Abstract
Background
Nonalcoholic fatty liver disease is associated with an increased cardiovascular disease (CVD) risk, although the exact mechanism(s) are less clear. Moreover, the relationship between newly redefined metabolic-associated fatty liver disease (MAFLD) and CVD risk has been poorly investigated. Data-driven machine learning (ML) techniques may be beneficial in discovering the most important risk factors for CVD in patients with MAFLD.
Methods
In this observational study, the patients with MAFLD underwent subclinical atherosclerosis assessment and blood biochemical analysis. Patients were split into two groups based on the presence of CVD (defined as at least one of the following: coronary artery disease; myocardial infarction; coronary bypass grafting; stroke; carotid stenosis; lower extremities artery stenosis).
The ML techniques were utilized to construct a model which could identify individuals with the highest risk of CVD. We exploited the multiple logistic regression classifier operating on the most discriminative patient’s parameters selected by univariate feature ranking or extracted using principal component analysis (PCA). Receiver operating characteristic (ROC) curves and area under the ROC curve (AUC) were calculated for the investigated classifiers, and the optimal cut-point values were extracted from the ROC curves using the Youden index, the closest to (0, 1) criteria and the Index of Union methods.
Results
In 191 patients with MAFLD (mean age: 58, SD: 12 years; 46% female), there were 47 (25%) patients who had the history of CVD. The most important clinical variables included hypercholesterolemia, the plaque scores, and duration of diabetes. The five, ten and fifteen most discriminative parameters extracted using univariate feature ranking and utilized to fit the ML models resulted in AUC of 0.84 (95% confidence interval [CI]: 0.77–0.90, p < 0.0001), 0.86 (95% CI 0.80–0.91, p < 0.0001) and 0.87 (95% CI 0.82–0.92, p < 0.0001), whereas the classifier fitted over 10 principal components extracted using PCA followed by the parallel analysis obtained AUC of 0.86 (95% CI 0.81–0.91, p < 0.0001). The best model operating on 5 most discriminative features correctly identified 114/144 (79.17%) low-risk and 40/47 (85.11%) high-risk patients.
Conclusion
A ML approach demonstrated high performance in identifying MAFLD patients with prevalent CVD based on the easy-to-obtain patient parameters.
Keywords: Cardiovascular disease, Metabolic-associated fatty liver disease, Machine learning
Background
According to the statistics from the Global Burden of Disease study 2017, a significant number of all deaths globally (over 70%) is caused by noncommunicable diseases, and CVD accounts for more than 43% [1]. The global prevalence of the non-alcoholic fatty liver disease (NAFLD) affects about 1 billion people worldwide [2] and patients with type 2 diabetes (T2DM) constitute the majority of cases [3]. NAFLD is the most rapidly increasing cause of liver-related mortality across the globe [3]. However, it is not the liver itself but CVD that is the leading cause of death in patients with NAFLD [4].
For the last 40 years, NAFLD was characterized as an excessive hepatic lipid accumulation associated with metabolic abnormalities in the absence of significant alcohol consumption and other known causes of liver disease [5, 6]. Because NAFLD has been increasingly associated with glucose and lipid metabolic abnormalities as well as cardiovascular risk that is why modification in the definition was proposed in early 2000s [7, 8]. Thus, the nomenclature changed from NAFLD to the metabolic-associated fatty liver disease (MAFLD) in 2020 [9] and there is increasing evidence proving its importance in multidisciplinary care [10, 11]. Since the diagnosis of MAFLD is relatively new and it differs from NAFLD as it requires the presence of the metabolic risk factors and does not require the exclusion of alcohol intake or the presence of other liver diseases, the clinical course of the disease in patients with MAFLD might be different from NAFLD.
It is important to note that both European and American guidelines recommend to screen for CVD in people with NAFLD [5, 12] and it was demonstrated recently that better prediction of the progression of atherosclerotic cardiovascular risk is obtained when the MAFLD (not NAFLD) definition is used [13, 14] Therefore, it is of paramount clinical importance to determine the factors associated with CVD in people with MAFLD because the CVD could be prevented if an efficient tool for early detection of the individuals at the highest risk was available.
Predicting CVD events within the next 10 years with the use of the traditional risk factors is commonly applied [15]. However, numerous studies have shown that the currently adopted 10-year risk calculators, including the 2013 American College of Cardiology/American Heart Association (ACC/AHA) Pooled Cohort Equations Risk Calculator [15], often overestimate the CVD events and in some cases, underestimate the risk [16–19], causing unnecessary prescriptions of drugs. Moreover, chronic CVD generate high socioeconomic cost, and hence it is a major public health task to find and manage people with risk factors before the onset of CVD, facilitating effective prevention strategies [20].
Machine learning (ML) is one method of artificial intelligence in which computers utilize statistical approaches to effectively learn from data without being explicitly programmed to tackle a specific task. A variety of ML techniques have been increasingly applied in the medical field, including for the prediction of ventilator-associated pneumonia in critical care patients [21], prolonged operative time in elective total shoulder arthroplasty [22], cancer-associated deep vein thrombosis [23], or the stroke risk in non-anticoagulated patients with and without atrial fibrillation [24]. In a recent study, Kakadiaris et al. showed that their ML Risk Calculator outperformed the ACC/AHA Risk Calculator, and proposed less drug therapies while missing fewer CVD events [25].
We applied ML to determine the MAFLD patients who are at high CVD risk, and to better define the underlying risk factors in a data-driven manner. To the best of our knowledge, there have been no studies performed to date that analyzed the associations between MAFLD and CVD risk using ML methods.
Methods
This single center, observational, study was performed in a cohort of MAFLD patients. Patients who had been previously diagnosed with fatty liver disease based on the liver ultrasonography were invited to participate in the study through the advertisement placed in the University Hospital in Zabrze and in the outpatient diabetology clinics and family doctor clinics in the Upper Silesia region in Poland. The eligibility criteria were simple, ie. patients at age ≥ 18 years who fulfilled diagnostic criteria of MAFLD. The only exclusion criteria was the lack of written informed consent for the participation in the study. We recorded demographic and clinical data (Table 1) and divided the patients in relation to the presence or absence of CVD. The presence of CVD was defined as one or more of the following: angiography-confirmed coronary artery disease; myocardial infarction; coronary bypass grafting (CABG); stroke; carotid stenosis of at least 50% in diameter; and/or angiography-confirmed, clinically-significant, lower extremities artery stenosis (peripheral artery disease). Every patient signed an informed consent agreement for participation in the study. The study protocol obtained the approval of the Ethics Committee by the Medical University of Silesia (KNW/0022/KB1/38/I/17).
Table 1.
