Abstract
Intermittent fasting is a non-pharmacological dietary approach to management of obesity and metabolic syndrome, involving periodic intervals of complete or near-complete abstinence from food and energy-containing fluids. This dietary strategy has recently gained significant popularity in mainstream culture and has been shown to induce weight loss in humans, reduce gut and systemic inflammation, and improve gut microbial diversity and dysbiosis (largely in animal models). It has been hypothesized that intermittent fasting could be beneficial in the management of nonalcoholic fatty liver disease, given the condition’s association with obesity. This review summarizes protocols, potential mechanisms of action, and evidence for intermittent fasting in nonalcoholic fatty liver disease. It also highlights practical considerations for implementing intermittent fasting in clinical practice. A search of the literature for English-language articles related to intermittent fasting or time-restricted feeding and liver disease was completed in PubMed and Google Scholar. Potential mechanisms of action for effects of intermittent fasting included modulation of circadian rhythm, adipose tissue and adipokines, gut microbiome, and autophagy. Preclinical, epidemiological, and clinical trial data suggested clinical benefits of intermittent fasting on metabolic and inflammatory markers in humans. However, there was a paucity of evidence of its effects in patients with nonalcoholic fatty liver disease. More clinical studies are needed to determine mechanisms of action and to evaluate safety and efficacy of intermittent fasting in this population.
Keywords: intermittent fasting, time-restricted feeding, intermittent energy restriction, alternate-day fasting, nonalcoholic fatty liver disease
1. Introduction
In 2015, the prevalence of overweight and obesity in adults in the United States was 64.2% and 28.3%, respectively [1]. Pathophysiological changes resulting from overweight and obesity lead to metabolic dysfunction, chronic inflammation, and impaired immune system regulation [2]. Obesity and insulin resistance are major risk factors for the development of NAFLD [3]. With a global prevalence rate of close to 30%, NAFLD is the most common cause of chronic liver disease worldwide [4,5], and the number of NAFLD cases globally is projected to increase by up to 56% between 2019 and 2030 [6]. In 2020, an international consensus panel proposed redefining the term “NAFLD” as “metabolic dysfunction-associated fatty liver disease” (MAFLD) to align the disease name closer to its pathophysiology [7]. However, because NAFLD and MAFLD each represent a different patient phenotype, those terms are not interchangeable. As MAFLD has only recently been defined, this review discusses evidence from studies in patients with NAFLD. Lifestyle management, including weight reduction and physical activity, continue to be primary treatment modalities for NAFLD [8]. Weight-loss reduction of ≥10% can decrease hepatic steatosis and result in fibrosis regression [8]. Despite studies demonstrating transformative effects of weight loss on NAFLD and metabolic outcomes, durable weight loss remains elusive for many. In a meta-analysis of 29 long-term weight-loss studies, more than half of lost weight was regained within 2 years, and nearly 80% of lost weight was regained within 5 years [9].
Intermittent fasting (IF) is a dietary intervention that involves periodic intervals of complete or almost complete abstinence from food and energy-containing fluids. The practice of IF has been performed since the time of the earliest civilizations, mainly for religious or cultural reasons [10], and may or may not include energy restriction. Moreover, IF has demonstrated health benefits without weight loss in cancer [11,12], cardiovascular disease [12], and cognitive and brain function [13]. IF has gained popularity with the public [14], with high-profile individuals endorsing its effectiveness, yet guidance for its use and/or implementation is not currently available for patients with NAFLD, highlighting the timely need for evidence-based recommendations for IF in those patients.
Observational studies have reported metabolic benefits of IF, including weight loss [15], improved glycosylated hemoglobin [15], decreased atherogenic risk [16,17], improved circulating cytokines [16,17], and immune cell proliferation [18]. Further, in a systematic review and meta-analysis of five randomized controlled trials (RCTs) comparing IF to energy restriction in patients with type 2 diabetes mellitus and metabolic syndrome, changes observed in glycosylated hemoglobin and fasting plasma glucose were similar between groups; however, IF appeared to have a greater weight-loss benefit (−1.70 kg, 95% confidence interval [CI]: −3.28 to −0.11 kg) [19].
Intervention studies have also reported weight loss [20], improvement in insulin resistance [20], reduced oxidative stress [20,21], improvements in serum cholesterol and triglycerides [21], and decreased levels of systemic inflammatory markers, including tumor necrosis factors (TNF)-α and brain-derived neurotrophic factors [21]. An umbrella review of 11 meta-analyses, including a total of 130 RCTs with comparator groups assigned either continuous energy restriction or regular diet, reported that IF was associated with weight loss; reduced fat mass; and improvements in blood lipids, fasting plasma glucose, fasting insulin, blood pressure, and C-reactive protein [22].
Based on results of observational and clinical studies in other disease states [23,24,25,26,27], it can be postulated that IF would confer metabolic and likely clinical benefits to patients with NAFLD, and clinical evidence is beginning to emerge for use of IF in management of the disease. In this narrative review, we describe current evidence for use of IF in management of NAFLD, as well as potential mechanisms of action, including those related to circadian rhythm, white adipose tissue (WAT), adipokines, the gut microbiome, and autophagy.
2. Search Methods
CML and AB conducted a search of the literature for English-language manuscripts in PubMed and Google Scholar. Search terms included “intermittent fasting”, “intermittent AND fasting”, “time-restricted feeding” AND “liver disease”, “nonalcoholic fatty liver disease”, and “NAFLD”. Articles were assessed if they included results of preclinical studies in animal models or of epidemiological or clinical trial studies in humans with NAFLD. Reference lists of identified articles were also assessed to identify additional manuscripts.
3. Intermittent Fasting Protocols
Fasting and feeding intervals vary in practice of IF. Various IF protocols are described in Table 1, including time-restricted feeding (TRF), intermittent energy restriction (IER), alternate-day fasting (ADF), 5:2 fasting, and fasting-mimicking diet (FMD).
Table 1.
Intermittent fasting protocols.
| Type of Intermittent Fasting Protocol | Description of Intermittent Fasting Protocol |
|---|---|
| Time-restricted feeding | Commonly entails a daily fast for 12 to 20 h |
| Intermittent energy restriction | Involves an energy-restricted fast during intermittent periods, during which some energy-laden foods or liquids are consumed |
| Alternate-day fasting | Involves fasting for 24 h, followed by a regular eating pattern for the following 24 h |
| 5:2 fasting | Consists of fasting on two non-consecutive days for every five days of regular intake |
| Fasting-mimicking diet | Includes some energy-laden liquids |
Specific recommendations regarding diet composition and macronutrient breakdown for patients with NAFLD could not be inferred from existing IF studies, given that IF protocols typically included ad libitum intake during the feeding period, and diet composition and nutrient intake during this feeding period were often not assessed. However, practical, general recommendations for IF implementation for both clinicians and patients are included in Table 2 [28,29].
Table 2.
