Abstract
Simple Summary
Nutritional and oncological assessments are important for predicting prognosis in cancer. We developed a modified albumin-bilirubin grade and α-fetoprotein (mALF) score based on the modified albumin-bilirubin (mALBI) grade and α-fetoprotein (AFP) level. Our results indicate that the mALF score has better predictive value for prognosis and shows greater sensitivity for predicting risk of postoperative complications as compared with mALBI or AFP in patients undergoing hepatectomy for hepatocellular carcinoma.
Abstract
We developed and evaluated a modified albumin-bilirubin grade and α-fetoprotein (mALF) score, a nutritional and oncological assessment tool for patients with hepatocellular carcinoma (HCC) after surgical resection. Patients (n = 480) who underwent R0 resection between 2010 and 2020 were analyzed retrospectively. The mALF score assigned one point for a modified albumin-bilirubin (mALBI) grade 2b or 3 and one point for an α-fetoprotein (AFP) level ≥ 100 ng/mL. Patients were classified by mALF scores of 0 (mALBI grade 1/2a, AFP < 100 ng/mL), 1 (mALBI grade 2b/3 or AFP ≥ 100 ng/mL), or 2 (mALBI grade 2b/3, AFP ≥ 100 ng/mL) points. Liver reserve deteriorated and cancer progressed with increasing score. Postoperative complications (Clavien–Dindo classification ≥ 3) differed significantly among groups. The 5-year recurrence-free survival (RFS) rates were 34.8%, 11.2%, and 0.0% for 0, 1, and 2 points, respectively (1 or 2 versus 0 points, p < 0.001). The 5-year overall survival (OS) rates were 66.0%, 29.7%, and 17.8% for 0, 1, and 2 points, respectively (1 or 2 versus 0 points, p < 0.001). The mALF score was an independent prognostic predictor of RFS and OS. In HCC, the mALF score was effective for predicting postoperative complications and long-term survival.
Keywords: hepatocellular carcinoma, modified albumin-bilirubin grade and α-fetoprotein score, modified albumin-bilirubin grade, α-fetoprotein, prognosis, complication
1. Introduction
Hepatocellular carcinoma (HCC) is the most common primary malignancy of the liver and the fifth most common of all malignancies [1]. In surgical treatment against malignant tumors, nutritional assessment is important for predicting prognosis. The prognostic nutritional index (PNI) [2,3], neutrophil/lymphocyte ratio (NLR) [4], platelet/lymphocyte ratio (PLR) [5], and controlling nutritional status (CONUT) score [6] were proposed as nutritional prognostic assessment tools. In addition, the Glasgow prognostic score (GPS) [7,8,9], defined based on C-reactive protein (CRP; 1.0 mg/dL) and serum albumin (3.5 g/dL) levels, was shown to be an important and useful nutritional assessment tool for predicting prognosis in patients with malignant tumors. Moreover, patients with a GPS score ≥ 1 have been reported to have a higher rate of complications following surgical resection for advanced gastric cancer compared with patients with a low GPS score (<1) [10]. Previously, we developed an improved GPS scoring method (neo-GPS) [11], based on the albumin-bilirubin (ALBI) grade, and reported that it identified the approximate borderline of amino-acid imbalance [12] and could be used instead of serum albumin for predicting prognosis following surgical resection.
In contrast, many studies have found that α-fetoprotein (AFP) and protein induced by vitamin K absence or antagonist-II (PIVKA-II), which are tumor markers for HCC, predict postoperative prognosis [13,14,15]. It is important to establish a simple scoring system that reflects preserved liver function and oncologic prognostic factors. Therefore, the aim of the current study was to develop a new, simple score using both the modified ALBI grade, which indicates the approximate borderline of amino-acid imbalance, and the AFP level to predict prognosis following surgical resection.
2. Materials and Methods
2.1. Patients
The records of all patients with HCC who underwent liver resection between January 2010 and September 2020 at Kansai Medical University Hospital (Osaka, Japan) were screened. A total of 480 patients who underwent an R0 resection, defined as macroscopic removal of all tumors, were enrolled in this study. Among them, 429 were classified as Child–Pugh class A. A single surgeon who had performed more than 1500 hepatic resection procedures was responsible for all patients analyzed in this study. The study protocol was approved by the institutional ethics committee of Kansai Medical University (reference number: KMU 2021311).
2.2. Underlying Liver Disease
HCC was considered due to hepatitis C virus (HCV) infection in cases with positive anti-HCV findings, while that due to hepatitis B virus (HBV) infection was determined in cases positive for the HBV surface antigen. Underlying liver disease was judged as related to alcohol for patients with a history of alcohol abuse (≥60 g/day) [16].
2.3. Liver Function and Nutritional Status Assessments
Child–Pugh score/classification [17], ALBI grade [18,19], and modified albumin-bilirubin (mALBI) grade [20] were used for hepatic reserve function assessment.
2.4. Clinicopathologic Variables, Treatment Algorithm for HCC, and Surgical Procedures
Patients were measured for the indocyanine green retention rate at 15 min (ICG-R15) and underwent conventional liver function tests prior to surgery. Patients also underwent measurement of levels of AFP and PIVKA-II. We used the updated treatment algorithm for HCC, which included a combination of five factors: liver function reserve, extrahepatic metastasis, vascular invasion, tumor number, and tumor size [21]. The degree of liver damage (including the ICG-R15) was used to determine the indication for hepatectomy. We summarized the new treatment algorithm as follows: patients with HCC with Child–Pugh class A/B liver function without extrahepatic metastasis or vascular invasion are recommended to receive one of three treatment regimens. First, either surgical resection or radiofrequency ablation is recommended with no priority for up to three tumors measuring ≤3 cm, or surgical resection is recommended as first-line therapy for a solitary tumor, regardless of size. Second, for up to three tumors measuring >3 cm, surgical resection is recommended as first-line therapy, and transarterial chemoembolization is recommended as second-line therapy. Third, for patients with HCC accompanied by vascular invasion without extrahepatic metastasis, a combination of embolization, hepatectomy, hepatic arterial infusion chemotherapy, and molecular targeted therapy is recommended. Treatment is selected for each patient according to the individual situation, including consideration of the following factors: liver function, the number and size of HCC lesions, and the extent of vascular invasion.
