Abstract
Simple Summary
Early, intermediate, and late-onset gastric cancer (EOGC, IOGC, LOGC) incidence and death rates differed globally, regionally, and nationally in 2019. From 1990 to 2019, EOGC showed a slower decrease in incidence rate worldwide than IOGC and LOGC, whereas EOGC and LOGC showed slower decreases in mortality than IOGC. The worldwide incidence rate of EOGC was predicted to increase substantially from 2020 to 2035, while that for LOGC was predicted to increase slightly and that for IOGC was predicted to remain stable over the same period. This study revealed significant differences in the burdens and temporal trends of EOGC, IOGC, and LOGC, and highlighted the importance of tailored cancer-control measures in neglected subpopulations, especially in patients with EOGC.
Abstract
Background: Evidence for estimating and predicting the temporal trends of gastric cancer in different age groups is lacking. Methods: Data of early-, intermediate-, and later-onset gastric cancer (EOGC, IOGC, LOGC) was from the Global Burden of Diseases Study 2019. The incidences and deaths due to EOGC, IOGC, and LOGC were analyzed by period, sex, geographic location, and sociodemographic incidence. Temporal trends were evaluated by estimated annual percentage changes (EAPCs). The incidences and temporal trends were predicted until 2035. Results: There were substantial differences in the incidence and death rates of the three populations at global, regional and national levels in 2019. From 1990 to 2019, EOGC (EAPC, −0.84) showed a slower decrease in incidence rate worldwide than IOGC (EAPC, −1.77) and LOGC (EAPC, −1.10), whereas EOGC and LOGC showed slower decreases in mortality than IOGC. The worldwide incidence rate of EOGC (EAPC, 1.44) was predicted to increase substantially from 2020 to 2035, while that for LOGC (EAPC, 0.43) was predicted to increase slightly and that for IOGC (EAPC, −0.01) was predicted to remain stable over the same period. Conclusions: This study revealed differences in the burdens and temporal trends of EOGC, IOGC, and LOGC, and highlighted the importance of tailored cancer-control measures in neglected subpopulations, especially in patients with EOGC.
Keywords: epidemiology, gastric cancer, temporal trend, prediction
1. Introduction
Gastric cancer remains an important cancer, with the fifth-highest incidence and fourth-highest mortality globally [1]. Despite steady declines in the incidence rate of gastric cancer over the last half century in many parts of the world, the incidence of early-onset gastric cancer (EOGC), diagnosed at age < 50 years, has been predicted to increase in both low- and high-risk countries in the next decade [2,3]. The reasons for the rise among young adults remain unknown but may be related to the rising prevalence of autoimmune gastritis, dysbiosis of the gastric microbiome, and the increased use of antibiotics among younger generations [4,5]. This rise in EOGC, together with various early-onset cancers in other organs, has attracted growing global concern [6].
Whether gastric cancer among younger adults represents a distinct disease from that in elderly adults is an important clinical issue. Gastric cancer among younger adults appears to be genetically and clinically distinct from traditional gastric cancer, and is associated with a more-diffuse histology, poor differentiation, and more peritoneal metastasis. Differences in the incidence and death rates among gastric cancers in different age groups are also unclear; for example, EOGC diagnosed at age <50 years, intermediate-onset gastric cancer (IOGC) diagnosed at age 50–54 years, and later-onset gastric cancer (LOGC) at age ≥55 years. Furthermore, the incidence and death rates of EOGC, IOGC, and LOGC have not been systematically estimated and predicted, especially at regional and national levels [7,8].
Based on the Global Burden of Disease (GBD) Study 2019 [9,10], we analyzed the incidences, deaths, and temporal trends of EOGC, IOGC, and LOGC from 1990 to 2019 at global, regional, and national levels in relation to period, sex, geographic location, and sociodemographic index (SDI). We also predicted the future incidences, deaths, and temporal trends at global and national levels from 2020 to 2035.
2. Materials and Methods
2.1. Definitions of EOGC, IOGC, and LOGC
All cases coded as C16–C16.9, Z12.0, and Z85.02–Z85.028 in the International Classification of Diseases 10th Revision (ICD–10) were considered to be gastric cancer [10,11]. In this cross-sectional study, EOGC was defined as gastric cancer diagnosed at age 15–49 years, IOGC as gastric cancer diagnosed at age 50–54 years, and LOGC as gastric cancer diagnosed at age ≥ 55 years.
2.2. Data Sources
Based on geographical locations, the GBD 2019 was grouped into 21 regions or 203 countries. All countries were further grouped into low-, low-middle-, middle-, high-middle-, and high-SDI regions [12]. The burdens and temporal trends in EOGC, IOGC, and LOGC were analyzed in relation to the 21 GBD regions, five SDI regions, and 203 countries, respectively. We extracted data from the GBD 2019 Data Resources (https://ghdx.healthdata.org/gbd-2019) (accessed on 18 January 2022) between 1990 and 2019 using the Global Health Data Exchange tool (GHDx).
This study was approved by the Institutional Ethics Committees of The Fourth Affiliated Hospital of China Medical University (EC–2021–KS–068) and was performed according to the guidelines of the Declaration of Helsinki. This study was reported according to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines [13].
2.3. Statistical Analysis
The incidences, deaths, and corresponding rates of EOGC, IOGC, and LOGC between 2019 and 1990 were estimated at global, regional, and national levels. The estimated annual percentage change (EAPC) was calculated to quantify time trends in incidence and death rates using Joinpoint software (version 4.7.0.0; National Cancer Institute, Rockville, MD, USA) and R version 4.1.2 (R Foundation for Statistical Computing, Vienna, Austria).
The expected relationships between SDI values and incidence and death rates were determined by fitting a Gaussian process regression to estimates at global, regional, and national levels from 1990 to 2019. The correlation between the EAPCs for incidence and death rates and SDI values in 2019 were further evaluated by Pearson’s correlation analyses.
Based on the GBD data from 2004 to 2019, we applied a Bayesian age–period–cohort model to predict the incidence rates from 2020 to 2035 at worldwide and national levels. The quality of data for each country was classified from 0–5 stars, as described previously [14,15]. We selected 12 study countries with high-quality data (3–5 stars).
Further details are provided in the Supplementary Methods.
3. Results
3.1. Burdens of EOGC, IOGC, and LOGC in 2019 vs. 1990
3.1.1. Global Burdens
Globally, there were 144,321 incident cases of EOGC in 2019 compared with 125,974 cases in 1990, with incidence rates of 3.7 and 4.6 per 100,000, respectively (Table 1; Figure 1A). For IOGC, there were 92,619 incident cases in 2019 and 74,469 cases in 1990, with respective incidence rates of 21.2 and 35.0 per 100,000. There were 1,032,865 incident cases of LOGC in 2019 and 682,952 cases in 1990, and the incidence rates were 101.8 and 73.5 per 100,000, respectively.
Table 1.
Incidences and temporal trends in gastric cancers globally and by sex, and SDI and GBD regions, 1990–2019.