Patient characteristics
| Parameter | Patients without CVD (n = 144) | Patients with CVD (n = 47) | p-value |
|---|---|---|---|
| Biochemical parameters | |||
| ALT [U/l] | 47.92 ± 38.60 (32.75) | 32.15 ± 15.44 (31.00) | 0.0330 |
| AST [U/l] | 38.40 ± 33.93 (28.10) | 28.83 ± 11.35 (25.80) | 0.1342 |
| eGFR [ml/min/1.73m2] | 88.98 ± 18.52 (90.86) | 76.31 ± 17.92 (78.08) | < 0.0001 |
| HbA1c [%] | 6.70 ± 1.73 (6.10) | 7.30 ± 1.76 (6.85) | 0.0025 |
| HDL-C[mmol/l] | 1.33 ± 0.57 (1.23) | 1.25 ± 0.39 (1.19) | 0.4144 |
| HOMA-IR | 7.58 ± 6.79 (5.80) | 6.94 ± 5.59 (5.89) | 0.7293 |
| TG [mmol/l] | 2.13 ± 1.95 (1.66) | 2.90 ± 3.05 (1.95) | 0.1220 |
| Total cholesterol [mmol/l] | 5.13 ± 1.57 (4.80) | 4.92 ± 1.98 (4.60) | 0.0839 |
| Demographical parameters | |||
| Age [years] | 56.03 ± 12.15 (57.00) | 65.68 ± 6.37 (66.00) | < 0.0001 |
| Gender (% of male) | 52.78 | 57.45 | 0.5771 |
| Clinical parameters | |||
| ACEi or ARB (% of yes) | 49.31 | 65.96 | 0.0469 |
| Active smoker (% of yes) | 14.58 | 17.02 | 0.6859 |
| Betablocker (% of yes) | 36.81 | 65.96 | 0.0005 |
| BMI [kg/m2] | 33.74 ± 4.83 (33.39) | 32.50 ± 4.83 (31.28) | 0.0415 |
| Diastolic BP [mmHg] | 81.83 ± 9.97 (80.00) | 78.91 ± 9.14 (80.00) | 0.0314 |
| T2DM (% of yes) | 58.33 | 85.11 | 0.0008 |
| Duration of T2DM [years] | 3.76 ± 5.60 (0.50) | 8.90 ± 7.69 (10.00) | < 0.0001 |
| Hypercholesterolemia (% of yes) | 27.08 | 70.21 | < 0.0001 |
| Hypertriglyceridemia (% of yes) | 7.64 | 10.64 | 0.5193 |
| Heart rate [beats/min] | 78.15 ± 15.84 (75.00) | 74.04 ± 8.96 (72.00) | 0.1940 |
| Hypertension (% of yes) | 70.14 | 93.62 | 0.0011 |
| Obesity (% of yes) | 78.47 | 65.96 | 0.0837 |
| Overweight (% of yes) | 18.75 | 31.91 | 0.0585 |
| Systolic BP [mmHg] | 132.70 ± 13.74 (130.00) | 133.60 ± 10.67 (132.00) | 0.5461 |
| WHR | 0.97 ± 0.10 (0.97) | 0.99 ± 0.09 (0.99) | 0.3318 |
| Carotid ultrasound parameters | |||
| Diameter of CCA L | 7.37 ± 0.85 (7.30) | 7.61 ± 1.40 (7.70) | 0.0192 |
| Diameter of CCA R | 7.71 ± 0.95 (7.70) | 7.92 ± 0.95 (7.90) | 0.2446 |
| IMT max CCA L | 0.83 ± 0.18 (0.83) | 0.85 ± 0.15 (0.84) | 0.4248 |
| IMT max CCA R | 0.82 ± 0.18 (0.80) | 0.85 ± 0.17 (0.81) | 0.2159 |
| Median IMT CCA R | 0.68 ± 0.16 (0.66) | 0.68 ± 0.15 (0.68) | 0.8730 |
| Median IMT CCA L | 0.68 ± 0.16 (0.68) | 0.71 ± 0.13 (0.69) | 0.1660 |
| Plaque area L | 0.04 ± 0.07 (0.00) | 0.16 ± 0.29 (0.08) | < 0.0001 |
| Plaque area R | 0.06 ± 0.23 (0.00) | 0.15 ± 0.22 (0.08) | < 0.0001 |
| Plaque score L | 0.76 ± 1.33 (0.00) | 2.24 ± 1.92 (2.00) | < 0.0001 |
| Plaque score R | 0.89 ± 1.47 (0.00) | 2.23 ± 1.86 (1.90) | < 0.0001 |
| Arterial stiffness-related parameters | |||
| cfPWV | 9.08 ± 2.03 (8.85) | 10.30 ± 2.42 (10.10) | < 0.0001 |
| crPWV | 9.80 ± 1.55 (9.84) | 9.73 ± 1.46 (9.60) | 0.4637 |
| Liver elastography parameters | |||
| Liver steatosis CAP [dB/m] | 316.30 ± 51.50 (323.00) | 315.20 ± 43.76 (311.00) | 0.4740 |
| Steatosis stage (S0-S3) | 2.36 ± 0.87 (3.00) | 2.28 ± 0.77 (2.00) | 0.2729 |
For each parameter (if applicable), we report its mean ± standard deviation, together with the median (in parentheses)
CVD cardiovascular disease, ALT alanine aminotransferase, AST aspartate aminotransferase, BP blood pressure, eGFR estimated glomerular filtration rate, HbA1c hemoglobin A1c, HOMA-IR homeostasis model assessment of insulin resistance, HDL-C high density lipoprotein cholesterol, TG triglycerides, ACEi angiotensin converting enzyme inhibitor, ARB angiotensin receptor blocker, MALFD metabolic-associated fatty liver disease, BMI body mass index, , CCA L left common carotid artery, CCA R right common carotid artery, IMT intima -media thickness, cfPWV carotid- femoral pulse wave velocity, crPWV carotid-radial pulse wave velocity, CAP controlled attenuation parameter, T2DM type 2 diabetes mellitus.
The p-values were obtained using the Mann–Whitney test or the Chi-square test, depending on the data characteristics
Anthropometric, demographic and clinical parameters
Anthropometric parameters, including height (meters) and weight (kilograms), as well as waist and hip circumference were measured (meters) by standard methods, and the body mass index (BMI) was calculated as weight/height2 (kg/m2). Additionally, the waist-to-hip ratio (WHR) was obtained. The obesity was diagnosed when BMI ≥ 30 whereas the overweight was diagnosed when BMI ≥ 25 but < 30. The patients were considered to have T2DM based on a known history of this disease. Blood pressure was measured three times after 5 min of rest in a sitting position, at least 2 min apart, and the mean blood pressure of the three measurements was calculated. Arterial hypertension was defined as a systolic blood pressure ≥ 140 mmHg and/or a diastolic blood pressure ≥ 90 mmHg or previous treatment with antihypertensive medications. Hypercholesterolemia was recognized when a patient had this diagnosis present in the documented medical history and/or there was newly recognized plasma high density lipoprotein cholesterol (HDL-C) < 1.0 mmol/l for men and < 1.3 mmol/l for women and/or patient was on statin therapy. Hypertriglyceridemia was recognized when a patient had this diagnosis present in the documented medical history and/or there was newly recognized plasma triglyceride ≥ 1.7 mmol/l and/or patient was on fibrate therapy. The history of all concomitant diseases was obtained from the patient and confirmed on the basis of documented medical data. No self-reported diseases without medically confirmed diagnosis were recorded.
MAFLD diagnostic criteria
The patients were diagnosed with MAFLD [26] if there was an evidence of steatosis acquired by the hepatic ultrasonography and presence of one of the following criteria: T2DM, overweight or obesity defined as BMI greater than or equal to 25 kg/m2 or at least two metabolic risk abnormalities, i.e., waist circumference ≥ 102 cm in men and ≥ 88 cm in women, blood pressure ≥ 130/85 mmHg or specific drug treatment, prediabetes, plasma triglycerides ≥ 1.7 mmol/l or specific drug treatment, plasma HDL-C < 1.0 mmol/l for men and < 1.3 mmol/l for women or specific drug treatment, Homeostatic Model Assessment of Insulin Resistance (HOMA- IR) ≥ 2.5, serum C-reactive protein level > 2 mg/l.
