Abstract
Background: Vaccine hesitancy decreases adult vaccination coverage and has been recognized by WHO as a major health threat. Primary care physicians (PCP) play a key role in vaccination by giving vaccine counselling to their patients. The aim of this systematic review is to identify the knowledge, beliefs, attitudes and barriers (KBAB) associated with own vaccination and patient recommendation in primary care physicians. Methods: MEDLINE/PubMed, EMBASE and Cochrane Library databases were used to search and identify relevant studies based on their title and abstract. In the next step, the full text of each previously selected article was read for eligibility. Articles were selected by two independent reviewers and data extraction was performed using tables. The following information was extracted: methodological characteristics, demographic factors, professional characteristics, and intrinsic or extrinsic factors influencing vaccination or recommendation. Results: Our search yielded 41 eligible papers, data-sources, previous practices, belief in the effectiveness or safety of the vaccine, perceived risk, and trust in health authorities were all shown to be related to own vaccination and patient recommendation. Conclusion: Internet is the main source of information for PCP related to vaccine hesitancy. It is therefore essential to increase the presence and access to pro-vaccination content in this area. In addition, involving PCP in the establishment of vaccination recommendations could improve their credibility in the institutions. On the other hand, training in communication skills and establishing reminder systems could reflect higher vaccination coverage among their patients.
Keywords: vaccination hesitancy, primary care physician, knowledge, perception, attitude, public health
1. Introduction
Vaccines rank among the greatest advances in world health, indisputably preventing over two million deaths per year [1]. In fact, it is the tool that reduces the most deaths from disease, second only to the introduction of safe drinking water [2]. Historically, immunization programs have been targeted at children, a strategy that has achieved notable success in the control of infectious diseases (smallpox, polio, etc.) [3], due to the extensive vaccine coverage achieved.
That said, however, in the case of vaccines targeted at the adult population, coverage has been far lower [4,5]. A large part of this low coverage among adults is attributable to vaccine hesitancy. This is a situation of doubt, which could be resolved toward pro-vaccination or anti-vaccination (dragged by the anti-vaccination movements) [6]. At present, the magnitude of the problem is such that in 2019 the World Health Organization (WHO) included it as one of the main threats to global health [7]. In addition, combating vaccine hesitancy is also a challenge for the WHO’s Immunization 2030 Agenda [8].
Primary care physicians (PCP) play a key role in the vaccination of adults [9,10,11]: on the one hand, their own immunization is important for their personal protection and that of their patients; and on the other hand, motivated physicians have been seen to be more effective when it comes to vaccinating their patients [12,13]. The role of the PCP in addressing vaccine hesitancy is decisive, as they are the first and most reliable source of information for patients when deciding whether to be vaccinated [14]. The aim of the study is to identify the factors (knowledge, beliefs, attitudes and barriers) that condition the vaccination of PCP and also the vaccination recommendations to their adult patients [15,16,17,18].
2. Material and Methods
2.1. Study Protocol and Registration
The review was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [19]. The protocol was registered in the PROSPERO International Register of Systematic Reviews (registration no. CRD42021227730).
2.2. Search Strategy
For the purpose of this systematic bibliographic review, we conducted a search in MEDLINE/PubMed, EMBASE and the Cochrane Library electronic databases covering the period 1 January 2011 to 6 November 2021. The search terms used to identify relevant papers is presented at Supplementary Materials.
2.3. Inclusion and Exclusion Criteria
Studies were considered eligible for review if they met the following criteria: (i) they had been published in English, Spanish or Portuguese; (ii) they were quantitative or mixed (considering only quantitative data); (iii) they sought to explore and identify the KBAB of PCP in relation to any adult vaccine; (iv) they assessed any association between KBAB and own vaccination and patient recommendation; and (v) their study population included any physicians performing primary care functions (family physicians/general practitioners/general internists/obstetrician gynecologists) but excluded medical residents. Furthermore, physicians working in a hospital setting were required to have spent at least 50% of their time in primary care.
Following deduplication, titles and abstracts were screened by two authors (RG, AP), working independently. All papers identified as potentially relevant were reviewed by the authors, and in the event of disagreement, the paper in question was examined by AF and MZ, who then took the final decision.
2.4. Data-Extraction and Analysis
For each study included in the review, a table was drawn up (see Table 1), with the following parameters: author; year; country; study population; number and type of primary care participants; response rate (%); vaccine; data-collection method; and final Newcastle-Ottawa Scale (NOS) score [20]. We have covered all vaccines used in adults, but the adult vaccination recommendations vary from country to country. However, influenza and HPV vaccines are recommended in many countries, so we have structured our tables and results according to: influenza, vaccine, HPV vaccine or adult vaccines in general. A second table also was likewise created (Table 2) showing the following socio-demographic factors and their influence on own vaccination and patient recommendation: age; gender; employment status; experience; number of patients; type of practice; and practice of alternative medicine.
Table 1.
Methodological characteristics of the papers selected.
| Author | Year | Country | Study Population | Number and Type of Primary Care Participants | Response Rate (%) | Vaccine | Data-Collection Method (Questionnaire) | Final NOS Score |
|---|---|---|---|---|---|---|---|---|
| With statistical hypothesis testing between KBAB and own vaccination and patient recommendation | ||||||||
| Verger P et al. [21] | 2021 | France | GP | 2755 GP | 43.9 T | COVID-19 | Online | 7 |
| Verger P et al. [22] | 2021 | France | GP | 2755 GP | 29 T | COVID-19 | Online | 7 |
| Arlt J et al. [23] | 2021 | Germany | GP | 308 FM, 111 IM, 24 WS (443) | 28.0 E | Influenza | 7 | |
| Neufeind J et al. [24] | 2020 | Germany | FP | 735 FP | 20.4 E | Adult vaccination: influenza, pertussis, hepatitis B, measles, DT | Phone | 6 |
| Verhees RAF et al. [25] | 2020 | Netherlands | GP | 552 GP | 31.7 E | Influenza | Online | 5 |
| Vezzosi L et al. [26] | 2019 | Italy | GP | 73 GP | 26.6 T | Adults ≥ 65: Seasonal Influenza (SI), Pneumococcus (PNV), Zoster (ZV) | Online | 3 |
| Yilmaz-Karadağ F et al. [27] | 2019 | Turkey | PCP | 49 FP, 172 GP (221) | 14.7 T | Adult risk groups: Influenza, Td, pneumococcal, meningococcal, HBV, HAV | Online | 5 |
| Akan H et al. [28] | 2016 | Turkey | FP | 606 | 27.5 E | Influenza | Online | 4 |
| Klett-Tammen CJ et al. [29] | 2016 | Germany | GP, PA | 774 GP | 13.4 E | Vaccines for the elderly: tetanus, influenza, pneumococcal | 6 | |
