Abstract
Background
The ongoing COVID-19 pandemic has had an unprecedented impact on the lives of people globally and is expected to have profound effects on mental health. Here we aim to describe the mental health burden experienced in Sweden using baseline data of the Omtanke2020 Study.
Method
We analysed self-reported, cross-sectional baseline data collected over a 12-month period (June 9, 2020–June 8, 2021) from the Omtanke2020 Study including 27,950 adults in Sweden. Participants were volunteers or actively recruited through existing cohorts and, after providing informed consent, responded to online questionnaires on socio-demographics, mental and physical health, as well as COVID-19 infection and impact. Poisson regression was fitted to assess the relative risk of demonstrating high level symptoms of depression, anxiety, and COVID-19 related distress.
Result
The proportion of persons with high level of symptoms was 15.6 %, 9.5 % and 24.5 % for depression, anxiety, and COVID-19 specific post-traumatic stress disorder (PTSD), respectively. Overall, 43.4 % of the participants had significant, clinically relevant symptoms for at least one of the three mental health outcomes and 7.3 % had significant symptoms for all three outcomes. We also observed differences in the prevalence of these outcomes across strata of sex, age, recruitment type, COVID-19 status, region, and seasonality.
Conclusion
While the proportion of persons with high mental health burden remains higher than the ones reported in pre-pandemic publications, our estimates are lower than previously reported levels of depression, anxiety, and PTSD during the pandemic in Sweden and elsewhere.
Keywords: Anxiety symptoms, COVID-19, Depressive symptoms, General population, Mental health, Omtanke2020 Study, Stress, Sweden
Since the appearance of the Coronavirus Disease (COVID-19) in late 2019, profuse attention has been given to the mental health aspects of this disease. By August 2022, Google Scholar had listed over 4,800,000 separate documents on COVID-19, of which more than 1,750,000 were about the mental health impact of the pandemic. Along with the proliferation of publications, many efforts have also been made in measuring prevalence of different mental health outcomes across the globe (e.g., Bäuerle et al., 2020; Cénat et al., 2021; Daly et al., 2020; Deng et al., 2021; McCracken et al., 2020; Pieh et al., 2020; Rondung et al., 2021; Xiong et al., 2020).
The coronavirus was declared to be present in Sweden on 31 January 2020, with community spread in Stockholm confirmed on 9 March 2020 and the first death caused by COVID-19 on 11 March 2020. By 13 March 2020, the virus was present in all 21 Swedish regions (Folkhälsomyndigheten [Swedish Public Health Agency], 2020). As of early August 2022, there were over 2.5 million confirmed cumulative cases and 19,433 deaths with confirmed COVID-19 infection, ranking Sweden 30th (out of 47) in Europe, per capita deaths (ECDC, 2022). However, about 14,500 of these deaths occurred between March 2020 and June 2021, including over 5500 deaths occurred before June 2020 due to the spreading of the virus in nursing homes (Brandén et al., 2020).
In contrast to many other countries that implemented strict lockdowns and legal restrictions, Swedish authorities responded with relatively limited measures throughout the pandemic. The Swedish population was expected to follow a series of recommendations from the Public Health Agency, including working from home when possible, limiting travel within the country, social distancing, and self-isolation for risk groups and people aged 70 years or older. During the most stringent periods, laws of banning gatherings and events with more than 50 people were also in place. Nevertheless, primary schools remained open throughout, and face masks were not mandatory. Vaccinations became available from December 2020 and vaccination passports were used between late 2021 and February 2022, when all pandemic measures were lifted. As of April 2022, 85 % of Swedish residents over the age of 12 years had been vaccinated with at least two doses (Folkhälsomyndigheten [Swedish Public Health Agency], 2022).
The Swedish health care system is primarily government-funded, whereas private health insurance accounts for less than 3 % of all expenses (Anell, 2008). Approximately 12 % of Sweden's GDP was spent on health care in 2015, in part explained by the fact that Sweden's population is relatively old. Health care coverage in Sweden is universal with all residents entitled to publicly financed health care, affordable, and decentralised (Rae, 2005). Sweden, as other Nordic countries, has well-developed national guidelines for care of mental health, including implementation of internet-delivered therapy for mental illness (Yogarajah et al., 2020). On the other hand, there is a shortage of primary care physicians and long waiting time for care despite the national guarantee of care, and access to health care is relatively inequitable. The latter is also elucidated by reports showing that individuals of non-Swedish ethnicities and those living in working class areas were more likely to die due to COVID-19 (Drefahl et al., 2020). During Spring 2020, to avoid overwhelming the health care system, a large proportion of healthcare visits, including surgeries, were postponed or cancelled (Carlén and Sima, 2020).
Strict stay-at-home policy is associated with greater anxiety, worry about finance, and loneliness (Tull et al., 2020). While such lockdowns were unknown in Sweden, voluntary self-isolation was shown to have a negative impact on mental health in Swedish elderly citizens (Gustavsson and Beckman, 2020) and university students (Berman et al., 2022), who were both shown to have a high compliance to the recommendations. Several other Swedish studies also reported increased mental health burden during the first wave of the pandemic (e.g., McCracken et al., 2020; Rondung et al., 2021; Skoog, 2020). For instance, in an online survey conducted in Spring 2020, an increased prevalence of depression (30 %), anxiety (24 %), and insomnia (38 %) was observed in Sweden (McCracken et al., 2020), in line with two meta-analyses showing a prevalence of depression from 15.2 % (Cénat et al., 2021) to 45 % (Deng et al., 2021).
To this end, we present data on several indicators of mental health among Swedish adults over a 12-month period during the COVID-19 pandemic (9 June 2020 to 8 June 2021) collected in the Omtanke2020 Study (https://ki.se/omtanke2020). The aim of this paper is twofold: (1) to introduce the Omtanke2020 Study and summarize its baseline data and (2) to provide estimates of several main mental health outcomes (e.g., depressive, anxiety, and COVID-19-related distress symptoms) among the study participants of the Omtanke2020 Study, overall and by age, sex, COVID-19 diagnosis, geographic area, and calendar period.
1. Methods
1.1. Participants and procedure
Enrolment for the Omtanke2020 Study was open from 9 June 2020 to 8 June 2021 to all adults in Sweden (18 years or older) who had a BankID (unique electronic identification possessed by over 98 % of Sweden's adult population) and could read and understand Swedish. The Omtanke2020 Study is hosted by Karolinska Institutet, Sweden's largest medical university located in Stockholm. The study is funded by NordForsk (project No. 105668) and Karolinska Institutet. Participants were invited through (social) media campaigns or through personal invitation via ongoing studies at Karolinska Institutet, including LifeGene (https://lifegene.se), Karolinska Mammography Project for Risk Prediction of Breast Cancer (KARMA, https://karmastudy.org), and the Swedish Twin Registry (STR, https://strdata.se). A total of 29,521 individuals participated in the study by giving informed consent, including 28,293 participants who answered at least one question. In this paper we present cross-sectional baseline data of the Omtanke2020 Study. Supplementary Fig. 1 portrays the flowchart of including participants in the analysis of the present study. We included all participants who answered at least three out of the four mental health measures, namely depression, anxiety, stress, and COVID-related distress, at baseline (N = 27,950).
1.2. Measures
Demographics. We collected data on age, sex, relationship and employment status, region, and general lifestyle and health (smoking and drinking habits, body mass index (BMI), chronic diseases, and previous psychiatric disorders). We also asked participants if they joined the study through personal invitation or through media campaigns or other outreach activities (recruitment type).
