Abstract
Purpose
To evaluate the effectiveness and safety of lurasidone 80 mg/day (versus the 40 mg/day dose) during a 12-week, open-label extension study in patients with an acute exacerbation of schizophrenia who had completed a 6-week double-blind study of lurasidone.
Patients and Methods
A total of 289 adult patients with schizophrenia completed the double-blind study and enrolled in the 12-week extension study. Lurasidone was flexibly dosed at 40 or 80 mg/day. Effectiveness measures included the Positive and Negative Syndrome Scale (PANSS) subscale scores, Clinical Global Impression-Severity Scale (CGI-S), and Calgary Depression Scale for Schizophrenia (CDSS), analyzed based on last observation carried forward (LOCF-endpoint). Safety/tolerability assessments included adverse events, body weight, laboratory tests, and discontinuation due to adverse events.
Results
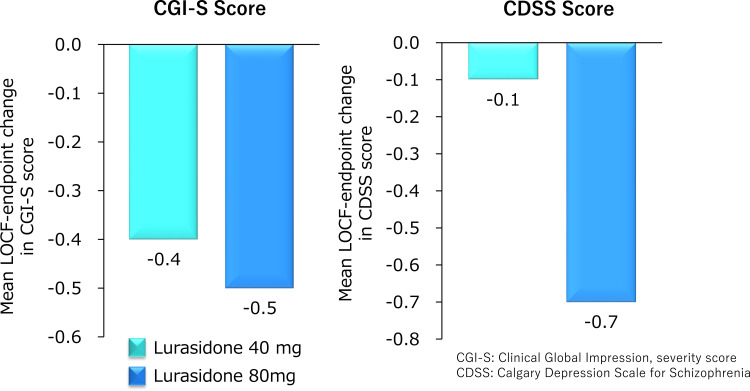
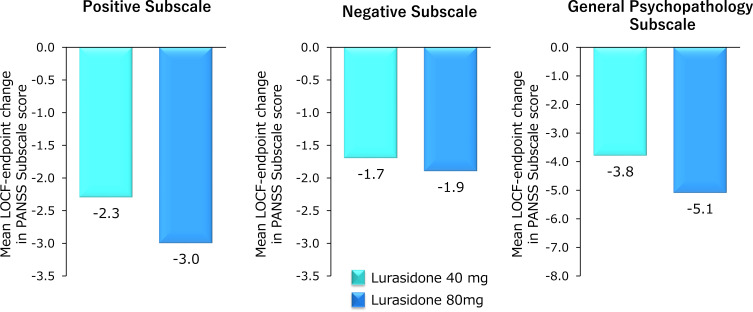
Mean endpoint change was greater for lurasidone in modal doses of 80 mg/d (N=136) vs 40 mg/d (N=153) on the PANSS positive subscale (−3.0 vs −2.3), PANSS negative subscale (−1.9 vs −1.7), PANSS General Psychopathology subscale (−5.1 vs −3.8), the CGI-S score (−0.5 vs −0.4), and the CDSS score (−0.7 vs −0.1). Discontinuation rates due to adverse events on lurasidone modal 80 mg/d vs 40 mg/d were 4.4% vs 7.2%; and the most common adverse events in the modal 80 mg/d group were nasopharyngitis, 7.4% (vs 4.6% on modal 40 mg/d), constipation, 5.9% (vs 2.0%), and headache, 5.9% (vs 2.0%).
Conclusion
In patients with acute schizophrenia treated with lurasidone 40 mg/d, increasing the dose to 80 mg/d was well tolerated, and was associated with greater improvement in PANSS subscale scores compared to continued treatment with a dose of 40 mg/d.
Keywords: lurasidone, schizophrenia, extension treatment, dose escalation, effectiveness, safety
Introduction
Schizophrenia is a psychiatric disorder that presents with a variety of symptoms, including positive symptoms such as hallucinations and delusions, negative symptoms such as apathy and social withdrawal, cognitive symptoms such as working memory, executive function, and processing speed deficits, and depressive symptoms.1,2 The lifetime prevalence of schizophrenia has been estimated to be approximately 0.48% (interquartile range, 0.26% to 0.51%), which translates into over 20 million people worldwide with the disorder.3,4 The disorder is associated with a high global economic burden, largely attributable to its typical onset in early adulthood, the chronicity of psychotic symptoms, and the moderate-to-marked impairment in social and occupational functioning.5 Individuals with a diagnosis of schizophrenia have a notably shorter life expectancy (mean, 14.5 years [95% CI, 11.2–17.8]) that is only partially due to a higher risk of suicide.6,7
Recommended treatment of schizophrenia involves a combination of pharmacotherapy and non-pharmacotherapy.2,8 For addressing the positive symptoms during the acute stage of treatment, antipsychotic medications are indicated.9 After the acute phase, symptoms are under some degree of control, continuation treatment with antipsychotics combined with non-pharmacotherapy interventions (eg, cognitive behavioral therapy for psychosis, psychoeducation, employment services) is recommended. The two-fold goal of continuation treatment is to achieve further reduction in psychotic symptoms, and to prevent an exacerbation of psychosis that will result in relapse.9 The ultimate goal of treatment is recovery, typically defined as remission of symptoms and return to normal levels of functioning; however, only one in seven individuals with schizophrenia achieves recovery.10 A number of factors hinder recovery including cognitive dysfunction,11 mood disorders,12 and poor adherence to medications.13
Lurasidone is a drug with a pharmacological profile that acts as an antagonist for dopamine D2, serotonin (5-HT)7 and 5-HT2A receptors, and as a partial agonist for 5-HT1A receptors, with minimal binding affinity for histamine H1 and muscarinic M1 receptors.14 In 2020, lurasidone 40 mg/d to 80 mg/d was approved in Japan for the treatment of schizophrenia based on the results of a 6-week double-blind, placebo-controlled study of the treatment of schizophrenia in some countries including Japan (JEWEL study; EudraCT number: 2016–000060-42),15 a 12-week open-label extension study (JEWEL extension study; EudraCT number: 2016–000061-23),16 and other clinical trials conducted in the USA and Europe countries.17–19 Lurasidone has also been approved in Japan for the treatment of bipolar depression.