Liver elastography with Fibroscan
Liver elastography was performed with the use of the Fibroscan 502TOUCH F611100049 device exploiting the XL 8 80,685 probe (2.5 Hz). The liver was tested after 6 h of fasting, and the test lasted from 5 to 10 min. In the patient lying in the dorsal position with the right arm extended, a gel-coated ultrasound probe was applied to the skin in the intercostal space above the right lobe of the liver. The time motion ultrasound image allows the operator to locate a fragment of the liver at least 6 cm thick and devoid of large vascular structures or ribs. The median and interquartile range (IQR) values of at least 10 successful liver stiffness measurements (LSM) and the controlled attenuation parameter (CAP), adequately defining fibrosis and steatosis, respectively, were calculated by the device. The results included the median and IQR of the CAP values (dB/m) and the median, IQR, IQR/median LSM (kPa), the success rate (i.e., the number of successful measurements/total number of attempts), the determination of the degree of steatosis (S0-S3) and liver fibrosis (F0-F4). The LSM classified as reliable are characterized by having all three of the following: ≥ 10 passed measurements, ≥ 60% success rate, and IQR/ median < 0.30.
Carotid ultrasound measurement
The ultrasound examination of the carotid arteries was performed using a high-resolution Doppler ultrasound with double imaging and color coding of the flow (Color Doppler Duplex, CDD) exploiting the Esaote MyLab60 ultrasound equipment by the same certified neurologist. The examinations were done in the supine position, without any additional preparation, with a linear ultrasound head emitting an ultrasonic wave with a variable frequency of 4 MHz to 15 MHz. In the 2D presentation, the common carotid artery (CCA), the separation (bifurcation) of the common carotid artery into the internal carotid artery and the external and internal carotid artery (ICA), alongside the external carotid artery (ECA) were determined. Measurement of the intima-media complex (KIM) thickness and the assessment of atherosclerotic lesions in the carotid arteries were performed.
Arterial stiffness assessment
For these measurements, piezoelectric mechanical transducers in the cervical, femoral and radial areas were used (Complior, Alam Medical, France). The velocity of the carotid-femoral pulse wave (cfPWV) was used to assess the stiffness of the central artery and the velocity of the carotid-radial pulse wave (crPWV) was used to assess the stiffness of the peripheral arteries. With the Seca mod. 207 height meter, the right carotid-femoral and carotid-radial distances were measured. Blood pressure was measured in the supine position after at least 5 min of rest with the Microlife BP A1 sphygmomanometer immediately prior to the PWV assessment, and the mean of the three measurements on both arms was calculated and recorded. Derivative variables such as the central blood pressure, central pulse pressure and the gain index were analyzed, calculated by the integrated software on the basis of the carotid pulse waveform.
Biochemical methods
Hemoglobin A1c (HbA1c) was determined using a high-performance liquid chromatography (HPLC) method, and the results were expressed in the National Glycohemoglobin Standardization Program/Diabetes Control and Complications trial units [27]. Cholesterol and triglycerides were measured using the enzymatic methods, with the HDL-C measured after precipitation of the very low-density lipoprotein cholesterol (VLDL-C). The concentration of the low density lipoprotein cholesterol (LDL-C) was calculated using the Friedewald formula [28]. Serum creatinine was measured by means of the Jaffe’s method. The estimated glomerular filtration rate (eGFR) per 1.73 m2 was calculated according to the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) formula [29]. Blood cell morphology to obtain the platelet count (PLT) was determined using the fluorescent flow cytometry with the Sysmex XN-1000 (Sysmex) hematology analyzer [30]. Serum C reactive protein concentration were measured by a latex particle-enhanced turbidimetric immunoassay [31]. Alanine and aspartate aminotransferase activities in serum were assayed by the kinetic method according to the IFCC reference procedure. Analyzes of serum C reactive protein, alanine and aspartate aminotransferase were carried out on the Cobas 6000 analyzer, c 501 module (Roche). Fasting glucose was assessed using the enzymatic method with the Cobas 6000 hexokinase analyzer, c501 module (Roche). Insulin concentration was measured by electrochemiluminescence using the Cobas 6000 analyzer (module E601) [32].
Identifying high-risk patients using machine learning
To automatically identify the patients with a high risk of overt CVD, we investigated biochemical (8 parameters), demographical [2], clinical [17], carotid ultrasound [10], arterial stiffness-related [2] and steatosis stage in elastography [3] parameters (42 parameters in total)—the parameters are summarized in Table 1. To handle the missing data, we imputed the mean values for each parameter—the percentage of patients for whom the parameter was missing never exceeded 5% of all patients (mean: 0.68%). Afterwards, the parameters underwent univariate feature ranking. First, we examined whether each feature (predictor variable) is independent of a response variable (low- vs. high-risk patient) by using individual chi-square tests. Then, the parameters were ranked using the p-values of the chi-square test statistics—here, the importance of a feature is quantified as , therefore a large score indicates that the corresponding predictor is important. The subsets of the most discriminative predictors were selected, and they were utilized to fitted the multiple logistic regression classifiers. Additionally, we fitted the classifiers over the principal components (PCs) extracted using PCA followed by the parallel analysis to determine the significant PCs [33]. For each model, we investigated the relationship between the model’s ability to correctly classify low- and high-risk patients using the ROC curve analysis, and we calculated the area under the ROC curve (AUC) as the summary metric to quantify the diagnostic ability of the corresponding classifier. To obtain the optimal cut-point value from each ROC curve, we exploited the (i) Index of Union (IoU), (ii) the closest to (0, 1) criteria (referred to as the Distance technique) and (iii) the Youden index methods [34]. For the selected cut-point values, we reported not only sensitivity and specificity of the corresponding classifier, but we also calculated its positive and negative predictive value (PPV and NPV, respectively), and the percentage of correctly classified low- and high-risk patients. The clinical utility of the developed ML models was investigated in the decision curve analysis. GraphPad Prism 9.4.1 was used for principal component, parallel analysis and other statistical processing, whereas MATLAB R2021b was exploited for feature selection (the fscchi2 function).