The Brisbane terminology proposed by Strasberg et al. was used to classify surgical procedures [22]. Anatomic resection was defined as resection of the tumor together with the related portal vein branches and corresponding hepatic territory. Anatomic resection was classified as hemihepatectomy (resection of half of the liver), extended hemihepatectomy (hemihepatectomy plus removal of additional contiguous segments), sectionectomy (resection of two Couinaud subsegments [23]), or segmentectomy (resection of one Couinaud subsegment). All other non-anatomic procedures were classified as limited resections. Limited resection was used to manage both peripheral and central tumors. Because partial hepatectomy allows adequate surgical margins, it was used to manage peripheral tumors and those with extrahepatic growth. Conversely, because of the difficulty and risks associated with achieving adequate margins, enucleation was used to manage central tumors near the hepatic hilum or major vessels. Each specimen was reviewed by a senior pathologist who performed a histological review to confirm the final diagnosis.
2.5. Modified ALBI Grade and AFP Score (mALF Score)
We developed a simple score, the modified albumin-bilirubin grade and AFP score (mALF score). We assigned 1 point for an mALBI grade 2b or 3 and 1 point for a baseline AFP level ≥ 100 ng/mL. Accordingly, a patient was classified by an mALF score of 0 points (mALBI grade 1 or 2a and AFP < 100 ng/mL), 1 point (either mALBI grade 2b or 3 and AFP ≥ 100 ng/mL), and 2 points (both mALBI grade 2b or 3 and AFP ≥ 100 ng/mL).
2.6. Evaluation of Complications Following Surgical Resection
For the evaluation of complications associated with surgical resection, the Clavien–Dindo classification [24] was used, with grade ≥3 considered to be a significant complication.
2.7. Statistical Analysis
Continuous variables were classified into two categories using the median value. Three groups of clinical characteristics were compared using the chi-square test or Fisher’s exact test, as appropriate. The probabilities of recurrence-free survival (RFS) and overall survival (OS) after hepatectomy were calculated using the Kaplan–Meier method. Hazard ratios for RFS and OS, and their 95% confidence intervals (CIs) were estimated using univariate Cox analysis. Multivariate analysis was performed using Cox proportional hazards analysis. For all analyses, p values less than 0.05 were considered to indicate statistical significance. The discriminating ability of the scoring models was assessed for prognostic ability using Harrell’s concordance-index (c-index). The R version 4.1.2 (R Foundation for Statistical Computing, Vienna, Austria) was used to perform the statistical analyses. Survival analysis was executed with the R package “survival”.
3. Results
3.1. Comparison of Perioperative Characteristics in Three Groups Classified by the mALF Scoring System
The characteristics of the patients classified into three groups by mALF score are shown in Table 1. There were significant differences among the three groups in the following: platelets, albumin, prothrombin time, CRP, AFP, PIVKA-II, ICGR15, ALBI score, Fib4-index, Child–Pugh score, fibrosis stage, degree of differentiation, number of tumors, portal vein invasion, hepatic vein invasion, and mALBI. As the score increased, liver reserve function deteriorated, and liver cancer progressed.
Table 1.
Clinical characteristics of 480 patients with hepatocellular carcinoma classified by mALF score.
| Variable | 0 Points (n = 289) |
1 Point (n = 157) |
2 Points (n = 34) |
p | Variable | 0 Points (n = 289) |
1 Point (n = 157) |
2 Points (n = 34) |
p | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age, Years | 0.423 | PIVKA-II (mAU/mL) | 0.004 | ||||||||||||
| <70 | 97 | (34%) | 58 | (37%) | 15 | (44%) | <107 | 151 | (54%) | 74 | (47%) | 8 | (24%) | ||
| ≥70 | 192 | (66%) | 99 | (63%) | 19 | (56%) | ≥107 | 127 | (46%) | 82 | (53%) | 25 | (76%) | ||
| Gender | 0.224 | ICGR15 (%) | 0.017 | ||||||||||||
| Male | 227 | (79%) | 112 | (71%) | 25 | (74%) | <14.8 | 157 | (55%) | 65 | (42%) | 14 | (41%) | ||
| Female | 62 | (21%) | 45 | (29%) | 9 | (26%) | ≥14.8 | 129 | (45%) | 91 | (58%) | 20 | (59%) | ||
| BMI, kg/m2 | 0.685 | ALBI score | <0.001 | ||||||||||||
| <24 | 161 | (56%) | 94 | (60%) | 20 | (59%) | Grade 1 | 206 | (71%) | 46 | (29%) | 0 | (0%) | ||
| ≥24 | 128 | (44%) | 63 | (40%) | 14 | (41%) | Grade 2 | 83 | (29%) | 106 | (68%) | 30 | (88%) | ||
| Alcohol | 0.481 | Grade 3 | 0 | (0%) | 5 | (3%) | 4 | (12%) | |||||||
| None | 189 | (65%) | 111 | (71%) | 24 | (71%) | Fib4-index | 0.001 | |||||||