Practical recommendations to implement intermittent fasting in patients with NAFLD.
| Steps | Recommendations for Each Step |
| Step 1: Determine if patient is overweight or obese | • Assess weight, anthropometrics, BMI, waist circumference, and metabolic comorbidities |
| • Rule out edema or ascites | |
| Step 2: Assess the patient’s history with weight-management strategies | • If patient is naïve to weight management, propose all dietary options, including IF |
| • If patient has experience with dietary weight-loss interventions that were ineffective, propose IF as an option | |
| Step 3: Screen for risk of malnutrition | • Screen for malnutrition risk using the abridged PG-SGA a |
| • Consider using the NIAS b to rule out avoidant and restrictive food behaviors that may increase the risk of malnutrition risk from an IF intervention | |
| Step 4: Support the patient as a partner in their journey | • Empower the patient with options for weight management, including but not limited to intermittent fasting. Other options include calorie-restriction, physical activity, and, when appropriate, anti-obesity medications and bariatric surgery |
| Step 5: Determine the IF protocol that appeals to the patient, matches their preferences/lifestyle, and is most likely to result in long-term adherence | • If the patient chooses IF, review different protocols and encourage the patient to consider factors such as sleep/wake cycles/times, shift work, current patterns of eating, diabetes, other comorbidities, etc. |
| • There was insufficient evidence to recommend one IF pattern over another; the choice should be determined based on lifestyle and other comorbidities (e.g., ADF may not be suitable for a patient treated with glucose-lowering medications) | |
| Step 6: Facilitate IF adherence and nutritional adequacy | Provide recommendations to: |
| • Optimize hydration with water | |
| • Limit sugar and artificially sweetened beverages | |
| • Choose high-fiber foods, such as fruits, vegetables, beans, and lentils, as tolerated | |
| • Include protein sources such as fish, poultry, eggs, beans, lentils, and cheese | |
| • Include 2–3 Tbsp of healthy fats each day, such as nuts, seeds, and olive oil | |
|
Step 7: Monitor for side effects and malnutrition While malnutrition and other adverse events are not expected, patient and clinician should both monitor for adverse outcomes |
Monitor for: |
| • Malnutrition risk (using the abridged PG-SGAa) | |
| • Fatigue, headache, and muscle cramps (ensure adequate intake of electrolytes, especially during the fasting period) | |
| • Excessive weight loss (greater than 1 kg per week) | |
| • Micronutrient deficiencies (iron, folate, vitamin B12) |
a Abridged patient-generated subjective global assessment [28]. b Nine item avoidant/restrictive food intake disorder screen [29]. Abbreviations: ADF, alternate-day fasting; BMI, body mass index; IF, intermittent fasting; NAFLD, nonalcoholic fatty liver disease; NIAS, nine item avoidant/restrictive food intake disorder screen; PG-SGA, patient-generated subjective global assessment; TRF, time-restricted feeding.
4. Potential Mechanisms of Action for Intermittent Fasting Effects
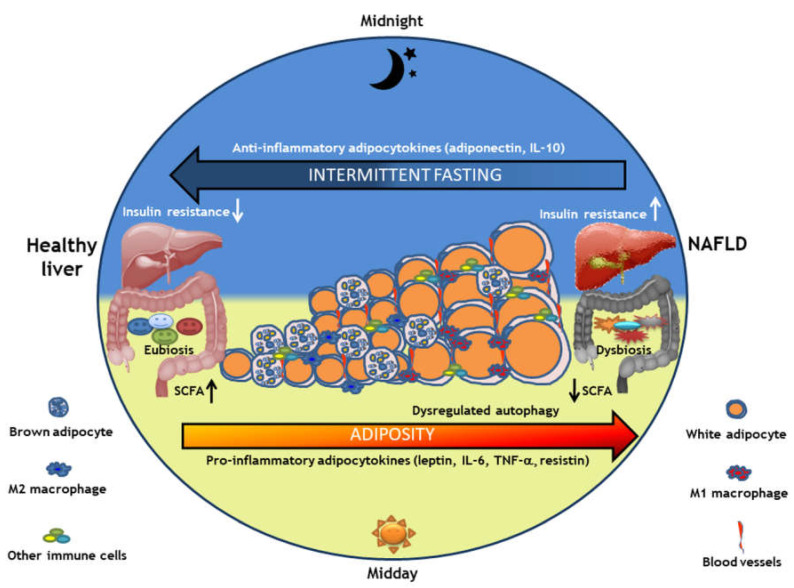
IF interventions appeared to confer health benefits independent of energy intake (Figure 1) [2,3,23,30,31,32,33,34,35,36,37,38,39,40,41]. For example, in two separate trials of overweight women, participants lost the same amount of weight during a 6-month period whether they followed an IF intervention or a 25% energy-restricted diet. However, those assigned to the IF group had greater improvement in insulin sensitivity and greater reduction in waist circumference [26,27]. Here, we review physiologic changes induced by IF and their resultant impacts on metabolic health.
Figure 1.
Potential mechanisms of action for effects of intermittent fasting in NAFLD. Obesity is a risk factor for NAFLD [3] and is associated with low-grade inflammation [2,32] marked by presence of increased white adipose tissue, increased pro-inflammatory M1 macrophages, decreased anti-inflammatory M2 macrophages [2], formation of new blood vessels (angiogenesis), increased gut microbial dysbiosis [40], and changes in autophagy-related physiological processes [41]. Intermittent fasting may play a role in circadian rhythm modulation [34,37], adipose tissue plasticity [35,36], adipokine production [23], and gut microbiome [23,33] through increased SCFA production [38,39] and autophagy [31], with potential to reverse inflammation, metabolic dysfunction, and impaired immune system regulation associated with NAFLD. Abbreviations: NAFLD, nonalcoholic fatty liver disease; SCFA, short-chain fatty acids.
4.1. Circadian Rhythm
Energy intake plays a fundamental role in controlling eating behavior due to the interaction between the central homeostatic and non-homeostatic (hedonic) systems [42]. Balance between homeostatic and hedonic eating behaviors is not only influenced by volume and composition of the diet, but also by timing and rhythmicity of food ingestion. Furthermore, circadian rhythm affects gut function as well as composition and interactions of the microbiome with the gut [33]. Circadian rhythm represents all physiological processes involved in a period of 1 day, such as sleep/wake cycle, vital signs, hormone secretion, cognitive performance, and mood regulation. Of interest: limiting time of food consumption appeared to readjust the circadian clock, implying that meal timing affects metabolism [43]. While the circadian system modulates both insulin and glucagon by controlling production and secretion, the system itself is regulated by numerous factors, including food intake. Although insulin production and secretion are maximal in the evening, around 5 p.m., and lowest in the early morning, at 4 a.m. [37], eating patterns alter blood nutrient levels and may override circadian patterns of hormonal release, which may have implications on various physiological processes.
For example, in a small study of 23 adults who fasted during the daytime for the month of Ramadan, evening cortisol levels were higher compared to those observed during a non-fasting month [44]. An increase in evening cortisol coincided with increased insulin levels in the evening and increased blood glucose levels in the morning. Another small study of 11 overweight adults participating in a 4-day randomized crossover study of TRF in which food was consumed either between 8 a.m. and 2 p.m. (early fasting) or 8 a.m. and 8 p.m. (control) demonstrated improved mean 24-h glucose levels and induced broad changes in circadian clock gene expression, as well as expression of hormones and genes related to longevity and autophagy in the early fasting group as compared to the control, implying anti-aging effects [34]. In a further delve into molecular mechanisms of IF, the hepatic macrophage glucocorticoid receptor was recently identified as an important component of fasting-induced macrophage secretion of inflammatory cytokines, and its relationship to influence of ketogenesis in hepatocytes was demonstrated [45].
In relation to NAFLD, Kettner et al. demonstrated that disruption of the circadian rhythm in jet-lag-induced mice fed ad libitum resulted in metabolic syndrome and liver injury, progressing from NAFLD to nonalcoholic steatohepatitis (NASH) and fibrosis, similar to those seen in mice lacking the circadian genes Bmal1, Per1; Per2, or Cry1; Cry2 and therefore lacking a circadian clock [46]. In a separate study, Chaix et al. demonstrated that weight gain and hepatic steatosis were prevented by TRF within a 10 h period in mice that were jet-lagged, similar to in mice without a circadian clock, also suggesting that eating patterns might override circadian rhythm [47].
