Abstract
Simple Summary
Located in the lateral facial region, the infratemporal fossa (ITF) is the primary site for tumors of various etiologies and comprise 0.5% of all head and neck cancers. Due to the anatomical relationship of ITF tumors with different cranial nerves and neurovascular structures, clinical presentations vary among patients. Our study aims to review the literature on the various tumors that present in this region, their reported treatment strategies, and patient outcomes. We found that trigeminal schwannomas and meningiomas are the most common tumors. In terms of management, nost patients had transcranial surgery, and three-quarters had a gross-total resection.
Abstract
Background: Infratemporal fossa (ITF) tumors represent various pathologies and are seldom described in the literature, reflecting their rarity. Here we review the literature on tumors invading ITF and describe patient characteristics, treatment strategies, and clinical outcomes. Methods: Relevant articles were retrieved from PubMed, Scopus, and Cochrane. A systematic review and meta-analysis were conducted on the clinical presentation, treatment protocols, and clinical outcomes. Result: A total of 27 articles containing 106 patients with ITF tumors (median tumor size: 24.3 cm3 [interquartile range, 15.2–42 cm3]) were included (median age: 46 years [interquartile range, 32–55 years]; 59.4% were males]). Of the confirmed tumor pathology data, schwannomas (n = 24; 26.1%) and meningiomas (n = 13; 14.1%) were the most common tumors. Facial hypoesthesia (n = 22; 18.5%), auricular/preauricular pain (n = 20; 16.8%), and headaches (n = 11; 9.2%) were the most common presenting symptoms. Of patients who had surgical resection (n = 97; 95.1%), 70 (73.7%) had transcranial surgery (TCS) and 25 (26.3%) had endoscopic endonasal surgery (EES). Among available details on the extent of resection (n = 84), gross-total resection (GTR) was achieved in 62 (73.8%), and 5 (6.0%) had biopsy only. Thirty-five (33.0%) patients had postoperative complications. Among cases with available data on reconstruction techniques (n = 8), four (50%) had adipofascial antero-lateral thigh flap, three (37.5%) had latissimus dorsi free flap, and one (12.5%) had antero-lateral thigh flap. Fourteen (13.2%) patients had adjuvant chemotherapy, and sixteen (15.1%) had adjuvant radiotherapy. During a median follow-up time of 28 months (IQR, 12.25–45.75 months), 15 (14.2%) patients had recurrences, and 18 (17.0%) patients died. The median overall survival (OS) time was 36 months (95% confidence interval: 29–41 months), and the 5-year progression-free survival (PFS) rate was 61%. Conclusion: Various tumor types with different biological characteristics invade the ITF. The present study describes patient demographics, clinical presentation, management, and outcomes. Depending on the tumor type and patient condition, patient-tailored management is recommended to optimize treatment outcomes.
Keywords: infratemporal fossa, skull base, meningiomas, schwannomas, transcranial surgery, endoscopic endonasal surgery
1. Introduction
Although approximately 80% are benign, infratemporal fossa (ITF) tumors are highly heterogenous. They include various tumor subtypes such as schwannomas, meningiomas, and sarcomas [1,2,3,4,5]. Due to the proximity of ITF tumors to different cranial nerves and neurovascular structures, ITF tumors also pose a surgical challenge and have highly variable clinical symptoms at presentation [1,2,3,4,5].
Although it varies based on the specific tumor type, the management paradigm of ITF tumors relies mainly on a combination of surgical resection, chemotherapy and/or radiotherapy [1,2,3,5]. Historically, ITF tumors were treated invasively with disfiguring surgical resections which carried a high risk of complications and high morbidity and mortality rates [1,6,7]. However, the past decade has provided major advances in skull base microsurgery techniques, ranging from transcranial (TCS) to endoscopic endonasal surgery (EES) [8,9]. EES allows for a more expansive view of the skull base and its feasibility has greatly improved since early technical reports. This has led to an increased use of EES in ITF tumor management [10].
Despite the clinical importance of ITF tumors, the literature relies on case reports and single-center experiences [1,2,3,5]. In the present study, we reviewed the current literature, summarized the available data on ITF tumors, and described the current management protocols and their clinical outcomes.
2. Materials and Methods
2.1. Literature Search
A systematic review, registered to PROSPERO (ID: CRD42022362805), was conducted per the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [11]. PubMed, Scopus, and Cochrane databases were searched from inception to June 2021. A medical subject headings (MeSH) term and keyword search of each database was conducted using the Boolean operators OR and AND. Terms used were as follows: “infratemporal fossa” AND “carcinoma OR cancer OR tumor OR malignancy.” Identified papers were uploaded into Mendeley (Versioin 2.80.1, Mendeley Ltd., 27 October 2022, London, England), and duplicates were eliminated.
2.2. Study Selection
Inclusion and exclusion criteria were predetermined. Studies were included if they: (1) involved patients with skull base tumors located within the ITF, (2) reported data on clinical features, treatment protocols, and outcomes; (3) were written in the English language. Studies were excluded if they: (1) were literature reviews, case reports, technical notes, abstracts, or autopsy reports; (2) did not clearly differentiate data of patients with ITF tumors from data of patients with tumors in different anatomical locations; or (3) lacked treatment and outcome data.
Two authors (P.U. and O.B.-A.) independently assessed the titles and abstracts of all extracted papers based on the inclusion and exclusion criteria. Studies that met inclusion criteria were then further evaluated independently with full text review by the same two authors, and disagreements were resolved via a third author (A.S.H.). References of the included articles were also screened to retrieve additional relevant articles.
2.3. Data Extraction
Data from included studies were extracted by one author (L.S.B.) and confirmed independently by two authors (O.B.-A. and P.P.) to ensure accuracy. Extraction variables included: (1) author’s name, (2) date of publication, (3) level of evidence, (4) sample size, (5) sex, (6) presenting symptoms, (7) histological and radiological features, (8) management course and treatment modalities used (radiotherapy, chemotherapy, surgical approach), (9) recurrence, (10) survival outcomes. Missing data are either not reported by the original article or reported indistinctively from other data. Tumor volumes were reported as they were reported in the included articles. If the volume was not reported, radiological dimensions were used instead, if available.
2.4. Data Synthesis and Quality Assessment
The primary outcomes of interest were the characteristics of ITF tumors, the overall survival (OS) and progression-free survival (PFS) of patients, and additional predictive survival factors. The level of evidence of each article was evaluated following the 2011 Oxford Centre for Evidence-Based Medicine guidelines, and all articles were categorized as level IV evidence [12]. The risk of bias was independently assessed for each article by two authors (O.B.-A. and P.P.) using the Joanna Briggs Institute checklists [13]. Risk-of-bias assessment resulted in a low risk of bias in all included papers (Supplementary Table S1).
2.5. Statistical Analysis
R (Version 4.2.2, RStudio, Inc., R Foundation for Statistical Computing, Vienna, Austria, http://www.R-project.org/, accessed on 31 October 2022) was used for all statistical analyses. Continuous variables were summarized as median and interquartile ranges (IQR), while categorical variables were summarized as frequencies and percentages. The survival data were reported as median months (95% confidence interval [CI]). Not applicable (NA) in the CI limits indicates infinity due to the skewness of the data. Chi-square analyses were used to test significant differences between categorical variables. Using the R package ‘survival’, OS and PFS were calculated using Kaplan–Meier curves. The Cox proportional hazard model was used for the univariable and multivariable analyses to evaluate factors potentially affecting survival. For testing the proportional hazards assumption, Schoenfeld’s global test was used to estimate time-varying covariance. The schwannoma tumor type violated the proportional hazards assumption in the OS Cox proportional hazard model and was employed as a stratifying factor. Logistic regression analysis for complications was conducted by testing multiple patient and treatment factors. Continuous variables were categorized based on the most significant point based on Log rank testing. A two-tailed p-value < 0.05 was deemed to be significant for all analyses.
