre J.L., Carlier V., Ermel G. Listeria monocytogenes in pork slaughtering and cutting plants: Use of RAPD, PFGE and PCR-REA for tracing and molecular epidemiology. Int. J. Food Microbiol. 1999;53:127–140. doi: 10.1016/S0168-1605(99)00141-5. [DOI] [PubMed] [Google Scholar]
- 105.Beloeil P.A., Chauvin C., Toquin M.T., Fablet C., Le Notre Y., Salvat G., Madec F., Fravalo P. Listeria monocytogenes contamination of finishing pigs: An exploratory epidemiological survey in France. Vet. Res. 2003;34:737–748. doi: 10.1051/vetres:2003031. [DOI] [PubMed] [Google Scholar]
- 106.Falardeau J., Johnson R.P., Pagotto F., Wang S. Occurrence, characterization, and potential predictors of verotoxigenic Escherichia coli, Listeria monocytogenes, and Salmonella in surface water used for produce irrigation in the Lower Mainland of British Columbia, Canada. PLoS ONE. 2017;12:e0185437. doi: 10.1371/journal.pone.0185437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Ojeniyi B., Wegener H.C., Jensen N.E., Bisgaard M. Listeria monocytogenes in poultry and poultry products: Epidemiological investigations in seven Danish abattoirs. J. Appl. Bacteriol. 1996;80:395–401. doi: 10.1111/j.1365-2672.1996.tb03234.x. [DOI] [PubMed] [Google Scholar]
- 108.Moosavy M.H., Shavisi N., Warriner K., Mosta-Favi E. Bacterial Contamination of Iranian Paper Currency. Iran. J. Public Health. 2013;42:1067–1070. [PMC free article] [PubMed] [Google Scholar]
- 109.Marshall J.C., Soboleva T.K., Jamieson P., French N.P. Estimating Bacterial Pathogen Levels in New Zealand Bulk Tank Milk. J. Food Prot. 2016;79:771–780. doi: 10.4315/0362-028X.JFP-15-230. [DOI] [PubMed] [Google Scholar]
- 110.Jongman M., Korsten L. Microbial quality and suitability of roof-harvested rainwater in rural villages for crop irrigation and domestic use. J. Water Health. 2016;14:961–971. doi: 10.2166/wh.2016.058. [DOI] [PubMed] [Google Scholar]
- 111.Ahlstrom C.A., Manuel C.S., Den Bakker H.C., Wiedmann M., Nightingale K.K. Molecular ecology of Listeria spp., Salmonella, Escherichia coli O157:H7 and non-O157 Shiga toxin-producing E. coli in pristine natural environments in Northern Colorado. J. Appl. Microbiol. 2018;124:511–521. doi: 10.1111/jam.13657. [DOI] [PubMed] [Google Scholar]
- 112.Dungan R.S., Klein M., Leytem A.B. Quantification of bacterial indicators and zoonotic pathogens in dairy wastewater ponds. Appl. Environ. Microbiol. 2012;78:8089–8095. doi: 10.1128/AEM.02470-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Belias A., Strawn L.K., Wiedmann M., Weller D. Small Produce Farm Environments Can Harbor Diverse Listeria monocytogenes and Listeria spp. Populations. J. Food Prot. 2021;84:113–121. doi: 10.4315/JFP-20-179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Jensen A., Thomsen L.E., Jorgensen R.L., Larsen M.H., Roldgaard B.B., Christensen B.B., Vogel B.F., Gram L., Ingmer H. Processing plant persistent strains of Listeria monocytogenes appear to have a lower virulence potential than clinical strains in selected virulence models. Int. J. Food Microbiol. 2008;123:254–261. doi: 10.1016/j.ijfoodmicro.2008.02.016. [DOI] [PubMed] [Google Scholar]
- 115.Lunden J.M., Autio T.J., Sjoberg A.M., Korkeala H.J. Persistent and nonpersistent Listeria monocytogenes contamination in meat and poultry processing plants. J. Food Prot. 2003;66:2062–2069. doi: 10.4315/0362-028X-66.11.2062. [DOI] [PubMed] [Google Scholar]
- 116.Kastbjerg V.G., Larsen M.H., Gram L., Ingmer H. Influence of sublethal concentrations of common disinfectants on expression of virulence genes in Listeria monocytogenes. Appl. Environ. Microbiol. 2010;76:303–309. doi: 10.1128/AEM.00925-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Rodrigues D., Cerca N., Teixeira P., Oliveira R., Ceri H., Azeredo J. Listeria monocytogenes and Salmonella enterica enteritidis biofilms susceptibility to different disinfectants and stress-response and virulence gene expression of surviving cells. Microb. Drug Resist. 2011;17:181–189. doi: 10.1089/mdr.2010.0183. [DOI] [PubMed] [Google Scholar]
- 118.Prates D.D., Haubert L., Wurfel S.D., Cavicchioli V.Q., Nero L.A., da Silva W.P. Listeria monocytogenes in dairy plants in Southern Brazil: Occurrence, virulence potential, and genetic diversity. J. Food Saf. 2019;39:e12695. doi: 10.1111/jfs.12695. [DOI] [Google Scholar]
- 119.Alessandria V., Rantsiou K., Dolci P., Cocolin L. Molecular methods to assess Listeria monocytogenes route of contamination in a dairy processing plant. Int. J. Food Microbiol. 2010;141:S156–S162. doi: 10.1016/j.ijfoodmicro.2010.02.001. [DOI] [PubMed] [Google Scholar]
- 120.Ibba M., Cossu F., Spanu V., Virdis S., Spanu C., Scarano C., De Santis E.P.L. Listeria monocytogenes contamination in dairy plants: Evaluation of Listeria monocytogenes environmental contamination in two cheese-making plants using sheeps milk. Ital. J. Food Saf. 2013;2:109–112. doi: 10.4081/ijfs.2013.e31. [DOI] [Google Scholar]
- 121.Mafu A.A., Roy D., Goulet J., Magny P. Attachment of Listeria monocytogenes to Stainless Steel, Glass, Polypropylene, and Rubber Surfaces After Short Contact Times. J. Food Prot. 1990;53:742–746. doi: 10.4315/0362-028X-53.9.742. [DOI] [PubMed] [Google Scholar]
- 122.Lawrence L.M., Gilmour A. Characterization of Listeria monocytogenes isolated from poultry products and from the poultry-processing environment by random amplification of polymorphic DNA and multilocus enzyme electrophoresis. Appl. Environ. Microbiol. 1995;61:2139–2144. doi: 10.1128/aem.61.6.2139-2144.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.