| Positive | 100 | (35%) | 46 | (29%) | 10 | (29%) | Low | 22 | (8%) | 4 | (3%) | 4 | (12%) | ||
| HBsAg | 0.976 | Middle | 112 | (39%) | 39 | (25%) | 9 | (26%) | |||||||
| Negative | 251 | (87%) | 135 | (86%) | 30 | (88%) | High | 155 | (54%) | 113 | (72%) | 21 | (62%) | ||
| Positive | 38 | (13%) | 22 | (14%) | 4 | (12%) | Child–Pugh score | <0.001 | |||||||
| HCV Ab | 0.375 | <6 | 248 | (86%) | 75 | (48%) | 1 | (3%) | |||||||
| Negative | 186 | (65%) | 92 | (59%) | 19 | (56%) | ≥6 | 41 | (14%) | 82 | (52%) | 33 | (97%) | ||
| Positive | 102 | (35%) | 64 | (41%) | 15 | (44%) | Fibrosis stage | 0.002 | |||||||
| Platelet (×104/μL) | 0.007 | f0 or 1 or 2 or 3 | 206 | (72%) | 87 | (57%) | 25 | (81%) | |||||||
| <15.5 | 130 | (45%) | 94 | (60%) | 14 | (41%) | f4 | 80 | (28%) | 65 | (43%) | 6 | (19%) | ||
| ≥15.5 | 159 | (55%) | 63 | (40%) | 20 | (59%) | Degree of differentiation | 0.043 | |||||||
| Albumin, g/dL | <0.001 | Well or moderate | 8 | (3%) | 6 | (4%) | 4 | (13%) | |||||||
| <3.9 | 70 | (24%) | 103 | (66%) | 34 | (100%) | Poor | 263 | (97%) | 139 | (96%) | 27 | (87%) | ||
| ≥3.9 | 219 | (76%) | 54 | (34%) | 0 | (0%) | Tumor size, cm | 0.292 | |||||||
| Total bilirubin, mg/dL | 0.372 | <3.0 | 116 | (40%) | 59 | (38%) | 9 | (26%) | |||||||
| <0.8 | 149 | (52%) | 73 | (46%) | 14 | (41%) | ≥3.0 | 173 | (60%) | 98 | (62%) | 25 | (74%) | ||
| ≥0.8 | 140 | (48%) | 84 | (54%) | 20 | (59%) | Number of tumors | <0.001 | |||||||
| ALT, IU/L | 0.355 | Solitary | 243 | (84%) | 111 | (71%) | 22 | (65%) | |||||||
| <29 | 147 | (51%) | 75 | (48%) | 13 | (38%) | Multiple | 46 | (16%) | 46 | (29%) | 12 | (35%) | ||
| ≥29 | 142 | (49%) | 82 | (52%) | 21 | (62%) | Portal vein invasion | 0.028 | |||||||
| Prothrombin time, % | 0.002 | Negative | 119 | (42%) | 52 | (35%) | 7 | (21%) | |||||||
| <87 | 123 | (43%) | 89 | (57%) | 23 | (68%) | Positive | 163 | (58%) | 98 | (65%) | 27 | (79%) | ||
| ≥87 | 165 | (57%) | 68 | (43%) | 11 | (32%) | Hepatic vein invasion | 0.031 | |||||||
| CRP, mg/dL | <0.001 | Negative | 196 | (70%) | 89 | (61%) | 17 | (50%) | |||||||
| <0.1 | 162 | (56%) | 69 | (44%) | 5 | (15%) | Positive | 86 | (30%) | 57 | (39%) | 17 | (50%) | ||
| ≥0.1 | 127 | (44%) | 88 | (56%) | 29 | (85%) | mALBI | <0.001 | |||||||
| AFP, ng/mL | <0.001 | 1 or 2a | 289 | (100%) | 84 | (54%) | 0 | (0%) | |||||||
| <100 | 289 | (100%) | 73 | (46%) | 0 | (0%) | 2b or 3 | 0 | (0%) | 73 | (46%) | 34 | (100%) | ||
| ≥100 | 0 | (0%) | 84 | (54%) | 34 | (100%) | |||||||||
Data are shown as n (%). mALF: modified albumin-bilirubin grade and α-fetoprotein; BMI: body mass index; HBsAg: hepatitis B surface antigen; HCV Ab: hepatitis C virus antibody; ALT: alanine aminotransferase; CRP: C-reactive protein; AFP: α-fetoprotein; PIVKA-II: protein induced by vitamin K absence or antagonist-II; ICGR15: indocyanine green retention rate at 15 min; ALBI: integration of albumin-bilirubin; mALBI: modified integration of albumin-bilirubin.
Perioperative characteristics are shown in Table 2. The operative time and postoperative complications (Clavien–Dindo classification ≥3, postoperative hospital stay, and readmission within 30 days) differed significantly among the three groups.
Table 2.
Perioperative characteristics of 480 patients with hepatocellular carcinoma classified by mALF score.
| Variable | 0 Points (n = 289) |
1 Point (n = 157) |
2 Points (n = 34) |
p | |||
|---|---|---|---|---|---|---|---|
| Surgical Procedure | 0.077 | ||||||
| Non-anatomic or segmentectomy | 141 | (49%) | 79 | (50%) | 10 | (29%) | |
| Sectionectomy or more than hemihepatectomy | 148 | (51%) | 78 | (50%) | 24 | (71%) | |
| Open, Laparoscopic | 0.344 | ||||||
| Open | 206 | (71%) | 110 | (70%) | 28 | (82%) | |
| Laparoscopic | 83 | (29%) | 47 | (30%) | 6 | (18%) | |
| Operative time, min | 0.016 | ||||||
| <330 | 151 | (52%) | 81 | (52%) | 9 | (26%) | |
| ≥330 | 138 | (48%) | 76 | (48%) | 25 | (74%) | |
| Operative blood loss, ml | 0.090 | ||||||
| <617 | 151 | (52%) | 78 | (50%) | 11 | (32%) | |
| ≥617 | 138 | (48%) | 79 | (50%) | 23 | (68%) | |
| Postoperative complications (Clavien–Dindo classification ≥3) |
<0.001 | ||||||
| No | 249 | (86%) | 111 | (71%) | 21 | (62%) | |
| Yes | 40 | (14%) | 46 | (29%) | 13 | (38%) | |
| Postoperative hospital stay, days | <0.001 | ||||||
| <14 | 153 | (53%) | 67 | (43%) | 5 | (15%) | |
| ≥14 | 136 | (47%) | 90 | (57%) | 29 | (85%) | |
| Readmission within 30 days | 0.008 | ||||||
| No | 272 | (95%) | 144 | (92%) | 24 | (80%) | |
| Yes | 13 | (5%) | 13 | (8%) | 6 | (20%) | |
mALF: modified albumin-bilirubin grade and alpha-fetoprotein.
