Abstract
This systematic review aims to take China as an example to determine the prevalence of mental health problems and associated influential factors of college students in different stages of the COVID-19 pandemic and provide a reference for effective intervention in the future. A systematic search was conducted on PubMed, Web of Science, Scopus, Science Direct, and Google scholar. A total of 30 articles were included. 1,477,923 Chinese college students were surveyed. In the early stage, the prevalence rates of depression, anxiety, stress, and PTSD ranged from 9.0% to 65.2%, 6.88%–41.1%, 8.53%–67.05%, and 2.7%–30.8%, respectively. Major risk factors were being a female, a medical student, isolation or quarantine, having family members or friends infected with COVID-19, and challenges of online learning. During the normalization stage, depression, anxiety, and insomnia prevalence rates ranged from 8.7% to 50.2%, 4.2%–34.6%, and 6.1%–35.0%, respectively. The main risk factors were self-quarantined after school reopening, regular taking temperature, and wearing face masks. The prevalence rates of mental health problems and associated influential factors unveiled in both stages showed that the students' mental health status was greatly affected. Therefore, a combination of efforts from the government, universities, and families or communities is highly needed to alleviate the mental health sufferings of students.
Keywords: Mental health, College students, Prevalence, Depression, Anxiety, Stress
1. Introduction
Since the global pandemic of the novel coronavirus (COVID-19) from 2020, it has been an ongoing crisis for two years (WHO, 2020). The pandemic has resulted in not only the risk of death but also psychological problems to people across the world (Cao et al., 2020). Recent studies have revealed that mental health problems such as fear, anxiety, depression, insomnia, post-traumatic stress disorder (PTSD) were prevalent among various populations such as the infected patients, psychiatric patients, children, pregnant women, healthcare workers, college students, and the general population during the pandemic (Fu et al., 2021a; Wang et al., 2020a; Sohrabi et al., 2020; Hao et al., 2020a, 2020b; Nguyen et al., 2022; Chew et al., 2020). As the first country reporting COVID-19 outbreak, 31 provinces and autonomous regions in China activated the level one public health emergency during the initial stage of the pandemic (January 2020) (Ma et al., 2020a). Strict epidemic control measures such as city lockdown, quarantine, suspension of social gatherings, closure of businesses and delayed starting schools were implemented (An update on the epidemiological, 2020; Meng et al., 2021a). China had achieved great success in controlling the epidemic at late April 2020. From May 2020, the newly confirmed cases per day kept at a low level with a clear downward trend nationwide. Since May 2020, the COVID-19 pandemic has been put under control in China. However, we can't ignore another aspect about COVID-19. Imported cases and local outbreak often occur here and there, regular prevention and control measures should be taken at the normalization period for a long time (Teng et al., 2021; Zhuo et al., 2021). It has been a continuing crisis, which might influence the uncertainties of the pandemic and bring pervasive impacts on individual's health (Teng et al., 2021; Zhuo et al., 2021).
Previous studies revealed that COVID-19 has led to persistent negative psychological effects on various populations. As a special group, college students' physical and mental development is not mature, and they are more vulnerable to have distress and mental health problems during the epidemic (Ren et al., 2021a). Previous studies also showed that college students have had higher prevalence of mental health problems during the different stages of COVID-19 epidemic. The prevalence of depressive symptoms is reported to range from 10.5 to 65.2% in the initial stage (Meng et al., 2021b; Jing et al., 2021a) and 8.7–50.2% (Wang et al., 2021a; Zheng et al., 2021) in the normalization stage in China. As the epidemic evolves, the mental health of college students may also change. In order to take timely and effective intervention measures accordingly, studies are needed to track the dynamic changes of the college students’ mental health status over time and find out the main mental health problems and related influential factors at different stages of the pandemic. This systematic review aims to take China as an example to determine the prevalence and associated influential factors of mental health problems of college students in different stages of COVID-19 pandemic and provides reference for effective intervention in the future.
2. Methods
2.1. Search process
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) was employed to select studies assessing the mental health problems including prevalence and associated influential factors among college students during the COVID-19 pandemic. A comprehensive literature search on original articles in electronic databases of PubMed, Web of Science, Scopus, Science Direct was conducted from inception until November 2021. An additional search on Google scholar was also included. Our search strategy was: ((mental health OR psychological health OR psychological distress OR depression OR anxiety OR PTSD OR psychological stress) AND (risk factors OR influencing factors) AND (university students OR college students OR higher education students) AND (novel coronavirus disease OR 2019 novel coronavirus OR COVID-19 OR 2019-nCOV)) on PubMed. ((TS=(mental health OR psychological health OR psychological distress OR depression OR anxiety OR PTSD OR psychological stress)) AND TS=(risk factors OR influencing factors)) AND TS=(university students OR college students OR higher education students)) AND TS=(novel coronavirus disease OR 2019 novel coronavirus OR COVID-19 OR 2019-nCOV)) on Web of Science. ((mental health OR psychological health) AND (university students OR college students) AND (risk factors OR influencing factors) AND (novel coronavirus OR COVID-19)) on Science Direct., and ((mental health∗ AND university students∗ AND risk factors∗ AND COVID-19∗)) on Scopus. A time span from January 2020 to November 2021 for published articles was considered. The search was conducted by two independent researchers. Each article underwent three rounds of the screening process. In the first round, titles were screened, and the abstracts of relevant articles were further assessed in the second round. In the third round, selected articles were screened for full-text to examine their eligibility.
2.2. Study selection and eligibility criteria
The titles and abstracts of each article were screened for significance. After the first screening process, the full-text articles were assessed for eligibility. Studies were included if they: (i) used cross-sectional study design (ii) assessed the mental health status of the university students during the COVID-19 pandemic including prevalence and risk factors (iii) used scales for measurement of mental health problems (iv) conducted in China. Studies were excluded if they were: (i) reviews (ii) no abstract or incomplete information (iii) inaccessibility of full-text (iv) duplicate.
2.3. Data extraction process
Two independent researchers (I.C and K.S.D) conducted the data extraction and assessment of methodological quality. Periodical meetings were held to minimize the risk of errors at each step of the review process. In the case of any discrepancy, they were asked to reach a consensus. A data extraction form was used for included articles and covered the following areas: (i) first author and publication year (ii) survey time (iii) survey region (iv) study design (v) sample size (vi) sample characteristics (vii) prevalence of depression/anxiety/PTSD/psychological stress or other mental health problems (viii) associated risk and protective factors.
2.4. Study quality appraisal
The Newcastle-Ottawa Scale (NOS) commonly used for cross-sectional studies was used for study quality appraisal. The scale is divided into three sections: Selection, Comparability, and Outcome. Overall, seven categories were included (assessment of sample representativeness, justification of sample size, comparison of respondents versus non-respondents, ascertainment of exposure, comparison according to study design or analysis, outcome assessment, and appropriateness of statistical analysis. A study that meets all of the criteria can be given a total score of ten stars. Selection gets a maximum of five stars, comparability gets two stars, and outcome gets three stars. A total of 9–10 stars (very good), 7–8 stars (good), 5–6 stars (satisfactory), and 0–4 stars (unsatisfactory) (Modesti et al., 2016).
3. Results
3.1. Characteristics of the included studies
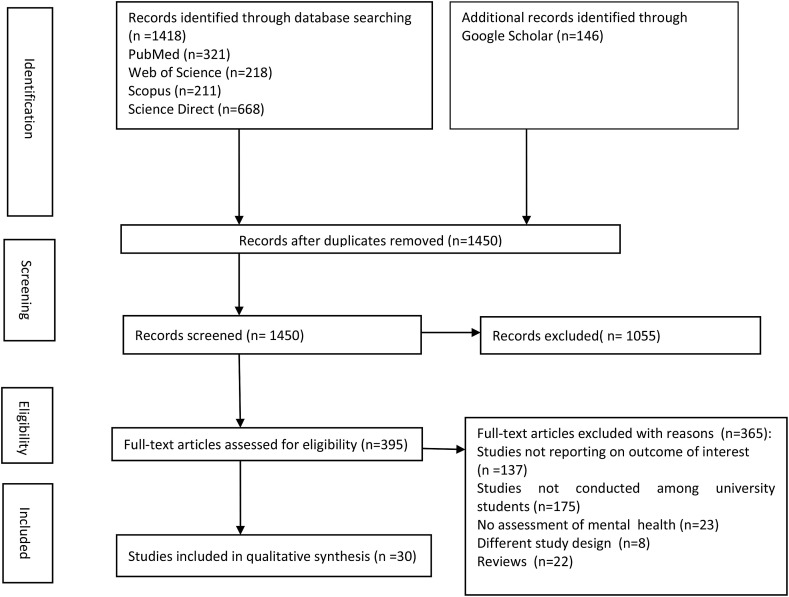
One thousand five hundred and sixty-four articles were identified through the database check. After screening for duplication and eligibility, 30 studies met the inclusion criteria and were included. A detailed workflow chart showing the study selection is presented in Fig. 1 and the characteristics of the included studies are displayed in Table 1 . In total, twenty-four and six studies assessed the prevalence of mental health problems and their influential factors of college students in China during the early and normalization stage of COVID-19 pandemic respectively. The earliest survey time was January 31, 2020, and the latest survey time was December 19, 2020. All the included studies employed an online cross-sectional survey. The surveyed regions came from various part of China, such as Guangzhou, Wuhan, Chengdu or other cities across China (see details in Table 1). A total of 1,477,923 participants were surveyed in the 30 studies. The sample size varied greatly, from 478 to 746,217 participants. Except for 4 studies, the included studies surveyed more female students than male students.
