Abstract
Purpose
High blood urea nitrogen (BUN) is associated with an elevated risk of mortality in various diseases, such as heart failure and pneumonia. Heart failure and pneumonia are common comorbidities of chronic obstructive pulmonary disease (COPD) exacerbation. However, data on the relationship of BUN levels with length of stay (LOS) in patients with pneumonic COPD exacerbation are sparse. The purpose of this study was to evaluate the correlation between BUN levels and LOS in a cohort of patients with pneumonic COPD exacerbation.
Patients and Methods
The present study was a multicentre, retrospective cohort study. A total of 1226 patients with pneumonic COPD exacerbation were included through a validated algorithm derived from the 10th revision of the International Classification of Diseases and Related Health Problems (ICD-10). It should be noted that the entire study was completed by Shiroshita et al, who uploaded the data to the DATADRYAD website. The author only used these data for secondary analysis.
Results
After adjusting for potential confounders (age, gender), a nonlinear relationship was detected between BUN levels less than 40 mg/dl and LOS. The effect sizes and the confidence intervals on the left and right sides of the inflection point were 0.27 (0.16, 0.39) and −0.17 (−0.34, 0.01), respectively.
Conclusion
High levels of BUN in the hospital may be associated with increased LOS. BUN was positively related to LOS when BUN was less than 40 mg/dl.
Keywords: pneumonia, chronic obstructive pulmonary disease, exacerbation, blood urea nitrogen, length of stay
Introduction
AECOPD affects long-term outcomes and is associated with substantial in-hospital mortality.1 The disease course is chronic and progressive, often with “worsening” caused by respiratory infections, multiple organ dysfunction, and comorbidities.2,3 High levels of BUN, suggestive of impaired heart and kidney function and poor neurohormonal activation, are often considered an ominous sign of various diseases.4 Studies have confirmed that in critically ill patients, elevated BUN levels are associated with increased mortality.5
Patients with AECOPD frequently experience hypoxia, carbon dioxide retention, and systemic inflammation that may affect cardiac function, renal function, and neurohumoural regulation.6 In addition, heart failure and pneumonia are common comorbidities in AECOPD, so high BUN levels may be associated with poor prognosis in AECOPD. However, to date, no studies have assessed the relationship between BUN levels at admission for pneumonic COPD exacerbation and LOS. Therefore, this study was based on a cohort of 1226 participants to further investigate the effect of BUN levels on LOS in patients with pneumonic COPD exacerbation.
This report is a secondary analysis based on existing published data.7 The BUN level was used as the independent variable in this secondary analysis, and most of the covariates were consistent with the original text.
Methods
Study Design and Participants
The study population was derived from a previously reported retrospective cohort study7 carried out across a secondary analysis in five acute general hospitals in Japan (Kameda Medical Center, Hyogo Prefectural Amagasaki General Medical Center, Awa Regional Medical Center, Saiseikai Yokohamashi Tobu Hospital, and Ichinomiyanishi Hospital). A total of 1226 patients with pneumonic COPD exacerbation (excluding 11 patients with missing breath levels) were included in this analysis. The inclusion criteria were hospitalized patients with pneumonic COPD exacerbation of age ≥40 years. As described in a previous article,8 we used a modified version of the patient selection algorithm based on the International Statistical Classification of Diseases and Related Health Problems (ICD-10) 10th edition. Inclusion criteria were as follows: (1) Diagnosis of initial pneumonia (ICD-10 codes: J12, J13, J14, J15, J16, J18, J69, and P23) at the time of admission with comorbid COPD (ICD-10 codes: J44.1 and J44.9); (2) Initial admission diagnosis of COPD exacerbation (ICD-10 code; J44.1) with comorbid pneumonia on admission (ICD-10 code; J12, J13, J14, J15, J18, J69 and P23). Exclusion criteria were as follows: diagnosis with other respiratory diseases and complicated pneumonia (asthma attack, pneumothorax or heart failure, obstructive pneumonia or empyema), diagnosis with severe cardiopulmonary disease (patients requiring tracheal intubation, tracheotomy or use of vasopressors on the day of admission).
The research protocol complied with the Declaration of Helsinki. In addition, the project was approved by the various hospital institutional review boards, and due to the retrospective nature of the study (approval number, 19-076), the Kameda Medical Center Institutional Review Board waived the need for written informed consent. Access to patient data was anonymous and confidential.