Despite the published studies on lurasidone for the treatment of schizophrenia in Japan and other countries, important clinical questions remain regarding dosage changes during ongoing, longer-term treatment. The primary placebo-controlled trial conducted in Japan and other countries only evaluated the 40 mg dosage over the course of 6 weeks of treatment. A common clinical decision, however, is whether to maintain 40 mg/d or increase dosage to 80 mg/d after evaluating response to short-term treatment. Longer-term open-label studies conducted in other countries used flexible dosing of lurasidone and did not examine efficacy or safety for 40 mg/d compared to 80 mg/d.20–22 A previous paper reported safety data for all patients (40 mg/d and 80 mg/d combined) during the open-label JEWEL extension study, and provided efficacy data on change in total symptomatology from open-label baseline for patients who received a modal dose of 40 mg/d or 80 mg/d during the 12-week extension phase.16 Because the clinical decision of an increase to 80 mg/d must be mindful of tolerability and safety, it is critical to examine tolerability and safety parameters for those who receive 80 mg/d separately from those who receive a lower dose. Moreover, the fact that negative symptoms adversely affect long-term functional outcomes in schizophrenia,23 the impact of a dosage increase to 80 mg/d on a broad range of outcomes, including negative symptoms, is particularly relevant to decisions about dosage increases during longer-term treatment.
The aim of the current post-hoc analysis of the extension phase of the JEWEL study was to evaluate the comparative efficacy and safety of patients treated with two active doses of lurasidone (40 mg/d and 80 mg/d) and the effectiveness of increasing the dose of lurasidone to 80 mg/d compared to continued treatment on a dose of 40 mg/d using a broader array of efficacy scores than previously reported.
Materials and Methods
Participants
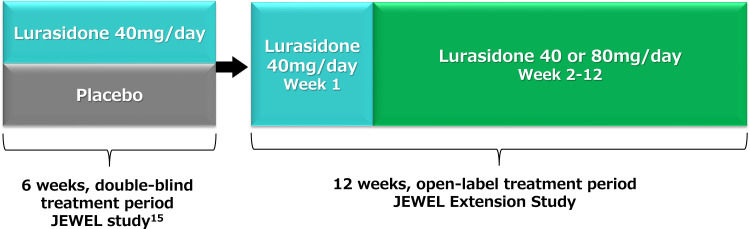
The data for present analysis were collected from the JEWEL Extension Study of lurasidone in people with schizophrenia (clinical trial registration: EudraCT Number: 2016–000061-23).16 The JEWEL Extension Study was 12-week open-label extension study to evaluate the safety and effectiveness of lurasidone flexibly dosed at 40 mg/d or 80 mg/d. The JEWEL Extension Study followed a multicenter, randomized, double-blind, placebo-controlled, parallel-group 6-week study that was designed to evaluate the efficacy and safety of lurasidone 40 mg/d administered to patients (age 18–74) with acute schizophrenia (clinical trial registration: EudraCT number: 2016–000060-42).15 The overall design of the double-blind phase followed by the extension phase is presented in Figure 1. The 6-week study was conducted at 73 clinical sites in 5 countries, including Japan, Ukraine, Russia, Romania, and Poland. Both the 6-week study and the 12-week extension phase were conducted, in accordance with the International Conference on Harmonization Guideline for Good Clinical Practice and the Declaration of Helsinki. The protocol was approved by the Ethics Committee at each participating center (Supplementary Tables 1 and 2) and regarding participation in the studies, use of data, and publication of results, written informed consent was obtained from each patient following an explanation of study procedures.
Figure 1.
Study design.