Fig. 1.
PRISMA flow chart showing the search strategy and selection of included studies.
Table 1.
Characteristics of the included studies.
| Early stage (January–May 2020) | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| First author and year of publication | Survey time | Region | Sample size | Sample characteristics | Measurement tool (s) | Prevalence (%) of mental health problems |
Related risk factors | Protective factors | NOS quality | |||||
| Anxiety | Depression | Stress | PTSD | Insomnia | Other | |||||||||
| Chi et al., 2020b | Feb12 to Feb 17, 2020 | China | 2500 | M ± SD: 20.6 ± 1.90 Sex (f/m): 1283/755 |
Z-SAS, PHQ-9, PCL, PTGI |
15.5 | 23.3 | – | 30.8 | – | PTG = 66.9% |
Anxiety, Depression, and PTSD: older age, knowing people who had been isolated, more ACEs, higher level of anxious attachment and avoidant attachment, and lower level of resilience PTG: higher subjective SES, knowing people who had been isolated, and the number of confirmed cases in participants' areas, fewer ACEs, lower level of avoidant attachment, and higher level of resilience |
– | Satisfactory |
| Fu et al., 2020 | May 10 to Jun 10, 2020. | Haikou | 89,588 | Sex (f/m): 50,394/39,194 Age group: 18–30 years |
GAD-7 | 41.1 | – | – | – | – | – |
Anxiety: female, age (26–30 years), being a sophomore, junior, and senior student, higher paternal education level, low economic status, and low social support. |
Good | |
| Guan et al., 2021 | Feb4 to Feb 12, 2020 |
Henan | 24,678 | M ± SD: 20.51 ± 1.28 Sex(f/m): 11,048/13,630 |
GAD-7 | 7.3 | – | – | – | – | – |
Anxiety: Sex, place of residence, high worried and fear level, low cognitive level, and behavior status. |
Anxiety: positive preventing behaviors | Satisfactory |
| Jia et al., 2021 | Feb 2020 | China | 740 | Sex (f/m): 458/282 |
SAS | 18.78 | – | – | – | – | – | Anxiety: female | Anxiety: knowledge and attitude regarding COVID-19 | Satisfactory |
| Jing et al., 2021 | Feb20 to Feb 22, 2020 |
China | 17,876 | M ± SD: 54.8 ± 9.0 Sex(f/m): 12,818/5058 |
SDS | – | 65.2 | – | – | – | – | Depression: female, moderate or high self-perceived risk of infection, moderately or highly impacted by the outbreak, and eager to go back to school |
Depression:personality type, educational level, moderate or high concern about the outbreak, moderate or high satisfaction with pandemic prevention and control measures, and health literacy on communicable diseases |
Satisfactory |
| Li (Xueguo) et al., 2020 | Feb13 to Feb 22, 2020. |
Guangdong | 304,167 | Age range: 18–26 years Sex(f/m): 182065/122102 |
IES-6 | - | – | 50.9 | – | – | – |
Stress: perceptions of COVID-19, self-perceived mental health and sleep quality |
– | Good |
| Li (Mengyao) et al., 2020 | Mar 3 to Mar 15, 2020. |
China | 1676 | M ± SD: 20.17 ± 1.497 Sex(f/m): 1088/588 |
HAI | 24.3 | – | – | – | – | Panic = 17.2% |
Anxiety: perceived lethality, being affected by the global spread, and impact on social contacts |
Anxiety: Knowledge of prognosis, preventive measures, wearing masks, and trust in mainstream media Panic: understanding the risk of COVID-19 and felt Less affected. |
Satisfactory |
| Li (Xueyan) et al., 2021 | Apr26 to Apr 29, 2020. | Wuhan | 4355 | Sex (f/m): 2146/2209 |
PTSD (IES-6) | – | – | – | 16.3 | – | – | PTSD: family members suspected with COVID-19, lost a loved one due to COVID-19, and family income decreased, online course difficulties and the difficulties in adapting oneself to the online courses, excessive collection of personal information, estrangement of family relatives, and harassment and insult from strangers. | – | Satisfactory |
| Ma et al., 2020 | Feb3 to Feb 10, 2020. | Guangdong, Jiangxi Province, and Wuhan city | 746, 217 | Age range: 18–26 years Sex (f/m): 414,604/331,613 |
IES-6, PHQ-9, GAD-7 | 11.0 | 21.1 | 34.9 | – | – | – |
Anxiety: Senior students and those who smoked Anxiety and depression:confirmed or suspected cases in one's community or village, low perceived social support, and prior mental health problems Stress: >3 h exposure to media coverage of the COVID-19 each day |
– | Good |
| Meng et al., 2021 | Feb14 to Feb 21, 2020. |
All over China | 3351 | M ± SD: 21.18 ± 2.66 Sex (f/m): 2002/130 |
GAD-7, PHQ-9 |
6.88 | 10.50 | – | – | – | – |
Anxiety: COVID-19- related factors, such as a history of close contact with people under quarantine, fever or cough, and mask usage,need ways to regulate emotions, professional and psychological hotline, and psychiatric visits provided by schools Depression: Married, undergraduate and postgraduate, non-medical, and urban students, COVID-19-related factors, such as a fever or cough, and hours spent browsing COVID-19-related information, needed ways to regulate their emotions, used professional and psychological hotlines, and had psychiatric visits provided by schools |
Anxiety: need online curricula or books, information on prevention and self-protection, and real-time epidemic data of the school Depression: needed prevention and self-protection information provided by schools. |
Satisfactory |
| Song et al., 2021 | Feb 17 to Feb 23, 2020. |
Anhui | 1128 | Age range: 18–27 years Sex(f/m): 632/496 |
SAS,SDS, CPSS |
8.4 | 22.7 | 42.9 | – | – | – |
Depression and stress: Parents' annual income, education level, and sex. Anxiety, depression, and stress:family conflicts and specialty. |
– | Satisfactory |
| Sun et al., 2021a | Mar20 to Apr 10, 2020 | Various regions of China | 1912 | M ± SD: 20.28 ± 2.10 Sex (f/m); 1334/578 |
GAD-7, PHQ-9; IES-6 |
34.73 | 46.55 | 67.05 | – | – | – |
Anxiety: higher level of COVID-19 prosocial behavior, perceived threat and stigma due to COVID-19, and financial stress due to COVID-19. Depression: financial stress due to COVID-19, perceived threat and societal stigma due to COVID-19, and screen media device usage. Stress: financial stress due to COVID-9, and Perceived threat and societal stigma due to COVID-19. |
Anxiety and depression: mindfulness and social support | Satisfactory |
| Tang et al., 2020 | Feb20 to Feb 27, 2020. |
Chengdu and Chongqing | 2485 | Age range: 16–27 years Sex (f/m): 1525/960 M ± SD: 19.81 ± 1.55 |
PCL, PHQ-9 | – | 9.0 | – | 2.7 | – | – | Depression and PTSD: feeling extreme fear, short sleep duration, living in the worst-hit areas, and being a graduating/final year student. | – | Good |
| Wang (Xing) et al., 2020 | Feb21 to Mar 7, 2020 |
China | 3092 | Sex (f/m): 2054/1038 |
GAD-7, PSS-10, SRSS |
16.8 | – | 43.7 | – | – | Sleep problems = 13.5% |
Anxiety: reading daily news, having sleep problems, and high perceived stress Stress: anxiety symptoms and sleep problems. Sleep problems: Postgraduates, frequency of going out per week (1–3 times), and higher perceived stress. |
Anxiety: carelessness with the number of remaining masks Sleep problems: frequency of daily news reading (1–3 times). Stress: higher frequency of daily news reading (4–7 times) and number of remaining masks (more than 20). |
Satisfactory |
| Wang (Zheng-He) et al., 2020 | Jan 31 to Feb 5, 2020. |
Guangzhou | 44,447 | Age group: 16–50 years M ± SD: 21.0 ± 2.4 Sex (f/m): 24,230/20,217 |
Z-SAS, CES-D |
7.7 | 12.2 | – | – | – | – |
Depression: lived in province where cumulative number of confirmed cases range from 1000 to 9999, have family members and relatives confirmed and suspected with COVID-19 Anxiety and depression: cumulative number of confirmed cases in the provinces; having infected family members and relatives or not, self-reported health condition, and education level. |
Anxiety and depression: postgraduate | Satisfactory |
| Wu et al., 2021 | Feb 4 to Feb 12, 2020 | China | 11,787 | M ± SD: 20.45 ± 1.76 Sex (f/m): 6731/5056 |
GAD-7, PHQ-9 |
17.8 | 25.9 | – | – | – | – | Anxiety and depression: history of residence in or travel to Wuhan in the past month, residing in Wuhan city, college location in Wuhan, and living in areas with a median number (200–600, >1000) of confirmed COVID-19 cases | – | Good |
| Xiang et al., 2020 | Feb 25 to Mar 5, 2020. |
China | 1396 | M ± SD: 20.68 ± 1.84 Sex(f/m): 515/881 |
SAS, SDS | 31.0 | 41.8 | – | – | – | – |
