Abstract
The primary functional units of the thyroid gland are follicles of various sizes comprised of a monolayer of epithelial cells (thyrocytes) surrounding an apical extracellular cavity known as the follicle lumen. In the normal thyroid gland, the follicle lumen is filled with secreted protein (referred to as colloid), comprised nearly exclusively of thyroglobulin with a half-life ranging from days to weeks. At the cellular boundary of the follicle lumen, secreted thyroglobulin becomes iodinated, resulting from the coordinated activities of enzymes localized to the thyrocyte apical plasma membrane. Thyroglobulin appearance in evolution is essentially synchronous with the appearance of the follicular architecture of the vertebrate thyroid gland. Thyroglobulin is the most highly expressed thyroid gene and represents the most abundantly expressed thyroid protein. Wildtype thyroglobulin protein is a large and complex glycoprotein that folds in the endoplasmic reticulum, leading to homodimerization and export via the classical secretory pathway to the follicle lumen. However, of the hundreds of human thyroglobulin genetic variants, most exhibit increased susceptibility to misfolding with defective export from the endoplasmic reticulum, triggering hypothyroidism as well as thyroidal endoplasmic reticulum stress. The human disease of hypothyroidism with defective thyroglobulin (either homozygous, or compound heterozygous) can be experimentally modeled in thyrocyte cell culture, or in whole animals, such as mice that are readily amenable to genetic manipulation. From a combination of approaches, it can be demonstrated that in the setting of thyroglobulin misfolding, thyrocytes under chronic continuous ER stress exhibit increased susceptibility to cell death, with interesting cell biological and pathophysiological consequences.
Keywords: endoplasmic reticulum, ER stress, secretory pathway, hormonogenesis, cell death
1. Role of the Endoplasmic Reticulum in Secretory Protein Synthesis and Intracellular Transport
The protein biosynthetic apparatus of cells is tightly linked to the differentiated phenotype of eukaryotic cells and tissues, by regulating the abundance and delivery of new proteins to the various organelles that control cellular function. Successful protein targeting to specific intracellular and extracellular destinations is dependent upon targeting information encoded with the polypeptide structure, and cellular machinery designed to ‘read’ that targeting information. The failure to either properly present or read such information provides an important entrance into the pathobiology of disease [1].
The endoplasmic reticulum (ER) is one of the largest organelles in eukaryotic cells. ER function contributes to multiple activities including protein synthesis, folding, and transport, as well as lipid and steroid synthesis, carbohydrate metabolism, and calcium storage [2], whereas ER dysfunction contributes to a large variety of diseases [3]. Proteins that follow the classical protein secretion pathway begin their life within the ER, and they remain intracellularly enclosed within specific membrane-bound compartments and vesicular-tubular transport intermediates as they migrate through the cytoplasm; at each successive station along this route, iterative decisions are made on the basis of anterograde transport signal-mechanisms (e.g., [4]) and retention signal-mechanisms (e.g., [5]). The process begins with translation of secretory proteins on the cytosolic side of the ER membrane; ribosomes reading secretory protein mRNAs are recruited to the ER membrane via recognition and binding of the of the signal peptide to the signal recognition particle (SRP) for delivery of the nascent polypeptide to the SRP receptor on the ER membrane [6]. The continuation of translation at the ER is coupled to co-translational translocation of the nascent polypeptide across the ER membrane [7]. During the translocation process, signal peptidase excises the short signal peptide [8], permitting subsequent steps in the nascent secretory maturation process within the ER lumen, including N-linked glycosylation [9], disulfide bond formation [10], and oligomerization [11]—each event stimulated via a number of ER molecular chaperones and folding enzymes [12,13]. These ER resident proteins contribute to a quality control function such that properly folded secretory proteins are allowed anterograde advance towards the Golgi complex, but those proteins that do not achieve an acceptable conformation are retained within the ER [14,15] and can subsequently become available for ER-associated degradation (ERAD, [16]), degradative ER-phagy [17], or may remain undegraded [18].
These general principles are not unique to thyrocytes, yet these cells do exhibit a uniquely high expression of a subset of gene products that encode thyroid-specific function, leading to the synthesis of thyroid hormones. Although thyroid hormone synthesis in lower organisms takes place in the absence of an organized thyroid gland architecture, in vertebrates, thyroid hormone synthesis occurs in thyroid follicles, each representing the basic functional unit of the thyroid gland, and each expressing the thyroglobulin (Tg) protein [19,20]. The thyroid follicle is composed of an epithelial monolayer of polarized thyrocytes with the basolateral surface facing the bloodstream and the apical surface delimiting a central cavity known as the follicle lumen; and it is primarily in this apical extracellular space wherein protein iodination leading to the formation of mono-iodotyrosine (MIT), di-iodotyrosine (DIT), and the thyroid hormones thyroxine (T4) and tri-iodothyronine (T3) actually takes place [21,22]. In the vertebrate thyroid gland, efficient production of thyroid hormones requires the proper synthesis, folding, and transport of Tg, the most abundantly expressed thyroid-specific gene product. Differentiated thyrocytes are powerfully dedicated to the biosynthesis of the Tg glycoprotein [23], which normally accounts for more than half of all the protein in the thyroid gland [24,25]. The newly-synthesized Tg protein is delivered via a short signal peptide to the ER lumen [26], wherein the protein acquires multiple N-linked glycans [27] and disulfide bonds [28] en route to formation of folded Tg monomers [19]. Due to the large size of the Tg polypeptide (~2750 residues), the post-translational Tg folding process is slow [29], involving a series of Tg folding intermediates [23], accompanied by extensive interaction with ER resident proteins participating in protein folding and quality control [30]. Perhaps unsurprisingly, amongst the most important of these ER resident proteins are BiP (the ER member of the hsp70 family [29]) as well as ER oxidoreductases ERp57, PDI, P5, and ERp72 [31,32], which are all highly abundantly expressed in the ER lumen. Most likely, different chaperone complexes and subcomplexes are involved with distinct regions of the Tg protein, and kinetically at different times during the Tg folding process [33]. Ultimately, significant Tg monomer folding is required for proper presentation of the Tg dimer interface necessary for homodimerization [34,35], which is a step that occurs largely, if not exclusively, prior to anterograde export from the ER [36].
2. Tg Folding and TG Mutations That Trigger Misfolding
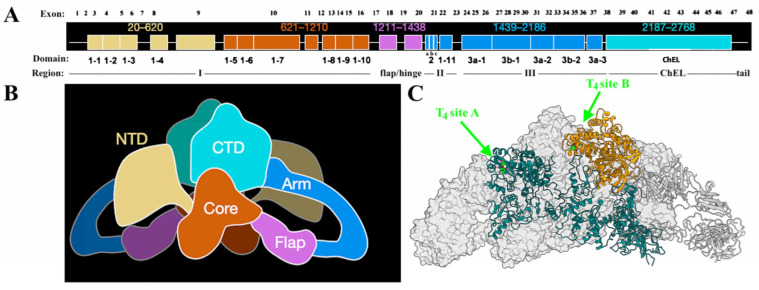
The organization of the TG gene and its 48 exons [37], as well as proven or predicted mutations that affect the Tg protein sequence [38] have been well described elsewhere. Here, we offer a few additional observations that have emerged from recent studies.