| Population | 1990 | 2019 | 1990–2019 | ||
|---|---|---|---|---|---|
| Incidence Cases | IR (per 100,000) | Incidence Cases | IR (per 100,000) | EAPC | |
| No. (95% UI) | No. (95% UI) | No. (95% UI) | No. (95% UI) | No. (95% CI) | |
| Global | |||||
| EOGC | 125,974 (118,140–133,956) | 4.6 (4.4–4.9) | 144,321 (130,473–158,789) | 3.7 (3.3–4.0) | −0.84 * (−0.99 to −0.69) |
| IOGC | 74,469 (69,424–79,643) | 35.0 (32.7–37.5) | 92,619 (81,908–104,377) | 21.2 (18.8–23.9) | −1.77 * (−2.03 to −1.50) |
| LOGC | 682,952 (645,714–718,165) | 101.8 (96.2–107.0) | 1,032,865 (934,144–1,135,210) | 73.5 (66.4–80.8) | −1.10 * (−1.25 to −0.95) |
| Sex | |||||
| Male | |||||
| EOGC | 73,551 (67,773–79,096) | 5.4 (4.9–5.8) | 90,805 (79,515–103,618) | 4.6 (4.0–5.2) | −0.44 * (−0.65 to −0.24) |
| IOGC | 50,923 (46,691–55,835) | 47.3 (43.4–51.9) | 64,844 (54,890–76,597) | 29.8 (25.2–35.2) | −1.56 * (−1.86 to −1.25) |
| LOGC | 423,665 (395,052–453,227) | 136.2 (127.0–145.7) | 691,222 (610,582–782,032) | 104.4 (92.2–118.1) | −0.85 * (−1.00 to −0.69) |
| Female | |||||
| EOGC | 52,423 (47,705–57,109) | 3.9 (3.6–4.3) | 53,516 (47,850–59,347) | 2.8 (2.5–3.1) | −1.45 * (−1.61 to −1.29) |
| IOGC | 23,545 (21,572–25,377) | 22.4 (20.6–24.2) | 27,775 (24,563–31,158) | 12.7 (11.2–14.2) | −2.15 * (−2.36 to −1.93) |
| LOGC | 259,287 (241,989–275,659) | 72.0 (67.2–76.6) | 341,643 (301,534–380,296) | 45.9 (40.5–51.1) | −1.62 * (−1.77 to −1.47) |
| Sociodemographic index (SDI) | |||||
| High SDI | |||||
| EOGC | 24,633 (24,089–25,167) | 5.7 (5.6–5.9) | 14,042 (12,929–15,275) | 3.0 (2.8–3.3) | −2.41 * (−2.49 to −2.32) |
| IOGC | 14,382 (13,895–14,824) | 33.0 (31.8–34.0) | 9392 (8471–10,436) | 13.7 (12.3–15.2) | −3.24 * (−3.33 to −3.15) |
| LOGC | 188,546 (180,270–192,729) | 107.4 (102.6–109.7) | 214,329 (187,179–235,870) | 68.8 (60.1–75.7) | −1.73 * (−1.80 to −1.65) |
| High-middle SDI | |||||
| EOGC | 35,030 (32,515–37,646) | 5.8(5.4–6.2) | 40,349 (35,304–45,650) | 5.5 (4.8–6.3) | −0.34 * (−0.51 to −0.16) |
| IOGC | 24,921 (23,304–26,742) | 44.1 (41.3–47.4) | 26,927 (22,777–31,567) | 26.4 (22.3–31.0) | −1.75 * (−2.08 to −1.41) |
| LOGC | 231,643 (218,770–244,500) | 125.1 (118.2–132.0) | 313,798 (278,349–351,211) | 88.5 (78.5–99.0) | −1.17 * (−1.37 to −0.97) |
| Middle SDI | |||||
| EOGC | 41,707 (37,520–46,082) | 4.6 (4.2–5.1) | 54,282 (47,259–61,912) | 4.3 (3.7–4.9) | −0.18 (−0.42 to 0.06) |
| IOGC | 23,115 (20,358–26,278) | 38.0 (33.5–43.2) | 37,838 (31,791–44,635) | 24.6 (20.7–29.1) | −1.53 * (−1.93 to −1.13) |
| LOGC | 186,596 (168,262–207,174) | 108.4 (97.7–120.3) | 366,101 (319,384–48,858) | 85.4 (74.5–97.7) | −0.64 * (−0.89 to −0.39) |
| Low-middle SDI | |||||
| EOGC | 18,731 (16,680–20,404) | 3.5 (3.1–3.8) | 26,153 (23,536–28,918) | 2.8 (2.5–3.1) | −0.70 * (−0.80 to −0.59) |
| IOGC | 9267 (8327–10,233) | 25.2 (22.6–27.8) | 14,138 (12,502–15,857) | 17.7 (15.7–19.9) | −1.29 * (−1.41 to −1.17) |
| LOGC | 57,799 (53,087–62,058) | 58.4 (53.6–62.7) | 108,896 (99,437–118,824) | 47.9 (43.7–52.3) | −0.66 * (−0.76 to −0.57) |
| Low SDI | |||||
| EOGC | 5836 (4921–6622) | 2.5 (2.1–2.8) | 9442 (8062–10,865) | 1.7 (1.5–2.0) | −1.28 * (−1.30 to −1.25) |
| IOGC | 2766 (2379–3127) | 18.7 (16.1–21.2) | 4296 (3674–4949) | 13.2 (11.3–15.2) | −1.35 * (−1.44 to −1.26) |
| LOGC | 18,167 (16,102–20,132) | 46.8 (41.5–51.9) | 29,451 (26,698–32,482) | 35.5 (32.2–39.2) | −0.97 * (−1.02 to −0.92) |
| GBD regions | |||||
| Andean Latin America | |||||
| EOGC | 985 (889–1096) | 5.3 (4.8–5.9) | 1511 (1177–1918) | 4.6 (3.6–5.8) | −0.62 * (−0.82 to −0.42) |
| IOGC | 429 (373–491) | 37.4 (32.5–42.7) | 702 (527–922) | 23.4 (17.6–30.8) | −1.58 * (−1.71 to −1.44) |
| LOGC | 4561 (4139–4987) | 135.7 (123.2–148.4) | 10,161 (8347–12,276) | 108.3 (89.0–130.9) | −0.77 * (−0.87 to −0.66) |
| Australasia | |||||
| EOGC | 211 (198–226) | 2.0 (1.8–2.1) | 242 (186–310) | 1.8 (1.4–2.3) | −0.24 * (−0.35 to −0.13) |
| IOGC | 114 (104–127) | 12.0 (10.8–13.3) | 147 (106–203) | 8.1 (5.8–11.1) | −1.30 * (−1.46 to −1.13) |
| LOGC | 2057 (1953–2147) | 52.2 (49.6–54.5) | 3060 (2451–3739) | 37.2 (29.8–45.4) | −1.47 * (−1.59 to −1.35) |
| Caribbean | |||||
| EOGC | 409 (349–453) | 2.2 (1.9–2.5) | 535 (432–644) | 2.2 (1.8–2.7) | 0.00 (−0.07 to 0.07) |
| IOGC | 211 (184–242) | 16.2 (14.1–18.6) | 335 (270–408) | 12.2 (9.9–14.9) | −0.69 * (−0.81 to −0.58) |
| LOGC | 2303 (2117–2434) | 53.3 (49.0–56.3) | 3486 (3023–3982) | 39.5 (34.2–45.1) | −0.93 * (−1.04 to −0.82) |
| Central Asia | |||||
| EOGC | 2161 (2077–2244) | 6.5 (6.2–6.7) | 1974 (1765–2230) | 4.0 (3.6–4.6) | −2.19 * (−2.40 to −1.98) |
| IOGC | 1618 (1537–1694) | 54.4 (51.7–57.0) | 1158 (1009–1341) | 24.2 (21.1–28.0) | −2.81 * (−2.92 to −2.69) |
| LOGC | 9613 (9274–9907) | 120.6 (116.3–124.3) | 8994 (8146–9923) | 69.1 (62.6–76.2) | −1.82 * (−1.94 to −1.69) |
| Central Europe | |||||
| EOGC | 2511 (2452–2570) | 4.1 (4.0–4.2) | 1460 (1262–1678) | 2.8 (2.4–3.2) | −1.85 * (−2.03 to −1.66) |
| IOGC | 1790 (1724–1863) | 26.0 (25.0–27.1) | 1113 (948–1299) | 14.9 (12.7–17.4) | −1.91 * (−2.05 to −1.77) |
| LOGC | 22,154 (21,540–22,588) | 84.8 (82.4–86.4) | 19,143 (16,883–19,143) | 52.6 (46.4–59.1) | −1.75 * (−1.83 to −1.66) |
| Central Latin America | |||||
| EOGC | 2590 (2515–2663) | 3.2 (3.1–3.3) | 4707 (3923–5598) | 3.6 (3.0–4.3) | 0.25 * (0.16 to 0.35) |
| IOGC | 1128 (1080–1176) | 23.2 (22.2–24.2) | 2239 (1859–2706) | 17.3 (14.3–20.9) | −1.14 * (−1.22 to −1.05) |
| LOGC | 11,778 (11,245–12,127) | 86.5 (82.6–89.0) | 23,563 (20,089–27,595) | 59.0 (50.3–69.1) | −1.66 * (−1.77 to −1.55) |
| Central sub-Saharan Africa | |||||
| EOGC | 544 (412–698) | 2.2 (1.7–2.9) | 905 (673–1187) | 1.5 (1.1–1.9) | −1.54 * (−1.61 to −1.46) |