Anxiety: lived in an only child family Depression: female and undergraduate. |
Anxiety: high level of physical activity (stretching and resistance training), Depression: moderate or high level of physical activity, (household chores and stretching) |
Satisfactory |
| Xiong et al., 2021 | Feb 20 to Mar 20, 2020 |
Guangdong | 563 | M±SD: 21.52 ± 2.50. Sex(f/m): 391/172 |
DASS-21 | Moderate to severe = 18.47 | Moderate to severe = 12.26 | Moderate to severe 8.53 | – | – | – |
Anxiety: mindful coping. Anxiety and depression: negative emotions, prevention of mindful coping Anxiety and stress: awareness and negative emotions prevention of mindful coping. |
– | Satisfactory |
| Yang et al., 2021 | Apr to May 2020 | Sichuan | 521 | M ± SD: 22.02 ± 1.761 Sex(f/m): 404/117 |
SAS | Mild = 31.5 Moderate = 8.1 Severe = 5.8 |
– | – | – | – | Distress = 19.0% |
Anxiety: medical student, paying attention to pandemic information (frequency of >10 times a day) Distress: medical student and general health status |
Distress: age (above 22 years) |
Satisfactory |
| Yu (Chang) et al., 2021 | Feb 15 to Feb 22, 2020. |
China | 1086 | Sex(f/m): 737/349 Age range: 18–60 years |
AIS, SRQ-20, CPSS | - | – | 40.70 | 16.67 | General psychological symptoms = 5.8% |
Insomnia: female, general psychological symptoms and living in an isolation unit. |
– | Satisfactory | |
| Yu (Mingli) et al., 2021 | Mar 3 to Mar 15, 2020 |
Various regions of China | 1681 | Sex (f/m): 1089/592 |
CES-D | – | 56.8 | – | – | – | – | Depression: sleep problems, family members' going out, perceived more stress for online education, fear of COVID-19, influence on social interaction and higher grades. |
Depression: Perceived social support, hope, female, and higher monthly disposable income. |
Satisfactory |
| Yu (Yanqiu) et al., 2021 | Feb1 to Feb 10, 2020. |
China | 23,863 | Sex (f/m): 16,258/7605 |
PHQ-9 | – | 39.1 | – | – | – | Mental distress: 47.1% |
Depression: mental distress due to COVID-19, number of confirmed cases (>300 cases) detected in the province Depression and mental distress: perceived infection risk, having close contacts with people who had visited Wuhan 2 weeks prior to the CNY, perceived discrimination due to COVID-19. |
Depression: staying in the city of the university, staying with family, and self-perceived physical health, | Satisfactory |
| Zhang (Xudong) et al., 2021 | Feb21 to Feb 24, 2020, |
China | 2270 | Age range: 18–25 years Sex (f/m): 1393/877 |
SAS, SDS | 8.2 | 21.0 | – | – | – | – |
Anxiety and depression: contact history of similar infectious disease, past medical history, and compulsive behaviors |
Anxiety and depression: Older students, regular daily life during the epidemic outbreak, exercise during the epidemic outbreak, and concerns related to COVID-19 | Satisfactory |
|
Zhou et al., 2020 |
Mar 1 to Mar 15, 2020, |
China |
11133 |
Age range: 18–35years Median = 21 Sex(f/m): 6938/4195 |
PHQ-9, GAD-7 |
24.9 |
37.0 |
– |
– |
– |
Suicidal ideation = 7.3% |
Anxiety and depression: female, graduate students, and those with COVID-19 exposure Suicidal ideation: anxiety and depressive symptoms |
Anxiety and depression: living with Parents, being familiar with COVID-19, actively taking preventive and control measures, and being optimistic about projections of COVID-19 |
Good |
| Normalization stage (June 2020∼current) | ||||||||||||||
|
First author and year of publication |
Time period |
Region |
Sample size |
Sample characteristics |
Measurement tool (s) |
Prevalence (%) of mental health problems |
Related risk factors |
Protective factors |
NOS quality |
|||||
|
Anxiety |
Depression |
Stress |
PTSD |
Insomnia |
Other |
|||||||||
| Ren et al., 2021 | Sept 14 to Sept 20,2020 | Shandong | 478 | Sex(f/m): 273/205 |
SAS, PHQ-9 | 15.5 | 32.4 | – | – | – | – |
Anxiety: taking temperature routinely, retaining holiday, taking the final examination after school reopening, lockdown restriction, exercise frequency, quarantine of classmates, take-out availability, alcohol use, availability of package delivery, school reopening, self-quarantine after school reopening, and the degree to which family economic status is influenced by COVID-19) Depression: routinely wearing masks, having relatives or friends who have been infected, satisfaction with living conditions in the school, several areas in school being closed due to COVID-19, self-rated sleep quality, lockdown restriction, exercise frequency, quarantine of classmates, alcohol use, self-quarantine after school reopening, and the degree to which family economic status is influenced by COVID-19) |
– | Satisfactory |
| Wang (Dongfang) et al., 2021 | Jun 1 to Jun 15, 2020 |
Guangdong | 8921 | Age range: 16–25 years M ± SD: 21.59 ± 1.81 Sex (f/m): 5857/3064 |
PHQ-9, GAD-7, IES-6, YSIS | 4.2 | 8.7 | 10.5 | – | 6.1 | – |
Stress: male gender, living in rural areas, or living with siblings. Anxiety, depression, and insomnia: history of psychiatric conditions Poor mental health: Sophomore, history of psychiatric conditions, and impacted academic activities and social communication |
Good | |
| Xu et al., 2021 | Jun 29 to Jul 18, 2020 |
Wuhan | 11,254 | Sex (f/m): 7200/4054 Age range: 15–20 years |
PHQ-9, GAD-7, ISI, PCL-5, | 32.6 | 41.5 | – | 8.5 | 35.0 | Suicidal behavior: 2.0% |
Mental health problems: positive family history of psychosis, and prior history of mental illness, distant relationship with parents, and changes in lifestyle and alcohol use Suicidal behavior: female, high stress, changes in lifestyle and alcohol use, and high stress |
Mental health problems: regular physical exercise, | Good |
| Yu (Jincong) et al., 2021 | Jul to Aug 2020 |
Wuhan | 9383 | Sex(f/m): 6698/2685 |
PHQ-9 | – | 15.8 | – | – | – | – |
Anxiety: academic stress and concerns about the epidemic Depression: experience of being quarantined for observation or treatment, family members or friends dying of COVID-19, rarely or never seeking help from others, fewer supportive relatives or friends, less support from family in the past month, a worse relationship with parents at home, a longer time spent daily on electronic devices except for online learning, and feeling anxious in the face of returning to school. |
– | Good |
| Zhang (Yifan) et al., 2021 | Jun1 to Jun 15, 2020 |
Guangdong | 146,102 | Age range: 16–25 years Sex(f/m): 90,701/55,401 |
YSIS | – | – | – | – | 16.9 | – |
Insomnia: female, living in urban area, having a history of physical illness, or suffering depressive and anxiety symptoms. |
Insomnia: College senior degree and 7–8 h' sleep duration per day | Good |
| Zheng et al., 2021 | Dec17 to Dec 19, 2020. |
Shandong | 954 | M ± SD: 21.1 ± 1.2 Age range = 18–28 years Sex(f/m): 588/366 |
PHQ-9, GAD-7, ISI. | 34.6 | 50.2 | – | 25.3 | – |
Anxiety: age Depression: age and living in rural areas Anxiety and depression: female and native of non-Shandong |
– | Satisfactory | |
Age was expressed as M ± SD: Mean age ± Standard deviation or range. Sex as (f/m): female/male. CS: Cross-sectional study.
PHQ-9: Patient Health Questionnaire −9, GAD-7: Generalized Anxiety Disorder-7, SDS: Self-Rating Depression Scale, SAS: Self-Rating Anxiety Scale, CES-D: Center for Epidemiologic Studies Depression Scale, Z-SAS: Zung's Self-rating Anxiety Scale, HAI: Health Anxiety Inventory subscale, CPSS:Chinese perceived stress scale, PSS-10: Perceived Stress Scale, DASS-21: Depression, Anxiety, and Stress Scale, IES-6: Impact of Event Scale 6-Item, YSIS:Youth Self-Rating Insomnia Scale, ISI: Insomnia Severity Index, AIS: Athens Insomnia Scale. PTSD: Post Traumatic Stress Disorder, PCL: PTSD Checklist, PCL-5: Post-traumatic Stress Disorder Checklist for DSM-5, PTGI: post-traumatic Growth Inventory, and SRQ-20: Self-Reporting Questionnaire-20. SRSS: Self-Rating Scale of Sleep.
3.2. Quality appraisal of included studies
Table 2 displayed the result of the quality appraisal using NOS. The overall quality of the selected studies was moderate with total stars ranging from five to seven. There were nine studies with five stars, eleven with six stars, and ten studies with seven stars.
Table 2.