After cleavage of its signal peptide, Tg is initially synthesized as a monomeric protein (whose primary structure has been divided into regions) although the final native structure is actually a homodimer [36]. The first ~80% of the Tg protein has been described informally as I-II-III [39] because it contains the first 10 Tg type 1 repeats in region I (each repeat is defined largely by the arrangement of cysteine residues that form internal disulfide bonds), separated by a flap/hinge region, from three short type 2 repeats, plus a final type 1 repeat in region II and followed by five Tg type 3 repeats in region III (Figure 1A; each of these repeats also forms internal disulfide bonds). The Tg protein concludes with the Cholinesterase-Like domain (ChEL, bearing three internal disulfide bonds) plus a short unique tail sequence (Figure 1A). Four recent papers have provided new insight into the three-dimensional structure of Tg (two human; two bovine) by modeling from cryogenic electron microscopy [28,34,40,41], and schematic of the 3D structure is shown in Figure 1B. Specifically, when the color-coded image of Figure 1B is considered alongside the color-coded primary structure of Tg in Figure 1A, it becomes apparent that globally, the monomer structure has an overall J-like shape, in which region I is roughly equally divided into an ‘N-terminal domain’ encoded by the first 9 exons (of a total of 48), and what has been called the ‘core domain’ is encoded by the next 7 exons. The following flap/hinge region essentially bisects the entire Tg monomer sequence, leading to an ‘arm domain’ encoded by 17 exons, which contains all of the Tg type 2 and type 3 repeats (as well as a single, 11th, type 1 repeat). The ‘C-terminal domain’ plus the short unique tail sequence together (encoded by the last 10 exons) contains one of the two preferred sites for the de novo formation of T4 as well as the one preferred site for the de novo formation of T3 [42]. Thus far, only one cryo-EM study has reported the successful simultaneous visualization of both of the two most-utilized sites for the de novo formation of thyroxine, including the most-important “site A” in the N-terminal domain, and the second-most- important “site B” in the ChEL domain (Figure 1C, [40]). The exons encoding these regionally distinct domains of Tg are likely to have distinct evolutionary ancestry, although the origins of these “pieces” of the Tg gene residing in invertebrates have not all been definitively identified [20].
Figure 1.
Thyroglobulin Organization (panel (A), exons listed above), Primary Structure (Panel (A), regions and domains shown below); Tertiary Structure from cryo-EM model (panel (B)), and the two most-utilized T4 formation sites (panel (C), in bright green).
What is known is that the expression of region I-II-III alone (product of the first 37 exons of Tg that linearly encompasses from the N-terminal domain through to the arm domain) yields a protein that is not competent for anterograde transport from the ER. Remarkably, co-expression of the C-terminal ChEL domain as an entirely independent secretory protein results in a tight association of region I-II-III with this separately-expressed domain, rescuing the anterograde transport of I-II-III, with the two components remaining associated after secretion from cells [39]. Moreover, the C-terminal ChEL domain is not only necessary but also sufficient for tail-to-tail dimerization as demonstrated both by sucrose gradient centrifugation and by the formation of an artificially constructed intermolecular disulfide bond that is spontaneously generated when a single unpaired cysteine is introduced into the short unique tail sequence—and this same cysteine can also engage in the same unique disulfide crosslink within the homodimer when it is similarly introduced into the sequence of full-length Tg [43]. Considerable monomer folding is needed for homodimerization (ordinarily noncovalent) in the thyrocyte ER, and this seems to be a precondition for passing the ER quality control requirements for Tg export [19]. With this in mind, it is not surprising that mutations affecting the Tg coding sequence in such a way as to impede the formation of disulfide bonds within the many repeating units—or the three-dimensional packing of the overall globular protein (Figure 1B)—result in a shared, common phenotype of defective export from the ER, with diminished delivery to the thyroid follicle lumen and, consequently, diminished iodination and thyroid hormonogenesis.
We note that one group has estimated the genetic frequency in the general human population of presumed likely pathogenic variants of TG (heterozygosity) at 1:320 people [44], and a second group has similarly estimated this frequency at 1:217 people [45]. Either way, the occurrence of individuals expressing misfolded Tg protein from at least one allele is likely to be rather common. However, hypothyroidism from defective thyroglobulin is inherited as an autosomal recessive trait [46]. These data provide genetic evidence that wildtype Tg expressed from a single allele, along with the natural plasticity and endocrine feedback built into the hypothalamic-pituitary-thyroid axis, is sufficient to provide for the body’s needs for thyroid hormone.
3. Tg Misfolding and Its Consequences in Cell Culture Models
Tg misfolding can be studied either in thyrocyte cell lines, or by use of a suitable vector for expression in non-thyroidal cells. The first approach requires perturbation of the folding of endogenous wildtype Tg, and the second approach employs transfection of heterologous cells. To achieve success with the first approach, interruption of Tg folding in thyrocytes can be achieved pharmacologically, whereas the second approach allows for mechanistic insight into the effect of specific mutations (that are known to be linked to congenital hypothyroidism in humans or animal models) on Tg protein folding and trafficking. Unsurprisingly, transient expression of mutant TG genes in such heterologous cells results in the misfolded Tg protein being trapped in the ER, unable to advance to the Golgi complex (and thus unable to be secreted) because of ER quality control [47]. Surprisingly, however, some mutant Tg may interact with and be partially rescued by co-expression with wildtype (i.e., in 293T cells), presumably via weak cross-dimerization between the more folding-competent wildtype Tg monomer and the less folding-competent mutant Tg [43,48].
Protein misfolding in the ER is continuously monitored through the activities of ER stress sensors IRE1, PERK, and ATF6, which transmit responses leading to repression of global translation while increasing the expression of ER chaperones (e.g., BiP) and protein folding factors, accompanied by increased ER-associated and autophagic degradation of misfolded proteins [49]. However, under conditions of unremitted ER stress [50], cell death pathways can be activated [51]. A CRISPR/Cas9-mediated disruption of the TG gene in PCCL3 cell clones leading to undetectable Tg synthesis results in a more than 30% decrease in basal levels of BiP mRNA, and reduced ER stress response or cell death in the face of tunicamycin [52], an inducer of ER stress that works by inhibiting all N-linked-glycosylation (including that of Tg, which is normally the major N-glycosylated protein of thyrocytes). These findings strongly suggest that the misfolding of Tg itself can be a major contributor to ER stress, ER stress response, and ER stress-related cell death in thyrocytes.
ER-mediated diseases including congenital hypothyroidism typically take months or years to become clinically apparent [11,53], which means that patients and animal models with mutant Tg suffer from chronic continuous ER stress in their thyrocytes. This is not an easy phenotype to model in cell culture, but it is possible to challenge PCCL3 thyrocytes pharmacologically with chronic tunicamycin treatment in order to mimic the chronic ER stress condition. Initially, adaptation to chronic tunicamycin exposure occurs by a suppressed expression of the tunicamycin transporter (encoded by Mfsd2a [54]), but this can be surmounted either by slow, stepwise increments of the tunicamycin dose over a series of cell culture passages—or by simply using CRISPR-mediated genetic deletion of Mfsd2a and then immediately and permanently challenging PCCL3 thyrocytes with the highest possible dose of tunicamycin. In either case, a thyrocyte culture model can be obtained that adapts and survives long-term in the presence of chronic, continuous ER stress [52]. The growth rate of such adapted thyrocytes appears relatively normal, and this may be consistent with the ability to grow a thyroid goiter in many humans and animal models expressing misfolded mutant Tg.