| Verger P et al. [30] | 2015 | France | GP | 1582 GP | 42.5 E | Influenza, hepatitis B, MMR, HPV, MenC, | Telephone | 6 |
| Flicoteaux R et al. [31] | 2014 | France | GP | 1431 GP | 36.8 E | Pandemic Influenza A/H1N1 | Telephone | 4 |
| Pulcini C et al. [32] | 2013 | France | GP | 1431 GP | 36.8 E | Hepatitis B, pertussis, seasonal and pandemic influenza | Telephone | 5 |
| Pulcini C et al. [33] | 2014 | France | GP | 329 GP | 36.3 E | MMR | Telephone | 3 |
| Verger P et al. [34] | 2012 | France | GP | 1431 GP | 36.8 E | Pandemic Influenza A:H1N1 | Telephone | 6 |
| NO statistical hypothesis testing between KBAB and own vaccination and patient recommendation | ||||||||
| Deruelle et al. [35] | 2021 | USA | GP, OB/GYN | 69 GP | 81.1 T | COVID-19 | Online | 5 |
| Bayliss J et al. [36] | 2021 | Australia | GP, AC | 412 GP | - | Adult vaccination (focus: pertussis) Influenza, Td, HBV, HBA, polio |
- | 3 |
| Hurley LP et al. [37] | 2021 | USA | PCP | 336 FP, 281 GIM (617) | 64.0 E | HPV | Mail or online | 4 |
| Napolitano F et al. [38] | 2021 | Italy | GP | 349 GP | 61.5 E | HPV | Online or Telephone | 7 |
| Celep G et al. [39] | 2020 | Turkey | PHW | 97 FP | - | Pregnancy (Td, Tdap, HBV, influenza) | Online or Telephone | 3 |
| Kalemaki D et al. [40] | 2020 | Greece | GP | 260 GP | 88.0 E | Influenza, measles, HBV, pertussis, Tdap | Online or Telephone | 4 |
| Meites E et al. [41] | 2020 | USA | PCP | 266 FM, 235 GIM (430) | 59.3 E | HPV | Mail or online | 6 |
| Awadlla NJ et al. [42] | 2019 | Saudi Arabia | PHW | 74 PCP | 77.0 E | Seasonal Influenza | Personally | 6 |
| Collange F et al. [43] | 2019 | France | GP | 2586 GP | 37.6 E | MMR, MenC, HBV, seasonal influenza, HPV | Telephone | 5 |
| Glavier M et al. [44] | 2019 | France | GP | 287 GP | 21.9 E | Vaccination practices with chemotherapy patients: influenza, pneumococcal, DTP | Fax, mail or online | 5 |
| Hurley LP et al. [45] | 2018 | USA | PCP | FP, GIM (603) | 65.0 E | Zoster Vaccine Live (ZVL) and New Recombinant Zoster Vaccine (RZV) | Mail or online | 5 |
| Le Marechal M et al. [46] | 2018 | France | GP | 1582 GP | 42.5 E | Seasonal Influenza, HBV, HPV | Telephone | 5 |
| Levi M et al. [47] | 2018 | Italy | GP | 1245 GP | 12.4 E | Seasonal Influenza | Online | 4 |
| Merriel SWD et al. [48] | 2018 | UK | GP, SHCP | 38 GP | - | HPV | Online | 5 |
| Steben M et al. [49] | 2018 | Canada | GP, OB/GYN | 378 GP | 8.0 E | HPV | Online | 5 |
| Desiante F et al. [50] | 2017 | Italy | GP | 229 GP | 48.6 E | Influenza | Online | 3 |
| Hurley LP et al. [51] | 2017 | USA | PCP | 317 GIM, 236 FP (553) | 66.4 E | Adult vaccination: zoster, hepatitis B, Tdap, hepatitis A, HPV, Meningococcal, chicken pox, Td, PVC13, seasonal influenza, PPSV23, MMR | Mail or online | 4 |
| Hurley LP et al. [52] | 2016 | USA | PCP | 352 GIM, 255 FP (607) | 71.8 E | Adult vaccination: seasonal influenza, pneumococcal, Tdap, Td, herpes zoster, MMR | Mail or online | 7 |
| Raude J et al. [53] | 2016 | France | GP | 1582 GP | 92.4 E | MMR, MenC, HPV, HBV, seasonal influenza | Telephone | 7 |
| Verger P et al. [54] | 2016 | France | GP | 1582 GP | 46 E | Influenza, dTP, HBV, MMR, MenC, HPV | Telephone | 6 |
| Massin S et al. [55] | 2015 | France | GP | 1136 GP | 29.2 E | Influenza | Telephone | 3 |
| Alsaleem MA [56] | 2013 | Saudi Arabia | PHW | 95 PCP | 81.2 E | H1N1 vaccine | - | 4 |
| François M et al. [57] | 2011 | France | FP | 341 FP | 17.0 E | Hepatitis B | Online | 4 |
| Inoue Y et al. [58] | 2011 | Japan | GP | 515 GP | 51.5 T | Novel Pandemic Vaccine Influenza A/H1N1 | 6 | |
| Lutringer-Magnin D et al. [59] | 2011 | France | GP | 279 GP | 93.0 T | HPV | 6 | |
| Rurik I et al. [60] | 2011 | Hungary | FP | 198 FP | 85.0 E | Pandemic Influenza | Personally | 3 |
| Ward K et al. [61] | 2011 | Australia | HCW | 79 GP | 36.0 E | Annual Influenza Vaccination | 4 | |
NOS: Newcastle-Ottawa Scale. Study population: AC: Adult consumer; GP: General Practitioner; HCW: Healthcare worker; PCP: Primary care physician; PHW: Primary healthcare worker; SHCP: Sexual healthcare professional. Number and type of primary care participants: FP: Family Physician; GIM: General Internal Medicine; WS: Without specialization. Response rate: E: Calculated from eligible subjects; T: Calculated from total subjects.
Table 2.
Demographic factors and professional characteristics.
| Author | Age | Gender | Status | Experience (Years of Practice) | No. Patients | Type of Practice (Single/Group) | Occasional Practice Alternative Medicine |
|---|---|---|---|---|---|---|---|
| Statistical hypothesis testing between KBAB and own vaccination and patient recommendation | |||||||
| Verger P et al. [21] | ♀: ↓ | ||||||
| Verger P et al. [22] | >age: ↑ | ♀: ↓ | |||||
| Arlt J et al. [23] | |||||||
| Neufeind J et al. [24] | >age: ↓ [OV] >age: ↓ MEAS [PR] |
♂: ↑ MEAS [PR] | Yes: ↓ INF [PR] | ||||
| Verhees RAF et al. [25] | ≥60: ↑ [OV] | ♂: ↑ [OV] | |||||
| Vezzosi L et al. [26] | |||||||
| Yilmaz-Karadağ F et al. [27] | 31–40: ↑ INF + Td + HBV [OV] 31–40: ↑ INF + Td + PNV [PR] |
♀: ↑ INF [OV] ♂: ↑ PNV + Td [PR] |
≅ | ≅ | |||
| Akan H et al. [28] | >age: ↑ [OV] | ≅ | >years: ↑ [OV] | ||||
| Klett-Tammen CJ et al. [29] | |||||||
| Verger P et al. [30] | |||||||
| Flicoteaux R et al. [31] | |||||||
| Pulcini C et al. [32] | <age: ↑ [OV] | >no.: ↑ [OV] | ≅ | Yes: ↓ [OV] | |||
| Pulcini C et al. [33] | ≅ | ≅ | ≅ | ≅ | ≅ | ||
| Verger P et al. [34] | ≅ | ≅ | ≅ | Group: ↑ [OV] | Yes: ↓ [OV] | ||
| NO statistical hypothesis testing between KBAB and own vaccination and patient recommendation | |||||||
| Deruelle et al. [35] | |||||||
| Bayliss J et al. [36] | |||||||
| Hurley LP et al. [37] | |||||||
| Napolitano F et al. [38] | |||||||
| Celep G et al. [39] | |||||||
| Kalemaki D et al. [40] | <age: ↑ MEAS [OV] <age: ↓ INF [OV] |
♀: ↑ HBV [OV] | |||||
| Meites E et al. [41] | |||||||
| Awadlla NJ et al. [42] | |||||||
| Collange F et al. [43] | |||||||
| Glavier M et al. [44] | ≅ | ||||||
| Hurley LP et al. [45] | FP: ↑ ZVL [PR] | Small: ↑ ZVL [PR] | |||||
| Le Marechal M et al. [46] | |||||||
| Levi M et al. [47] | >age: ↑ seasonal INF >age: ↓ Td [OV] |
♂: ↑ seasonal INF, pandemic INF, PNV [OV] | >years: ↑ PNV >40 years: ↑ pandemic INF |
||||
| Merriel SWD et al. [48] | |||||||
| Steben M et al. [49] | ≅ | ||||||
| Desiante F et al. [50] | ≅ | ♂: ↑ [OV] | ≅ | >no.: ↑ [OV] | |||
| Hurley LP et al. [51] | ≅ | ||||||
| Hurley LP et al. [52] | |||||||
| Raude J et al. [53] | |||||||
| Verger P et al. [54] | ≅ | ≅ | ≅ | Yes: ↓ | |||
| Massin S et al. [55] | >age: ↑ pandemic INF [OV] | ♀: ↓ seasonal INF [OV] | High: ↑ seasonal + pandemic INF [OV] pandemic INF [PR] | Group: ↑ seasonal + pandemic INF [OV] | Yes: ↓ seasonal + pandemic INF [OV] | ||
| Alsaleem MA [56] | |||||||
| François M et al. [57] | >age: ↑ [PR] | ≅ | >3/day: ↑ [PR] | Yes: ↓ [PR] | |||
| Inoue Y et al. [58] | |||||||
| Lutringer-Magnin D et al. [59] | |||||||
| Rurik I et al. [60] | |||||||
| Ward K et al. [61] | |||||||
INF (influenza); HPV (human papillomavirus vaccine); HBV (hepatitis B); MEAS (measles); MMR (measles, mumps and rubella); PER (pertussis); PNV (pneumococcal vaccine); PPSV23 (pneumococcal polysaccharide vaccine); ZV (zoster vaccine); RVZ (recombinant zoster vaccine); ZVL (zoster live-attenuated vaccine); TT (tetanus vaccine); Td (tetanus-diphtheria); Tdap (tetanus, diphtheria, pertussis). [OV]: Own vaccination. [PR]: Patient recommendation. ≅ factor was not statistically significant; ↑ Factor leads to a statistically significant increase in own vaccination, patient recommendation; ↓ Factor leads to a statistically significant decrease in own vaccination, patient recommendation; ♀: Women; ♂: Man.