Results
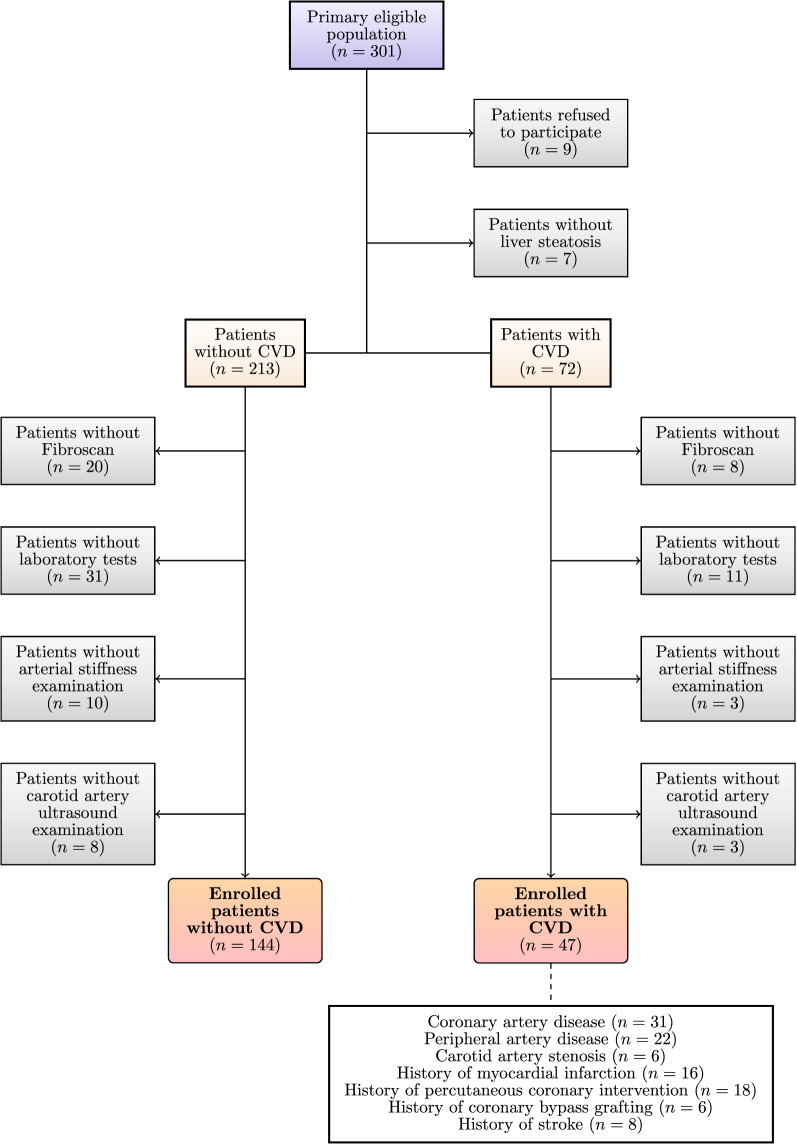
There were 301 potentially eligible patients identified, and from these, only 191 individuals (mean age 58, SD 12, median: 60, IQR: 15 years; 46% female) fulfilled the inclusion/exclusion criteria for the study (Fig. 1). The patient characteristics are gathered in Table 1.
Fig. 1.
Patient flow. Out of 301 potentially eligible patients, 191 patients fulfilled the inclusion criteria (144 without CVD and 47 with CVD). CVD – cardiovascular disease
In feature selection, we focused on Top-5, Top-10, and Top-15 most important predictors (with the 5, 10, and 15 highest importance scores, respectively) which are summarized in Table 2. The most important 5 clinical variables included hypercholesterolemia, the plaque score of the left internal carotid artery, plaque score of the right internal artery, duration of T2DM and plaque area of the right internal carotid artery, which were all positively associated with overt CVD.
Table 2.
The 15 most discriminative features (with the largest importance scores)
| Parameter | Importance score | Spearman’s (r) | p-value |
|---|---|---|---|
| Hypercholesterolemia | 15.96 | 0.38 | < 0.0001 |
| Plaque score L | 12.68 | 0.41 | < 0.0001 |
| Plaque score R | 10.94 | 0.38 | < 0.0001 |
| Duration of T2DM | 10.65 | 0.32 | < 0.0001 |
| Plaque area R | 10.00 | 0.34 | < 0.0001 |
| Age | 8.60 | 0.37 | < 0.0001 |
| Plaque area L | 8.36 | 0.35 | < 0.0001 |
| Betabloker | 7.66 | 0.25 | 0.0004 |
| T2DM | 7.08 | 0.24 | 0.0008 |
| Hypertension | 6.83 | 0.24 | 0.0010 |
| cfPWV | 6.64 | 0.28 | < 0.0001 |
| ALT | 4.69 | –0.15 | 0.0329 |
| eGFR | 3.51 | –0.28 | < 0.0001 |
| HbA1c | 3.19 | 0.22 | 0.0025 |
| Obesity | 3.17 | –0.15 | 0.0421 |
We report the two-tailed p-values for nonparametric Spearman correlation to verify if the correlation is due to random sampling (if p < 0.05 this hypothesis can be rejected)
T2DM type 2 diabetes mellitus, cfPWV carotid-femoral pulse wave velocity, ALT alanine aminotransferase, eGFR estimated glomerular filtration rate, HbA1c hemoglobin A1c
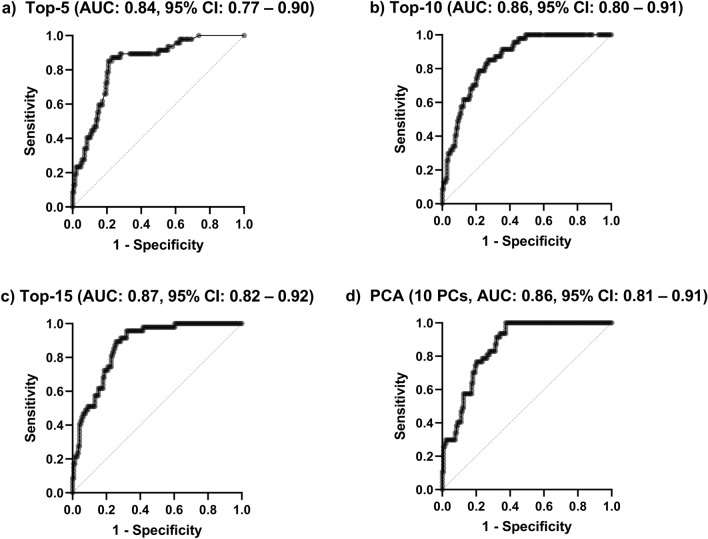
We investigated the performance of the multiple regression classifier fitted to ten PCs extracted by PCA, as ten PCs were found significant in the parallel analysis. The ROC analysis (Fig. 2) of the models fitted over the selected parameters, alongside the extracted PCs revealed that the highest AUC amounted to 0.87 (95% confidence interval [CI]: 0.82–0.92, p < 0.0001) for the model fitted to 15 most discriminative features (Top-15), whereas the worst AUC was 0.84 (95% CI 0.77–0.90, p < 0.0001) for the classifier operating on 5 features with the highest importance scores (Top-5). The multiple regression model fitted over 10 PCs resulted in AUC of 0.86 (95% CI 0.81–0.91, p < 0.0001)–utilizing 10 most important predictors led to the same AUC of 0.86 (95% CI 0.80–0.91, p < 0.0001). Once the optimal cut-point values have been elaborated for all models, the results were further analyzed—the performance (specificity, sensitivity, percentage of all correctly classified [CC] patients, percentage of CC low- and high-risk patients reported separately, positive and negative predictive values) of the multiple regression classifiers for the cut-point values determined using the i) IoU, ii) Distance and iii) Youden methods are reported in Table 3. The best machine learning model, as quantified by CC All and operating over five most discriminative features correctly identified 114/144 (79.17%) low-risk patients and 40/47 (85.11%) high-risk patients (Top-5 with the cut-point selected using the IoU and Distance methods).
Fig. 2.
The ROC curves obtained using the multiple logistic regression classifiers over the a Top-5, b Top-10, and c Top-15 most discriminative patient parameters (according to their important scores), and over d 10 principal components (PCs). We report the area under the ROC curve (AUC) for each classifier
Table 3.