3.2. Long-Term Survival
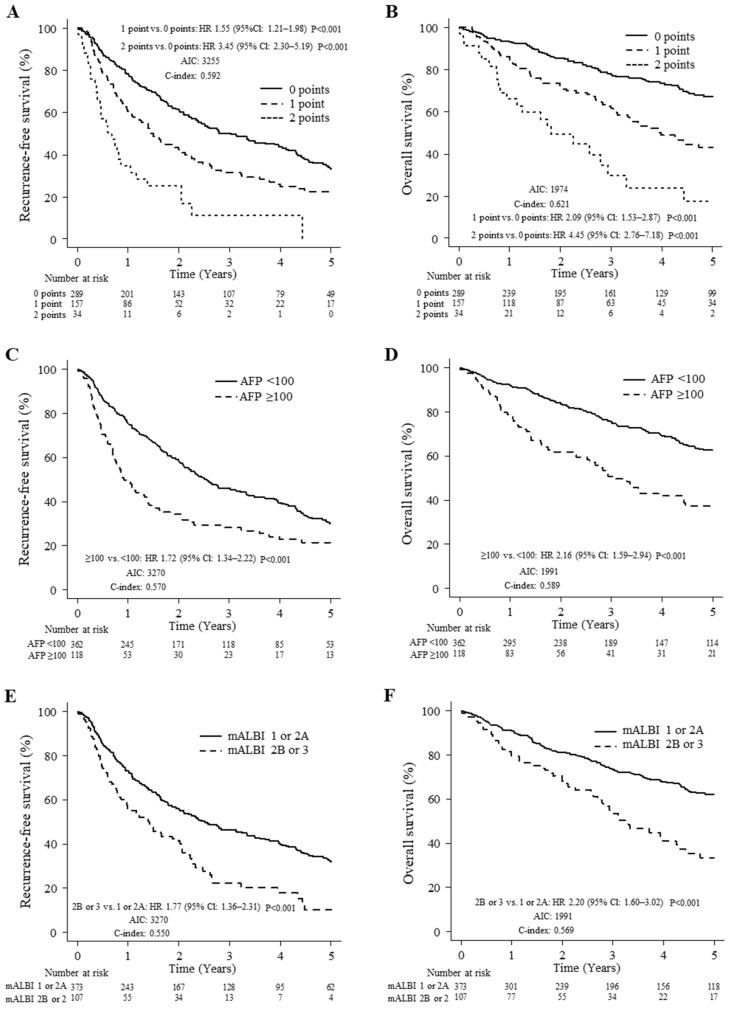
Patient survival was determined in the three groups, and the Kaplan–Meier curves demonstrated that the mALF score enabled satisfactory risk evaluations of survival (Figure 1). The 1-, 3-, and 5-year RFS rates of the groups were significantly different, at 78.3%, 50.2%, and 33.5%, respectively, for 0 points; at 60.5%, 31.4%, and 22.5%, respectively, for 1 point; and at 34.8%, 11.2%, and 0.0%, respectively, for 2 points (1 or 2 versus 0 points: p < 0.001; Figure 1A). The patients were divided into three risk classifications of OS, and the 1-, 3-, and 5-year OS rates of the groups were significantly different at 93.2%, 77.6%, and 67.4%, respectively, for 0 points; at 84.7%, 61.6%, and 43.0%, respectively, for 1 point; and at 66.0%, 29.7% and 17.8%, respectively, for 2 points (1 or 2 versus 0 points: p < 0.001; Figure 1B).
Figure 1.
Comparison of mALF, AFP, and mALBI for prediction of recurrence-free survival (RFS) and overall survival (OS). (A) RFS in patients with mALF scores of 0, 1, and 2 points. (B) OS in patients with mALF scores of 0, 1, and 2 points. (C) RFS in patients with AFP <100 and ≥100 ng/mL. (D) OS in patients with AFP <100 and ≥100 ng/mL. (E) RFS in patients with mALBI 1 or 2A and 2B or 3. (F) OS in patients with mALBI 1 or 2A and 2B or 3.
For comparison to our preoperative staging system, Kaplan–Meier curves for RFS and OS based on serum AFP levels and mALBI grade are presented in Figure 1C–F. The 1-, 3-, and 5-year RFS rates of the groups were significantly different, at 75.8%, 45.9%, and 30.1%, respectively, for AFP < 100 ng/mL and 49.9%, 28.1%, and 21.4%, respectively for AFP ≥ 100 ng/mL (<100 versus ≥100 groups: p < 0.001; Figure 1C), and the 1-, 3-, and 5-year OS rates of the groups were significantly different, at 91.7%, 75.1%, and 62.6%, respectively, for AFP < 100 mg/mL and at 78.8%, 50.9%, and 37.2%, respectively, for AFP ≥ 100 ng/mL (<100 versus ≥100 groups: p < 0.001; Figure 1D). The 1-, 3-, and 5-year RFS rates of the groups were significantly different, at 73.2%, 46.5%, and 32.1%, respectively, for mALBI 1 or 2A and at 56.2%, 22.5%, and 10.1%, respectively, for mALBI 2B or 3 (1 or 2A versus 2B or 3 groups: p < 0.001; Figure 1E), and the 1-, 3-, and 5-year OS rates of the groups were significantly different at 91.1%, 73.4%, and 62.2%, respectively, for mALBI 1 or 2A and at 79.4%, 53.4%, and 33.5%, respectively, for mALBI 2B or 3 (1 or 2A versus 2B or 3 groups: p < 0.001; Figure 1F).
In the comparison of RFS, the c-index was higher (0.592 versus 0.570 or 0.550) according to the mALF scoring system as compared with AFP or the mALBI grading system. Additionally, in a comparison of OS, the c-index was higher (0.621 versus 0.589 or 0.569) based on the mALF scoring system.
3.3. Univariate and Multivariate Analysis of Prognostic Factors for Long-Term Survival
Cox proportional hazards analysis revealed five independent prognostic predictors for both RFS and OS (Table 3): prothrombin time ≥ 87% (RFS: hazard ratio, 0.69; 95% CI, 0.52–0.90; p = 0.007, OS: hazard ratio, 0.68; 95% CI, 0.48–0.97; p = 0.034), PIVKA-II ≥ 107 mAU/mL (RFS: hazard ratio, 1.48; 95% CI, 1.12–1.94; p = 0.005, OS: hazard ratio, 1.67; 95% CI, 1.16–2.42; p = 0.006), number of tumors ≥ 2 (RFS: hazard ratio, 1.66; 95% CI, 1.24–2.21; p < 0.001, OS: hazard ratio, 1.46; 95% CI, 1.01–2.11; p = 0.047), mALF point 1 (RFS: hazard ratio, 1.35; 95% CI, 1.02–1.78; p = 0.036, OS: hazard ratio, 1.95; 95% CI, 1.36–2.80; p < 0.001), and mALF score 2 points (RFS: hazard ratio, 3.02; 95% CI, 1.83–4.98; p < 0.001, OS: hazard ratio, 3.67; 95% CI, 2.03–6.63; p < 0.001).
Table 3.