Key inclusion criteria for the 6-week study were a diagnosis of schizophrenia based on the Mini-International Neuropsychiatric Interview (MINI)24 6.0.0 using the Diagnostic and Statistical Manual of Mental Disorder, 4th Edition, Text Revision (DSM-IV-TR)25 criteria, a Positive and Negative Symptom Scale (PANSS)26 total score ≥80, a PANSS item score ≥4 (moderate) on 2 or more certain PANSS items (delusions, conceptual disorganization, hallucinations, suspiciousness, or unusual thought content) at both screening and baseline, and a score of 4 (moderately ill) or higher on the Clinical Global Impressions-Severity of Illness (CGI-S)27 at screening and baseline. Further selection details are given in the previous article describing the 6-week study.15
Patients were eligible for extension phase study if they completed the short-term double-blind study having received either placebo or lurasidone 40 mg/d during the 6-week trial and completed all assessments on the final visit of that trial. Excluded from the extension phase were patients judged to be an imminent risk of suicide or injury to self or others or who answered “yes” to item 4 (active suicidal ideation with some intent to act, without specific plan) or item 5 (active suicidal ideation with specific plan and intent) on the Columbia-Suicide Severity Rating Scale (C-SSRS)28 at the baseline visit of the extension phase. Also excluded from the extension phase were patients who exhibited evidence of severe tardive dyskinesia, severe dystonia, or other severe movement disorder, as determined by the investigator, or who required treatment with any potent cytochrome P450 (CYP) 3A4 inhibitors or inducers during the study.
Drug Administration
Open-label lurasidone 40 mg/d was administered during the first week of the 12-week extension phase. Starting at day 8, flexible dosing of lurasidone up to 80 mg/d was allowed based on clinical judgment by the investigator. Dosing adjustments at each subsequent visit could then occur. Study visits occurred at baseline and weeks 1, 2, 4, 8, and 12 of the extension phase plus a follow-up visit at week 13. Study drug consisted of tablets containing lurasidone 40 mg administered orally, as one for 40 mg and two for 80 mg once daily, in the evening, with food or within 30 minutes after eating.
Concomitant Medications
To participate in the initial 6-week double-blind trial, patients were required to discontinue antipsychotics, antidepressants, mood stabilizers, and other psychotropics. However, during the extension phase, treatment could be initiated with antidepressant medications (except fluvoxamine) and/or mood stabilizers (except carbamazepine and oxcarbazepine). Benztropine (≤6 mg/d) was permitted as needed during both the 6-week double-blind phase and 12-week extension phase for the management of treatment-emergent movement disorders. If a subject had an inadequate response or intolerability to benztropine treatment, biperiden, trihexyphenidyl, diphenhydramine or promethazine were permitted. Treatment with propranolol (≤120 mg/d) was allowed for akathisia. During both the 6-week trial and extension phase, concomitant use of lorazepam, zolpidem, temazepam, brotizolam, triazolam, lormetazepam, zopiclone, or eszopiclone was permitted. Prohibited during the extension phase were fluoxetine, monoamine oxidase inhibitors, additional antipsychotic medications, electroconvulsive therapy, herbal supplements (for psychotropic reasons), and antiarrhythmic drugs of Class 1A or of Class 3.
Effectiveness Assessments
Effectiveness assessments included the standard PANSS subscales (positive symptoms, negative symptoms, and general psychopathology),26 CGI-S,27 and the Calgary Depression Scale for Schizophrenia score (CDSS).29 The PANSS and CGI were evaluated at open-label baseline and weeks 1, 2, 4, 8, and 12. The CDSS was obtained at open-label baseline and weeks 4 and 12.
Safety Assessments
Safety endpoints reported here include treatment-emergent adverse events (TEAEs), laboratory tests (HbA1c, total cholesterol, triglycerides, fasting blood glucose, serum prolactin), and body weight (from physical). TEAEs and body weight were measured at each study visit during the extension phase. Laboratory tests were conducted at open-label baseline and weeks 4, 8, and 12 of the extension phase. TEAEs were classified using MedDRA Version 19.1.
Statistical Methods
The safety population was defined as patients who received at least 1 dose of open-label study drug during the extension phase. An intention-to-treat (ITT) population was defined for the effectiveness analysis as all patients who received at least 1 dose of open-label study drug during the extension phase and had both open-label baseline and at least 1 post-open-label baseline PANSS assessment. Data were examined for patients who had received a modal dose of lurasidone 40 mg/d during the extension phase and also separately for those who received a modal dose of 80 mg/d during the extension phase. Modal dose was defined the dose received for the most days during the extension phase.
Because there was no random assignment, only descriptive statistics were used to summarize safety and effectiveness outcomes. No statistical inference methods were used. Analyses consisted of descriptive summaries (number and percent of patients) of TEAEs and discontinuation rates, as well as mean change from open-label baseline to week 12 for body weight, laboratory values, PANSS subscale scores, CDSS total score, and CGI-S score. TEAEs were also examined for the 80 mg/d maximum dose, separately for weekly periods at the initial dose increase from 40 to 80 mg/d (even if the dose was increased from 40 mg to 80 mg more than once) during the extension phase. A last observation carried forward (LOCF) endpoint used for patients whose week 12 measure was missed. The LOCF value was derived using the last post-baseline value in the extension phase up to 7 days after the last dose of open-label study drug. Analyses were conducted using SAS Version 9.4 or later.
Results
Participant Disposition and Characteristics
In the initial 6-week double-blind study, 483 patients were randomized to lurasidone 40 mg/d (N=247) or placebo (N=236). A total of 375 patients (lurasidone, N=199; placebo, N=176) completed the 6-week study, of whom 289 (77.1%) enrolled in the 12-week extension phase. All patients in the extension study who received at least one dose of study drug were included in the safety analyses. Two patients enrolled in the extension phase did not have post-baseline assessments (both treated with lurasidone 40 mg/d in the 6-week study) and therefore were excluded from the effectiveness analysis.