Depression. The Patient Health Questionnaire (PHQ-9) is a validated screening tool for depressive symptoms and their severity, consisting of nine items measured on a four-point Likert scale (0 = not at all, 1 = some days, 2 = more than half of the days, 3 = nearly every day). Hence, the PHQ-9 total score ranges from 0 to 27. The suggested cut-off points for mild, moderate, moderately severe, and severe depression are 5, 10, 15, and 20, respectively (Kroenke et al., 2001). The use of cut-off of 10 to create a binary outcome (i.e., depression) has been reported to have 88 % specificity and 88 % sensitivity. The internal consistency for the PHQ-9 based on the present study sample was α = 0.88.
Anxiety. The General Anxiety Disorder (GAD-7) scale is a validated screening tool for symptoms of generalized anxiety disorder. The scale consists of seven items measured on a four-point Likert scale and the total score lies between 0 and 21. The suggested cut-off points for mild, moderate, and severe anxiety are 5, 10, and 15, respectively (Spitzer et al., 2006). The use cut-off of 10 to create a binary outcome (i.e., anxiety) has been reported to have 82 % specificity and 89 % sensitivity. The internal consistency for the GAD-7 based on the present study sample was α = 0.90.
COVID-19-related distress. We used a COVID-19-adapted Primary Care PTSD Screen consisting of five items, which is a post-traumatic stress disorder (PTSD) screen for DSM V (PC-PTSD-5), to identify COVID-19 specific PTSD. The use of cut-off of four to create a binary outcome (i.e., PTSD) was shown to have 82 % specificity and 91 % sensitivity (Prins et al., 2016). We modified all questions to relate to COVID-19. For example, “…have you had nightmares about the event(s) …” was replaced with “… have you had nightmares about COVID-19 …”. Because of this change, we refer to this scale as “COVID-related distress” and to the questionnaire as “C-19 PC-PTSD-5” in the text. The internal consistency for the PC-PTSD-5 based on the present study sample was α = 0.77.
Stress. The four-item version of the Perceived Stress Scale (PSS-4) was used to assess stress levels on a five-point Likert-scale, assessing the occurrence of symptoms from 1 = never to 5 = very often (Cohen and Williamson, 1988). The negatively coded (reversed) items were recoded before analysis. This scale has no established cut-off.
Other mental health indicators. Sleep quantity measured as hours slept per night on average during the last 14 days as well as sleep quality on a five-point Likert scale were collected (1 the worst and 5 the best quality). These items were taken from the Pittsburgh Sleep Quality Index (PSQI; Buysse et al., 1989). Loneliness as well as general physical and mental well-being were all measured with one item, each on a five-point Likert scale, whereas happiness was measured with one item on a ten-point Likert scale.
COVID-19. COVID-19 status was based on self-reported, confirmed diagnosis with PCR or antibody test. Data about which test was taken, as well as the date and result of test were also collected.
1.3. Statistical analyses
Missing data. Participants always had the response option “I cannot/do not want to answer” resulting in missing values. For demographic variables, missing values are indicated in Table 1 . For mental health measures, incompleteness was less than 2 % for items of PHQ-9 and GAD-7 and less than 5 % for items of C-19 PC-PTSD-5. However, as each scale has multiple items, the missingness became greater when calculating the total score through summarising all items in each scale. For this reason, imputation based on the joint distribution was performed if the number of missing items from the measure was less than 35 % (i.e., allowing a maximum of three missing items for PHQ-9, two for GAD-7, and one for PSS-4 and C-19 PC-PTSD-5). If more items were missing, the score of the specific measure was not calculated for the participant. We chose imputation as complete case analysis not only reduces sample size but can also lead to biased estimates when the percentage of missingness is not low or missingness is not completely at random (Little and Rudin, 2002).
Table 1.
Socio-demographic characteristics of the participants.
| Variable | Started the survey (N = 28,311) |
Included in analysis (N = 27,950) |
Tested positive for COVID-19 (N = 2387) |
Tested negative for COVID-19 (N = 11,887) |
Not tested for COVID-19 (N = 13,676) |
|---|---|---|---|---|---|
| Sex | |||||
| Male | 5234 (18.5 %) | 5171 (18.5 %) | 491 (20.6 %) | 2242 (18.9 %) | 2438 (17.8 %) |
| Female | 23,077 (81.5 %) | 22,779 (81.5 %) | 1896 (79.4 %) | 9645 (81.1 %) | 11,238 (82.2 %) |
| Age (years) | |||||
| Mean age (SD) | 48.6 (15.8) | 48.7 (15.8) | 44.5 (13.0) | 45.4 (14.1) | 52.3 (16.7) |
| 18–29 | 3940 (13.9 %) | 3859 (13.8 %) | 377 (15.8 %) | 1738 (14.6 %) | 1744 (12.8 %) |
| 30–39 | 5218 (18.4 %) | 5107 (18.3 %) | 499 (20.9 %) | 2819 (23.7 %) | 1789 (13.1 %) |
| 40–49 | 5411 (19.1 %) | 5342 (19.1 %) | 595 (24.9 %) | 2686 (22.6 %) | 2061 (15.1 %) |
| 50–59 | 6043 (21.4 %) | 5992 (21.4 %) | 616 (25.8 %) | 2545 (21.4 %) | 2831 (20.7 %) |
| 60–69 | 4462 (15.8 %) | 4435 (15.9 %) | 247 (10.4 %) | 1465 (12.3 %) | 2723 (19.9 %) |
| 70+ | 3237 (11.4 %) | 3215 (11.5 %) | 53 (2.2 %) | 634 (5.3 %) | 2528 (18.5 %) |
| Relationship status | |||||
| In a relationship | 20,500 (72.4 %) | 20,234 (72.4 %) | 1800 (75.4 %) | 8668 (72.9 %) | 9766 (71.4 %) |
| Single | 7664 (27.1 %) | 7664 (27.1 %) | 577 (24.2 %) | 3162 (26.6 %) | 3835 (28.0 %) |
| Missing | 147 (0.5 %) | 142 (0.50 %) | 10 (0.4 %) | 57 (0.5 %) | 75 (0.5 %) |
| Employment status | |||||
| Full-time work | 14,940 (52.8 %) | 14,752 (52.8 %) | 1590 (66.6 %) | 7289 (61.3 %) | 5873 (42.9 %) |
| Part-time work | 2112 (7.5 %) | 2075 (7.4 %) | 188 (7.9 %) | 950 (8.0 %) | 937 (6.9 %) |
| Not working | 2179 (7.7 %) | 2139 (7.7 %) | 172 (7.2 %) | 897 (7.5 %) | 1070 (7.8 %) |
| Retired | 6895 (24.4 %) | 6836 (24.5 %) | 263 (11.0 %) | 1826 (15.4 %) | 4747 (34.7 %) |