3. Results
3.1. Study Selection
The initial literature search yielded 2435 citations (Figure 1).
Figure 1.
PRISMA 2020 Flow-Diagram.
After elimination of duplicates, there were 1529 articles. A total of 1417 studies were excluded based on title and abstract screening. Of the 112 papers selected for retrieval, 85 articles failed to meet our inclusion criteria and were subsequently excluded. Thus, 27 articles were included in this systematic review based upon the prespecified criteria (Supplementary Table S2) [1,2,3,6,7,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35].
3.2. Demographics and Clinical Features
The present study included one hundred six patients with ITF tumors (median tumor size: 24.3 cm3 [IQR, 15.2–42 cm3]). The cohort’s median age was 46 years (IQR, 32–55 years), and males constituted 59.4% (n = 63) of the demographics (Table 1).
Table 1.
Demographics and clinical characteristics of the cohort (n = 106).
| Variable | n (%) |
|---|---|
| Age, years | 46 (IQR, 32–55) |
| Male sex | 63 (59.4%) |
| Tumor size, cm3 | 24.3 (15.2–42) |
| Involved structures | n = 111 |
| Pterygopalatine fossa | 29 (26.1%) |
| Temporomandibular Joint | 14 (12.6%) |
| The orbit | 14 (12.6%) |
| Maxilla | 12 (10.8%) |
| Cavernous sinus | 10 (9.0%) |
| Middle cranial fossa | 10 (9.0%) |
| Nasopharynx | 9 (8.1%) |
| Paranasal sinus | 6 (5.4%) |
| Zygomatic arch | 3 (2.7%) |
| Hard and soft palate | 1 (0.9%) |
| Temporomandibular fossa | 1 (0.9%) |
| Petroclival region | 1 (0.9%) |
| Oropharynx | 1 (0.9%) |
| Histopathology | n = 92 |
| Schwannoma | 24 (26.1%) |
| Meningioma | 13 (14.1%) |
| Synovial chondromatosis | 11 (12.0%) |
| Squamous cell carcinoma | 5 (5.4%) |
| Adenoid cystic carcinoma | 5 (5.4%) |
| Embryonal rhabdomyosarcoma | 4 (4.4%) |
| Synovial sarcoma | 3 (3.3%) |
| Lipomas | 2 (2.2%) |
| Solitary fibrous tumor | 2 (2.2%) |
| Pigmented villonodular synovitis | 2 (2.2%) |
| Synovial sarcoma | 2 (2.2%) |
| Neurofibroma | 2 (2.2%) |
| High-grade round-cells | 2 (2.2%) |
| Undifferentiated spindle-cells | 2 (2.2%) |
| Chondrosarcoma | 2 (2.2%) |
| Ameloblastoma | 1 (1.1%) |
| Sclerosing epithelioid fibrosarcoma | 1 (1.1%) |
| Alveolar soft part sarcoma | 1 (1.1%) |
| Hemangiopericytoma | 1 (1.1%) |
| Mucoepidermoid carcinoma | 1 (1.1%) |
| Nasopharyngeal carcinoma | 1 (1.1%) |
| Chondroma | 1 (1.1%) |
| Nasopharyngeal angiofibroma | 1 (1.1%) |
| Capillary hemangioma | 1 (1.1%) |
| Venous malformation a | 1 (1.1%) |
| Leiomyosarcoma | 1 (1.1%) |
| Presentation symptoms | n = 119 |
| Facial hypoesthesia | 22 (18.5%) |
| Auricular/preauricular pain | 20 (16.8%) |
| Headaches | 11 (9.2%) |
| Jaw deviation | 11 (9.2%) |
| Hearing loss | 9 (7.6%) |
| Facial pain | 8 (6.7%) |
| Trismus | 6 (5.0%) |
| Temporomandibular Joint pain | 4 (3.4%) |
| Diplopia | 3 (2.5%) |
| Decreased vision | 3 (2.5%) |
| Nasal obstruction/congestion | 2 (1.7%) |
| Vertigo | 2 (1.7%) |
| Trigeminal neuralgia | 2 (1.7%) |
| Exophthalmos | 2 (1.7%) |
| Otitis media | 1 (0.8%) |
| Dysarthria | 1 (0.8%) |
| Dysphagia | 1 (0.8%) |
| Dementia | 1 (0.8%) |
| Ptosis | 1 (0.8%) |
| Involved cranial nerves | n = 15 |
| CN III | 2 (13.3%) |
| CN IV | 1 (6.7%) |
| CN V | 7 (46.7%) |
| CN VI | 3 (20.0%) |
| CN VII | 1 (6.7%) |
| CN IX | 1 (6.7%) |
| Patients had surgical resection | 97 (95.1%) |
| Surgical approach | n = 95 * |
| TCS | 70 (73.7%) |
| EES | 25 (26.3%) |
| Mandibulotomy approach | 16 (17.8%) |
| Condylotomy with posterior disc attachment release | 14 (15.6%) |
| Unspecified endoscopic endonasal approach | 13 (14.4%) |
| Middle fossa/zygomatic approach | 9 (10.0%) |
| Endoscopic prelacrimal recess approach | 6 (6.7%) |
| Endoscopic extended medial maxillectomy | 5 (5.6%) |
| Cervical approach | 3 (3.3%) |
| Transmandibular approach | 3 (3.3%) |
| Submandibular and preauricular approach | 2 (2.2%) |
| Latero-facial approach | 2 (2.2%) |
| Degloving approach | 2 (2.2%) |
| Parotidectomy incision | 2 (2.2%) |
| Submandibular cutaneous incision | 1 (1.1%) |
| Preauricular subtemporal approach | 1 (1.1%) |
| Orbito-zygomatic approach | 1 (1.1%) |
| Left temporal craniotomy | 1 (1.1%) |
| Temporal and buccal incision | 1 (1.1%) |
| Weber Fergusson approach | 1 (1.1%) |
| Transzygomatic arch approach | 1 (1.1%) |
| Transcochlear approach | 1 (1.1%) |
| Orbito-zygomatic osteotomy | 1 (1.1%) |
| Zygomatic osteotomy | 1 (1.1%) |
| Antero-lateral, transcraniofacial, subtemporal, extradural approach | 1 (1.1%) |
| Coronal approach | 1 (1.1%) |
| Endoscopic Denker’s approach | 1 (1.1%) |
| Extent of surgical resection | n = 84 |
| Gross-total resection | 62 (73.8%) |
| Subtotal resection | 17 (20.2%) |
| Biopsy | 5 (6.0%) |
| Surgical complications | |
| All complications | 35 (33.0%) |
| Lingual nerve complication | 8 (22.9%) |
| Inferior alveolar nerve complication | 7 (20.0%) |
| Facial paresis | 7 (20.0%) |
| Partial facial numbness | 3 (8.6%) |
| Facial pain | 2 (5.7%) |
| Deep vein thrombosis | 2 (5.7%) |
| CN III Deficit | 1 (2.9%) |
| CN VI Deficit | 2 (5.7%) |
| CN VII Deficit | 1 (2.9%) |
| CN VIIII Deficit | 1 (2.9%) |
| Wound dehiscence | 1 (2.9%) |
| Reconstruction techniques and material | n = 8 |
| Adipofascial antero-lateral thigh flap | 4 (50%) |
| Latissimus dorsi free flap | 3 (37.5%) |
| Antero-lateral thigh flap | 1 (12.5%) |
| Adjuvant chemotherapy | n = 14 (13.2%) |
| Methotrexate | 1 (7.1%) |
| Cisplatin | 1 (7.1%) |
| Ifosfamide | 1 (7.1%) |
| Doxorubicin | 1 (7.1%) |
| Unknown | 10 (71.4%) |
| Adjuvant radiotherapy | n = 16 (15.1%) |
| EBRT | 3 (18.8%) |
| GKRS | 2 (12.5%) |
| Proton beam therapy | 1 (6.3%) |
| Unknown | 10 (62.5%) |
| Recurrence | 15 (14.2%) |
| Status | n = 97 |
| Alive | 88 (83.0%) |
| Dead | 18 (17.0%) |
| Survival rates | |
| 5-year OS | 20% |
| 5-year PFS | 61% |
| Median follow-up time in months (IQR) | 28 months (12.3–45.8) |
Data are reported as median and interquartile range (Q1–Q3) or frequencies and percentages. CN, cranial nerve; GKRS, Gamma Knife radiosurgery; EBRT, external beam radiotherapy; TCS, transcranial surgery EES, endoscopic endonasal surgery. * The transcranial approaches in the table do not sum up to the total number of transcranial surgery because many surgical approaches were unclarified. a This was reported by Liu et al. [16].
