Abstract
Background and aim
There is growing interest in using herbs and supplementary medications to treat and/or prevent COVID-19, evidenced by multiple reports exploring their effectiveness and safety. From a health psychology perspective, the desire to use herbs and supplementary medications to prevent and/or treat COVID-19 is a health behavior which is attributed to attitudes and beliefs. This systematic review critically appraised and synthesized the data from studies investigating these attitudes and beliefs.
Methods
EMBASE, PubMed, ScienceDirect, Scopus, Cochrane (library), and WebOfScience were searched from inception to December 13, 2021 for studies investigating attitudes and beliefs on the use of herbs and supplementary medications to treat and/or prevent COVID-19.
Results
A total of 17 articles were identified for inclusion. All except one were of cross-sectional design. Participants across most studies had a positive attitude towards using herbs and supplementary medications. They believed that herbs and supplementary medications were effective and were confident in their value in preventing and/or treating COVID-19 symptoms. The majority of included studies had significant flaws in study design and reporting, including inconsistent definitions of herbs and supplementary medications, a lack of theoretical models and conceptual frameworks underpinning the study of beliefs and attitudes, in addition to methodological issues of robustness affecting the validity and reliability of data.
Conclusion
The use of herbs and supplementary medicines to prevent and/or treat COVID-19 could well be driven by a positive attitude stemming from beliefs of effectiveness and safety. There is a need for well-designed studies on attitudes and beliefs that are driven by health behavior theories to permit generalizability of findings and establish more conclusive relationships between beliefs, attitudes and the decision to use herbs and supplementary medications to treat and/or prevent COVID-19.
Keywords: COVID-19, Herbs, Supplementary medications, Systematic review, Attitudes, Beliefs
1. Introduction
The coronavirus disease 2019 (COVID-19) pandemic has had an unprecedented and overwhelming burden on health systems worldwide with far-reaching health and socio-economic implications. The concerted efforts to devise treatment strategies to curb infection spreading, disease severity, and mortality rates had limited success including trials investigating the role of antivirals or repurposed drugs.1, 2, 3, 4 The limited availability and/or accessibility to antiviral treatment stimulated interest in exploring alternative approaches including complementary and alternative medicine (CAM).5 , 6 The US National Center for Complementary and Integrative Health (NCCIH) defines CAM as non-mainstream practice that is used together with or in place of conventional medicine.7 The implication of this definition is that CAM incorporates a diverse group of interventions that exist outside the realm of conventional medicine whilst having some degree of overlap with mainstream practices. The lack of standardization and scrutinized safety and efficacy seem to be the common theme among these practices that sets them apart from normative health systems.8 NCCIH organizes these modalities into five broad systems of practice and treatment methods, namely: ‘alternative medical systems’; ‘mind-body interventions’; ‘manipulative and body-based methods’; ‘energy therapies’ and ‘biologically based treatments’.7 The latter comprises substances that are intended to promote health including herbs and supplementary medications (such as vitamins); both of which are the focus of this study. It is important to note that the use of vitamins in this review (as supplementary medications) refers to their use to promote health rather than to treat or prevent diseases, in cases where vitamin deficiency is established (conventional medicine). This is in line with the operational definition of vitamins as part of the CAM realm, as reported in literature.9
There is strong interest in exploring the merit of using CAMs, in general, and herbs and supplementary medications, in particular, to prevent and/or treat COVID-19 as reflected by reports exploring their value and relevance in clinical practice.10 , 11 A recent systematic review of 14 studies which evaluated the effect of CAM on COVID-19 patients demonstrated that different CAM interventions improved mental and physical symptoms in COVID-19 patients.11 A recently published evidence map of CAM interventions to manage COVID-19 showed a clear focus on the role of herbs and supplementary medications with 46 out of 62 of the identified interventions, in 126 systematic reviews and controlled clinical studies, investigating effects of herbs and supplementary medications.12 This is further corroborated by findings of a more recent overview of systematic reviews on the effectiveness and safety of CAM interventions, where out of the 24 identified systematic reviews, 23 were focused on herbs and supplementary medications (traditional Chinese medicine and vitamin D supplementation to be precise).13
The most substantiated evidence showing that herbs and supplementary medications may be effective and safe to treat COVID-19 when combined with conventional therapy comes from studies investigating the use of herbs in the context of traditional Chinese medicine (TCM).13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25 This evidence base demonstrated a marked improvement in treatment effectiveness as illustrated by improved outcomes including clinical cure and reduced clinical deterioration and symptom scores in mild to moderate cases.13, 14, 15, 16, 17, 18, 19, 20, 21, 22 In the case of supplementary medications, the evidence is less conclusive with vitamin D being most investigated. In fact, vitamin D supplementation may be associated with improved clinical outcomes including decreased mortality rate, severity of disease, and serum levels of the inflammatory markers.26, 27, 28 The strong link between vitamin D deficiency and risk of contracting COVID-19 further supported the role of vitamin D in managing COVID-19. 29 , 30 Other studies, however, showed that vitamin C or D supplementation had no significant impact on major health outcomes in COVID-19. 31, 32, 33
The desire to use herbs and supplementary medications could be driven by their widespread availability, perception of safety, and the lack of cure options offered by conventional medicine in the context of managing COVID-19. 34, 35, 36, 37, 38, 39, 40 This desire to use herbs and supplementary medications among COVID-19 patients could also be looked at from a health psychology perspective as a health behavior which is informed by psychological antecedents including attitudes and beliefs.41 , 42 Attitudes are considered a key construct in health psychology due to the pivotal role they play in driving and changing health behavior.43 They are defined as ‘a psychological tendency that is expressed by evaluating a particular entity (object) with some degree of favor or disfavor’ [positive/negative attitudes].44 Attitudes are considered as an umbrella expression of an individual's psychological characteristics which include beliefs (cognitive component), feelings (affective component) which together with accumulated information (knowledge) and experiences drive the tendency to act in a specific way (behavioral component).45 The belief element refers to ‘the degree to which the object is perceived to have a particular attribute’.46
Many psychological models and frameworks of theories have been proposed to characterize, predict and facilitate/change health behaviors. Some are unique while others share overlapping characteristics owing to the common roots from which they have evolved. These include the Health Belief Model (HBM),47 the Theory of Reasoned Action (TRA),48 the Theory of Planned Behavior (TPB),49 the Trans-Theoretical Model (TTM)50 and the Theoretical Domains Framework (TDF).51 52 These models and frameworks reflect the significance of considering patients' beliefs, attitudes, experiences and behaviors in understanding trends in medication use as reflected in qualitative research.53 , 54 It is also translated in the successful application of models and frameworks of theory to characterize patient health behaviors and implement health interventions.42 , 55 , 56 Incorporating these psychological dimensions is indeed crucial in implementing a holistic approach to patient-centered care which improves health system effectiveness and, importantly, patient health outcomes.57 Patient-centered care is a concept which goes beyond the patient to include families, caregivers and health professionals involved in their care. Understanding beliefs and attitudes of health professionals including pharmacists and pharmacy practitioners, and their impact on shaping the patient's decision is hence essential to obtain a more clear picture on the use of herbs and supplementary medications to treat and/or prevent an array of clinical conditions.58, 59, 60, 61, 62, 63
This review presents an attempt to synthesize and appraise evidence relating to beliefs, and attitudes of patients and other key stakeholders which influence the use of herbs and supplementary medications to prevent and/or treat COVID-19. The outcomes of this study will be relevant to pharmacy practice by providing an insight to help care providers be better informed of the nuances that are prevalent with the use of herbs and supplementary medications with COVID-19. Thus, the delivery of care and selection of individualized recommendations may be provided in a way that is both patient-centered and sensitive to this specific context with an overall aim to improve patient health outcomes.