A proteomic analysis of cultured thyrocytes adapted to chronic continuous ER stress revealed many up-regulated proteins, indicating stimulation of ER chaperones, oxidoreductases, stress responses, and lipid biosynthesis pathways [52], some of which had already been observed in in vivo models [55]. Furthermore, ER stress-adapted PCCL3 thyrocytes exhibited up-regulated AMP-Kinase activity (suggested by increased phosphorylation of AMPK), and decreased mTOR activity (suggested by diminished phosphorylation of S6-kinase and protein translation)—and a chemical AMPK activator was found to decrease the death of acutely ER-stress-challenged PCCL3 cells—all appearing consistent with the activation of conserved cell survival/adaptation pathways [52]. Additionally, subtle signs of de-differentiation including diminished PAX8, FOXE1, and TPO protein levels, along with decreased thyroglobulin mRNA levels were also observed in chronically ER stress-adapted cultured thyrocytes [52]. Furthermore, among the adaptive responses of chronically ER-stressed, partially de-differentiated PCCL3 cells included an apparent suppression of the mRNA level of Cidea (cell death-inducing DFFA-like effector-A, a protein of lipid droplets), as well as a blunted Cidea mRNA response (and blunted cell death response) to a new and unrelated acute ER stress challenge. In contrast, an acute ER stress challenge of either PCCL3 cells or several non-thyroid cell lines results in an acute increase of Cidea mRNA levels, indicating that CIDE-A is a novel noncanonical ER stress marker, which may have implications for cell death (when it is elevated) and cell survival (when it is suppressed) [56]. As CIDE-A may downregulate AMPK activity [57,58] to promote stress-mediated autophagy and cell survival, these observations might help to explain thyrocyte survival in the face of chronic continuous ER stress derived from misfolded Tg protein [52].
4. Tg Misfolding and Its Consequences for Animal Models and Humans
In congenital hypothyroidism with biallelic TG mutation, negative feedback from the intact hypothalamic-pituitary-thyroid axis results in chronic and dramatic elevation of circulating TSH. A prolonged stimulation of thyrocyte proliferation [59] induces thyroid growth (goiter) both in animals [60,61] and in patients [46,62,63,64]. However, linkage analysis suggests that the TG gene is also linked to congenital hypothyroidism in some families without goitrogenesis [65].
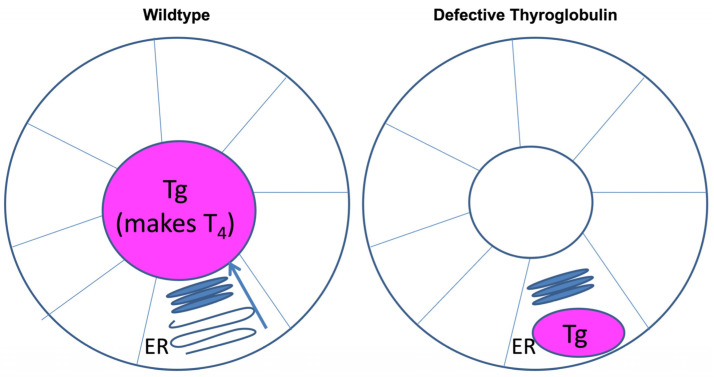
Biallelic TG mutations, with or without goiter, have also been described in rodent models. The well-known cog/cog mice are famous for (and receive their name from) “congenital goiter” [61]. The cog-TG gene encodes the mouse Tg-L2263P protein [66], which is misfolded and defective for intracellular transport from the ER to the Golgi complex [55,67]. Accumulation of the misfolded Tg induces ER stress that includes a marked elevation of ER chaperones and oxidoreductases [68,69] accompanied by massive ER expansion (Figure 2). A hypothyroid rat model known as rdw/rdw (encoding Tg-G2298R [47,70]) also exhibits dramatic ER stress response and massive ER expansion triggered by the misfolded rdwTg [71,72], resulting in an increase of cell size of individual thyrocytes [73,74]. However, the overall thyroid of rdw/rdw rats has been characterized as hypoplastic or atrophic [73,75], in contrast with the goiter of cog/cog mice (in which thyroid tissue ultimately weighs > 20-fold greater than normal [61]).
Figure 2.
The distribution of thyroglobulin protein in thyroid follicles under conditions that are either wildtype (left), or in case of Hypothyroidism with Defective Thyroglobulin (right). In wildtype thyroid (left), Tg is synthesized in the ER of within the thyroid epithelial monolayer. From there, Tg undergoes intracellular trafficking leading to its secretion into the follicular lumen. Secreted Tg serves as the primary substrate of thyroid hormone biosynthesis, utilizing thyroidal iodination machinery that is located at the apical membrane. In hypothyroidism with defective Tg (right), misfolded Tg is blocked in intracellular transport from the ER, inducing ER stress with massive ER expansion. Tg remaining within the ER of the thyroid epithelial monolayer is unavailable for thyroid hormone biosynthesis.
The reason for why hypothyroid rdw/rdw rats do not develop a goiter has been a research mystery for decades. A hypothesis was initially presented that the failure of thyroid gland growth may be secondary to thyrocyte cell death in rdw/rdw rats [72]. More specifically, the thinking was that thyroid enlargement in this animal model might be limited by an increased proteotoxicity of rdwTg as compared to goitrogenic TG variants, e.g., cogTg. However, it was later discovered that widespread thyrocyte cell death is a finding that is not exclusive to rdw/rdw rats, as this also occurs in cog/cog mice as well as a human patient with a similar biallelic TG mutation [76].
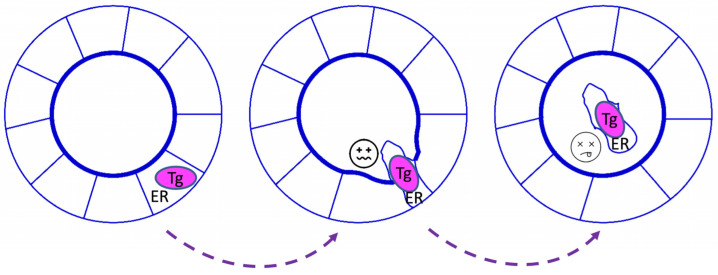
It is not easy to compare cog/cog thyroids in the AKR/J mouse strain background versus rdw/rdw thyroids in the Wistar-Imamichi rat strain background, for obvious reasons. Recently, an rdw/rdw knock-in model was generated in the C57BL6J mouse background using CRISPR/Cas9 technology [74]. Nowadays, cog/cog mice ordered from JAX laboratories are also distributed in the same strain background, making it possible to perform side-by-side examination of the cell biological and physiological impact of the two Tg mutants in the same genetic background [74]. Comparative studies of the two models have demonstrated that rdw/rdw (knock-in) mice do not exhibit greater ER stress or thyrocyte cell death compared to cog/cog mice, and both strains readily exhibit widespread thyrocyte cell death (Figure 3). Additionally, the proliferation of thyroid cells in rdw/rdw (knock-in) mice is not less than that found in cog/cog mice. As a result, the development of a goiter was not impaired in rdw/rdw (knock-in) mice when compared to cog/cog mice, indicating that the Tg-G2298R missense mutant is not intrinsically more proteotoxic than the Tg-L2263P mutant [74]. Rather, the absence of goiter in rdw/rdw rats appears to be linked primarily to strain-specific differences in thyroid gland growth [74]. Specifically, the rdw/rdw rats exhibit a failure to sustain thyroid cell proliferation despite ongoing TSH stimulation caused by primary hypothyroidism.
Figure 3.