The performance of the multiple regression classifiers
| Cut-point | Top-5 | Top-10 | Top-15 | PCA (10 PCs) | |||||
|---|---|---|---|---|---|---|---|---|---|
| i, ii | iii | i, iii | ii | i | ii | iii | i, ii | iii | |
| Specificity | 0.79 | 0.77 | 0.73 | 0.78 | 0.75 | 0.74 | 0.68 | 0.80 | 0.63 |
| Sensitivity | 0.85 | 0.87 | 0.85 | 0.79 | 0.87 | 0.89 | 0.96 | 0.77 | 1.00 |
| CC low-risk [%] | 79.17 | 77.08 | 72.92 | 78.47 | 75.00 | 74.31 | 68.06 | 79.86 | 62.50 |
| CC high-risk [%] | 85.11 | 87.23 | 85.11 | 78.72 | 87.23 | 89.36 | 95.74 | 76.60 | 100.0 |
| CC All [%] | 80.63 | 79.58 | 75.92 | 78.53 | 78.01 | 78.01 | 74.87 | 79.06 | 71.73 |
| PPV [%] | 57.14 | 55.41 | 50.63 | 54.41 | 53.25 | 53.16 | 49.45 | 55.38 | 46.53 |
| NPV [%] | 94.21 | 94.87 | 93.75 | 91.87 | 94.74 | 95.54 | 98.00 | 91.27 | 100.0 |
The best results are boldfaced, whereas the second best are underlined
CC correctly classified, PPV positive predictive value, NPV negative predictive value
In Fig. 3, the clinical utility of the three best-performing ML models (according to all quality metrics gathered in Table 3) was investigated. In general, all classifiers had significantly better clinical utility (above the probability threshold of 10%) in terms of net benefit than the two alternative treatment strategies, ie. treat all or none. The logistic regression model operating on top 5 most discriminative features outperformed two other ones (exploiting 10 principal components) above the probability threshold of 25%.
Fig. 3.
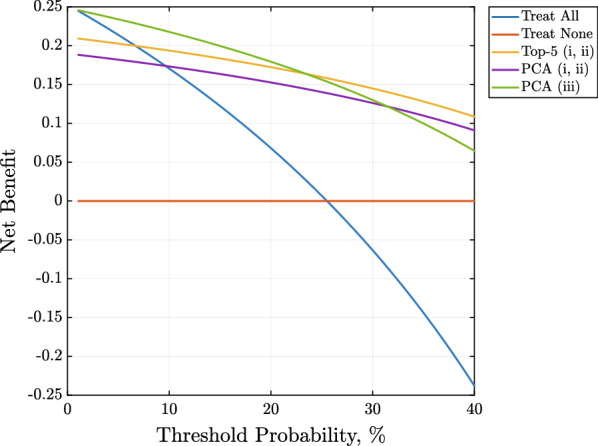
Decision curve analysis showing clinical utility of using the three best-performing ML models according to all classification performance metrics. One top-performing logistic regression classifier operated on top-5 most discriminative features with the optimal cut-point value selected using the i) Index of Union (IoU) and ii) the closest to (0, 1) criteria (yellow line), whereas two operated on 10 principal components with the optimal cut-point value selected using i) Index of Union (IoU) and ii) the closest to (0, 1) criteria (violet line) method, and using iii) the Youden index method (green line)
Discussion
In this study our principal findings are as follows: (i) we determined the most discriminative patient's parameters which can be used to build a ML model for identifying MAFLD patients with high CVD risk, (ii) we showed that using five interpretable and easy-to-obtain clinical parameters (including hypercholesterolemia, the plaque score of the left internal carotid artery, plaque score of the right internal artery, duration of T2DM and plaque area of the right internal carotid artery) is enough to elaborate well-generalizing logistic regression classifiers to the above-mentioned task; and (iii) we demonstrated better clinical utility of the developed ML models when compared to the “treat all” and “no treatment” strategies.
Shortly after the new definition of the fatty liver has emerged, it is still unknown how it will influence the clinical practice. Indeed, this does not represent a simple change in the nomenclature: differently from NAFLD, MAFLD can be recognized in patients who present with fatty liver and dysmetabolism, even when alcohol intake is reported yet not in lean ones without metabolic comorbidities [35]. It has been shown that NAFLD contributes to subclinical atherosclerosis [36–38] and that there is an independent association of NAFLD and higher prevalence of CVD in patients with DM [39]. However, it is still unclear if it is a direct effect of NAFLD per se or is it just due to the cardiometabolic risk factors shared between NAFLD and CVD [4]. It has been proved recently that presence of metabolic dysfunction, rather than alcohol consumption, may be the element which could be responsible for the superiority of MAFLD over NAFLD for discriminating worsening of atherosclerotic CVD risk in patients with fatty liver [13]. That is why it seems justified to look closer at risk factors of CVD in patients with MALFD.
In this study, 25% of relatively young patients with the Fibroscan-confirmed MAFLD presented with CVD. We have carefully reviewed the patients’ medical documentation and, surprisingly, none of the patients presented with a history of heart failure which accounts for about 2% of world adult population [40, 41]. It is, however, possible since – as the epidemiological data suggest – there is still a high number of unrecognized heart insufficiency cases [42, 43].
The feature analysis indicated that simple to obtain in everyday clinical practice parameters, such as carotid ultrasound, and clinical and biochemical ones can be discriminative in patients with overt CVD. This is very important from the practical point of view because before overt CVD occurs there is a long period of the silent disease presence and knowing the patient's parameters which could be potentially associated with overt CVD gives the clinicians a chance to improve the prevention and screening methods of CVD.
The ML models operating on such features achieved high predictive performance with the AUC values ranging from 0.84 to 0.87 (Fig. 2). Similarly, in a recent study, Oh et al. [44] analyzed the Korean national epidemiological data and demonstrated that the proposed classifiers can achieve a comparable performance (with AUC exceeding 0.85). Oh et al. determined that the most significant risk factors of CVD were age, gender, and hypertension, and they identified the positive correlation with hypertension, age, and BMI, and the negative correlation with the gender, alcohol consumption and monthly income [44]. Another study by Alaa et al. revealed that there are easy to collect, non-laboratory predictors of CVD, such as self-reported health ratings and usual walking pace which could be used in practice [45].
In our study, the top 5 most discriminative features (hypercholesterolemia, the plaque score of the left internal carotid artery, plaque score of the right internal artery, duration of diabetes and plaque area of the right internal carotid artery; are positively associated with overt CVD) could correctly identify 85.11% patients who present with CVD. While the highest score was seen for traditional risk factors, such as hypercholesterolemia and the duration of diabetes, there were also plaque related risk factors (both the plaque score and the plaque area) when taking into account top 5 most discriminative CVD features. The plaque score has been indeed identified as a factor associated with the long-term coronary artery disease risk in middle-aged asymptomatic individuals [46, 47]. Hypercholesterolemia, contrary to the duration time of diabetes, is a modifiable traditional risk factor which stress the necessity to treat this metabolic abnormalities underlined in both cardiology as well as diabetology guidelines for the management of patients with diabetes [48, 49].
When looking closer at the top 10 features which could discriminate the vulnerable patients, these are again the traditional risk factors—like being diagnosed with T2DM and hypertension—but also the use of betablocker, with all the features being positively associated with CVD. An interesting parameter which was among the top 15 ones associated with CVD is the parameter related to the arterial stiffness which is already recognized as the one which improves cardiovascular event prediction [50], and this one was also positively associated with CVD. On the other hand, other top 15 parameters (including ALT, eGFR and obesity) were negatively associated with overt CVD. Since it is understandable in relation to the kidney function expressed as eGFR which is a known risk factor of CVD, the negative association of ALT and obesity is surprising. The explanation of the negative association of obesity with CVD may be that nowadays there is a high emphasis on a healthy lifestyle, and patients who participated in our study were interested in their health since they answered the advertisement. Thus, it is also possible that they have already lost weight just before the participation in the study.