| IOGC | 306 (224–406) | 20.7 (15.1–27.4) | 498 (353–678) | 13.2 (9.4–18.0) | −1.59 * (−1.67 to −1.52) |
| LOGC | 1875 (1552–2241) | 49.4 (40.9–59.0) | 2846 (2308–3538) | 33.3 (27.0–41.3) | −1.46 * (−1.55 to −1.37) |
| East Asia | |||||
| EOGC | 49,305 (42,924–56,328) | 7.1 (6.2–8.2) | 68,382 (56,611–81,595) | 9.2 (7.6–10.9) | 0.98 * (0.69 to 1.27) |
| IOGC | 29,578 (25,111–34,639) | 59.3 (50.3–69.5) | 50,893 (41,026–62,257) | 39.5 (31.8–48.3) | −1.30 * (−1.75 to −0.84) |
| LOGC | 246,831 (217,625–277,992) | 164.6 (145.1–185.4) | 507,214 (428,407–597,285) | 139.3 (117.6–164.0) | −0.32 (−0.67 to 0.03) |
| Eastern Europe | |||||
| EOGC | 9948 (9280–10,298) | 9.0 (8.4–9.3) | 6053 (5379–6793) | 6.2 (5.5–6.9) | −2.26 * (−2.66 to −1.87) |
| IOGC | 9558 (9066–9932) | 60.3 (57.2–62.6) | 3525 (3098–4038) | 27.2 (23.9–31.2) | −3.34 * (−3.66 to −3.02) |
| LOGC | 67,527 (65,586–68,832) | 138.1 (134.2–140.8) | 44,541 (40,280–49,271) | 72.0 (65.1–79.6) | −2.62 * (−2.81 to −2.42) |
| Eastern sub-Saharan Africa | |||||
| EOGC | 1917 (1532–2213) | 2.3 (1.8–2.7) | 2711 (2257–3265) | 1.4 (1.1–1.6) | −2.14 * (−2.27 to −2.01) |
| IOGC | 868 (736–1004) | 18.7 (15.8–21.6) | 1127 (936–1341) | 10.7 (8.9–12.7) | −2.16 * (−2.25 to −2.06) |
| LOGC | 5449 (4774–6059) | 44.8 (39.3–49.8) | 7917 (7025–8913) | 30.7 (27.2–34.6) | −1.44 * (−1.52 to −1.37) |
| High-income Asia Pacific | |||||
| EOGC | 16,695 (16,188–17,190) | 18.0 (17.4–18.5) | 6408 (5628–7283) | 7.9 (6.9–9.0) | −3.08 * (−3.23 to −2.92) |
| IOGC | 9563 (9133–9981) | 92.0 (87.9–96.0) | 4235 (3569–4926) | 31.2 (26.3–36.3) | −3.80 * (−3.97 to −3.64) |
| LOGC | 97,474 (93,352–99,971) | 278.6 (266.8–285.7) | 117,525 (98,815–135,906) | 169.8 (142.8–196.3) | −1.84 * (−1.90 to −1.77) |
| High-income North America | |||||
| EOGC | 2493 (2423–2554) | 1.7 (1.6–1.7) | 2785 (2405–3259) | 1.7 (1.4–2.0) | −0.17 (−0.39 to 0.05) |
| IOGC | 1298 (1254–1343) | 10.2 (9.8–10.5) | 1872 (1578–2211) | 8.0 (6.8–9.5) | −0.76 * (−0.84 to −0.68) |
| LOGC | 26,528 (25,281–27,293) | 45.6 (43.5–47.0) | 32,927 (28,746–37,397) | 30.4 (26.6–34.6) | −1.82 * (−1.96 to −1.67) |
| North Africa and Middle East | |||||
| EOGC | 4441 (3843–4988) | 2.7 (2.4–3.1) | 7272 (6171–8484) | 2.2 (1.8–2.5) | −0.84 * (−1.14 to −0.54) |
| IOGC | 2226 (1779–2407) | 20.7 (17.4–23.5) | 3672 (3153–4263) | 13.2 (11.3–15.3) | −1.53 * (−1.77 to −1.30) |
| LOGC | 16,928 (14,683–18,502) | 59.1 (51.2–64.5) | 31,315 (28,294–34,373) | 43.9 (39.7–48.2) | −0.90 * (−1.06 to −0.74) |
| Oceania | |||||
| EOGC | 126 (95–158) | 4.0 (3.0–5.0) | 294 (212–392) | 4.3 (3.1–5.8) | 0.38 * (0.29 to 0.48) |
| IOGC | 41 (29–56) | 21.4 (15.4–29.1) | 100 (69–139) | 19.7 (13.5–27.4) | −0.19 * (−0.25 to −0.13) |
| LOGC | 252 (200–309) | 52.1 (41.3–63.8) | 543 (423–679) | 47.9 (37.3–59.8) | −0.40 * (−0.47 to −0.32) |
| South Asia | |||||
| EOGC | 14,580 (12,912–16,083) | 2.8 (2.4–3.0) | 21,127 (18,261–24,233) | 2.2 (1.9–2.5) | −0.81 * (−0.90 to −0.73) |
| IOGC | 6075 (5300–6752) | 16.8 (14.7–18.7) | 9650 (8097–11,374) | 12.1 (10.2–14.3) | −1.16 * (−1.44 to −0.88) |
| LOGC | 36,919 (33,052–40,694) | 39.6 (35.4–43.6) | 68,622 (60,511–78,365) | 29.2 (25.8–33.4) | −1.15 * (−1.23 to −1.06) |
| Southeast Asia | |||||
| EOGC | 5693 (4810–6437) | 2.4 (2.0–2.7) | 6354 (5397–7407) | 1.8 (1.5–2.0) | −1.32 * (−1.48 to −1.16) |
| IOGC | 2728 (2339–3126) | 17.2 (14.8–19.7) | 3728 (3151–4364) | 9.7 (8.2–11.4) | −2.05 * (−2.11 to −2.00) |
| LOGC | 19,648 (16,960–21,782) | 46.4 (40.0–51.4) | 29,973 (26,787–33,361) | 28.6 (25.6–31.9) | −1.92 * (−2.02 to −1.83) |
| Southern Latin America | |||||
| EOGC | 845 (810–885) | 3.5 (3.3–3.6) | 916 (704–1197) | 2.7 (2.1–3.5) | −0.88 * (−0.98 to −0.78) |
| IOGC | 536 (500–576) | 24.4 (22.7–26.2) | 583 (425–790) | 15.9 (11.6–21.5) | −1.31 * (−1.40 to −1.22) |
| LOGC | 7075 (6817–7297) | 89.3 (86.1–92.2) | 9195 (7372–11,407) | 65.0 (52.1–80.7) | −1.18 * (−1.27 to −1.09) |
| Southern sub-Saharan Africa | |||||
| EOGC | 562 (514–608) | 2.2 (2.0–2.3) | 619 (522–728) | 1.5 (1.2–1.7) | −1.75 * (−2.06 to −1.43) |
| IOGC | 221 (196–250) | 14.4 (12.8–16.4) | 311 (262–372) | 9.7 (8.1–11.5) | −1.32 * (−1.74 to −0.90) |
| LOGC | 1636 (1465–1795) | 36.3 (32.5–39.9) | 2680 (2476–2912) | 28.4 (26.3–30.9) | −1.03 * (−1.43 to −0.63) |
| Tropical Latin America | |||||
| EOGC | 2493 (2410–2578) | 3.2 (3.1–3.3) | 3064 (2911–3226) | 2.6 (2.4–2.7) | −0.73 * (−0.87 to −0.60) |
| IOGC | 1417 (1351–1493) | 26.8 (25.6–28.3) | 1864 (1749–1990) | 14.4 (13.5–15.3) | −2.06 * (−2.14 to −1.99) |
| LOGC | 12,199 (11,659–12,610) | 80.7 (77.1–83.4) | 19,609 (18,270–20,572) | 47.0 (43.8–49.3) | −1.99 * (−2.10 to −1.88) |
| Western Europe | |||||
| EOGC | 6143 (6008–6270) | 3.2 (3.1–3.2) | 4612 (3924–5399) | 2.4 (2.1–2.8) | −0.97 * (−1.13 to −0.81) |
| IOGC | 4129 (3966–4295) | 18.0 (17.3–18.7) | 3601 (3031–4261) | 11.2 (9.4–13.2) | −1.59 * (−1.66 to −1.53) |
| LOGC | 83,680 (79,788–85,815) | 86.1 (82.1–88.3) | 78,242 (67,832–88,026) | 54.1 (46.9–60.9) | −1.72 * (−1.79 to −1.65) |
| Western sub-Saharan Africa | |||||
| EOGC | 1321 (1109–1516) | 1.6 (1.3–1.8) | 2389 (1933–2896) | 1.1 (0.9–1.3) | −1.06 * (−1.13 to −0.99) |
| IOGC | 742 (618–872) | 14.2 (11.8–16.7) | 1266 (1022–1552) | 9.9 (8.0–12.2) | −1.07 * (−1.12 to −1.03) |
| LOGC | 6465 (5634–7235) | 45.0 (39.2–50.4) | 11,307 (9863–12,868) | 37.4 (32.6–42.5) | −0.43 * (−0.52 to −0.33) |
CI, confidence interval; EAPC, estimated annual percentage change; EOGC, early-onset gastric cancer (15–49 years); IR, incidence rate; IOGC, intermediate-onset gastric cancer (50–54 years); LOGC, later-onset gastric cancer (≥55 years); UI, uncertainty interval. * Indicates statistical significance.
