Abstract
There is limited information concerning the nature and extent of the immune response to the virulence determinants of Yersinia pestis during the course of plague infection. In this study, we evaluated the humoral immune response of mice that survived lethal Y. pestis aerosol challenge after antibiotic treatment. Such a model may replicate the clinical situation in humans and indicate which virulence determinants are expressed in vivo. Immunoglobulin G enzyme-linked immunosorbent assay and immunoblotting were performed by using purified, recombinant antigens including F1, V antigen, YpkA, YopH, YopM, YopB, YopD, YopN, YopE, YopK, plasminogen activator protease (Pla), and pH 6 antigen as well as purified lipopolysaccharide. The major antigens recognized by murine convalescent sera were F1, V antigen, YopH, YopM, YopD, and Pla. Early treatment with antibiotics tended to reduce the immune response and differences between antibiotic treatment regimens were noted. These results may indicate that only some virulence factors are expressed and/or immunogenic during infection. This information may prove useful for selecting potential vaccine candidates and for developing improved serologic diagnostic assays.
Yersinia pestis, the etiologic agent of bubonic and pneumonic plague, possesses virulence determinants encoded on each of three plasmids and its chromosome (reviewed in reference 42). The 70- to 75-kb low-calcium response (Lcr) plasmid, which is homologous in the two other pathogenic Yersinia species, Y. pseudotuberculosis and Y. enterocolitica, encodes V antigen (LcrV) and a group of highly conserved Yersinia outer proteins (Yops) known to be essential for virulence (14). Maximum expression of V antigen and Yops occurs in vitro at 37°C either in low-calcium medium (57) or after intimate contact of the bacteria with the plasma membrane of eucaryotic target cells (49, 54). The Yops shown to be necessary for full virulence in Y. pestis (where tested) or the other Yersinia species include those translocated into the eucaryotic cytosol: YopE, which indirectly depolymerizes actin microfilaments (47, 48, 49, 53); YopH, a tyrosine protein phosphatase (23, 43); YpkA, a serine/threonine protein kinase (22, 26); YopM, which binds α-thrombin and blocks platelet activation (8, 33, 45); and YopB, YopD, YopK, and YopN, involved in controlling Yop translocation (8, 19, 25, 29, 30, 43, 48, 49, 53, 54). V antigen has an antihost function and is involved in regulating the low-calcium response (7, 51). The 100-kb plasmid encodes a murine toxin and the capsular protein, F1 (44), necessary for full virulence in some animal species (61). The third plasmid of 10 kb encodes the bacteriocin, pesticin, and a plasminogen activator protease (Pla) necessary in most strains for virulence from a subcutaneous site (52). Other factors involved in virulence include the chromosomally encoded pH 6 antigen, which may be an adhesin (34), and lipopolysaccharide (LPS).
Serodiagnosis of human plague infections is based on measurement of the immune response to F1 (11). However, there is little information available on the immune response to other Y. pestis antigens. Most prior studies measured the immune response to Y. pestis infection by using uncharacterized cell extracts from Y. enterocolitica, Y. pseudotuberculosis, or Y. pestis as the antigens (9, 15, 36). In these studies, it was not possible to definitively determine the identity of the antigens analyzed since many of the Lcr plasmid-specific proteins have very similar molecular weights. More recently, the immune response to purified V antigen, YopM (41), and Pla (16) was reported for small numbers of cases of human plague. In this study, we undertook a more comprehensive analysis of the humoral immune response to highly purified individual Y. pestis antigens by using a murine model of antibiotic-treated pneumonic plague.
MATERIALS AND METHODS
Bacterial strains and reagents.
Wild-type Y. pestis CO92 was kindly provided by the laboratory of T. Quan, Centers for Disease Control, Fort Collins, Colo. An attenuated Pgm− derivative of this strain was obtained by serial passage on Congo red medium (59).
For the Y. pestis challenge, wild-type CO92 frozen stocks were streaked on tryptose blood agar base (Difco Laboratories, Detroit, Mich.) slants and incubated at 28°C for 2 days. Cells were harvested in 5 ml of heart infusion broth (HIB; Difco) and adjusted to an A620 of 1.0, and 2.0 ml of the suspension was used to inoculate 100 ml of HIB supplemented with 0.2% xylose. The cultures were grown for 24 h at 30°C, centrifuged, washed with HIB, adjusted to an A620 of 10.0, and diluted to the appropriate challenge dose.
Animal challenge with Y. pestis CO92.
Female, 6- to 8-week-old Swiss-Webster mice (Hsd:ND4; Harlan Sprague Dawley) weighing 20 to 24 g were used for the experimental plague challenge as previously described (10). Experiments with animals were conducted in accordance with Guide for the Care and Use of Laboratory Animals (13). Throughout the experiment, mice were given food and water ad libitum.
Mice were challenged with wild-type Y. pestis CO92 by nose-only aerosol in a modified Henderson exposure system (17, 28). The aerosol was generated with a Collison nebulizer (35), and mice were exposed to approximately 100 50% lethal doses (LD50; 1 LD50 = 2 × 104 CFU) of Y. pestis (61). Samples of the aerosol were collected during each exposure and plated on blood agar to determine the actual challenge dose. The inhaled dose was estimated by using Guyton’s formula (24).
Either 24 or 42 h postchallenge, mice were treated with antibiotics. Antibiotic therapy lasted 5 days, and antibiotics were administered by intraperitoneal injection every 6 h. The doses of antibiotics used were 30 mg/kg for ofloxacin (Ortho Pharmaceuticals, Raritan, N.J.) and 40 mg/kg for streptomycin (Pfizer, New York, N.Y.). Animals were monitored daily for disease symptoms or death. At 30 days postchallenge, survivors were deeply anesthetized and blood was obtained by intracardiac puncture.
Expression and purification of Y. pestis antigens. (i) F1.
F1 was purified from an E. coli recombinant strain as previously described (3).
(ii) V antigen.
V antigen was expressed and purified as previously described (27). Briefly, the V antigen PCR product from plasmid DNA was ligated into pET15b, and the protein was expressed with an N-terminal histidine tag in the protease-deficient Escherichia coli strain BL21(DE3) (Novagen, Madison, Wis.). The protein was partially purified on a Ni2+ affinity column and further purified by ion-exchange chromatography with Whatman DE-52 cellulose.
(iii) YopB, YopD, YopK, YopE, and YpkA.