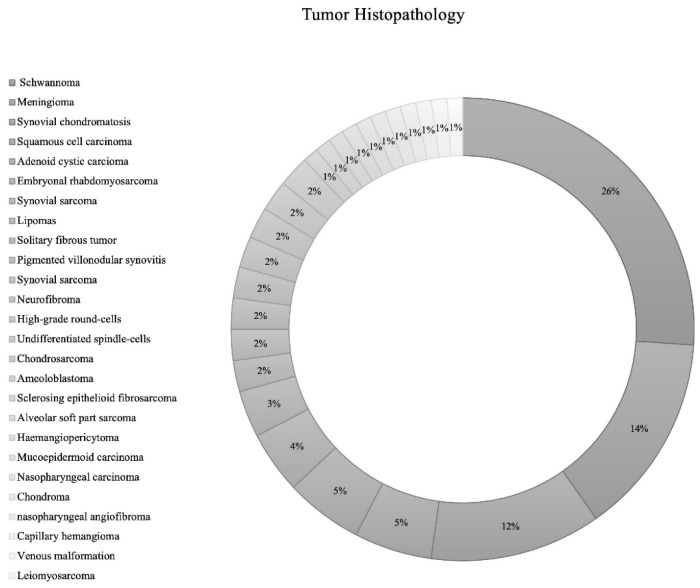
The most common structures invaded by ITF tumors were pterygopalatine fossa (n = 29; 26.1%), temporomandibular joint (n = 14; 12.6%), and the orbit (n = 14; 12.6%) (Table 1). While the included IFT tumors had various etiologies., the most common tumor types were schwannoma (n = 24; 26.1% [Trigeminal schwannoma n = 19; malignant schwannoma n = 1; facial schwannoma n = 1; unspecified cranial nerve schwannoma n = 3]), followed by meningioma (n = 13; 14.1% [grade 1 = 12; grade 2 = 1]), synovial chondromatosis (n = 11; 12.0%), squamous cell carcinoma (n = 5; 5.4%), and adenoid cystic carcinoma (n = 5; 5.4%) (Table 1; Figure 2).
Figure 2.
Pie chart of tumor histopathology.
The most common presenting symptoms included facial hypoesthesia (n = 22; 18.5%), auricular/preauricular pain (n = 20; 16.8%), headaches (n = 11; 9.2%), jaw deviation (n = 11; 9.2%), hearing loss (n = 9; 7.6%), and facial pain (n = 8; 6.7%). The trigeminal nerve was the most commonly impacted cranial nerve (n = 7; 46.7%), followed by the abducent (n = 3; 20.0%) and oculomotor (n = 2; 13.3%) cranial nerves (Table 1).
3.3. Management Paradigm and Postoperative Complications
Ninety-seven (95.1%) patients had surgical resections. Of these patients, 70 (73.7%) had TCS, and 25 (26.3%) had EES. The surgical method was not specified in two cases. Among cases with details on surgical approach, the most employed surgical approach was mandibulotomy (n = 16; 17.8%), followed by condylotomy with posterior disc attachment release (n = 14; 15.6%), unspecified endoscopic endonasal approach (n = 13; 14.4%), and middle fossa/zygomatic approach (n = 9; 10.0%). Of the cases that specified the extent of resection (n = 84), 62 (73.8%) patients had gross-total resection (GTR), 17 (20.2%) had subtotal resection (STR), and 5 (6.0%) had biopsy only. Among the various tumors, EES was employed in 19 (86%) trigeminal schwannomas, 2 (16.7%) benign meningiomas, 1 (33%) squamous cell carcinoma, and 1 (100%) atypical meningioma fibrous meningioma (Table 2; p < 0.01). The rest of the tumors had TCS.
Table 2.
Patient outcomes based on surgical approaches and tumor histology.
| Surgical Access Based on Tumor Histology | Number of Patients with Available Data | Endonasal Access No. (%) |
p-Value ^ |
|---|---|---|---|
| Trigeminal schwannoma | 22 | 19 (86%) | <0.01 |
| Grade 1 meningioma | 12 | 2 (16.7%) | |
| Squamous cell carcinoma | 3 | 1 (33%) | |
| Grade 2 meningioma | 1 | 1 (100%) | |
| The rest | 54 | 0 | |
| Complication Based on Surgical Access | Total Number of Patients with Each Access |
Complications
No. (%) |
p-Value ^ |
| Transcranial access | 70 | 33 (47.1%) | 0.01 |
| Endonasal access | 25 | 2 (8.0%) | |
| Complication Based on Surgical Approach | Total Number of Patients with Each Approach |
Complications
No. (%) |
p-Value ^ |
| Parotidectomy incision | 2 | 2 (100.0%) | <0.01 |
| Transzygomatic arch approach | 1 | 1 (100.0%) | |
| Latero-facial approach | 2 | 2 (100.0%) | |
| Mandibulotomy approach | 16 | 9 (56.3%) | |
| Middle fossa/zygomatic approach | 9 | 3 (33.3%) | |
| Endoscopic prelacrimal recess | 6 | 1 (16.7%) | |
| Cervical approach | 3 | 1 (33.3%) | |
| Condylotomy with posterior disc attachment release | 14 | 2 (14.3%) | |
| Endoscopic endonasal approach | 13 | 1 (7.7%) | |
| Recurrence Rate Based on Tumor Histology | Total Number of Patients |
Death
No. (%) |
p-Value ^ |
| Trigeminal schwannoma | 22 | 1 (5%) | 0.04 |
| Grade 1 meningioma | 12 | 3 (25%) | |
| Adenoid cystic carcinoma | 5 | 2 (40%) | |
| Squamous cell carcinoma | 5 | 1 (20%) | |
| Synovial sarcoma | 5 | 3 (60%) | |
| Alveolar soft part sarcoma | 1 | 1 (100%) | |
| Sclerosing epithelioid fibrosarcoma | 1 | 1 (100%) | |
| Grade 2 meningioma | 1 | 1 (100%) | |
| Capillary hemangioma | 1 | 1 (100%) | |
| The rest | 39 | 0 | |
| Mortality Rates Based on Tumor Histology | Total Number of Patients |
Death
No. (%) |
p -Value ^ |
| Trigeminal schwannoma | 22 | 3 (13.6%) | <0.01 |
| Grade 1 meningioma | 12 | 1 (8.3%) | |
| Adenoid cystic carcinoma | 5 | 1 (20%) | |
| Synovial sarcoma | 5 | 4 (80%) | |
| Neurofibroma | 2 | 2 (100%) | |
| Undifferentiated spindle cells | 2 | 2 (100%) | |
| Alveolar soft part sarcoma | 1 | 1 (100%) | |
| Sclerosing epithelioid fibrosarcoma | 1 | 1 (100%) | |
| The rest | 42 | 0 |
^ Chi-square test.