Since this paper is a secondary analysis of a retrospective study, it has been approved by the Ethics Committee of Shaanxi Provincial People’s Hospital.
Data Source
We retrieved data information from the “DATADRYAD” database. The study cites the Dryad packet from Shiroshita et al 2020. The variables analysed included age, gender, use of steroid treatment, activity of daily living (full assistance or not), BUN levels, respiratory rate (rr), altered mental status(AMS), heart rate (hr), information regarding wheezing lung sounds, fever, clinical stability, hospital discharge, and tracheal intubation.
Statistical Analysis
Data were analysed in this study using R statistical software (https://www.r-project.org) and EmpowerStats (http://www.empowerstats.com, X&Y Solutions, Inc. Boston MA). Continuous variables are presented as the mean±standard deviation or median (interquartile range, 25th-75th percentile), and categorical variables are presented as numbers and percentages. Statistical differences were determined using the chi-square test, one-way ANOVA, and Kruskal‒Wallis H-test. In addition, a generalized additive model (GAM) was used to analyse the nonlinear relationship between BUN levels and LOS in pneumonic COPD exacerbation patients. A P value <0.05 was considered statistically significant.
Results
Patients’ Baseline Characteristics
A total of 1226 hospitalized patients with pneumonic COPD exacerbation were included in this study (Table 1). BUN-stratified groups defined by quartiles were Q1 group (<13.80), Q2 group (14.00–17.70), Q3 group (18.00–24.80) and Q4 group (25.00–152.00). Compared with subjects in the highest quartile of BUN levels (Q4), patients in the other three groups (Q1-Q3) had significantly lower changes in age, rr, LOS, and AMS (p<0.05).
Table 1.
Baseline Characteristics of Participants
| Bun Quartile | Q1 (<13.8) | Q2 (14.00–17.70) | Q3 (18.00–24.80) | Q4 (25.00–152.00) | P-value |
|---|---|---|---|---|---|
| Number of patients | 290 | 283 | 342 | 311 | |
| Age (mean ±sd) | 75.66±8.84 | 78.02±7.80 | 79.94±7.76 | 82.84±7.38 | <0.001 |
| RR (mean ±sd) | 23.38±5.62 | 24.27±7.15 | 24.55±6.10 | 25.37±6.27 | 0.003 |
| HR (mean ±sd) | 102.77±19.74 | 101.80±18.39 | 101.65±19.39 | 99.01±19.33 | 0.098 |
| LOS (mean ±sd) | 14.69±11.86 | 15.42±16.02 | 17.08±16.03 | 20.42±19.05 | <0.001 |
| Time to stability (mean ±sd) | 3.97±4.35 | 3.40±3.66 | 4.31±4.87 | 3.72±4.56 | 0.069 |
| Gender (n, %) | 0.049 | ||||
| Male | 249 (85.86%) | 258 (91.17%) | 314 (91.81%) | 284 (91.32%) | |
| Female | 41 (14.14%) | 25 (8.83%) | 28 (8.19%) | 27 (8.68%) | |
| Steroid (n, %) | 0.627 | ||||
| No | 135 (46.55%) | 142 (50.18%) | 158 (46.20%) | 140 (45.02%) | |
| Yes | 155 (53.45%) | 141 (49.82%) | 184 (53.80%) | 171 (54.98%) | |
| Hospital (n, %) | <0.001 | ||||