The Y. pestis loci yopB, yopD, yopK, yopE, and ypkA were PCR amplified, cloned, and sequenced as previously described (4, 56). Briefly, the PCR-amplified products were ligated into the pET19b expression vector (Novagen), and positive clones were transferred into the protease-deficient E. coli strain BL21(DE3)pLysS or BLR (Novagen). The yop products were expressed as histidine-tagged fusion proteins, denatured with 6 M urea (Sigma Chemical Co., St. Louis, Mo.), and purified by the Novagen Ni2+ affinity chromatography system as described by the manufacturer.
(iv) YopH, YopN, and Pla.
YopH, YopN, and Pla were cloned by Perimmune, Inc. (Rockville, Md.) (4). The yopH, yopN, and pla loci were PCR amplified, cloned into pET21a (Novagen), and sequenced as described above for the other Yops. Proteins were expressed in E. coli BL21(DE3)pLysS or BLR. Recombinant Pla was histidine tagged and purified in the presence of 6 M urea by Ni2+ affinity chromatography. YopH was purified by high-pressure liquid chromatography (HPLC) cation-exchange and size exclusion chromatography, and YopN was denatured with 6 M urea and purified by HPLC anion-exchange and size exclusion chromatography.
(v) YopM.
Purified YopM was kindly provided by S. Straley (University of Kentucky, Lexington) and purified as previously described (41).
(vi) pH 6 antigen.
Y. pestis pH 6.0 antigen was extracted and purified from the recombinant E. coli strain pDG27, kindly provided by L. Lindler (Walter Reed Army Institute of Research, Washington, D.C.) (34) by a method similar to that for purifying the F1 capsular antigen (3). Briefly, nutrient agar isolates of E. coli pDG27 were examined by immunoblotting for the ability to produce high levels of pH 6 antigen at 37°C. Selected isolates were transferred to 1 to 2 liters of HIB (Difco) and grown overnight at 37°C. The bacteria were then separated from the growth medium by centrifugation, and cell-free pH 6 antigen was precipitated directly from culture supernatants by gradually adding 30% ammonium sulfate at 4°C. After dialysis against phosphate-buffered saline (PBS), crude pH 6 antigen preparations were passed across a Superdex-200 preparative gel filtration column (Pharmacia Biotech Inc., Piscataway, N.J.). Purified pH 6 antigen was isolated in the column void volume as a high-molecular-mass (>2-MDa) aggregate of the 15-kDa structural subunit.
(vii) LPS.
Y. pestis LPS was purified by hot phenol-water extraction from a pLcr− Pgm− pPst− derivative of Y. pestis CO92, using a modification of the method of Westphal and Jann (62).
Sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE) and immunoblotting.
Purified Y. pestis antigens (approximately 1.0 μg/lane) were separated by denaturing gel electrophoresis at 125 V on 10% Tricine gels (Novex, San Diego, Calif.). Proteins were visualized by staining with Coomassie blue, and the gels were scanned with a PDI 420oe scanner with a QS30 optically enhanced densitometry system, version 1.0 (PDI, Huntington Station, N.Y.).
For immunoblotting, approximately 2.5 μg of denatured protein was run in the large well of 10% Tris-glycine gels with two-dimensional preparative combs (Novex); prestained standards were run in the smaller well. The proteins were electrophoretically transferred to nitrocellulose (60) and blocked with 5% (wt/vol) nonfat dry milk in Tris-buffered saline (pH 7.4) containing 0.5% Tween 20. To test all serum samples simultaneously, the membranes were then placed in a Mini-PROTEAN II multiscreen apparatus (Bio-Rad, Hercules, Calif.) and probed with a 1:1,000 dilution of the serum samples overnight at 4°C. The membranes were washed with Tris-buffered saline–Tween 20 and incubated with horseradish peroxidase-conjugated, goat anti-mouse immunoglobulin G (IgG) (Kirkegaard & Perry, Gaithersburg, Md.). After extensive washing, immunoreactivity was visualized by enhanced chemiluminescence (ECL) Western blotting reagent (Amersham, Arlington Heights, Ill.). All antigens were probed with known positive sera or ascites fluid as a positive control and uninfected mouse sera as a negative control. The ECL reactions were overexposed to ensure that all positive reactions would be visualized.
IgG ELISAs.
Serum antibody titers were determined by direct IgG enzyme-linked immunosorbent assay (ELISA). For the soluble antigens (F1, V antigen, YopH, YopM, YopK, pH 6 antigen, and LPS), 96-well plates (Dynatech, Chantilly, Va.) were coated with 100 μl of antigen (1.0 μg/ml in PBS [pH 7.4]) per well and incubated overnight at 4°C. The water-insoluble antigens (YpkA, YopB, YopD, YopE, YopN, and Pla) were dissolved in 4 M urea (pH 7.5); then antigen preparations (100 μl per well at 1.0 μg/ml) were coated on plates pretreated with 0.025% glutaraldehyde in 0.1 M Na2CO3 (pH 9.0) according to the method of Klasen et al. (31) and incubated overnight at room temperature. Following overnight incubation, the procedure for all plates was the same. Plates were washed three times in PBS (pH 7.4) with 0.1% Tween 20. Serum samples were applied at a starting dilution of 1:100 in PBS (pH 7.4)–0.1% Tween 20–5% (wt/vol) skim milk and serially diluted twofold to 1:12,800 or 1:3,276,800 in a final volume of 100 μl/well. The plates were incubated for 1 h at 37°C and washed; then a 1:2,000 dilution of horseradish peroxidase-conjugated goat anti-mouse IgG (Kirkegaard & Perry) was added at 100 μl per well. After a 1-h incubation at 37°C, plates were washed, and 100 μl of 2,2′-azinobis(3-ethylbenzthiazolinesulfonic acid) (ABTS) two-component substrate system (Kirkegaard & Perry) was added. Following incubation at 37°C for 30 min, plates were read at 405 nm on a Dynatech MRX plate reader. The endpoint titer was determined by the highest test serum dilution with optical density at 405 nm (OD405) of ≥0.20 after subtraction of the OD405 for the blank wells with no antigen. The results are expressed as the geometric mean titer of the reciprocal endpoint dilution for three separate experiments. A negative result means the test serum was less than twofold higher than normal mouse serum tested against the same antigen.
RESULTS
SDS-PAGE of purified Y. pestis antigens.