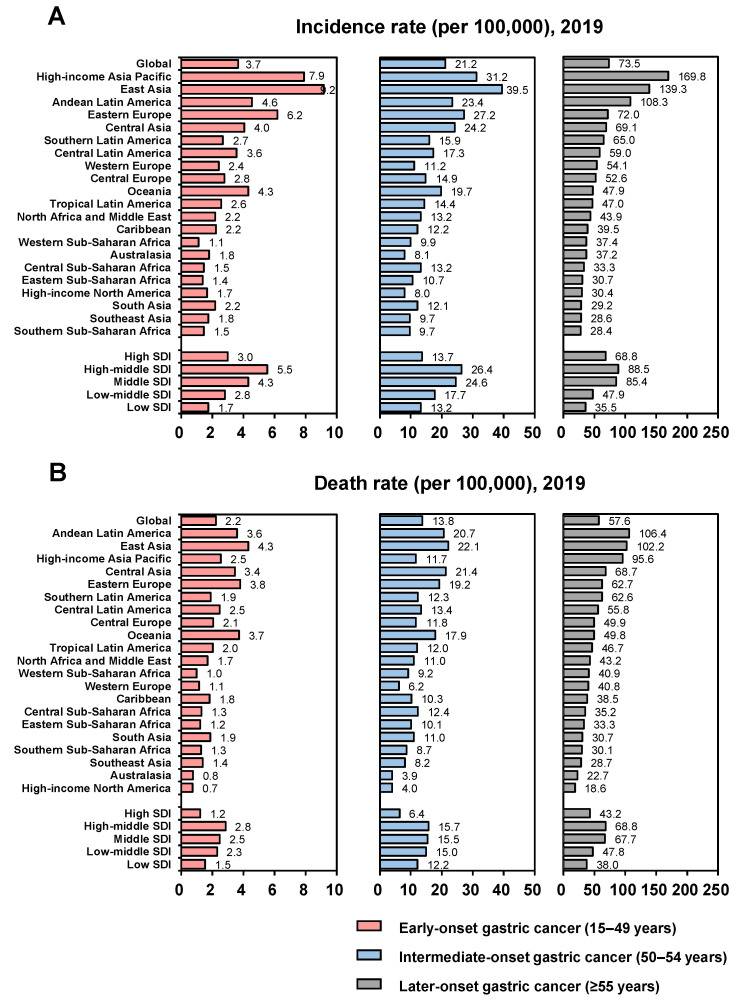
Figure 1.
Incidence and death rates globally and by SDI and GBD regions in 2019. (A) Incidence rates globally and by SDI and GBD regions in 2019; (B) Death rates globally and by SDI and GBD regions in 2019.
The global numbers of deaths due to EOGC were 87,333 in 2019 and 97,383 in 1990, corresponding to death rates of 2.2 and 3.6 per 100,000, respectively (Table S1; Figure 1B). The corresponding figures for IOGC were 60,169 deaths in 2019 and 60,688 in 1990, with respective death rates of 13.8 and 28.5 per 100,000, and the numbers for LOGC were 809,683 deaths in 2019 compared with 630,247 in 1990, with death rates of 57.6 and 93.9 per 100,000, respectively. The incidence and death rates in relation to sex are presented in Figures S1 and S2.
3.1.2. Regional Burdens
In 2019, the highest incidence rate of EOGC was in East Asia (9.2 per 100,000), followed by high-income Asia Pacific, and the highest death rate was also found in East Asia (4.3 per 100,000), followed by Eastern Europe (Table 1; Figure 1). The highest incidence rate of IOGC was also in East Asia (39.5 per 100,000), followed by high-income Asia Pacific, while the highest death rate was in East Asia (22.1 per 100,000), followed by Central Asia. The highest incidence rate of LOGC was in high-income Asia Pacific (169.8 per 100,000), followed by East Asia, whereas the highest death rate was in Andean Latin America (106.4 per 100,000), followed by East Asia. The highest incidence and death rates of EOGC, IOGC, and LOGC in 2019 were all in high-middle SDI regions in 2019. The incidence and death rates in the 21 GBD regions in relation to sex are presented in Figures S1 and S2.
3.1.3. National Burdens
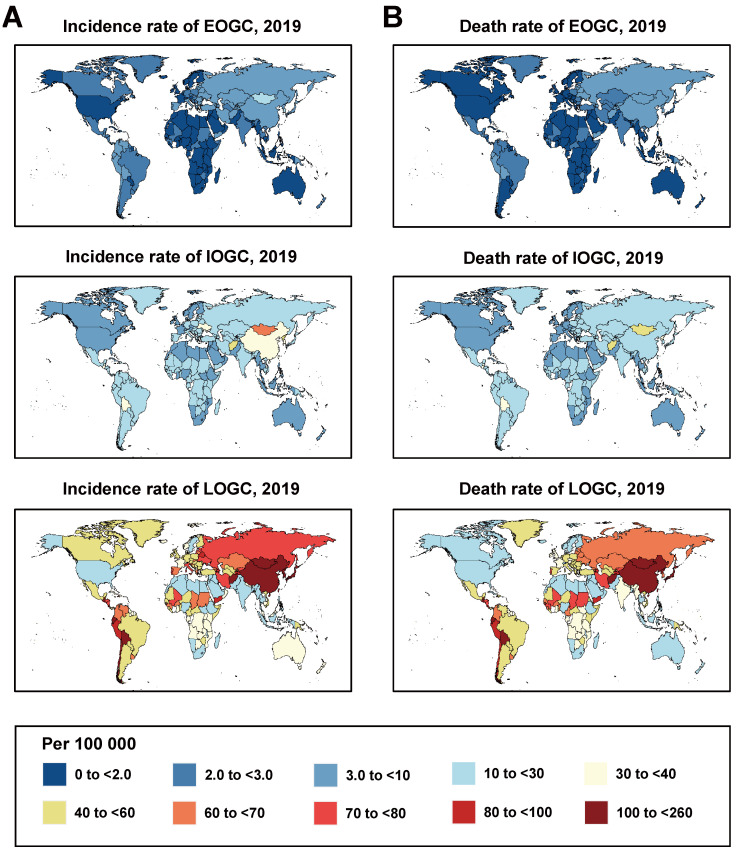
The burdens of EOGC, IOGC, and LOGC varied widely among countries and between sexes (Figure 2 and Figures S3 and S4; Tables S2–S7). In 2019, the highest incidence rate of EOGC was in the Solomon Islands (10.7 per 100,000), followed by Mongolia, and the highest death rate was in Mongolia (9.3 per 100,000), followed by the Solomon Islands. For IOGC, the highest incidence rate (64.1 per 100,000) and death rate (58.0 per 100,000) were in Mongolia, followed by Afghanistan, while the highest incidence rate of LOGC was in Japan (185.7 per 100,000), followed by Mongolia, and the highest death rate was in Mongolia (181.1 per 100,000), followed by Bolivia.
Figure 2.
Incidence and death rates of gastric cancer globally in 2019. (A) Incidence rates of gastric cancer globally in 2019; (B) Death rates of gastric cancer globally in 2019.
3.2. Temporal Trends of EOGC, IOGC, and LOGC, 1990–2019
3.2.1. Global Trends
From 1990 to 2019, the incidence rates of EOGC (EAPC, −0.84; 95% CI, −0.99 to −0.69), IOGC (EAPC, −1.77; 95% CI, −2.03 to −1.50), and LOGC (EAPC, −1.10; 95% CI, −1.25 to −0.95) showed overall decreasing trends worldwide, and the death rates of EOGC (EAPC, −1.78; 95% CI, −2.00 to −1.57), IOGC (EAPC, −2.55; 95% CI, −2.85 to −2.26) and LOGC (EAPC, −1.69; 95% CI, −1.88 to −1.51) also presented overall decreasing trends in the same period (Table 1 and Table S1; Figures S5–S10).