Of the 289 patients in the safety population, the modal dose of lurasidone was 40 mg/d in 153 patients (52.9%) and 80 mg/d in 136 patients (47.1%). There were 166 patients who received an increase in dose from 40 to 80 mg/d, 155 of whom were maintained on a dose of 80 mg/d throughout in the extension phase. Overall, the median duration of days of study drug exposure was 84 days.
The demographic and clinical characteristics of the ITT population were generally similar for patients who received a modal dose of 40 mg/d compared to those who received a modal dose of 80 mg/d, however open-label baseline scores for each effectiveness assessment tended to be higher in the modal dose 80 mg group than those in the modal dose 40 mg group (Table 1). For the ITT population as whole, there were similar proportions of males, with an average age of about 40 years.
Table 1.
Patient Demographics and Clinical Characteristics at Baseline (ITT Population)
| Total (N=287) | Modal 40 mg Group (n=151) | Modal 80 mg Group (n=136) | |
|---|---|---|---|
| Sex (Male) [n (%)] | 143 (49.8) | 78 (51.7) | 65 (47.8) |
| Age (Years) [mean (SD)] | 40.1 (11.26) | 41.2 (11.44) | 38.8 (10.96) |
| Double-blind baseline score [mean (SD)] | |||
| PANSS total | 101.1 (11.00) | 100.2 (10.51) | 102.1 (11.47) |
| Positive subscale | 25.3 (3.80) | 25.0 (3.66) | 25.8 (3.93) |
| Negative subscale | 24.2 (4.08) | 24.0 (3.84) | 24.5 (4.33) |
| General Psychopathology Subscale | 51.5 (6.41) | 51.2 (6.22) | 51.8 (6.62) |
| CGI-S | 4.9 (0.60) | 4.8 (0.59) | 5.0 (0.60) |
| CDSS | 4.1 (3.73) (n=286) | 3.9 (3.58) (n=150) | 4.4 (3.88) |
| Open-label baseline score [mean (SD)] | |||
| PANSS total | 80.5 (15.80) | 75.3 (14.50) | 86.4 (15.17) |
| Positive subscale | 19.0 (5.31) | 17.6 (4.45) | 20.6 (5.74) |
| Negative subscale | 20.7 (4.49) | 19.4 (4.45) | 22.0 (4.16) |
| General Psychopathology Subscale | 40.9 (8.29) | 38.3 (7.92) | 43.8 (7.73) |
| CGI-S | 3.9 (0.89) | 3.6 (0.78) | 4.1 (0.93) |
| CDSS | 2.4 (2.85) | 2.0 (2.33) | 2.9 (3.28) |
Notes: Modal 40 mg group: Subjects who received 40 mg for most days during the extension phase. Modal 80 mg group: Subjects who received 80 mg for most days during the extension phase.
Abbreviations: PANSS, Positive and Negative Syndrome Scale, CGI-S, Clinical Global Impressions – Severity scale; CDSS, Calgary Depression Scale for Schizophrenia; ITT, intention-to-treat; SD, standard deviation.
The discontinuation rates were similar: 17.6% in the modal 80 mg/d group and 19.6% in the modal 40 mg/d group. The discontinuation rates due to adverse events were 4.4% in the modal 80 mg/d group and 7.2% in the modal 40 mg/d group.
Effectiveness
Patients increased to a modal 80 mg/d showed continued improvement across the range of outcome measures. For the ITT population, mean endpoint (week 12) change from open-label baseline for lurasidone modal 80 mg/d vs modal 40 mg/d was −0.5 vs −0.4 on the CGI-S score and −0.7 vs −0.1 on the CDSS score (Figure 2). For the ITT population, treatment with lurasidone modal 80 mg/d was associated with slightly greater reduction compared to modal 40 mg/d in the PANSS positive (−3.0 vs −2.3), negative (−1.9 vs −1.7), and general psychopathology subscale scores (−5.1 vs −3.8) (Figure 3).
Figure 2.
Mean change from open-label baseline in CGI-S and CDSS score at Week 12. Modal 40 mg group: Subjects who received 40 mg for most days during the extension phase. Modal 80 mg group: Subjects who received 80 mg for most days during the extension phase.
Abbreviations: LOCF, last observation carried forward; CGI-S, Clinical Global Impressions – Severity scale; CDSS, Calgary Depression Scale for Schizophrenia.
Figure 3.
Mean change from open-label baseline in PANSS subscale scores at Week 12. Modal 40 mg group: Subjects who received 40 mg for most days during the extension phase. Modal 80 mg group: Subjects who received 80 mg for most days during the extension phase.
Abbreviations: LOCF, last observation carried forward; PANSS, Positive and Negative Syndrome Scale.