The results obtained for PCA indicated that the best-generalizing multiple regression classifiers were elaborated using interpretable features, and the models operating on the five most important features outperformed all other classifiers (exploiting more features and PCs) for the selected cut-point values, and correctly classified 80.63% of all patients (Table 3). This observation was further manifested while analyzing the clinical utility of the three best ML models – for the probability threshold of 25%, a logistic regression classifier operating on 5 patient parameters outperformed two other models, both exploiting 10 PCs which are more challenging to interpret in clinical practice. Such models directly operating on patient parameters and uncovering their interrelationships with the CVD risk are not only easier to interpret, but also are they less likely to overfit to our relatively small patient cohort. Finally, the results show that the ROC curve analysis may effectively lead to the classifiers with higher specificity or sensitivity, depending on the clinical scenario.
Most of the studies targeting the prediction of the CVD risk focus on the self-reported patient parameters which are not necessarily proved by medical documentation, hence may lead to biased outcomes. In our study, we have addressed this issue, and we analyzed a very well-defined population of patients whose concomitant diseases were medically documented. We used ML, which has been increasingly used to assess the risk of adverse outcomes in chronic disease states, outperforming simple clinical risk assessments [46, 47]. Most importantly, we are unaware of any studies to date which has assessed the risk factors in patients with MAFLD, let alone with the use of novel approaches such as ML.
Limitations
We are aware that there are important limitations of our study, which was a proof of concept for a wider program of work. This would include larger cohorts and further external validation, as well as prospective observations for all of them. Also, the patients were not asked whether they had lost their weight before participating in the study, which could explain the negative association of obesity with CVD. An important aspect of cardiovascular pharmacologic management is antiplatelet treatment. However, we were unable to gather reliable information related to this type of treatment in patients without CVD, hence we excluded this parameter from the analysis due to a large amount of missing data. Moreover we included patients with at least 50% of carotid artery stenosis qualifying them as those with overt CVD since 50% is a cut point of stroke related to large artery atherosclerosis [51–53]. In this context, one should notice that the plaque score has been identified as one of the top 5 risk factors related to CVD so this information potentially could be biased. Finally, exploiting the recent deep learning advances which established the state of the art in various medical data analysis tasks could help us further improve the classification performance of the CVD patients, but it would also require focusing on the interpretability of such large-capacity learners, to make their deployment in clinical setting much easier [48, 49].
Conclusion
The use of a ML approach demonstrated high performance in identifying MAFLD patients with high CVD risk based on the subset of the most discriminative, interpretable and easy-to-obtain patient's parameters. Our approach has the potential to facilitate timely diagnoses and management of prevalent CVD risk in patients who present with MAFLD in routine clinical practice.
Acknowledgements
The authors thank Agata M. Wijata for providing a MATLAB implementation of the Decision Curve Analysis.
Abbreviations
- ACC
American College of Cardiology
- ACEi
Angiotensin converting enzyme inhibitor
- AHA
American Heart Association
- ALT
Alanine aminotransferase
- ARB
Angiotensin receptor blocker
- AST
Aspartate aminotransferase
- AUC
Area under the receiver operating characteristic curve
- BMI
Body mass index
- BP
blood pressure
- CABG
Coronary bypass grafting
- CAP
Controlled attenuation parameter
- CC
Correctly classified
- CCA
Common carotid artery
- CDD
Color Doppler Duplex
- cfPWV
Carotid-femoral pulse wave velocity
- CI
Confidence interval
- CKD-EPI
Chronic Kidney Disease Epidemiology Collaboration
- crPWV
Carotid-radial pulse wave velocity
- CVD
Cardiovascular disease
- ECA
External carotid artery
- eGFR
Estimated glomerular filtration rate
- HbA1c
Hemoglobin A1c
- HDL-C
High-density lipoprotein cholesterol
- HOMA-IR
Homeostatic Model Assessment of Insulin Resistance
- HPLC
High-performance liquid chromatography
- ICA
Internal carotid artery
- IoU
Index of Union
- IQR
Interquartile range
- IMT
Intima-media thickness
- LSM
Liver stiffness measurement
- MAFLD
Metabolic - associated fatty liver disease
- ML
Machine learning
- NAFLD
Non-alcoholic fatty liver disease
- NPV
Negative predictive value
- PCA
Principal component analysis
- PCs
Principal components
- PLT
Platelet count
- PPV
Positive predictive value
- ROC
Receiver operating characteristic
- T2DM
Type 2 diabetes mellitus
- TG
Triglycerides
- VLDL-C
Very low-density lipoprotein cholesterol
- WHR
Waist-to-hip ratio
Author contributions
KD, KN, HK, JG, GL—substantial contribution to the conception and design of the work; KD, KN, HK, MH, AO, AT, WB—collected the data and performed patients examination; JN—designed, implemented and verified the machine learning algorithms; JN—performed the computational experiments; JN—performed the data analysis; KD, KN, HK, JN—prepared tables and figures; KD, KN, JN—drafted the work; JG, GL—substantially revised the work. All of the authors approved the submitted version of the paper. All authors read and approved the final manuscript.
Funding
Statutory Work of Medical University of Silesia (KNW-1-007/N/8/K and KNW-1-175-K/9/K). JN was supported by the Silesian University of Technology funds through the grant for maintaining and developing research potential.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
Every patient signed an informed consent agreement for participation in the study. The study protocol obtained the approval of the Ethics Committee by the Medical University of Silesia (KNW/0022/KB1/38/I/17).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Estes C, Anstee QM, Arias-Loste MT, et al. Modeling NAFLD disease burden in China, France, Germany, Italy, Japan, Spain, United Kingdom, and United States for the period 2016–2030. J Hepatol. 2018;69(4):896–904. 10.1016/j.jhep.2018.05.036. [DOI] [PubMed]
- 2.Younossi Z, Anstee QM, Marietti M, Hardy T, Henry L, Eslam M, et al. Global burden of NAFLD and NASH: trends, predictions, risk factors and prevention. Nat Rev Gastroenterol Hepatol. 2018;15(1):11–20. doi: 10.1038/nrgastro.2017.109. [DOI] [PubMed] [Google Scholar]
- 3.Chan KE, Koh TJL, Tang ASP, Quek J, Yong JN, Tay P, et al. Global prevalence and clinical characteristics of metabolic-associated fatty liver disease: a meta-analysis and systematic review of 10 739 607 individuals. J Clin Endocrinol Metab. 2022;107(9):2691–2700. doi: 10.1210/clinem/dgac321. [DOI] [PubMed] [Google Scholar]