In addition, the intrinsic and extrinsic factors reported by each study and their influence on own vaccination and patient recommendation (if any) were extracted and, respectively, listed in a third table (Table 3).
Table 3.
Intrinsic and extrinsic factors reported by each study and their influence on OV&PR.
| Author | Data and Data-Sources | Knowledge | Safety | Efficacy/Benefits | Perceived Risk | Trust | Protection | Important |
|---|---|---|---|---|---|---|---|---|
| Verger P et al. [21] | - | - | Safe OR: 1.93 | - | No perceived risk OR: 0.47 | Trust in institutions OR: 0.86 | - | - |
| Verger P et al. [22] | - | - | Safe OR:0.27 | - | Perceived risk OR: 7.56 |
Trust in institutions OR: 0.10 | - | - |
| Arlt J et al. [23] | Co-workers OR: 2.26 Media News OR: 0.16 |
- | - | - | - | - | - | - |
| Neufeind J et al. [24] | Official Sources OR: 6.95 [INF] [PR] | - | Safe OR: 1.64 [INF] [PR] Safe OR: 1.28 [MEAS] [PR] Safe OR: 1.42 [INF, PER, HBV] [OV] |
- | - | Trust in institutions OR: 1.43 [INF] [PR] | - | No importance OR: 0.71 [INF, PER, HBV] [OV] |
| Verhees RAF et al. [25] | - | - | - | Efficacy p = 0.00 [OV] | - | - | - | - |
| Vezzosi L et al. [26] | - | GAP OR: 0.07 [ZV] [PR] | - | - | - | - | - | - |
| Yilmaz-Karadağ F et al. [27] | - | - | - | - | - | - | - | - |
| Akan H et al. [28] | - | - | Safe 1.55 < OR < 2.45 Median (OR): 2.08 |
Benefits 5.18 < OR < 9.29 Median (OR): 8.73 |
Perceived Risk 1.77 < OR < 7.49 Median (OR): 4.27 [OV] |
Trust in institutions OR: 2.52 | Natural Protection OR: 0.39 | - |
| Klett-Tammen CJ et al. [29] | - | - | - | - | - | - | - | - |
| Verger P et al. [30] | - | - | - | - | - | - | - | - |
| Flicoteaux R et al. [31] | Official Sources OR: 2.03 Media News OR: 0.57 |
- | Safe OR:0.17 [PR] | Efficacy OR: 0.28 [PR] | No Perceived Risk OR:0.6 [PR] |
- | - | - |
| Pulcini C et al. [32] | Internet OR: 0.92 [INF] | - | - | - | - | - | - | - |
| Pulcini C et al. [33] | Official Sources OR: 7.37 | - | - | - | No Dangerous disease OR: 0.32 [MEAS] [PR] |
- | - | - |
| Verger P et al. [34] | Official Sources p < 0.0001 No Media News p < 0.0001 |
- | Safe p < 0.0001 | Efficacy p < 0.0001 | Perceived Risk, Dangerous Disease p < 0.0001 | Trust in institutions p < 0.0001 [OV] | - | - |
| Author | Responsibility | Attitude | Extrinsic Factors | Practices (Behaviors) | Experiences | |||
| Verger P et al. [21] | - | - | - | - | - | |||
| Verger P et al. [22] | - | - | - | - | - | |||
| Arlt J et al. [23] | - | - | Organizational Factor OR: 4.31 [P] Patient Facilitator OR: 3.20 |
- | - | |||
| Neufeind J et al. [24] | Responsibility OR: 1.82 [INF, PER, HBV] [OV] | - | - | Vaccination History OR: 44.09 [INF] [R] | - | |||
| Verhees RAF et al. [25] | - | - | - | - | - | |||
| Vezzosi L et al. [26] | - | Attitude + OR: 13.67 [PNV, ZV] [R] | - | Vaccination History OR: 5.44 [PNV] [R] Vaccination History OR: 19.36 [ZV] [R] |
Patient Experience OR: 6.61 [ZV] [R] | |||
| Yilmaz-Karadağ F et al. [27] | - | - | - | Vaccination History p > 0.05 [R] | - | |||
| Akan H et al. [28] | - | Attitude + 3.06 < OR < 10.93 Median (OR): 7.245 |
Organizational Factor 2.64 < OR < 13.75 Median (OR): 6.57 |
Vaccination History OR: 15.1 Reminder System OR:1.66 |
- | |||
| Klett-Tammen CJ et al. [29] | - | - | - | - | - | |||
| Verger P et al. [30] | - | - | - | Vaccination History OR: 2.95 [INF] [R] Vaccination History OR: 1.90 [HBV] [R] |
- | |||
| Flicoteaux R et al. [31] | - | - | - | - | Patient Experience OR: 2.81 [R] PE (30.2%) |
|||
| Pulcini C et al. [32] | - | - | - | Vaccination History 1.08 < OR < 3.08 Mediana (OR): 1.2 [P] | - | |||
| Pulcini C et al. [33] | - | - | - | Check vaccination status OR: 3.38 | - | |||
| Verger P et al. [34] | - | - | - | - | - | |||
[OV]: Own vaccination; [PR]: patient recommendation; INF (influenza); HPV (human papillomavirus vaccine); HBV (hepatitis B); MEAS (measles); MMR (measles, mumps and rubella); PER (pertussis); PNV (pneumococcal vaccine); PPSV23 (pneumococcal polysaccharide vaccine); ZV (zoster vaccine); RVZ (recombinant zoster vaccine); ZVL (zoster live-attenuated vaccine); TT (tetanus vaccine); Td (tetanus-diphtheria); Tdap (tetanus, diphtheria, pertussis).
For studies that performed statistical hypothesis testing between the KBAB model and own vaccination and patient recommendation, we collected the relevant odds ratios (OR), and in any case where these were not available, the p-values and percentages. For results purposes, vaccines were classified into three groups: vaccines in general (studies that included a number of vaccines); influenza vaccine; and human papillomavirus (HPV) vaccine. This classification was chosen because a large proportion of the published studies included in our review addressed only influenza vaccine, a large proportion included only HPV vaccine, and the remaining studies addressed several vaccines at the same time. Data were extracted by two authors (RG, AP). Differences of opinion were resolved by discussion between the two authors, and if no agreement could be reached, it was left to AF and MZ to decide the matter.
2.5. Quality Assessment
To assess risk of bias in the studies selected for inclusion, we used the Newcastle-Ottawa Scale adapted for cross-sectional studies [20]. Two authors (RG, AP) independently assessed the quality of the studies. Any differences of opinion were resolved by consensus, and in any case where consensus could not be reached, the paper was then examined by AF and MZ.
3. Results
3.1. Search Results
The chosen strategy retrieved a total of 815 articles in MEDLINE/PubMed, 107 in Cochrane Library and 3 in EMBASE. After de-duplication, 802 studies were included. Examination of the abstracts led to 108 papers being selected for a reading of the full text. A total of 41 papers were finally included (Figure 1).
Figure 1.
Flow diagram of literature-review search process.
Screening process to identify the articles included in our systematic review.
3.2. Quality Assessment
Subject to the main limitations specific to cross-sectional studies, the studies generally displayed a similar quality. The median scores were as follows: scale item selection, 3/5; comparability, 0/2; and outcome, 2/3 (Table 1).
3.3. Characteristics of Selected Studies
The general characteristics of the studies are summarized in Table 1. The studies were drawn from four different continents, albeit mainly from Europe (n = 29): seven studies had been conducted in North America, three in Asia, and two in Oceania (Australia). The median sample size was 552, and the median response rate was 37.6% in papers that considered the eligible population.