3.2.2. Regional Trends
The incidence and death rates of EOGC, IOGC, and LOGC decreased in all five SDI regions from 1990 to 2019 (Table 1 and Tables S8 and S9; Figures S5–S10). The greatest decreases in incidence rates of EOGC (EAPC, −2.41; 95% CI, −2.49 to −2.32), IOGC (EAPC, −3.24; 95% CI, −3.33 to −3.15), and LOGC (EAPC, −1.73; 95% CI, −1.80 to −1.65) occurred in high-SDI regions, while the death rates (EOGC: EAPC, −3.31; 95% CI, −3.40 to −3.22; IOGC: EAPC, −3.81; 95% CI, −3.94 to −3.68; LOGC: EAPC, −2.16; 95% CI, −2.23 to −2.10) also decreased most in high-SDI regions. The incidence and death rates in SDI regions during specific periods are presented in Tables S8–S9.
From 1990 to 2019, the incidence and death rates of EOGC showed overall downward trends in most GBD regions (Table 1 and Tables S10 and S11; Figures S11–S16). The incidence rate of EOGC decreased most from 1990 to 2019 in high-income Asia Pacific (EAPC, −3.08; 95% CI, −3.23 to −2.92), followed by Eastern Europe, and increased most in East Asia (EAPC, 0.98; 95% CI, 0.69−1.27). The death rate of EOGC also decreased most in high-income Asia Pacific (EAPC, −4.45; 95% CI, −4.62 to −4.28), followed by Eastern Europe, with only Oceania (EAPC, 0.41; 95% CI, 0.30–0.51) showing an upward trend from 1990 to 2019. The incidence and death rates of IOGC and LOGC showed overall declining trends from 1990 to 2019 in all regions. Both the incidence rate (EAPC, −3.80; 95% CI, −3.97 to −3.64) and death rate (EAPC, −4.75; 95% CI, −4.88 to −4.62) of IOGC decreased most in high-income Asia Pacific, followed by Eastern Europe, while the greatest decreasing trend in the incidence rate of LOGC was in Eastern Europe (EAPC, −2.62; 95% CI, −2.81 to −2.42), followed by tropical Latin America, and the largest decreasing trend in death rate was in high-income North America (EAPC, −2.37; 95% CI, −2.51 to −2.22), followed by Western Europe. The temporal trends in incidence and death rates of EOGC, IOGC, and LOGC in relation to SDI and GBD regions during specific periods are shown in Tables S10 and S11.
3.2.3. National Trends
We further analyzed the temporal trends of incidence and death rates of EOGC, IOGC, and LOGC in 203 countries from 1990 to 2019, and substantial differences were also found at the national level (Tables S12 and S13).
3.3. Impact of SDI on Incidence and Death Rates, 1990–2019
The relationship between the global- and regional-level incidence and death rates and SDI values are shown in Figure S17. At the global level, the incidence and death rates of EOGC, IOGC, and LOGC all showed decreasing trends with increasing SDI values. The incidence and death rates of EOGC showed decreasing trends with increasing SDI values in most regions; however, there were variations, with Western sub-Saharan Africa and Eastern Europe showing the largest decreases in incidence rates with increasing SDI values, and East Asia and Oceania showing increasing trends in incidence rates. Similarly, Western sub-Saharan Africa and Eastern Europe showed the largest decreases in death rates with increasing SDI values, and only Oceania showed an increasing trend. The incidence and death rates of IOGC and LOGC in all regions showed decreasing trends with increasing SDI values. The relationships between SDI values and incidence and death rates in relation to sex are shown in Figures S18 and S19.
The relationships between incidence and death rates and SDI values at the national level are shown in Figures S20 and S21. There were large differences; for example, China and the Republic of Korea had much higher incidence rates than expected for EOGC, IOGC, and LOGC, whereas South Africa and Nigeria had lower values than expected based on SDI values. Similarly, the death rates due to EOGC, IOGC, and LOGC in China and the Republic of Korea were much higher than expected, while South Africa and Nigeria had lower values than expected based on SDI.
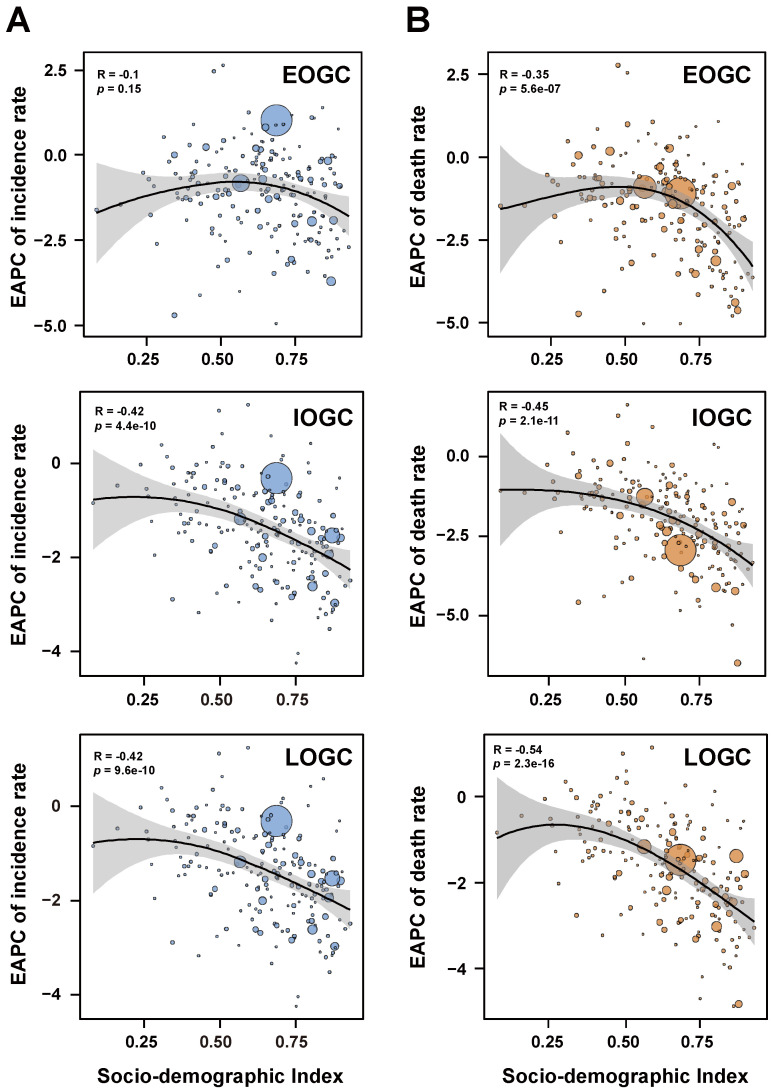
We further analyzed the association between EAPC and SDI values (Figure 3). There was no significant correlation between the EAPC of incidence rate for EOGC and SDI values (ρ = −0.1, p = 0.15). However, the EAPCs of incidence rates for IOGC and LOGC were negatively associated with SDI values (ρ = −0.42, ρ = −0.42, respectively; both p < 0.001) (Figure 3A), while the EAPCs of deaths rates for EOGC, IOGC, and LOGC were also negatively correlated with SDI values (ρ = −0.35, ρ = −0.45, ρ = −0.54, respectively; all p < 0.001) (Figure 3B).
Figure 3.
Correlations between estimated annual percentage changes in gastric cancer and SDI values. (A) Correlations between estimated annual percentage changes of incidence rates in gastric cancer and SDI values; (B) Correlations between estimated annual percentage changes of death rates in gastric cancer and SDI values.