2. Aim
This systematic review critically appraised and synthesized the data from studies reporting attitudes and beliefs regarding the use of herbs and supplementary medications to prevent and/or treat COVID-19.
3. Methods
This systematic review was in accordance with the Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) guidelines.64 , 65 The protocol was registered on the International Prospective Register of Systematic Reviews (PROSPERO) database (registration number: CRD42022304871).
3.1. Eligibility criteria
Peer-reviewed original research articles published in English were included if they reported on attitudes and beliefs of health professionals, adult patients (aged over 18), and adult members of the general public, regarding the use of herbs and/or supplementary medications with COVID-19.
Studies reporting on the behaviors or prevalence of use of herbs and/or supplementary medications with COVID-19, with no data on attitudes/beliefs were excluded. Additionally, studies that investigated complementary medicine practices other than herbs and/or supplementary medications, or studies which did not report on the specific complementary medicine practice separately were also excluded. Reviews, commentaries, editorials, theses, and dissertations were excluded. Conference abstracts where the full-text was not available were also excluded.
3.2. Search strategy
The following electronic databases were systematically searched from inception until December 13, 2021: EMBASE, PubMed, ScienceDirect, Scopus, Cochrane (library), and WebOfScience. Table S1 provides full details of the search strategies employed in each of the databases above.Where applicable, Medicine Subject Headings (MeSH) and subject headings were used in the electronic search. Truncation was used to include any variations of terms and Boolean operators ‘AND’ and ‘OR’ applied. For all of the databases, appropriate adaptations of the following search were used (Table S1): TITLE-ABS-KEY ((“behavior” OR “attitude” OR perception OR “culture” OR “health” OR “believe” OR experience) AND (“COVID-19″ OR “sars-cov-2″ OR “sars-cov-2 variants” OR “novel coronavirus” OR “coronavirus disease”) AND (“medicinal plants” OR “vitamins” OR “micronutrients” OR “traditional medicine” OR herbs OR minerals OR “food supplements” OR “herbal products”)). Bibliographies of included articles and Google Scholar were used as an additional tracking resource to identify any further studies not retrieved from the systematic search.
3.3. Study selection, quality assessment, data extraction and synthesis
Manuscripts that fulfilled the inclusion criteria were exported to the support platform for the development of systematic reviews Rayyan QCRI®.66
Two reviewers independently screened all articles by title and abstract for eligibility followed by full text screening. Discrepancies were resolved through discussion or in consultation with a third reviewer. The quality assessment was performed using an adapted version of the National Institutes of Health (NIH) quality assessment tool.67 Items relevant to a cohort study design were removed while those that target cross-sectional design were maintained. Two reviewers used the NIH tool independently to quality assess all included articles. Discrepancies were resolved through discussion or in consultation with a third reviewer.
A data extraction sheet was created to align to the research objectives and piloted on 3 selected articles. The following items were extracted: title, authors, year of publication, country, setting, definition of herbs and supplementary medications, objective, study design, inclusion and exclusion criteria, recruitment method, sample size/response rate, list of herbs/supplementary medications investigated, main findings, study limitations, and conclusions. Data extraction was conducted by two independent reviewers, with discrepancies resolved as before.
A descriptive narrative approach was employed to synthesize the data in relation to the specific research objectives (i.e., what are the perceptions of health professionals, adult patients, and members of the general public, regarding the use of herbs and/or supplementary medications with COVID-19). Studies in which a common distinction was made in the type of herb/supplementary medication under investigation were grouped together. Similarly, studies were grouped together where there was a common distinction regarding the specific perception (i.e. beliefs vs attitudes).