4.2. White Adipose Tissue Browning
Historically, adipose tissue has been viewed as an inert, passive pool for energy storage, and while that is accurate, its endocrine functions have also been widely established [48]. Adipose tissue has been demonstrated to express and secrete a wide variety of bioactive peptides, collectively referred to as adipokines. Examples of adipokines include leptin, adiponectin, TNF-α, interleukin (IL)-6, and resistin, among others. Adipokines may act either locally, using paracrine or autocrine signaling, or systemically, through neurocrine and endocrine pathways. Adipose tissue may be subdivided into WAT and brown adipose tissue (BAT), and further into visceral and subcutaneous depots of fat. Adipose tissue sub-types and compartments have varying impacts upon health and disease.
The main role of WAT is storage of energy as triglycerides [49], whereas BAT is involved in thermogenesis [49,50], which may counteract the effects of increased energy intake and promote weight loss. Consequently, browning of WAT may represent a promising therapeutic target for obesity and metabolic diseases. A preclinical study performed in mice reported that IF promoted WAT browning and ameliorated obesity, insulin resistance, and hepatic steatosis by altering the gut microbiome [36]. In another pre-clinical study, isocaloric IF improved metabolic homeostasis through adipose thermogenesis by WAT browning due to M2 anti-inflammatory macrophage activation and increased vascular endothelial growth factor expression [35].
4.3. Adipokines
Adipose tissue is comprised of several different types of cells, including fibroblasts, endothelial cells, and different types of immune cells. In the context of obesity, immune-cell composition of adipose tissue undergoes major changes, with abnormal adipokine and chemokine production as well as activation of inflammatory signaling pathways [51]. Adipokines exert anti-inflammatory or pro-inflammatory effects in different organs. Generally, pro-inflammatory adipokines include leptin, visfatin, IL-6, TNF-α, resistin, and fatty acid binding protein 4, whereas examples of anti-inflammatory cytokines include adiponectin, IL-10, omentin-1, vaspin and apelin [52].
With obesity, greater secretion of pro-inflammatory adipokines (including leptin, IL-6, TNF-α, and resistin) was observed, affecting satiety and lipid metabolism, along with a decrease in anti-inflammatory and insulin-sensitizing cytokines such as adiponectin and IL-10 [51]. Of fat depots, visceral adipose tissue (VAT) was the major determinant of inflammatory cytokine production, and decreases in VAT were associated with improved inflammatory outcomes [53]. Even a decrease in weight as low as 2.5% reduced fat mass after 3 weeks of IF in subjects without obesity [54] and reduced VAT area after 8 weeks of IF in subjects with obesity [55]. This is of particular relevance in NAFLD, as VAT area is associated with greater risk of developing NAFLD [56], with fibrosis [57,58], and with lower likelihood of disease improvement [56]. A recent narrative review described the link between adipokines and NAFLD and progression to NASH and cirrhosis. Low levels of leptin with high levels of adiponectin were protective against hepatic steatosis, whereas high levels of leptin and resistin acted to increase hepatic fibrosis [59]. Those effects highlighted a plausible role for alteration of adipokine secretion, through interventions such as IF, to limit the progression of liver disease.
In the context of intestinal inflammation, it has been proposed that adipokines arising from VAT, such as leptin, may increase permeability of mucosa, thereby facilitating bacterial translocation and the inflammatory process [60,61]. Decreased leptin with increased adiponectin levels has been observed in humans who fasted on alternate days for 12 weeks [24]. However, in a different study, leptin levels decreased in subjects with overweight or obesity who followed an ADF protocol, but adiponectin levels did not change, nor did other biomarkers of inflammation, including resistin, IL-6, or TNF-α [62].
Similarly, in a pilot RCT in patients with multiple-sclerosis that compared ADF with energy intake restricted to 500 kcal/day on fasting days to ad libitum diet for 15 days, reduced leptin levels were found after ADF, but no differences were noted in adiponectin levels between IF and ad libitum diet [23]. Differences in sample size, adherence, and drop-out may have accounted for these divergent results. Further studies are warranted to better delineate the specific mechanistic effects of fasting on adipokines, which could potentially be useful for biomarkers of fasting and inflammation in clinical practice.
4.4. Adipose Tissue–Gut Microbiome Axis
The gut microbiome is increasingly recognized for its role in systemic metabolism [63,64]. Gut microbiota mediate hepatic production of triglycerides and promote storage of triglycerides in adipocytes by suppressing expression of lipoprotein lipase inhibitors [64]. Gut microbial dysbiosis, characterized by decreased microbial gene richness and altered abundance of microbial groups when compared to those of people of normal weight, was noted in individuals with obesity [65]. Specifically, an increased Firmicutes to Bacteroidetes ratio, increased abundance of Lactobacillus and Bifidobacterium, and decreased abundance of Akkermansia muciniphila were observed in individuals with obesity [66,67,68].
Notably, gut microbial dysbiosis seemed to contribute to the conversion of choline into methylamines and to alter bile acid metabolism, both of which can induce hepatic inflammation, leading to NAFLD [69]. Therefore, improving microbial dysbiosis may be an important mechanism in reducing hepatic inflammation and limiting the progression of NAFLD. Interestingly, studies in humans have also noted changes in the microbiome during IF. Results from a pilot observational study of Ramadan fasting demonstrated an increase in A. muciniphila and Bacteroides fragilis, with an amelioration of lipid and glucose profiles [70]. Furthermore, a recent clinical review described the positive association of A. muciniphila with IF-mediated improvements in host energy metabolism and circadian rhythm [71].
Gut microbiota may contribute to obesity pathogenesis through modulation of energy metabolism via enabling of energy extraction from otherwise indigestible foods, which may provide as much as 10% of the daily energy requirement [72]. Further, lipopolysaccharide from the outer membrane of Gram-negative bacteria may translocate through the intestinal barrier and contribute to systemic inflammation [73]. Metabolic endotoxemia has been shown to influence onset and progression of insulin resistance and metabolic disease, which is of relevance to NAFLD pathogenesis [74]. Finally, the gut microbiome contributes to appetite by modifying gut hormones released by the enteroendocrine cells, such as ghrelin, peptide YY, leptin, and glucagon-like peptide 1.
Preclinical studies have demonstrated the ability of IF to beneficially modulate the gut microbiome. IF for 28 days in mouse models of type 2 diabetes mellitus improved intestinal permeability, decreased plasma lipopolysaccharide, improved gut microbial diversity, and increased abundance of several bacteria at the genus level, including butyrate producer Odoribacter [75]. Moreover, ADF compared to isocaloric intake in mice induced WAT browning, weight loss, and changes in gut microbiota, including an increase in Firmicutes to Bacteroides ratio [36]. Of note is that microbiota-depleted mice were resistant to IF-induced WAT browning, while fecal microbiota transplantation from IF-treated mice to microbiome-depleted mice activated WAT browning, providing a potential gut-microbiota-driven mechanism to explain WAT browning and a rationale for treating metabolic diseases.