All the studies selected were cross-sectional in nature, with 40 of them being quantitative and 1 classified as mixed [59]. Of the 38 papers, statistical hypothesis testing between KBAB and own vaccination and patient recommendation was found in 14 but not in the remaining 27.
The study population comprised general practitioners (n = 30), family physicians (n = 10), general internists (n = 5), and primary care physicians without specification (n = 2).
In terms of data-collection, all the studies used questionnaire. While 21 studies employed online questionnaires and 11 studies used mail questionnaires, 14 studies applied their questionnaire interviewing participants by telephone, 2 in person and 1 by fax.
3.4. Vaccines in General
Although we located 19 papers that examined KBAB in respect of multiple general vaccines, only 7 reported statistical hypothesis testing between the KBAB model and own vaccination and patient recommendation.
3.4.1. Studies without Statistical Hypothesis Testing between KBAB and Own Vaccination and Patient Recommendation
We found that the main data sources consulted were official and scientific information resources (n = 5), such as vaccination schedules. In some cases, PCP reported that the information received was inadequate. As regards the level of knowledge, as many as 8 papers reported shortfalls, due to ignorance of the composition of the vaccine or even of its very existence, misconceptions or lack of knowledge about health insurance cover in some countries, such as the USA.
With reference to vaccine safety, of all the papers which assessed this perception (n = 11), it was only in five that more than half of the PCP considered vaccines safe, since, in general, health professionals feared adverse reactions or long-term complications.
Similarly, when the perceived efficacy/benefits of vaccination were assessed in 11 papers, the participants were found to harbor many doubts about the utility of vaccines. Only in three studies did over half of the PCP believe in the benefits of the vaccine and its capacity to reduce complications. With respect to perceived risk (n = 10), 13% to 29% of physicians felt that there was no danger of suffering a vaccination-preventable disease and believed that they were not susceptible, except in 5 studies in which fear of suffering some chronic disease or presenting with some risk factor predominated. The importance attached by participants to vaccination (n = 5) was likewise found to be low: PCP showed themselves to be skeptical about the need for vaccination and did not consider it a priority.
Physicians’ attitudes toward vaccines were described in seven papers, which generally reported positive and favorable attitudes.
Certain external factors were seen to act as a barrier in the own vaccination and patient recommendation decision, with seven studies pinpointing organizational or logistical difficulties linked to the healthcare system, five papers detecting conflicts when it came to convincing the patient, and two studies identifying cost-related problems.
PCP’s previous practices were recorded in 10 papers. In most cases, these consisted of discussing vaccination with the patient, ascertaining patients’ vaccination status, using vaccine reminder systems, and storing vaccines.
3.4.2. Studies with Statistical Hypothesis Testing between KBAB and Own Vaccination and Patient Recommendation
The studies that cited data sources (n = 4) showed that browsing the Internet was associated with a lower recommendation of vaccination, in contrast to what occurred when official or scientific sources were accessed.
PCP’s previous own and routine vaccine practices had an impact on their recommendations (n = 5). Thus, their own proactive behavior vis-à-vis vaccination, the fact of being active in the recommendation of vaccines in general and making a practice of ascertaining their patients’ immunization status, all had a positive influence on own vaccination and patient recommendation.
The occasional practice of alternative medicine was associated with lower acceptance of vaccines in two papers.
3.5. Influenza Vaccines
A total of 12 papers examined KBAB associated with the influenza vaccine, with statistical hypothesis testing for the KBAB model and own vaccination and patient recommendation being reported in five.
3.5.1. Studies without Statistical Hypothesis Testing between KBAB and Own Vaccination and Patient Recommendation
The data sources consulted were diverse and were described in four papers. In two of these, the participants reported receiving very little information from the relevant public institutions. The level of knowledge among PCP was not adequate: proof of this is that gaps or misconceptions were identified in five papers.
While vaccine safety was questioned in eight papers, 40% to 90% of PCP considered the vaccine safe in only two, and PCP reported doubts about the efficacy and benefits of vaccines in another three. Whereas the perceived risk (n = 8) of being susceptible or falling ill was seen as non-existent by most participants in four papers and in another four, one or more PCP was found to be risk averse. We located five papers which referred to the protection offered by the vaccine. The participants attached greatest value to personal protection, followed by protection of their patients, relatives, and friends. The trust placed by PCP in pharmaceutical companies or in reported data was found to be scant, which can be explained by previous studies that have shown that healthcare professionals believe that the pharmaceutical industry seeks financial gain through the sale of its products and control in clinical trials, rather than patient safety [62,63].
External factors that might act as drawbacks for acceptance of the vaccine (n = 7) related to the healthcare system and the way it was organized, and/or to financial barriers.
3.5.2. Studies with Statistical Hypothesis Testing between KBAB and Own Vaccination and Patient Recommendation
When it came to data sources (n = 3), those of an official origin led to good own vaccination and patient recommendation practices, whereas those stemming from the mass media or involving disinformation had the contrary effect.
Believing in the efficacy or benefits of the vaccine (n = 4) and considering it to be safe (n = 3) were the factors most closely related with acceptance of the influenza vaccine. Hence, believing the vaccine to be safe and effective was positively linked to own vaccination and patient recommendation, and doubting its safety or efficacy was associated with lower acceptance of the vaccine.
The following were also associated with favorable behavior in own vaccination and patient recommendation: (1) perceived risk of contracting the disease or experiencing a severe form of it; (2) trust in the health authorities; (3) changing vaccine efficacy from year to year, healthcare organization and patients, all of which acted as external factors; and (4) previous practices or favorable behaviors with respect to other vaccines and past history of vaccination.
More advanced ages and group practices showed a statistically positive correlation with higher vaccination rates among PCP. Having longer clinical experience and a greater burden of care were also associated with favorable results in own vaccination and patient recommendation, whereas occasional practice of alternative medicine decreased vaccination.
3.6. HPV Vaccines
Studies without Statistical Hypothesis Testing between KBAB and Own Vaccination and Patient Recommendation
All the papers that furnished information on HPV vaccine and KBAB (n = 6) were descriptive. Most physicians consulted official data-sources or scientific journals (n = 4), and some PCP were confused about the guidelines due to lack of information. Despite the variability of knowledge evaluated by each study in response to the questions posed, all highlighted shortfalls (n = 4), particularly when it came to vaccination counselling afforded to older and/or male patients versus young woman patients.
In general, while PCP did not fear the adverse effects of vaccine, 10% to 37% displayed uneasiness about its safety in three studies. In these same papers, most of the participants acknowledged the benefits and efficacy of the vaccine in the prevention of HPV-related diseases.
The studies that described communication with patients about vaccination (n = 4) reflected good practices. In other words, most PCP discussed the benefits and risks of the HPV vaccine, informed young women about it, and collected data on sexual practices.
3.7. COVID-19 Vaccines
We found three papers (one of them descriptive) that assessed vaccination against SARS-CoV-2, the cause of the current COVID-19 pandemic. In all the articles, participants reported concerns about the safety of vaccines due to their rapid development in a pandemic situation, as well as lack of trust in the health authorities and the information they provide. Finally, low perceived risk among those who consider that the pandemic is not serious and have not received influenza vaccine in previous practices are also related to lower acceptance of COVID-19 vaccines.