- 4.Targher G, Byrne CD, Tilg H. NAFLD and increased risk of cardiovascular disease: Clinical associations, pathophysiological mechanisms and pharmacological implications. Gut. 2020;69:1691–705. doi: 10.1136/gutjnl-2020-320622. [DOI] [PubMed] [Google Scholar]
- 5.Marchesini G, Day CP, Dufour JF, Canbay A, Nobili V, Ratziu V, et al. EASL-EASD-EASO clinical practice guidelines for the management of non-alcoholic fatty liver disease. J Hepatol. 2016;64(6):1388–1402. doi: 10.1016/j.jhep.2015.11.004. [DOI] [PubMed] [Google Scholar]
- 6.Ludwig J, Viggiano TR, McGill DB, Ott BJ. Nonalcoholic steatohepatitis. Mayo clinic experiences with a hitherto unnamed disease. Mayo Clin Proc. 1980;55(7):434–8. [PubMed] [Google Scholar]
- 7.Neuschwander-Tetri BA, Caldwell SH. Nonalcoholic steatohepatitis: summary of an AASLD single topic conference. Hepatology. 2003 doi: 10.1002/hep.510380242. [DOI] [PubMed] [Google Scholar]
- 8.Byrne CD, Targher G. NAFLD: a multisystem disease. J Hepatol. 2015;62(1):S47–64. doi: 10.1016/j.jhep.2014.12.012. [DOI] [PubMed] [Google Scholar]
- 9.Eslam M, Sanyal AJ, George J, Sanyal A, Neuschwander-Tetri B, Tiribelli C, et al. MAFLD: a consensus-driven proposed nomenclature for metabolic associated fatty liver disease. Gastroenterology. 2020;158(7):1999–2014.e1. doi: 10.1053/j.gastro.2019.11.312. [DOI] [PubMed] [Google Scholar]
- 10.Méndez-Sánchez N, Bugianesi E, Gish RG, Lammert F, Tilg H, Nguyen MH, et al. Global multi-stakeholder endorsement of the MAFLD definition. Lancet Gastroenterol Hepatol. 2022;7(5):388–90. doi: 10.1016/S2468-1253(22)00062-0. [DOI] [PubMed] [Google Scholar]
- 11.Eslam M, Ahmed A, Després J-P, Jha V, Halford JCG, Wei Chieh JT, et al. Incorporating fatty liver disease in multidisciplinary care and novel clinical trial designs for patients with metabolic diseases. Lancet Gastroenterol Hepatol. 2021;6(9):743–53. doi: 10.1016/S2468-1253(21)00132-1. [DOI] [PubMed] [Google Scholar]
- 12.Chalasani N, Younossi Z, Lavine JE, Charlton M, Cusi K, Rinella M, et al. The diagnosis and management of nonalcoholic fatty liver disease: practice guidance from the American Association For The Study Of Liver Diseases. Hepatology. 2017 doi: 10.1002/hep.29367. [DOI] [PubMed] [Google Scholar]
- 13.Tsutsumi T, Eslam M, Kawaguchi T, Yamamura S, Kawaguchi A, Nakano D, et al. MAFLD better predicts the progression of atherosclerotic cardiovascular risk than NAFLD: generalized estimating equation approach. Hepatol Res. 2021;51(11):1115–1128. doi: 10.1111/hepr.13685. [DOI] [PubMed] [Google Scholar]
- 14.Alharthi J, Gastaldelli A, Cua IH, Ghazinian H, Eslam M. Metabolic dysfunction-associated fatty liver disease: a year in review. Curr Opin Gastroenterol. 2022;38(3):251–260. doi: 10.1097/MOG.0000000000000823. [DOI] [PubMed] [Google Scholar]
- 15.Goff DCJ, Lloyd-Jones DM, Bennett G, Coady S, D’Agostino RBS, Gibbons R, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63(25):2935–59. doi: 10.1016/j.jacc.2013.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ridker PM, Cook NR. Statins: new American guidelines for prevention of cardiovascular disease. Lancet (London, England) 2013;382(9907):1762–1765. doi: 10.1016/S0140-6736(13)62388-0. [DOI] [PubMed] [Google Scholar]
- 17.Muntner P, Colantonio LD, Cushman M, Goff DCJ, Howard G, Howard VJ, et al. Validation of the atherosclerotic cardiovascular disease pooled cohort risk equations. JAMA. 2014;311(14):1406–1415. doi: 10.1001/jama.2014.2630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kavousi M, Leening MJG, Nanchen D, Greenland P, Graham IM, Steyerberg EW, et al. Comparison of application of the ACC/AHA guidelines, adult treatment panel III guidelines, and European society of cardiology guidelines for cardiovascular disease prevention in a European cohort. JAMA. 2014;311(14):1416–1423. doi: 10.1001/jama.2014.2632. [DOI] [PubMed] [Google Scholar]
- 19.DeFilippis AP, Young R, McEvoy JW, Michos ED, Sandfort V, Kronmal RA, et al. Risk score overestimation: the impact of individual cardiovascular risk factors and preventive therapies on the performance of the American Heart Association-American College of Cardiology-Atherosclerotic Cardiovascular disease risk score in a modern mul. Eur Heart J. 2017;38(8):598–608. doi: 10.1093/eurheartj/ehw301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gheorghe A, Griffiths U, Murphy A, Legido-Quigley H, Lamptey P, Perel P. The economic burden of cardiovascular disease and hypertension in low- and middle-income countries: a systematic review. BMC Public Health. 2018;18(1):975. doi: 10.1186/s12889-018-5806-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Liang Y, Zhu C, Tian C, Lin Q, Li Z, Li Z, et al. Early prediction of ventilator-associated pneumonia in critical care patients: a machine learning model. BMC Pulm Med. 2022;22(1):250. doi: 10.1186/s12890-022-02031-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lopez CD, Constant M, Anderson MJJ, Confino JE, Lanham NS, Jobin CM. Using machine learning methods to predict prolonged operative time in elective total shoulder arthroplasty. Semin Arthroplast JSES. 2022;32(3):452–61. doi: 10.1053/j.sart.2022.01.003. [DOI] [Google Scholar]
- 23.Jin S, Qin D, Liang B-S, Zhang L-C, Wei X-X, Wang Y-J, et al. Machine learning predicts cancer-associated deep vein thrombosis using clinically available variables. Int J Med Inform. 2022;161:104733. doi: 10.1016/j.ijmedinf.2022.104733. [DOI] [PubMed] [Google Scholar]
- 24.Lip GYH, Tran G, Genaidy A, Marroquin P, Estes C, Landsheft J. Improving dynamic stroke risk prediction in non-anticoagulated patients with and without atrial fibrillation: comparing common clinical risk scores and machine learning algorithms. Eur Hear journal Qual care Clin outcomes. 2022;8(5):548–556. doi: 10.1093/ehjqcco/qcab037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kakadiaris IA, Vrigkas M, Yen AA, Kuznetsova T, Budoff M, Naghavi M. Machine learning outperforms ACC / AHA CVD risk calculator in MESA. J Am Heart Assoc. 2018;7(22):e009476. doi: 10.1161/JAHA.118.009476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Eslam M, Newsome PN, Sarin SK, Anstee QM, Targher G, Romero-Gomez M, et al. A new definition for metabolic dysfunction-associated fatty liver disease: an international expert consensus statement. J Hepatol. 2020;73:202–9. doi: 10.1016/j.jhep.2020.03.039. [DOI] [PubMed] [Google Scholar]
- 27.Little RR. Glycated hemoglobin standardization–national glycohemoglobin standardization program (NGSP) perspective. Clin Chem Lab Med. 2003;41(9):1191–1198. doi: 10.1515/CCLM.2003.183. [DOI] [PubMed] [Google Scholar]
- 28.Nauck M, Warnick GR, Rifai N. Methods for measurement of LDL-cholesterol: a critical assessment of direct measurement by homogeneous assays versus calculation. Clin Chem. 2002;48(2):236–254. doi: 10.1093/clinchem/48.2.236. [DOI] [PubMed] [Google Scholar]