The mechanism of thyroid hormones synthesis in hypothyroidism with defective thyroglobulin. Thyrocytes under massive ER stress (left) lose epithelial cell-cell contact, likely from diminished cell junctional integrity, and progress to cell death (right). Dying thyrocytes that have been extruded into the follicle lumen eventually disintegrate and their macromolecular components are exposed to iodination and ingestion by surrounding live thyrocytes.
Simple goiter has been characterized as either a compensatory response to insufficient thyroid hormone production or as a maladaptation [77]. Interestingly, it has been found that patients bearing biallelic TG mutation with a large goiter could ultimately achieve nearly normal levels of thyroid hormone even when treatment with levothyroxine was not implemented (due to noncompliance or other reasons) [78,79]. Similarly, cog/cog mice were also found to be able to ‘spontaneously’ correct their serum T4 levels to nearly normal in the absence of levothyroxine treatment. The rise in serum T4 levels occurs slowly, and appears to parallel the growth of the thyroid gland [80]. Indeed, long-standing goiters resulting from untreated biallelic TG mutations have been reported to be associated with an increased risk of thyroid cancer [81,82,83]. It is conceivable that adenomatous and even malignant transformation might emerge from a prolonged hyperproliferative state, and this has been suggested based on studies in Wistar Hannover GALAS Rats (encoding Tgc.749−1G > T [84]), which display thyroid focal hyperplastic lesions in later life [85].
A comparative evaluation of the thyroids of untreated cog/cog mice, and a patient bearing homozygous Tg-W2346R, as well as rdw/rdw rats, revealed an unusual pathway of thyroid hormone synthesis that was shared by each case. Specifically, in all three species, thyrocyte cell death was observed, with entry of the dead, ER-stressed thyrocytes into the lumen of thyroid follicles still surrounded by other living thyrocytes [76]. This can lead to the iodination of proteins derived from decaying cells contained within the thyroid follicle lumen (which includes the mutant Tg protein), followed by the cannibalism of the iodinated luminal detritus of the dead thyrocytes (Figure 3). From the iodoproteins generated by iodination of the proteome of dead thyrocytes, some thyroxine can be formed within mutant Tg itself [76], although this is likely to be far less efficient than normal thyroid hormonogenesis. Interestingly, the compromised efficiency of iodoprotein synthesis could be partially improved with excess iodide supplement in a goat model [86] and in human patients [87].
Why are dead thyrocytes found within the thyroid follicle lumen? Interestingly, it has been observed that cell death in other epithelial tissues (including renal tubular epithelial cells, mammary epithelial cells, bronchial epithelial cells, etc.) results in dead cell extrusion selectively to the apical side of the epithelium [88,89,90]. Thyroid follicles are similar, organized as a classically polarized epithelial monolayer, with typical tight junctions and gap junctions [91], such as adherens junctions [92] and desmosomes [93]. Adherens junctions primarily consist of protein complexes between the transmembrane protein cadherin and intracellular catenin, and these complexes are linked to the actin cytoskeleton [94]. The formation of adherens junctions is a prerequisite for the proper assembly of tight junctions [95]; indeed, cadherin and other cell-adhesion proteins mediate many facets of epithelial morphogenesis [96]. Thyroid cells express E-cadherin and thyroid (and kidney)-specific cadherin-16 [97], which also contributes to the apical–basal follicular polarization [98] that is essential to efficient thyroid hormonogenesis [21,22]. On the other hand, decreased expression of cadherins favors epithelial cell disaggregation, as happens in epithelial-mesenchymal transition that can occur during the development of various cancers [99]. It is thought that thyroidal ER stress (triggered pharmacologically, and potentially also pathologically from Tg misfolding) induces a thyroid de-differentiation response [52,100] that includes not only gene products directly implicated in thyroid hormonogenesis, but also diminished expression of E-cadherin and cadherin-16. This may bring about thyrocyte cell shape change, as well loss of cortical actin, formation of stress fibers, and significantly, a loss of epithelial cell-cell contact. Such changes in the thyrocyte cytoskeleton and accompanying loss of cell-cell junctional contacts might account for why—in patients and animal models with biallelic TG mutation—dead ER-stressed thyrocytes are observed to be extruded apically into the thyroid follicular lumen [76]. Indeed, not only may dead thyrocytes be released into the thyroid follicular lumen, but it is also conceivable that live follicular epithelial cells might also enter the thyroid follicle lumen, although it remains to be tested the extent to which this occurs, and if so, whether the driving mechanisms are the same.
Interestingly, in the early days of life, rdw/rdw rats actually show mild thyroid gland enlargement compared to that of wildtype animals, and this corresponds to a short period in the life of the mutant animals during which serum T4 levels are actually increasing (although still abnormally low). This stage of life is then followed by a sustained period during which a decrease of both thyroid gland size and serum T4 levels is observed [76]. Although the production of thyroid hormones via the iodination of disintegrating thyrocytes in the follicular lumen is very inefficient, nevertheless this highly unusual mechanism is a key source for providing thyroid hormone synthesis, and blocking this source is actually lethal to the animals [76]. Thus, in comparing cog/cog mice to rdw/rdw rats, it appears that the goiter is necessary in order to provide a continuous supply of thyrocytes, that upon entry and disintegrations within the follicle lumen, ultimately provide the substrate that allows for ongoing thyroid hormone biosynthesis. Conversely, failure to grow the thyroid gland causes rdw/rdw rats, and probably some human patients, to become depleted of the substrate needed to sustain thyroid hormonogenesis.
Acknowledgments
This work was supported by National Institutes of Health grants R01 DK132017 (to P.A.).