4. Discussion
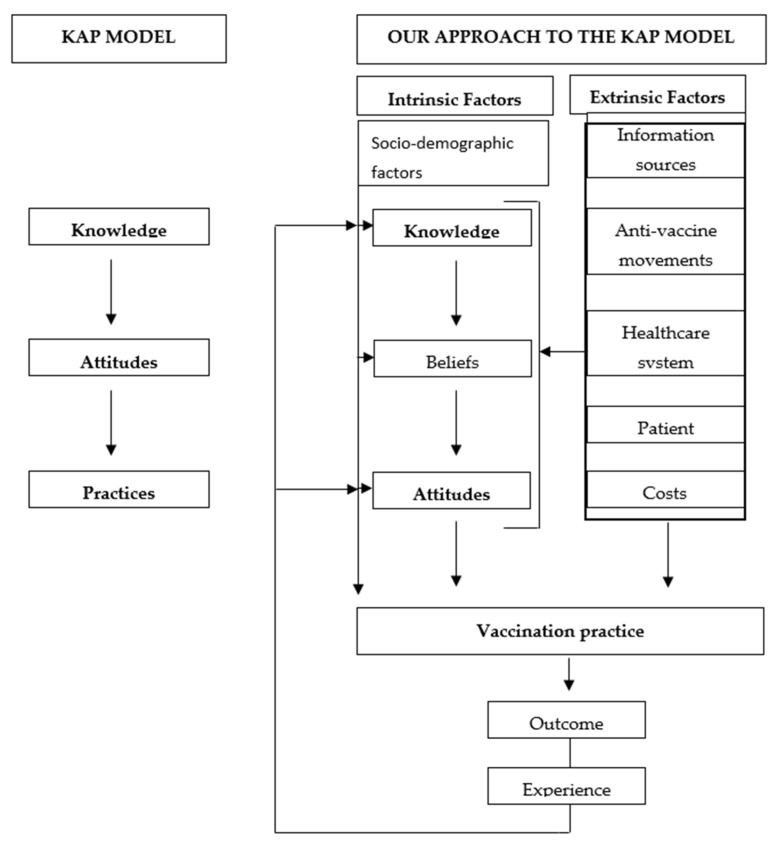
Currently one of the main public health challenges is vaccine hesitancy, particularly in the adult population. PCP can play a decisive role in encouraging immunization among their patients because they are not only the main professionals offering vaccine counselling to them, but also their most important source of information. To explain the own vaccination and patient recommendation process, we proposed a modified KAP model (Figure 2).
Figure 2.
Theoretical framework of the influence of and interconnection among factors that influence vaccination practices (based on A. Teixeira Rodrigues et al.’s model).
When it comes to deciding on their own vaccination or on counselling and making recommendations to patients, physicians’ lack of the necessary knowledge is an obstacle that can, in great measure, hinder the process [26,33,45,48,56,59]. To obtain the proper knowledge, it is essential to have access to data sources based on scientific evidence or official resources (EMA, CDC, FDA), which are linked to with higher own vaccination and patient recommendation [24,29,31,33,34,64,65].
According to our model, beliefs are formed based on knowledge, and it therefore follows that if the latter is inappropriate or inadequate, the resulting beliefs are not going to be accurate. Believing that the vaccine is safe [24,28,34] and effective [28,34], and trusting in health institutions [24,28,34] are positively related with own vaccination and patient recommendation, as are being aware of the risk [28,34] and feeling responsible for the vaccination process [24]. Since hesitancy is not stable, strategies can be put in place to reduce it; combating misinformation in networks and the media; informing the process of vaccine development; and increasing credibility in the institutions.
Interestingly, very few studies included in our review displayed an association between socio-demographic factors and own vaccination and patient recommendation, something that is relevant, given that these are not modifiable factors. These results are in line with those of other reviews of physicians’ behavior in matters such as notification of adverse drug reactions [66] or prescription of antibiotics [67]. Only the practice of alternative medicine (homeopathy, acupuncture, etc.) was negatively associated with own vaccination and patient recommendation in a number of studies [24,32,34,54,55,57]. It could be explained because the practice of alternative medicine brings with it a distrustful attitude toward conventional medicine and concerns about the safety of medicines. In addition, disinformation and anti-vaccine campaigns often recommend alternative practices [68].
Our analysis highlights the fact that there are other extrinsic factors, proposed in the modified KAP model, which influence own vaccination and patient recommendation. Hence, there are a number of coexisting determinants that are related with: the patient (baseline level of vaccination hesitancy and resistance to vaccination) [69]. It is therefore important to implement: (1) physician communication training, essentially equipping PCP with the necessary persuasive skills to enable them to convey the importance of vaccination to their patients; and (2) awareness-raising campaigns and educational programs targeted at the entire population, which could serve to counteract the disinformation published by anti-vaccine groups [70,71,72].
Lastly, according to our model, the health outcomes (effectiveness, non-prevention of the disease, adverse reactions) observed in previous vaccination campaigns, generate clinical experiences [22,27] for PCP which may be decisive, on interfering -positively or negatively- in KBAB and, by extension, in ensuing behaviors [24,26,28,29,30,32,33] (Figure 2).
To date, very few specific interventions have been undertaken to reduce vaccine hesitancy on the part of PCP [73,74,75] but none of these has yielded the benefits that were sought [76]. In order for interventions to be effective, they will probably have to be purpose-designed on the basis of gaps identified in the health professionals working in this area [77,78,79]. An improvement in professionals’ communication skills might also enhance the effectiveness of such interventions, as has been shown in other settings [80].
Some of the limitations of our review stem from the quality of the studies included: (1) most of the studies only furnish descriptive information, without performing an analysis of the statistical association between KBAB and own vaccination and patient recommendation (n = 25); (2) the fact that the outcome measure (vaccination) was questionnaire- as opposed to record-based, implies that there may be a misclassification risk; (3) use of questionnaires which are not fully validated means that important factors may not have been included in the questionnaires, or that there may be misclassification in the exposures; and (4) several studies did not have a satisfactory response rate or sample size and failed to compare their participants against subjects who did not participate so as to assess the risk of selection bias.
Insofar as the review itself is concerned, the main limitation is the heterogeneity present in the definition of the variables, and the way in which these were measured by the component studies, something that makes it impossible to conduct a meta-analysis, and means that on many occasions, when the studies did not define the variables, this work was done by the authors. Future studies will be needed to study the influence of knowledge, beliefs, attitudes and barriers on adult vaccination, and in which the dependent variable (full adult vaccination yes/no) is based on vaccination records, and in which the questionnaires used are fully validated, as has already been done successfully in other domains, such as determinants of antibiotic prescribing, antibiotic dispensing or adverse reaction reporting [67,81].
Main model of attitudes, knowledge and practices, modified by the conditioning factors of vaccination in our systematic review.
5. Conclusions
The own vaccination and patient recommendation decision is a complex process in which multiple factors come into play. The own vaccination and patient recommendation decision is a complex process in which multiple factors come into play. This study is a first step to identify those factors, which are responsible for increasing vaccine hesitancy in society and among health professionals. Now, it is time to take action on each of the identified factors: by facilitating access to accurate information about vaccines on the internet, by involving PCPs in setting recommendations, by strengthening their communication skills and reminder systems, and developing specific multi-component interventions for their training.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ijerph192113872/s1, Table S1: Intrinsic and extrinsic factors reported by each study and their influence on vaccination/recommendation. Table S2: Quality NOS * assessment, * Newcastle-Ottawa scale for cross-sectional studies.
Author Contributions
Conceptualization, M.Z.-C., M.T.H., F.R. and A.F.; methodology, M.Z.-C., M.T.H., F.R., A.F., Á.P.-C. and R.M.G.-Á.; validation, formal analysis, investigation, M.Z.-C., M.T.H., F.R., A.L.-D. and A.F.; resources, data curation, writing—original draft preparation, Á.P.-C. and R.M.G.-Á.; writing—review and editing, Á.P.-C. and R.M.G.-Á.; visualization, M.Z.-C., M.T.H., F.R. and A.F.; supervision, M.Z.-C., M.T.H., F.R., A.L.-D. and A.F.; project administration, M.Z.-C., M.T.H., F.R., A.L.-D. and A.F. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Mehta B., Chawla S., Kumar V., Jindal H., Bhatt B. Adult immunization: The need to address. Hum. Vaccines Immunother. 2014;10:306–309. doi: 10.4161/hv.26797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Weniger B.G., Papania M.J. Vaccines. Elsevier; Amsterdam, The Netherlands: 2013. Alternative vaccine delivery methods; pp. 1200–1231. [DOI] [Google Scholar]
- 3.Ecarnot F., Maggi S., Michel J.P. Strategies to Improve Vaccine Uptake throughout Adulthood. Interdiscip. Top Gerontol. Geriatr. 2020;43:234–248. doi: 10.1159/000504486. [DOI] [PubMed] [Google Scholar]
- 4.Arribas J.L., Hernández-Navarrete M.J., Solano V.M. Adult vaccination update. Enferm. Infecc. Microbiol. Clin. 2004;22:342–354. doi: 10.1157/13063047. [DOI] [PubMed] [Google Scholar]
- 5.Nanni A., Meredith S., Gati S., Holm K., Harmon T., Ginsberg A. Strengthening global vaccine access for adolescents and adults. Vaccine. 2017;35:6823–6827. doi: 10.1016/j.vaccine.2017.10.023. [DOI] [PubMed] [Google Scholar]
- 6.Burki T. The online anti-vaccine movement in the age of COVID-19. Lancet Digit. Health. 2020;2:e504–e505. doi: 10.1016/S2589-7500(20)30227-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.World Health Organization Ten threats to global health in 2019. 2018. [(accessed on 28 June 2021)]. Available online: https://www.who.int/es/news-room/spotlight/ten-threats-to-global-health-in-2019.