| Student | 2006 (7.1 %) | 1972 (7.1 %) | 159 (6.7 %) | 867 (7.3 %) | 946 (6.9 %) |
| Missing | 200 (0.6 %) | 176 (0.6 %) | 15 (0.6 %) | 58 (0.5 %) | 103 (0.7 %) |
| Body Mass Index | |||||
| Normal weight (<25) | 14,467 (51.1 %) | 14,465 (51.8 %) | 1207 (50.6 %) | 6361 (53.5 %) | 6897 (50.4 %) |
| Overweight (25–30) | 8169 (28.9 %) | 8168 (29.2 %) | 695 (29.1 %) | 3421 (28.8 %) | 4052 (29.6 %) |
| Obese (>30) | 3707 (13.1 %) | 3707 (13.3 %) | 364 (15.2 %) | 1534 (12.9 %) | 1809 (13.2 %) |
| Missing | 1968 (6.9 %) | 1610 (5.8 %) | 121 (5.0 %) | 571 (4.8 %) | 918 (6.7 %) |
| Current smoking | |||||
| No | 22,824 (80.6 %) | 22,818 (81.6 %) | 1915 (80.2 %) | 9659 (81.3 %) | 11,244 (82.2 %) |
| Yes | 4662 (16.5 %) | 4662 (16.7 %) | 434 (1.8 %) | 2102 (17.7 %) | 2126 (15.5 %) |
| Missing | 825 (2.9 %) | 470 (1.7 %) | 38 (1.6 %) | 126 (1.1 %) | 306 (2.2 %) |
| Binge drinking | |||||
| No | 14,985 (52.9 %) | 14,984 (53.6 %) | 1317 (55.2 %) | 6752 (56.8 %) | 6915 (50.6 %) |
| Yes | 7285 (25.7 %) | 7283 (26.1 %) | 658 (27.6 %) | 3008 (25.3 %) | 3617 (26.4 %) |
| Missing | 6062 (21.4 %) | 5683 (20.3 %) | 412 (17.3 %) | 2127 (17.9 %) | 3144 (23.0 %) |
| Somatic diseases | |||||
| None | 18,726 (66.1 %) | 18,720 (67.0 %) | 1700 (71.2 %) | 8376 (70.5 %) | 8644 (63.2 %) |
| One | 6500 (23.0 %) | 6500 (23.3 %) | 512 (21.4 %) | 2602 (21.9 %) | 3386 (24.8 %) |
| Two | 1731 (6.1 %) | 1731 (6.2 %) | 115 (4.8 %) | 617 (5.2 %) | 999 (7.3 %) |
| Three or more | 604 (2.1 %) | 604 (2.2 %) | 30 (1.3 %) | 194 (1.6 %) | 380 (2.8 %) |
| Missing | 750 (2.6 %) | 395 (1.4 %) | 30 (1.3 %) | 98 (0.8 %) | 267 (2.0 %) |
| Previous psychiatric disorder | |||||
| No | 17,824 (63.0 %) | 17,812 (63.7 %) | 1485 (62.2 %) | 7245 (60.9 %) | 9082 (66.4 %) |
| Yes | 9480 (33.4 %) | 9475 (33.9 %) | 857 (35.9 %) | 4436 (37.3 %) | 4182 (30.6) |
| Missing | 1028 (3.6 %) | 663 (2.4 %) | 45 (1.9 %) | 98 (0.8 %) | 412 (3.0 %) |
| Self-recruitment | |||||
| No | 12,125 (42.8 %) | 12,122 (43.4 %) | 865 (36.2 %) | 4936 (41.5 %) | 6321 (46.2 %) |
| Yes | 16,207 (57.2 %) | 15,928 (56.6 %) | 1522 (63.8 %) | 6951 (58.5 %) | 7355 (53.8 %) |
| Time of participation | |||||
| Jun-Aug 2020 | 7689 (27.1 %) | 7566 (27.1 %) | 494 (20.7 %) | 2083 (17.5 %) | 4990 (36.5 %) |
| Sep-Nov 2020 | 8588 (30.3 %) | 8520 (30.5 %) | 413 (17.3 %) | 2876 (24.2 %) | 5231 (38.3 %) |
| Dec 2020-Feb 2021 | 7532 (26.6 %) | 7411 (26.5 %) | 708 (29.7 %) | 4189 (35.2 %) | 2514 (18.4 %) |
| Mar 2021-Jun 2021 | 4523 (16.0 %) | 4453 (15.9 %) | 772 (32.3 %) | 2740 (23.1 %) | 941 (6.9 %) |
Analyses. We used Spearman correlation coefficients with confidence limits to calculate correlations of the scores of the four mental health measures and other mental health indicators, due to the skewness of these variables. Pairwise deletion was used, with at least 27,000 observations included for each correlation coefficient. We used modified Poisson regression to analyse binary outcomes, as suggested by Kroenke et al. (2001) for depression, Spitzer et al. (2006) for anxiety, and Prins et al. (2016) for PTSD, to estimate the prevalence of depression, anxiety, and COVID-19 specific PTSD, adjusted for age, sex, and recruitment type, unless otherwise indicated. We report the relative risk of depression, anxiety, and COVID-19 specific PTSD with 95 % confidence intervals.
2. Results
2.1. Descriptives
Descriptives of the demographic characteristics among the participants included in the present study and all participants of the Omtanke2020 Study are given in Table 1. Age ranged from 18 to 94 years (mean age: 48.7 years; SD: 15.8 years) and 5107 (18.5 %) were male. All Swedish counties were represented with an over-representation of Stockholm region (12,296 persons, 44.0 %). 43.4 % of the participants were invited from previously established cohorts at Karolinska Institutet, mainly from KARMA (N = 5342; 44.1 %; all women), LifeGene (N = 3592; 29.6 %), and STR (N = 3459; 28.5 %). A participant might belong to more than one of these cohorts. Participation rate among those invited ranged 7–11 %, depending on the cohort.
2387 participants (8.5 %) had been diagnosed with COVID-19 before joining the study. Table 1 also shows the descriptives of the participants depending on COVID-19 test and diagnosis status, including three groups of participants, namely those who tested positive or negative for COVID-19 and those who had not taken any test before study entry. The three groups were comparable, although those who were not tested were slightly older (mean age 52.3 compared to mean age 44.5 and 45.4 for positive and negative participants, respectively) and had a much higher percentage of retirees (35 % compared to 11 % and 15 % for positive and negative participants, respectively). The group of COVID-19 infected participants had, in general, a slightly higher proportion of obesity (15.2 % vs. 12.9 % and 13.2 % among those tested negative or those not tested), current smoking (18.2 % vs. 17.7 % and 15.5 % among those tested negative or those not tested), and binge drinking (27.6 % vs. 25.3 % and 26.4 % among those tested negative or those not tested), a slightly lower proportion of somatic comorbidity (71.2 % without a somatic disease vs. 70.5 % and 63.2 % among those tested negative or those not tested), and a higher proportion of self-recruitment (63.8 % vs. 58.8 % and 53.8 % among those tested negative or those not tested).
2.2. Mental health measures
Descriptives and unadjusted rank correlations between the scores of the four mental health measures and other mental health indicators are displayed in Table 2 . All these measures included data from at least 27,500 participants. For each measure, the whole range of possible values could be observed. PHQ-9, GAD-7, and C-19 PC-PTSD-5 all had skewed distributions. 21,991 participants (78.7 %) had minimal or mild whereas 2550 (9.1 %) had moderately severe or severe level of depressive symptoms. Anxiety was even more skewed with 23,763 (85.1 %) and 1599 (5.7 %) participants had minimal and mild or severe anxiety symptoms, respectively.
Table 2.
Mental health outcomes.