| 1 | 150 (51.72%) | 148 (52.30%) | 122 (35.67%) | 110 (35.37%) | |
| 2 | 76 (26.21%) | 85 (30.04%) | 134 (39.18%) | 141 (45.34%) | |
| 3 | 18 (6.21%) | 12 (4.24%) | 19 (5.56%) | 13 (4.18%) | |
| 4 | 18 (6.21%) | 15 (5.30%) | 33 (9.65%) | 21 (6.75%) | |
| 5 | 28 (9.66%) | 23 (8.13%) | 34 (9.94%) | 26 (8.36%) | |
| Full assisting in daily activities (n, %) | <0.001 | ||||
| No | 264 (91.03%) | 246 (86.93%) | 302 (88.30%) | 236 (75.88%) | |
| Yes | 26 (8.97%) | 37 (13.07%) | 40 (11.70%) | 75 (24.12%) | |
| Wheezing lung sound (n, %) | 0.119 | ||||
| No | 186 (64.14%) | 199 (70.32%) | 249 (72.81%) | 212 (68.17%) | |
| Yes | 104 (35.86%) | 84 (29.68%) | 93 (27.19%) | 99 (31.83%) | |
| AMS (n, %) | <0.001 | ||||
| No | 261 (90.31%) | 250 (88.34%) | 293 (85.67%) | 224 (72.73%) | |
| Yes | 28 (9.69%) | 33 (11.66%) | 49 (14.33%) | 84 (27.27%) | |
| Fever (n, %) | 0.389 | ||||
| No | 213 (73.45%) | 216 (76.33%) | 263 (76.90%) | 247 (79.42%) | |
| Yes | 77 (26.55%) | 67 (23.67%) | 79 (23.10%) | 64 (20.58%) | |
| Stability (n, %) | 0.013 | ||||
| No | 41 (14.14%) | 46 (16.25%) | 46 (13.45%) | 69 (22.19%) | |
| Yes | 249 (85.86%) | 237 (83.75%) | 296 (86.55%) | 242 (77.81%) | |
| Discharge (n, %) | 0.003 | ||||
| No | 17 (5.86%) | 15 (5.30%) | 19 (5.56%) | 37 (11.90%) | |
| Yes | 273 (94.14%) | 268 (94.70%) | 323 (94.44%) | 274 (88.10%) | |
| Intubation (n, %) | 0.243 | ||||
| No | 287 (98.97%) | 281 (99.29%) | 341 (100.00%) | 307 (98.71%) | |
| Yes | 3 (1.03%) | 2 (0.71%) | 0 (0.00%) | 4 (1.29%) |
Abbreviations: RR, respiratory rate; HR, heart rate; LOS, length of stay; AMS, altered mental status; 1, Kameda Medical Center; 2, Hyogo Prefectural Amagasaki General Medical Center; 3, Awa Regional Medical Center; 4, Saiseikai Yokohamashi Tobu Hospital; 5, Ichinomiyanishi Hospital.
Univariate Analysis of All Variables
The results of univariate analysis showed that age, BUN, rr, AMS, and intubation were positively related to LOS. Full assistance in daily activities, wheezing lung sounds and stability were negatively correlated with LOS. However, gender was not associated with LOS (Table 2).
Table 2.
The Results of Univariate Analysis
| Characteristics | Statistics | β (95% CI) | P-value |
|---|---|---|---|
| Age | 79.27±8.35 | 0.11 (0.01, 0.22) | 0.0403 |
| Gender | |||
| Male | 1105 (90.13%) | Ref | |
| Female | 121 (9.87%) | −2.67 (−5.67, 0.33) | 0.0811 |
| Steroid | |||
| No | 575 (46.90%) | Ref | |
| Yes | 651 (53.10%) | 1.07 (−0.73, 2.87) | 0.2452 |
| Hospital | |||
| 1 | 530 (43.23%) | Ref | |
| 2 | 436 (35.56%) | 0.95 (−1.07, 2.98) | 0.3570 |
| 3 | 62 (5.06%) | −5.00 (−9.17, −0.84) | 0.0187 |
| 4 | 87 (7.10%) | 3.28 (−0.34, 6.91) | 0.0757 |
| 5 | 111 (9.05%) | 1.40 (−1.88, 4.69) | 0.4024 |
| Full assisting in daily activities | |||
| No | 1048 (85.48%) | Ref | |