- 29.Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF, 3rd, Feldman HI, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150(9):604–612. doi: 10.7326/0003-4819-150-9-200905050-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Xu W, Yu Q, Xie L, Chen B, Zhang L. Evaluation of Sysmex XN-1000 hematology analyzer for cell count and screening of malignant cells of serous cavity effusion. Medicine (Baltimore) 2017;96(27):e7433. doi: 10.1097/MD.0000000000007433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sişman AR, Küme T, Taş G, Akan P, Tuncel P. Comparison and evaluation of two C-reactive protein assays based on particle-enhanced immunoturbidimetry. J Clin Lab Anal. 2007;21(2):71–76. doi: 10.1002/jcla.20141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.van Gammeren AJ, van Gool N, de Groot MJM, Cobbaert CM. Analytical performance evaluation of the Cobas 6000 analyzer - special emphasis on trueness verification. Clin Chem Lab Med. 2008;46(6):863–871. doi: 10.1515/CCLM.2008.159. [DOI] [PubMed] [Google Scholar]
- 33.Dobriban E, Owen AB. Deterministic parallel analysis: an improved method for selecting factors and principal components. J R Stat Soc Ser B. 2019;81(1):163–83. doi: 10.1111/rssb.12301. [DOI] [Google Scholar]
- 34.Unal I. Defining an optimal cut-point value in ROC analysis: an alternative approach. Comput Mathemat Methods Med. 2017 doi: 10.1155/2017/3762651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Valenti L, Pelusi S. Redefining fatty liver disease classification in 2020. Liver Int: official Journal of the International Association for the Study of the Liver. 2020;40:1016–7. doi: 10.1111/liv.14430. [DOI] [PubMed] [Google Scholar]
- 36.Zhou YY, Zhou XD, Wu SJ, Fan DH, Van Poucke S, Chen YP, et al. Nonalcoholic fatty liver disease contributes to subclinical atherosclerosis: a systematic review and meta-analysis. Hepatol Commun. 2018;2(4):376–392. doi: 10.1002/hep4.1155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zhou Y-Y, Zhou X-D, Wu S-J, Fan D-H, Van PS, Chen Y-P, et al. Nonalcoholic fatty liver disease contributes to subclinical atherosclerosis: a systematic review and meta-analysis. Hepatol Commun. 2018;2:376–392. doi: 10.1002/hep4.1155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chang Y, Ryu S, Sung K-C, Kyun Y, Sung E, Kim H-N, et al. Alcoholic and non-alcoholic fatty liver disease and associations with coronary artery calcification: evidence from the Kangbuk Samsung health study. Gut. 2019;68:1667–1675. doi: 10.1136/gutjnl-2018-317666. [DOI] [PubMed] [Google Scholar]
- 39.Zhou Y-Y, Zhou X-D, Wu S-J, Hu X-Q, Tang B, van Poucke S, et al. Synergistic increase in cardiovascular risk in diabetes mellitus with nonalcoholic fatty liver disease: a meta-analysis. Eur J Gastroenterol Hepatol. 2018;30(6):631–6. doi: 10.1097/MEG.0000000000001075. [DOI] [PubMed] [Google Scholar]
- 40.Metra M, Teerlink JR. Heart failure. Lancet (London, England) 2017;390(10106):1981–1995. doi: 10.1016/S0140-6736(17)31071-1. [DOI] [PubMed] [Google Scholar]
- 41.Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution. Eur J Heart Fail. 2016;18(8):891–975. doi: 10.1002/ejhf.592. [DOI] [PubMed] [Google Scholar]
- 42.Rutten FH, Cramer M-JM, Grobbee DE, Sachs APE, Kirkels JH, Lammers J-WJ, et al. Unrecognized heart failure in elderly patients with stable chronic obstructive pulmonary disease. Eur Heart J. 2005;26(18):1887–94. doi: 10.1093/eurheartj/ehi291. [DOI] [PubMed] [Google Scholar]
- 43.Boonman-de Winter LJM, Rutten FH, Cramer MJM, Landman MJ, Liem AH, Rutten GEHM, et al. High prevalence of previously unknown heart failure and left ventricular dysfunction in patients with type 2 diabetes. Diabetologia. 2012;55(8):2154–62. doi: 10.1007/s00125-012-2579-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Oh T, Kim D, Lee S, Won C, Kim S, Yang J, et al. Machine learning-based diagnosis and risk factor analysis of cardiocerebrovascular disease based on KNHANES. Sci Rep. 2022;12(1):2250. doi: 10.1038/s41598-022-06333-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Alaa AM, Bolton T, Di Angelantonio E, Rudd JHF, van der Schaar M. Cardiovascular disease risk prediction using automated machine learning: a prospective study of 423,604 UK Biobank participants. PLoS ONE. 2019;14(5):e0213653. doi: 10.1371/journal.pone.0213653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kannel WB, Dawber TR, Kagan A, Revotskie N, Stokes J., 3rd Factors of risk in the development of coronary heart disease–six year follow-up experience the Framingham study. Ann Intern Med. 1961;55:33–50. doi: 10.7326/0003-4819-55-1-33. [DOI] [PubMed] [Google Scholar]
- 47.Mehta A, Rigdon J, Tattersall MC, German CA, Barringer TA, Joshi PH, et al. Association of carotid artery plaque with cardiovascular events and incident coronary artery calcium in individuals with absent coronary calcification. Circ Cardiovasc Imaging. 2021;14(4):e011701. doi: 10.1161/CIRCIMAGING.120.011701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Association AD. Standards of medical care in diabetes—2022 abridged for primary care providers. Clin Diabetes. 2022;40(1):10–38. doi: 10.2337/cd22-as01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Cosentino F, Grant PJ, Aboyans V, Bailey CJ, Ceriello A, Delgado V, et al. 2019 ESC guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD: the task force for diabetes, pre-diabetes, and cardiovascular diseases of the European Society of Cardiology (ESC) and the European Associ. Eur Heart J. 2020;41(2):255–323. doi: 10.1093/eurheartj/ehz486. [DOI] [PubMed] [Google Scholar]
- 50.Ben-Shlomo Y, Spears M, Boustred C, May M, Anderson SG, Benjamin EJ, et al. Aortic pulse wave velocity improves cardiovascular event prediction: an individual participant meta-analysis of prospective observational data from 17,635 subjects. J Am Coll Cardiol. 2014;63(7):636–646. doi: 10.1016/j.jacc.2013.09.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kleindorfer DO, Towfighi A, Chaturvedi S, Cockroft KM, Gutierrez J, Lombardi-Hill D, et al. 2021 Guideline for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline from the American heart association/American Stroke Association. Stroke. 2021;52(7):e364–467. doi: 10.1161/STR.0000000000000375. [DOI] [PubMed] [Google Scholar]
- 52.Joh JH, Cho S. Cardiovascular risk of carotid atherosclerosis: global consensus beyond societal guidelines. Lancet Glob Heal. 2020;8(5):e625–e626. doi: 10.1016/S2214-109X(20)30132-7. [DOI] [PubMed] [Google Scholar]
- 53.Krist AH, Davidson KW, Mangione CM, Barry MJ, Cabana M, Caughey AB, et al. Screening for asymptomatic carotid artery stenosis: US preventive services task force recommendation statement. JAMA. 2021;325(5):476–481. doi: 10.1001/jama.2020.26988. [DOI] [PubMed] [Google Scholar]
- 54.Bosowski P, Bosowska J, Nalepa J. Evolving Deep Ensembles For Detecting Covid-19 In Chest X-Rays. In: 2021 IEEE International Conference on Image Processing (ICIP). 2021. p. 3772–6.
- 55.Yadav SS, Jadhav SM. Deep convolutional neural network based medical image classification for disease diagnosis. J Big Data. 2019;6(1):113. doi: 10.1186/s40537-019-0276-2. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.