4. Results
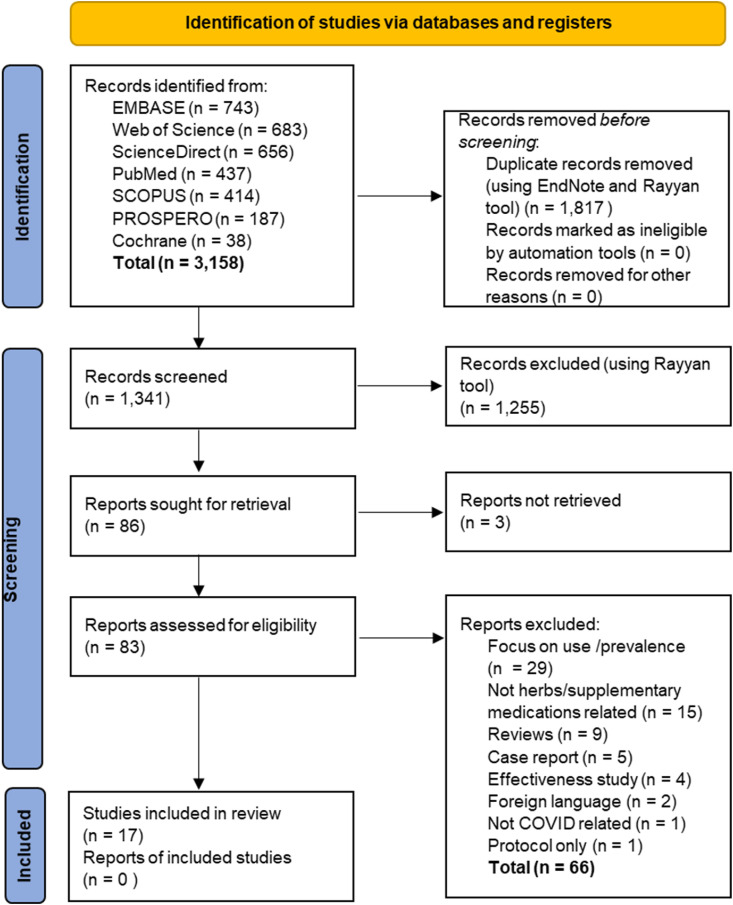
Database searches retrieved 3158 article citations, of which 86 were retained for full-text screening following removal of duplicates and screening of titles and abstracts. Seventeen articles were included in the review. The PRISMA flowchart (Fig. 1 ) summarizes the number of titles, abstracts, and full papers that were excluded (studies reporting use and prevalence only (n = 29), not herbs- and supplementary medications-related (n = 14) or were reviews (n = 9).
Fig. 1.
Study Selection Process.65
4.1. Characteristics of the included studies
Included studies were conducted in Saudi Arabia (n = 4), Turkey (n = 3), China (n = 3), Indonesia (n = 1), Canada (n = 1), India (n = 1), Poland (n = 1), Tanzania (n = 1), Lebanon (n = 1), and Vietnam (n = 1). One study was reported to cover participants of Indian nationality across the world covering a total of eleven countries. All studies but one were of cross-sectional design (the exception being an interview-based qualitative study68), with 15 studies distributing questionnaires via social media and two studies via mobile phone applications.
Thirteen studies included aspects of attitudes and beliefs in their primary objective, with this being a minor component in the other five. The main researched stakeholder group was the general population, with three studies targeting healthcare providers. Table 1 summarizes the characteristics of the included studies.
Table 1.
Study characteristics.
| Author year country | Study aim/objective | Definition of herbs/supplementary medications used – Definition source | Stakeholder involved (n) | % of herbs/supplementary medications users before vs during COVID-19 | Reported specific herbs/supplementary medications used (%) | Reasons for using herbs/supplementary medications (%) |
|---|---|---|---|---|---|---|
| Teke et al.74 2021 Turkey |
To analyze HCP's attitudes toward TCoM and life satisfaction due to COVID-19 |
|
HCP (nurses, doctors, dentists, medical technicians, midwives, dieticians, and physiotherapists) n = 560 |
31.6% before 45.5% during |
|
|
| d’Arqom et al.81 2021 Indonesia |
To explore the mental health of mothers with school-age children, during COVID-19 and its relationship with the consumption of “anti-COVID” medications and supplements. | NP | General population: Mothers with school age children n = 610 |
NR | Natural products:
|
|
| Kong et al.73 2021 Canada |
To assess the attitudes towards the use of TCM in relation to Western medicine among Chinese immigrants in Canada during the early stage of the COVID-19 pandemic. | TCM encompasses a broad range of therapies, such as herbal medicine, acupuncture, massage, Qigong and dietary therapy Source: a review article87 |
General population: Chinese immigrants n = 754 |
NR | NR | NR |
| AlNajrany et al.70 2021 KSA |
To investigate the use of prescription medications, awareness of the viral nature of COVID-19 infection and its common symptoms, and the commonly utilized herbal and/or dietary supplements. | NP are generally classified as DS and include products such as herbs, vitamins and minerals, and probiotics Source: National Center for Complementary and Integrative Health |
General population n = 1473 |
NR |
|
To boost immunity against the infection (64.0%) |
| Puścion-Jakubik et al.83 2021 Poland |
To assess the knowledge and intake of FS during the COVID-19 pandemic, with particular focus on FS containing zinc and Vit D. | FS is a foodstuff intended to be a complement to a normal diet and is a concentrated source of nutrients (vitamins, minerals) or other substances with a nutritional or physiological effect. Source: European Food Safety Authority |
General population n = 935 |
Before: NR 23.5% first COVID wave 25.6%, Second COVID wave 39.1% third COVID wave |
Zinc and Vit D | NR |
| Mshana et al.68 2021 Tanzania |
To explore the effects of COVID-19 on women and how the women and communities dealt with the threat of COVID-19, including the treatment practices | The term traditional medicine and local remedies are used interchangeably to refer to a wide range of herbal remedies in their various forms. This does not imply that these remedies originate in these communities, but there is exchange and adaptation of treatment paradigms between societies. Source: NR |
General population: women between 27 and 57 years old n = 18 |
100% before 100% during |
|
|
| Alshammari et al.79 2021 KSA |
To explore the beliefs and habits and the effect of the COVID-19 pandemic on DS consumption. | DS: substance intake by individuals to supplement the diet by increasing the total dietary consumption, concentrate, metabolite, constituent, extract, or combination of the preceding substances.” They includes vitamins, minerals, herbs, amino acids, and enzymes Source: FDA |
General population n = 575 |
14.8% before 25.2% during 66% indicated no change in consumption due to COVID |
DS vitamins and multivitamins (25.5%) | NR |
| Li et al.75 2021 China |
To investigate the COVID-19 prevention knowledge and practices of supermarket staff, and the factors affecting their concerns about returning to work and to investigate attitudes toward preventing COVID-19 by means of TCM, the demand for related TCM products, and the feasibility of promoting TCM as an additional COVID-19 prevention measure. | NR | General population: supermarket staff n = 2309 |
NR | NR | |
| Altun et al.77 2021 Turkey |
To evaluate the dietary habits of the dietitians who had a leading role in this regard during the pandemic and their use of DS, functional food and HM. |
|
HCP (dieticians) n = 550 |
42.4% used DS before 44.5% using HM during |
Dietary supplements
|
|
| Xia et al.71 2021 China |
Use the theory of planned behavior to identify factors that affect the intention to use TCM. | NR | General population n = 10,824 |
NR | NR | NR |
| Alyami et al.76 2020 KSA |