- 8.World Health Organization Immunization Agenda 2030: A Global Strategy To Leave No One Behind. 2020. [(accessed on 14 October 2022)]. Available online: https://www.who.int/publications/m/item/immunization-agenda-2030-a-global-strategy-to-leave-no-one-behind.
- 9.Starfield B., Shi L., Macinko J. Contribution of primary care to health systems and health. Milbank Q. 2005;83:457–502. doi: 10.1111/j.1468-0009.2005.00409.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Maltezou H.C., Wicker S., Borg M., Heininger U., Puro V., Theodoridou M., Poland G.A. Vaccination policies for health-care workers in acute health-care facilities in Europe. Vaccine. 2011;29:9557–9562. doi: 10.1016/j.vaccine.2011.09.076. [DOI] [PubMed] [Google Scholar]
- 11.Campos-Outcast D., Jeffcott-Pera M., Carter-Smith P., Schoof B.K., Young H.F. Vaccines provided by family physicians. Ann. Fam. Med. 2010;8:507–510. doi: 10.1370/afm.1185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bovier P.A., Chamot E., Bouvier Gallacchi M., Loutan L. Importance of patients’ perceptions and general practitioners’ recommendations in understanding missed opportunities for immunisations in Swiss adults. Vaccine. 2001;19:4760–4767. doi: 10.1016/S0264-410X(01)00223-7. [DOI] [PubMed] [Google Scholar]
- 13.Godoy P., Castilla J., Mayoral J.M., Martín V., Astray J., Torner N., Toledo D., Soldevila N., González-Candelas F., García S., et al. Influenza vaccination of primary healthcare physicians may be associated with vaccination in their patients: A vaccination coverage study. BMC Fam. Pract. 2015;16:44. doi: 10.1186/s12875-015-0259-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Paterson P., Meurice F., Stanberry L.R., Glismann S., Rosenthal S.L., Larson H.J. Vaccine hesitancy and healthcare providers. Vaccine. 2016;34:6700–6706. doi: 10.1016/j.vaccine.2016.10.042. [DOI] [PubMed] [Google Scholar]
- 15.Lin C., Mullen J., Smith D., Kaplan S.J., Tu P. Healthcare Providers’ Vaccine Perceptions, Hesitancy, and Recommendation to Patients: A Systematic Review. Vaccines. 2021;9:713. doi: 10.3390/vaccines9070713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Herzog R., Álvarez-Pasquin M.J., Díaz C., Del Barrio J.L., Estrada J.M., Gil Á. Are healthcare workers’ intentions to vaccinate related to their knowledge, beliefs and attitudes? A systematic review. BMC Public Health. 2013;13:154. doi: 10.1186/1471-2458-13-154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pavlovic D., Sahoo P., Larson H.J., Karafillakis E. Factors influencing healthcare professionals’ confidence in vaccination in Europe: A literature review. Hum. Vaccines Immunother. 2022;18:2041360. doi: 10.1080/21645515.2022.2041360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Collange F., Verger P., Launay O., Pulcini C. Knowledge, attitudes, beliefs and behaviors of general practitioners/family physicians toward their own vaccination: A systematic review. Hum. Vaccines Immunother. 2016;12:1282–1292. doi: 10.1080/21645515.2015.1138024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liberati A., Altman D.G., Tetzlaff J., Mulrow C., Gøtzsche P.C., Ioannidis J.P., Clarke M., Devereaux P.J., Kleijnen J., Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. J. Clin. Epidemiol. 2009;62:e1–e34. doi: 10.1016/j.jclinepi.2009.06.006. [DOI] [PubMed] [Google Scholar]
- 20.Moskalewicz A., Oremus M. No clear choice between Newcastle-Ottawa Scale and Appraisal Tool for Cross-Sectional Studies to assess methodological quality in cross-sectional studies of health-related quality of life and breast cancer. J. Clin. Epidemiol. 2020;120:94–103. doi: 10.1016/j.jclinepi.2019.12.013. [DOI] [PubMed] [Google Scholar]
- 21.Verger P., Scronias D., Fradier Y., Meziani M., Ventelou B. Online study of health professionals about their vaccination attitudes and behaviour in the COVID-19 era: Addressing participation bias. Hum. Vaccines Immunother. 2021;17:2934–3939. doi: 10.1080/21645515.2021.1921523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Verger P., Scronias D. Changes in general practitioners’ attitudes toward COVID-19 vaccination after first interim results: A longitudinal approach in France. Hum. Vaccines Immunother. 2021;17:3408–3412. doi: 10.1080/21645515.2021.1943990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Arlt J., Flaegel K., Goetz K., Steinhaeuser J. Regional differences in general practitioners’ behaviours regarding influenza vaccination: A cross-sectional study. BMC Health Serv. Res. 2021;21:197. doi: 10.1186/s12913-021-06177-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Neufeind J., Betsch C., Habersaat K.B., Eckardt M., Schmid P., Wichmann O. Barriers and drivers to adult vaccination among family physicians—Insights for tailoring the immunization program in Germany. Vaccine. 2020;38:4252–4262. doi: 10.1016/j.vaccine.2020.04.052. [DOI] [PubMed] [Google Scholar]
- 25.Verhees R.A.F., Snellings R., Dinant G.J., Knottnerus J.A. Influenza vaccination among Dutch general practitioners and their attitude toward influenza vaccination in the elderly. Hum. Vaccines Immunother. 2020;16:2709–2718. doi: 10.1080/21645515.2020.1732728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vezzosi L., Riccò M., Agozzino E., Odone A., Signorelli C. Knowledge, attitudes, and practices of General Practitioners from the Province of Parma (Northern Italy) towards vaccinations in adults ≥65 year-old. Acta Biomed. 2019;90:71–75. doi: 10.23750/abm.v90i9-S.8704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yılmaz Karadağ F., Sağlam Z.A. Assessment of the factors influencing primary care physicians’ approach to vaccination of adult risk groups in Istanbul, Turkey. PeerJ. 2019;7:e7516. doi: 10.7717/peerj.7516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Akan H., Yavuz E., Yayla M.E., Külbay H., Kaspar E.Ç., Zahmacıoğlu O., Badur S. Factors affecting uptake of influenza vaccination among family physicians. Vaccine. 2016;34:1712–1718. doi: 10.1016/j.vaccine.2016.01.057. [DOI] [PubMed] [Google Scholar]
- 29.Klett-Tammen C.J., Krause G., von Lengerke T., Castell S. Advising vaccinations for the elderly: A cross-sectional survey on differences between general practitioners and physician assistants in Germany. BMC Fam. Pract. 2016;17:98. doi: 10.1186/s12875-016-0502-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Verger P., Fressard L., Collange F., Gautier A., Jestin C., Launay O., Raude J., Pulcini C., Peretti-Watel P. Vaccine Hesitancy Among General Practitioners and Its Determinants During Controversies: A National Cross-sectional Survey in France. EBioMedicine. 2015;2:891–897. doi: 10.1016/j.ebiom.2015.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Flicoteaux R., Pulcini C., Carrieri P., Schwarzinger M., Leport C., Verger P. Correlates of general practitioners’ recommendations to patients regarding vaccination for the 2009–2010 pandemic influenza (A/H1N1) in France: Implications for future vaccination campaigns. Vaccine. 2014;32:2281–2287. doi: 10.1016/j.vaccine.2014.02.074. [DOI] [PubMed] [Google Scholar]
- 32.Pulcini C., Massin S., Launay O., Verger P. Factors associated with vaccination for hepatitis B, pertussis, seasonal and pandemic influenza among French general practitioners: A 2010 survey. Vaccine. 2013;31:3943–3949. doi: 10.1016/j.vaccine.2013.06.039. [DOI] [PubMed] [Google Scholar]