To identify conclusively the Y. pestis virulence determinants, which are expressed and immunogenic during pneumonic plague in mice, purified, recombinant proteins were used as the antigens for the immunological assays in this study. The Y. pestis antigens used included purified recombinant proteins F1, V antigen, YpkA, YopH, YopM, YopB, YopD, YopN, YopE, YopK, Pla, and pH 6 antigen as well as purified LPS. To determine the molecular mass and relative purity of the antigen preparations, proteins were separated by SDS-PAGE (results not shown). All proteins had molecular masses similar to those reported in the literature and contained only minor contaminants. Purified Y. pestis LPS analyzed by SDS-PAGE and silver staining showed a characteristic, rough phenotype (results not shown), as previously reported (12).
IgG ELISA response to Y. pestis antigens in mice surviving pneumonic plague.
A previously described experimental model of pneumonic plague in mice was used in this study (10). Briefly, mice were aerosol challenged with approximately 100 LD50 of Y. pestis CO92 and subsequently treated with antibiotics starting either 24 or 42 h postchallenge. Thirty days postchallenge, sera from surviving mice which were treated with ofloxacin starting 42 h after aerosol challenge with Y. pestis were collected and analyzed by ELISA for IgG antibody response to Y. pestis antigens.
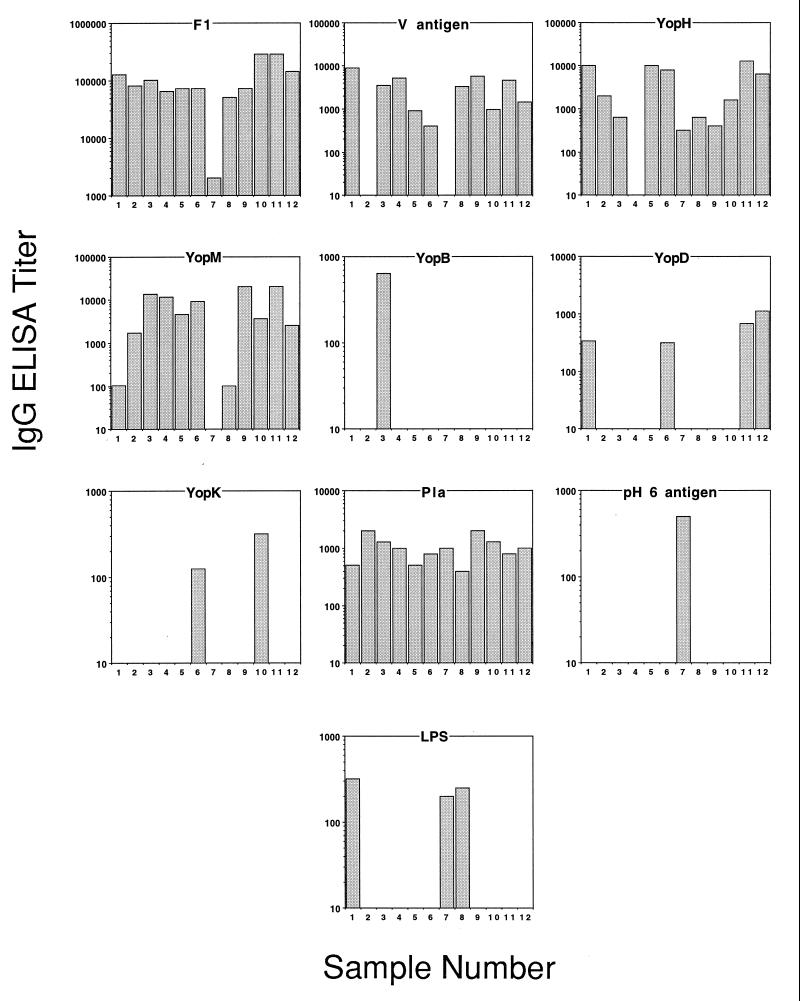
Figure 1 shows the immunological responses of 12 separate animals to 10 different Y. pestis antigens; the immune response to three other antigens tested (YpkA, YopE, YopN) was negative for all sera, and these data are not shown.
FIG. 1.
IgG response to Y. pestis antigens in mice surviving pneumonic plague. Each graph represents a separate antigen tested against individual serum samples from 12 mice treated with ofloxacin starting 42 h postchallenge. The IgG ELISA titers are the geometric mean reciprocal endpoint dilutions from three separate assays. Note differences in the scale of the abscissa. No data shown indicates that the mean for that sample was less than twofold different from normal mouse serum tested with the same antigen.
The results indicate F1 is the immunodominant antigen both in percent responders (100%, n = 12) and in magnitude of response, with titers ranging from 1:2,000 to 1:250,000. Pla was also recognized by 100% of the animals tested; however, the titers ranged from only 1:400 to 1:2,000. Prominent responses to other virulence factors were observed, including those to YopH (11 of 12), YopM (11 of 12), and V antigen (10 of 12), with titers ranging from 1:300 to 1:13,000, 1:100 to 1:20,000, and 1:400 to 1:9,000, respectively. A smaller percentage of animals had a positive response to YopD and LPS, while only two animals responded positively to YopK. One animal each showed a response to YopB or pH 6 antigen.
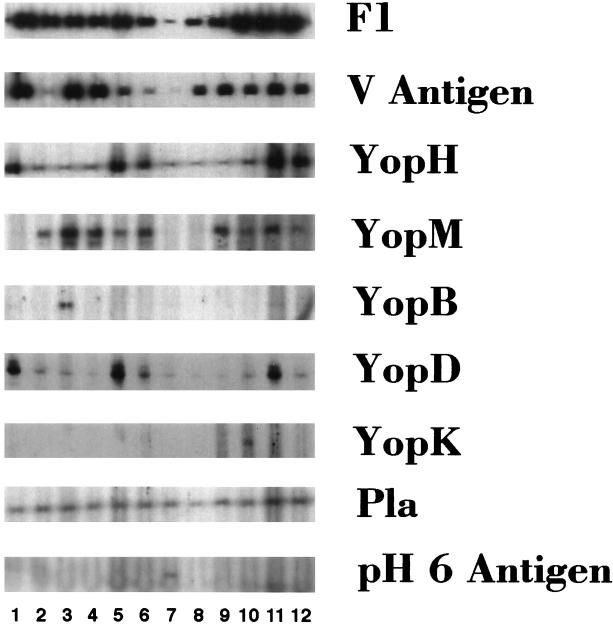
Immunoblot analysis of IgG antibody response to Y. pestis antigens in mice surviving pneumonic plague.