Safety
There was no evidence of additional safety concerns within the modal 80 mg/d group. The most common treatment-emergent adverse events (≥5.0%) in the modal 80 mg/d group were nasopharyngitis (7.4%), constipation (5.9%), headache (5.9%), schizophrenia symptoms (5.1%), blood prolactin increased (5.1%), and insomnia (5.1%) (Table 2). The most common adverse events in the modal 40 mg/d group were akathisia (9.2%), and schizophrenia symptoms (5.9%). Note that the adverse event “schizophrenia symptoms” denotes an increase in the severity of any of the symptoms of schizophrenia enumerated in the DSM-5 [2]. There were no clinically meaningful mean changes from open-label baseline to week 12 in body weight or laboratory parameters (including cholesterol measures, triglycerides, blood glucose, and serum prolactin) for each group (Table 3).
Table 2.
Adverse Events (Safety Analysis Population)
| Adverse Events [n (%)] | Modal 40 mg Group (N=153) | Modal 80 mg Group (N=136) |
|---|---|---|
| Any adverse events | 71 (46.4) | 75 (55.1) |
| Common adverse eventsa | ||
| Akathisia | 14 (9.2) | 5 (3.7) |
| Nasopharyngitis | 7 (4.6) | 10 (7.4) |
| Schizophrenia | 9 (5.9) | 7 (5.1) |
| Insomnia | 6 (3.9) | 7 (5.1) |
| Nausea | 7 (4.6) | 5 (3.7) |
| Blood prolactin increased | 4 (2.6) | 7 (5.1) |
| Constipation | 3 (2.0) | 8 (5.9) |
| Headache | 3 (2.0) | 8 (5.9) |
| Anxiety | 4 (2.6) | 5 (3.7) |
| Back pain | 2 (1.3) | 4 (2.9) |
| Cough | 2 (1.3) | 4 (2.9) |
| Parkinsonism | 3 (2.0) | 3 (2.2) |
Notes: a≥2% in safety analysis population. Modal 40 mg group: Subjects who received 40 mg for most days during the extension phase. Modal 80 mg group: Subjects who received 80 mg for most days during the extension phase.
Table 3.
Mean Change from Open-Label Baseline to Week 12 in Weight and Laboratory Parameters (Safety Population)
| Modal 40 mg Group (N=153) | Modal 80 mg Group (N=136) | |||
|---|---|---|---|---|
| n | Mean (SD) Change | n | Mean (SD) Change | |
| Body weight (kg) | 126 | 0.37 (2.31) | 116 | −0.11 (2.70) |
| Fasting total cholesterol (mg/dL) | 117 | 4.6 (36.6) | 109 | 1.8 (30.0) |
| Fasting LDL cholesterol (mg/dL) | 117 | 2.2 (29.0) | 109 | −2.1 (24.3) |
| Fasting HDL cholesterol (mg/dL) | 117 | 1.8 (13.3) | 109 | 4.0 (11.0) |
| Fasting triglycerides (mg/dL) | 117 | 1.6 (70.9) | 109 | −0.8 (54.4) |
| Fasting blood glucose (mg/dL) | 117 | 2.4 (16.8) | 106 | −0.9 (12.9) |
| Blood prolactin, overall (μg/L) | 124 | 0.22 (12.00) | 112 | 3.01 (35.26) |
| Males | 64 | −0.27 (7.18) | 56 | −0.54 (11.22) |
| Females | 60 | 0.74 (15.64) | 56 | 6.55 (48.55) |
Notes: Modal 40 mg group: Subjects who received 40 mg for most days during the extension phase. Modal 80 mg group: Subjects who received 80 mg for most days during the extension phase.
Abbreviation: SD, standard deviation.
Among the subgroup that received a dose increase from 40 to 80 mg/d (N=166), the discontinuation rate was 18.1%, of which the discontinuation rate due to adverse events was 5.4%. The incidence of total adverse events was somewhat higher in the first 7 days after the dose of lurasidone was increased to 80 mg/d (Supplementary Table 3). However, the overall adverse event rate was relatively low after the dose increase, and no clear temporal pattern of onset was evident for individual adverse events (Supplementary Table 3).
Discussion
The current report provides novel data on the clinical decision to increase dosage from 40 to 80 mg/d over the course of 12-weeks of open-label extension treatment. Regarding efficacy, patients with schizophrenia who received a modal dose of 80 mg/d of lurasidone displayed continued improvement across the range of psychiatric outcome measures (including the PANSS positive and negative subscales, CDSS, and CGI-S) over the course of 12 weeks of open-label treatment that followed a 6-week double-blind trial. Changes from open-label baseline to week 12 (LOCF) on the PANSS subscale scores were numerically greater for patients treated with lurasidone 80 mg/d compared to 40 mg/d. In addition, a previous report on the extension phase found that the subgroup of patients who did not meet the response criteria (≥20% reduction in PANSS total score) during double-blind treatment with lurasidone 40 mg/d, had greater mean improvement from open-label baseline in PANSS total score when treated with a modal dose of 80 mg/d compared to patients treated with a modal dose of 40 mg/d. Similarly, greater improvement was also observed in both the subgroup that did not meet more stringent double-blind response criteria (≥30% reduction in PANSS total score) and the subgroup with an open-label baseline PANSS total score ≥80.16
In the ITT population, the positive, negative, and general psychopathology subscales of the PANSS all showed continued improvements during the extension phase in the modal 80 mg/d group. Both doses of lurasidone improved positive symptoms more than negative symptoms which is consistent with previous short-term double-blind trials.15,17–19 Of particular note, however, was that negative symptoms continued to improve when dosage was increased to 80 mg/d during 12-weeks of extension treatment that followed a 6-week double-blind trial.