- 33.Pulcini C., Massin S., Launay O., Verger P. Knowledge, attitudes, beliefs and practices of general practitioners towards measles and MMR vaccination in southeastern France in 2012. Clin. Microbiol. Infect. 2014;20:38–43. doi: 10.1111/1469-0691.12194. [DOI] [PubMed] [Google Scholar]
- 34.Verger P., Flicoteaux R., Schwarzinger M., Sagaon-Teyssier L., Peretti-Watel P., Launay O., Sebbah R., Moatti J.P. Pandemic influenza (A/H1N1) vaccine uptake among French private general practitioners: A cross sectional study in 2010. PLoS ONE. 2012;7:e41837. doi: 10.1371/journal.pone.0041837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Deruelle P., Couffignal C., Sibiude J., Vivanti A.J., Anselem O., Luton D., Benachi A., Mandelbrot L., Vauloup-Fellous C., Cordier A.G., et al. Prenatal care providers´perceptions of the SARS-Cov-2 vaccine for themselves and for pregnant women. PLoS ONE. 2021;16:e0256080. doi: 10.1371/journal.pone.0256080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bayliss J., Randhawa R., Oh K.B., Kandeil W., Jenkins V.A., Turriani E., Nissen M. Perceptions of vaccine preventable diseases in Australian healthcare: Focus on pertussis. Hum. Vaccines Immunother. 2021;17:344–350. doi: 10.1080/21645515.2020.1780848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hurley L.P., O’Leary S.T., Markowitz L.E., Crane L.A., Cataldi J.R., Brtnikova M., Beaty B.L., Gorman C., Meites E., Lindley M.C., et al. US Primary Care Physicians’ Viewpoints on HPV Vaccination for Adults 27 to 45 Years. J. Am. Board Fam. Med. 2021;34:162–170. doi: 10.3122/jabfm.2021.01.200408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Napolitano F., Pelullo C.P., Della Polla G., Angelillo I.F. HPV Vaccination Attitudes and Behaviors among General Practitioners in Italy. Vaccines. 2021;9:63. doi: 10.3390/vaccines9010063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Celep G., Duyan Çamurdan A., Baran Aksakal F.N., Kara O.F. Different perspectives of immunizations during pregnancy. Turk. J. Med. Sci. 2020;50:316–323. doi: 10.3906/sag-1910-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kalemaki D., Karakonstantis S., Galanakis E., Lionis C. Vaccination coverage of general practitioners: A cross-sectional study from Greece. Public Health. 2020;181:110–113. doi: 10.1016/j.puhe.2019.12.012. [DOI] [PubMed] [Google Scholar]
- 41.Meites E., Markowitz L.E., Kempe A., O’Leary S.T., Crane L.A., Hurley L.P., Brtnikova M., Beaty B.L., Stokley S., Lindley M.C. Primary care physician support for harmonizing HPV vaccination recommendations across genders—United States, 2018. Vaccine. 2020;38:3699–3701. doi: 10.1016/j.vaccine.2020.03.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Awadalla N.J., Al-Musa H.M., Al-Musa K.M., Asiri A.M., Albariqi A.A., Majrashi H.M., Alasim A.A., Almuslah A.S., Alshehri T.K., AlFlan M.A., et al. Seasonal influenza vaccination among primary health care workers in Southwestern Saudi Arabia. Hum. Vaccines Immunother. 2020;16:321–326. doi: 10.1080/21645515.2019.1666500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Collange F., Zaytseva A., Pulcini C., Bocquier A., Verger P. Unexplained variations in general practitioners’ perceptions and practices regarding vaccination in France. Eur. J. Public Health. 2019;29:2–8. doi: 10.1093/eurpub/cky146. [DOI] [PubMed] [Google Scholar]
- 44.Glavier M., Puyade M., Roblot F., Rammaert B. Vaccination of cancer patients treated with chemotherapy: A survey among general practitioners. Med. Mal. Infect. 2019;49:586–592. doi: 10.1016/j.medmal.2019.09.004. [DOI] [PubMed] [Google Scholar]
- 45.Hurley L.P., Allison M.A., Dooling K.L., O’Leary S.T., Crane L.A., Brtnikova M., Beaty B.L., Allen J.A., Guo A., Lindley M.C., et al. Primary care physicians’ experience with zoster vaccine live (ZVL) and awareness and attitudes regarding the new recombinant zoster vaccine (RZV) Vaccine. 2018;36:7408–7414. doi: 10.1016/j.vaccine.2018.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Le Marechal M., Fressard L., Agrinier N., Verger P., Pulcini C. General practitioners’ perceptions of vaccination controversies: A French nationwide cross-sectional study. Clin. Microbiol. Infect. 2018;24:858–864. doi: 10.1016/j.cmi.2017.10.021. [DOI] [PubMed] [Google Scholar]
- 47.Levi M., Bonanni P., Biffino M., Conversano M., Corongiu M., Morato P., Maio T. Influenza vaccination 2014–2015: Results of a survey conducted among general practitioners in Italy. Hum. Vaccines Immunother. 2018;14:1342–1350. doi: 10.1080/21645515.2018.1430543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Merriel S.W.D., Flannagan C., Kesten J.M., Shapiro G.K., Nadarzynski T., Prue G. Knowledge and Attitudes of General Practitioners and Sexual Health Care Professionals Regarding Human Papillomavirus Vaccination for Young Men Who Have Sex with Men. Int. J. Environ. Res. Public Health. 2018;15:151. doi: 10.3390/ijerph15010151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Steben M., Durand N., Guichon J.R., Greenwald Z.R., McFaul S., Blake J. A National Survey of Canadian Physicians on HPV: Knowledge, Barriers, and Preventive Practices. J. Obstet. Gynaecol. Can. 2019;41:599–607.E3. doi: 10.1016/j.jogc.2018.09.016. [DOI] [PubMed] [Google Scholar]
- 50.Desiante F., Caputi G., Cipriani R., Nanula C., Aprile I., Pesare A., Conversano M. Assessment of coverage and analysis of the determinants of adherence to influenza vaccination in the general practitioners of Taranto. Ann. Ig. 2017;29:256–263. doi: 10.7416/ai.2017.2157. [DOI] [PubMed] [Google Scholar]
- 51.Hurley L.P., Lindley M.C., Allison M.A., Crane L.A., Brtnikova M., Beaty B.L., Snow M., Bridges C.B., Kempe A. Primary care physicians’ perspective on financial issues and adult immunization in the Era of the Affordable Care Act. Vaccine. 2017;35:647–654. doi: 10.1016/j.vaccine.2016.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hurley L.P., Bridges C.B., Harpaz R., Allison M.A., O’Leary S.T., Crane L.A., Brtnikova M., Stokley S., Beaty B.L., Jimenez-Zambrano A., et al. Physician Attitudes Toward Adult Vaccines and Other Preventive Practices, United States, 2012. Public Health Rep. 2016;131:320–330. doi: 10.1177/003335491613100216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Raude J., Fressard L., Gautier A., Pulcini C., Peretti-Watel P., Verger P. Opening the ‘Vaccine Hesitancy’ black box: How trust in institutions affects French GPs’ vaccination practices. Expert Rev. Vaccines. 2016;15:937–948. doi: 10.1080/14760584.2016.1184092. [DOI] [PubMed] [Google Scholar]
- 54.Verger P., Collange F., Fressard L., Bocquier A., Gautier A., Pulcini C., Raude J., Peretti-Watel P. Prevalence and correlates of vaccine hesitancy among general practitioners: A cross-sectional telephone survey in France, April to July 2014. Euro Surveill. 2016;21:30406. doi: 10.2807/1560-7917.ES.2016.21.47.30406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Massin S., Ventelou B., Nebout A., Verger P., Pulcini C. Cross-sectional survey: Risk-averse French general practitioners are more favorable toward influenza vaccination. Vaccine. 2015;33:610–614. doi: 10.1016/j.vaccine.2014.12.038. [DOI] [PubMed] [Google Scholar]
- 56.Alsaleem M.A. Acceptance of H1N1 vaccine among healthcare workers at primary healthcare centres in Abha, KSA. J. Egypt Public Health Assoc. 2013;88:32–39. doi: 10.1097/01.EPX.0000426292.89751.ca. [DOI] [PubMed] [Google Scholar]