To explore the knowledge about COVID-19 preventive measures and their belief about the consumption of herbal products for the prevention of COVID-19 infection. | NR | General population n = 5258 |
Before: NR 22.1% during |
|
|
| Pu et al.69 2021 China |
To investigate the knowledge of HCP, their practices, and their attitudes toward TCM for the prevention and treatment of COVID-19 and then assess factors influencing their decisions. | NR | HCP (doctors and nurses) n = 401 |
59.4% reported using TCM in the past 5 years | NR | NR |
| Mohsen et al.82 2021 Lebanon |
To assess the usage, knowledge and attitudes towards DS before and during the COVID-19 pandemic in Lebanon | DS is a non-drug product intended to supplement the diet with one or more of the following: vitamins, minerals, herbs, and amino acids Source: FDA |
General population n = 2966 |
73.3% before 69.9% during |
|
NR |
| Bhol et al.84 2021 International |
To evaluate knowledge and attitude regarding immuno-nutrition in Indians residing in different parts of the world and to evaluate the food and nutrition based practices adopted during lockdown to boost immunity | NR | General population: Indians living across different countries n = 325 |
NR |
|
To boost immunity by participants. |
| Alotiby et al.78 2021 KSA |
To estimate the prevalence of using herbs and NP during the COVID-19 pandemic, determine reasons for using them, and evaluate their potential side effects. | NR | General population n = 1054 |
7.3% before 92.70% during |
|
|
| Karataş et al.72 2021 Turkey |
To determine the use and belief about TCoM during the COVID-19 outbreak. | TCoM refers to therapeutic products and procedures that are not a part of conventional medical care, and are often used by patients without medical supervision Source: National Cancer Institute |
General population n = 389 |
31.6% before 39.3% during |
Herbal medicines (30.8%)
Different multivitamins and minerals like calcium and iron, others |
To prevent COVID-19 infection (39.3%) |
| Nguyen et al.80 2021 Vietnam |
To examine the prevalence and indications for HM use, the factors associated with HM use, and Vietnamese peoples' attitudes towards HM. | NR | General population n = 508 |
NR |
|
|
HCP: Health care provider, NR: not reported KSA: Kingdom of Saudi Arabia; TCoM: traditional complementary medicine; TCM: Traditional Chinese Medicine; DS: Dietary supplements; HM: Herbal medicine; NP: natural products; FS: Food supplements; yrs: years.
*age as reported within the articles; Vit: Vitamin.
COVID-19 first global wave took place between March and end of June 2020 and the second wave between November 2020 and June 2021. Most of the identified studies of this review (12 out of 17 studies) collected data between February and September 2020, coinciding mostly with the first COVID-19 wave.68, 69, 70, 71, 72, 73, 74, 75, 76, 77, 78, 79 Data collection of 3 studies coincided with the second COVID-19 wave.80, 81, 82 Reported data by Puścion-Jakubik et al. were collected over an extended period (July 2020–April 2021), falling within the second and third COVID-19 waves.83 One out of the seventeen identified studies did not mention a specific data collection period.84
4.2. Quality of included studies
Supplementary Table S2 presents the quality of the included studies using the modified NIH Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies. All studies had a clear aim or objective statement, and all clearly specified the targeted population except for one study which did not specify the targeted population nor describe the inclusion/exclusion criteria.84 All studies used social media, or mobile applications to disseminate their questionnaires which rendered calculating the response rate impractical. Three studies targeted the full population (supermarket staff, dietitians, and doctors and nurses)69 , 75 , 77 and reported 100% response rate. The sampling strategy was not described in any of the studies while nine studies provided justification for the sample size. As for the validity and reliability of measurements, the majority of studies (n = 13) did not describe the development, reliability testing or piloting of the questionnaire. Only one study utilized a theory in developing their questionnaire.71
Only one study68 was qualitative in design, therefore the Critical Appraisal Skills Program (CASP) tool for qualitative studies was used for quality appraisal of this study.85 The study had a clear aim and detailed description of the methodology. However, the recruited participants were interviewees who were involved in a previous study which had a different context, aim, and purpose.86 Other than using the same sample pool for the COVID-19 study, there was no sufficient rationale given for the chosen participants.
4.3. Definitions used
The included studies investigated a range of herbs and supplementary medications and they adopted diverse terminologies. The terms “dietary supplements”, “food supplements”, ‘traditional medicine”, “complementary medicine”, “traditional Chinese medicine”, “herbal medicine”, and “traditional complementary medicine” all appeared to have very similar meanings and use across the seventeen studies with only ten studies providing a general definition for the terms used. The main observed difference was between the definition of herbals and dietary supplements where the former covers plants and the latter covers vitamins and minerals. There was no main reference for the definitions used; several references were used such as the FDA, the WHO, the National Center for Complementary and Integrative Health, the European Food and Safety Authority, the Turkish Medical Association, and the National Cancer Institute.
4.4. Beliefs and attitudes towards herbs and or supplementary medications
Table 1, Table 2 provide an overview of the main characteristics and findings and highlight the heterogeneity across the studies.
Table 2.