Quality appraisal of the included studies using Newcastle Ottawa Scale (NOS).
| Study | Selection |
Comparability |
Outcome |
Total score | Quality | ||||
|---|---|---|---|---|---|---|---|---|---|
| Representativeness of the sample | Sample size | Non - respondents | Ascertainment of exposure | Based on design and analysis | Assessment of outcome | Statistical test | |||
| Chi et al., 2020b | ∗ | ∗ | ∗∗ | ∗ | ∗ | 6 | Satisfactory | ||
| Fu et al., 2020 | ∗ | ∗ | ∗∗ | ∗ | ∗ | ∗ | 7 | Good | |
| Guan et al., 2021 | ∗ | ∗∗ | ∗ | ∗ | ∗ | 6 | Satisfactory | ||
| Jia et al., 2021 | ∗ | ∗∗ | ∗ | ∗ | ∗ | 6 | Satisfactory | ||
| Jing et al., 2021 | ∗ | ∗∗ | ∗ | ∗ | ∗ | 6 | Satisfactory | ||
| Li (Xueguo) et al., 2020 | ∗ | ∗ | ∗∗ | ∗ | ∗ | ∗ | 7 | Good | |
| Li (Mengyao) et al., 2020 | ∗∗ | ∗ | ∗ | ∗ | 5 | Satisfactory | |||
| Li (Xueyan) et al., 2021 | ∗ | ∗ | ∗∗ | ∗ | ∗ | 6 | Satisfactory | ||
| Ma et al., 2020 | ∗ | ∗ | ∗∗ | ∗ | ∗ | ∗ | 7 | Good | |
| Meng et al., 2021 | ∗∗ | ∗ | ∗ | ∗ | 5 | Satisfactory | |||
| Ren et al., 2021 | ∗ | ∗∗ | ∗ | ∗ | 5 | Satisfactory | |||
| Song et al., 2021 | ∗ | ∗∗ | ∗ | ∗ | 5 | Satisfactory | |||
| Sun et al., 2021a | ∗ | ∗∗ | ∗ | ∗ | 5 | Satisfactory | |||
| Tang et al., 2020 | ∗ | ∗ | ∗∗ | ∗ | ∗ | ∗ | 7 | Good | |
| Wang (Dongfang) et al., 2021 | ∗ | ∗ | ∗∗ | ∗ | ∗ | ∗ | 7 | Good | |
| Wang (Xing) et al., 2020 | ∗ | ∗∗ | ∗ | ∗ | 5 | Satisfactory | |||
| Wang (Zheng-He) et al., 2020 | ∗ | ∗∗ | ∗ | ∗ | ∗ | 6 | Satisfactory | ||
| Wu et al., 2021 | ∗ | ∗ | ∗∗ | ∗ | ∗ | ∗ | 7 | Good | |
| Xiang et al., 2020 | ∗ | ∗∗ | ∗ | ∗ | 5 | Satisfactory | |||
| Xiong et al., 2021 | ∗ | ∗∗ | ∗ | ∗ | 5 | Satisfactory | |||
| Xu et al., 2021 | ∗ | ∗ | ∗∗ | ∗ | ∗ | ∗ | 7 | Good | |
| Yang et al., 2021 | ∗ | ∗∗ | ∗ | ∗ | ∗ | 6 | Satisfactory | ||
| Yu (Chang) et al., 2021 | ∗ | ∗∗ | ∗ | ∗ | 5 | Satisfactory | |||
| Yu (Mingli) et al., 2021 | ∗ | ∗∗ | ∗ | ∗ | ∗ | 6 | Satisfactory | ||
| Yu (Jincong) et al., 2021 | ∗ | ∗ | ∗∗ | ∗ | ∗ | ∗ | 7 | Good | |
| Yu (Yanqiu) et al., 2021 | ∗ | ∗ | ∗∗ | ∗ | ∗ | 6 | Satisfactory | ||
| Zhang (Xudong) et al., 2021 | ∗ | ∗∗ | ∗ | ∗ | ∗ | 6 | Satisfactory | ||
| Zheng et al., 2021 | ∗ | ∗ | ∗∗ | ∗ | ∗ | 6 | Satisfactory | ||
| Zhou et al., 2020 | ∗ | ∗ | ∗∗ | ∗ | ∗ | ∗ | 7 | Good | |
| Zhang (Yifan) et al., 2021 | ∗ | ∗ | ∗∗ | ∗ | ∗ | ∗ | 7 | Good | |
3.3. Mental health problems and associated influential factors during different stages of COVID-19 pandemic
Depression, anxiety, stress, PTSD, and insomnia were major mental health problems reported among Chinese college students during different pandemic stages in the included studies. A few of these studies reported other mental health problems such as sleep problems, panic, mental distress, suicidal ideation, post-traumatic growth (PTG), and general psychological symptoms. Besides, relatively different protective factors were reported among the study subjects from a few studies (Table 1). The detailed prevalences and associated influential factors about mental health problems were outlined below:
3.4. Depression and associated influential factors
Fifteen studies conducted from January to April 2020 reported depression as a significant mental health problem among Chinese college students during the early stage of the COVID-19 pandemic (Chi et al., 2020a; Jing et al., 2021b; Ma et al., 2020b; Meng et al., 2021c; Song et al., 2021; Sun et al., 2021a; Tang et al., 2020; Wang et al., 2020b; Wu et al., 2021; Xiang et al., 2020a; Xiong et al., 2021a; Yu et al., 2021a, 2021b; Zhang et al., 2021a; Zhou et al., 2021). The reported prevalence of depressive symptoms among the 15 studies ranges from 9.0% to 65.2%. Eight of the studies used the PHQ-9 scale (Meng et al., 2021b; Sun et al., 2021a; Tang et al., 2020; Wu et al., 2021; Yu et al., 2021b; Zhou et al., 2021; Chi et al., 2020b; Ma et al., 2020c), four used SDS (Jing et al., 2021a; Song et al., 2021; Xiang et al., 2020a; Zhang et al., 2021a), two used CES-D (Wang et al., 2020b; Yu et al., 2021a), and one used the DASS-21 scale (Xiong et al., 2021a) to assess depressive symptoms. These studies' findings were relatively similar in that depression was reported as a significant mental health problem among the study participants. However, except for being a female in three studies (Jing et al., 2021a; Xiang et al., 2020a; Zhou et al., 2021) and undergraduate in two studies (Meng et al., 2021c; Xiang et al., 2020a) observed as risk factors for depression, there were differences in risk factors for depressive symptoms among the 15 studies. With regards to protective factors, nine studies (Meng et al., 2021b; Jing et al., 2021a; Sun et al., 2021a; Wang et al., 2020b; Xiang et al., 2020a; Yu et al., 2021a, 2021b; Zhang et al., 2021a; Zhou et al., 2021) identified protective factors for depression. Among these studies, two studies discovered that social support (Sun et al., 2021a; Yu et al., 2021a), living with family members (Yu et al., 2021b; Zhou et al., 2021), and physical activity (Xiang et al., 2020a; Zhang et al., 2021a) as protective factors for depression. The rest reported on varying protective factors for depression. During the normalization stage, five studies carried out between September to December 2020 rated depression as a primary mental health problem among Chinese college students (Wang et al., 2021a; Zheng et al., 2021; Ren et al., 2021b; Xu et al., 2021; Yu et al., 2021c). The prevalence of depressive symptoms among these studies ranges from 8.7% to 50.2%. PHQ-9 scale was the measurement tool used to assess depressive symptoms in the five studies. Nevertheless, these studies reported several different risk factors leading to the development of depression. A study by Xu et al. (2021) noticed frequent physical exercise as a protective factor for depression.
3.5. Anxiety and associated influential factors
A total of seventeen studies conducted from January to May 2020 reported anxiety as a fundamental mental health problem among Chinese college students during the early stage of the COVID-19 pandemic (Ma et al., 2020b; Meng et al., 2021c; Song et al., 2021; Sun et al., 2021a; Wang et al., 2020b, 2020c; Wu et al., 2021; Xiang et al., 2020a; Xiong et al., 2021a; Zhang et al., 2021a; Zhou et al., 2021; Chi et al., 2020b; Fu et al., 2021b; Guan et al., 2021a; Jia et al., 2021a; Li et al., 2020a; Yang et al., 2021a). The prevalence of anxiety symptoms reported by these studies ranges from 6.88% to 41.1%. Eight studies used GAD-7 scale (Meng et al., 2021b; Sun et al., 2021a; Wu et al., 2021; Zhou et al., 2021; Ma et al., 2020c; Fu et al., 2021b; Guan et al., 2021a; Wang et al., 2020c), five studies used SAS (Song et al., 2021; Xiang et al., 2020a; Zhang et al., 2021a; Jia et al., 2021a; Yang et al., 2021a), two used Z-SAS (Wang et al., 2020b; Chi et al., 2020b), and one used HAI (Li et al., 2020a) and DASS-21 (Xiong et al., 2021a) to measure anxiety symptoms among the students. Except for being a female student (Zhou et al., 2021; Fu et al., 2021b; Jia et al., 2021a) and a senior student (Ma et al., 2020b; Fu et al., 2021b) noticed as risk factors for anxiety in three studies and two studies respectively, different risk factors for anxiety symptoms were reported by the 17 studies. Among the 17 studies, 10 studies reported on protective factors for anxiety (Meng et al., 2021b; Sun et al., 2021a; Wang et al., 2020b, 2020c; Xiang et al., 2020a; Zhang et al., 2021a; Zhou et al., 2021; Guan et al., 2021a; Jia et al., 2021a; Li et al., 2020a). Varying protective factors for anxiety were disclosed by these studies. In the normalization stage, four studies assessed anxiety symptoms from September to December 2020 with a prevalence of 4.2%–34.6% (Wang et al., 2021a; Zheng et al., 2021; Ren et al., 2021b; Xu et al., 2021). Anxiety symptoms were measured by GAD-7 (n = 3) (Wang et al., 2021a; Zheng et al., 2021; Xu et al., 2021) and SAS (n = 1) (Ren et al., 2021b). The included studies also reported different risk factors for anxiety symptoms. Frequent physical exercise was revealed by Xu et al. (2021) as a protective factor for anxiety.