Cox proportional hazards regression analysis for recurrence-free survival and overall survival in patients with hepatocellular carcinoma who underwent hepatic resection.
| Variable | Univariate Analysis | Multivariate Analysis | Univariate Analysis | Multivariate Analysis | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HR | (95% CI) | p | HR | (95% CI) | p | HR | (95% CI) | p | HR | (95% CI) | p | |
| Age ≥ 70 years (versus < 70 years) | 0.99 | (0.78–1.25) | 0.918 | 0.95 | (0.71–1.25) | 0.695 | 1.18 | (0.87–1.60) | 0.287 | 1.09 | (0.75–1.56) | 0.655 |
| HCV Ab Positive (versus Negative) | 1.05 | (0.83–1.33) | 0.669 | 0.96 | (0.73–1.28) | 0.796 | 1.10 | (0.81–1.48) | 0.536 | 0.84 | (0.58–1.22) | 0.363 |
| Platelets ≥ 15.5 (versus <15.5 × 104/μL) | 1.13 | (0.90–1.42) | 0.295 | 1.27 | (0.92–1.77) | 0.146 | 1.14 | (0.85–1.53) | 0.364 | 1.39 | (0.92–2.12) | 0.122 |
| Albumin ≥ 3.9 (versus <3.9 g/dL) | 0.54 | (0.43–0.69) | <0.001 | 0.42 | (0.31–0.56) | <0.001 | ||||||
| ALT ≥ 29 (versus <29 IU/L) | 1.09 | (0.87–1.37) | 0.461 | 1.03 | (0.79–1.35) | 0.806 | 1.00 | (0.74–1.33) | 0.973 | 0.97 | (0.69–1.38) | 0.884 |
| Prothrombin time ≥ 87 (versus < 87 %) | 0.66 | (0.53–0.83) | <0.001 | 0.69 | (0.52–0.90) | 0.007 | 0.63 | (0.47–0.84) | 0.002 | 0.68 | (0.48–0.97) | 0.034 |
| AFP ≥ 100 (versus < 100 ng/mL) | 1.72 | (1.34–2.22) | <0.001 | 2.16 | (1.59–2.94) | <0.001 | ||||||
| PIVKA-II ≥ 107 (versus < 107 mAU/mL) | 1.68 | (1.33–2.12) | <0.001 | 1.48 | (1.12–1.94) | 0.005 | 2.04 | (1.51–2.77) | <0.001 | 1.67 | (1.16–2.42) | 0.006 |
| ICGR15 ≥ 14.8 (versus < 14.8%) | 1.14 | (0.91–1.44) | 0.253 | 0.87 | (0.65–1.17) | 0.361 | 1.40 | (1.04–1.88) | 0.025 | 1.16 | (0.80–1.69) | 0.430 |
| ALBI score Grade 2 (versus 1) | 1.88 | (1.49–2.37) | <0.001 | 2.61 | (1.92–3.55) | <0.001 | ||||||
| ALBI score Grade 3 (versus 1) | 2.59 | (1.14–5.90) | 0.023 | 3.24 | (1.18–8.94) | 0.023 | ||||||
| Fib4-index Middle (versus Low) | 1.12 | (0.67–1.87) | 0.675 | 1.21 | (0.68–2.15) | 0.524 | 1.46 | (0.70–3.06) | 0.317 | 1.55 | (0.68–3.50) | 0.296 |
| Fib4-index High (versus Low) | 1.35 | (0.82–2.22) | 0.235 | 1.58 | (0.84–2.98) | 0.154 | 1.86 | (0.91–3.81) | 0.089 | 2.42 | (0.99–5.93) | 0.053 |
| Fibrosis stage f4 (versus f0 or 1 or 2 or 3) | 1.12 | (0.88–1.43) | 0.358 | 1.19 | (0.85–1.65) | 0.309 | 1.00 | (0.73–1.38) | 0.977 | 1.12 | (0.73–1.72) | 0.601 |
| Degree of differentiation Poor (versus Well or Mode) | 0.89 | (0.48–1.68) | 0.730 | 0.93 | (0.46–1.85) | 0.826 | 0.80 | (0.35–1.81) | 0.590 | 0.63 | (0.25–1.54) | 0.309 |
| Tumor size ≥3.0 (versus <3.0 cm) | 1.38 | (1.09–1.75) | 0.008 | 1.21 | (0.90–1.62) | 0.216 | 1.44 | (1.05–1.97) | 0.022 | 1.04 | (0.71–1.53) | 0.847 |
| Number of tumors ≥ 2 (versus 1) | 1.90 | (1.48–2.44) | <0.001 | 1.66 | (1.24–2.21) | <0.001 | 1.75 | (1.28–2.39) | <0.001 | 1.46 | (1.01–2.11) | 0.047 |
| Portal vein invasion Positive (versus Negative) | 1.42 | (1.11–1.81) | 0.006 | 1.21 | (0.91–1.61) | 0.193 | 1.77 | (1.26–2.48) | 0.001 | 1.52 | (1.01–2.28) | 0.043 |
| mALBI 2b or 3 (versus 1 or 2a) | 1.77 | (1.36–2.31) | <0.001 | 2.20 | (1.60–3.02) | <0.001 | ||||||
| Surgical procedure Sectionectomy or more than hemihepatectomy (versus non-anatomic or segmentectomy) |
1.32 | (1.05–1.67) | 0.016 | 0.96 | (0.72–1.28) | 0.800 | 1.50 | (1.12–2.02) | 0.007 | 1.33 | (0.91–1.93) | 0.136 |
| Operative blood loss ≥ 617 (versus <617 mL) | 1.35 | (1.08–1.70) | 0.009 | 1.19 | (0.91–1.55) | 0.195 | 1.51 | (1.12–2.03) | 0.007 | 1.16 | (0.82–1.64) | 0.398 |
| mALF 1 point (versus 0 points) | 1.55 | (1.21–1.98) | <0.001 | 1.35 | (1.02–1.78) | 0.036 | 2.09 | (1.53–2.86) | <0.001 | 1.95 | (1.36–2.80) | <0.001 |
| mALF 2 points (versus 0 points) | 3.45 | (2.30–5.19) | <0.001 | 3.02 | (1.83–4.98) | <0.001 | 4.45 | (2.76–7.18) | <0.001 | 3.67 | (2.03–6.63) | <0.001 |
HR; hazard ratio; CI; confidence interval; HCV Ab: hepatitis C virus antibody; ALT: alanine aminotransferase; AFP: alpha-fetoprotein; PIVKA-II: protein induced by vitamin K absence or antagonist-II; ICGR15: indocyanine green retention rate at 15 min; ALBI: integration of albumin-bilirubin; mALBI: modified integration of albumin-bilirubin; mALF: modified albumin-bilirubin grade and α-fetoprotein.