3.4. Predicted Incidences from 2020 to 2035
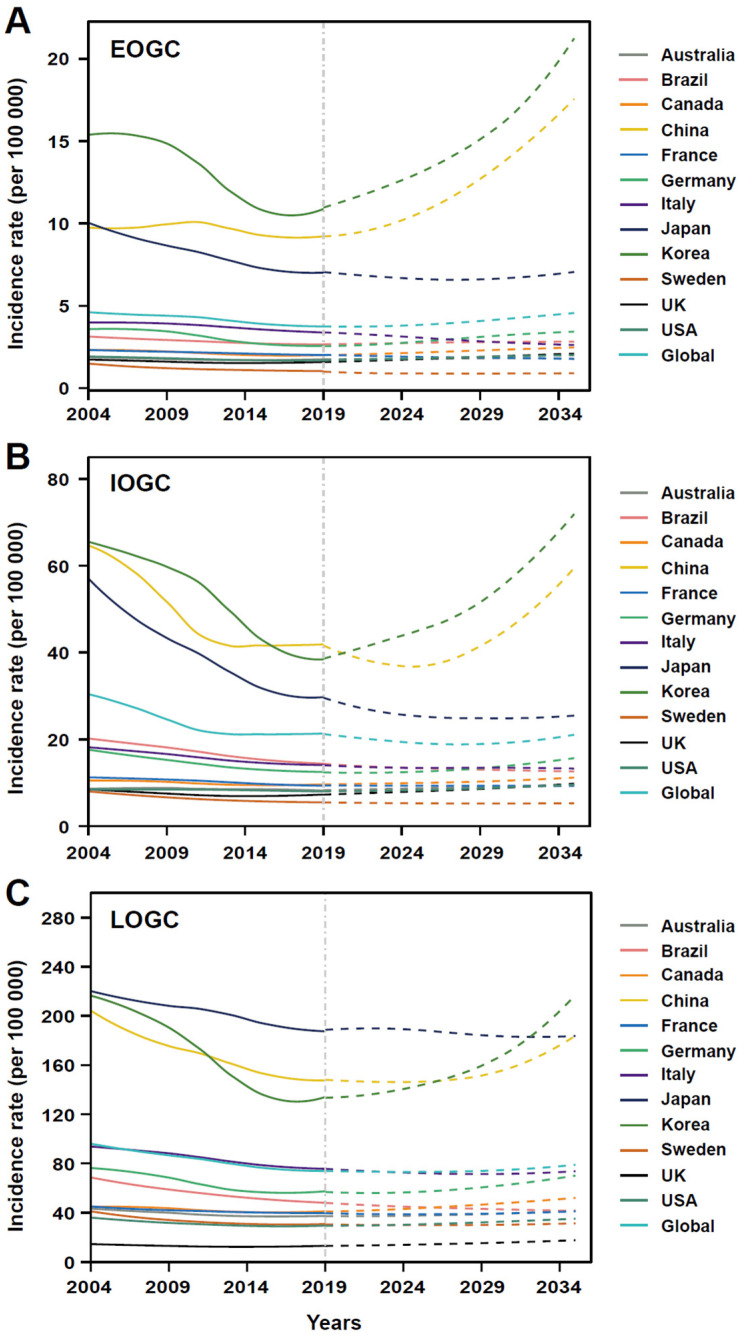
The incidences and incidence rates of EOGC, IOGC, and LOGC were predicted worldwide and in the 12 studied countries from 2020 to 2035 (Figure 4; Table S14). The incidence of EOGC was predicted to almost double in 2035 compared with 2019 in China and Korea, while a slight decrease was predicted in Japan. The global incidence rate of EOGC was expected to increase from 3.7 per 100,000 in 2021 to 4.6 per 100,000 in 2035 (Figure 4A). Notably, the incidence rates in China and Korea were predicted to increase substantially, from 9.2 and 10.9 per 100,000 in 2019 to 17.6 and 21.4 per 100,000 in 2035, respectively, while the incidence rate in Japan was expected to decline to 6.6 per 100,000 in 2028 and then rise again to 7.1 per 100,000 in 2035. The incidence rates in Australia and the United States of America were predicted to change only slightly or remain stable.
Figure 4.
Predictions for gastric cancer from 2020 to 2035 globally and in 12 countries. (A) Predictions of incidence rate for early-onset gastric cancer from 2020 to 2035 globally and in 12 countries; (B) Predictions of incidence rate for intermediate-onset gastric cancer from 2020 to 2035 globally and in 12 countries; (C) Predictions of incidence rate for later-onset gastric cancer from 2020 to 2035 globally and in 12 countries.
The incidence of IOGC was predicted to increase in Korea and the USA, and to decrease slightly or remain stable in Japan and France (Table S14), while the global incidence rate was predicted to decrease from 21.1 per 100,000 in 2019 to 18.8 per 100,000 in 2027, and then increase again to 21.1 per 100,000 in 2035 (Figure 4B). Similarly, the incidence rate in China was expected to decrease from 41.2 per 100,000 in 2019 to 36.8 per 100,000 in 2025, and then increase significantly to >59 per 100,000 in 2035, while the incidence rate in Korea was predicted to increase substantially from 9.2 per 100,000 in 2019 to 21.4 per 100,000 in 2035. The incidence rates in Japan and South Africa were predicted to decrease rapidly from 29.9 and 7.7 per 100,000 in 2019 to 24.5 and 2.3 per 100,000 in 2035, respectively.
The number of new LOGC cases was expected to increase in most of the studied countries (Table S14). Globally, the incidence rate of LOGC was predicted to change slightly, with similar trends in many countries, including Japan, France, and Italy (Figure 4C). However, the incidence rates in China and Korea were predicted to increase sharply from 148.0 and 134.0 per 100,000 in 2019 to 183.9 and 217.6 per 100,000 in 2035, while the incidence rate in Brazil was predicted to decline from 48.1 per 100,000 in 2019 to 41.3 per 100,000 in 2035.
4. Discussion
To the best of our knowledge, this study provides the first analyses of the burden, temporal trends, and predicted trends in EOGC, IOGC, and LOGC worldwide, according to GBD regions, SDI regions, and countries, thus providing important epidemiological information. We reported the population-based incidences, deaths, and temporal trends from 1990−2019, and the predictions from 2020−2035 in relation to period, sex, geographic location, and SDI. Furthermore, we analyzed the clinicopathological, somatic, and survival characteristics of patients with EOGC, IOGC, and LOGC.
The estimations from the GBD 2019 were consistent with previous studies. For example, GLOBOCAN estimated 1,033,701 incident cases and 782,685 deaths due to gastric cancer in 185 countries in 2018, while GBD 2019 estimated 1,238,326 cases and 938,560 deaths in 203 countries in 2018 [1]. A total of 390,182 deaths were reported in China in 2018, compared with 412,924 estimated by GBD 2019 [16]. The reported number of gastric cancers in the Republic of Korea in 2018 was 29,279, compared with 25,074 estimated by the GBD 2019 [17]. Overall, the estimations of the GBD 2019 should thus be considered reliable.
Persistent decreasing trends in the incidence and death rates of EOGC, IOGC, and LOGC have been observed globally from 1990 to 2019. These observed declines in the incidence and death from gastric cancer have been considered as “an unplanned triumph” in cancer prevention, given that they occurred in the absence of active primary prevention programs, except for population-based screening in Japan and South Korea [18,19,20]. These decreasing trends can partly be explained by improved food-preservation methods, improved living conditions, economic developments, reduced overcrowding, better hygiene, and advances in Helicobacter pylori eradication [21,22,23]. Notably, the decreasing trend in incidence rate during the past three decades was more apparent for IOGC compared with EOGC and LOGC, although the reasons for this difference remain unclear.
Our predictions suggest that the incidence rates of EOGC and LOGC will increase worldwide from 2020 to 2035. However, EOGC is predicted to increase more than LOGC globally, and in both high-risk countries (e.g., China and the Republic of Korea) and low-risk countries (e.g., the USA and United Kingdom). Gastric cancers located in both the cardia and corpus have been increasing, especially in younger generations [4,5] with obesity and gastroesophageal reflux disease considered to be the main risk factors for this increase [2,4,24].
The incidence and death rates of gastric cancer in relation to SDI raise important issues. Notably, consistent with established epidemiological data, reductions in gastric cancer burden occurred mainly in high- and high-middle SDI regions. We accordingly found significant negative correlations between SDI values and temporal trends (EAPCs) in incidence and death rates, with more obvious downward trends in incidence and death rates in countries with higher SDI values. Importantly, low-SDI regions showed similarly low incidence and death rates to high-SDI regions in 2019; however, we cannot exclude the possibility that the apparently low burden in low-SDI regions may be due to underestimations of cancer incidence and deaths in limited-resource settings, due to potential misdiagnosis or missed diagnosis, or underdeveloped cancer register systems [25].