Evidence synthesis from the included studies.
| Ref | herbs/supplementary medications used | Attitudes/beliefs |
|---|---|---|
| Articles with a clear distinction being made between herbs and supplementary medications | ||
| Li et al.75 | Traditional Chinese Medicine | Described as attitudes regarding TCM COVID-19 prevention (n = 2309).
|
| Xia et al.71 | Traditional Chinese Medicine | Described as attitude scored using a questionnaire. (n = 10,824) No percentages provided
|
| Pu et al.69 | Traditional Chinese Medicine | Described as attitude:
|
| Mohsen et al.82 | Dietary supplements | Described as beliefs
|
| Alshammari et al.79 | Dietary supplements | Described as beliefs (n = 575)
|
| Puścion-Jakubik et al.83 | Food supplements | Described as beliefs
|
| Altun et al.77 | Dietary supplements | Described as beliefs (n = 550)
|
| Herbal medicine | Described as beliefs (n = 550)
|
|
| Nguyen et al.80 | Herbal medicine | Described as attitude
|
| Alyami et al.76 | Herbal medicines | Described as beliefs (n = 5245)
|
| Articles with NO clear distinction is made between herbs and supplementary medications used | ||
| Karataş et al.72 | Described as beliefs
|
|
| Teke et al.74 | Described as attitude scored using a questionnaire. (n = 560) No percentages provided
|
|
| A3 Kong et al.73 |
Describes beliefs of traditional Chinese modalities
|
|
| Mshana et al.68 | Describes the beliefs of traditional medicine and local remedies
|
|
| Articles where NO clear distinction is made in terms of attitudes, beliefs and behavior | ||
| d’Arqom et al.81 | Article describes why participants used “anti-COVID” medications and supplements.
|
|
| AlNajrany et al.70 | Article describes why participants used herbal products
|
|
| Bhol et al.84 | Article describes why participants use immuno-nutrition
|
|
| Alotiby et al.78 | Article describes why participants use herbal and natural products
|
|
The three studies that focused on TCM did not provide a clear definition of the term, nor describe the herbs under investigation. The studies provided an overview of the attitudes of the general population71 , 75 or healthcare providers69 in China. Overall, 73.4% of the participants had a positive attitude towards the use of TCM in the treatment of COVID-19 and between 55.2% and 79.9% has a positive attitude towards the use of TCM in prevention of COVID-19 69,75, and around 60% agreed that TCM can help in improving COVID-19 symptoms.69 Xia et al. (2021) highlighted that a positive attitude correlated with higher likelihood of using TCM among the general population.71
Three studies explicitly investigated “dietary supplements” while one study used “food supplements” as terms. Mohsen et al. and Alshummari et al. both used the FDA definition of dietary supplements and included herbs along with vitamins and minerals in this classification.79 , 82 While Altun et al. and Puścion-Jakubik et al. considered the Turkish medical association definition, and that of the European food and safety authority, respectively, which separated herbs from minerals and vitamins.77 , 83 Mohsen et al. highlighted that 76% of the participants believed that dietary supplements are pre-tested for safety, yet only 33% believed they are considered safe.82 While 41.2% in Alshummari's et al. study believed that dietary supplements are safe.79
Additionally, three studies used the term “herbal medicine” without providing a definition, and employed different statements reflecting attitudes and beliefs.76 , 80 , 83 Alyami et al. (2020) included in the questionnaire specific items to investigate different herbs used in COVID-19. Their findings revealed that 34.4% of the general population sample believed that eating garlic increases immunity and reduces the chances of contracting COVID-19 76. Four studies provided collated responses of beliefs and attitudes; and findings relating to herbs and supplementary medications were reported cumulatively68 , 72, 73, 74 Four studies did not define specific statements included in their questionnaire as beliefs or attitudes (Table 2 ).70 , 78 , 81 , 84
4.5. Factors influencing attitudes, and beliefs
Only one study (Xia et al., 2021) investigated the intentions to use TCM using the theoretical framework of the Theory of Planned Behavior.71 The authors found that attitude, subjective norms, and perceived behavioral control all contributed to the increased use of TCM. Additionally, past behavior of using TCM contributed to the increased use during the pandemic. The authors reported that past behavior reflected unconscious automatic psychological processes. The final model that included the four factors (attitude, subjective norms, perceived behavioral control, and past behavior) explained 77% of the intention to use TCM. Past behavior was also identified as an influencing factor by Teke et al.74 and Pu et al., 69 along with other factors such as age and level of education.
Other studies that investigated the influencing factors, did so statistically through logistic regression. The identified factors were different from one study to another. Kong et al. identified age as an influencing factor whereby participants above 55 years old were more likely to believe the effectiveness of TCM against COVID-19 73. It is also of note that Puścion-Jakubik et al. highlighted that the use of vitamin C and zinc (the primary investigated supplements) increased with the higher level of education of the participants in Poland which could reflect the increased level of knowledge and awareness of the benefits of these supplements amongst the well-educated.83 Alshammari et al.79 and Nguyen et al.80 both indicated that the higher the income the higher the use, while Mohsen et al. reported an overall reduced use of herbs/supplementary medications during the pandemic as a result of the economic crisis in Lebanon.82
Mshana et al. used qualitative interviews with women in Tanzania and concluded that the perceived efficacy of traditional medicine was reinforced by personal experience and testimonies from the close social network.68 Similarly, Alshammari et al. highlighted that family and friends influenced behavior concerning the use of supplements.79 While social media and the internet were identified as influencing factors by three studies.70 , 72 , 76
5. Discussion
5.1. Statement of key findings
This systematic review revealed a limited number of studies investigating attitudes and beliefs towards the use of herbs and supplementary medications to treat and/or prevent COVID-19. Most of the included studies had methodological issues, with very few adopting conceptual frameworks to underpin their investigations; thus, placing significant limitations on data synthesis. The reported evidence suggests that despite the limited evidence-base there exists a general positive attitude amongst patients and the public towards the use of these modalities and a belief that they are somewhat effective, with participants expressing few concerns over their safety.