4.5. Autophagy
Autophagy is a vital catabolic process by which cells degrade and recycle endogenous and exogenous components to maintain cellular homeostasis [76]. It facilitates eradication of damaged cell organelles or unused proteins, and is stimulated by various conditions of stress, including starvation. Autophagy is necessary when a cell is deprived of compounds needed for survival. Therefore, calorie restriction is the most robust modifiable inducer of autophagy, and, interestingly, nutrient depletion or limitation is associated with longevity [77]. Alternatively, dysregulated autophagy is associated with several chronic disorders, including metabolic diseases [78].
Given the potency of calorie restriction to induce autophagy, it can be posited that IF could attenuate this dysregulation. Indeed, mice that had fasted in an Alzheimer’s disease model showed an increase in number and size of autophagosomes in neurons [31]. Another preclinical study in a mouse model of Charcot–Marie–Tooth syndrome demonstrated five months of IF increased expression of autophagy-associated proteins, ATG7, and microtubule-associated protein 1 light chain 3, as well as decreased levels of p62 protein, collectively suggesting increased autophagy [79].
5. Studies of Intermittent Fasting in Nonalcoholic Fatty Liver Disease
Lifestyle modification consisting of dietary intervention and physical activity remains the only therapeutic option for most patients with NAFLD [3,80,81]. However, there was limited evidence as to which dietary interventions are most effective at improving or resolving NAFLD [3,8,80,81]. There were few head-to-head RCTs that evaluated the efficacy of specific dietary interventions on hepatic, metabolic, and weight-loss outcomes in patients with NAFLD, and it is widely accepted that more high-quality dietary studies are needed to confirm a successful approach [82].
Preclinical evidence in NAFLD animal models supported further clinical inquiry into IF as a potential therapy [83,84], and observational [85] and retrospective [86] studies on the effects of fasting during Ramadan supported use of IF for management of NAFLD. To date, three RCTs have evaluated the use of IF in patients with NAFLD [87,88,89].
In a 12-week RCT, 271 adult patients with NAFLD were randomly assigned to an ADF, a TRF, or a control group [87]. Patients in the ADF group consumed 25% of their energy needs on fasting days and ate ad libitum on non-fasting days. Patients in the TRF group ate ad libitum during any consecutive 8 h window of their choice each day. Patients in the control group consumed 80% of their energy needs despite not being given guidance or restrictions regarding their usual intake. Energy intake on feeding days was not different between the groups. Composition of macronutrient intake was not reported. At 12 weeks, patient-reported dietary adherence was 97.5%, with no significant differences between the three groups. Body weight decreased significantly from baseline in both the ADF (−5.4 ± 0.7%) and TRF (−4.3 ± 0.9%) groups as compared to the control (−2.54 ± 0.9%) after 12 weeks, which was attributed largely to loss of fat mass. Compared to controls, total cholesterol decreased with ADF but not TRF, while triglycerides decreased with both IF protocols. No differences were found in fasting insulin, glucose, or blood pressure, although study duration was quite short. Liver stiffness, assessed by FibroScan®, was not different within or between groups after 12 weeks, and no other liver-related biomarkers, including liver enzymes or sonographic features of steatosis, were assessed in the study.
However, in another 8-week RCT, liver steatosis and fibrosis, assessed using ultrasound and two-dimensional shear wave elastography, respectively, decreased significantly with ADF as compared to the control [88]. In this study, patients with NAFLD were randomly assigned 3:1 either to follow an ADF (n = 33) that consisted of 30% of energy needs on fasting days and ad libitum consumption on non-fasting days or to maintain habitual intake (control; n = 10). Overall energy and composition of macronutrient intake were not assessed on feeding days. ADF also reduced body weight, body mass index (BMI), alanine transferase, and aspartate transferase as compared to controls.
Improvements were also seen with IF in another 12-week RCT of adults with NAFLD [89]. Patients were randomly assigned to receive either 5:2 IER (n = 25); a low-carbohydrate, high-fat (LCHF) diet (n = 25); or standard-of-care (SoC) as a control (n = 24). The 5:2 IER protocol consisted of fasting on two non-consecutive days per week, wherein patients restricted energy intake on fasting days to 500 and 600 kcal/day for women and men, respectively. In both the 5:2 IER and LCHF groups, women and men consumed an average daily caloric intake of 1600 and 2000 kcal/day, respectively, over 7 days. The 5:2 diet was based on Nordic Nutrition Recommendations [90] and consisted of 45–60%, 25%, and 10–20% energy from carbohydrates, fat, and protein [89]. The LCHF diet consisted of 5–10%, 50–80%, and 15–40% of energy from carbohydrates, fat, and protein, respectively. Patients in the SoC arm received advice to follow a healthy diet, increase intake of unsaturated fat while reducing intake of saturated fat, reduce sweets, limit portion sizes, and eat three meals per day, although adherence to these recommendations was not assessed. Change in liver steatosis was measured by magnetic resonance spectroscopy and liver stiffness was assessed by radiology or FibroScan®. Patients following either the 5:2 IER or LCHF diet achieved reductions in steatosis and body weight (−7.4%, 95% CI: −8.7 to −6.2% for IER and −7.7%, 95% CI: −10.0 to −5.4% for LCHF) as compared to SoC (−2.6%, 95% CI: −3.7 to −1.5%), but only patients in the 5:2 IER and SoC groups attained reduced liver stiffness.
Collectively, these results suggest that IF may be a promising therapy for reducing body weight, liver steatosis, and liver stiffness in patients with NAFLD. Given differences in methodologies, whereby not all studies assessed or reported differences in total energy or macronutrient intake, it is unknown whether differences in outcomes between the groups were related to timing of IF protocol, related energy restriction, or related changes in diet composition. More and longer-term studies are needed to assess comparative efficacy of various IF protocols versus emerging pharmacotherapies, adherence to IF, and long-term responses.
6. Potential Risks of Intermittent Fasting
Despite potential benefits of IF, the practice may not be appropriate for all patients or populations. First, while evidence on the effects of fasting on mothers and offspring during pregnancy is emerging, it is conflicting, and long-term effects are not known. Therefore, IF during gestation should be advised against until more substantial evidence is available. Second, although IF appears safe for people with type 2 diabetes [19,91], caution is warranted for anyone taking glucose-lowering medication. These patients should be followed closely by their healthcare providers to ensure proper monitoring and adjustments to their glucose-lowering medications, as needed. Finally, all patients should be made aware of potential physical or psychosocial effects of IF. Side effects that have been reported in studies of IF include reduced energy levels, headache, presyncope, decreased concentration, mood swings or bad temper, feeling cold, constipation, bad breath, and preoccupation with food [26,27].
7. Conclusions
Obesity has an integral role in development of NAFLD. Sustainable weight loss remains challenging for most patients, and there is rationale from preclinical studies as to potential benefits and mechanisms of IF to ameliorate metabolic disturbances, influence the gut microbiome and bacterial translocation, and contribute to modest weight loss. While epidemiological and clinical trial data were encouraging for clinical benefits of IF on various metabolic and inflammatory markers in humans, there were limited data for effects in human subjects with NAFLD. High-quality clinical studies of patients with NAFLD are needed to identify mechanisms of action as well as effectiveness, safety, and efficacy of IF in this population. Priorities for future research include the impact of IF on long-term natural history, fibrosis regression, potential effect modification between diet and pharmacologic therapy, and comparative efficacy of different IF protocols. Furthermore, those studies should also evaluate dietary intake during feeding periods, measured through validated food frequency questionnaires and/or 24 h recalls, to inform an optimal dietary pattern in the setting of IF interventions.