To confirm the results obtained by the ELISA and to examine the effect of denaturation of the antigens on the results, the mouse sera were also analyzed by immunoblotting. For the ELISA, half of the antigens were coated on the plates in PBS and half were in urea; for immunoblotting, all of the antigens were denatured in the same SDS sample buffer. Each strip in Fig. 2 represents an individual antigen tested against each different serum sample.
FIG. 2.
Immunoblot analysis of IgG antibody response to Y. pestis protein antigens. Y. pestis antigen preparations (2.5 μg per gel) were isolated by SDS-PAGE on 10% Tris-glycine gels (Novex) and transferred to nitrocellulose membranes. All 12 serum samples from the group of mice treated 42 h postchallenge with ofloxacin were incubated overnight against each antigen at a serum dilution of 1:1000 with a Mini-PROTEAN II multiscreen apparatus (Bio-Rad). Positive reactions were visualized by ECL.
In general, the results of the immunoblotting confirmed the ELISA results that showed F1 was the dominant antigen recognized, with the intensity of the bands corresponding to the ELISA titers. Similar to the ELISA results, all animals showed a response by immunoblot to Pla. The immunoblot also yielded similar results for V antigen, 11 of 12 positive, and YopH, 12 of 12 positive. For YopM, 9 of 12 samples were positive by immunoblotting; the two animals with the lowest ELISA titers were negative by immunoblotting. The greatest difference between the ELISA and immunoblot results was for YopD. Immunoblotting showed increased sensitivity for YopD, with the number of animals responding increasing from 4 of 12 for the ELISA to 12 of 12 for the immunoblot analysis, although some of the positive responses were very weak. One sample was still positive for YopB and one was positive for pH 6 antigen, and only one animal was positive for YopK, compared to two animals for the ELISA. In agreement with the ELISA results, no sera were positive by immunoblot for YpkA, YopE, or YopN (data not shown). However, no animals had an immunoblot positive against LPS (not shown) compared to the ELISA, which indicated that 3 of 12 samples were positive although of low titer.
Effect of antibiotics and time of treatment on IgG response.
In addition to the 12 animals treated with ofloxacin starting 42 h postchallenge, the immune response of mice treated with ofloxacin starting 24 h postchallenge (n = 18) or with streptomycin starting 42 h postchallenge (n = 7) was also analyzed by ELISA (Table 1). Early treatment with ofloxacin at 24 h compared to late treatment at 42 h significantly reduced the immune response. A statistically significant (by two-tailed Fisher exact test) reduction in the percent responders comparing late treatment to early treatment was shown for V antigen (83 to 6%, P < 0.0001), YopH (92 to 11%, P < 0.0001), YopM (92 to 11%, P < 0.0001), and Pla (100 to 39%, P = 0.006). While the percent of responders to F1 was not reduced, we noted a reduction of approximately 75-fold in the geometric mean titer in the 24-h treatment group compared to the 42-h treatment group.
TABLE 1.
Effect of antibiotic and time of treatment on the IgG ELISA response to Y. pestis antigens in mice surviving pneumonic plague
| Antibiotic treatment | No. of positive sera/total tested (% positive)
|
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| F1 | V antigen | YpkA | YopH | YopM | YopB | YopD | YopN | YopE | YopK | Pla | pH 6 antigen | LPS | |
| Ofloxacin, starting 24 h postchallenge | 16/18 (88) | 1/18 (6) | 0/18 (0) | 2/18 (11) | 2/18 (11) | 0/18 (0) | 3/18 (17) | 0/18 (0) | 0/18 (0) | 1/18 (6) | 7/18 (39) | 0/18 (0) | 0/18 (0) |
| Ofloxacin, starting 42 h postchallenge | 12/12 (100) | 10/12 (83) | 0/12 (0) | 11/12 (92) | 11/12 (92) | 1/12 (8) | 4/12 (33) | 0/12 (0) | 0/12 (0) | 2/12 (17) | 12/12 (100) | 1/12 (8) | 3/12 (25) |
| Streptomycin, starting 42 h postchallenge | 7/7 (100) | 2/7 (29) | 0/7 (0) | 2/7 (29) | 2/7 (29) | 0/7 (0) | 2/7 (29) | 0/7 (0) | 0/7 (0) | 2/6 (33) | 4/7 (57) | 1/7 (14) | 3/7 (43) |
| Total | 35/37 (95) | 13/37 (35) | 0/37 (0) | 15/37 (41) | 15/37 (41) | 1/37 (3) | 9/37 (24) | 0/37 (0) | 0/37 (0) | 5/36 (14) | 23/37 (62) | 2/37 (5) | 6/37 (16) |
Treatment with ofloxacin and streptomycin both administered 42 h postchallenge resulted in similar responses to F1, both in the number of responders and the magnitude of response. However, compared to ofloxacin, streptomycin treatment yielded a statistically significant reduction in the percent of responders to V antigen (83 to 29%, P = 0.045), YopH (92 to 29%, P < 0.01), YopM (92 to 29%, P < 0.01), and Pla (100 to 57%, P = 0.036).
DISCUSSION
In this study, we analyzed the immune response of mice surviving lethal aerosol infection with Y. pestis to gain insight into the in vivo expression and immunogenicity of Y. pestis virulence determinants during infection. Although similar experiments were reported previously (9, 15, 36), this study is the first time that all of the antigens used were purified free from other Yersinia components and thus could be definitively identified. Our results indicated the predominant antibody response of mice surviving pneumonic plague after treatment with antibiotics was to F1, V antigen, YopH, YopM, YopD, and Pla.
It was previously shown that convalescent plague serum recognizes Yops. Antibodies to Lcr plasmid-specific proteins of ∼36 and ∼24 kDa were identified in human and mouse serum after plague infection with cell extracts from either Y. pseudotuberculosis or Y. enterocolitica (9, 36) as the antigen source. Although our results suggest the ∼36-kDa protein could be V antigen or YopD, we did not see a response to a protein with a mass of ∼24 kDa. This protein could be a degradation product of V antigen or another protein expressed from the Lcr plasmid that we did not test for, such as the Yop secretion (Ysc) or specific Yop chaperone (Syc) proteins. A recent study showed guinea pigs infected with Y. pestis had an immune response to F1 and to plasmid-specific antigens with molecular masses of 76, 41, and 34 kDa, using Y. pseudotuberculosis extracts as the antigen source (15). These proteins were not identified, but based on the molecular mass, the 76-kDa protein could be YpkA, which we did not see a response to, or LcrD, which we did not test for. However, it was difficult to identify the 41- and 34-kDa proteins, based only on molecular mass, as many of the Lcr proteins have similar molecular masses. Our results in mice agree with the recent findings that some human convalescent serum from plague patients contains antibodies to YopM and V antigen (41) and also to Pla (16). The limited data for humans were obtained from cases of bubonic plague resulting from flea bites, while our studies used mice that recovered from pneumonic plague. We believe that the present results are likely to be similar to those seen after subcutaneous or flea bite exposure because most of the antigens analyzed are required for full virulence of the organism by the subcutaneous or systemic route of inoculation. Further studies on human sera to confirm this are in progress.