| Yes | 178 (14.52%) | −6.59 (−9.05, −4.03) | <0.0001 |
| Wheezing lung sound | |||
| No | 846 (60.00%) | Ref | |
| Yes | 380 (31.00%) | −3.43 (−5.36, −1.50) | 0.0005 |
| RR | 24.42±6.31 | 0.25 (0.10, 0.40) | 0.0009 |
| AMS | |||
| No | 1028 (84.12%) | Ref | |
| Yes | 194 (15.88%) | 3.36 (0.91, 5.82) | 0.0073 |
| HR | 101.28±19.26 | −0.00 (−0.05, 0.04) | 0.8779 |
| Fever | |||
| No | 939 (76.59%) | Ref | |
| Yes | 287 (23.41%) | 0.18 (−1.94, 2.31) | 0.8651 |
| Stability | |||
| No | 202 (16.48%) | Ref | |
| Yes | 1024 (83.52%) | −4.09 (−6.50, −1.69) | 0.0009 |
| Discharge | |||
| No | 88 (7.18%) | Ref | |
| Yes | 1138 (92.82%) | −3.38 (−6.87, 0.11) | 0.0577 |
| Intubation | |||
| No | 1216 (99.27%) | Ref | |
| Yes | 9 (0.73%) | 39.10 (28.76, 49.44) | <0.0001 |
| Bun | 21.39 ± 12.53 | 0.14 (0.07, 0.21) | 0.0002 |
| Bun quartile | |||
| Q1 | 290 (23.65%) | Ref | |
| Q2 | 283 (23.08%) | 0.73 (−1.89, 3.35) | 0.5849 |
| Q3 | 342 (27.90%) | 2.39 (−0.12, 4.89) | 0.0621 |
| Q4 | 311 (25.37%) | 5.73 (3.17, 8.29) | <0.0001 |
Abbreviations: RR, respiratory rate; HR, heart rate; LOS, length of stay; AMS, altered mental status; 1, Kameda Medical Center; 2, Hyogo Prefectural Amagasaki General Medical Center; 3, Awa Regional Medical Center; 4, Saiseikai Yokohamashi Tobu Hospital; 5, Ichinomiyanishi Hospital.
Relationship Between BUN Levels and LOS
As shown in Table 3, in the crude model, every 1 mg/dl increase in BUN extended LOS by 0.1 days (95% CI 0.1 to 0.2, p<0.001). In Model I (adjusted for age and gender) and model II (further adjusted for steroids, full assistance in daily activities, wheezing lung sounds, rr, AMS, hr, fever stability, discharge and intubation), the correlations were similar to those in the crude model. To confirm the stability of the results, this study performed a sensitivity analysis of BUN levels by categorical variables (quartiles). The results showed that BUN levels were positively correlated with LOS (Table 3).
Table 3.
Association Between BUN Levels and LOS
| Crude Model | Model I | Model II | |
|---|---|---|---|
| β (95% CI) P-value | β (95% CI) P-value | β (95% CI) P-value | |
| Bun | 0.1 (0.1, 0.2) <0.001 | 0.1 (0.1, 0.2) <0.001 | 0.1 (0.0, 0.2) 0.011 |
| Bun quartile | |||
| Q1 | Ref | Ref | Ref |
| Q2 | 0.7 (−1.9, 3.4) 0.585 | 0.5 (−2.1, 3.2) 0.702 | 0.3 (−2.3, 3.0) 0.793 |
| Q3 | 2.4 (−0.1, 4.9) 0.062 | 2.1 (−0.5, 4.6) 0.111 | 1.6 (−0.9, 4.1) 0.213 |
| Q4 | 5.7 (3.2, 8.3) <0.001 | 5.3 (2.6, 8.0) <0.001 | 4.6 (1.9, 7.3) <0.001 |
| p for trend | 1.9 (1.1, 2.7) <0.001 | 1.8 (0.9, 2.6) <0.001 | 1.5 (0.6, 2.3) <0.001 |
Notes: Crude model adjust for: None. Model I adjust for: age; gender. Model II adjust for: age; gender; steroid; full assisting in daily activities; wheezing lung sound; rr; AMS; hr; fever; stability; discharge; intubation.