A total of 35 (33.0%) patients had surgical complications. The most common complications were lingual nerve complication (n = 8; 22.9%), inferior alveolar nerve complication (n = 7; 20.0%), and facial paresis (n = 7; 20.0%; Table 1). Complication rates were significantly higher among patients that had TCS (47.1%) when compared to EES (8.0%; p = 0.01; Table 2). Complication rates differed by surgical approach (Table 2; p < 0.01), and the highest complication rates were associated with the parotidectomy incision approach (100%), the transzygomatic arch approach (100%), and the latero-facial approach (100%).
Reconstruction techniques and material were reported in eight patients: four (50%) had adipofascial antero-lateral thigh flap, three (37.5%) had latissimus dorsi free flap, and one (12.5%) had antero-lateral thigh flap (Table 1).
Fourteen (13.2%) patients had adjuvant chemotherapy. One (7.1%) patient had Methotrexate, one (7.1%) had Cisplatin, one (7.1%) had Ifosfamide, and one (7.1%) had Doxorubicin. However, the chemotherapeutic agent was unknown in 10 (71.4%) patients.
Sixteen (15.1%) patients had adjuvant radiotherapy. Three (18.8%) had external beam radiotherapy, two (12.5%) had Gamma Knife radiosurgery, and one (6.3%) had proton beam therapy. However, radiotherapy modality was not specified in 10 (62.5%) patients (Table 1).
3.4. Patient Clinical and Survival Outcomes
During a median follow-up time of 28 months (IQR, 12.25–45.75 months), 15 (14.2%) patients had a tumor recurrence, and 18 (17.0%) patients died. The recurrence rate was highest among alveolar soft part sarcoma (n = 1; 100%), sclerosing epithelioid fibrosarcoma (n = 1; 100%), atypical meningioma (n = 1; 100%), capillary hemangioma (n = 1; 100%), and synovial sarcoma (n = 3; 60%; p = 0.04; Table 2). The mortality rate was highest among neurofibroma (n = 2; 100%), undifferentiated spindle cells (n = 2; 100%), alveolar soft part sarcoma (n = 1; 100%), and sclerosing epithelioid fibrosarcoma (n = 1; 100%; p < 0.01; Table 2). The 5-year OS rate was 20%, and the median OS time was 36 months (95% CI: 29–41 months; Table 1; Figure 3A). The 5-year PFS rate was 61%, and the median PFS time was not reached (95% CI: 48.0-NA; Table 1; Figure 3B). Disparity in the survival results was because the progression status was not reported in many patients and was considered censored.
Figure 3.
Kaplan–Meier curves of the (A) overall survival and (B) progression-free survival. The curve doted lines represent the 95% confidence intervals. The doted straight lines represent the. median.
Multivariable analyses of OS (Table 3) and PFS (Table 4) Cox proportional hazards did not result in any significant predictors.
Table 3.
Overall survival Cox proportional hazards of patient and treatment characteristics.
| Variable | Overall Survival | |||
|---|---|---|---|---|
| Univariable Analysis | Multivariable Analysis | |||
| HR (95% CI) | p Value | HR (95% CI) | p Value | |
| Age | 1.0 (0.9–1.0) | 0.4 | 1.0 (1.0–1.0) | 0.45 |
| Male sex | 0.9 (0.5–1.4) | 0.6 | 1.4 (0.6–3.4) | 0.42 |
| Schwannoma | 0.6 (0.3–1.1) | 0.09 | NA | NA |
| Meningioma | 1.5 (0.6–3.8) | 0.4 | NA | NA |
| Tumor volume cc | 1.0 (0.9–1.0) | 0.3 | 1.0 (1.0–1.0) | 0.09 |
| EES (Vs. TCS) | 0.7 (0.4–1.1) | 0.2 | NA | NA |
| GTR (Vs. STR) | 1.1 (0.8–1.6) | 0.2 | 6.5 (1.4–29.0) | 0.02 |
| Adjuvant chemotherapy | 0.6 (0.3–1.2) | 0.1 | 0.6 (0–52.4) | 0.82 |
| Adjuvant radiotherapy | 0.9 (0.4–1.9) | 0.7 | NA | NA |
Table 4.
Progression-free survival Cox proportional hazards of patient and treatment.
| Variable | Progression-Free Survival | |||
|---|---|---|---|---|
| Univariable Analysis | Multivariable Analysis | |||
| HR (95% CI) | p Value | HR (95% CI) | p Value | |
| Age | 0.9 (0.9–1.0) | 0.6 | 1 (0.9–1.2) | 0.6 |
| Male sex | 0.8 (0.3–2.1) | 0.6 | 9.37 × 108 (0-inf) | 1 |
| Schwannoma | 0.0 (0-inf) | 1 | 2.2 (0-inf) | 1 |
| Meningioma | 0.31 (0.1–1.0) | 0.04 | NA | NA |
| Tumor volume cc | 1.0 (1.0–1.0) | 0.9 | 1.0 (1.0–1.0) | 0.8 |
| EES (Vs. TCS) | 3.7 (0.8–16.4) | 0.08 | 2.66 × 108 (0-inf) | 1 |
| GTR (Vs. STR) | 2.5 (1.5–4.1) | <0.01 | 2.70 × 10−5 (0-inf) | 1 |
| Adjuvant chemotherapy | 0.26 (0.1–0.7) | <0.01 | 9.50 × 10−11 (0-inf) | 1 |
| Adjuvant radiotherapy | 0.32 (0.1–0.9) | 0.02 | NA | NA |
Similarly, the multivariable logistic regression analyses did not detect any significant correlation between postoperative complications and any of the patient or treatment factors (Table 5).
Table 5.
Logistic regression of complications.
| Variable | Complications | |||
|---|---|---|---|---|
| Univariable Analysis | Multivariable Analysis | |||
| OR (95% CI) | p Value | OR (95% CI) | p Value | |
| Age > 46 years | 2.4 (0.7–9.8) | 0.2 | 5.58 × 108 (1.59 × 10−209-NA) | 1.0 |
| Male sex | 0.3 (0.1–1.1) | 0.09 | 5.58 × 108 (0–1) | 0.1 |
| Tumor volume > 24.3 cc | 2.1 (0.19–48.4) | 0.6 | 2.6 (0.1–236.5) | 0.6 |
| EES (Vs. TCS) | 4.1 (1.1–27.1) | 0.07 | 0.4 (0–16.9) | 0.6 |
| GTR (Vs. STR) | 1.5 (0.8–2.7) | 0.18 | 4.5 (0–1.6 × 1095) | 1.0 |
4. Discussion
Our systematic review found high rates of schwannoma and meningioma among tumors involving the ITF. Most of these tumors were resected using transcranial surgery (73.7%), and gross-total resection was achieved in 20.2% of cases. The median OS time was 36 months (95% CI: 29–41 months), and the 5-year PFS rate was 61%. The multivariable analysis did not detect any significant predictors of OS, PFS, or complication rates.