After infection with Y. enterocolitica, rats make antibodies to V antigen, YopM, and YopH, and also to YopD and YopE (20), while rabbits make antibody to V antigen and YopH (18). These results following Y. enterocolitica infection in rodents and rabbits are similar to our results following Y. pestis infection in mice. The lower response to YopE observed in our study, compared to the findings in rats, may be due to the late or low level of expression of this antigen after infection, as no antibiotics were given to the rats. It is also possible that the differences between this study and previous studies may be due to the route of exposure, as we used an aerosol challenge model, and some antigens may be differentially expressed. However, since most of the antigens analyzed are required for full virulence of the organism, we would expect similar results for both bubonic and pneumonic plague.
In our study, the greatest antibody responses were to F1, both in the percentage of animals that responded and in the magnitude of response, regardless of the time of antibiotic treatment or the antibiotic administered. This result supports the continued use of detection of antibodies to F1 for serodiagnosis of human plague (46). Both F1, a capsular protein, and Pla, a membrane protein known to be on the surface of the bacteria (5, 52), should be readily accessible to the immune system of the host. Consequently, it is not surprising that after combining data for all of the antibiotic treatment groups, we found that the highest percentages of animals responded to F1 and Pla (95 and 62%, respectively). Interestingly, both of these proteins have been tested as possible vaccine candidates against Y. pestis infection, and while F1 is efficacious (3), Pla is not (50).
In addition to F1 and Pla, the antigens that induced significant antibody responses in this study, V antigen, YopH, YopM, and YopD, are all encoded on the Lcr plasmid. The in vivo expression of the virulence proteins encoded on the Lcr plasmid is not well characterized; however, the results of our present study suggest that at least V antigen, YopM, YopH, and YopD are synthesized in vivo. The evidence that V antigen is a protective antigen by both active (2, 32, 38, 40) and passive (37, 58) immunization and that it suppresses the cytokines tumor necrosis factor alpha and interferon gamma (39, 40) supports the idea that V antigen is secreted in vivo. The high antibody response to V antigen in this study is also consistent with this idea. YopE, YpkA, YopH, and YopM are all essential for full virulence of Yersinia species (22, 23, 33, 47, 48) and have been shown in in vitro models to be translocated to the host target cell cytoplasm (7, 26, 43, 49, 53, 54); however, YopM also functions extracellularly (33, 45). Therefore, it is interesting that an immune response was generated to YopM and YopH but not to YopE or YpkA. While the reason for this difference is not known, it may be that YopH, like YopM, has an extracellular function in vivo. However, vaccination with either YopH (4) or YopM (41) did not protect mice from Y. pestis challenge, suggesting that although these proteins are expressed and accessible to the humoral immune response system during infection, their essential function in virulence may be intracellular or not neutralizable by the antibody generated from active vaccination. YopD, the only other antigen that generates a significant immune response, functions, along with YopB, YopN, and YopK, in the translocation of other Yops in Yersinia species (8, 19, 25, 29, 30, 43, 48, 49, 53, 54) and plays a role in the negative regulation of the low-calcium response in vitro (63). Interestingly, vaccination with YopD, but not YopB, YopN, or YopK, protects mice from challenge with an F1− Y. pestis strain, C12 (4). These results suggest that YopD is expressed in vivo, induces an immune response, and is accessible to antibody in vivo.
It is much more difficult to make any conclusions about the antigens that elicited minimal or no antibody responses, as many possible explanations exist. First, these proteins may not be expressed at all in vivo during infection. This is unlikely since most of the antigens tested are known to be necessary for full virulence. Second, they may be expressed and biologically active in vivo at subimmunogenic amounts as is reported for botulism and tetanus, in which infection does not lead to the induction of immunity (6, 55). It is also possible the antigens are expressed very late in the infectious process so that their synthesis is blocked by the antibiotic treatment. In addition, these proteins may be expressed but are not accessible to antigen-presenting cells inducing a humoral immune response either because they are located intracellularly or because they are translocated directly by intimate cell contact from the bacteria to the host cytoplasm. Another possibility is that these proteins are synthesized in vivo, but because of poor intrinsic antigenicity, a humoral immune response is not generated. Finally, the perceived lack of response to some antigens may be due to the assay method. Perhaps an immune response was generated but it was below the limit of detection for the ELISA or immunoblot analysis. In addition, most of the antigen preparations were recombinant proteins, which may not have folded into their native conformations or were denatured; thus, we would not detect antibodies to conformational epitopes of the native protein. Experiments with gene fusions may offer another approach to determining whether the specific Y. pestis genes are transcribed in vivo.
This study focused on animals that were treated with ofloxacin starting 42 h postchallenge, when they were bacteremic (10), to allow for the greatest antigen expression. These animals had the greatest antibody response to the antigens tested. Earlier treatment with ofloxacin at 24 h postchallenge, when the animals were not bacteremic (10), reduced the immune response to Y. pestis antigens, which was likely due to the reduced proliferation of the bacteria. Streptomycin, the drug of choice for plague, when given 42 h after challenge, also elicited a reduced antibody response compared to ofloxacin administered at the same time, although all animals were bacteremic and the two antibiotics had similar protective efficacies (10). The lower antibody response after streptomycin treatment could be due to the differences in the mechanisms of action of these two drugs; streptomycin directly inhibits protein synthesis by irreversibly binding the 30S ribosomal subunit, whereas ofloxacin is a DNA gyrase inhibitor. Both are bactericidal, but streptomycin inhibits protein synthesis faster, resulting in a lower expression of protein potentially leading to the reduced antibody response that we observed. Alaparthy and Barrett (1) suggest that the fluoroquinolones, although not ofloxacin specifically, may have immunity-enhancing effects which may also explain the difference in immune response profiles for the different antibiotics. Future experiments to compare the effect of other or multiple antibiotics on the immune response to Y. pestis will be informative and important, especially in light of the discovery of multiple-antibiotic resistance in Y. pestis (21).