| Descriptives | |||||||
|---|---|---|---|---|---|---|---|
| Variable | N | Mean | Std Dev | Median | Minimum | Maximum | High score means |
| PHQ-9 | 27,950 | 5.83 | 5.51 | 4 | 0 | 27 | More symptoms |
| GAD-7 | 27,950 | 4.43 | 4.78 | 3 | 0 | 21 | More symptoms |
| PSS-4 | 27,916 | 7.53 | 2.27 | 8 | 0 | 16 | More symptoms |
| PC-PTSD-5 | 27,658 | 4.71 | 3.97 | 4 | 0 | 20 | More symptoms |
| Loneliness | 27,886 | 1.68 | 0.96 | 1 | 1 | 4 | Lonelier |
| Happiness | 27,027 | 7.05 | 1.97 | 7 | 1 | 10 | Happier |
| Physical health | 27,944 | 2.90 | 0.84 | 2 | 1 | 4 | Better health |
| Mental health | 27,939 | 2.85 | 0.92 | 2 | 1 | 4 | Better health |
| Frequencies for the categorised PHQ-9 and GAD-7 | |||||
|---|---|---|---|---|---|
| PHQ-9 | GAD-7 | Total score | |||
| Minimal | 14,580 | (52.2 %) | 17,514 | (62.7 %) | 0–4 |
| Mild | 7411 | (26.5 %) | 6249 | (22.4 %) | 5–9 |
| Moderate | 3411 | (12.2 %) | 2588 | (9.3 %) | 10–14 |
| (Moderately) severe | 1684 | (6.0 %) | 1599 | (5.7 %) | 15+ |
| SEVERE | 866 | (3.1 %) | 20+ (for PHQ-9 only) | ||
| PHQ-9 | GAD-7 | PSS-4 | PC-PTSD | Loneliness | Happiness | Mental health | |
|---|---|---|---|---|---|---|---|
| Spearman correlation coefficients and confidence limits of mental health measures | |||||||
| GAD-7 | 0.78 | ||||||
| (0.78–0.79) | |||||||
| PSS-4 | 0.28 | 0.34 | |||||
| (0.27–0.29) | (0.33–0.35) | ||||||
| PC-PTSD-5 | 0.47 | 0.51 | 0.23 | ||||
| (0.46–0.48) | (0.50–0.52) | (0.21–0.24) | |||||
| Loneliness | 0.56 | 0.51 | 0.19 | 0.39 | |||
| (0.56–0.57) | (0.50–0.51) | (0.18–0.20) | (0.37–0.40) | ||||
| Happiness | −0.64 | −0.56 | −0.16 | −0.36 | −0.56 | ||
| (−0.65–0.63) | (−0.57–0.55) | (−0.17–0.14) | (−0.37–0.35) | (−0.57–0.55) | |||
| Mental health | −0.70 | −0.66 | −0.21 | −0.39 | −0.48 | 0.64 | |
| (−0.70–0.69) | (−0.67–0.65) | (−0.22–0.19) | (−0.40–0.38) | (−0.49–0.48) | (0.63–0.65) | ||
| Physical health | −0.43 | −0.33 | −0.10 | −0.24 | −0.24 | 0.37 | 0.49 |
| (−0.44–0.42) | (−0.34–0.32) | (−0.11–0.09) | (−0.26–0.23) | (−0.25–0.23) | (0.36–0.38) | (0.48–0.50) | |
| Spearman correlation coefficients and confidence limits of other variables | |||||||
| Age | −0.34 | −0.38 | −0.13 | −0.10 | −0.23 | 0.23 | −0.31 |
| (−0.35 to −0.33) | (−0.40 to −0.38) | (−0.15 to −0.12) | (−0.11 to −0.8) | (−0.24 to −0.22) | (0.22–0.24) | (−0.32 to −0.30) | |
| BMI | 0.09 | 0.01 | −0.01 | 0.06 | 0.03 | −0.03 | 0.07 |
| (0.08–0.10) | (0.00–0.03) | (−0.03 to −0.00) | (0.05–0.07) | (0.01–0.04) | (−0.05 to −0.02) | (0.06–0.08) | |
| Sleep quality | −0.55 | −0.45 | 0.14 | 0.28 | 0.29 | 0.39 | 0.42 |
| (−0.54 to −0.56) | (−0.46 to −0.44) | (0.13–0.15) | (0.27–0.29) | (0.28–0.30) | (0.38–0.40) | (0.41–0.43) | |
| Sleep quantity | −0.24 | −0.20 | −0.06 | −0.12 | −0.12 | 0.16 | −0.16 |
| (−0.26 to −0.23) | (−0.21–0.19) | (−0.07 to −0.05) | (−0.13 to −0.10) | (−0.13 to −0.11) | (0.15–0.17) | (−0.17 to −0.15) | |
| Disruption to daily life | 0.37 | 0.38 | 0.18 | 0.49 | 0.31 | −0.30 | 0.28 |
| (0.36–0.38) | (0.37–0.39) | (0.17–0.19) | (0.48.0.49) | (0.30–0.32) | (−0.31 to −0.29) | (0.27–0.29) | |
| Economic difficulties | 0.29 | 0.29 | 0.12 | 0.21 | 0.23 | −0.25 | 0.32 |
| (0.28–0.30) | (0.28–0.30) | (0.11–0.14) | (0.19–0.22) | (0.22–0.24) | (−0.26 to −0.24) | (0.31–0.33) | |
| COVID-19 worries | 0.21 | 0.27 | 0.10 | 0.49 | 0.16 | 0.15 | −0.19 |
| (0.19–0.22) | (0.26–0.28) | (0.09–0.11) | (0.48–0.50) | (0.15–0.17) | (0.14–0.16) | (−0.21 to −0.18) | |
| Comorbidities (N) | 0.04 | −0.00 | −0.00 | 0.10 | 0.03 | −0.02 | 0.03 |
| (0.03–0.05) | (−0.01–0.01) | (−0.02–0.01) | (0.08–0.11) | (0.01–0.04) | (−0.03 to −0.01) | (0.01–0.04) | |
All mental health measures were correlated to each other with a correlation coefficient ranging from 0.10 to 0.78. PSS-4 had the lowest correlations with the other measures, while PHQ-9 was highly correlated with the other measures, especially GAD-7 (0.78), general mental health (−0.70), and self-rated happiness (−0.64). Happiness was more strongly correlated with mental health (0.64) than physical health (0.37). The correlation between mental and physical health was however moderate (0.49).
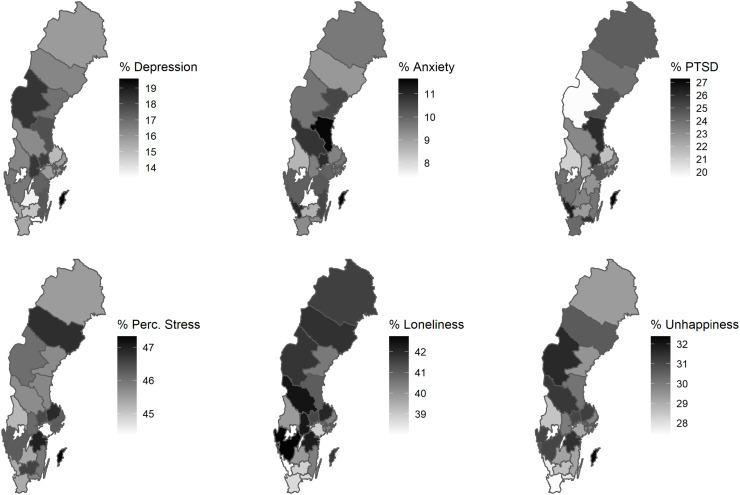
Fig. 1 shows the county-level prevalence of depression, anxiety, and COVID-19 specific PTSD (i.e., scores of PHQ-9, GAD-7, and C-19 PC-PTSD-5 above cut-off) and means of perceived stress (PSS-4), loneliness, and unhappiness (happiness inverted), converted to a 0–100 scale, after adjustment for age, sex, and recruitment type. While most measures showed a regional difference of 2.5 % (PSS-4) to 4 % (unhappiness), prevalence of depression and COVID-19 specific PTSD seemed to vary more across regions. In general, regions with the highest prevalence of COVID-19 specific PTSD had also the highest prevalence of anxiety.
Fig. 1.
Geographical differences in mental health outcomes across Sweden.
BMI, number of comorbidities, and sleep quantity were less correlated to depression, anxiety, and COVID-19 specific PTSD symptoms (correlation coefficients below 0.25) (Table 2). Age was inversely correlated to depression and anxiety and, to a very small extent, COVID-19 specific PTSD symptoms. Perceived disruption to daily life, economic difficulties, and worries about COVID-19 were all correlated to the mental health measures although to a varying degree (correlation coefficients ranged from 0.21 to 0.49). Sleep quality had a strong negative correlation with depression and anxiety but not COVID-19 specific PTSD symptoms. Perceived stress was again correlated to these variables to a very low degree. For this reason and given the lack of an established cut-off for the PSS-4, the rest of the analyses focused on PHQ-9, GAD-7, and C-19 PC-PTSD-5.