Author Contributions
C.M.L. and A.B.: Contributed to conception of the work, searched the literature, drafted the original version, and revised and gave intellectual input to the manuscript. C.M.: Revised and gave intellectual input to the manuscript. M.R.: Contributed to conception of the work, searched the literature, drafted the original version, and revised and gave intellectual input to the manuscript. All authors have read and agreed to the published version of the manuscript.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Chooi Y.C., Ding C., Magkos F. The epidemiology of obesity. Metabolism. 2019;92:6–10. doi: 10.1016/j.metabol.2018.09.005. [DOI] [PubMed] [Google Scholar]
- 2.Lumeng C.N., Saltiel A.R. Inflammatory links between obesity and metabolic disease. J. Clin. Invest. 2011;121:2111–2117. doi: 10.1172/JCI57132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chalasani N., Younossi Z., Lavine J.E., Charlton M., Cusi K., Rinella M., Harrison S.A., Brunt E.M., Sanyal A.J. The diagnosis and management of nonalcoholic fatty liver disease: Practice guidance from the American Association for the Study of Liver Diseases. Hepatology. 2018;67:328–357. doi: 10.1002/hep.29367. [DOI] [PubMed] [Google Scholar]
- 4.Younossi Z.M., Koenig A.B., Abdelatif D., Fazel Y., Henry L., Wymer M. Global epidemiology of nonalcoholic fatty liver disease—Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64:73–84. doi: 10.1002/hep.28431. [DOI] [PubMed] [Google Scholar]
- 5.Liu J., Tian Y., Fu X., Mu C., Yao M., Ni Y., Liu Y., Li Z. Estimating global prevalence, incidence, and outcomes of non-alcoholic fatty liver disease from 2000 to 2021: Systematic review and meta-analysis. Chin. Med. J. 2022;135:1682–1691. doi: 10.1097/CM9.0000000000002277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Huang D.Q., El-Serag H.B., Loomba R. Global epidemiology of NAFLD-related HCC: Trends, predictions, risk factors and prevention. Nat. Rev. Gastroenterol. Hepatol. 2021;18:223–238. doi: 10.1038/s41575-020-00381-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fouad Y., Elwakil R., Elsahhar M., Said E., Bazeed S., Ali Gomaa A., Hashim A., Kamal E., Mehrez M., Attia D. The NAFLD-MAFLD debate: Eminence vs evidence. Liver Int. 2021;41:255–260. doi: 10.1111/liv.14739. [DOI] [PubMed] [Google Scholar]
- 8.Younossi Z.M., Corey K.E., Lim J.K. AGA clinical practice update on lifestyle modification using diet and exercise to achieve weight loss in the management of nonalcoholic fatty liver disease: Expert review. Gastroenterology. 2021;160:912–918. doi: 10.1053/j.gastro.2020.11.051. [DOI] [PubMed] [Google Scholar]
- 9.Anderson J.W., Konz E.C., Frederich R.C., Wood C.L. Long-term weight-loss maintenance: A meta-analysis of US studies. Am. J. Clin. Nutr. 2001;74:579–584. doi: 10.1093/ajcn/74.5.579. [DOI] [PubMed] [Google Scholar]
- 10.Malik S., Hamer R., Shabir S., Youssouf S., Morsy M., Rashid R., Waqar S., Ghouri N. Effects of fasting on solid organ transplant recipients during Ramadan—A practical guide for healthcare professionals. Clin. Med. 2021;21:e492–e498. doi: 10.7861/clinmed.2021-0250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Clifton K.K., Ma C.X., Fontana L., Peterson L.L. Intermittent fasting in the prevention and treatment of cancer. CA Cancer J. Clin. 2021;71:527–546. doi: 10.3322/caac.21694. [DOI] [PubMed] [Google Scholar]
- 12.Christensen R.A.G., Kirkham A.A. Time-restricted eating: A novel and simple dietary intervention for primary and secondary prevention of breast cancer and cardiovascular disease. Nutrients. 2021;13:3476. doi: 10.3390/nu13103476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gudden J., Arias Vasquez A., Bloemendaal M. The effects of intermittent fasting on brain and cognitive function. Nutrients. 2021;13:3166. doi: 10.3390/nu13093166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Obert J., Pearlman M., Obert L., Chapin S. Popular weight loss strategies: A review of four weight loss techniques. Curr. Gastroenterol. Rep. 2017;19:61. doi: 10.1007/s11894-017-0603-8. [DOI] [PubMed] [Google Scholar]
- 15.Yeoh E.C., Zainudin S.B., Loh W.N., Chua C.L., Fun S., Subramaniam T., Sum C.F., Lim S.C. Fasting during Ramadan and associated changes in glycaemia, caloric intake and body composition with gender differences in Singapore. Ann. Acad. Med. Singap. 2015;44:202–206. doi: 10.47102/annals-acadmedsg.V44N6p202. [DOI] [PubMed] [Google Scholar]
- 16.Aksungar F.B., Eren A., Ure S., Teskin O., Ates G. Effects of intermittent fasting on serum lipid levels, coagulation status and plasma homocysteine levels. Ann. Nutr. Metab. 2005;49:77–82. doi: 10.1159/000084739. [DOI] [PubMed] [Google Scholar]
- 17.Aksungar F.B., Topkaya A.E., Akyildiz M. Interleukin-6, C-reactive protein and biochemical parameters during prolonged intermittent fasting. Ann. Nutr. Metab. 2007;51:88–95. doi: 10.1159/000100954. [DOI] [PubMed] [Google Scholar]
- 18.Faris M.A., Kacimi S., Al-Kurd R.A., Fararjeh M.A., Bustanji Y.K., Mohammad M.K., Salem M.L. Intermittent fasting during Ramadan attenuates proinflammatory cytokines and immune cells in healthy subjects. Nutr. Res. 2012;32:947–955. doi: 10.1016/j.nutres.2012.06.021. [DOI] [PubMed] [Google Scholar]
- 19.Wang X., Li Q., Liu Y., Jiang H., Chen W. Intermittent fasting versus continuous energy-restricted diet for patients with type 2 diabetes mellitus and metabolic syndrome for glycemic control: A systematic review and meta-analysis of randomized controlled trials. Diabetes Res. Clin. Pract. 2021;179:109003. doi: 10.1016/j.diabres.2021.109003. [DOI] [PubMed] [Google Scholar]
- 20.Cienfuegos S., Gabel K., Kalam F., Ezpeleta M., Wiseman E., Pavlou V., Lin S., Oliveira M.L., Varady K.A. Effects of 4- and 6-h time-restricted feeding on weight and cardiometabolic health: A randomized controlled trial in adults with obesity. Cell Metab. 2020;32:366–378.e3. doi: 10.1016/j.cmet.2020.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Johnson J.B., Summer W., Cutler R.G., Martin B., Hyun D.H., Dixit V.D., Pearson M., Nassar M., Telljohann R., Maudsley S., et al. Alternate day calorie restriction improves clinical findings and reduces markers of oxidative stress and inflammation in overweight adults with moderate asthma. Free Radic. Biol. Med. 2007;42:665–674. doi: 10.1016/j.freeradbiomed.2006.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Patikorn C., Roubal K., Veettil S.K., Chandran V., Pham T., Lee Y.Y., Giovannucci E.L., Varady K.A., Chaiyakunapruk N. Intermittent fasting and obesity-related health outcomes: An umbrella review of meta-analyses of randomized clinical trials. JAMA Netw. Open. 2021;4:e2139558. doi: 10.1001/jamanetworkopen.2021.39558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cignarella F., Cantoni C., Ghezzi L., Salter A., Dorsett Y., Chen L., Phillips D., Weinstock G.M., Fontana L., Cross A.H., et al. Intermittent fasting confers protection in CNS autoimmunity by altering the gut microbiota. Cell Metab. 