Author Contributions
Conceptualization, X.Z., C.Y., Y.M., K.K., O.O.K., O.B.C., B.D.J. and P.A.; resources, P.A.; writing—original draft preparation X.Z., C.Y., Y.M., P.A. and X.Z.; writing—review and editing, all co-authors; visualization, P.A.; supervision, P.A.; funding acquisition, P.A. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research was funded by National Institute of Diabetes and Digestive and Kidney Diseases, grant number R01 DK132017.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Hung M.C., Link W. Protein localization in disease and therapy. Pt 20J. Cell Sci. 2011;124:3381–3392. doi: 10.1242/jcs.089110. [DOI] [PubMed] [Google Scholar]
- 2.Schwarz D.S., Blower M.D. The endoplasmic reticulum: Structure, function and response to cellular signaling. Cell. Mol. Life Sci. 2016;73:79–94. doi: 10.1007/s00018-015-2052-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Perkins H.T., Allan V. Intertwined and Finely Balanced: Endoplasmic Reticulum Morphology, Dynamics, Function, and Diseases. Cells. 2021;10:2341. doi: 10.3390/cells10092341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Meras I., Maes J., Lefrancois S. Mechanisms regulating the sorting of soluble lysosomal proteins. Biosci. Rep. 2022;42:BSR20211856. doi: 10.1042/BSR20211856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Banfield D.K. Mechanisms of protein retention in the Golgi. Cold Spring Harb. Perspect. Biol. 2011;3:a005264. doi: 10.1101/cshperspect.a005264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McRae M.S., Wang B., Hyson R.G., Siddiquee R., Duff A.P., Ataide S.F., Kwan A.H. Expression and purification of the NG domain from human SRalpha, a key component of the Signal Recognition Particle (SRP) receptor. Protein Expr. Purif. 2022;198:106121. doi: 10.1016/j.pep.2022.106121. [DOI] [PubMed] [Google Scholar]
- 7.Song J., Becker T. Fidelity of organellar protein targeting. Curr. Opin. Cell Biol. 2022;75:102071. doi: 10.1016/j.ceb.2022.02.005. [DOI] [PubMed] [Google Scholar]
- 8.Liaci A.M., Forster F. Take Me Home, Protein Roads: Structural Insights into Signal Peptide Interactions during ER Translocation. Int. J. Mol. Sci. 2021;22:11871. doi: 10.3390/ijms222111871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Esmail S., Manolson M.F. Advances in understanding N-glycosylation structure, function, and regulation in health and disease. Eur. J. Cell Biol. 2021;100:151186. doi: 10.1016/j.ejcb.2021.151186. [DOI] [PubMed] [Google Scholar]
- 10.Medinas D.B., Rozas P., Hetz C. Critical roles of protein disulfide isomerases in balancing proteostasis in the nervous system. J. Biol. Chem. 2022;298:102087. doi: 10.1016/j.jbc.2022.102087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Morishita Y., Arvan P. Lessons from animal models of endocrine disorders caused by defects of protein folding in the secretory pathway. Mol. Cell. Endocrinol. 2020;499:110613. doi: 10.1016/j.mce.2019.110613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gidalevitz T., Stevens F., Argon Y. Orchestration of secretory protein folding by ER chaperones. Biochim. Biophys. Acta. 2013;1833:2410–2424. doi: 10.1016/j.bbamcr.2013.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Adams B.M., Canniff N.P., Guay K.P., Hebert D.N. Progress in Molecular and Subcellular Biology. Volume 59. Springer; Cham, Switzerland: 2021. The Role of Endoplasmic Reticulum Chaperones in Protein Folding and Quality Control; pp. 27–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Phillips B.P., Gomez-Navarro N., Miller E.A. Protein quality control in the endoplasmic reticulum. Curr. Opin. Cell Biol. 2020;65:96–102. doi: 10.1016/j.ceb.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wiseman R.L., Mesgarzadeh J.S., Hendershot L.M. Reshaping endoplasmic reticulum quality control through the unfolded protein response. Mol. Cell. 2022;82:1477–1491. doi: 10.1016/j.molcel.2022.03.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Needham P.G., Guerriero C.J., Brodsky J.L. Chaperoning Endoplasmic Reticulum-Associated Degradation (ERAD) and Protein Conformational Diseases. Cold Spring Harb. Perspect. Biol. 2019;11:a033928. doi: 10.1101/cshperspect.a033928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mochida K., Nakatogawa H. ER-phagy: Selective autophagy of the endoplasmic reticulum. EMBO Rep. 2022;23:e55192. doi: 10.15252/embr.202255192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Graham K.S., Le A., Sifers R.N. Accumulation of the insoluble PiZ variant human a1-antitrypsin within the hepatic endoplasmic reticulum does not elevate the steaty-state level of grp78/BiP. J. Biol. Chem. 1990;265:20463–20468. doi: 10.1016/S0021-9258(17)30527-6. [DOI] [PubMed] [Google Scholar]
- 19.Di Jeso B., Arvan P. Thyroglobulin from Molecular and Cellular Biology to Clinical Endocrinology. Endocr. Rev. 2016;37:2–36. doi: 10.1210/er.2015-1090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Holzer G., Morishita Y., Fini J.B., Lorin T., Gillet B., Hughes S., Tohme M., Deleage G., Demeneix B., Arvan P., et al. Thyroglobulin Represents a Novel Molecular Architecture of Vertebrates. J. Biol. Chem. 2016;291:16553–16566. doi: 10.1074/jbc.M116.719047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang Y., Shimizu H., Xiang Y.-Y., Sugihara J., Lu W.-Y., Liao X.-H., Cho H.-R., Toba H., Bai X.-H., Asa S.L., et al. XB130 Deficiency Causes Congenital Hypothyroidism in Mice due to Disorganized Apical Membrane Structure and Function of Thyrocytes. Thyroid. 2021;31:1650–1661. doi: 10.1089/thy.2021.0195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wang Y., Xiang Y.-Y., Sugihara J., Lu W.-Y., Liao X.-H., Arvan P., Refetoff S., Liu M. XB130 Plays an Essential Role in Folliculogenesis through Mediating Interactions between Microfilament and Microtubule Systems in Thyrocytes. Thyroid. 2022;32:128–137. doi: 10.1089/thy.2021.0461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Di Jeso B., Ulianich L., Pacifico F., Leonardi A., Vito P., Consiglio E., Formisano S., Arvan P. Folding of thyroglobulin in the calnexin/calreticulin pathway and its alteration by loss of Ca2+ from the endoplasmic reticulum. Pt 2Biochem. J. 2003;370:449–458. doi: 10.1042/bj20021257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Van Herle A.J., Vassart G., Dumont J.E. Control of thyroglobulin synthesis and secretion. (First of two parts) N. Engl. J. Med. 1979;301:239–249. doi: 10.1056/NEJM197908023010504. [DOI] [PubMed] [Google Scholar]
- 25.Dunn J.T., Dunn A.D. The importance of thyroglobulin structure for thyroid hormone biosynthesis. Biochimie. 1999;81:505–509. doi: 10.1016/S0300-9084(99)80102-3. [DOI] [PubMed] [Google Scholar]
- 26.Rivolta C.M., Targovnik H.M. Molecular advances in thyroglobulin disorders. Clin. Chim. Acta. 2006;374:8–24. doi: 10.1016/j.cca.2006.05.043. [DOI] [PubMed] [Google Scholar]