Table 3 shows the prevalence of depression, anxiety, and COVID-19 specific PTSD for the entire study sample as well as by sex, age group, recruitment type, and COVID-19 status. The prevalence was lowest for anxiety (9.5 %, 4187 participants) and highest for COVID-specific PTSD (24.5 %, 8572 participants). The prevalence of depression, anxiety, and COVID-19 specific PTSD was higher in female participants, i.e., 3.7 % and 3.3 % higher for depression and anxiety, respectively, comparing female with male participants. The sex difference was greater for COVID-19 specific PTSD (12.8 % higher in female). Prevalence of depression and anxiety decreased with age, although the prevalence of COVID-19 specific PTSD demonstrated a U-shaped form with the youngest (27.3 %) and oldest (30.0 %) participants scoring high. The biggest differences were seen between invited and self-recruited participants, where self-recruited participants had doubled prevalence of all three measures, compared with the invited participants. Participants with a confirmed COVID-19 diagnosis before joining the study had slightly higher prevalence of depression and anxiety, but slightly lower prevalence of COVID-19 specific PTSD, compared with others.
Table 3.
Proportion of participants with high depressive, anxiety and PTSD symptoms.
| Overall proportiona | Depression |
Anxiety |
PTSD |
|||
|---|---|---|---|---|---|---|
| 5961 | 15.3 % (14.8 %–15.9 %) | 4187 | 9.5 % (9.1 %–10.0 %) | 8572 | 24.5 % (23.8 %–25.2 %) | |
| Sexb | ||||||
| Female | 5500 | 17.3 % (16.8 %–17.8 %) | 3598 | 11.3 % (10.9 %–11.8 %) | 7561 | 31.7 % (31.0 %–32.3 %) |
| Male | 911 | 13.6 % (12.8 %–14.4 %) | 589 | 8.0 % (7.4 %–8.7 %) | 1011 | 18.9 % (17.9 %–20.0 %) |
| Age groupc | ||||||
| 18–29 | 1622 | 32.2 % (30.7 %–33.7 %) | 1266 | 24.0 % (22.6 %–25.4 %) | 1407 | 27.3 % (26.1 %–28.7 %) |
| 30–39 | 1457 | 22.1 % (20.9 %–23.7 %) | 1103 | 15.9 % (15.0 %–17.0 %) | 1666 | 24.6 % (23.5 %–25.8 %) |
| 40–49 | 1113 | 16.7 % (15.7 %–17.7 %) | 790 | 11.3 % (10.5 %–12.1 %) | 1487 | 21.3 % (20.3 %–22.3 %) |
| 50–59 | 995 | 14.6 % (13.8 %–15.6&) | 593 | 8.3 % (7.7 %–9.0 %) | 1632 | 22.1 % (21.1 %–23.2 %) |
| 60–69 | 491 | 10.1 % (9.3 %–11.0 %) | 284 | 5.6 % (5.0 %–6.3 %) | 1295 | 24.3 % (23.1 %–25.6 %) |
| 70–94 | 283 | 8.6 % (7.7 %–9.6 %) | 151 | 4.4 % (3.8 %–5.2 %) | 1085 | 30.0 % (28.5 %–31.7 %) |
| Recruitment typed | ||||||
| Self-recruited | 4526 | 21.1 % (20.3 %–22.0 %) | 3256 | 13.4 % (12.7 %–14.1 %) | 5773 | 31.0 % (30.0 %–32.0 %) |
| Invited | 1435 | 11.1 % (10.6 %–11.7 %) | 931 | 6.8 % (6.3 %–7.2 %) | 2799 | 19.4 % (18.6 %–20.1 %) |
| Confirmed COVID-19 diagnosisa | ||||||
| No | 5336 | 15.2 % (14.6 %–15.8 %) | 3760 | 9.5 % (9.0 %–9.9 %) | 12,555 | 24.7 % (24.0 %–25.5 %) |
| Yes | 625 | 16.8 % (15.7 %–18.1 %) | 427 | 10.4 % (9.2 %–11.0 %) | 1122 | 22.2 % (20.8 %–23.8 %) |
a – Adjusted to age 50 years, sex and recruitment type; b – Adjusted to age 50 years and recruitment type; c – Adjusted for sex and recruitment type; d – Adjusted to age 50 years, and sex.
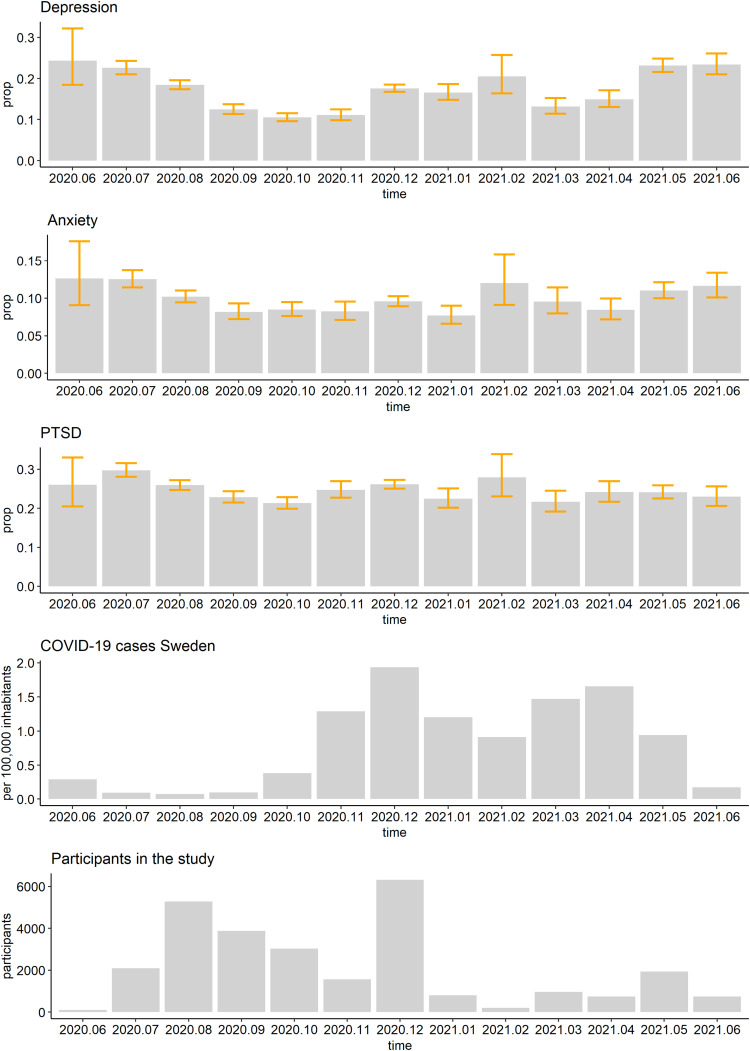
Fig. 2 shows the prevalence of depression, anxiety, and COVID-19 specific PTSD, plus confidence interval, per calendar month, after adjustment for age, sex, and recruitment type, along with number of COVID-19 cases in Sweden and number of newly recruited study participants on the same time scale. The prevalence of depression showed the greatest variation (10.5 % in October 2020 vs 24.4 % in June 2020 and 23.4 % in June 2021) while the prevalence of COVID-19 specific PTSD was relatively stable over time (21.3 % in October 2020 to 29.6 % in July 2020).
Fig. 2.
Proportion of participants above cut-off for depressive, anxiety and PTSD symptoms, COVID-19 monthly incidence per 100,000 inhabitants in Sweden, and number of new participants joining the Omtanke2020 study per month.