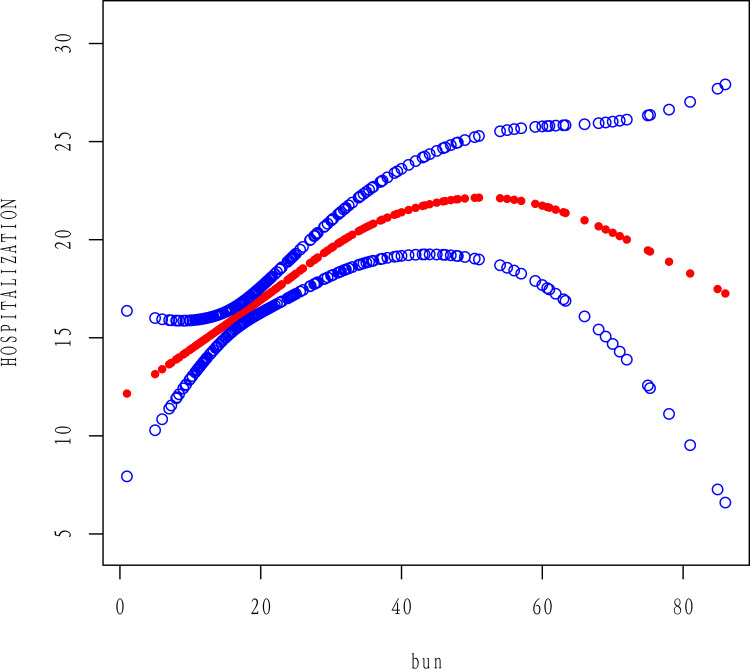
Nonlinear Relationship Analysis
As shown in Figure 1, after adjusting for age, gender, steroid use, full assistance in daily activities, wheezing lung sounds, rr, AMS, hr, fever, stability, discharge and intubation, our analysis found a nonlinear relationship between BUN levels and LOS. Through the analysis of the two-segment regression model, it was found that the inflection point was 40. The effect size and confidence interval to the left of this inflection point were 0.27 (0.16–0.39, P<0.0001). However, to the right of the inflection point, we did not observe an association between BUN levels and LOS (P=0.0632) (Table 4).
Figure 1.
A non-linear relationship of BUN levels with LOS.
Table 4.
The Results of Two-Piecewise Linear Regression Model
| Inflection Point of BUN Levels (mg/dl) | (β) 95% CI | P-value |
|---|---|---|
| <40 | 0.27 (0.16, 0.39) | <0.0001 |
| ≥40 | −0.17 (−0.34, 0.01) | 0.0632 |
Notes: Effect: LOS. Cause: BUN levels. Adjusted: age; gender; steroid; full assisting in daily activities; wheezing lung sound; rr; AMS; hr; fever; stability; discharge; intubation.
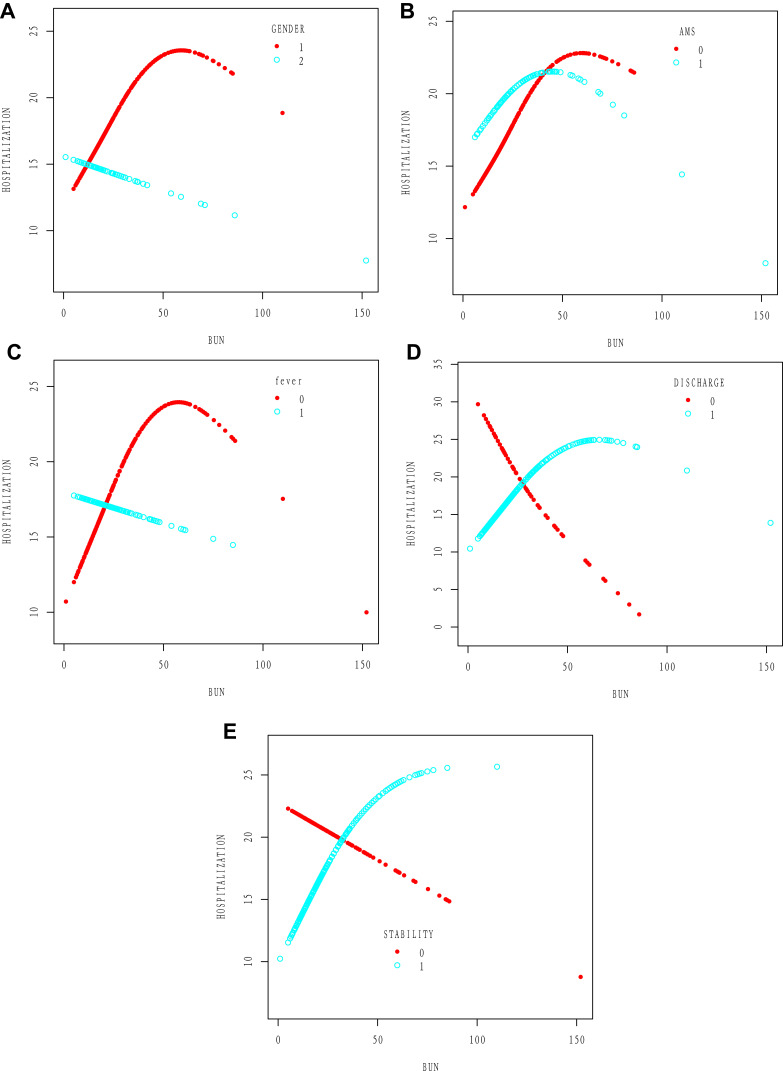
Subgroup Analysis
To further analyse the impact of other risk factors associated with BUN levels and LOS, this study performed subgroup analyses on the following stratified variables: age, gender, steroid use, full assistance in daily activities, wheezing lung sounds, rr, AMS, hr, fever, stability, discharge and intubation (Table 5). Additive interactions between BUN levels and LOS were observed for gender, AMS, fever, stability and discharge. (P value for interaction<0.05). Stronger correlations were found in participants with gender, AMS, fever, stability and discharge (Figure 2). However, significant interactions were not found for age, steroid use, rr, hr, intubation, full assistance in daily activities, or wheezing lung sounds.