These findings are of benefit to health professionals who are involved in delivering patient care since beliefs and attitudes towards herbs and supplementary medications are likely determinants of patients’ use of these modalities; not only for the management of COVID-19, but one may expect similar behavioral patterns in other therapeutic areas. With such an insight, health care professionals, including pharmacy professionals, are better-informed of the diversity of potential factors that may need to be negotiated to achieve a mutual therapeutic goal with patients.
5.2. Strengths and weaknesses
The review was conducted and reported in accordance with PRISMA (Preferred Reporting Items for Systematic Review and Meta-Analysis) standards.65 In addition, this systematic review followed best practices using guidelines and definitions from the Center for Reviews and Dissemination.88 Each identified study was independently reviewed by two authors using standard evidence-based critical appraisal rules.67 , 85
It was challenging to generate generalizable conclusions from this review as it was not possible to pool data from the included studies in a coherent way due to the significant heterogeneity of the investigations and their inherent weaknesses (as will be discussed below). It is also noteworthy that the adopted inclusion criteria may have resulted in overlooking further relevant work. The generalizability and transferability of the review findings may be limited given that most studies were conducted in Asia, reporting on an array of herbs and/or supplementary medications.
5.3. Interpretation
This review set out to shed light on the attitudes and beliefs of all stakeholders regarding the use of herbs and supplementary medications to prevent and/or treat COVID-19. This included health professionals who play a significant role in shaping health behavior while providing and directing patient care.89 , 90 However, there was a lack of investigations of health professionals (only two studies investigating ‘health professionals’69 , 74 and one investigating dietitians specifically77) which limited the opportunity to establish further important insights. Further research is required to gain a better understanding of their perspective.
Beyond this, there were several deficiencies in the included studies which made the process of evidence synthesis challenging. Of note, the definition of CAMs was applied inconsistently in the included studies. Consequently, there were significant challenges in attempting to pool data in an appropriate manner to generate credible and generalizable conclusions.
Moreover, the frequent use of social media and SMS to disseminate study questionnaires made it impractical to ascertain if the sample was representative of the study population. Evans and Mathur noted that although social media affords benefits in terms of potential reach, flexibility and speed, there are major weaknesses of an unknown sampling frame, sampling bias, poor and unknown response rates, potential multiple submissions, perceptions of lacking scientific robustness, and issues of confidentiality.91 Because the studies were predominantly cross-sectional, it is very difficult to conclude whether reported attitudes and beliefs were held prior, or if they are in fact a precipitation of subsequent experiences.
There was also a notable paucity of qualitative studies; only one study by Mshana et al. involving 18 participants.68 Qualitative research offers trustworthiness by conveying the views of participants and in-depth explanation of results,92 unlike quantitative self-reported questionnaire responses which cannot be validated and may be influenced by social desirability biases. In addition, qualitative research can be based on specific theoretical frameworks which can help identify behavioral determinants affecting an intervention such as attitudes and beliefs.93
In this review, only one study adopted theory in developing the data collection tool.71 The benefits of theory-informed research are well-established,94 including providing comprehensive explanations of the phenomena under investigation, enhancing the research robustness and rigor, as well as increasing the relevance and impact of research findings. Moreover, developing a research instrument (e.g. questionnaire) about attitudes and beliefs on a theoretical model improves the predictive accuracy of a health behavior study.95 The lack of theory may have been a factor that led to a significant proportion of the studies failing to differentiate between the concepts of attitudes and beliefs; the two were often misconstrued as a single construct.
Regarding the findings of this review, most participants viewed herbs and supplementary medications as being safe; such views have been reported in similar studies that investigated various stakeholders. These studies included using herbs and supplementary medications during pregnancy,59 breastfeeding,60 cancer,61 , 62 , 96 psychiatric disorders97 and HIV.98 Further studies have elucidated these findings and revealed a close association between their use and perceived non-toxicity and a belief that these modalities were ‘safe and natural treatments’.63 , 99, 100, 101, 102, 103, 104
Stakeholders' positive attitudes toward herbs and complementary medicines have also been reported in studies exploring potential factors which influence the use of these modalities.63 These positive attitudes may be explained by findings from a 2010 study which as well as reporting a relationship between attitudes toward CAM and CAM use, also concludes that CAM use is linked to a patient's desire for control over their own health rather than attributing health decisions to others like doctors, family, or chance.105
Such explanations warrant further investigations to probe for greater understanding and identify their possible generalizability. It is well established within the medical field (and beyond) that persons' attitudes, beliefs and views influence their behaviors. Notably, a study of complementary medicine use, underpinned with the Theory of Planned Behavior (TPB) as a behavioral theory, revealed that cancer patients’ attitudes and beliefs were predictive of their decision to use complementary medicines.61 Similarly, attitudes and beliefs underpinned by TPB could predict complementary medicine use by older adults106 and patients with anxiety.107
Healthcare professionals' awareness of patients' beliefs, views and attitudes facilitates the provision of person-centered care (PCC). Indeed, Standard 1 of the United Kingdom, General Pharmaceutical Council Standards for pharmacy professionals and students, is to Provide person-centered care, which is stated to include recognizing patients’ own values and beliefs.108 The delivery of PCC has been shown to reduce cost of care, while improving health care responsiveness, quality, and outcomes.57 , 109
Therefore, since the findings from this study provide further details of attitudes and beliefs held by patients towards the use of herbs and supplementary medications in the management of COVID-19; health professionals may develop a greater understanding of potential patient behaviors regarding the general use of herbs and supplementary medications and be better placed to deliver PCC.
5.4. Further work
The included studies suffered from several deficits in structure and design. To gain a better understanding of attitudes and beliefs influencing the use of herbs and supplementary medications to prevent and or/treat COVID-19, there is a need to expand the evidence base. This includes moving beyond cross-sectional surveys to well-designed mixed-method studies incorporating behavior theories, which can offer answers on attitudes and beliefs predating the use of these modalities. It also involves shedding some light on the relationship and interplay between experiences, behaviors, attitudes, and beliefs of different stakeholders when using herbs and supplementary medications to treat and/or prevent COVID-19.