This study had several limitations that should be noted before interpreting the main findings. The accuracy of the results depended on the quality and availability of the data at a given time and in a given country, and the poor availability and quality of data from some low-SDI countries with large rural populations could only be partially overcome by improving the estimation framework. We were also unable to analyze the possible risk factors for EOGC, IOGC, and LOGC due to the unavailability of data from the GBD 2019. In addition, the association between SDI values and the burdens of EOGC, IOGC, and LOGC should be interpreted with caution, given that we did not control for other potential factors due to the unavailability of covariate data. Finally, further studies are warranted to develop a forecast model including possible changes in influencing factors.
5. Conclusions
There were substantial differences in the incidence and death rates of EOGC, IOGC, and LOGC at global, regional and national levels in 2019. EOGC showed a slower decrease in incidence rate than IOGC and LOGC globally from 1990 to 2019, whereas EOGC and LOGC showed slower decreases in death rates than IOGC. The incidence rate of EOGC is generally predicted to increase substantially from 2020 to 2035 worldwide, while the rate for LOGC will only increase slightly, and the rate for IOGC is predicted to remain stable over the same period. This study thus revealed variations among gastric cancers in different age groups in relation to period, sex, geographic location, and SDI, and it highlighted the importance of tailored cancer-control measures in neglected subpopulations, especially in patients with EOGC. The results of this study may thus help policymakers to make better public policy decisions.
Acknowledgments
We thank the Global Burden of Diseases, Injuries, and Risk Factors Study (GBD) 2019. We also thank all the individuals who contributed to these databases for their extensive support in finding, cataloging, and analyzing data and facilitating communications. Chun-Dong Zhang (C.-D.Z.) was partly supported by the China Scholarship Council (number 201908050148).
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/cancers14215417/s1, File S1: Supplementary Methods; Figure S1: Incidence rates globally and by sex, and SDI and GBD regions in 2019; Figure S2: Death rates globally and by sex, and SDI and GBD regions in 2019; Figure S3: Incidence rates of gastric cancer globally and by sex, 2019; Figure S4: Death rates of gastric cancer globally and by sex, 2019; Figure S5: Temporal trends in incidence rates of early-onset gastric cancer in five SDI regions, 1990–2019; Figure S6: Temporal trends in incidence rates of intermediate-onset gastric cancer in five SDI regions, 1990–2019; Figure S7: Temporal trends in incidence rates of later-onset gastric cancer in five SDI regions, 1990–2019; Figure S8: Temporal trends in death rates of early-onset gastric cancer in five SDI regions, 1990–2019; Figure S9: Temporal trends in death rates of intermediate-onset gastric cancer in five SDI regions, 1990–2019; Figure S10: Temporal trends in death rates of later-onset gastric cancer in five SDI regions, 1990–2019; Figure S11: Temporal trends in incidence rate of early-onset gastric cancer in 21 GBD regions, 1990–2019; Figure S12: Temporal trends in incidence rates of intermediate-onset gastric cancer in 21 GBD regions, 1990–2019; Figure S13: Temporal trends in incidence rates of later-onset gastric cancer in 21 GBD regions, 1990–2019; Figure S14: Temporal trends in death rates of early-onset gastric cancer in 21 GBD regions, 1990–2019; Figure S15: Temporal trends in death rates of intermediate-onset gastric cancer in 21 GBD regions, 1990–2019; Figure S16: Temporal trends in death rates of later-onset gastric cancer in 21 GBD regions, 1990–2019; Figure S17: Correlations between SDI values and incidence and death rates, 1990–2019; Figure S18: Correlations between SDI values and incidence rates by sex and GBD regions, 1990–2019; Figure S19: Correlations between SDI values and death rates by sex and GBD regions, 1990–2019; Figure S20: Correlations between SDI values and incidence rates in 203 countries, 1990–2019; Figure S21: Correlations between SDI values and death rates in 203 countries, 1990–2019. Table S1: Death and temporal trends globally and by sex, and SDI and GBD regions, 1990–2019; Table S2: Incidence of early-onset gastric cancer in 203 countries, 2019 versus 1990; Table S3: Incidence of intermediate-onset gastric cancer in 203 countries, 2019 versus 1990; Table S4: Incidence of later-onset gastric cancer in 203 countries, 2019 versus 1990; Table S5: Deaths due to early-onset gastric cancer in 203 countries, 2019 versus 1990; Table S6: Deaths due to intermediate-onset gastric cancer in 203 countries, 2019 versus 1990; Table S7: Deaths due to of later-onset gastric cancer in 203 countries, 2019 versus 1990; Table S8: Temporal trends of incidence rates of gastric cancer globally and in SDI quintiles, 1990–2019; Table S9: Temporal trends of death rates of gastric cancer globally and in SDI quintiles, 1990–2019; Table S10: Temporal trends of incidence rates of gastric cancer in 21 GBD regions, 1990–2019; Table S11: Temporal trends of death rates of gastric cancer in 21 GBD regions, 1990–2019; Table S12: Temporal trends of incidence rates of gastric cancer in 203 countries, 1990–2019; Table S13: Temporal trends of death rates of gastric cancer in 203 countries, 1990–2019; Table S14: Incidence (2004–2019) and prediction (2020–2035) of gastric cancer globally and in 12 countries. References [26,27,28,29,30,31,32] are cited in the supplementary materials.
Author Contributions
Conceptualization, F.-L.N., N.-N.Z. and C.-D.Z.; methodology, F.-L.N., N.-N.Z., Z.-M.Z. and C.-D.Z.; software, N.-N.Z., Z.-M.Z. and C.-D.Z.; validation, F.-L.N., N.-N.Z., Z.-M.Z., M.A., W.-Y.D., Y.-J.Z., J.-P.P. and C.-D.Z.; formal analysis, F.-L.N., N.-N.Z. and C.-D.Z.; investigation, F.-L.N. and C.-D.Z.; resources, F.-L.N., Z.-M.Z. and C.-D.Z.; data curation, F.-L.N., N.-N.Z., Z.-M.Z. and C.-D.Z.; writing—original draft preparation, F.-L.N. and C.-D.Z.; writing—review and editing, F.-L.N., N.-N.Z., Z.-M.Z., M.A., W.-Y.D., Y.-J.Z., J.-P.P. and C.-D.Z.; visualization, C.-D.Z.; supervision, C.-D.Z.; project administration, C.-D.Z.; funding acquisition, none. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki. Data of this study were extracted from the GBD 2019, and IRB approval was therefore not necessary.
Informed Consent Statement
The data released from the Global Health Data Exchange query did not require informed consent from participants.