It should be noted that the PANSS total and subscale score in this study tended to be higher at open-label baseline for the modal 80 mg/d group compared to the modal 40 mg/d group. This may have increased the response to 80 mg/d during the extension phase, particularly among patients who had an inadequate response during the double-blind study. This likelihood was supported by the fact that more patients in the lurasidone modal 80 mg/d group, compared to the modal 40 mg/d group, had an inadequate response to 40 mg/d in the double-blind phase (28 subjects in the modal 80 mg/d group and 11 subjects in the modal 40 mg/d group with <20% improvement in PANSS total score in the double-blind phase).
The effectiveness results presented here for lurasidone 80 mg/d and 40 mg/d doses are consistent with previous short-term efficacy data comparing 40 and 80 mg of lurasidone in the treatment of schizophrenia. A pooled analysis of short-term (6-week) studies of fixed doses of lurasidone for schizophrenia found significant improvement for both 40 mg/d and 80 mg/d compared with placebo, but the drug vs placebo effect size was greater for 80 mg/d than for 40 mg/d.30 Although the current report does not directly statistically compare the effects of 40 mg/d and 80 mg/d, the results of the pooled analysis30 taken together with the present analysis provide preliminary evidence for greater effectiveness of 80 mg/d compared to 40 mg/d in some patients. Given that a meta-analysis of various antipsychotics (lurasidone not included) indicated an increased risk of relapse at lower than standard doses,31 identifying the effective dose for patients with schizophrenia is an important clinical priority. Our results suggest that the optimal dose of lurasidone may vary among patients. In view of the current trend for personalization of medical care, the clinical recommendation for confirming the optimal dose of lurasidone should include increasing the dose to 80 mg/d if an adequate response to 40 mg/d has not been obtained. However, no randomized studies have been conducted to verify the dose-escalation effect from 40 mg/d to 80 mg/d, and such studies are needed to provide confirmation on the dose-escalation effect to 80 mg/d.
Safety/tolerability analyses revealed no increase in the rate of discontinuation due to adverse events in the modal dose of 80 mg/d group. Although adverse events occurred at a higher rate in the modal 80 mg/d group (55.1%) than in the modal 40 mg/d group (46.4%), there were not substantial differences between doses. In addition, the proportion of patients who increased to 80 mg/d and withdrew without dose reduction to 40 mg/d, and the incidence of each adverse event after the 80 mg/d dose increase, were not significantly different from the overall proportions. Further, there was no major trend in the time of onset for each individual adverse event after the dose was increased to 80 mg/d. Based on the results, there appears to be no major safety or tolerability problem when increasing the dose from 40 mg/d to 80 mg/d in the treatment of schizophrenia.
Limitations
The results of this study should be understood in the context of several limitations. A major limitation is that patients were not randomly assigned to the dose levels during the extension phase and therefore inferential statistical comparisons of the modal 40 mg/d and modal 80 mg/d were not conducted. In addition, because the design of the study included lurasidone 40 mg/d or placebo in the double-blind phase, followed by flexible dosing of 40 mg/d or 80 mg/d during the extension phase, no patients received a fixed dose of 80 mg/d throughout. Only a modal dose of 80 mg/d in the extension phase was examined and therefore the effectiveness and safety of a beginning at 80 mg/d and continuing at that dose was not assessed. Further, only patients who tolerated 40 mg/d (this may have limited the reporting of adverse events), and with an insufficient response to 40 mg/d, may have been included in the modal 80 mg/d group of this analysis. An additional limitation is that the assessment of PANSS subscales in the modal 80 mg/d group and safety assessment in the 80 mg/d dose-escalation group were post-hoc analyses not specified prior to the conduct of the study. A final limitation is that we do not know if the results of this study can be generalized to other types of patients, and other durations of treatment, because the study population consists of patients who met the specific inclusion and exclusion criteria and the duration of evaluation was only 12 weeks.
Conclusion
For patients with an acute exacerbation of schizophrenia, an increase of dose to 80 mg/d of lurasidone resulted in substantial improvement in multiple outcome measures, including negative symptoms, over the course of 12-weeks of extension phase treatment. In addition, extension phase treatment was well tolerated with both 40 mg/d and 80 mg/d doses. The percent of patients who were increased to 80 mg/d and withdrew without dose reduction to 40 mg/d, and the incidence of each adverse event after the 80 mg/d dose increase, were not significantly different from the overall proportions. These results suggest that increasing the dose of lurasidone from 40 mg/d to 80 mg/d may be a useful therapeutic option for selected patients with schizophrenia who do not achieve sufficient response after 6 weeks of treatment with a 40 mg/d dose.
Acknowledgments
We thank the patients and providers who participated in the study. We also thank Kentaro Takai, who is a member of Sumitomo Pharma Co., Ltd. and Masatoshi Nakamura, who is a former member of Sumitomo Pharma Co., Ltd. for providing support in performing the post-hoc analysis.