4. Discussion
Inflammatory biomarkers have a strong prognostic value in surgically treated patients with HCC; however, the underlying pathogenic mechanisms are not completely clear. Conversely, nutritional biomarkers predict the outcomes after hepatic resection for HCC but not after liver transplantation (LT). Pravisani et al. reported that at 1 year after LT, the nutritional status of patients with HCC who received LT significantly improved, although the inflammatory state tended to persist. HCC in LT candidates with high PLR and/or NLR may have a more aggressive biology, requiring these patients to be thoroughly and more carefully assessed in the pre-LT workup. Moreover, NLR and PLR may be also used as reliable prognostic parameters for long-term clinical surveillance [25,26].
The major findings of the present study are that mALBI grade 2b or 3 and AFP ≥ 100 ng/mL were identified as independent unfavorable prognostic factors in multivariate analysis and that we developed an easy and widely applicable score, the mALF score, for patients with HCC undergoing hepatic resection. The mALF score used a newly developed assessment tool based on hepatic function and a tumor factor. This mALF score showed the best c-index for predicting prognosis for OS and RFS among other AFP as a tumor factor and mALBI as an hepatic function index. Finally, the mALF score was prognostic for RFS and OS in multivariate analysis, and it was found to be a better predictor of high Clavien–Dindo classification (≥3; Table 2). Thus, it is thought that the mALF score can be an important prognostic predictive assessment tool in patients with HCC.
The liver damage system, which is treated as a more suitable assessment tool than the Child–Pugh classification because it uses ICG-R15, has been used generally for patients treated with surgical resection. In contrast, the ALBI score has been shown not only to have good relationships with ICG-R15 (r = 0.563, 95% CI: 0.550–0.570, p < 0.0001) [20] but also to behave as a more detailed assessment tool than the liver damage system [27]. According to data from a Japanese nationwide survey, the mALBI grade can evaluate preserved liver function more precisely and accurately than the Child–Pugh classification [20]. In addition, the mALBI grade can predict and stratify the prognosis of patients with HCC [20].
AFP is a well-known tumor marker and is widely used in the management of HCC, such as in surveillance, diagnosis, monitoring of treatment response, and prognosis [28]. An elevated AFP level shows a poor prognosis across all stages of HCC [29]. An elevated AFP level was also related to a high risk of tumor recurrence after surgical resection [13,14,15] and liver transplantation [30]. An analysis of transcriptome data, whole-exome sequencing data, and DNA methylome profiling demonstrated that AFP-high tumors showed a different phenotype characterized by poor differentiation, enrichment of progenitor features and enhanced proliferation compared with AFP-low tumors [31]. From the above findings, it is easy to understand that the mALF score, which uses the mALBI grade and AFP level, showed the best predictive values not only for prognosis, and but also for high Clavien–Dindo classification (≥3). Because a high rate of complications is expected when hepatectomy is planned in patients with HCC with high mALF (2 points), nutritional intervention should be considered in such patients. Kaido and colleagues reported the importance of nutritional intervention in liver transplantation [32]. Recently, muscle volume decline has been reported to be an important prognostic factor for recurrence and OS [33]. As hepatic reserve function worsened, the frequency of muscle abnormalities increased [34]. However, a relationship between mALF score and muscle abnormality was not elucidated in the present study because there was no information on muscle volume (pre-sarcopenia) in the present database. This study was limited by its retrospective nature. From now on, in addition to assessment using the mALF score, an assessment for sarcopenia should be performed, and further examination must be set to elucidate their relationship in the near future.
Patients with compensated cirrhosis and large liver functional reserve can always receive the most radical treatment in terms of potential survival benefit according to their tumor stage, provided that there is no significant extrahepatic disease. Conversely, a more detailed and individualized assessment should be carried out in patients with poorer liver functional reserve. Such an assessment must balance the expected antitumor efficacy of any given locoregional therapy with the risk of deterioration in liver function, particularly considering the risk of progression to frank Child–Pugh class B or borderline Child–Pugh class A; this may limit the possibility of receiving multiple lines of systemic therapy, for which the clinical potential is rapidly increasing. The most balanced and potentially most complete treatment strategy should be foreseen and designed from the outset, considering the potential for several lines of therapy and not just the most readily available treatment [35,36].
5. Conclusions
The newly developed mALF score, based on the mALBI grade and AFP level, is a valuable prognostic nutritional and oncological assessment tool for prediction of postoperative complications and prognosis in patients with HCC after surgical resection.
Author Contributions
Conceptualization, M.K. and T.H.; methodology, M.K.; investigation, M.K.; resources, M.K.; data curation, K.M., H.M., H.K., H.Y., K.A., T.Y., and K.Y. (Katsunori Yoshida); writing—original draft preparation, M.K.; writing—review and editing, M.K. and A.H.; visualization, M.K. and K.Y. (Kengo Yoshii); Formal analysis, K.Y. (Kengo Yoshii); supervision, T.H., A.H., T.T., T.K., and M.S.; project administration, M.K. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study protocol was approved by the institutional ethics committee of Kansai Medical University (reference number: KMU 2021311, 11 March 2021). After receiving official approval, this study was conducted as a retrospective analysis of database records based on the Guidelines for Clinical Research issued by the Ministry of Health and Welfare of Japan. All procedures were carried out in accordance with the Declaration of Helsinki. The data were made anonymous before analysis to protect patient privacy.
Informed Consent Statement
Written informed consent was obtained from all patients before treatment, and this study received ethical approval for the use of an opt-out methodology based on low risk to the participants.
Data Availability Statement
Due to the nature of this research, participants in this study could not be contacted regarding whether the findings could be shared publicly; thus, supporting data are not available. The datasets generated and/or analyzed for the current study are not publicly available due to the nature of the research, as noted above.
Conflicts of Interest
None of the authors has potential conflicts of interest to declare.