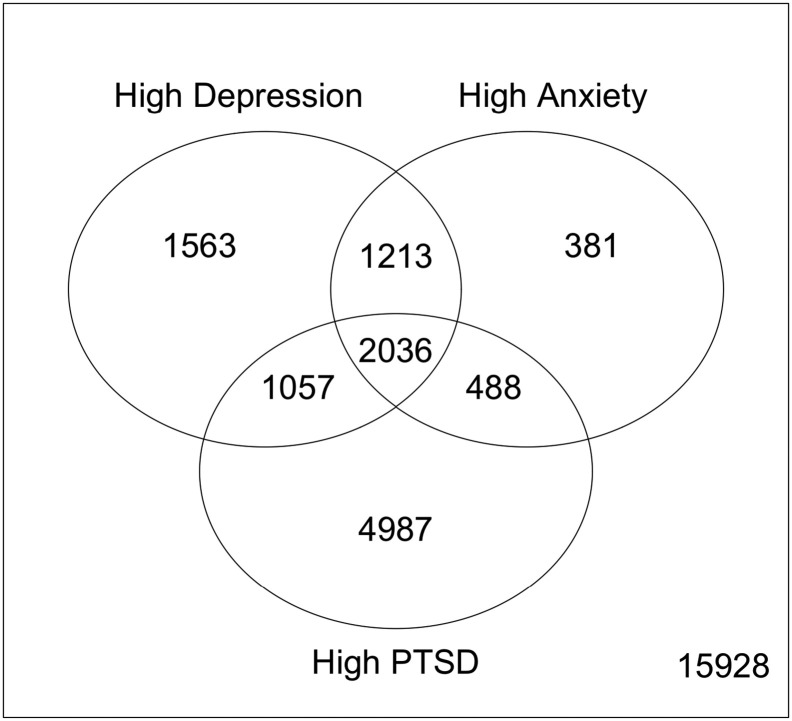
Fig. 3 shows the pattern of comorbidities between depression, anxiety, and COVID-19 specific PTSD. 11,725 participants (43.4 %) had at least one of the three outcomes, among which, most had COVID-19 specific PTSD alone (4987 persons, 18.0 %), followed by those with all three outcomes (2036 persons; 7.4 %). The least common was to have only anxiety (381 persons, 1.4 %), followed by to have anxiety plus COVID-19 specific PTSD (488 persons, 1.8 %). The results by age, sex, and COVID-19 status show similar pattern whereas self-recruited participants showed higher prevalence of all mental health outcomes, compared with participants recruited by invitation (data not shown).
Fig. 3.
Venn diagram of the different profiles of participants with mental disorder symptoms.
3. Discussion
In the present paper, we described the mental health of adults in Sweden over a 12-month period during the ongoing COVID-19 pandemic. We focused on depressive, anxiety, and COVID-19 related distress symptoms and provided prevalence estimates of depression, anxiety, and COVID-19 specific PTSD by sex, age group, recruitment type, COVID-19 status, region, and calendar time. Compared to what has been reported during Spring 2020 in Sweden (McCracken et al., 2020), our results suggest more moderate prevalence of depression (15.3 % vs 30 %) and anxiety (9.5 % vs 24.2 %). This difference could have arisen both from the difference in study period (Spring 2020 vs June 2020–June 2021) and data collection method (recruitment through social media only vs recruitment through both social media and personal invitation). We demonstrated that participants recruited through social and traditional media outlets tended to demonstrate higher burden of mental health symptoms. We also found that women and younger participants had a higher prevalence of depression, anxiety, and COVID-19 specific PTSD, which is supported by a large number of studies and meta-analyses (Bäuerle et al., 2020; Daly et al., 2020; Pieh et al., 2020; Xiong et al., 2020).
3.1. Results in context
The pre-pandemic prevalence of depression in Sweden was estimated as 8.75 % (95 % CI: 8.0 %–9.5 %) in one study (Arias-de la Torre et al., 2021) and 10.8 % (95 % CI: 9.1 %–12.5 %) in another (Johansson et al., 2013). The study by Johansson et al. (2013) used a lower cut-off (eight instead of 10) for GAD-7 and estimated the prevalence of anxiety as 14.7 % (95 % CI: 12.7 %–16.6 %). With different methodology, Munk-Jørgensen et al. (2006) obtained prevalence estimates of 5.6 % for anxiety (95 % CI: 3.4–7.7 for men and 3.9–7.2 for women) and of 7.2 for depression among men and 11.8 % among women. Pre-pandemic prevalence of PTSD was estimated as 5.6 % (Frans et al., 2005). In conclusion, we observed in general slightly higher prevalence of depression, anxiety, and COVID-19 specific PTSD in the present study, compared with pre-pandemic levels.
To put the findings into context, we compared our results to what has been reported in other countries. Bäuerle et al. (2020) obtained responses from over 15,000 German residents between March and May 2020 and reported an unadjusted prevalence of depression and anxiety as 14.3 % and 16.8 %, respectively. Pre-pandemic prevalence of depression in Germany was estimated at 9.7 % by Arias-de la Torre et al. (2021). Moreover, the unadjusted prevalence showed very similar sex differences (15.1 % and 12.2 % for depression and 18.3 % and 10.6 % for anxiety among women and men, respectively) and a decreasing trend by age. In Austria, based on a sample of 1005 adults, the unadjusted prevalence was 21 % for depression and 19 % for anxiety during the lockdown period in April 2020 (Pieh et al., 2020). A large-scale meta-analysis including a sample size of 146,139 adults from worldwide data collected in Spring-Summer 2020 by Liu et al. (2021) resulted in a prevalence of 27.6 % (95 % CI: 24.0 %–31.1 %) for depression, 32.6 % (95 % CI: 29.1 %–36.3 %) for anxiety, and 16.7 % (95 % CI: 27.5 %–36.7 %) for PTSD. The much higher estimates in the last study may be partially attributed to the inclusion of studies of severely ill COVID-19 patients and front-line health-care workers, as well as the inclusion of many studies conducted during the peak of the first wave when the mental health burden was reported to be the highest. In a longitudinal study, Daly et al. (2020) found that from Spring to Summer 2020, the prevalence of mental health problems measured with the GHQ-12 decreased over time but remained significantly higher than the pre-pandemic levels. A comparison of our findings to the ones of other Nordic countries can be found in a recent publication by Unnarsdóttir et al. (2022), which reported age- and sex-adjusted prevalence of depression as 7.6 % (95 % CI: 7.4 %–7.9 %) for Denmark, 16.6 % (95 % CI: 16.0 %–17.2 %) for Iceland, and 17.1 % (95 % CI: 16.1 %–18.1 %) and 4.2 % (95 % CI: 4.0 %–4.3 %) for two different cohorts in Norway.
Although there is a rich literature on the prevalence of depression and anxiety, partly also for PTSD, during the pandemic, relatively few studies have focused on the co-occurrence or co-prevalence of different mental health problems during the pandemic. A preprint from Nepal (Sigdel et al., 2020) reported a prevalence of 23.2 % for depression-anxiety comorbidity during April 2020. In that study, the prevalence of depression and anxiety was estimated as 34.0 % and 31.0 %, respectively, close to the pooled estimate from Liu et al.'s meta-analysis (2021), concerning a similar calendar period. The prevalence of depression-anxiety comorbidity is higher than the 11.6 % we observed in the present study. However, together with the high prevalence of depression and anxiety observed in that study, it might suggest that it is more common to have only depression or anxiety in Nepal than in Sweden. An Irish study reported a prevalence of 17.7 % (95 % CI: 15.4 %–20.0 %) for COVID-19 related PTSD and found very high comorbidity between PTSD and anxiety (49.5 %), as well as between PTSD and depression (53.8 %) (Karatzias et al., 2020). As we used an adapted questionnaire to assess PTSD symptoms, direct comparison between the two studies is likely not meaningful. Regardless, we identified 11.1 % of the participants to have both depression and COVID-19 specific PTSD, and 9.0 % with both anxiety and COVID-19 specific PTSD, also indicating high levels of comorbidity.