2018;27:1222–1235.e6. doi: 10.1016/j.cmet.2018.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Varady K.A., Bhutani S., Klempel M.C., Kroeger C.M., Trepanowski J.F., Haus J.M., Hoddy K.K., Calvo Y. Alternate day fasting for weight loss in normal weight and overweight subjects: A randomized controlled trial. Nutr. J. 2013;12:146. doi: 10.1186/1475-2891-12-146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Trepanowski J.F., Kroeger C.M., Barnosky A., Klempel M.C., Bhutani S., Hoddy K.K., Gabel K., Freels S., Rigdon J., Rood J., et al. Effect of alternate-day fasting on weight loss, weight maintenance, and cardioprotection among metabolically healthy obese adults: A randomized clinical trial. JAMA Intern. Med. 2017;177:930–938. doi: 10.1001/jamainternmed.2017.0936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Harvie M.N., Pegington M., Mattson M.P., Frystyk J., Dillon B., Evans G., Cuzick J., Jebb S.A., Martin B., Cutler R.G., et al. The effects of intermittent or continuous energy restriction on weight loss and metabolic disease risk markers: A randomized trial in young overweight women. Int. J. Obes. 2011;35:714–727. doi: 10.1038/ijo.2010.171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Harvie M., Wright C., Pegington M., McMullan D., Mitchell E., Martin B., Cutler R.G., Evans G., Whiteside S., Maudsley S., et al. The effect of intermittent energy and carbohydrate restriction v. daily energy restriction on weight loss and metabolic disease risk markers in overweight women. Br. J. Nutr. 2013;110:1534–1547. doi: 10.1017/S0007114513000792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ottery F.D. Definition of standardized nutritional assessment and interventional pathways in oncology. Nutrition. 1996;12((Suppl. S1)):S15–S19. doi: 10.1016/0899-9007(95)00067-4. [DOI] [PubMed] [Google Scholar]
- 29.Zickgraf H.F., Ellis J.M. Initial validation of the nine item avoidant/restrictive food intake disorder screen (NIAS): A measure of three restrictive eating patterns. Appetite. 2018;123:32–42. doi: 10.1016/j.appet.2017.11.111. [DOI] [PubMed] [Google Scholar]
- 30.Chan S.S.M., Chen Y., Casey K., Olen O., Ludvigsson J.F., Carbonnel F., Oldenburg B., Gunter M.J., Tjønneland A., Grip O. Obesity is associated with increased risk of Crohn’s disease, but not ulcerative colitis: A pooled analysis of five prospective cohort studies. Clin. Gastroenterol. Hepatol. 2021;20:1048–1058. doi: 10.1016/j.cgh.2021.06.049. [DOI] [PubMed] [Google Scholar]
- 31.Chen X., Kondo K., Motoki K., Homma H., Okazawa H. Fasting activates macroautophagy in neurons of Alzheimer’s disease mouse model but is insufficient to degrade amyloid-beta. Sci. Rep. 2015;5:12115. doi: 10.1038/srep12115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Corrêa L.H., Heyn G.S., Magalhaes K.G. The impact of the adipose organ plasticity on inflammation and cancer progression. Cells. 2019;8:662. doi: 10.3390/cells8070662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Frank J., Gupta A., Osadchiy V., Mayer E.A. Brain-gut-microbiome interactions and intermittent fasting in obesity. Nutrients. 2021;13:584. doi: 10.3390/nu13020584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jamshed H., Beyl R.A., Della Manna D.L., Yang E.S., Ravussin E., Peterson C.M. Early time-restricted feeding improves 24-hour glucose levels and affects markers of the circadian clock, aging, and autophagy in humans. Nutrients. 2019;11:1234. doi: 10.3390/nu11061234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kim K.H., Kim Y.H., Son J.E., Lee J.H., Kim S., Choe M.S., Moon J.H., Zhong J., Fu K., Lenglin F., et al. Intermittent fasting promotes adipose thermogenesis and metabolic homeostasis via VEGF-mediated alternative activation of macrophage. Cell Res. 2017;27:1309–1326. doi: 10.1038/cr.2017.126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Li G., Xie C., Lu S., Nichols R.G., Tian Y., Li L., Patel D., Ma Y., Brocker C.N., Yan T., et al. Intermittent fasting promotes white adipose browning and decreases obesity by shaping the gut microbiota. Cell Metab. 2017;26:672–685.e4. doi: 10.1016/j.cmet.2017.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Manoogian E.N.C., Panda S. Circadian rhythms, time-restricted feeding, and healthy aging. Ageing Res. Rev. 2017;39:59–67. doi: 10.1016/j.arr.2016.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zhang X., Zou Q., Zhao B., Zhang J., Zhao W., Li Y., Liu R., Liu X., Liu Z. Effects of alternate-day fasting, time-restricted fasting and intermittent energy restriction DSS-induced on colitis and behavioral disorders. Redox Biol. 2020;32:101535. doi: 10.1016/j.redox.2020.101535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhang X., Zou Q., Zhao B., Zhang J., Zhao W., Li Y., Liu R., Liu X., Liu Z. Corrigendum to “Effects of alternate-day fasting, time-restricted fasting and intermittent energy restriction DSS-induced on colitis and behavioral disorders”. Redox Biol. 2021;44:101955. doi: 10.1016/j.redox.2021.101955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cuevas-Sierra A., Ramos-Lopez O., Riezu-Boj J.I., Milagro F.I., Martinez J.A. Diet, gut microbiota, and obesity: Links with host genetics and epigenetics and potential applications. Adv. Nutr. 2019;10((Suppl. S1)):S17–S30. doi: 10.1093/advances/nmy078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lu G., Wang Y., Shi Y., Zhang Z., Huang C., He W., Wang C., Shen H.M. Autophagy in health and disease: From molecular mechanisms to therapeutic target. MedComm. 2022;3:e150. doi: 10.1002/mco2.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Liu C.M., Kanoski S.E. Homeostatic and non-homeostatic controls of feeding behavior: Distinct vs. common neural systems. Physiol. Behav. 2018;193 Pt B:223–231. doi: 10.1016/j.physbeh.2018.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Almoosawi S., Vingeliene S., Karagounis L.G., Pot G.K. Chrono-nutrition: A review of current evidence from observational studies on global trends in time-of-day of energy intake and its association with obesity. Proc. Nutr. Soc. 2016;75:487–500. doi: 10.1017/S0029665116000306. [DOI] [PubMed] [Google Scholar]