4.1. Patient Clinical Characteristics
In line with other skull base neoplastic lesions, the median age was 46 years and 59.4% of the patients were males [36,37,38]. The pterygopalatine fossa, temporomandibular joint, and the orbit were the most invaded structures [39,40]. The most common tumor types in our study were meningiomas and schwannomas. This is more a reflection of the general prevalence of these tumor types, as meningiomas and schwannomas are among the most common primary intracranial tumors [41,42,43].
The clinical presentation of ITF tumors in our study mainly included facial hypoesthesia, auricular/preauricular pain, headaches, and jaw deviation. Clinical symptoms were concordant with the anatomical location affecting the surrounding craniofacial structures [44,45].
4.2. Management and Survival Outcomes
In our study, 73.7% of the cohort had a transcranial approach. However, our review encompasses data in studies published before the EES era. While different transcranial approaches have been used since then, EES has been increasingly adopted in the skull base literature due to its low postoperative complications and shorter preparative stay [46,47,48]. Several authors have further advanced the techniques and proposed alternative approaches which has led to maximized exposure of the posterolateral wall of the maxillary sinus [1,39,40]. We found that the EES was more frequently implemented for benign tumors, such as trigeminal schwannomas and meningiomas, that are accessible by endoscopic endonasal access, whereas TCS was mainly employed for malignant tumors with extracranial extension. This trend was corroborated in other reports, where tumors resected using EES appeared to be largely benign and anatomically located within the field of endoscopic endonasal access [49,50]. The data represents the clinical paradigm of managing primary malignant disease with radical resections, despite correspondingly higher comorbidity, whereas a partial resection could still yield good long-term results in the setting of benign tumors. Although postoperative complications were significantly more common among patients who had TCS than EES, our logistic regression analysis did not find any significant predictors of complications. However, we attribute the absence of significance to the small sample size among which complication details were reported. An increasing body of the literature has shown that EES has offered a minimally invasive option while achieving comparative extents of resection for different anterior and middle skull base lesions; although conclusive results are yet to be published [47,51,52]. In a comparative analysis, Bander et al. [53] compared EES and TCS for tuberculum sellae and planum sphenoidale meningiomas. They found a higher rate of visual symptoms improvement (EES: 93% vs. TCS: 56%; p = 0.049) and a lower rate of visual function deterioration (EES: 0% vs. TCS: 44%; p = 0.012) among EES compared to TCS. Similarly, Jimenez et al. [54] conducted a meta-analysis comparing the TCS and EES for suprasellar meningiomas. Their analysis showed that EES had significantly higher odds of visual improvement (Odds Ratio [OR] = 3.24, p = 0.0053) compared to TCS but had significantly higher odds of a cerebrospinal fluid leak (OR = 3.71, p = 0.0098) compared to TCS. Although generally multifactional, our results, in addition to the literature, highlight a better postoperative recovery related to EES and advocate for EES, when possible, to minimize complications attributed to the invasiveness of transcranial access. As a general paradigm, benign tumors within the field of endoscopic endonasal exposure should undergo EES, while malignant tumors in difficult locations may undergo TCS with maximum safe resection to provide the best possible outcomes.
In the realm of skull base surgery, reconstruction techniques and materials are essential aspects of surgical planning. Among available data, 50% of patients had adipofascial anterolateral thigh flap and 37.5% had latissimus dorsi free flap. Several techniques and materials are described in the literature for different locations of the skull base [55,56]. The decision typically relies on different factors including support rigidity and the vascular supply. For instance, since lateral skull base lesions often do not require firm support, the repair of the middle fossa floor is typically performed using a temporalis muscle flap [18]. However, numerous necrosis events have been reported, deeming muscle vasculature maintenance essential and leading others to adopt vascularly rich flaps, such as free rectus abdominis [57,58].
Although only in the univariable analysis, we found that adjuvant radiotherapy and chemotherapy independently decreased the risk of tumor progression. Our results confirmed the established role of adjuvant chemotherapy and radiotherapy in the management paradigm for different skull base lesions. While chemotherapy has been documented to improve survival in malignant lesions, radiotherapy as a primary or adjuvant modality aims mainly to halt tumor progression. Studies that investigated the efficacy of radiotherapy for meningiomas and schwannomas reported high 10-year PFS rates of up to 90–98% [59,60,61,62,63,64,65,66]. However, since different tumor types respond differently to various modalities, it is essential to tailor a personalized management plan based on the patient tumor pathology and their clinical condition.
4.3. Limitations
Our results were limited by several factors, including the retrospective nature of the included articles, their inclusion criteria, methodology, treatment protocols, and clinical outcomes evaluated in each included article. Different pathologies were included with insufficient data to delineate the analysis based on the tumor type. The statistical power of multiple endpoints was reduced by the small sample sizes of the present article. Further studies are needed to investigate the impact of different surgical approaches on various pathologies and describe their complication profile and reconstruction methods.
5. Conclusions
The ITF is invaded by various neoplastic pathologies, presenting a management challenge due to the wide range of invading tumors that exhibit different biological behaviors. Tumor pathology and overall patient condition should be used to devise a multimodal treatment regimen combining surgical resection, chemotherapy, and/or radiotherapy to optimize therapeutic benefit and minimize postoperative morbidity.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/cancers14215420/s1, Supplementary Table S1: Risk of bias assessments for all included studies. Supplementary Table S2. Overview of included articles.