Table 5.
Effect of BUN Levels on LOS by Subgroups
| Characteristics | N | (β) 95% CI | P-value | P (Interaction) |
|---|---|---|---|---|
| Age | 0.7690 | |||
| 47–75 | 388 | 0.12 (−0.02, 0.26) | 0.0846 | |
| 76–82 | 390 | 0.16 (0.00, 0.32) | 0.0460 | |
| 83–105 | 448 | 0.10 (−0.00, 0.20) | 0.0601 | |
| Gender | 0.0104 | |||
| Male | 1105 | 0.18 (0.10, 0.27) | <0.0001 | |
| Female | 121 | −0.05 (−0.15, 0.04) | 0.2916 | |
| Steroid | 0.5770 | |||
| No | 575 | 0.12 (0.02, 0.21) | 0.0163 | |
| Yes | 651 | 0.16 (0.05, 0.26) | 0.0036 | |
| RR group | 0.2809 | |||
| 0–21 | 372 | 0.25 (0.10, 0.40) | 0.0008 | |
| 22–25 | 338 | 0.10 (−0.03, 0.23) | 0.1396 | |
| 26–81 | 408 | 0.13 (0.00, 0.25) | 0.0485 | |
| AMS | 0.0288 | |||
| No | 1028 | 0.18 (0.10, 0.27) | <0.0001 | |
| Yes | 194 | 0.01 (−0.14, 0.16) | 0.9253 | |
| HR group | 0.7309 | |||
| 30–91 | 390 | 0.16 (0.04, 0.29) | 0.0119 | |
| 92–108 | 403 | 0.15 (0.05, 0.26) | 0.0035 | |
| 109–200 | 419 | 0.09 (−0.07, 0.25) | 0.2625 | |
| Fever | 0.0248 | |||
| No | 939 | 0.18 (0.10, 0.26) | <0.0001 | |
| Yes | 287 | −0.04 (−0.20, 0.12) | 0.6096 | |
| Stability | <0.0001 | |||
| No | 202 | −0.092 (−0.252, 0.069) | 0.2626 | |
| Yes | 1024 | 0.235 (0.154, 0.317) | <0.0001 | |
| Discharge | <0.0001 | |||
| No | 88 | −0.357 (−0.643, −0.072) | 0.0162 | |
| Yes | 1138 | 0.208 (0.134, 0.281) | <0.0001 | |
| Intubation | 0.9303 | |||
| No | 1216 | 0.125 (0.055, 0.195) | 0.0005 | |
| Yes | 9 | 0.15 (−0.30, 0.59) | 0.5188 | |
| Full assisting in daily activities | 0.8599 | |||
| No | 1048 | 0.110 (0.031, 0.188) | 0.0061 | |
| Yes | 178 | 0.125 (−0.061, 0.310) | 0.1907 | |
| Wheezing lung sound | 0.3701 | |||
| No | 846 | 0.158 (0.064, 0.251) | 0.001 | |
| Yse | 380 | 0.086 (−0.010, 0.183) | 0.0793 |
Figure 2.