This study suggests that serodiagnosis of plague may be improved by assaying the immune response to Pla, V antigen, YopH, YopM, or YopD, particularly for infection with an F1− strain of Y. pestis. We are currently analyzing the IgG antibody response to the antigens used in this study in acute and convalescent sera from human plague cases to determine if the immune response is similar to that observed in mice surviving pneumonic plague.
ACKNOWLEDGMENTS
We thank Alfred O’Quinn and Ronald Dicks for technical assistance and Paul Gibbs for statistical analysis.
REFERENCES
- 1.Alaparthy S, Barrett J F. Abstracts of the 97th General Meeting of the American Society for Microbiology 1997. Washington, D.C: American Society for Microbiology; 1997. Superinduction of IL-12 p40 gene expression by fluoroquinolones and its regulation of the Th1 cytokine profiles, abstr. E-2. [Google Scholar]
- 2.Anderson G W, Jr, Leary S E C, Williamson E D, Titball R W, Welkos S L, Worsham P L, Friedlander A M. Recombinant V antigen protects mice against pneumonic and bubonic plague caused by F1-capsule-positive and -negative strains of Yersinia pestis. Infect Immun. 1996;64:4580–4585. doi: 10.1128/iai.64.11.4580-4585.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Andrews G P, Heath D G, Anderson G W, Jr, Welkos S L, Friedlander A M. Fraction 1 capsular antigen (F1) purification from Yersinia pestis CO92 and an Escherichia coli recombinant strain and efficacy against lethal plague challenge. Infect Immun. 1996;64:2180–2187. doi: 10.1128/iai.64.6.2180-2187.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Andrews, G. P., S. T. Strachan, G. E. Benner, A. K. Sample, J. J. Adamovicz, G. W. Anderson, Jr., S. L. Welkos, and A. M. Friedlander. Unpublished observations.
- 5.Beesley E D, Brubaker R R, Janssen W A, Surgalla M J. Pesticins. III. Expression of coagulase and mechanisms of fibrinolysis. J Bacteriol. 1967;94:19–26. doi: 10.1128/jb.94.1.19-26.1967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Beller M, Middaugh J P. Repeated type E botulism in an Alaskan Eskimo. N Engl J Med. 1990;322:855. doi: 10.1056/NEJM199003223221220. [DOI] [PubMed] [Google Scholar]
- 7.Bergman T S, Håkansson S, Forsberg Å, Norlander L, Macallaro A, Backman A, Bölin I, Wolf-Watz H. Analysis of the V antigen lcrGVH-yopBD operon of Yersinia pseudotuberculosis: evidence for a regulatory role of LcrH and LcrV. J Bacteriol. 1991;173:1607–1616. doi: 10.1128/jb.173.5.1607-1616.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Boland A, Sory M P, Iriarte M, Kerbourch C, Wattiau P, Cornelis G R. Status of YopM and YopN in the Yersinia Yop virulon: YopM of Yersinia enterocolitica is internalized inside the cytosol of PU5-1.8 macrophages by the YopB, D, N delivery apparatus. EMBO J. 1996;15:5191–5201. [PMC free article] [PubMed] [Google Scholar]
- 9.Bölin I, Portnoy D A, Wolf-Watz H. Expression of the temperature-inducible outer membrane proteins of yersiniae. Infect Immun. 1985;48:234–240. doi: 10.1128/iai.48.1.234-240.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Byrne W R, Welkos S L, Pitt M L, Davis K J, Brueckner R P, Ezzell J W, Nelson G O, Vaccaro J R, Battersby L C, Friedlander A M. Antibiotic treatment of experimental pneumonic plague in mice. Antimicrob Agents Chemother. 1998;42:675–681. doi: 10.1128/aac.42.3.675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cavanaugh D C, Fortier M K, Robinson D M, Williams J E, Rust J H., Jr Application of the ELISA technique to problems in the serologic diagnosis of plague. Bull Pan Am Health Org. 1979;13(4):399–402. [PubMed] [Google Scholar]
- 12.Chart H, Cheasty T, Rowe B. Differentiation of Yersinia pestis and Y. pseudotuberculosis by SDS-PAGE analysis of lipopolysaccharide. Lett Appl Microbiol. 1995;20:369–370. doi: 10.1111/j.1472-765x.1995.tb01323.x. [DOI] [PubMed] [Google Scholar]
- 13.Committee on Care and Use of Laboratory Animals of the Institute of Laboratory Animals Resources, National Resource Council. Guide for the care and use of laboratory animals, revised. National Institutes of Health publication no. 85-23. Bethesda, Md: National Institutes of Health; 1996. [Google Scholar]
- 14.Cornelis G R, Biot T, Lambert de Rouvroit C, Michiels T, Mulder B, Sluiters C, Sory M-P, Van Bouchaute M, Vanootegham J-C. The Yersinia yop regulon. Mol Microbiol. 1989;3:1455–1459. doi: 10.1111/j.1365-2958.1989.tb00129.x. [DOI] [PubMed] [Google Scholar]
- 15.Drobkov V I, Marakulin I V, Pogorelsky I P, Darmov I V, Smirnov E V. Antibody spectrum after the inoculation of Yersinia pestis and Yersinia pseudotuberculosis to susceptible animals. Zh Mikrobiol. 1996;2:81–85. [PubMed] [Google Scholar]
- 16.Easterbrook T J, Reddin K, Robinson A, Modi N. Studies on the immunogenicity of the Pla protein from Yersinia pestis. Contrib Microbiol Immunol. 1995;13:214–215. [PubMed] [Google Scholar]
- 17.Estep J E, Pitt M L M, Welkos S L, Davis K, Friedlander A. Abstracts of the 94th General Meeting of the American Society for Microbiology 1994. Washington, D.C: American Society for Microbiology; 1994. Pneumonic plague: development of a rodent animal model using nose-only aerosol exposure, abstr. B-212. [Google Scholar]
- 18.Fernnandez-Lago L, Gomez M, Vizcaino N, Chordi A. Analysis of the immune response to Yersinia enterocolitica serotype-O:9-released proteins by immunoblot and ELISA. Res Microbiol. 1994;145:553–561. doi: 10.1016/0923-2508(94)90032-9. [DOI] [PubMed] [Google Scholar]
- 19.Forsberg Å, Viitanen A-M, Skurnik M, Wolf-Watz H. The surface-located YopN protein is involved in calcium signal transduction in Yersinia pseudotuberculosis. Mol Microbiol. 1991;5:977–986. doi: 10.1111/j.1365-2958.1991.tb00773.x. [DOI] [PubMed] [Google Scholar]