6. Conclusion
The limited evidence base regarding the attitudes and beliefs on the use of herbs and supplementary medications to prevent and/or treat COVID-19 warrants future investigation based on mixed-methods research, which incorporates behavior theories. These future studies will help to better understand the factors influencing stakeholders' behaviors, beliefs, and attitudes; thus providing greater opportunity for health professionals to enhance the delivery of person-centered care.
Authors contributions
All authors had (a) substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; AND (b) drafting the work or revising it critically for important intellectual content; AND (c) final approval of the version to be published; AND (d) agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Funding
Qatar National Research Fund (QNRF) grant number RRC02-0807-210,022 to AS. The funding source (QNRF) had no role in study design, in the collection, analysis and interpretation of data, in the writing of the manuscript, or in the decision to submit the article for publication.
Ethical disclosure
No ethical approval was required for this article.
Data sharing statement
Data were collected from already published articles.
Declaration of competing interest
All authors declare no conflict of interests.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.sapharm.2022.11.004.
Appendix A. Supplementary data
The following is/are the supplementary data to this article:
References
- 1.World Health organization Q&A on coronaviruses (COVID-19) 2020. https://www.who.int/news-room/questions-and-answers/item/coronavirus-disease-covid-19 Published October 24.
- 2.Zhang J., Xie B., Hashimoto K. Current status of potential therapeutic candidates for the COVID-19 crisis. Brain Behav Immun. 2020;87:59–73. doi: 10.1016/j.bbi.2020.04.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.WHO Solidarity Trial Consortium Repurposed antiviral drugs for Covid-19—interim WHO solidarity trial results. N Engl J Med. 2021;384(6):497–511. doi: 10.1056/NEJMoa2023184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Martinez M.A. Clinical trials of repurposed antivirals for SARS-CoV-2. Antimicrob Agents Chemother. 2020;64(9):e01101–e01120. doi: 10.1128/AAC.01101-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.National Center for Complementary and Integrative Health COVID-19 and “alternative” treatments: what you need to know. NCCIH. https://www.nccih.nih.gov/health/covid-19-and-alternative-treatments-what-you-need-to-know Published October 15, 2021.
- 6.Peng Y., Tao H., Satyanarayanan S.K., Jin K., Su H. A comprehensive summary of the knowledge on COVID-19 treatment. Aging and disease. 2021;12(1):155. doi: 10.14336/AD.2020.1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Complementary, alternative, or integrative health: what's in a name? NCCIH. https://www.nccih.nih.gov/health/complementary-alternative-or-integrative-health-whats-in-a-name
- 8.Mainardi T., Kapoor S., Bielory L. Complementary and alternative medicine: herbs, phytochemicals and vitamins and their immunologic effects. J Allergy Clin Immunol. 2009;123(2):283–294. doi: 10.1016/j.jaci.2008.12.023. [DOI] [PubMed] [Google Scholar]
- 9.Wieland L.S., Manheimer E., Berman B.M. Development and classification of an operational definition of complementary and alternative medicine for the Cochrane collaboration. Alternative Ther Health Med. 2011;17(2):50. [PMC free article] [PubMed] [Google Scholar]
- 10.Paudyal V., Sun S., Hussain R., Abutaleb M.H., Hedima E.W. Complementary and alternative medicines use in COVID-19: a global perspective on practice, policy and research. Res Soc Adm Pharm. 2022;18(3):2524–2528. doi: 10.1016/j.sapharm.2021.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Badakhsh M., Dastras M., Sarchahi Z., Doostkami M., Mir A., Bouya S. Reviews on environmental health; 2021. Complementary and Alternative Medicine Therapies and COVID-19: A Systematic Review. Published online. [DOI] [PubMed] [Google Scholar]
- 12.Portella C.F.S., Ghelman R., Abdala C.V.M., Schveitzer M.C. Evidence map on the contributions of traditional, complementary and integrative medicines for health care in times of COVID-19. Integrative medicine research. 2020;9(3) doi: 10.1016/j.imr.2020.100473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jeon S.R., Kang J.W., Ang L., Lee H.W., Lee M.S., Kim T.H. Complementary and alternative medicine (CAM) interventions for COVID-19: an overview of systematic reviews. Integrative medicine research. 2022 doi: 10.1016/j.imr.2022.100842. Published online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liu M., Gao Y., Yuan Y., et al. Efficacy and safety of integrated traditional Chinese and western medicine for corona virus disease 2019 (COVID-19): a systematic review and meta-analysis. Pharmacol Res. 2020;158 doi: 10.1016/j.phrs.2020.104896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kumar A., Rai A., Khan M.S., et al. Role of herbal medicines in the management of patients with COVID-19: a systematic review and meta-analysis of randomized controlled trials. Journal of traditional and complementary medicine. 2022;Volume 12:100–113. doi: 10.1016/j.jtcme.2022.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Runfeng L., Yunlong H., Jicheng H., et al. Lianhuaqingwen exerts anti-viral and anti-inflammatory activity against novel coronavirus (SARS-CoV-2) Pharmacol Res. 2020;156 doi: 10.1016/j.phrs.2020.104761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhou L., peng Wang, Xie J., hua R., et al. The effects of traditional Chinese medicine as an auxiliary treatment for COVID-19: a systematic review and meta-analysis. J Alternative Compl Med. 2021;27(3):225–237. doi: 10.1089/acm.2020.0310. [DOI] [PubMed] [Google Scholar]