- 57.François M., Alla F., Rabaud C., Raphaël F. Hepatitis B virus vaccination by French family physicians. Med. Mal. Infect. 2011;41:518–525. doi: 10.1016/j.medmal.2011.07.002. [DOI] [PubMed] [Google Scholar]
- 58.Inoue Y., Matsui K. Physicians’ recommendations to their patients concerning a novel pandemic vaccine: A cross-sectional survey of the 2009 influenza A/H1N1 pandemic in Japan. Environ. Health Prev. Med. 2011;16:320–326. doi: 10.1007/s12199-010-0202-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lutringer-Magnin D., Kalecinski J., Barone G., Leocmach Y., Regnier V., Jacquard A.C., Soubeyrand B., Vanhems P., Chauvin F., Lasset C. Human papillomavirus (HPV) vaccination: Perception and practice among French general practitioners in the year since licensing. Vaccine. 2011;29:5322–5328. doi: 10.1016/j.vaccine.2011.05.006. [DOI] [PubMed] [Google Scholar]
- 60.Rurik I., Langmár Z., Márton H., Kovács E., Szigethy E., Ilyés I. Knowledge, motivation, and attitudes of Hungarian family physicians toward pandemic influenza vaccination in the 2009/10 influenza season: Questionnaire study. Croat. Med. J. 2011;52:134–140. doi: 10.3325/cmj.2011.52.134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ward K., Seale H., Zwar N., Leask J., Macintyre C.R. Annual influenza vaccination: Coverage and attitudes of primary care staff in Australia. Influenza Other Respir. Viruses. 2011;5:135–141. doi: 10.1111/j.1750-2659.2010.00158.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Holzmann-Littig C., Braunisch M.C., Kranke P., Popp M., Seeber C., Fichtner F., Littig B., Carbajo-Lozoya J., Allwang C., Frank T., et al. COVID-19 Vaccination Acceptance and Hesitancy among Healthcare Workers in Germany. Vaccines. 2021;9:777. doi: 10.3390/vaccines9070777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Tracy C.S., Dantas G.C., Upshur R.E. Evidence-based medicine in primary care: Qualitative study of family physicians. BMC Fam. Pract. 2003;4:6. doi: 10.1186/1471-2296-4-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Karafillakis E., Dinca I., Apfel F., Cecconi S., Wűrz A., Takacs J., Suk J., Celentano L.P., Kramarz P., Larson H.J. Vaccine hesitancy among healthcare workers in Europe: A qualitative study. Vaccine. 2016;34:5013–5020. doi: 10.1016/j.vaccine.2016.08.029. [DOI] [PubMed] [Google Scholar]
- 65.Larson H.J., Jarrett C., Eckersberger E., Smith D.M., Paterson P. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: A systematic review of published literature, 2007–2012. Vaccine. 2014;32:2150–2159. doi: 10.1016/j.vaccine.2014.01.081. [DOI] [PubMed] [Google Scholar]
- 66.Gonzalez-Gonzalez C., Lopez-Gonzalez E., Herdeiro M.T., Figueiras A. Strategies to improve adverse drug reaction reporting: A critical and systematic review. Drug Saf. 2013;36:317–328. doi: 10.1007/s40264-013-0058-2. [DOI] [PubMed] [Google Scholar]
- 67.Zapata-Cachafeiro M., González-González C., Váquez-Lago J.M., López-Vázquez P., López-Durán A., Smyth E., Figueiras A. Determinants of antibiotic dispensing without a medical prescription: A cross-sectional study in the north of Spain. J. Antimicrob. Chemother. 2014;69:3156–3160. doi: 10.1093/jac/dku229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Zuzak T.J., Zuzak-Siegrist I., Rist L., Staubli G., Simoes-Wüst A.P. Attitudes towards vaccination: Users of complementary and alternative medicine versus non-users. Swiss Med. Wkly. 2008;138:713–718. doi: 10.4414/smw.2008.12423. [DOI] [PubMed] [Google Scholar]
- 69.Baars E.W., Zoen E.B., Breitkreuz T., Martin D., Matthes H., von Schoen-Angerer T., Soldner G., Vagedes J., van Wietmarschen H., Patijn O., et al. The Contribution of Complementary and Alternative Medicine to Reduce Antibiotic Use: A Narrative Review of Health Concepts, Prevention, and Treatment Strategies. Evid.-Based Complement. Alternat. Med. 2019;2019:5365608. doi: 10.1155/2019/5365608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Durando P., Alicino C., Dini G., Barberis I., Bagnasco A.M., Iudici R., Zanini M., Martini M., Toletone A., Paganino C., et al. Determinants of adherence to seasonal influenza vaccination among healthcare workers from an Italian region: Results from a cross-sectional study. BMJ Open. 2016;6:e010779. doi: 10.1136/bmjopen-2015-010779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Tafuri S., Gallone M.S., Cappelli M.G., Martinelli D., Prato R., Germinario C. Addressing the anti-vaccination movement and the role of HCWs. Vaccine. 2014;32:4860–4865. doi: 10.1016/j.vaccine.2013.11.006. [DOI] [PubMed] [Google Scholar]
- 72.Succi R.C.M. Vaccine refusal—What we need to know. J. Pediatr. Rio J. 2018;94:574–581. doi: 10.1016/j.jped.2018.01.008. [DOI] [PubMed] [Google Scholar]
- 73.Jarrett C., Wilson R., O’Leary M., Eckersberger E., Larson H.J., SAGE Working Group on Vaccine Hesitancy Strategies for addressing vaccine hesitancy—A systematic review. Vaccine. 2015;33:4180–4190. doi: 10.1016/j.vaccine.2015.04.040. [DOI] [PubMed] [Google Scholar]
- 74.Uskun E., Uskun S.B., Uysalgenc M., Yagiz M. Effectiveness of a training intervention on immunization to increase knowledge of primary healthcare workers and vaccination coverage rates. Public Health. 2008;122:949–958. doi: 10.1016/j.puhe.2007.10.005. [DOI] [PubMed] [Google Scholar]
- 75.Llupià A., García-Basteiro A.L., Olivé V., Costas L., Ríos J., Quesada S., Varela P., Bayas J.M., Trilla A. New interventions to increase influenza vaccination rates in health care workers. Am. J. Infect. Control. 2010;38:476–481. doi: 10.1016/j.ajic.2010.01.013. [DOI] [PubMed] [Google Scholar]
- 76.Dubé E., Gagnon D., MacDonald N.E. Strategies intended to address vaccine hesitancy: Review of published reviews. Vaccine. 2015;33:4191–4203. doi: 10.1016/j.vaccine.2015.04.041. [DOI] [PubMed] [Google Scholar]
- 77.Figueiras A., Herdeiro M.T., Polonia J., Gestal-Otero J.J. An educational intervention to improve physician reporting of adverse drug reactions: A cluster-randomized controlled trial. JAMA. 2006;296:1086–1093. doi: 10.1001/jama.296.9.1086. [DOI] [PubMed] [Google Scholar]
- 78.Herdeiro M.T., Polonia J., Gestal-Otero J.J., Figueiras A. Improving the reporting of adverse drug reactions: A cluster-randomized trial among pharmacists in Portugal. Drug Saf. 2008;31:325–344. doi: 10.2165/00002018-200831040-00007. [DOI] [PubMed] [Google Scholar]
- 79.Figueiras A., López-Vázquez P., Gonzalez-Gonzalez C., Vázquez-Lago J.M., Piñeiro-Lamas M., López-Durán A., Sánchez C., Herdeiro M.T., Zapata-Cachafeirom M., GREPHEPI Group Impact of a multifaceted intervention to improve antibiotic prescribing: A pragmatic cluster-randomised controlled trial. Antimicrob. Resist. Infect. Control. 2020;9:195. doi: 10.1186/s13756-020-00857-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Strumann C., Steinhaeuser J., Emcke T., Sönnichsen A., Goetz K. Communication training and the prescribing pattern of antibiotic prescription in primary health care. PLoS ONE. 2020;15:e0233345. doi: 10.1371/journal.pone.0233345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Herdeiro M.T., Figueiras A., Polónia J., Gestal-Otero J.J. Physicians’ attitudes and adverse drug reaction reporting: A case-control study in Portugal. Drug Saf. 2005;28:825–833. doi: 10.2165/00002018-200528090-00007. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.