- 27.Kayili H.M., Salih B. Site-specific N-glycosylation analysis of human thyroid thyroglobulin by mass spectrometry-based Glyco-analytical strategies. J. Proteom. 2022;267:104700. doi: 10.1016/j.jprot.2022.104700. [DOI] [PubMed] [Google Scholar]
- 28.Adaixo R., Steiner E.M., Righetto R.D., Schmidt A., Stahlberg H., Taylor N.M.I. Cryo-EM structure of native human thyroglobulin. Nat. Commun. 2022;13:61. doi: 10.1038/s41467-021-27693-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kim P., Bole D., Arvan P. Transient aggregation of nascent thyroglobulin in the endoplasmic reticulum: Relationship to the molecular chaperone, BiP. J. Cell Biol. 1992;118:541–549. doi: 10.1083/jcb.118.3.541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wright M.T., Kouba L., Plate L. Thyroglobulin Interactome Profiling Defines Altered Proteostasis Topology Associated With Thyroid Dyshormonogenesis. Mol. Cell. Proteom. 2021;20:100008. doi: 10.1074/mcp.RA120.002168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Di Jeso B., Park Y.-N., Ulianich L., Treglia A.S., Urbanas M.L., High S., Arvan P. Mixed-disulfide folding intermediates between thyroglobulin and ER resident oxidoreductases ERp57 and PDI. Mol. Cell. Biol. 2005;25:9793–9805. doi: 10.1128/MCB.25.22.9793-9805.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Di Jeso B., Morishita Y., Treglia A.S., Lofrumento D.D., Nicolardi G., Beguinot F., Kellogg A.P., Arvan P. Transient covalent interactions of newly synthesized thyroglobulin with oxidoreductases of the endoplasmic reticulum. J. Biol. Chem. 2014;289:11488–11496. doi: 10.1074/jbc.M113.520767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Arvan P., Kim P.S., Kuliawat R., Prabakaran D., Muresan Z., Yoo S.E., Hossain S.A. Intracellular protein transport to the thyrocyte plasma membrane: Potential implications for thyroid physiology. Thyroid. 1997;7:89–105. doi: 10.1089/thy.1997.7.89. [DOI] [PubMed] [Google Scholar]
- 34.Coscia F., Taler-Vercic A., Chang V.T., Sinn L., O’Reilly F.J., Izore T., Renko M., Berger I., Rappsilber J., Turk D., et al. The structure of human thyroglobulin. Nature. 2020;578:627–630. doi: 10.1038/s41586-020-1995-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tosatto L., Coscia F. A glance at post-translational modifications of human thyroglobulin: Potential impact on function and pathogenesis. Eur. Thyroid J. 2022;11 doi: 10.1530/ETJ-22-0046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Citterio C.E., Targovnik H.M., Arvan P. The role of thyroglobulin in thyroid hormonogenesis. Nat. Rev. Endocrinol. 2019;15:323–338. doi: 10.1038/s41574-019-0184-8. [DOI] [PubMed] [Google Scholar]
- 37.Mendive F.M., Rivolta C.M., Moya C.M., Vassart G., Targovnik H.M. Genomic organization of the human thyroglobulin gene: The complete intron-exon structure. Eur. J. Endocrinol. 2001;145:485–496. doi: 10.1530/eje.0.1450485. [DOI] [PubMed] [Google Scholar]
- 38.Citterio C.E., Rivolta C.M., Targovnik H.M. Structure and genetic variants of thyroglobulin: Pathophysiological implications. Mol. Cell. Endocrinol. 2021;528:111227. doi: 10.1016/j.mce.2021.111227. [DOI] [PubMed] [Google Scholar]
- 39.Lee J., Di Jeso B., Arvan P. The cholinesterase-like domain of thyrogobulin functions as an intramolecular chaperone. J. Clin. Investig. 2008;118:2950–2958. doi: 10.1172/JCI35164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kim K., Kopylov M., Bobe D., Kelley K., Eng E.T., Arvan P., Clarke O.B. The structure of natively iodinated bovine thyroglobulin. Pt 11Acta Crystallogr. D Struct. Biol. 2021;77:1451–1459. doi: 10.1107/S2059798321010056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Marechal N., Serrano B.P., Zhang X., Weitz C.J. Formation of thyroid hormone revealed by a cryo-EM structure of native bovine thyroglobulin. Nat. Commun. 2022;13:2380. doi: 10.1038/s41467-022-30082-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Citterio C.E., Morishita Y., Dakka N., Veluswamy B., Arvan P. Relationship between the dimerization of thyroglobulin and its ability to form triiodothyronine. J. Biol. Chem. 2018;293:4860–4869. doi: 10.1074/jbc.RA118.001786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wang X., Lee J., Di Jeso B., Treglia A.S., Comoletti D., Dubi N., Taylor P., Arvan P. Cis and trans actions of the cholinesterase-like domain within the thyroglobulin dimer. J. Biol. Chem. 2010;285:17564–17573. doi: 10.1074/jbc.M110.111641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pio M.G., Siffo S., Scheps K.G., Molina M.F., Adrover E., Abelleyro M.M., Rivolta C.M., Targovnik H.M. Curating the gnomAD database: Report of novel variants in the thyrogobulin gene using in silico bioinformatics algorithms. Mol. Cell. Endocrinol. 2021;534:111359. doi: 10.1016/j.mce.2021.111359. [DOI] [PubMed] [Google Scholar]
- 45.Park K.S. Analysis of Worldwide Carrier Frequency and Predicted Genetic Prevalence of Autosomal Recessive Congenital Hypothyroidism Based on a General Population Database. Genes. 2021;12:863. doi: 10.3390/genes12060863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Siffo S., Adrover E., Citterio C.E., Miras M.B., Balbi V.A., Chiesa A., Weill J., Sobrero G., Gonzalez V.G., Papendieck P., et al. Molecular analysis of thyroglobulin mutations found in patients with goiter and hypothyroidism. Mol. Cell. Endocrinol. 2018;473:1–16. doi: 10.1016/j.mce.2017.12.009. [DOI] [PubMed] [Google Scholar]
- 47.Kim P.S., Ding M., Menon S., Jung C.G., Cheng J.M., Miyamoto T., Li B., Furudate S., Agui T. A missense mutation G2320R in the thyroglobulin gene causes non-goitrous congenital primary hypothyroidism in the WIC-rdw rat. Mol. Endocrinol. 2000;14:1944–1953. doi: 10.1210/mend.14.12.0571. [DOI] [PubMed] [Google Scholar]
- 48.Wright J., Wang X., Haataja L., Kellogg A.P., Lee J., Liu M., Arvan P. Dominant protein interactions that influence the pathogenesis of conformational diseases. J. Clin. Investig. 2013;123:3124–3134. doi: 10.1172/JCI67260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Han J., Kaufman R.J. Physiological/pathological ramifications of transcription factors in the unfolded protein response. Genes Dev. 2017;31:1417–1438. doi: 10.1101/gad.297374.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Tsang K.Y., Chan D., Bateman J.F., Cheah K.S. In Vivo cellular adaptation to ER stress: Survival strategies with double-edged consequences. Pt 13J. Cell Sci. 2010;123:2145–2154. doi: 10.1242/jcs.068833. [DOI] [PubMed] [Google Scholar]
- 51.Ghosh R., Colon-Negron K., Papa F.R. Endoplasmic reticulum stress, degeneration of pancreatic islet β-cells, and therapeutic modulation of the unfolded protein response in diabetes. Mol. Metab. 2019;27:S60–S68. doi: 10.1016/j.molmet.2019.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Morishita Y., Kabil O., Young K.Z., Kellogg A.P., Chang A., Arvan P. Thyrocyte cell survival and adaptation to chronic endoplasmic reticulum stress due to misfolded thyroglobulin. J. Biol. Chem. 2020;295:6876–6887. doi: 10.1074/jbc.RA120.012656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kim P.S., Arvan P. Endocrinopathies in the family of endoplasmic reticulum (ER) storage diseases: Disorders of protein trafficking and the role of ER molecular chaperones. Endocr. Rev. 1998;19:173–202. doi: 10.1210/edrv.19.2.0327. [DOI] [PubMed] [Google Scholar]