3.2. Strengths and limitations
The strengths of the study include a complex and inclusive recruitment strategy, allowing interested people enough time to join the study. We also have a much larger sample size than previous studies from Sweden (1503 in Rondung et al. (2021) and 1212 in McCracken et al. (2020)). Our study also has limitations. First, while the survey has been open to all, selection bias cannot be neglected. More than 80 % of the sample were women partly because women are more likely to participate in survey research and partly because the KARMA cohort (contributing over 5500 participants) is made up entirely by women. Similarly, the younger age groups were under-represented, relative to older age groups. Further, recruitment type was strongly related to mental health outcomes. For this reason, we corrected all analyses for this factor. However, leftover influence of this factor might still have impacted the results to some extent. Regardless, the fact that over 43 % of the participants scored above cut-off values of at least one of the mental health measures indicates the notable mental health burden of COVID-19. This is also very close to the 45.6 % reported by McCracken et al., although their third outcome was insomnia (McCracken et al., 2020).
3.3. Other considerations and future perspectives
The modified PTSD scale reflects the distress related specifically to COVID-19. Although the original PC-PTSD-5 has two established cut-offs, three or four, we, in the present study, chose the higher cut-off (i.e., four), which is known to have a lower sensitivity but a higher specificity, compared to the lower cut-off (i.e., three) (Prins et al., 2016). As the item about thinking about the traumatic event (“Tried hard not to think about COVID-19”) is something 2/3 of the participants of the present Study experienced at least occasionally, we prioritized specificity over sensitivity to avoid inflating the proportion of participants with a score above cut-off. Further, the Cronbach's alpha of the modified COVID-19 scale was found to be 77 % in the present study, suggesting that the internal consistency of this scale is likely satisfactory. Regardless, although this scale has indeed been used in other Nordic studies (for example by Saevarsdóttir et al., 2021), a formal validation study of the COVID-19 specific PC-PTSD-5 is currently lacking and needed.
We also observed weak correlation between PSS-4 and other mental health outcomes, including the COVID-related distress scale. There could be several reasons for this. First, PSS-4 is an ordinal measure consisting of the total score of the four items, usually compared to normative values which are not available for Sweden to our knowledge. Second, the four-item version is the short form of the original ten-item scale and short forms tend to have worse psychometric properties compared to the longer surveys (e.g., Kruyen et al., 2013). Third, the reliability of this four-item measure was relatively low in our sample.
We found mild to moderate correlations between economic difficulties and the studied mental health outcomes, in contrast to earlier results from Sweden by Rondung et al. (2021). Being worried about COVID-19 also had little effect on the mental health measures, except for the COVID-related distress symptoms. Underlying reasons for such differences need further research. As depression and anxiety have a relatively strong link with sleep quality, future work is also needed to unravel the roles of these mental health outcomes on sleep. Further, more effort is needed to examine and validate the regional differences in mental health burden in Sweden, as well as in other countries. Understanding the underlying reasons for regional differences might be essential to understand how to mitigate the mental health burden of the pandemic and set up adequate intervention programmes.
It is interesting to note that self-recruited participants of the Omtanke2020 Study had a higher burden of mental health symptoms compared to participants enrolled through personal invitation. There are multiple potential explanations for such. First, participants of the existing cohort studies at the Karolinska Institutet who agreed to participate in yet another study during the pandemic might be healthier mentally, compared to others, regardless of the pandemic exposure. Second, psychological distress and mental symptoms experienced during the pandemic, due to direct or indirect impact of COVID-19, might be a strong motivation for people to enrol themselves to the Omtanke2020 Study. Regardless, this observation pinpoints the importance of knowledge about the representativeness of study participants in studies of mental health burden in the pandemic. This is also likely an important contributor to the noted differences in the estimates of mental health burden between studies. For instance, the present study has information on recruitment type and adjusted for this variable in all analyses, whereas many previous studies have not specifically addressed this. Regardless, direct comparison of estimates of mental health burden across the globe is inherently difficult, regardless of methodological differences between studies. For instance, Sweden has a unique welfare and health care system and has had very different mitigating strategies in response to the pandemic compared to other countries. Any observed difference in mental health burden between Sweden and other countries might therefore also be due to such differences and therefore true.
4. Conclusion
In summary, we presented baseline data of our newly established Omtanke2020 Study, collecting data from nearly 28,000 adult participants in Sweden. While the proportion of persons with depression, anxiety, and PTSD remains higher than observed before the pandemic, our estimates are considerably lower than previously reported.
The following are the supplementary data related to this article.
Flowchart of participants.
CRediT authorship contribution statement
All co-authors contributed to the design of the study. AL and JG-H performed the statistical analyses, AL drafted the manuscript. All co-authors critically revised the draft and approved the final version.
Funding
The Omtanke2020 study is supported by NordForsk (project No. 105668) and Karolinska Institute (Strategic Research Area in Epidemiology and Senior Researcher Award). We acknowledge The Swedish Twin Registry for access to contact information to participating twins. The Swedish Twin Registry is managed by Karolinska Institutet and receives funding through the Swedish Research Council under the grant no 2017-00641. The Funding Sources had no direct or indirect impact on the analysis and interpretation of the results.
Ethical standard
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. The Omtanke2020 study has been registered and approved (DNR 2020-01785) by Etikprövningsmyndigheten (Swedish National Ethics Board) on 3 June 2020.
Conflict of Interest
The authors have no known conflict of interest to disclose.
Acknowledgement
This study was funded with grants from NordForsk (CovidMent, 105668), Horizon 2020 (CoMorMent, 847776), and the Karolinska Institutet.
References
- Anell A. The Swedish Health Care System. 2008. http://www.pnhp.org/PDF_files/LSE_Country_Profiles.pdf Online: Retrieved: 06-08-2022.
- Arias-de la Torre J., Vilagut G., Ronaldson A., Serrano-Blanco A., Martín V., Peters M., Alonso J.… Prevalence and variability of current depressive disorder in 27 european countries: a population-based study. Lancet Public Health. 2021;6(10):e729–e738. doi: 10.1016/S2468-2667(21)00047-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bäuerle A., Teufel M., Musche V., Weismüller B., Kohler H., Hetkamp M., Skoda E.M.… Increased generalized anxiety, depression and distress during the COVID-19 pandemic: a cross-sectional study in Germany. J. Public Health. 2020;42(4):672–678. doi: 10.1093/pubmed/fdaa106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berman A.H., Bendtsen M., Molander O., Lindfors P., Lindner P., Granlund L., Andersson C.… Compliance with recommendations limiting COVID-19 contagion among university students in Sweden: associations with self-reported symptoms, mental health and academic self-efficacy. Scand. J. Public Health. 2022;50(1):70–84. doi: 10.1177/14034948211027824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brandén M., Aradhya S., Kolk M., Härkönen J., Drefahl S., Malmberg B., Mussino E.… Residential context and COVID-19 mortality among adults aged 70 years and older in Stockholm: a population-based, observational study using individual-level data. Lancet Healthy Longev. 2020;1(2):e80–e88. doi: 10.1016/S2666-7568(20)30016-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buysse D.J., Reynolds C.F., III, Monk T.H., Berman S.R., Kupfer D.J. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- Carlén L., Sima L. SVT Nyheter (in Swedish); 2020. Nära hälften av alla planerade operationer inställda.https://www.svt.se/nyheter/inrikes/nara-halften-av-alla-planerade-operationer-installda Online: Retrieved 06-08-2022. [Google Scholar]
- Cénat J.M., Blais-Rochette C., Kokou-Kpolou C.K., Noorishad P.G., Mukunzi J.N., McIntee S.E., Labelle P.R.… Prevalence of symptoms of depression, anxiety, insomnia, posttraumatic stress disorder, and psychological distress among populations affected by the COVID-19 pandemic: a systematic review and meta-analysis. Psychiatry Res. 2021;295 doi: 10.1016/j.psychres.2020.113599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S., Williamson G. In: The Social Psychology of Health. Spacapan S., Oskamp S., editors. Sage Publications Inc; 1988. Perceived stress in a probability sample of the United States; pp. 31–67. [Google Scholar]
- Daly M., Sutin A.R., Robinson E. Longitudinal changes in mental health and the COVID-19 pandemic: evidence from the UK household longitudinal study. Psychol. Med. 2020;1–10 doi: 10.1017/S0033291720004432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deng J., Zhou F., Hou W., Silver Z., Wong C.Y., Chang O., Zuo Q.K.… The prevalence of depression, anxiety, and sleep disturbances in COVID-19 patients: a meta-analysis. Ann. N. Y. Acad. Sci. 2021;1486(1):90–111. doi: 10.1111/nyas.14506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drefahl S., Wallace M., Mussino E., Aradhya S., Kolk M., Brandén M., Andersson G.… A population-based cohort study of socio-demographic risk factors for COVID-19 deaths in Sweden. Nat. Commun. 2020;11(1):1–7. doi: 10.1038/s41467-020-18926-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ECDC COVID-19 situation update for the EU/EEA, as of 3 August 2022. 2022. https://www.ecdc.europa.eu/en/cases-2019-ncov-eueea Online: Retrieved: 06-08-2022.