Effect of BUN levels on LOS by subgroups of gender, AMS, fever, discharge and stability (A–E).
Discussion
Based on the current research literature, this is the first study to investigate the association between BUN levels and LOS in patients with pneumonic COPD exacerbation. It is well known that the level of BUN is a biomarker that is widely used in clinical practice and that can be quickly obtained as a test result. Our study demonstrated a nonlinear association between BUN levels and LOS in patients with pneumonic COPD exacerbation; namely, when the BUN level was below the inflection point of 40 mg/dl, LOS was positively correlated with the BUN level. Furthermore, to reduce the likelihood of bias and overestimation of correlations, we adjusted for a range of potential confounders. In multivariate logistic regression analyses, BUN as a categorical or continuous variable was significantly associated with LOS, and consistent results were observed in stratified analyses. The relationship between BUN levels and LOS in patients with pneumonic COPD exacerbation was further confirmed. The findings of this study may be helpful to clinicians. At the time of emergency admission, appropriate interventions can be selected according to the BUN level.
In patients with other lung disease types, BUN levels have also been shown to correlate with poor prognosis. A retrospective study of patients with acute pulmonary embolism showed that patients with higher BUN levels had adverse hospital outcomes at a significantly higher rate than those with lower BUN levels.9 In patients with aspiration pneumonia and community-acquired pneumonia, BUN levels were significantly different between the surviving and nonsurviving groups.10 BUN levels were also identified as a major risk factor associated with poor COVID-19 outcomes.11 In a study of elderly emergency patients and critically ill patients, BUN levels were also shown to be associated with poor outcomes.12 Therefore, BUN may contribute to increased LOS in patients with pneumonic COPD exacerbation. Possible explanations are as follows: BUN levels are considered to be markers of neurohumoural activity, cardiorenal function, and catabolic conditions. Cardiovascular disease, although often undetected, is prevalent in COPD patients and activates the SNS and RAS, which in turn reduces eGFR and increases urea reabsorption. Respiratory infections are the main cause of “exacerbations” in COPD patients. Patients with pneumonia often have a state of hydration that results in increased renal reabsorption of urea, and elevated BUN levels are frequently observed. It has been reported that in patients with pulmonary infection, higher BUN levels are generally associated with a worse prognosis,13 which may be due to catabolic abnormalities caused by the inflammatory response and dehydration state in patients with pneumonia. However, the impact of these mechanisms should be assessed through further studies.14,15 In this study, all patients with pneumonic COPD exacerbation contributed to the correlation of BUN levels with LOS.
Furthermore, our study has certain limitations. First, the study was a retrospective cohort study, so some bias may have inevitably been introduced. Excluded patients may have influenced the study results, and we were unable to assess this. Second, due to the limitations of the raw data, we were unable to obtain detailed information on the baseline characteristics and experimental parameters of all patients, such as patient BMI, smoking history, disease history, pulmonary function (FEV1), and blood oxygen saturation. Third, we performed a secondary analysis of limited raw data. The target population consisted of relatively elderly Japanese patients with pneumonic COPD exacerbation. Ninety percent of the population was male, which may be related to the higher incidence in males and strict exclusion criteria, which of course also causes a certain gender bias.
Conclusion
In our cohort study, the BUN concentration on admission was closely related to LOS in pneumonic COPD exacerbation patients, showing a nonlinear relationship, and when the BUN level was less than 40 mg/dl, LOS was positively correlated with BUN level. As an inexpensive and readily determined parameter, elevated BUN levels on admission should be a red flag to alert physicians regarding early intervention.
Funding Statement
The present study was supported by Funds of the Shaanxi Provincial People’s Hospital Science and Technology Talent Support Program [grant numbers 2021JY-42] and Shaanxi Provincial People’s Hospital Science and Technology Development Incubation Fund Project [grant numbers 2021YJY-33].