3.6. Stress and associated influential factors
During the early stage, seven studies assessed the symptoms of stress from February to April 2020 among Chinese college students (Ma et al., 2020b; Song et al., 2021; Sun et al., 2021a; Xiong et al., 2021a; Wang et al., 2020c; Li et al., 2020b; Yu et al., 2021d). The prevalence of stress ranges from 8.53% to 67.05%. Measurement tools such as IES-6 (n = 3) (Sun et al., 2021a; Ma et al., 2020c; Li et al., 2020c), CPSS (n = 2) (Song et al., 2021; Yu et al., 2021d), PSS-10 (n = 1) (Wang et al., 2020c), and DASS-21 (n = 1) (Xiong et al., 2021a) were used by the included studies to measure stress. The included studies discovered different risk factors for stress. Moreover, among the seven studies, only one study (Wang et al., 2020c) revealed higher frequency of daily news reading (4–7 times) and number of remaining masks (greater than 20) were protecive factors for stress. In the normalization stage, a study conducted in June 2020 reported stress as a significant mental health problem among the students (Wang et al., 2021a). The prevalence of stress was 10.5%. The risk factors for stress were being a male student and living with siblings or in rural areas.
3.7. PTSD and associated influential factors
An aggregate of three studies conducted between February to April 2020 investigated the symptoms of PTSD among students during the early stage (Tang et al., 2020; Chi et al., 2020b; Li et al., 2021a). According to these studies, the prevalence of PTSD symptoms ranges from 2.7% to 30.8%. Two studies used PCL (Tang et al., 2020; Chi et al., 2020b), and one study used IES-6 (Li et al., 2021a) to assess the symptoms of PTSD. The three studies' risk factors leading to the development of PTSD were relatively different. However, in the normalization stage, a survey in June 2020 reported PTSD as a vital mental health problem among the students (Xu et al., 2021). The prevalence of PTSD was 8.5%. The risk factors for PTSD were history of mental illness, positive history of family psychosis, changes in lifestyle, and distant relationship with parents. Also, protective for PTSD was frequent physical exercise.
3.8. Insomnia and associated influential factors
A survey conducted in February 2020 investigated insomnia as an essential mental health problem among Chinese college students during the early stage (Yu et al., 2021d). AIS was the tool used to measure insomnia. The prevalence of insomnia was 16.67%. The risk factors for insomnia included being a female student, living in an isolation unit, and general psychological symptoms. Amidst the normalization stage, four studies performed between June to December 2020 assessed insomnia among the study participants (Wang et al., 2021a; Zheng et al., 2021; Xu et al., 2021; Zhang et al., 2021b). As reported by these studies, the prevalence of insomnia ranges from 6.1% to 35.0%. Two studies used YSIS (Wang et al., 2021a; Zhang et al., 2021b) and ISI (Zheng et al., 2021; Xu et al., 2021) to assess insomnia. The four studies identified independent risk factors for insomnia. Frequent physical exercise (Xu et al., 2021), and college senior degree and 7–8 h’ sleep duration daily (Zhang et al., 2021b) served as protective factors for insomnia.
3.9. Other mental health problems and associated influential factors
Mental health problems such as post-traumatic growth (PTG = 66.9%) (Chi et al., 2020b), sleep problems (13.5%) (Wang et al., 2020c), panic (17.2%) (Li et al., 2020a), mental distress (47.1%) (Yu et al., 2021b), suicidal ideation (7.3%) (Zhou et al., 2021), and general psychological symptoms (5.8%) (Yu et al., 2021d) were also reported during the early stage. These mental health problems were investigated between February to March 2020. The risk factors for PTG were higher subjective SES and knowing people who had been isolated (Chi et al., 2020b). According to Wang et al. (2020c), the risk factors for sleep problems were high perceived stress and anxiety symptoms. Also, protective factor for sleep problems was frequency of daily news reading (1–3 times). With reference to Zhou et al. (2021), having anxiety and depressive symptoms were risk factors for suicidal ideation. Additionally, the risk factors for mental distress were perceived infection risk or discrimination and having close contact with people who had visited Wuhan 2 weeks before the Chinese New Year (Yu et al., 2021b). In the normalization, a study performed in June 2020, reported that suicidal behavior with a prevalence of 2.0% is another mental health problem that affected students during the COVID-19 pandemic (Xu et al., 2021).
4. Discussion
This systematic review assessed the mental health problems, including prevalence and influential factors among Chinese college students during different stages of the COVID-19 pandemic. Depression, anxiety, stress, PTSD, and insomnia were the most common mental health problems reported. Main risk factors include isolation or quarantine, being a female or medical student, fear about COVID-19 infection, having family members or friends suspected or confirmed with COVID-19, and challenges of online learning were reported in the early stage. In the normalization stage, the identified risk factors were self-quarantined after school reopened, wearing face masks, and increased stress level. In both stages, frequent physical exercise, availability of social support, and staying with family members were significant protective factors for mental health problems.
Overall, the prevalence rates of depression, anxiety, stress, PTSD, and insomnia ranged from 8.7% to 65.2%, 4.2%–41.1%, 10.5%–67.05%, 2.7%–30.8%, and 6.1%–35.0% respectively. The prevalence rates of mental health disorders reported in this review were higher than the prevalence rates reported before the pandemic (Huang et al., 2019; de Paula et al., 2020; Dang et al., 2004; Yueqin et al., 2003; Li et al., 2011). Nonetheless, these prevalence rates were higher than a multinational study that investigated the mental health status of participants who lived in seven middle income countries (MICs) in Asia (China, Iran, Malaysia, Pakistan, Philippines, Thailand, and Vietnam) during the pandemic (Wang et al., 2021b). In comparison with college students in other countries, these prevalence rates were higher than studies conducted in Bangladesh (Islam et al., 2020; Khan et al., 2020) and Pakistan (Salman et al., 2020; Asif and Sattar, 2020). The prevalence rates reported in this study were lowered than the prevalence rates reported in a systematic review that investigated the mental disorders of Bangladeshi students during the COVID-19 pandemic and noted depression (46.92%–82.4%), anxiety (26.6%–96.82%), and stress (28.5%–70.1%) (Al Mamun et al., 2021).
During the early stage (January–May 2020) of the pandemic in China, the prevalence rates of depression, anxiety, stress, and PTSD ranged from 9.0% to 65.2%, 6.88%–41.1%, 8.53%–67.05%, and 2.7%–30.8% respectively. Whereas only one study investigated the prevalence of insomnia (16.67%) during this stage. In the normalization stage (June – current time) of the pandemic, the prevalence rates of depression, anxiety, and insomnia ranged from 8.7% to 50.2%, 4.2%–34.6%, 6.1%–35.0% respectively. While the prevalence rates of stress (10.5%) and PTSD (8.5%) were reported. The prevalence rates variations in this study could be attributed to different sample size, measurement tools and cut-off values, time periods and regions, and reporting styles utilized as demonstrated in Table 1. However, higher prevalence rates of mental health problems were reported in the early stage as opposed to the normalization stage. An essential reason could be the extensive implementation of prevention and control measures such as isolation, quarantine, lockdown, shutdown of educational institutions and businesses, closure of offices and public areas (clubs, restaurants, and shopping places etc), massive testing, and restriction of social movement and interaction across regions in China during the early stage. Moreover, students were locked down and urged to take online classes to keep the learning process going. These measures were revealed to have made students more prone to develop mental health problems. Despite the epidemic was controlled in the normalization stage, students also suffered from mental health issues and this might be the global spread of the virus which resulted in a pandemic and stringent actions were also implemented by the Chinese government to prevent the escalation of new and imported cases.
During the pandemic, studies also revealed that students’ mental health was greatly affected by a number of factors ranging from epidemic measures, gender, student category, information received, family support, geographic location, and online learning in the early and normalization stage. These factors were found to be associated with symptoms of mental health problems. The outbreak struck at a time when most Chinese citizens including college students stopped their work or academic activities to enjoy the Chines New Year (CNY) which usually lasted for a month. Symptoms of mental health problems were expected to be lowered than previous periods but due to the occurrence of COVID-19 (early stage), epidemic-control measures were implemented across different regions in China and studies have found that such measures were significantly associated with higher risk of mental health problems. Students who were isolated at home for a long time faced a range of emotional stress responses (Fu et al., 2021a). Again, students having a history of quarantine were found to experience elevated levels of psychological distress and significantly at higher risk of anxiety and depression than those without (Meng et al., 2021d; Ren et al., 2021c). Prolong isolation can make people especially students to become bored and absorb excessive negative information, which also escalates possible risks of mental health disorders (Zhou et al., 2020; Gostic et al., 2020). Prolonged lockdown had caused diverse negative psychological impacts on people particularly students due to delays in school re-opening, postponement of examinations, and uncertainty about graduations (Wang et al., 2020d).
With regards to gender, female students demonstrated an increased risk of developing symptoms of mental health problems than their male counterparts (Fu et al., 2021a; Sun et al., 2021a; Wu et al., 2021; Zhou et al., 2020; Jia et al., 2021b; Li et al., 2020d).
Moreover, female gender is associated with depression in the world even before the pandemic (Lim et al., 2018). A possible explanation could be females are considered to be more frequently, emotionally, and relatively exposed to tension which in tend to increase the occurrence of symptoms of depression as opposed to males (Wu et al., 2021). Another reason could be that the stress reactions of females become extremely intense compared to males during epidemics. Physiologically, female hormones tend to swing and enhance very strong responses in the face of extremities than males. In addition, stress responses were also linked to the production of anxiety, tension, worry, or even emotions (Zhang et al., 2021c). Again, studies found that medical students were at greater risk of developing anxiety and depressive symptoms compared to non-medical students (Meng et al., 2021a; Yang et al., 2021b). This could be explained due to perhaps medical students had an improved knowledge and understanding of COVID-19 and were more abreast of protective and preventive measures compared to non-medical students (Zheng et al., 2021). Another possible reason could be medical students encountered excessive study pressure, limited social activities, and vulnerability to death and sufferings in caring for patients which made them susceptible to higher risks of depression and anxiety (Meng et al., 2021d).