- 44.Bahijri S., Borai A., Ajabnoor G., Abdul Khaliq A., AlQassas I., Al-Shehri D., Chrousos G. Relative metabolic stability, but disrupted circadian cortisol secretion during the fasting month of Ramadan. PLoS ONE. 2013;8:e60917. doi: 10.1371/annotation/8d92315c-9944-4470-9bbb-806a26b0809b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Loft A., Schmidt S.F., Caratti G., Stifel U., Havelund J., Sekar R., Kwon Y., Sulaj A., Chow K.K., Alfaro A.J., et al. A macrophage-hepatocyte glucocorticoid receptor axis coordinates fasting ketogenesis. Cell Metab. 2022;34:473–486.e9. doi: 10.1016/j.cmet.2022.01.004. [DOI] [PubMed] [Google Scholar]
- 46.Kettner N.M., Voicu H., Finegold M.J., Coarfa C., Sreekumar A., Putluri N., Katchy C.A., Lee C., Moore D.D., Fu L. Circadian homeostasis of liver metabolism suppresses hepatocarcinogenesis. Cancer Cell. 2016;30:909–924. doi: 10.1016/j.ccell.2016.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chaix A., Lin T., Le H.D., Chang M.W., Panda S. Time-restricted feeding prevents obesity and metabolic syndrome in mice lacking a circadian clock. Cell Metab. 2019;29:303–319.e4. doi: 10.1016/j.cmet.2018.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kershaw E.E., Flier J.S. Adipose tissue as an endocrine organ. J. Clin. Endocrinol. Metab. 2004;89:2548–2556. doi: 10.1210/jc.2004-0395. [DOI] [PubMed] [Google Scholar]
- 49.Saely C.H., Geiger K., Drexel H. Brown versus white adipose tissue: A mini-review. Gerontology. 2012;58:15–23. doi: 10.1159/000321319. [DOI] [PubMed] [Google Scholar]
- 50.Cannon B., Nedergaard J. Nonshivering thermogenesis and its adequate measurement in metabolic studies. Pt 2J. Exp. Biol. 2011;214:242–253. doi: 10.1242/jeb.050989. [DOI] [PubMed] [Google Scholar]
- 51.Maurizi G., Della Guardia L., Maurizi A., Poloni A. Adipocytes properties and crosstalk with immune system in obesity-related inflammation. J. Cell Physiol. 2018;233:88–97. doi: 10.1002/jcp.25855. [DOI] [PubMed] [Google Scholar]
- 52.Sahu B., Bal N.C. Adipokines from white adipose tissue in regulation of whole body energy homeostasis. Biochimie. 2022 doi: 10.1016/j.biochi.2022.09.003. in press . [DOI] [PubMed] [Google Scholar]
- 53.Le Jemtel T.H., Samson R., Milligan G., Jaiswal A., Oparil S. Visceral adipose tissue accumulation and residual cardiovascular risk. Curr. Hypertens. Rep. 2018;20:77. doi: 10.1007/s11906-018-0880-0. [DOI] [PubMed] [Google Scholar]
- 54.Heilbronn L.K., Smith S.R., Martin C.K., Anton S.D., Ravussin E. Alternate-day fasting in nonobese subjects: Effects on body weight, body composition, and energy metabolism. Am. J. Clin. Nutr. 2005;81:69–73. doi: 10.1093/ajcn/81.1.69. [DOI] [PubMed] [Google Scholar]
- 55.Klempel M.C., Kroeger C.M., Bhutani S., Trepanowski J.F., Varady K.A. Intermittent fasting combined with calorie restriction is effective for weight loss and cardio-protection in obese women. Nutr. J. 2012;11:98. doi: 10.1186/1475-2891-11-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kim D., Chung G.E., Kwak M.S., Seo H.B., Kang J.H., Kim W., Kim Y.J., Yoon J.H., Lee H.S., Kim C.Y. Body fat distribution and risk of incident and regressed nonalcoholic fatty liver disease. Clin Gastroenterol Hepatol. 2016;14:132–138.e4. doi: 10.1016/j.cgh.2015.07.024. [DOI] [PubMed] [Google Scholar]
- 57.van der Poorten D., Milner K.L., Hui J., Hodge A., Trenell M.I., Kench J.G., London R., Peduto T., Chisholm D.J., George J. Visceral fat: A key mediator of steatohepatitis in metabolic liver disease. Hepatology. 2008;48:449–457. doi: 10.1002/hep.22350. [DOI] [PubMed] [Google Scholar]
- 58.Saponaro C., Sabatini S., Gaggini M., Carli F., Rosso C., Positano V., Armandi A., Caviglia G.P., Faletti R., Bugianesi E., et al. Adipose tissue dysfunction and visceral fat are associated with hepatic insulin resistance and severity of NASH even in lean individuals. Liver Int. 2022;42:2418–2427. doi: 10.1111/liv.15377. [DOI] [PubMed] [Google Scholar]
- 59.Acierno C., Caturano A., Pafundi P.C., Nevola R., Adinolfi L.E., Sasso F.C. Nonalcoholic fatty liver disease and type 2 diabetes: Pathophysiological mechanisms shared between the two faces of the same coin. Explor. Med. 2020;1:287–306. [Google Scholar]
- 60.Le Dréan G., Haure-Mirande V., Ferrier L., Bonnet C., Hulin P., de Coppet P., Segain J.P. Visceral adipose tissue and leptin increase colonic epithelial tight junction permeability via a RhoA-ROCK-dependent pathway. Faseb. J. 2014;28:1059–1070. doi: 10.1096/fj.13-234203. [DOI] [PubMed] [Google Scholar]
- 61.Paeschke A., Erben U., Kredel L.I., Kühl A.A., Siegmund B. Role of visceral fat in colonic inflammation: From Crohn’s disease to diverticulitis. Curr. Opin. Gastroenterol. 2017;33:53–58. doi: 10.1097/MOG.0000000000000324. [DOI] [PubMed] [Google Scholar]
- 62.Trepanowski J.F., Kroeger C.M., Barnosky A., Klempel M., Bhutani S., Hoddy K.K., Rood J., Ravussin E., Varady K.A. Effects of alternate-day fasting or daily calorie restriction on body composition, fat distribution, and circulating adipokines: Secondary analysis of a randomized controlled trial. Clin. Nutr. 2018;37 Pt A:1871–1878. doi: 10.1016/j.clnu.2017.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Khan M.T., Nieuwdorp M., Bäckhed F. Microbial modulation of insulin sensitivity. Cell Metab. 2014;20:753–760. doi: 10.1016/j.cmet.2014.07.006. [DOI] [PubMed] [Google Scholar]
- 64.Bäckhed F., Ding H., Wang T., Hooper L.V., Koh G.Y., Nagy A., Semenkovich C.F., Gordon J.I. The gut microbiota as an environmental factor that regulates fat storage. Proc. Natl. Acad. Sci. USA. 2004;101:15718–15723. doi: 10.1073/pnas.0407076101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Lee C.J., Sears C.L., Maruthur N. Gut microbiome and its role in obesity and insulin resistance. Ann. N. Y. Acad. Sci. 2020;1461:37–52. doi: 10.1111/nyas.14107. [DOI] [PubMed] [Google Scholar]
- 66.Everard A., Belzer C., Geurts L., Ouwerkerk J.P., Druart C., Bindels L.B., Guiot Y., Derrien M., Muccioli G.G., Delzenne N.M. Cross-talk between Akkermansia muciniphila and intestinal epithelium controls diet-induced obesity. Proc. Natl. Acad. Sci. USA. 2013;110:9066–9071. doi: 10.1073/pnas.1219451110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Xiao H., Kang S. The role of the gut microbiome in energy balance with a focus on the gut-adipose tissue axis. Front Genet. 2020;11:297. doi: 10.3389/fgene.2020.00297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Özdemir A., Yozgat A., Işgın-Atıcı K., Avcı E., Yıldız B.D., Gündoğdu A., Nalbantoğlu U., Turhan T., Doğruman-Al F., Büyüktuncer Z. Potential associations between alterations in gut microbiome and obesity-related traits after the bariatric surgery. J. Hum. Nutr. Diet. 2022;80:OCE2. doi: 10.1111/jhn.13087. [DOI] [PubMed] [Google Scholar]