Data Availability Statement
The data generated and analyzed in this study are available from the Global Health Data Exchange query tool (http://ghdx.healthdata.org/gbd-results-tool) (accessed on 18 January 2022). The data that support the main findings of this study are also available from the corresponding author upon reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Sung H., Ferlay J., Siegel R.L., Laversanne M., Soerjomataram I., Jemal A., Bray F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021;71:209–249. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 2.Arnold M., Park J.Y., Camargo M.C., Lunet N., Forman D., Soerjomataram I. Is gastric cancer becoming a rare disease? A global assessment of predicted incidence trends to 2035. Gut. 2020;69:823–829. doi: 10.1136/gutjnl-2019-320234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Heer E.V., Harper A.S., Sung H., Jemal A., Fidler-Benaoudia M.M. Emerging cancer incidence trends in Canada: The growing burden of young adult cancers. Cancer. 2020;126:4553–4562. doi: 10.1002/cncr.33050. [DOI] [PubMed] [Google Scholar]
- 4.Anderson W.F., Rabkin C.S., Turner N., Fraumeni J.F., Jr., Rosenberg P., Camargo M.C. The Changing Face of Noncardia Gastric Cancer Incidence Among US Non-Hispanic Whites. JNCI J. Natl. Cancer Inst. 2018;110:608–615. doi: 10.1093/jnci/djx262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Camargo M.C., Anderson W.F., King J.B., Correa P., Thomas C.C., Rosenberg P., Eheman C.R., Rabkin C.S. Divergent trends for gastric cancer incidence by anatomical subsite in US adults. Gut. 2011;60:1644–1649. doi: 10.1136/gut.2010.236737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sung H., Siegel R.L., Rosenberg P.S., Jemal A. Emerging cancer trends among young adults in the USA: Analysis of a population-based cancer registry. Lancet Public Health. 2019;4:e137–e147. doi: 10.1016/S2468-2667(18)30267-6. [DOI] [PubMed] [Google Scholar]
- 7.Bautista M.C., Jiang S.-F., Armstrong M.A., Postlethwaite D., Li D. Impact of Age on Clinicopathological Features and Survival of Patients with Noncardia Gastric Adenocarcinoma. J. Gastric Cancer. 2014;14:238–245. doi: 10.5230/jgc.2014.14.4.238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bergquist J.R., Leiting J.L., Habermann E.B., Cleary S.P., Kendrick M.L., Smoot R.L., Nagorney D.M., Truty M.J., Grotz T.E. Early-onset gastric cancer is a distinct disease with worrisome trends and oncogenic features. Surgery. 2019;166:547–555. doi: 10.1016/j.surg.2019.04.036. [DOI] [PubMed] [Google Scholar]
- 9.GBD 2017 Causes of Death Collaborators Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1736–1788. doi: 10.1016/S0140-6736(18)32203-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.GBD 2019 Diseases and Injuries Collaborators Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1204–1222. doi: 10.1016/S0140-6736(20)30925-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ning F.-L., Lyu J., Pei J.-P., Gu W.-J., Zhang N.-N., Cao S.-Y., Zeng Y.-J., Abe M., Nishiyama K., Zhang C.-D. The burden and trend of gastric cancer and possible risk factors in five Asian countries from 1990 to 2019. Sci. Rep. 2022;12:5980. doi: 10.1038/s41598-022-10014-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.GBD 2017 Population and Fertility Collaborators Population and fertility by age and sex for 195 countries and territories, 1950–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1995–2051. doi: 10.1016/S0140-6736(18)32278-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Von Elm E., Altman D.G., Egger M., Pocock S.J., Gøtzsche P.C., Vandenbroucke J.P., STROBE Initiative The strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. Int. J. Surg. 2014;12:1495–1499. doi: 10.1016/j.ijsu.2014.07.013. [DOI] [PubMed] [Google Scholar]
- 14.GBD 2016 Causes of Death Collaborators Global, regional, and national age-sex specific mortality for 264 causes of death, 1980–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390:1151–1210. doi: 10.1016/S0140-6736(17)32152-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gu W.-J., Ning F.-L., Jin H.-R., Zhao Z.-M., Lyu J., Pei J.-P., Cao S.-Y., Zeng Y.-J., Abe M., Nishiyama K., et al. Burden and Trends of Inflammatory Bowel Disease in Five Asian Countries From 1990 To 2019: A Comparison With the United States and the United Kingdom. Dis. Colon Rectum. 2022 doi: 10.1097/DCR.0000000000002491. [DOI] [PubMed] [Google Scholar]
- 16.Feng R.M., Zong Y.N., Cao S.M., Xu R.H. Current cancer situation in China: Good or bad news from the 2018 Global Cancer Statistics? Cancer Commun. 2019;39:22. doi: 10.1186/s40880-019-0368-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hong S., Won Y.J., Lee J.J., Jung K.W., Kong H.J., Im J.S., Seo H.G. The Community of Population-Based Regional Cancer Registries Cancer Statistics in Korea: Incidence, Mortality, Survival, and Prevalence in 2018. Cancer Res. Treat. 2021;53:301–315. doi: 10.4143/crt.2021.291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhang X., Li M., Chen S., Hu J., Guo Q., Liu R., Zheng H., Jin Z., Yuan Y., Xi Y., et al. Endoscopic Screening in Asian Countries Is Associated With Reduced Gastric Cancer Mortality: A Meta-analysis and Systematic Review. Gastroenterology. 2018;155:347–354.e9. doi: 10.1053/j.gastro.2018.04.026. [DOI] [PubMed] [Google Scholar]
- 19.Suh M., Song S., Cho H.N., Park B., Jun J.K., Choi E., Kim Y., Choi K.S. Trends in Participation Rates for the National Cancer Screening Program in Korea, 2002–2012. Cancer Res. Treat. 2017;49:798–806. doi: 10.4143/crt.2016.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Asaka M., Kato M., Sakamoto N. Roadmap to eliminate gastric cancer with Helicobacter pylori eradication and consecutive surveillance in Japan. J. Gastroenterol. 2014;49:1–8. doi: 10.1007/s00535-013-0897-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Babaei M., Pourfarzi F., Yazdanbod A., Chiniforush M.M., Derakhshan M., Mousavi S.M., Samadi F., Rahimi G. Gastric cancer in Ardabil, Iran—A review and update on cancer registry data. Asian Pac. J. Cancer Prev. 2010;11:595–599. [PubMed] [Google Scholar]
- 22.Asaka M., Kobayashi M., Kudo T., Akino K., Asaka Y., Fujimori K., Kikuchi S., Kawai S., Kato M. Gastric cancer deaths by age group in Japan: Outlook on preventive measures for elderly adults. Cancer Sci. 2020;111:3845–3853. doi: 10.1111/cas.14586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kato M., Ota H., Okuda M., Kikuchi S., Satoh K., Shimoyama T., Suzuki H., Handa O., Furuta T., Mabe K., et al. Guidelines for the management of Helicobacter pylori infection in Japan: 2016 Revised Edition. Helicobacter. 2019;24:e12597. doi: 10.1111/hel.12597. [DOI] [PubMed] [Google Scholar]
- 24.Arnold M., Abnet C.C., Neale R.E., Vignat J., Giovannucci E.L., McGlynn K.A., Bray F. Global Burden of 5 Major Types of Gastrointestinal Cancer. Gastroenterology. 2020;159:335–349.e15. doi: 10.1053/j.gastro.2020.02.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Morhason-Bello I.O., Odedina F., Rebbeck T.R., Harford J., Dangou J.-M., Denny L., Adewole I.F. Challenges and opportunities in cancer control in Africa: A perspective from the African Organisation for Research and Training in Cancer. Lancet Oncol. 2013;14:e142–e151. doi: 10.1016/S1470-2045(12)70482-5. [DOI] [PubMed] [Google Scholar]
- 26.Gao S., Yang W.-S., Bray F., Va P., Zhang W., Gao J., Xiang Y.-B. Declining rates of hepatocellular carcinoma in urban Shanghai: Incidence trends in 1976–2005. Eur. J. Epidemiol. 2011;27:39–46. doi: 10.1007/s10654-011-9636-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Deng Y., Zhao P., Zhou L., Xiang D., Hu J., Liu Y., Ruan J., Ye X., Zheng Y., Yao J., et al. Epidemiological trends of tracheal, bronchus, and lung cancer at the global, regional, and national levels: A population-based study. J. Hematol. Oncol. 2020;13:98. doi: 10.1186/s13045-020-00915-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hankey B.F., Ries L.A., Kosary C.L., Feuer E.J., Merrill R.M., Clegg L.X., Edwards B.K. Partitioning linear trends in age-adjusted rates. Cancer Causes Control. 2000;11:31–35. doi: 10.1023/A:1008953201688. [DOI] [PubMed] [Google Scholar]
- 29.Yang X., Zhang T., Zhang Y., Chen H., Sang S. Global burden of COPD attributable to ambient PM2.5 in 204 countries and territories, 1990 to 2019: A systematic analysis for the Global Burden of Disease Study 2019. Sci. Total Environ. 2021;796:148819. doi: 10.1016/j.scitotenv.2021.148819. [DOI] [PubMed] [Google Scholar]
- 30.Yu J., Yang X., He W., Ye W. Burden of pancreatic cancer along with attributable risk factors in Europe between 1990 and 2019, and projections until 2039. Int. J. Cancer. 2021;149:993–1001. doi: 10.1002/ijc.33617. [DOI] [PubMed] [Google Scholar]
- 31.Knoll M., Furkel J., Debus J., Abdollahi A., Karch A., Stock C. An R package for an integrated evaluation of statistical approaches to cancer incidence projection. BMC Med. Res. Methodol. 2020;20:257. doi: 10.1186/s12874-020-01133-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Du Z., Chen W., Xia Q., Shi O., Chen Q. Trends and projections of kidney cancer incidence at the global and national levels, 1990–2030: A Bayesian age-period-cohort modeling study. Biomark. Res. 2020;8:16. doi: 10.1186/s40364-020-00195-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data generated and analyzed in this study are available from the Global Health Data Exchange query tool (http://ghdx.healthdata.org/gbd-results-tool) (accessed on 18 January 2022). The data that support the main findings of this study are also available from the corresponding author upon reasonable request.