Author Contributions
Conceptualization, O.B.-A. and A.S.H.; methodology, O.B.-A.; validation, K.B., O.B.-A. and A.S.H.; formal analysis, O.B.-A.; resources, G.F., A.V., V.Z., P.U., K.Y., A.A.C.-G. and T.Y.E.A.; data curation, L.S.B.; writing—original draft preparation, O.B.-A.; writing—review and editing, G.F., P.P., K.Y., A.A.C.-G., T.Y.E.A. and A.S.H.; visualization, O.B.-A.; supervision, A.S.H.; project administration, P.P. and G.F. All authors have read and agreed to the published version of the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Zhou B., Huang Q., Shen P.-H., Cui S.-J., Wang C.-S., Li Y.-C., Yu Z.-K., Chen X.-H., Ye T. The Intranasal Endoscopic Removal of Schwannoma of the Pterygopalatine and Infratemporal Fossae via the Prelacrimal Recess Approach. J. Neurosurg. 2016;124:1068–1073. doi: 10.3171/2015.3.JNS132702. [DOI] [PubMed] [Google Scholar]
- 2.Shin M., Shojima M., Kondo K., Hasegawa H., Hanakita S., Ito A., Kin T., Saito N. Endoscopic Endonasal Craniofacial Surgery for Recurrent Skull Base Meningiomas Involving the Pterygopalatine Fossa, the Infratemporal Fossa, the Orbit, and the Paranasal Sinus. World Neurosurg. 2018;112:E302–E312. doi: 10.1016/j.wneu.2018.01.041. [DOI] [PubMed] [Google Scholar]
- 3.Nomura F., Kishimoto S. Synovial Sarcoma of the Temporomandibular Joint and Infratemporal Fossa. Auris Nasus Larynx. 2014;41:572–575. doi: 10.1016/j.anl.2014.07.001. [DOI] [PubMed] [Google Scholar]
- 4.Hughes K.V., Olsen K.D., McCaffrey T.V. Parapharyngeal Space Neoplasms. Head Neck. 1995;17:124–130. doi: 10.1002/hed.2880170209. [DOI] [PubMed] [Google Scholar]
- 5.Das U.C., Stephen A., Ross A., Chary G., Chand A.K. Facial Translocation Approach to Infratemporal Fossa and Cranial Base in Extensive Angiofibroma: A Review of 7 Cases. Indian J. Otolaryngol. Head Neck Surg. 2005;57:17. doi: 10.1007/BF02907619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Murayama S., Suzuki I., Nagase M., Shingaki S., Kawasaki T., Nakajima T., Fukushima M., Ishiki T. Chondrosarcoma of the Mandible. Report of Case and a Survey of 23 Cases in the Japanese Literature. J. Craniomaxillofac. Surg. 1988;16:287–292. doi: 10.1016/S1010-5182(88)80063-5. [DOI] [PubMed] [Google Scholar]
- 7.Shapshay S.M., Elber E., Strong M.S. Occult Tumors of the Infratemporal Fossa: Report of Seven Cases Appearing as Preauricular Facial Pain. Arch. Otolaryngol. 1976;102:535–538. doi: 10.1001/archotol.1976.00780140067006. [DOI] [PubMed] [Google Scholar]
- 8.Stippler M., Gardner P.A., Snyderman C.H., Carrau R.L., Prevedello D.M., Kassam A.B. Endoscopic Endonasal Approach for Clival Chordomas. Neurosurgery. 2009;64:268. doi: 10.1227/01.NEU.0000338071.01241.E2. [DOI] [PubMed] [Google Scholar]
- 9.Wang E.W., Zanation A.M., Gardner P.A., Schwartz T.H., Eloy J.A., Adappa N.D., Bettag M., Bleier B.S., Cappabianca P., Carrau R.L., et al. ICAR: Endoscopic Skull-Base Surgery. Int. Forum Allergy Rhinol. 2019;9:S145–S365. doi: 10.1177/1945892418817221. [DOI] [PubMed] [Google Scholar]
- 10.Kassam A.B., Gardner P., Snyderman C., Mintz A., Carrau R. Expanded Endonasal Approach: Fully Endoscopic, Completely Transnasal Approach to the Middle Third of the Clivus, Petrous Bone, Middle Cranial Fossa, and Infratemporal Fossa. Neurosurg. Focus. 2005;19:E6. doi: 10.3171/foc.2005.19.1.7. [DOI] [PubMed] [Google Scholar]
- 11.Moher D., Liberati A., Tetzlaff J., Altman D.G., Altman D., Antes G., Atkins D., Barbour V., Barrowman N., Berlin J.A., et al. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Howick J., Chalmers I., Glasziou P., Greenhalgh T., Heneghan C., Liberati A., Hodgkinson M. The Oxford 2011 Levels of Evidence. Oxford Centre Evidence-Based Medicine. [(accessed on 15 March 2009)]. Available online: https://www.cebm.ox.ac.uk/resources/levels-of-evidence/ocebm-levels-of-evidence.
- 13.Munn Z., Barker T.H., Moola S., Tufanaru C., Stern C., McArthur A., Stephenson M., Aromataris E. Methodological Quality of Case Series Studies: An Introduction to the JBI Critical Appraisal Tool. JBI Evid. Synth. 2020;18:2127–2133. doi: 10.11124/JBISRIR-D-19-00099. [DOI] [PubMed] [Google Scholar]
- 14.Wenig B.M., Abbondanzo S.L., Childers E.L., Kapadia S.B., Heffner D.R. Extranodal Sinus Histiocytosis with Massive Lymphadenopathy (Rosai-Dorfman Disease) of the Head and Neck. Hum. Pathol. 1993;24:483–492. doi: 10.1016/0046-8177(93)90160-I. [DOI] [PubMed] [Google Scholar]
- 15.Chung J.W., Ahn J.H., Kim J.H., Nam S.Y., Kim C.-J., Lee K.-S. Facial Nerve Schwannomas: Different Manifestations and Outcomes. Surg. Neurol. 2004;62:245–252; discussion 452. doi: 10.1016/j.surneu.2003.09.034. [DOI] [PubMed] [Google Scholar]
- 16.Liu X., Wan S., Abdelrehem A., Chen M., Yang C. Benign Temporomandibular Joint Tumours with Extension to Infratemporal Fossa and Skull Base: Condyle Preserving Approach. Int. J. Oral Maxillofac. Surg. 2020;49:867–873. doi: 10.1016/j.ijom.2019.12.009. [DOI] [PubMed] [Google Scholar]
- 17.Zhang Q., Feng K., Ge C., Hongchuan G., Mingchu L. Endoscopic Endonasal Management of Trigeminal Schwannomas Extending into the Infratemporal Fossa. J. Clin. Neurosci. 2012;19:862–865. doi: 10.1016/j.jocn.2011.09.023. [DOI] [PubMed] [Google Scholar]
- 18.Colmenero C., Perez Alvarez M., Alonso A. Adenoid Cystic Carcinoma of the Infraspheno-Temporal Fossa. Latero-Facial Resection Combined with Multiple Osteotomies. J. Craniomaxillofac. Surg. 1991;19:212–216. doi: 10.1016/S1010-5182(05)80550-5. [DOI] [PubMed] [Google Scholar]
- 19.Galioto S., Valentini V., Fatone F.M.G., Rabagliati M., Autelitano L., Iannetti G. Solitary Fibrous Tumours of the Infratemporal Fossa. Two Case Reports. J. Craniomaxillofac. Surg. 2006;34:494–501. doi: 10.1016/j.jcms.2006.07.864. [DOI] [PubMed] [Google Scholar]
- 20.Chatni S.S., Sharan R., Patel D., Iyer S., Tiwari R.M., Kuriakose M.A. Transmandibular Approach for Excision of Maxillary Sinus Tumors Extending to Pterygopalatine and Infratemporal Fossae. Oral Oncol. 2009;45:720–726. doi: 10.1016/j.oraloncology.2008.11.005. [DOI] [PubMed] [Google Scholar]
- 21.Kakudo N., Kusumoto K., Takemoto T., Tanaka Y., Kurokawa I., Ogawa Y. Dumbbell-Formed Lipomas under the Zygomatic Arch. J. Plast. Reconstr. Aesthet. Surg. 2008;61:107–110. doi: 10.1016/j.bjps.2006.06.011. [DOI] [PubMed] [Google Scholar]