The original studies were sponsored by, and designed and analyzed by Sumitomo Pharma Co., Ltd. Sumitomo Pharma Co., Ltd owns the data and the participants of these studies consented to the use of anonymized data. Medical writing assistance was provided by Edward Schweizer, MD, of Paladin Consulting Group, Inc. (Princeton, NJ).
Funding Statement
This work was funded by Sumitomo Pharma Co., Ltd.
Data Sharing Statement
Sumitomo Pharma makes individual patient, de-identified data sets and associated clinical documents such as study protocol, statistical analysis plan and clinical study report available upon request via the Clinical Study Data Request site (https://www.clinicalstudydatarequest.com/ Study-Sponsors.aspx). Access is provided after a research proposal is submitted and has received approval from the Independent Review Panel and after a Data Sharing Agreement is in place. Access is provided for an initial period of 12 months, but an extension can be granted, when justified, for up to another 12 months.
Disclosure
Itaru Miura reports personal fees from Sumitomo Pharma Co., Ltd. Kei Watabe, Reiko Sakaguchi, Keisuke Okamoto, and Hidenori Maruyama are employees of Sumitomo Pharma. The authors report no other conflicts of interest in this work.
References
- 1.McCutcheon RA, Reis Marques T, Howes OD. Schizophrenia-an overview. JAMA Psychiatry. 2020;77(2):201–210. doi: 10.1001/jamapsychiatry.2019.3360 [DOI] [PubMed] [Google Scholar]
- 2.American Psychiatric Association. Schizophrenia spectrum and other psychotic disorders. In diagnostic and statistical manual of mental disorders; 2013. Available from: https://doi-org.ezproxy.frederick.edu/10.1176/appi.books.9780890425596.dsm03. Accessed October 25, 2022.
- 3.Simeone JC, Ward AJ, Rotella P, Collins J, Windisch R. An evaluation of variation in published estimates of schizophrenia prevalence from 1990─2013: a systematic literature review. BMC Psychiatry. 2015;15:193. doi: 10.1186/s12888-015-0578-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization. Schizophrenia fact sheet; 2019. Available from: https://www.who.int/news-room/fact-sheets/detail/schizophrenia. Accessed October 25, 2022.
- 5.Chong HY, Teoh SL, Wu DB, Kotirum S, Chiou CF, Chaiyakunapruk N. Global economic burden of schizophrenia: a systematic review. Neuropsychiatr Dis Treat. 2016;12:357–373. doi: 10.2147/NDT.S96649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lu L, Dong M, Zhang L, et al. Prevalence of suicide attempts in individuals with schizophrenia: a meta-analysis of observational studies. Epidemiol Psychiatr Sci. 2019;29:e39. doi: 10.1017/S2045796019000313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hjorthøj C, Stürup AE, McGrath JJ, Nordentoft M. Years of potential life lost and life expectancy in schizophrenia: a systematic review and meta-analysis [published correction appears in Lancet Psychiatry. Lancet Psychiatry. 2017;4(4):295–301. doi: 10.1016/S2215-0366(17)30078-0 [DOI] [PubMed] [Google Scholar]
- 8.Goff DC, Falkai P, Fleischhacker WW, et al. The long-term effects of antipsychotic medication on clinical course in schizophrenia. Am J Psychiatry. 2017;174(9):840–849. doi: 10.1176/appi.ajp.2017.16091016 [DOI] [PubMed] [Google Scholar]
- 9.Keepers GA, Fochtmann LJ, Anzia JM, et al. The American psychiatric association practice guideline for the treatment of patients with schizophrenia. Am J Psychiatry. 2020;177(9):868–872. doi: 10.1176/appi.ajp.2020.177901 [DOI] [PubMed] [Google Scholar]
- 10.Jääskeläinen E, Juola P, Hirvonen N, et al. A systematic review and meta-analysis of recovery in schizophrenia. Schizophr Bull. 2013;39(6):1296–1306. doi: 10.1093/schbul/sbs130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Green MF. Impact of cognitive and social cognitive impairment on functional outcomes in patients with schizophrenia. J Clin Psychiatry. 2016;77(Suppl 2):8–11. doi: 10.4088/JCP.14074su1c.02 [DOI] [PubMed] [Google Scholar]
- 12.Van Eck RM, Burger TJ, Vellinga A, Schirmbeck F, de Haan L. The relationship between clinical and personal recovery in patients with schizophrenia spectrum disorders: a systematic review and meta-analysis. Schizophr Bull. 2018;44(3):631–642. doi: 10.1093/schbul/sbx088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Caqueo-Urízar A, Urzúa A, Mena-Chamorro P, Bravo de la Fuente J. Effects of adherence to pharmacological treatment on the recovery of patients with schizophrenia. Healthcare. 2021;9(9):1230. doi: 10.3390/healthcare9091230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ishibashi T, Horisawa T, Tokuda K, et al. Pharmacological profile of lurasidone, a novel antipsychotic agent with potent 5-hydroxytryptamine 7 (5-HT7) and 5-HT1A receptor activity. J Pharmacol Exp Ther. 2010;334(1):171–181. doi: 10.1124/jpet.110.167346 [DOI] [PubMed] [Google Scholar]