- 20.Gaede K, Mack D, Heesemann J. Experimental Yersinia enterocolitica infection in rats: analysis of the immune response to plasmid-encoded antigens of arthritis-susceptible Lewis rats and arthritis-resistant Fisher rats. Med Microbiol Immunol. 1992;181:165–172. doi: 10.1007/BF00202056. [DOI] [PubMed] [Google Scholar]
- 21.Galimand M, Guiyoule A, Gerbaub G, Rasoamanana B, Chanteau S, Carniel E, Courvalin P. Multidrug resistance in Yersinia pestis mediated by a transferable plasmid. N Engl J Med. 1997;337:677–680. doi: 10.1056/NEJM199709043371004. [DOI] [PubMed] [Google Scholar]
- 22.Galyov E E, Håkansson S, Forsberg Å, Wolf-Watz H. A secreted protein kinase of Yersinia pseudotuberculosis is an indispensable virulence determinant. Nature. 1993;361:730–732. doi: 10.1038/361730a0. [DOI] [PubMed] [Google Scholar]
- 23.Guan K, Dixon J E. Protein tyrosine phosphatase activity of an essential virulence determinant in Yersinia. Science. 1990;249:553–556. doi: 10.1126/science.2166336. [DOI] [PubMed] [Google Scholar]
- 24.Guyton A C. Measurement of the respiratory volumes of laboratory animals. Am J Physiol. 1947;150:70–77. doi: 10.1152/ajplegacy.1947.150.1.70. [DOI] [PubMed] [Google Scholar]
- 25.Håkansson S, Persson C, Schesser K, Galyov E E, Rosqvist R, Wolf-Watz H. The YopB protein of Yersinia pseudotuberculosis is essential for translocation of Yop effector proteins across the target cell plasma membrane and displays contact-dependent membrane-disrupting activity. EMBO J. 1996;15:5812–5823. [PMC free article] [PubMed] [Google Scholar]
- 26.Håkansson S, Galyov E E, Rosqvist R, Wolf-Watz H. The Yersinia YpkA ser/thr kinase is translocated and subsequently targeted to the inner surface of the HeLa cell plasma membrane. Mol Microbiol. 1996;20:593–603. doi: 10.1046/j.1365-2958.1996.5251051.x. [DOI] [PubMed] [Google Scholar]
- 27.Heath D G, Anderson G W, Jr, Mauro J M, Welkos S L, Andrews G P, Adamovicz J J, Friedlander A M. Protection against experimental bubonic and pneumonic plague by a recombinant capsular F1-V antigen fusion protein vaccine. Vaccine. 1998;16:1131–1137. doi: 10.1016/s0264-410x(98)80110-2. [DOI] [PubMed] [Google Scholar]
- 28.Henderson D W. An apparatus for the study of airborne infection. J Hyg. 1952;50:53–68. doi: 10.1017/s0022172400019422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Holstrom A, Rosqvist R, Wolf-Watz H, Forsberg Å. Virulence plasmid-encoded YopK is essential for Yersinia pseudotuberculosis to cause systemic infection in mice. Infect Immun. 1995;63:2269–2276. doi: 10.1128/iai.63.6.2269-2276.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Holstrom A, Pettersson J, Rosqvist R, Håkansson S, Tafazoli F, Fallman M, Magnusson K-E, Wolf-Watz H, Forsberg Å. YopK of Yersinia pseudotuberculosis controls translocation of Yop effectors across the eukaryotic cell membrane. Mol Microbiol. 1997;24:73–91. doi: 10.1046/j.1365-2958.1997.3211681.x. [DOI] [PubMed] [Google Scholar]
- 31.Klasen E A, Rigutti A, Bos A, Bernini L F. Development of a screening system for detection of somatic mutations. I. Enzyme immunoassay for detection of antibodies against specific hemoglobin determinants. J Immunol Methods. 1982;54:241–250. doi: 10.1016/0022-1759(82)90065-5. [DOI] [PubMed] [Google Scholar]
- 32.Leary S E C, Williamson E D, Griffin K F, Russell P, Eley S M, Titball R W. Active immunization with recombinant V antigen from Yersinia pestis protects mice against plague. Infect Immun. 1995;63:2854–2858. doi: 10.1128/iai.63.8.2854-2858.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Leung K Y, Reisner B S, Straley S C. YopM inhibits platelet aggregation and is necessary for virulence of Yersinia pestis in mice. Infect Immun. 1990;58:3262–3271. doi: 10.1128/iai.58.10.3262-3271.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lindler L E, Tall B D. Yersinia pestis pH 6 antigen forms fimbriae and is induced by intracellular association with macrophages. Mol Microbiol. 1993;8:311–324. doi: 10.1111/j.1365-2958.1993.tb01575.x. [DOI] [PubMed] [Google Scholar]
- 35.May K R. The Collison nebulizer, description, performance, and applications. J Aerosol Sci. 1973;4:235–243. [Google Scholar]
- 36.Mazza G, Karu A E, Kingsbury D T. Immune response to plasmid- and chromosome-encoded Yersinia antigens. Infect Immun. 1985;48:676–685. doi: 10.1128/iai.48.3.676-685.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Motin V L, Nakajima R, Smirnov G B, Brubaker R R. Passive immunity to yersiniae mediated by anti-recombinant V antigen and protein A-V antigen fusion peptide. Infect Immun. 1994;62:4192–4201. doi: 10.1128/iai.62.10.4192-4201.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Motin V L, Nedialkov Y A, Brubaker R R. V antigen-polyhistidine fusion peptide: binding to LcrH and active immunity against plague. Infect Immun. 1996;64:4313–4318. doi: 10.1128/iai.64.10.4313-4318.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nakajima R, Brubaker R R. Association between virulence of Yersinia pestis and suppression of gamma interferon and tumor necrosis factor alpha. Infect Immun. 1993;61:23–31. doi: 10.1128/iai.61.1.23-31.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Nakajima R, Motin V L, Brubaker R R. Suppression of cytokines in mice by protein A-V antigen fusion peptide and restoration of synthesis by active immunization. Infect Immun. 1995;63:3021–3029. doi: 10.1128/iai.63.8.3021-3029.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nemeth J, Straley S C. Effect of Yersinia pestis YopM on experimental plague. Infect Immun. 1997;65:924–930. doi: 10.1128/iai.65.3.924-930.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Perry R D, Fetherston J D. Yersinia pestis—etiological agent of plague. Clin Microbiol Rev. 1997;10:35–66. doi: 10.1128/cmr.10.1.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Persson C, Nordfelth R, Holstrom A, Håkansson S, Rosqvist R, Wolf-Watz H. Cell surface bound Yersinia translocate the protein tyrosine phosphatase YopH by a polarized mechanism into the target cell. Mol Microbiol. 1995;18:135–150. doi: 10.1111/j.1365-2958.1995.mmi_18010135.x. [DOI] [PubMed] [Google Scholar]