- 54.Reiling J.H., Clish C.B., Carette J.E., Varadarajan M., Brummelkamp T.R., Sabatini D.M. A haploid genetic screen identifies the major facilitator domain containing 2A (MFSD2A) transporter as a key mediator in the response to tunicamycin. Proc. Natl. Acad. Sci. USA. 2011;108:11756–11765. doi: 10.1073/pnas.1018098108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kim P.S., Kwon O.-Y., Arvan P. An endoplasmic reticulum storage disease causing congenital goiter with hypothyroidism. J. Cell Biol. 1996;133:517–527. doi: 10.1083/jcb.133.3.517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Morishita Y., Kellogg A.P., Larkin D., Chen W., Vadrevu S., Satin L., Liu M., Arvan P. Cell death-associated lipid droplet protein CIDE-A is a noncanonical marker of endoplasmic reticulum stress. JCI Insight. 2021;6:143980. doi: 10.1172/jci.insight.143980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Rohm M., Schafer M., Laurent V., Ustunel B.E., Niopek K., Algire C., Hautzinger O., Sijmonsma T.P., Zota A., Medrikova D., et al. An AMP-activated protein kinase-stabilizing peptide ameliorates adipose tissue wasting in cancer cachexia in mice. Nat. Med. 2016;22:1120–1130. doi: 10.1038/nm.4171. [DOI] [PubMed] [Google Scholar]
- 58.Qi J., Gong J., Zhao T., Zhao J., Lam P., Ye J., Li J.Z., Wu J., Zhou H.M., Li P. Downregulation of AMP-activated protein kinase by Cidea-mediated ubiquitination and degradation in brown adipose tissue. EMBO J. 2008;27:1537–1548. doi: 10.1038/emboj.2008.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kimura T., Van Keymeulen A., Golstein J., Fusco A., Dumont J.E., Roger P.P. Regulation of thyroid cell proliferation by TSH and other factors: A critical evaluation of in vitro models. Endocr. Rev. 2001;22:631–656. doi: 10.1210/edrv.22.5.0444. [DOI] [PubMed] [Google Scholar]
- 60.de Vijlder J.J., van Voorthuizen W.F., van Dijk J.E., Rijnberk A., Tegelaers W.H. Hereditary congenital goiter with thyroglobulin deficiency in a breed of goats. Endocrinology. 1978;102:1214–1222. doi: 10.1210/endo-102-4-1214. [DOI] [PubMed] [Google Scholar]
- 61.Beamer W.G., Maltais L.J., DeBaets M.H., Eicher E.M. Inherited congenital goiter in mice. Endocrinology. 1987;120:838–840. doi: 10.1210/endo-120-2-838. [DOI] [PubMed] [Google Scholar]
- 62.Targovnik H.M., Vono J., Billerbeck A.E., Cerrone G.E., Varela V., Mendive F., Wajchenberg B.L., Medeiros-Neto G. A 138-nucleotide deletion in the thyroglobulin ribonucleic acid messenger in a congenital goiter with defective thyroglobulin synthesis. J. Clin. Endocrinol. Metab. 1995;80:3356–3360. doi: 10.1210/jcem.80.11.7593451. [DOI] [PubMed] [Google Scholar]
- 63.Caputo M., Rivolta C.M., Esperante S.A., Gruñeiro-Papendieck L., Chiesa A., Pellizas C.G., González-Sarmiento R., Targovnik H.M. Congenital hypothyroidism with goitre caused by new mutations in the thyroglobulin gene. Clin. Endocrinol. 2007;67:351–357. doi: 10.1111/j.1365-2265.2007.02889.x. [DOI] [PubMed] [Google Scholar]
- 64.Targovnik H.M., Rivolta C.M., Mendive F.M., Moya C.M., Vono J., Medeiros-Neto G. Congenital goiter with hypothyroidism caused by a 5′ splice site mutation in the thyroglobulin gene. Thyroid. 2001;11:685–690. doi: 10.1089/105072501750362763. [DOI] [PubMed] [Google Scholar]
- 65.Ahlbom B.E., Yaqoob M., Gustavsson P., Abbas H.G., Annerén G., Larsson A., Wadelius C. Linkage analysis identifies the thyroglobulin gene region as a major locus for familial congenital hypothyroidism. Hum. Genet. 2002;110:145–147. doi: 10.1007/s00439-002-0680-z. [DOI] [PubMed] [Google Scholar]
- 66.Kim P.S., Hossain S.A., Park Y.N., Lee I., Yoo S.E., Arvan P. A single amino acid change in the acetylcholinesterase-like domain of thyroglobulin causes congenital goiter with hypothyroidism in the cog/cog mouse: A model of human endoplasmic reticulum storage diseases. Proc. Natl. Acad. Sci. USA. 1998;95:9909–9913. doi: 10.1073/pnas.95.17.9909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Basche M., Beamer W.G., Schneider A.B. Abnormal properties of thyroglobulin in mice with inherited congenital goiter (cog/cog) Endocrinology. 1989;124:1822–1829. doi: 10.1210/endo-124-4-1822. [DOI] [PubMed] [Google Scholar]
- 68.Mayerhofer A., Amador A.G., Beamer W.G., Bartke A. Ultrastructural aspects of the goiter in cog/cog mice. J. Hered. 1988;79:200–203. doi: 10.1093/oxfordjournals.jhered.a110492. [DOI] [PubMed] [Google Scholar]
- 69.Medeiros-Neto G., Kim P.S., Yoo S.E., Vono J., Targovnik H.M., Camargo R., Hossain S.A., Arvan P. Congenital hypothyroid goiter with deficient thyroglobulin. Identification of an endoplasmic reticulum storage disease with induction of molecular chaperones. J. Clin. Investig. 1996;98:2838–2844. doi: 10.1172/JCI119112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Hishinuma A., Furudate S., Oh-Ishi M., Nagakubo N., Namatame T., Ieiri T. A novel missense mutation (G2320R) in thyroglobulin causes hypothyroidism in rdw rats. Endocrinology. 2000;141:4050–4055. doi: 10.1210/endo.141.11.7794. [DOI] [PubMed] [Google Scholar]
- 71.Baryshev M., Sargsyan E., Wallin G., Lejnieks A., Furudate S., Hishinuma A., Mkrtchian S. Unfolded protein response is involved in the pathology of human congenital hypothyroid goiter and rat non-goitrous congenital hypothyroidism. J. Mol. Endocrinol. 2004;32:903–920. doi: 10.1677/jme.0.0320903. [DOI] [PubMed] [Google Scholar]
- 72.Menon S., Lee J., Abplanalp W.A., Yoo S.E., Agui T., Furudate S., Kim P.S., Arvan P. Oxidoreductase interactions include a role for ERp72 engagement with mutant thyroglobulin from the rdw/rdw rat dwarf. J. Biol. Chem. 2007;282:6183–6191. doi: 10.1074/jbc.M608863200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Sakai Y., Yamashina S., Furudate S.I. Missing secretory granules, dilated endoplasmic reticulum, and nuclear dislocation in the thyroid gland of rdw rats with hereditary dwarfism. Anat. Rec. 2000;259:60–66. doi: 10.1002/(SICI)1097-0185(20000501)259:1<60::AID-AR7>3.0.CO;2-F. [DOI] [PubMed] [Google Scholar]
- 74.Zhang X., Malik B., Young C., Zhang H., Larkin D., Liao X.H., Refetoff S., Liu M., Arvan P. Maintaining the thyroid gland in mutant thyroglobulin-induced hypothyroidism requires thyroid cell proliferation that must continue in adulthood. J. Biol. Chem. 2022;298:102066. doi: 10.1016/j.jbc.2022.102066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Umezu M., Kagabu S., Jiang J., Sato E. Evaluation and characterization of congenital hypothyroidism in rdw dwarf rats. Lab. Anim. Sci. 1998;48:496–501. [PubMed] [Google Scholar]