- 69.Rinaldi L., Pafundi P.C., Galiero R., Caturano A., Morone M.V., Silvestri C., Giordano M., Salvatore T., Sasso F.C. Mechanisms of non-alcoholic fatty liver disease in the metabolic syndrome. A narrative review. Antioxidants. 2021;10:270. doi: 10.3390/antiox10020270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Özkul C., Yalınay M., Karakan T. Islamic fasting leads to an increased abundance of Akkermansia muciniphila and Bacteroides fragilis group: A preliminary study on intermittent fasting. Turk. J. Gastroenterol. 2019;30:1030–1035. doi: 10.5152/tjg.2019.19185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Rong B., Wu Q., Saeed M., Sun C. Gut microbiota-a positive contributor in the process of intermittent fasting-mediated obesity control. Anim. Nutr. 2021;7:1283–1295. doi: 10.1016/j.aninu.2021.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Rosenbaum M., Knight R., Leibel R.L. The gut microbiota in human energy homeostasis and obesity. Trends Endocrinol. Metab. 2015;26:493–501. doi: 10.1016/j.tem.2015.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Cani P.D., Bibiloni R., Knauf C., Waget A., Neyrinck A.M., Delzenne N.M., Burcelin R. Changes in gut microbiota control metabolic endotoxemia-induced inflammation in high-fat diet-induced obesity and diabetes in mice. Diabetes. 2008;57:1470–1481. doi: 10.2337/db07-1403. [DOI] [PubMed] [Google Scholar]
- 74.Nier A., Huber Y., Labenz C., Michel M., Bergheim I., Schattenberg J.M. Adipokines and endotoxemia correlate with hepatic steatosis in non-alcoholic fatty liver disease (NAFLD) Nutrients. 2020;12:699. doi: 10.3390/nu12030699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Liu Z., Dai X., Zhang H., Shi R., Hui Y., Jin X., Zhang W., Wang L., Wang Q., Wang D., et al. Gut microbiota mediates intermittent-fasting alleviation of diabetes-induced cognitive impairment. Nat. Commun. 2020;11:855. doi: 10.1038/s41467-020-14676-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Galluzzi L., Baehrecke E.H., Ballabio A., Boya P., Bravo-San Pedro J.M., Cecconi F., Choi A.M., Chu C.T., Codogno P., Colombo M.I., et al. Molecular definitions of autophagy and related processes. Embo. J. 2017;36:1811–1836. doi: 10.15252/embj.201796697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Kroemer G., Mariño G., Levine B. Autophagy and the integrated stress response. Mol. Cell. 2010;40:280–293. doi: 10.1016/j.molcel.2010.09.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Glick D., Barth S., Macleod K.F. Autophagy: Cellular and molecular mechanisms. J. Pathol. 2010;221:3–12. doi: 10.1002/path.2697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Madorsky I., Opalach K., Waber A., Verrier J.D., Solmo C., Foster T., Dunn W.A., Jr., Notterpek L. Intermittent fasting alleviates the neuropathic phenotype in a mouse model of Charcot-Marie-Tooth disease. Neurobiol. Dis. 2009;34:146–154. doi: 10.1016/j.nbd.2009.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Arab J.P., Dirchwolf M., Álvares-da-Silva M.R., Barrera F., Benítez C., Castellanos-Fernandez M., Castro-Narro G., Chavez-Tapia N., Chiodi D., Cotrim H., et al. Latin American Association for the Study of the Liver (ALEH) practice guidance for the diagnosis and treatment of non-alcoholic fatty liver disease. Ann. Hepatol. 2020;19:674–690. doi: 10.1016/j.aohep.2020.09.006. [DOI] [PubMed] [Google Scholar]
- 81.European Association for the Study of the Liver (EASL) European Association for the Study of Diabetes (EASD) European Association for the Study of Obesity (EASO) EASL-EASD-EASO Clinical Practice Guidelines for the management of non-alcoholic fatty liver disease. J. Hepatol. 2016;64:1388–1402. doi: 10.1016/j.jhep.2015.11.004. [DOI] [PubMed] [Google Scholar]
- 82.Saeed N., Nadeau B., Shannon C., Tincopa M. Evaluation of dietary approaches for the treatment of non-alcoholic fatty liver disease: A systematic review. Nutrients. 2019;11:3064. doi: 10.3390/nu11123064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Chung H., Chou W., Sears D.D., Patterson R.E., Webster N.J., Ellies L.G. Time-restricted feeding improves insulin resistance and hepatic steatosis in a mouse model of postmenopausal obesity. Metabolism. 2016;65:1743–1754. doi: 10.1016/j.metabol.2016.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Elsayed H.R.H., El-Nablaway M., Khattab B.A., Sherif R.N., Elkashef W.F., Abdalla A.M., El Nashar E.M., Abd-Elmonem M.M., El-Gamal R. Independent of calorie intake, short-term alternate-day fasting alleviates NASH, with modulation of markers of lipogenesis, autophagy, apoptosis, and inflammation in rats. J. Histochem. Cytochem. 2021;69:575–596. doi: 10.1369/00221554211041607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Aliasghari F., Izadi A., Gargari B.P., Ebrahimi S. The effects of Ramadan fasting on body composition, blood pressure, glucose metabolism, and markers of inflammation in NAFLD patients: An observational trial. J. Am. Coll. Nutr. 2017;36:640–645. doi: 10.1080/07315724.2017.1339644. [DOI] [PubMed] [Google Scholar]
- 86.Mari A., Khoury T., Baker M., Said Ahmad H., Abu Baker F., Mahamid M. The impact of Ramadan fasting on fatty liver disease severity: A retrospective case control study from Israel. Isr. Med. Assoc. J. 2021;23:94–98. [PubMed] [Google Scholar]
- 87.Cai H., Qin Y.L., Shi Z.Y., Chen J.H., Zeng M.J., Zhou W., Chen R.Q., Chen Z.Y. Effects of alternate-day fasting on body weight and dyslipidaemia in patients with non-alcoholic fatty liver disease: A randomised controlled trial. BMC Gastroenterol. 2019;19:219. doi: 10.1186/s12876-019-1132-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Johari M.I., Yusoff K., Haron J., Nadarajan C., Ibrahim K.N., Wong M.S., Hafidz M.I.A., Chua B.E., Hamid N., Arifin W.N., et al. A randomised controlled trial on the effectiveness and adherence of modified alternate-day calorie restriction in improving activity of non-alcoholic fatty liver disease. Sci. Rep. 2019;9:11232. doi: 10.1038/s41598-019-47763-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Holmer M., Lindqvist C., Petersson S., Moshtaghi-Svensson J., Tillander V., Brismar T.B., Hagström H., Stål P. Treatment of NAFLD with intermittent calorie restriction or low-carb high-fat diet—A randomised controlled trial. JHEP Rep. 2021;3:100256. doi: 10.1016/j.jhepr.2021.100256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Nordic Council of Ministers . Nordic Nutrition Recommendations 2012: Integrating Nutrition and Physical Activity. 5th ed. Nordisk Ministerråd; Copenhagen, Denmark: 2014. 627p [Google Scholar]
- 91.Kahleova H., Belinova L., Malinska H., Oliyarnyk O., Trnovska J., Skop V., Kazdova L., Dezortova M., Hajek M., Tura A., et al. Eating two larger meals a day (breakfast and lunch) is more effective than six smaller meals in a reduced-energy regimen for patients with type 2 diabetes: A randomised crossover study. Diabetologia. 2014;57:1552–1560. doi: 10.1007/s00125-014-3253-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.