Regarding regions, studies conducted in Guangdong, Hubei, and Shangdong province reported higher prevalence rates of mental health problems (Jing et al., 2021a; Zheng et al., 2021; Ma et al., 2020c; Ren et al., 2021b; Xu et al., 2021; Xiang et al., 2020b). Wuhan, the capital of Hubei province, known to identify the first case of COVID-19 and the worst-hit region in China, was completely lockdown, and use of face masks as well as social distancing were made mandatory in order to curb the spread of the virus. Similarly, Guangzhou, the capital of Guangdong province, was the second worst-hit region after Wuhan. It is the largest industrial and trade hub in China. To curtail the spread of the virus, lockdown and travel restrictions were also implemented and massive COVID-19 testing was carried out across the region following the detection of the second variant (Delta) of the new coronavirus (Guo et al., 2020). Shangdong being the second largest population in China set up an epidemic prevention and control task force groups and various cities also created a command system to respond to public health emergencies. The level one public health emergency was also implemented following the high incidence of COVID-19 and all educational institutions shutdown, businesses and social gatherings suspended to slow down the spread of the virus (Shi et al., 2021). The severity of the disease and wide implementation of epidemic prevention and control measures in these regions could have greatly impacted the mental health status of students. Furthermore, students who lived in provinces where the total number of infected cases span from 1000 to 9999 were 0.25 times at risk of anxiety and depressive symptoms in comparison with those living in provinces where the total number of infected cases span from 1 to 49 (Wang et al., 2020e). Additionally, students living in urban areas were at higher risk of anxiety or depressive symptoms contrary to those in rural areas (Meng et al., 2021d; Guan et al., 2021b). This situation happened due to the severe and robust actions to curb the spread and transmission of the virus in urban areas as opposed to rural areas (Alam et al., 2021).
As most students lived with their family members or relatives during the pandemic, studies have shown that there was an association between living with family members and mental health status. According to Wang et al. (2020b) and Li et al. (2021b) students whose family members were suspected, confirmed, or died of COVID-19 were significantly at risk of developing symptoms of PTSD and depression, and further developed extreme levels of panic and uncertainty. Also, students whose family members (or persons staying together with them) went outside for recreational activities during the quarantine period were reported to have severe symptoms of depression than those whose family members stayed at home (Meng et al., 2021d; Yu et al., 2021e). Consequently, these students might have been worried about their own health, family health status, spread of the virus to other members, and mortality rate, which in tend increased their risk of mental health disorders (Elsharkawy and Abdelaziz, 2021). Further, some studies have shown that economic instability might increase anxiety among university students, particularly during epidemic situations. College students having lower economic status were reported to be at greater risk of developing anxiety symptoms in contrast with those of higher economic status (Fu et al., 2021a). Similarly, low social support was also found to be a risk factor for developing depression and anxiety symptoms among students (Fu et al., 2021a; Ma et al., 2020a).
In February 2020, China Ministry of Education (MoE) postponed all educational activities and urged schools including higher educational institutions to use online medium as an alternative to face-to-face teaching in order to restore the normal teaching process and prevent the spread of the virus (China's education arrangements during COVID, 2020). The introduction of online learning was perceived by many students as a good idea but studies have revealed that students who participated in online learning were at risk of developing symptoms of mental health problems as opposed to students who did not participate (Yu et al., 2021a; Li et al., 2021a; Xiong et al., 2021b). A study by Albagmi et al. revealed that university students encountered the greatest level of anxiety in contrast to other professions, this was linked to the suspension of traditional (face-to-face) forms of learning and switched to online learning during the COVID-19 pandemic (Albagmi et al., 2021). Also, students were more prone to develop anxiety or depressive symptoms in the face of online learning due to the increased demand for new technological skills and use of electronic gadgets, efficiency, and excessive information and workload (Alibudbud, 2021).
Despite the mental health status of most students being greatly affected during the pandemic, a number of studies have outlined some protective factors against mental health issues. Knowledge about infectious diseases and moderate or high satisfaction with prevention and control measures (Jing et al., 2021a), use of face masks (Wang et al., 2020f), frequent physical exercise (Xu et al., 2021), positive about projections of COVID-19 trends and effectively adhering to COVID-19 preventive and control measures (Zhou et al., 2021), hope and availability of huge personal income (Yu et al., 2021f), mindfulness and perceived social support (Sun et al., 2021b), resilience (Chi et al., 2020a), extraordinary sense of control (Xiong et al., 2021b), and positive preventive behaviors and attitudes (Guan et al., 2021b), were among the protective factors of mental health problems.
The high prevalence rates and risk factors of mental health problems uncovered in this study depicted that the mental health of students was largely affected during the early and normalization stage, and therefore collective actions from different entities are needed to relieve the mental health sufferings of students. Firstly, students should be encouraged to adapt to healthy lifestyles like regular physical exercise and recreational activities. Regular physical exercise has been reported to lower mental health distress by improving sleep quality. Recreational activities can provide rest and relaxation resulting in a reduction in stress levels during pandemic (Sultana et al., 2021). Secondly, universities should provide psychosocial support and mental health services to students, particularly those who were at greater risk of developing mental health issues. Special consideration should be given to students who were infected with COVID-19, had family members or relatives infected, and lost loved ones during the pandemic (Ma et al., 2020a). The most evidence-based treatment is cognitive behaviour therapy (CBT), especially Internet CBT that can prevent the spread of infection during the pandemic (Ho et al., 2020a; Zhang et al., 2017; Soh et al., 2020). Online psychotherapy should be adopted by mental health providers (Wang et al., 2020d). Also, universities should organize health education and promotion programs. Greater attention should be given to females, junior and medical students in the health education and promotion programs (Jing et al., 2021c). Thirdly, governments should continue to strengthen public health education required for the circulation of information on preventive and control measures during the COVID-19 pandemic (Li et al., 2020e). Again, governments should continue to give out more prevention and control services to the student population to increase their knowledge and promote their levels of confidence and trust to help fight against the COVID-19 pandemic (Jing et al., 2021b). Finally, families and communities should provide adequate care and support to students to assist them in suppressing negative psychological problems of COVID-19 or any other emerging epidemic diseases (Psychiatry ResearchPsychiatry ResearchCao et al., 2020).
5. Strength
To the best of our knowledge, this is the first systematic review to assess and summarize previous studies that investigated the mental health status, including the prevalence and associated influential factors of mental health problems among Chinese college students amid the early and normalization stage of the COVID-19 pandemic.
6. Limitations
Studies were conducted at different stages and time periods of the pandemic resulting in variations in prevalence rates and risk factors affecting the mental health of students. All included studies used an online cross-sectional study design and therefore causal conclusions could not have been established. The collection of data via an online survey by the included studies may have created different objectives among respondents in the absence of a trained and qualified psychiatrist or researcher, and this might caused bias and inconsistencies in the professional assessment of psychiatric symptoms.
This study mainly used self-reported questionnaires to measure psychiatric symptoms and did not make clinical diagnosis. The gold standard for establishing psychiatric diagnosis involved structured clinical interview and functional neuroimaging should be applied in the future face-to-face research after COVID-19 restrictions are removed (Husain et al., 2020a, 2020b; Ho et al., 2020b). Another possible limitation is the larger number of female participants reported over males in most studies resulting in over-representation and selection bias. Most included studies may not be a good representative of the actual population due to over representation and selection bias.
7. Conclusion
This systematic review presents an overview of prevalence rates of symptoms of mental health disorders particularly depression, anxiety, stress, PTSD, and insomnia including associated influential factors that affected students amid the early and normalization stage of the pandemic. Higher prevalence rates of mental health disorders were reported in the early stage as compared to the normalization stage. In general, the prevalence rates of mental health problems were reported to be increased as opposed to before the pandemic. A combination of efforts from the government, universities, families or communities together with students is highly needed to alleviate the mental health sufferings during the pandemic or future outbreaks of any epidemic disease. Hence, future research is needed to assess the current mental health problems of students due to the fact that included studies were only conducted during the early and normalization stage of the pandemic.
Funding
This review received no external funding.
CRediT authors contribution statement
Ishmail Conteh: Conceptualization, Methodology, Investigation, Formal analysis, Validation, Data Curation, Writing-Original draft.
Junxia Yan: Conceptualization, Methodology, Investigation, Data Curation, Writing-Original draft.
Kodzovi Sylvain Dovi: Formal analysis, Validation, Investigation.
Ousman Bajinka: Supervision, Writing - Review & Editing.
Isaac Yaw Massey: Supervision, Writing - Review & Editing.
Bashiru Turay: Visualization, Writing - Review & Editing.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Not applicable.