Funding Statement
This research received no external funding.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Parkin D.M., Bray F., Ferlay J., Pisani P. Estimating the world cancer burden: Globocan 2000. Int. J. Cancer. 2001;94:153–156. doi: 10.1002/ijc.1440. [DOI] [PubMed] [Google Scholar]
- 2.Onodera T., Goseki N., Kosaki G. Prognostic nutritional index in gastrointestinal surgery of malnourished cancer patients. Nihon Geka Gakkai Zasshi. 1984;85:1001–1005. (Abstract in English) [PubMed] [Google Scholar]
- 3.Broggi M.S., Patil D., Baum Y., Nieh P.T., Alemozaffar M., Pattaras J.G., Ogan K., Master V.A. Onodera’s Prognostic Nutritional Index as an independent prognostic factor in clear cell renal cell carcinoma. Urology. 2016;96:99–105. doi: 10.1016/j.urology.2016.05.064. [DOI] [PubMed] [Google Scholar]
- 4.Motomura T., Shirabe K., Mano Y., Muto J., Toshima T., Umemoto Y., Fukuhara T., Uchiyama H., Ikegami T., Yoshizumi T., et al. Neutrophil-lymphocyte ratio reflects hepatocellular carcinoma recurrence after liver transplantation via inflammatory microenvironment. J. Hepatol. 2013;58:58–64. doi: 10.1016/j.jhep.2012.08.017. [DOI] [PubMed] [Google Scholar]
- 5.Kinoshita A., Onoda H., Imai N., Iwaku A., Oishi M., Fushiya N., Koike K., Nishino H., Tajiri H. Comparison of the prognostic value of inflammation-based prognostic scores in patients with hepatocellular carcinoma. Br. J. Cancer. 2012;107:988–993. doi: 10.1038/bjc.2012.354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ignacio de Ulíbarri J., González-Madroño A., de Villar N.G., González P., González B., Mancha A., Rodríguez F., Fernández G. CONUT: A tool for controlling nutritional status. First validation in a hospital population. Nutr. Hosp. 2005;20:38–45. [PubMed] [Google Scholar]
- 7.Forrest L.M., McMillan D.C., McArdle C.S., Angerson W.J., Dunlop D.J. Evaluation of cumulative prognostic scores based on the systemic inflammatory response in patients with inoperable non-small-cell lung cancer. Br. J. Cancer. 2003;89:1028–1030. doi: 10.1038/sj.bjc.6601242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Elahi M.M., McMillan D.C., McArdle C.S., Angerson W.J., Sattar N. Score based on hypoalbuminemia and elevated C-reactive protein predicts survival in patients with advanced gastrointestinal cancer. Nutr. Cancer. 2004;48:171–173. doi: 10.1207/s15327914nc4802_6. [DOI] [PubMed] [Google Scholar]
- 9.Crumley A.B., McMillan D.C., McKernan M., McDonald A.C., Stuart R.C. Evaluation of an inflammation-based prognostic score in patients with inoperable gastro-oesophageal cancer. Br. J. Cancer. 2006;94:637–641. doi: 10.1038/sj.bjc.6602998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shimoda Y., Fujikawa H., Komori K., Watanabe H., Kano K., Yamada T., Shiozawa M., Morinaga S., Katsumata K., Tsuchida A., et al. Preoperative utility of the Glasgow Prognostic Score on outcomes of patients with locally advanced gastric cancer. J. Gastrointest. Cancer. 2022;53:265–271. doi: 10.1007/s12029-021-00584-3. [DOI] [PubMed] [Google Scholar]
- 11.Kaibori M., Hiraoka A., Matsui K., Matsushima H., Kosaka H., Yamamoto H., Yamaguchi T., Yoshida K., Sekimoto M. Predicting complications following surgical resection of hepatocellular carcinoma using newly developed Neo-Glasgow Prognostic Score with ALBI grade: Comparison of open and laparoscopic surgery cases. Cancers. 2022;14:1402. doi: 10.3390/cancers14061402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hiraoka A., Kato M., Marui K., Murakami T., Onishi K., Adachi T., Matsuoka J., Ueki H., Yoshino T., Tsuruta M., et al. Easy clinical predictor for low BCAA to tyrosine ratio in chronic liver disease patients with hepatocellular carcinoma: Usefulness of ALBI score as nutritional prognostic marker. Cancer Med. 2021;10:3584–3592. doi: 10.1002/cam4.3908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kaibori M., Matsui Y., Yanagida H., Yokoigawa N., Kwon A.H., Kamiyama Y. Positive status of alpha-fetoprotein and des-gamma-carboxy prothrombin: Important prognostic factor for recurrent hepatocellular carcinoma. World J. Surg. 2004;28:702–707. doi: 10.1007/s00268-004-7205-y. [DOI] [PubMed] [Google Scholar]
- 14.Toyoda H., Kumada T., Tada T., Niinomi T., Ito T., Kaneoka Y., Maeda A. Prognostic significance of a combination of pre- and post-treatment tumor markers for hepatocellular carcinoma curatively treated with hepatectomy. J. Hepatol. 2012;57:1251–1257. doi: 10.1016/j.jhep.2012.07.018. [DOI] [PubMed] [Google Scholar]
- 15.Kamiyama T., Yokoo H., Kakisaka T., Orimo T., Wakayama K., Kamachi H., Tsuruga Y., Yamashita K., Shimamura T., Todo S., et al. Multiplication of alpha-fetoprotein and protein induced by vitamin K absence-II is a powerful predictor of prognosis and recurrence in hepatocellular carcinoma patients after a hepatectomy. Hepatol. Res. 2015;45:E21–E31. doi: 10.1111/hepr.12451. [DOI] [PubMed] [Google Scholar]
- 16.EASL clinical practical guidelines: Management of alcoholic liver disease. J. Hepatol. 2012;57:399–420. doi: 10.1016/j.jhep.2012.04.004. [DOI] [PubMed] [Google Scholar]
- 17.Pugh R.N., Murray-Lyon I.M., Dawson J.L., Pietroni M.C., Williams R. Transection of the oesophagus for bleeding oesophageal varices. Br. J. Surg. 1973;60:646–649. doi: 10.1002/bjs.1800600817. [DOI] [PubMed] [Google Scholar]
- 18.Johnson P.J., Berhane S., Kagebayashi C., Satomura S., Teng M., Reeves H.L., O’Beirne J., Fox R., Skowronska A., Palmer D., et al. Assessment of liver function in patients with hepatocellular carcinoma: A new evidence-based approach-the ALBI grade. J. Clin. Oncol. 2015;33:550–558. doi: 10.1200/JCO.2014.57.9151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hiraoka A., Kumada T., Michitaka K., Toyoda H., Tada T., Ueki H., Kaneto M., Aibiki T., Okudaira T., Kawakami T., et al. Usefulness of albumin-bilirubin grade for evaluation of prognosis of 2584 Japanese patients with hepatocellular carcinoma. J. Gastroenterol. Hepatol. 2016;31:1031–1036. doi: 10.1111/jgh.13250. [DOI] [PubMed] [Google Scholar]