- 22.Morace R., Marongiu A., Vangelista T., Galasso V., Colonnese C., Giangaspero F., Innocenzi G., Esposito V., Cantore G. Intracranial Capillary Hemangioma: A Description of Four Cases. World Neurosurg. 2012;78:191.E15–191.E21. doi: 10.1016/j.wneu.2011.09.017. [DOI] [PubMed] [Google Scholar]
- 23.Wang X., Bao Y., Chen G., Guo H., Li M., Liang J., Bai X., Ling F. Trigeminal Schwannomas in Middle Fossa Could Breach into Subdural Space: Report of 4 Cases and Review of Literature. World Neurosurg. 2019;127:e534–e541. doi: 10.1016/j.wneu.2019.03.194. [DOI] [PubMed] [Google Scholar]
- 24.Kekatpure V.D., Hedne N., Chavre S., Pillai V., Trivedi N., Kuriakose M.A. Versatility of Adipofascial Anterolateral Thigh Flap for Reconstruction of Maxillary Defects with Infratemporal Fossa Extension. Craniomaxillofac. Trauma Reconstr. 2014;7:213–217. doi: 10.1055/s-0034-1371973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Krishnamurthy S., Holmes B., Powers S.K. Schwannomas Limited to the Infratemporal Fossa: Report of Two Cases. J. Neuro-Oncol. 1998;36:269–277. doi: 10.1023/A:1005827010429. [DOI] [PubMed] [Google Scholar]
- 26.Xu F., Sun X., Hu L., Wang J., Wang D., Pasic T.R., Kern R.C. Endoscopic Surgical Treatment of Neurogenic Tumor in Pterygopalatine and Infratemporal Fossae via Extended Medial Maxillectomy. Acta Otolaryngol. 2011;131:161–165. doi: 10.3109/00016489.2010.522594. [DOI] [PubMed] [Google Scholar]
- 27.Deneuve S., Teissier N., Jouffroy T., Helfre S., Boissonnet H., Freneaux P., Peuchmaur M., Brisse H., Van Den Abbeele T., Orbach D. Skull Base Surgery for Pediatric Parameningeal Sarcomas. Head Neck. 2012;34:1057–1063. doi: 10.1002/hed.21865. [DOI] [PubMed] [Google Scholar]
- 28.Sichel J.Y., Monteil J.P., Elidan J. Skull Base Chondroma of Extracranial Origin. Head Neck. 1994;16:578–581. doi: 10.1002/hed.2880160614. [DOI] [PubMed] [Google Scholar]
- 29.Haidar H., Deveze A., Lavieille J.P. Mini-Invasive Surgery of Infratemporal Fossa Schwannomas. J. Laryngol. Otol. 2015;129:187–193. doi: 10.1017/S0022215114003120. [DOI] [PubMed] [Google Scholar]
- 30.Dare A.O., Gibbons K.J., Proulx G.M., Fenstermaker R.A. Resection Followed by Radiosurgery for Advanced Juvenile Nasopharyngeal Angiofibroma: Report of Two Cases. Neurosurgery. 2003;52:1207–1211; discussion 1211. [PubMed] [Google Scholar]
- 31.Folk G.S., Williams S.B., Foss R.B., Fanburg-Smith J.C. Oral and Maxillofacial Sclerosing Epithelioid Fibrosarcoma: Report of Five Cases. Head Neck Pathol. 2007;1:13–20. doi: 10.1007/s12105-007-0002-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Al-Daraji W., Lasota J., Foss R., Miettinen M. Synovial Sarcoma Involving the Head: Analysis of 36 Cases with Predilection to the Parotid and Temporal Regions. Am. J. Surg. Pathol. 2009;33:1494–1503. doi: 10.1097/PAS.0b013e3181aa913f. [DOI] [PubMed] [Google Scholar]
- 33.Lee J.T., Suh J.D., Carrau R.L., Chu M.W., Chiu A.G. Endoscopic Denker’s Approach for Resection of Lesions Involving the Anteroinferior Maxillary Sinus and Infratemporal Fossa. Laryngoscope. 2017;127:556–560. doi: 10.1002/lary.26237. [DOI] [PubMed] [Google Scholar]
- 34.Buchanan G. Two Rare Tumours Involving the Infratemporal Fossa: Alveolar Soft Part Sarcoma and Haemangiopericytoma. J. Laryngol. Otol. 1975;89:375–389. doi: 10.1017/S0022215100080506. [DOI] [PubMed] [Google Scholar]
- 35.Pieper D.R., Al-Mefty O. Management of Intracranial Meningiomas Secondarily Involving the Infratemporal Fossa: Radiographic Characteristics, Pattern of Tumor Invasion, and Surgical Implications. Neurosurgery. 1999;45:231–237. doi: 10.1097/00006123-199908000-00005. [DOI] [PubMed] [Google Scholar]
- 36.Liu D.Y., Yuan X.R., Liu Q., Jiang X.J., Jiang W.X., Peng Z.F., Ding X.P., Luo D.W., Yuan J. Large Medial Sphenoid Wing Meningiomas: Long-Term Outcome and Correlation with Tumor Size after Microsurgical Treatment in 127 Consecutive Cases. Turk. Neurosurg. 2012;22:547–557. doi: 10.5137/1019-5149.JTN.5142-11.1. [DOI] [PubMed] [Google Scholar]
- 37.Sheehan J.P., Starke R.M., Kano H., Kaufmann A.M., Mathieu D., Zeiler F.A., West M., Chao S.T., Varma G., Chiang V.L.S., et al. Gamma Knife Radiosurgery for Sellar and Parasellar Meningiomas: A Multicenter Study. J. Neurosurg. 2015;127:A1562–A1563. doi: 10.3171/2014.2.JNS13139. WE-Science Citation Index Expanded. [DOI] [PubMed] [Google Scholar]
- 38.Mühl-Benninghaus R., Neumann J. Malignant tumors of the skull base. Radiologe. 2019;59:1064–1070. doi: 10.1007/s00117-019-00600-5. [DOI] [PubMed] [Google Scholar]
- 39.Taylor R.J., Patel M.R., Wheless S.A., McKinney K.A., Stadler M.E., Sasaki-Adams D., Ewend M.G., Germanwala A.V., Zanation A.M. Endoscopic Endonasal Approaches to Infratemporal Fossa Tumors: A Classification System and Case Series. Laryngoscope. 2014;124:2443–2450. doi: 10.1002/lary.24638. [DOI] [PubMed] [Google Scholar]
- 40.Theodosopoulos P.V., Guthikonda B., Brescia A., Keller J.T., Zimmer L.A. Endoscopic Approach to the Infratemporal Fossa: Anatomic Study. Neurosurgery. 2010;66:196–202. doi: 10.1227/01.NEU.0000359224.75185.43. [DOI] [PubMed] [Google Scholar]
- 41.Longstreth W.T.J., Dennis L.K., McGuire V.M., Drangsholt M.T., Koepsell T.D. Epidemiology of Intracranial Meningioma. Cancer. 1993;72:639–648. doi: 10.1002/1097-0142(19930801)72:3<639::AID-CNCR2820720304>3.0.CO;2-P. [DOI] [PubMed] [Google Scholar]
- 42.Wiemels J., Wrensch M., Claus E.B. Epidemiology and Etiology of Meningioma. J. Neurooncol. 2010;99:307–314. doi: 10.1007/s11060-010-0386-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Berkowitz O., Iyer A.K., Kano H., Talbott E.O., Lunsford L.D. Epidemiology and Environmental Risk Factors Associated with Vestibular Schwannoma. World Neurosurg. 2015;84:1674–1680. doi: 10.1016/j.wneu.2015.07.007. [DOI] [PubMed] [Google Scholar]
- 44.Cherekaev V.A., Korshunov A.G., Kornienko V.N., Bekiashev A.K., Belov A.I., Vinokurov A.G., Tsikarishvili V.M., Kadasheva A.B., Smirnov R.A. Skull base meningiomas spreading into the infratemporal fossa: Clinical picture, diagnosis, and treatment policy. Zhurnal Vopr. Neirokhirurgii Im. NN Burd. 2004;4:6–11. [PubMed] [Google Scholar]