References
- Al Mamun F., et al. vol. 14. 2021. p. 645. (Mental Disorders of Bangladeshi Students during the COVID-19 Pandemic: a Systematic Review). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alam M.K., et al. 2021. Assessing the Mental Health Condition of Home-Confined University Level Students of Bangladesh Due to the COVID-19 Pandemic; pp. 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albagmi F.M., AlNujaidi H.Y., Al Shawan D.S. vol. 14. 2021. p. 2161. (Anxiety Levels amid the COVID-19 Lockdown in Saudi Arabia). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alibudbud R. On online learning and mental health during the COVID-19 pandemic: perspectives from the Philippines. Asian journal of psychiatry. 2021;66:102867. doi: 10.1016/j.ajp.2021.102867. 102867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [An update on the epidemiological characteristics of novel coronavirus pneumonia (COVID-19)] Zhonghua Liuxingbingxue Zazhi. 2020;41(2):139–144. doi: 10.3760/cma.j.issn.0254-6450.2020.02.002. [DOI] [PubMed] [Google Scholar]
- Asif H.M., Sattar H.A. 2020. Impact of COVID-19 Pandemic on Mental Health of University Students in Pakistan. [Google Scholar]
- Cao W., et al. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatr. Res. 2020;287 doi: 10.1016/j.psychres.2020.112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chew N.W., et al. vol. 88. 2020. pp. 559–565. (A Multinational, Multicentre Study on the Psychological Outcomes and Associated Physical Symptoms Amongst Healthcare Workers during COVID-19 Outbreak). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chi X., et al. vol. 11. 2020. p. 803. (Prevalence and Psychosocial Correlates of Mental Health Outcomes Among Chinese College Students during the Coronavirus Disease (COVID-19) Pandemic). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chi X., et al. 2020. Prevalence and Psychosocial Correlates of Mental Health Outcomes Among Chinese College Students during the Coronavirus Disease (COVID-19) Pandemic; p. 803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- China's education arrangements during COVID-19 pandemic period. 2020. https://internationaleducation.gov.au/international-network/china/PolicyUpdates-China/Pages/China's-education-arrangements-during-COVID-19-pandemic-period.aspx Available from:
- Dang W.-m., et al. vol. 13. 2004. pp. 437–439. (Analysis of Anxiety and Depression Symptoms and Related Factors in Three Universities during SARS Epidemic in Beijing). [Google Scholar]
- de Paula W., et al. vol. 3. 2020. pp. 8739–8756. (Prevalence of Anxiety, Depression, and Suicidal Ideation Symptoms Among University Students: a Systematic Review). 4. [Google Scholar]
- Elsharkawy N.B., Abdelaziz E.M. vol. 57. 2021. pp. 1356–1364. (Levels of Fear and Uncertainty Regarding the Spread of Coronavirus Disease (COVID-19) Among University Students). 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fu W., et al. Mental health of college students during the COVID-19 epidemic in China. J. Affect. Disord. 2021;280(Pt A):7–10. doi: 10.1016/j.jad.2020.11.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fu W., et al. Mental health of college students during the COVID-19 epidemic in China. J. Affect. Disord. 2021;280:7–10. doi: 10.1016/j.jad.2020.11.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gostic K., et al. vol. 9. 2020. (Estimated Effectiveness of Symptom and Risk Screening to Prevent the Spread of COVID-19). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guan J., et al. vol. 18. 2021. p. 4974. (Prevalence and Factors for Anxiety during the COVID-19 Pandemic Among College Students in China). 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guan J., et al. Prevalence and factors for anxiety during the COVID-19 pandemic among college students in China. Int. J. Environ. Res. Publ. Health. 2021;18(9) doi: 10.3390/ijerph18094974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo X.-J., Zhang H., Zeng Y.-P. Transmissibility of COVID-19 in 11 major cities in China and its association with temperature and humidity in Beijing, Shanghai, Guangzhou, and Chengdu. Infectious Diseases of Poverty. 2020;9(1):87. doi: 10.1186/s40249-020-00708-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hao F., et al. Do psychiatric patients experience more psychiatric symptoms during COVID-19 pandemic and lockdown? A case-control study with service and research implications for immunopsychiatry. Brain Behav. Immun. 2020;87:100–106. doi: 10.1016/j.bbi.2020.04.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hao F., et al. vol. 10. 2020. pp. 1–14. (A Quantitative and Qualitative Study on the Neuropsychiatric Sequelae of Acutely Ill COVID-19 Inpatients in Isolation Facilities). 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho C.S., Chee C.Y., Ho R.C. vol. 49. 2020. pp. 1–3. (Mental Health Strategies to Combat the Psychological Impact of COVID-19 beyond Paranoia and Panic). 1. [PubMed] [Google Scholar]
- Ho C.S., et al. vol. 11. 2020. p. 378. (Diagnostic and Predictive Applications of Functional Near-Infrared Spectroscopy for Major Depressive Disorder: a Systematic Review). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang Y., et al. Prevalence of mental disorders in China: a cross-sectional epidemiological study. Lancet Psychiatr. 2019;6(3):211–224. doi: 10.1016/S2215-0366(18)30511-X. [DOI] [PubMed] [Google Scholar]
- Husain S.F., et al. vol. 10. 2020. pp. 1–9. (Validating a Functional Near-Infrared Spectroscopy Diagnostic Paradigm for Major Depressive Disorder). 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Husain S.F., et al. vol. 51. 2020. (Cortical Haemodynamic Response Measured by Functional Near Infrared Spectroscopy during a Verbal Fluency Task in Patients with Major Depression and Borderline Personality Disorder). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Islam M.A., et al. Depression and anxiety among university students during the COVID-19 pandemic in Bangladesh: a web-based cross-sectional survey. PLoS One. 2020;15(8) doi: 10.1371/journal.pone.0238162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jia Y., et al. vol. 11. 2021. (Knowledge–attitude–practice and Psychological Status of College Students during the Early Stage of COVID-19 Outbreak in China: A Cross-Sectional Study). 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jia Y.H., et al. Knowledge-attitude-practice and psychological status of college students during the early stage of COVID-19 outbreak in China: a cross-sectional study. BMJ Open. 2021;11(2) doi: 10.1136/bmjopen-2020-045034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jing Y., et al. vol. 12. 2021. p. 595. (Network-Based Online Survey Exploring Self-Reported Depression Among University and College Students during the Early Days of the COVID-19 Outbreak). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jing Y.R., et al. Network-based online survey exploring self-reported depression among university and college students during the early days of the COVID-19 outbreak. Front. Psychiatr. 2021;12 doi: 10.3389/fpsyt.2021.658388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jing Y., et al. Network-based online survey exploring self-reported depression among university and college students during the early days of the COVID-19 outbreak. Front. Psychiatr. 2021;12 doi: 10.3389/fpsyt.2021.658388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan A.H., et al. vol. 277. 2020. pp. 121–128. (The Impact of COVID-19 Pandemic on Mental Health & Wellbeing Among Home-Quarantined Bangladeshi Students: a Cross-Sectional Pilot Study). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li J., et al. vol. 38. 2011. pp. 3036–3042. (Investigation of Knowledge of Prevention and Control and Psychological Anxiety about H1N1 Influenza Among College Students in a University, Zhengzhou). [Google Scholar]
- Li M., et al. vol. 22. 2020. (Psychological Impact of Health Risk Communication and Social Media on College Students during the COVID-19 Pandemic: Cross-Sectional Study). 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li X., et al. 2020. COVID-19 in Guangdong: Immediate Perceptions and Psychological Impact on 304,167 College Students; p. 2024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li X., et al. COVID-19 in Guangdong: immediate perceptions and psychological impact on 304,167 college students. Front. Psychol. 2020:2024. doi: 10.3389/fpsyg.2020.02024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li X., et al. vol. 304. 2020. p. 11. (COVID-19 in Guangdong: Immediate Perceptions and Psychological Impact on). 167 college students. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li X.G., et al. COVID-19 in Guangdong: immediate perceptions and psychological impact on 304,167 college students. Front. Psychol. 2020;11 doi: 10.3389/fpsyg.2020.02024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li X., et al. vol. 18. 2021. p. 771. (COVID-19 Stress and Mental Health of Students in Locked-Down Colleges). 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li X.Y., et al. COVID-19 stress and mental health of students in locked-down colleges. Int. J. Environ. Res. Publ. Health. 2021;18(2) doi: 10.3390/ijerph18020771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim G., et al. Prevalence of depression in the community from 30 countries between 1994 and 2014. Sci. Rep. 2018;8(1):2861. doi: 10.1038/s41598-018-21243-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma Z., et al. vol. 29. Epidemiology and Psychiatric Sciences; 2020. (Mental Health Problems and Correlates Among 746 217 College Students during the Coronavirus Disease 2019 Outbreak in China). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma Z., et al. Mental health problems and correlates among 746 217 college students during the coronavirus disease 2019 outbreak in China. Epidemiol. Psychiatr. Sci. 2020;29:e181. doi: 10.1017/S2045796020000931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma Z., et al. vol. 29. Epidemiol Psychiatr Sci; 2020. (Mental Health Problems and Correlates Among 746 217 College Students during the Coronavirus Disease 2019 Outbreak in China). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meng N., et al. vol. 27. Medical Science Monitor; 2021. (Beyond Sociodemographic and COVID-19-Related Factors: the Association between the Need for Psychological and Information Support from School and Anxiety and Depression). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meng N., et al. Beyond sociodemographic and COVID-19-related factors: the association between the need for psychological and information support from school and anxiety and depression. Med. Sci. Mon. Int. Med. J. Exp. Clin. Res. 2021;27:e929280–e929281. doi: 10.12659/MSM.929280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meng N., et al. vol. 27. 2021. pp. e929280–e929281. (Beyond Sociodemographic and COVID-19-Related Factors: the Association between the Need for Psychological and Information Support from School and Anxiety and Depression). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meng N., et al. Beyond sociodemographic and COVID-19-related factors: the association between the need for psychological and information support from school and anxiety and depression. Med. Sci. Mon. Int. Med. J. Exp. Clin. Res. 2021;27 doi: 10.12659/MSM.929280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Modesti P.A., et al. vol. 11. 2016. (Panethnic Differences in Blood Pressure in Europe: a Systematic Review and Meta-Analysis). 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen L.H., et al. COVID-19 and delayed antenatal care impaired pregnant women's quality of life and psychological well-being: what supports should be provided? Evidence from Vietnam. J. Affect. Disord. 2022;298:119–125. doi: 10.1016/j.jad.2021.10.102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Psychiatry ResearchPsychiatry ResearchCao W., et al. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatr. Res. 2020;287 doi: 10.1016/j.psychres.2020.112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ren Z., et al. vol. 12. 2021. (Psychological Impact of COVID-19 on College Students after School Reopening: a Cross-Sectional Study Based on Machine Learning). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ren Z., et al. vol. 12. 2021. p. 1346. (Psychological Impact of COVID-19 on College Students after School Reopening: a Cross-Sectional Study Based on Machine Learning). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ren Z.Y., et al. Psychological impact of COVID-19 on college students after school reopening: a cross-sectional study based on machine learning. Front. Psychol. 2021;12 doi: 10.3389/fpsyg.2021.641806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salman M., et al. Psychological impact of COVID-19 on Pakistani university students and how they are coping. medRxiv. 2020 [Google Scholar]
- Shi J., et al. Spatio-temporal evolution and influencing mechanism of the COVID-19 epidemic in Shandong province, China. Sci. Rep. 2021;11(1):7811. doi: 10.1038/s41598-021-86188-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soh H.L., et al. vol. 75. 2020. pp. 315–325. (Efficacy of Digital Cognitive Behavioural Therapy for Insomnia: a Meta-Analysis of Randomised Controlled Trials). [DOI] [PubMed] [Google Scholar]
- Sohrabi C., et al. vol. 76. 2020. pp. 71–76. (World Health Organization Declares Global Emergency: A Review of the 2019 Novel Coronavirus (COVID-19)). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song H.-T., et al. 2021. Investigation on the Psychological Status of College Students during the Coronavirus Disease-2019 Epidemic; pp. 1–12. [DOI] [PubMed] [Google Scholar]
- Sultana M.S., et al. vol. 122. 2021. (Prevalence and Predictors of Post-traumatic Stress Symptoms and Depressive Symptoms Among Bangladeshi Students during COVID-19 Mandatory Home Confinement: A Nationwide Cross-Sectional Survey). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun S., et al. vol. 17. 2021. pp. 1–14. (Psychiatric Symptoms, Risk, and Protective Factors Among University Students in Quarantine during the COVID-19 Pandemic in China). 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun S., et al. Psychiatric symptoms, risk, and protective factors among university students in quarantine during the COVID-19 pandemic in China. Glob. Health. 2021;17(1):15. doi: 10.1186/s12992-021-00663-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang W., et al. vol. 274. 2020. pp. 1–7. (Prevalence and Correlates of PTSD and Depressive Symptoms One Month after the Outbreak of the COVID-19 Epidemic in a Sample of Home-Quarantined Chinese University Students). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teng Y.-M., Wu K.-S., Xu D.J. vol. 9. 2021. p. 557. (The Association between Fear of Coronavirus Disease 2019, Mental Health, and Turnover Intention Among Quarantine Hotel Employees in China). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Publ. Health. 2020;17(5):1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Z.-H., et al. Prevalence of anxiety and depression symptom, and the demands for psychological knowledge and interventions in college students during COVID-19 epidemic: a large cross-sectional study. J. Affect. Disord. 2020;275:188–193. doi: 10.1016/j.jad.2020.06.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang X., et al. 2020. Anxiety and Sleep Problems of College Students during the Outbreak of COVID-19; p. 1173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., et al. vol. 87. 2020. pp. 40–48. (A Longitudinal Study on the Mental Health of General Population during the COVID-19 Epidemic in China). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Z.H., et al. Prevalence of anxiety and depression symptom, and the demands for psychological knowledge and interventions in college students during COVID-19 epidemic: a large cross-sectional study. J. Affect. Disord. 2020;275:188–193. doi: 10.1016/j.jad.2020.06.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., et al. vol. 11. 2020. (The Association between Physical and Mental Health and Face Mask Use during the COVID-19 Pandemic: a Comparison of Two Countries with Different Views and Practices). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang D., et al. Is returning to school during the COVID-19 pandemic stressful? A study on immediate mental health status of Chinese college students. J. Affect. Disord. 2021;287:261–267. doi: 10.1016/j.jad.2021.03.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., et al. vol. 16. 2021. (The Impact of COVID-19 Pandemic on Physical and Mental Health of Asians: A Study of Seven Middle-Income Countries in Asia). 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO Coronvirus disease 2019. 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019 Available from:
- Wu X., et al. vol. 23. 2021. (Geographic Distribution of Mental Health Problems Among Chinese College Students during the COVID-19 Pandemic: Nationwide, Web-Based Survey Study). 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiang M.-Q., et al. 2020. Relationship of Physical Activity with Anxiety and Depression Symptoms in Chinese College Students during the COVID-19 Outbreak; p. 2860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiang M.-Q., et al. vol. 11. 2020. p. 2860. (Relationship of Physical Activity with Anxiety and Depression Symptoms in Chinese College Students during the COVID-19 Outbreak). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiong P., et al. vol. 9. 2021. p. 417. (Factors Influencing Mental Health Among Chinese Medical and Non-medical Students in the Early Stage of COVID-19 Pandemic). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiong P., et al. Factors influencing mental health among Chinese medical and non-medical students in the early stage of the COVID-19 pandemic. Front. Public Health. 2021;9 doi: 10.3389/fpubh.2021.603331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu Y., et al. vol. 12. 2021. (Prevalence and Risk Factors of Mental Health Symptoms and Suicidal Behavior Among University Students in Wuhan, China during the COVID-19 Pandemic). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang K.H., et al. Impact of coronavirus disease 2019 on the mental health of university students in Sichuan Province, China: an online cross-sectional study. Int. J. Ment. Health Nurs. 2021;30(4):875–884. doi: 10.1111/inm.12828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang K.H., et al. Impact of coronavirus disease 2019 on the mental health of university students in Sichuan Province, China: an online cross-sectional study. Int. J. Ment. Health Nurs. 2021;30(4):875–884. doi: 10.1111/inm.12828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu M., et al. vol. 21. 2021. pp. 1–8. (Prevalence and its Associated Factors of Depressive Symptoms Among Chinese College Students during the COVID-19 Pandemic). 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu Y., et al. vol. 8. 2021. (Factors Influencing Depression and Mental Distress Related to COVID-19 Among University Students in China: Online Cross-Sectional Mediation Study). 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu J., et al. Prevalence of and factors associated with depressive symptoms among college students in wuhan, China during the normalization stage of CoViD-19 prevention and control. Front. Psychiatr. 2021;12 doi: 10.3389/fpsyt.2021.742950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu C., et al. vol. 12. 2021. (Prevalence, Risk Factors, and Clinical Correlates of Insomnia in China College Student during the COVID-19). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu M.L., et al. Prevalence and its associated factors of depressive symptoms among Chinese college students during the COVID-19 pandemic. BMC Psychiatr. 2021;21(1) doi: 10.1186/s12888-021-03066-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu M., et al. Prevalence and its associated factors of depressive symptoms among Chinese college students during the COVID-19 pandemic. BMC Psychiatr. 2021;21(1):66. doi: 10.1186/s12888-021-03066-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yueqin H., Weimin D., Zhaorui L.J. 2003. Psychosocial Aspects in Three Universities during SARS Epidemic in Beijing. [Google Scholar]
- Zhang M.W., Ho R.J.T., Care H. vol. 25. 2017. pp. 163–165. (Moodle: the Cost Effective Solution for Internet Cognitive Behavioral Therapy (I-CBT) Interventions). 1. [DOI] [PubMed] [Google Scholar]
- Zhang X., et al. vol. 23. 2021. (Risk Factors of Psychological Responses of Chinese University Students during the COVID-19 Outbreak: Cross-Sectional Web-Based Survey Study). 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y., et al. vol. 304. 2021. (Insomnia and Other Sleep-Related Problems during the Remission Period of the COVID-19 Pandemic: a Large-Scale Survey Among College Students in China). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y., et al. vol. 125. 2021. (Psychological Stress of University Students in the Hardest-Hit Areas at Different Stages of the COVID-19 Epidemic). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng X., et al. vol. 12. 2021. p. 909. (A Cross-Sectional Study on Mental Health Problems of Medical and Nonmedical Students in Shandong during the COVID-19 Epidemic Recovery Period). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou S.-J., et al. 2020. Mental Health Problems and Related Factors in Chinese University Students during the COVID-19 Pandemic. [Google Scholar]
- Zhou S.-J., et al. 2021. Depression, Anxiety, and Suicidal Ideation in Chinese University Students during the COVID-19 Pandemic; p. 3389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhuo L., et al. COVID-19-related intolerance of uncertainty and mental health among back-to-school students in Wuhan: the moderation effect of social support. Int. J. Environ. Res. Publ. Health. 2021;18(3):981. doi: 10.3390/ijerph18030981. [DOI] [PMC free article] [PubMed] [Google Scholar]