- 15.Iyo M, Ishigooka J, Nakamura M, et al. Efficacy and safety of lurasidone in acutely psychotic patients with schizophrenia: a 6-week, randomized, double-blind, placebo-controlled study. Psychiatry Clin Neurosci. 2021;75(7):227–235. doi: 10.1111/pcn.13221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Iyo M, Ishigooka J, Nakamura M, et al. Safety and effectiveness of lurasidone in patients with schizophrenia: a 12-week, open-label extension study. Neuropsychiatr Dis Treat. 2021;17:2683–2695. doi: 10.2147/NDT.S320021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nasrallah HA, Silva R, Phillips D, et al. Lurasidone for the treatment of acutely psychotic patients with schizophrenia: a 6-week, randomized, placebo-controlled study. J Psychiatr Res. 2013;47(5):670–677. doi: 10.1016/j.jpsychires.2013.01.020 [DOI] [PubMed] [Google Scholar]
- 18.Meltzer HY, Cucchiaro J, Silva R, et al. Lurasidone in the treatment of schizophrenia: a randomized, double-blind, placebo- and olanzapine-controlled study. Am J Psychiatry. 2011;168(9):957–967. doi: 10.1176/appi.ajp.2011.10060907 [DOI] [PubMed] [Google Scholar]
- 19.Loebel A, Cucchiaro J, Sarma K, et al. Efficacy and safety of lurasidone 80 mg/d and 160 mg/d in the treatment of schizophrenia: a randomized, double-blind, placebo- and active-controlled trial. Schizophr Res. 2013;145(1–3):101–109. doi: 10.1016/j.schres.2013.01.009 [DOI] [PubMed] [Google Scholar]
- 20.Stahl SM, Cucchiaro J, Simonelli D, Hsu J, Pikalov A, Loebel A. Effectiveness of lurasidone for patients with schizophrenia following 6 weeks of acute treatment with lurasidone, olanzapine, or placebo: a 6-month, open-label, extension study. J Clin Psychiatry. 2013;74:507–515. doi: 10.4088/JCP.12m08084 [DOI] [PubMed] [Google Scholar]
- 21.Loebel A, Cucchiaro J, Xu J, Sarma K, Pilalov A, Kane JM. Effectiveness of lurasidone vs. quetiapine XR for relapse prevention in schizophrenia: a 12-month, double-blind, noninferiority study. Schizophr Res. 2013;147:95–102. doi: 10.1016/j.schres.2013.03.013 [DOI] [PubMed] [Google Scholar]
- 22.Correll CU, Cucchiaro J, Silva R, Hsu J, Pikalov A, Loebel A. Long-term safety and effectiveness of lurasidone in schizophrenia: a 22-month, open-label extension study. CNS Spectr. 2016;21:393–402. doi: 10.1017/S1092852915000917 [DOI] [PubMed] [Google Scholar]
- 23.Milev P, Ho BC, Arndt S, Andreasen NC. Predictive values of neurocognition and negative symptoms on functional outcome in schizophrenia: a longitudinal first-episode study with 7-year follow-up. Am J Psychiatry. 2005;162:495–506. doi: 10.1176/appi.ajp.162.3.495 [DOI] [PubMed] [Google Scholar]
- 24.Sheehan DV, Lecrubier Y, Sheehan KH, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(Suppl 20):22–33. [PubMed] [Google Scholar]
- 25.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Washington, DC: American Psychiatric Press; 2000. [Google Scholar]
- 26.Kay S, Fiszbein A, Opler L. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13:261–276. doi: 10.1093/schbul/13.2.261 [DOI] [PubMed] [Google Scholar]
- 27.Guy W. ECDEU Assessment Manual for Psychopharmacology (Revised). Rockville, MD: National Institute of Mental Health; 1976. [Google Scholar]
- 28.Posner K, Brown GK, Stanley B, et al. The Columbia-suicide severity rating scale: initial validity and internal consistency findings from three multisite studies with adolescents and adults. Am J Psychiatry. 2011;168:1266–1277. doi: 10.1176/appi.ajp.2011.10111704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Addington D, Addington J, Maticka-Tyndale E. Assessing depression in schizophrenia: the Calgary depression scale. Br J Psychiatry. 1993;163:39–44. doi: 10.1192/S0007125000292581 [DOI] [PubMed] [Google Scholar]
- 30.Loebel A, Cucchiaro J, Silva R, et al. Efficacy of lurasidone across five symptom dimensions of schizophrenia: pooled analysis of short-term, placebo-controlled studies. Eur Psychiatry. 2015;30(1):26–31. doi: 10.1016/j.eurpsy.2014.08.001 [DOI] [PubMed] [Google Scholar]
- 31.Højlund M, Kemp AF, Haddad PM, Neill JC, Correll CU. Standard versus reduced dose of antipsychotics for relapse prevention in multi-episode schizophrenia: a systematic review and meta-analysis of randomised controlled trials. Lancet Psychiatry. 2021;8(6):471–486. doi: 10.1016/S2215-0366(21)00078-X [DOI] [PubMed] [Google Scholar]