- 45.Bouaziz A., Chabardes E., Laccourreye O., Menard M., Brasnu D., Laccourreye H. Extension to the infratemporal fossa of malignant tumors of the face. Ann. Otolaryngol. Chir. Cervicofac. 1991;108:113–118. [PubMed] [Google Scholar]
- 46.Paluzzi A., Gardner P., Fernandez-Miranda J.C., Snyderman C. The Expanding Role of Endoscopic Skull Base Surgery. Br. J. Neurosurg. 2012;26:649–661. doi: 10.3109/02688697.2012.673649. [DOI] [PubMed] [Google Scholar]
- 47.Raza S.M., Amine M.A., Anand V., Schwartz T.H. Endoscopic Endonasal Resection of Trigeminal Schwannomas. Neurosurg. Clin. N. Am. 2015;26:473–479. doi: 10.1016/j.nec.2015.03.010. [DOI] [PubMed] [Google Scholar]
- 48.Oakley G.M., Harvey R.J. Endoscopic Resection of Pterygopalatine Fossa and Infratemporal Fossa Malignancies. Otolaryngol. Clin. N. Am. 2017;50:301–313. doi: 10.1016/j.otc.2016.12.007. [DOI] [PubMed] [Google Scholar]
- 49.Borg A., Kirkman M.A., Choi D. Endoscopic Endonasal Anterior Skull Base Surgery: A Systematic Review of Complications During the Past 65 Years. World Neurosurg. 2016;95:383–391. doi: 10.1016/j.wneu.2015.12.105. [DOI] [PubMed] [Google Scholar]
- 50.Gaillard S. The Transition from Microscopic to Endoscopic Transsphenoidal Surgery in High-Caseload Neurosurgical Centers: The Experience of Foch Hospital. World Neurosurg. 2014;82:S116–S120. doi: 10.1016/j.wneu.2014.07.033. [DOI] [PubMed] [Google Scholar]
- 51.Zhang Q., Wang Z., Guo H., Yan B., Wang Z., Zhao H., Sahyouni R., Kuan E.C. Direct Transcavernous Sinus Approach for Endoscopic Endonasal Resection of Intracavernous Sinus Tumors. World Neurosurg. 2019;128:e478–e487. doi: 10.1016/j.wneu.2019.04.182. [DOI] [PubMed] [Google Scholar]
- 52.Lucas J.W., Zada G. Endoscopic Endonasal and Keyhole Surgery for the Management of Skull Base Meningiomas. Neurosurg. Clin. N. Am. 2016;27:207–214. doi: 10.1016/j.nec.2015.11.008. [DOI] [PubMed] [Google Scholar]
- 53.Bander E.D., Singh H., Ogilvie C.B., Cusic R.C., Pisapia D.J., Tsiouris A.J., Anand V.K., Schwartz T.H. Endoscopic Endonasal versus Transcranial Approach to Tuberculum Sellae and Planum Sphenoidale Meningiomas in a Similar Cohort of Patients. J. Neurosurg. 2018;128:40–48. doi: 10.3171/2016.9.JNS16823. [DOI] [PubMed] [Google Scholar]
- 54.Jimenez A.E., Harrison Snyder M., Rabinovich E.P., Malkawi D., Chakravarti S., Wei O., Cheshire M., Carrie Price M.L.S., Khalafallah A.M., Rowan N.R., et al. Comparison and Evolution of Transcranial versus Endoscopic Endonasal Approaches for Suprasellar Meningiomas: A Systematic Review. J. Clin. Neurosci. 2022;99:302–310. doi: 10.1016/j.jocn.2022.03.029. [DOI] [PubMed] [Google Scholar]
- 55.Van Ngo C., Nguyen H., Aklinski J., Minh L.H.N., Le H.H., Nguyen K.N., Tran U.H., Le N., Huynh Le P., Tran T.M. Reconstruction of Large Anterior Skull Base Defects After Resection of Sinonasal Tumors With Intracranial Extension by Using Pedicled Double Flap Techniques. J. Craniofac. Surg. 2022 doi: 10.1097/SCS.0000000000008976. [DOI] [PubMed] [Google Scholar]
- 56.Qadeer N., Mehrara B.J., Cohen M., Tabar V., Shahzad F. Endoscopic Endonasal Repair of Recurrent Cerebrospinal Fluid Leak With Adipofascial Anterolateral Thigh Free Flap: Case Report and Review of Literature. Eplasty. 2022;22:e32. [PMC free article] [PubMed] [Google Scholar]
- 57.Smith P.G., Grubb R.L., Kletzker G.R., Leonetti J.P. Combined Pterional-Anterolateral Approaches to Cranial Base Tumors. Otolaryngol. Head Neck Surg. 1990;103:357–363. doi: 10.1177/019459989010300304. [DOI] [PubMed] [Google Scholar]
- 58.Sekhar L.N., Schramm V.L.J., Jones N.F., Yonas H., Horton J., Latchaw R.E., Curtin H. Operative Exposure and Management of the Petrous and Upper Cervical Internal Carotid Artery. Neurosurgery. 1986;19:967–982. doi: 10.1227/00006123-198612000-00012. [DOI] [PubMed] [Google Scholar]
- 59.Tysome J.R., Macfarlane R., Durie-Gair J., Donnelly N., Mannion R., Knight R., Harris F., Vanat Z.H., Tam Y.C., Burton K., et al. Surgical Management of Vestibular Schwannomas and Hearing Rehabilitation in Neurofibromatosis Type 2. Otol. Neurotol. 2012;33:466–472. doi: 10.1097/MAO.0b013e318248eaaa. [DOI] [PubMed] [Google Scholar]
- 60.Nowak A., Dziedzic T., Czernicki T., Kunert P., Morawski K., Niemczyk K., Marchel A. Strategy for the Surgical Treatment of Vestibular Schwannomas in Patients with Neurofibromatosis Type 2. Neurol. Neurochir. Pol. 2015;49:295–301. doi: 10.1016/j.pjnns.2015.06.008. [DOI] [PubMed] [Google Scholar]
- 61.Samii M., Gerganov V., Samii A. Microsurgery Management of Vestibular Schwannomas in Neurofibromatosis Type 2: Indications and Results. Prog. Neurol. Surg. 2008;21:169–175. doi: 10.1159/000156905. [DOI] [PubMed] [Google Scholar]
- 62.Johnson S., Kano H., Faramand A., Pease M., Nakamura A., Hassib M., Spencer D., Sisterson N., Faraji A.H., Arai Y., et al. Long Term Results of Primary Radiosurgery for Vestibular Schwannomas. J. Neurooncol. 2019;145:247–255. doi: 10.1007/s11060-019-03290-0. [DOI] [PubMed] [Google Scholar]
- 63.Ogino A., Lunsford L.D., Long H., Johnson S., Faramand A., Niranjan A., Flickinger J.C., Kano H. Stereotactic Radiosurgery as the First-Line Treatment for Intracanalicular Vestibular Schwannomas. J. Neurosurg. 2021;135:1051–1057. doi: 10.3171/2020.9.JNS202818. [DOI] [PubMed] [Google Scholar]
- 64.Ogino A., Lunsford L.D., Long H., Johnson S., Faramand A., Niranjan A., Flickinger J.C., Kano H. Stereotactic Radiosurgery as the Primary Management for Patients with Koos Grade IV Vestibular Schwannomas. J. Neurosurg. 2021;12:1–9. doi: 10.3171/2020.8.JNS201832. [DOI] [PubMed] [Google Scholar]
- 65.Bunevicius A., Anand R.K., Suleiman M., Nabeel A.M., Reda W.A., Tawadros S.R., Abdelkarim K., El-Shehaby A.M.N., Emad R.M., Chytka T., et al. Stereotactic Radiosurgery for Perioptic Meningiomas: An International, Multicenter Study. Neurosurgery. 2021;88:828–837. doi: 10.1093/neuros/nyaa544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Bin-Alamer O., Alnefaie N., Qedair J., Chaudhary A., Hallak H., Abdulbaki A., Mallela A.N., Palmisciano P., Gersey Z.C., Legarreta A.D., et al. Single Session versus Multisession Stereotactic Radiosurgery for the Management of Intracranial Meningiomas: A Systematic Review and Meta-Analysis. J. Neurooncol. 2022 doi: 10.1007/s11060-022-04112-6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.