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Nilsson U, Vanfleteren LEGW. Troponin as a biomarker for mortality in stable COPD. Eur Respir J. 2020;55(2):1902447. doi: 10.1183/13993003.02447-2019 [DOI] [PubMed] [Google Scholar]
- 2.Kahnert K, Alter P, Young D, et al. The revised GOLD 2017 COPD categorization in relation to comorbidities. Respir Med. 2018;134:79–85. doi: 10.1016/j.rmed.2017.12.003 [DOI] [PubMed] [Google Scholar]
- 3.Singh D, Agusti A, Anzueto A, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease: the GOLD science committee report 2019. Eur Respir J. 2019;53(5):1900164. doi: 10.1183/13993003.00164-2019 [DOI] [PubMed] [Google Scholar]
- 4.Feng DY, Zhou YQ, Zou XL, et al. Elevated blood urea nitrogen-to-serum albumin ratio as a factor that negatively affects the mortality of patients with hospital-acquired pneumonia. Can J Infect Dis Med Microbiol. 2019;2019:1547405. doi: 10.1155/2019/1547405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Beier K, Eppanapally S, Bazick HS, et al. Elevation of blood urea nitrogen is predictive of long-term mortality in critically ill patients independent of “normal” creatinine. Crit Care Med. 2011;39(2):305–313. doi: 10.1097/CCM.0b013e3181ffe22a [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Thomsen M, Ingebrigtsen TS, Marott JL, et al. Inflammatory biomarkers and exacerbations in chronic obstructive pulmonary disease. JAMA. 2013;309(22):2353–2361. doi: 10.1001/jama.2013.5732 [DOI] [PubMed] [Google Scholar]
- 7.Shiroshita A, Shiba H, Tanaka Y, et al. Effectiveness of steroid therapy on pneumonic chronic obstructive pulmonary disease exacerbation: a multicenter, retrospective cohort study. Int J Chron Obstruct Pulmon Dis. 2020;15:2539–2547. doi: 10.2147/COPD.S271844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Scholl T, Kiser TH, Vondracek SF. Evaluation of systemic corticosteroids in patients with an acute exacerbation of COPD and a diagnosis of pneumonia. Chron Obstr Pulmon Dis. 2018;5(1):57–65. doi: 10.15326/jcopdf.5.1.2017.0157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tatlisu MA, Kaya A, Keskin M, et al. The association of blood urea nitrogen levels with mortality in acute pulmonary embolism. J Crit Care. 2017;39:248–253. doi: 10.1016/j.jcrc.2016.12.019 [DOI] [PubMed] [Google Scholar]
- 10.Ryu S, Oh SK, Cho SU, et al. Utility of the blood urea nitrogen to serum albumin ratio as a prognostic factor of mortality in aspiration pneumonia patients. Am J Emerg Med. 2021;43:175–179. doi: 10.1016/j.ajem.2020.02.045 [DOI] [PubMed] [Google Scholar]
- 11.Cheng A, Hu L, Wang Y, et al. Diagnostic performance of initial blood urea nitrogen combined with D-dimer levels for predicting in-hospital mortality in COVID-19 patients. Int J Antimicrob Ag. 2020;56(3):106110. doi: 10.1016/j.ijantimicag.2020.106110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dundar ZD, Kucukceran K, Ayranci MK. Blood urea nitrogen to albumin ratio is a predictor of in-hospital mortality in older emergency department patients. Am J Emerg Med. 2021;46:349–354. doi: 10.1016/j.ajem.2020.10.008 [DOI] [PubMed] [Google Scholar]
- 13.Lee JH, Kim J, Kim K, et al. Albumin and C-reactive protein have prognostic significance in patients with community-acquired pneumonia. J Crit Care. 2011;26(3):287–294. doi: 10.1016/j.jcrc.2010.10.007 [DOI] [PubMed] [Google Scholar]
- 14.Akahane J, Ushiki A, Kosaka M, et al. Blood urea nitrogen-to-serum albumin ratio and A-DROP are useful in assessing the severity of Pneumocystis pneumonia in patients without human immunodeficiency virus infection. J Infect Chemother. 2021;27(5):707–714. doi: 10.1016/j.jiac.2020.12.017 [DOI] [PubMed] [Google Scholar]
- 15.Feng DY, Zhou YQ, Zhou M, Zou XL, Wang YH, Zhang TT. Risk factors for mortality due to ventilator-associated pneumonia in a Chinese Hospital: a retrospective study. Med Sci Monit. 2019;25:7660–7665. doi: 10.12659/MSM.916356 [DOI] [PMC free article] [PubMed] [Google Scholar]