- Folkhälsomyndigheten [Swedish Public Health Agency] Veckorapport om COVID-19, vecka 11. 2020. https://www.folkhalsomyndigheten.se/globalassets/statistik-uppfoljning/smittsamma-sjukdomar/veckorapporter-covid-19/2020/covid-19-veckorapport-vecka-11-2020.pdf Online: Retrievered: 01-08-2022.
- Folkhälsomyndigheten [Swedish Public Health Agency] Statistik för vaccination mot COVID-19. 2022. https://www.folkhalsomyndigheten.se/smittskydd-beredskap/utbrott/aktuella-utbrott/covid-19/statistik-och-analyser/statistik-over-registrerade-vaccinationer-covid-19/ Online: Retrieved: 06-08-2022.
- Frans Ö., Rimmö P.A., Åberg L., Fredrikson M. Trauma exposure and post-traumatic stress disorder in the general population. Acta Psychiatr. Scand. 2005;111(4) doi: 10.1111/j.1600-0447.2004.00463.x. 291-290. [DOI] [PubMed] [Google Scholar]
- Gustavsson J., Beckman L. Compliance to recommendations and mental health consequences among elderly in Sweden during the initial phase of the COVID-19 pandemic—a cross sectional online survey. Int. J. Environ. Res. Public Health. 2020;17(15):5380. doi: 10.3390/ijerph17155380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johansson R., Carlbring P., Heedman Å., Paxling B., Andersson G. Depression, anxiety and their comorbidity in the swedish general population: point prevalence and the effect on health-related quality of life. PeerJ. 2013;1 doi: 10.7717/peerj.98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karatzias T., Shevlin M., Murphy J., McBride O., Ben-Ezra M., Bentall R.P., Hyland P.… Posttraumatic stress symptoms and associated comorbidity during the COVID-19 pandemic in Ireland: a population-based study. J. Trauma. Stress. 2020;33(4):365–370. doi: 10.1002/jts.22565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B.W. The PHQ-9: validity of a brief depression severity measure. J. Gen. Intern. Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kruyen P.M., Emons W.H., Sijtsma K. On the shortcomings of shortened tests: a literature review. Int. J. Test. 2013;13(3):223–248. doi: 10.1080/15305058.2012.703734. [DOI] [Google Scholar]
- Little R.J.A., Rudin D. 2nd ed. Wiley; Hoboken, NJ: 2002. Statistical Analysis with Missing Data. [Google Scholar]
- Liu X., Zhu M., Zhang R., Zhang J., Zhang C., Liu P., Chen Z.… Public mental health problems during COVID-19 pandemic: a large-scale meta-analysis of the evidence. Transl. Psychiatry. 2021;11(1):1–10. doi: 10.1038/s41398-021-01501-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCracken L.M., Badinlou F., Buhrman M., Brocki K.C. Psychological impact of COVID- 19 in the swedish population: depression, anxiety, and insomnia and their associations to risk and vulnerability factors. Eur. Psychiatry. 2020;63(1):1–9. doi: 10.1192/j.eurpsy.2020.81. e81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munk-Jørgensen P., Allgulander C., Dahl A.A., Foldager L., Holm M., Rasmussen I., Wittchen H.U.… Prevalence of generalized anxiety disorder in general practice in Denmark, Finland, Norway, and Sweden. Psychiatr. Serv. 2006;57(12):1738–1744. doi: 10.1176/ps.2006.57.12.1738s. [DOI] [PubMed] [Google Scholar]
- Pieh C., Budimir S., Probst T. The effect of age, gender, income, work, and physical activity on mental health during coronavirus disease (COVID-19) lockdown in Austria. J. Psychosom. Res. 2020;136 doi: 10.1016/j.jpsychores.2020.110186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prins A., Bovin M.J., Smolenski D.J., Marx B.P., Kimerling R., Jenkins-Guarnieri M.A., Tiet Q.Q.… The primary care PTSD screen for DSM-5 (PC-PTSD-5): development and evaluation within a veteran primary care sample. J. Gen. Intern. Med. 2016;31(10):1206–1211. doi: 10.1007/s11606-016-3703-5. 0.1007/s11606-016-3703-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rae D. 2005. Getting Better Value for Money from Sweden's Healthcare System. OECD Economics Department Working Papers No. 443. [DOI] [Google Scholar]
- Rondung E., Leiler A., Meurling J., Bjärtå A. Symptoms of depression and anxiety during the early phase of the COVID-19 pandemic in Sweden. Front. Public Health. 2021;9:690. doi: 10.3389/fpubh.2021.562437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saevarsdóttir K.S., Hilmarsdóttir H.Ý., Magnúsdóttir I., Hauksdóttir A., Thordardottir E.B., Gudjónsdóttir Á.B., Valdimarsdóttir U.… Illness severity and risk of mental morbidities among patients recovering from COVID-19: a cross-sectional study in the icelandic population. BMJ Open. 2021;11(7) doi: 10.1136/bmjopen-2021-049967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sigdel A., Bista A., Bhattarai N., Poon B.C., Giri G., Marqusee H. MedRxiv; 2020. Depression, Anxiety and Depression-anxiety Comorbidity Amid COVID-19 Pandemic: An Online Survey Conducted During Lockdown in Nepal. [DOI] [Google Scholar]
- Skoog I. COVID-19 and mental health among older people in Sweden. Int. Psychogeriatr. 2020;32(10):1173–1175. doi: 10.1017/S104161022000143X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B.W., Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Intern. Med. 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Tull M.T., Edmonds K.A., Scamaldo K.M., Richmond J.R., Rose J.P., Gratz K.L. Psychological outcomes associated with stay-at-home orders and the perceived impact of COVID-19 on daily life. Psychiatry Res. 2020;289 doi: 10.1016/j.psychres.2020.113098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Unnarsdóttir A.B., Lovik A., Fawns-Ritchie C., Ask H., Kõiv K., Hagen K., Valdimarsdóttir U.A.… Cohort profile: COVIDMENT: COVID-19 cohorts on mental health across six nations. Int. J. Epidemiol. 2022;5(3):e108–e122. doi: 10.1093/ije/dyab234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiong J., Lipsitz O., Nasri F., Lui L.M., Gill H., Phan L., McIntyre R.S.… Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J. Affect. Disord. 2020 doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yogarajah A., Kenter R., Lamo Y., Kaldo V., Nordgreen T. Internet-delivered mental health treatment systems in Scandinavia–A usability evaluation. Internet Interv. 2020;20 doi: 10.1016/j.invent.2020.100314. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Flowchart of participants.