- 44.Protsenko O A, Anisimov P I, Mosarov O T, Donnov N P, Popov Y A, Kokushkin A M. Detection and characterization of Yersinia pestis plasmids determining pesticin I, fraction I antigen and mouse toxin synthesis. Genetika. 1983;19:1081–1090. [PubMed] [Google Scholar]
- 45.Reisner B S, Straley S C. Yersinia pestis YopM: thrombin binding and overexpression. Infect Immun. 1992;60:5242–5252. doi: 10.1128/iai.60.12.5242-5252.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rasoamanana B, Leroy F, Boisier P, Rasolomaharo M, Buchy P, Carniel E, Chanteau S. Field evaluation of an immunoglobulin G anti-F1 enzyme-linked immunosorbent assay for serodiagnosis of human plague in Madagascar. Clin Diagn Lab Immunol. 1997;4:587–591. doi: 10.1128/cdli.4.5.587-591.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rosqvist R, Forsberg Å, Rimpiläinen M, Bergman T, Wolf-Watz H. The cytotoxic protein YopE of Yersinia obstructs the primary host defense. Mol Microbiol. 1990;4:657–667. doi: 10.1111/j.1365-2958.1990.tb00635.x. [DOI] [PubMed] [Google Scholar]
- 48.Rosqvist R, Forsberg Å, Wolf-Watz H. Intracellular targeting of the Yersinia YopE cytotoxin in mammalian cells induces actin microfilament disruption. Infect Immun. 1991;59:4562–4569. doi: 10.1128/iai.59.12.4562-4569.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rosqvist R, Magnusson K E, Wolf-Watz H. Target cell contact triggers expression and polarized transfer of Yersinia YopE cytotoxin into mammalian cells. EMBO J. 1994;13:964–972. doi: 10.1002/j.1460-2075.1994.tb06341.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Sample, A. K., and A. M. Friedlander. Unpublished observations.
- 51.Skrzypek E, Straley S C. Differential effects of deletions in LcrV on secretion of V antigen, regulation of the low-Ca2+ response, and virulence of Yersinia pestis. J Bacteriol. 1995;177:2530–2542. doi: 10.1128/jb.177.9.2530-2542.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sodeinde O A, Gougen J D. Genetic analysis of the 9.5-kilobase virulence plasmid of Yersinia pestis. Infect Immun. 1988;56:2743–2758. doi: 10.1128/iai.56.10.2743-2748.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sory M P, Cornelis G R. Translocation of a hybrid YopE-adenylate cyclase from Yersinia enterocolitica into HeLa cells. Mol Microbiol. 1994;14:583–594. doi: 10.1111/j.1365-2958.1994.tb02191.x. [DOI] [PubMed] [Google Scholar]
- 54.Sory M P, Boland A, Lambermont I, Cornelis G R. Identification of the YopE and YopH domains required for secretion and internalization into the cytosol of macrophages using the cyaA gene fusion approach. Proc Natl Acad Sci USA. 1995;92:11998–12002. doi: 10.1073/pnas.92.26.11998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Spenny J G, Lamb R N, Cobbs C G. Recurrent tetanus. South Med J. 1971;64:859. doi: 10.1097/00007611-197107000-00017. [DOI] [PubMed] [Google Scholar]
- 56.Strachan S D, Andrews G P, Friedlander A M. Abstracts of the 96th General Meeting of the American Society of Microbiology 1996. Washington, D.C: American Society of Microbiology; 1996. Cloning, expression and characterization of the Yersinia outer membrane protein B (YopB) from Yersinia pestis, abstr. B-217. [Google Scholar]
- 57.Straley S C, Plano G V, Skrzypek E, Haddix P L, Fields K A. Regulation by Ca2+ in Yersinia low-Ca2+ response. Mol Microbiol. 1993;8:1005–1010. doi: 10.1111/j.1365-2958.1993.tb01644.x. [DOI] [PubMed] [Google Scholar]
- 58.Straley S C, Skrzypek E, Haddix P L, Fields K A. Yops of Yersinia spp. pathogenic for humans. Infect Immun. 1993;61:3105–3110. doi: 10.1128/iai.61.8.3105-3110.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Surgalla M J, Beesley E D. Congo red-agar plating medium for detecting pigmentation in Pasteurella pestis. Appl Microbiol. 1969;18:834–837. doi: 10.1128/am.18.5.834-837.1969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Towbin H, Staehelin T, Gordon J. Electrophoretic transfer of proteins from polyacrylamide gels to nitrocellulose sheets: procedure and some applications. Proc Natl Acad Sci USA. 1979;76:4350–4354. doi: 10.1073/pnas.76.9.4350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Welkos S L, Davis K M, Pitt M L M, Worsham P L, Friedlander A M. Studies on the contribution of the F1 capsule-associated plasmid pFra to the virulence of Yersinia pestis. Contrib Microbiol Immunol. 1995;13:299–305. [PubMed] [Google Scholar]
- 62.Westphal O, Jann K. Bacterial lipopolysaccharides: extraction with phenol-water and further applications of the procedure. In: Whistler R C, editor. Methods in carbohydrate chemistry. Vol. 5. New York, N.Y: Academic Press Inc.; 1962. pp. 83–91. [Google Scholar]
- 63.Williams A W, Straley S C. YopD of Yersinia pestis plays a role in negative regulation of the low-calcium response in addition to its role in translocation of Yops. J Bacteriol. 1998;180:350–358. doi: 10.1128/jb.180.2.350-358.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]