- 20.Hiraoka A., Michitaka K., Kumada T., Izumi N., Kadoya M., Kokudo N., Kubo S., Matsuyama Y., Nakashima O., Sakamoto M., et al. Validation and potential of albumin-bilirubin grade and prognostication in a nationwide survey of 46,681 hepatocellular carcinoma patients in Japan: The need for a more detailed evaluation of hepatic function. Liver Cancer. 2017;6:325–336. doi: 10.1159/000479984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kokudo N., Takemura N., Hasegawa K., Takayama T., Kubo S., Shimada M., Nagano H., Hatano E., Izumi I., Kaneko S., et al. Clinical practice guidelines for hepatocellular carcinoma: The Japan Society of Hepatology 2017 (4th JSH-HCC guidelines) 2019 update. Hepatol. Res. 2019;49:1109–1113. doi: 10.1111/hepr.13411. [DOI] [PubMed] [Google Scholar]
- 22.Strasberg S.M., Belghiti J., Clavien P.A., Gadzijev E., Garden J.O., Lau W.Y., Makuuchi M., Strong R.W. The Brisbane 2000 Terminology of Liver Anatomy and Resections. HPB. 2000;2:333–339. doi: 10.1016/S1365-182X(17)30755-4. [DOI] [Google Scholar]
- 23.Couinaud C. Le Foie: Études Anatomiques et Chirurgicales. Masson; Paris, France: 1957. [Google Scholar]
- 24.Dindo D., Demartines N., Clavien P.A. Classification of surgical complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann. Surg. 2004;240:205–213. doi: 10.1097/01.sla.0000133083.54934.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pravisani R., Mocchegiani F., Isola M., Lorenzin D., Adani G.L., Cherchi V., Righi E., Terrosu G., Vivarelli M., Risaliti A., et al. Controlling nutritional status score does not predict patients’ overall survival or hepatocellular carcinoma recurrence after deceased donor liver transplantation. Clin. Transplant. 2020;34:e13786. doi: 10.1111/ctr.13786. [DOI] [PubMed] [Google Scholar]
- 26.Pravisani R., Mocchegiani F., Isola M., Lorenzin D., Adani G.L., Cherchi V., De Martino M., Risaliti A., Lai Q., Vivarelli M., et al. Postoperative trends and prognostic values of inflammatory and nutritional biomarkers after liver transplantation for hepatocellular carcinoma. Cancers. 2021;13:513. doi: 10.3390/cancers13030513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hiraoka A., Kumada T., Kudo M., Hirooka M., Tsuji K., Itobayashi E., Kariyama K., Ishikawa T., Tajiri K., Ochi H., et al. Albumin-bilirubin (ALBI) grade as part of the Evidence-Based Clinical Practice Guideline for HCC of the Japan Society of Hepatology: A comparison with the Liver Damage and Child-Pugh Classifications. Liver Cancer. 2017;6:204–215. doi: 10.1159/000452846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Galle P.R., Foerster F., Kudo M., Chan S.L., Llovet J.M., Qin S., Schelman W.R., Chintharlapalli S., Abada P.B., Sherman M., et al. Biology and significance of alpha-fetoprotein in hepatocellular carcinoma. Liver Int. 2019;39:2214–2229. doi: 10.1111/liv.14223. [DOI] [PubMed] [Google Scholar]
- 29.Llovet J.M., Kelley R.K., Villanueva A., Singal A.G., Pikarsky E., Roayaie S., Lencioni R., Koike K., Zucman-Rossi J., Finn R.S. Hepatocellular carcinoma. Nat. Rev. Dis. Prim. 2021;7:6. doi: 10.1038/s41572-020-00240-3. [DOI] [PubMed] [Google Scholar]
- 30.Notarpaolo A., Layese R., Magistri P., Gambato M., Colledan M., Magini G., Miglioresi L., Vitale A., Vennarecci G., Ambrosio C.D., et al. Validation of the AFP model as a predictor of HCC recurrence in patients with viral hepatitis-related cirrhosis who had received a liver transplant for HCC. J. Hepatol. 2017;66:552–559. doi: 10.1016/j.jhep.2016.10.038. [DOI] [PubMed] [Google Scholar]
- 31.Montal R., Andreu-Oller C., Bassaganyas L., Esteban-Fabró R., Moran S., Montironi C., Moeini A., Pinyol R., Peix J., Cabellos L., et al. Molecular portrait of high alpha-fetoprotein in hepatocellular carcinoma: Implications for biomarker-driven clinical trials. Br. J. Cancer. 2019;121:340–343. doi: 10.1038/s41416-019-0513-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kaido T., Ogawa K., Fujimoto Y., Ogura Y., Hata K., Ito T., Tomiyama K., Yagi S., Mori A., Uemoto S. Impact of sarcopenia on survival in patients undergoing living donor liver transplantation. Am. J. Transplant. 2013;13:1549–1556. doi: 10.1111/ajt.12221. [DOI] [PubMed] [Google Scholar]
- 33.Chang K.V., Chen J.D., Wu W.T., Huang K.C., Hsu C.T., Han D.S. Association between loss of skeletal muscle mass and mortality and tumor recurrence in hepatocellular harcinoma: A systematic review and meta-analysis. Liver Cancer. 2018;7:90–103. doi: 10.1159/000484950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hiraoka A., Michitaka K., Ueki H., Kaneto M., Aibiki T., Okudaira T., Kawakami T., Yamago H., Suga Y., Tomida H., et al. Sarcopenia and two types of presarcopenia in Japanese patients with chronic liver disease. Eur. J. Gastroenterol. Hepatol. 2016;28:940–947. doi: 10.1097/MEG.0000000000000661. [DOI] [PubMed] [Google Scholar]
- 35.Granito A., Bolondi L. Non-transplant therapies for patients with hepatocellular carcinoma and Child-Pugh-Turcotte class B cirrhosis. Lancet Oncol. 2017;18:e101–e112. doi: 10.1016/S1470-2045(16)30569-1. [DOI] [PubMed] [Google Scholar]
- 36.D’Avola D., Granito A., de la Torre-Aláez M., Piscaglia F. The importance of liver functional reserve in the non-surgical treatment of hepatocellular carcinoma. J. Hepatol. 2022;76:1185–1198. doi: 10.1016/j.jhep.2021.11.013. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Due to the nature of this research, participants in this study could not be contacted regarding whether the findings could be shared publicly; thus, supporting data are not available. The datasets generated and/or analyzed for the current study are not publicly available due to the nature of the research, as noted above.