- 76.Zhang X., Kellogg A.P., Citterio C.E., Zhang H., Larkin D., Morishita Y., Targovnik H.M., Balbi V.A., Arvan P. Thyroid hormone synthesis continues despite biallelic thyroglobulin mutation with cell death. JCI Insight. 2021;6:148496. doi: 10.1172/jci.insight.148496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Dumont J.E., Ermans A.M., Maenhaut C., Coppee F., Stanbury J.B. Large goitre as a maladaptation to iodine deficiency. Clin. Endocrinol. 1995;43:1–10. doi: 10.1111/j.1365-2265.1995.tb01886.x. [DOI] [PubMed] [Google Scholar]
- 78.van de Graaf S.A., Ris-Stalpers C., Veenboer G.J., Cammenga M., Santos C., Targovnik H.M., de Vijlder J.J., Medeiros-Neto G. A premature stopcodon in thyroglobulin messenger RNA results in familial goiter and moderate hypothyroidism. J. Clin. Endocrinol. Metab. 1999;84:2537–2542. doi: 10.1210/jcem.84.7.5862. [DOI] [PubMed] [Google Scholar]
- 79.Hermanns P., Refetoff S., Sriphrapradang C., Pohlenz J., Okamato J., Slyper L., Slyper A.H. A clinically euthyroid child with a large goiter due to a thyroglobulin gene defect: Clinical features and genetic studies. J. Pediatr. Endocrinol. Metab. 2013;26:119–123. doi: 10.1515/jpem-2012-0287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Adkison L.R., Taylor S., Beamer W.G. Mutant gene-induced disorders of structure, function and thyroglobulin synthesis in congenital goitre (cog/cog) in mice. J. Endocrinol. 1990;126:51–58. doi: 10.1677/joe.0.1260051. [DOI] [PubMed] [Google Scholar]
- 81.Hishinuma A., Fukata S., Kakudo K., Murata Y., Ieiri T. High incidence of thyroid cancer in long-standing goiters with thyroglobulin mutations. Thyroid. 2005;15:1079–1084. doi: 10.1089/thy.2005.15.1079. [DOI] [PubMed] [Google Scholar]
- 82.Raef H., Al-Rijjal R., Al-Shehri S., Zou M., Al-Mana H., Baitei E.Y., Parhar R.S., Al-Mohanna F.A., Shi Y. Biallelic p.R2223H mutation in the thyroglobulin gene causes thyroglobulin retention and severe hypothyroidism with subsequent development of thyroid carcinoma. J. Clin. Endocrinol. Metab. 2010;95:1000–1006. doi: 10.1210/jc.2009-1823. [DOI] [PubMed] [Google Scholar]
- 83.Yoon J.H., Hong A.R., Kim H.K., Kang H.C. Anaplastic Thyroid Cancer Arising from Dyshormonogenetic Goiter: C.3070T>C and Novel c.7070T>C Mutation in the Thyroglobulin Gene. Thyroid. 2020;30:1676–1680. doi: 10.1089/thy.2020.0248. [DOI] [PubMed] [Google Scholar]
- 84.Sato A., Abe K., Yuzuriha M., Fujii S., Takahashi N., Hojo H., Teramoto S., Aoyama H. A novel mutation in the thyroglobulin gene that causes goiter and dwarfism in Wistar Hannover GALAS rats. Mutat. Res. 2014;762:17–23. doi: 10.1016/j.mrfmmm.2014.02.003. [DOI] [PubMed] [Google Scholar]
- 85.Kokoshima H., Doi T., Yamada N., Tsuchitani M. Proliferative lesions in thyroid follicular cells of dwarfs derived from Wistar Hannover GALAS rats. Toxicol. Pathol. 2014;42:565–572. doi: 10.1177/0192623313491858. [DOI] [PubMed] [Google Scholar]
- 86.van Voorthuizen W.F., de Vijlder J.J., van Dijk J.E., Tegelaers W.H. Euthyroidism via iodide supplementation in hereditary congenital goiter with thyroglobulin deficiency. Endocrinology. 1978;103:2105–2111. doi: 10.1210/endo-103-6-2105. [DOI] [PubMed] [Google Scholar]
- 87.Vono J., Lima N., Knobel M., Medeiros-Neto G. The effect of oral administration of iodine to patients with goiter and hypothyroidism due to defective synthesis of thyroglobulin. Thyroid. 1996;6:11–15. doi: 10.1089/thy.1996.6.11. [DOI] [PubMed] [Google Scholar]
- 88.Arandjelovic S., Ravichandran K.S. Phagocytosis of apoptotic cells in homeostasis. Nat. Immunol. 2015;16:907–917. doi: 10.1038/ni.3253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Juncadella I.J., Kadl A., Sharma A.K., Shim Y.M., Hochreiter-Hufford A., Borish L., Ravichandran K.S. Apoptotic cell clearance by bronchial epithelial cells critically influences airway inflammation. Nature. 2013;493:547–551. doi: 10.1038/nature11714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Pan H., Shen K., Wang X., Meng H., Wang C., Jin B. Protective effect of metalloporphyrins against cisplatin-induced kidney injury in mice. PLoS ONE. 2014;9:e86057. doi: 10.1371/journal.pone.0086057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Munari-Silem Y., Mesnil M., Selmi S., Bernier-Valentin F., Rabilloud R., Rousset B. Cell-cell interactions in the process of differentiation of thyroid epithelial cells into follicles: A study by microinjection and fluorescence microscopy on in vitro reconstituted thyroid follicles. J. Cell. Physiol. 1990;145:414–427. doi: 10.1002/jcp.1041450305. [DOI] [PubMed] [Google Scholar]
- 92.Sastre-Perona A., Santisteban P. Wnt-independent role of β-catenin in thyroid cell proliferation and differentiation. Mol. Endocrinol. 2014;28:681–695. doi: 10.1210/me.2013-1377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Dockhorn-Dworniczak B., Franke W.W., Schröder S., Czernobilsky B., Gould V.E., Böcker W. Patterns of expression of cytoskeletal proteins in human thyroid gland and thyroid carcinomas. Differentiation. 1987;35:53–71. doi: 10.1111/j.1432-0436.1987.tb00151.x. [DOI] [PubMed] [Google Scholar]
- 94.Lien W.-H., Klezovitch O., Vasioukhin V. Cadherin-catenin proteins in vertebrate development. Curr. Opin. Cell Biol. 2006;18:499–506. doi: 10.1016/j.ceb.2006.07.001. [DOI] [PubMed] [Google Scholar]
- 95.Campbell H.K., Maiers J.L., DeMali K.A. Interplay between tight junctions & adherens junctions. Exp. Cell Res. 2017;358:39–44. doi: 10.1016/j.yexcr.2017.03.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Adil M.S., Narayanan S.P., Somanath P.R. Cell-cell junctions: Structure and regulation in physiology and pathology. Tissue Barriers. 2021;9:1848212. doi: 10.1080/21688370.2020.1848212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Calì G., Gentile F., Mogavero S., Pallante P., Nitsch R., Ciancia G., Ferraro A., Fusco A., Nitsch L. CDH16/Ksp-cadherin is expressed in the developing thyroid gland and is strongly down-regulated in thyroid carcinomas. Endocrinology. 2011;153:522–534. doi: 10.1210/en.2011-1572. [DOI] [PubMed] [Google Scholar]
- 98.Koumarianou P., Goméz-López G., Santisteban P. Pax8 controls thyroid follicular polarity through cadherin-16. J. Cell Sci. 2017;130:219–231. doi: 10.1242/jcs.184291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Dongre A., Weinberg R.A. New insights into the mechanisms of epithelial-mesenchymal transition and implications for cancer. Nat. Rev. Mol. Cell Biol. 2019;20:69–84. doi: 10.1038/s41580-018-0080-4. [DOI] [PubMed] [Google Scholar]
- 100.Ulianich L., Mirra P., Garbi C., Cali G., Conza D., Treglia A.S., Miraglia A., Punzi D., Miele C., Raciti G.A., et al. The Pervasive Effects of ER Stress on a Typical Endocrine Cell: Dedifferentiation, Mesenchymal Shift and Antioxidant Response in the Thyrocyte. Front. Endocrinol. 2020;11:588685. doi: 10.3389/fendo.2020.588685. [DOI] [PMC free article] [PubMed] [Google Scholar]