- 18.Liu M., Gao Y., Yuan Y., et al. Efficacy and safety of herbal medicine (Lianhuaqingwen) for treating COVID-19: a systematic review and meta-analysis. Integrative medicine research. 2021;10(1) doi: 10.1016/j.imr.2020.100644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hu C., Liang M., Gong F., He B., Zhao D., Zhang G. Efficacy of Lianhua Qingwen compared with conventional drugs in the treatment of common pneumonia and COVID-19 pneumonia: a meta-analysis. Evid base Compl Alternative Med. 2020:2020. doi: 10.1155/2020/5157089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liang S.B., Fang M., Liang C.H., et al. Therapeutic effects and safety of oral Chinese patent medicine for COVID-19: a rapid systematic review and meta-analysis of randomized controlled trials. Compl Ther Med. 2021;60 doi: 10.1016/j.ctim.2021.102744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Du X., Shi L., Cao W., Zuo B., Zhou A. Add-on effect of Chinese herbal medicine in the treatment of mild to moderate COVID-19: a systematic review and meta-analysis. PLoS One. 2021;16(8) doi: 10.1371/journal.pone.0256429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wang H., Xu B., Zhang Y., et al. Efficacy and safety of traditional Chinese medicine in Coronavirus Disease 2019 (COVID-19): a systematic review and meta-analysis. Front Pharmacol. 2021:12. doi: 10.3389/fphar.2021.609213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Feng Z., Yang J., Xu M., et al. Dietary supplements and herbal medicine for COVID-19: a systematic review of randomized control trials. Clinical Nutrition ESPEN. 2021;44:50–60. doi: 10.1016/j.clnesp.2021.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Alam S., Sarker M., Rahman M., et al. Traditional herbal medicines, bioactive metabolites, and plant products against COVID-19: update on clinical trials and mechanism of actions. Front Pharmacol. 2021;12:1248. doi: 10.3389/fphar.2021.671498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Xiao M., Tian J., Zhou Y., et al. Efficacy of Huoxiang Zhengqi dropping pills and Lianhua Qingwen granules in treatment of COVID-19: a randomized controlled trial. Pharmacol Res. 2020;161 doi: 10.1016/j.phrs.2020.105126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pal R., Banerjee M., Bhadada S.K., Shetty A.J., Singh B., Vyas A. Vitamin D supplementation and clinical outcomes in COVID-19: a systematic review and meta-analysis. J Endocrinol Invest. 2021:1–16. doi: 10.1007/s40618-021-01614-4. Published online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hariyanto T.I., Intan D., Hananto J.E., Harapan H., Kurniawan A. Vitamin D supplementation and Covid‐19 outcomes: a systematic review, meta‐analysis and meta‐regression. Rev Med Virol. 2022;32(2):e2269. doi: 10.1002/rmv.2280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nikniaz L., Akbarzadeh M.A., Hosseinifard H., Hosseini M.S. The impact of vitamin D supplementation on mortality rate and clinical outcomes of COVID-19 patients: a systematic review and meta-analysis. Pharmaceut Sci. 2021;27(Covid-19):S1–S12. [Google Scholar]
- 29.Teshome A., Adane A., Girma B., Mekonnen Z.A. The impact of vitamin D level on COVID-19 infection: systematic review and meta-analysis. Front Public Health. 2021;9:169. doi: 10.3389/fpubh.2021.624559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ghasemian R., Shamshirian A., Heydari K., et al. The role of vitamin D in the age of COVID‐19: a systematic review and meta‐analysis. Int J Clin Pract. 2021;75(11) doi: 10.1111/ijcp.14675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rawat D., Roy A., Maitra S., Gulati A., Khanna P., Baidya D.K. Vitamin C and COVID-19 treatment: a systematic review and meta-analysis of randomized controlled trials. Diabetes Metabol Syndr: Clin Res Rev. 2021;15(6) doi: 10.1016/j.dsx.2021.102324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bassatne A., Basbous M., Chakhtoura M., El Zein O., Rahme M., Fuleihan G.E.H. The link between COVID-19 and VItamin D (VIVID): a systematic review and meta-analysis. Metabolism. 2021;119 doi: 10.1016/j.metabol.2021.154753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rawat D., Roy A., Maitra S., Shankar V., Khanna P., Baidya D.K. Vitamin D supplementation and COVID-19 treatment: a systematic review and meta-analysis. Diabetes Metabol Syndr: Clin Res Rev. 2021;15(4) doi: 10.1016/j.dsx.2021.102189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chu C.M., Cheng V.C.C., Hung I.F.N., et al. Role of lopinavir/ritonavir in the treatment of SARS: initial virological and clinical findings. Thorax. 2004;59(3):252. doi: 10.1136/thorax.2003.012658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sheahan T.P., Sims A.C., Graham R.L., et al. Broad-spectrum antiviral GS-5734 inhibits both epidemic and zoonotic coronaviruses. Sci Transl Med. 2017;9(396) doi: 10.1126/scitranslmed.aal3653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sheahan T.P., Sims A.C., Leist S.R., et al. Comparative therapeutic efficacy of remdesivir and combination lopinavir, ritonavir, and interferon beta against MERS-CoV. Nat Commun. 2020;11(1):1–14. doi: 10.1038/s41467-019-13940-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Grein J., Ohmagari N., Shin D., et al. Compassionate use of remdesivir for patients with severe Covid-19. N Engl J Med. 2020;382(24):2327–2336. doi: 10.1056/NEJMoa2007016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cao B., Wang Y., Wen D., et al. A trial of lopinavir–ritonavir in adults hospitalized with severe Covid-19. N Engl J Med. 2020;382:1787–1799. doi: 10.1056/NEJMoa2001282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gao J., Tian Z., Breakthrough Yang X. Chloroquine phosphate has shown apparent efficacy in treatment of COVID-19 associated pneumonia in clinical studies. Bioscience trends. 2020;14(1):72–73. doi: 10.5582/bst.2020.01047. [DOI] [PubMed] [Google Scholar]
- 40.Gautret P., Lagier J.C., Parola P., et al. Hydroxychloroquine and azithromycin as a treatment of COVID-19: results of an open-label non-randomized clinical trial. Int J Antimicrob Agents. 2020;56(1) doi: 10.1016/j.ijantimicag.2020.105949. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 41.Abraham C., Sheeran P., Johnston M. From health beliefs to self-regulation: theoretical advances in the psychology of action control. Psychol Health. 1998;13(4):569–591. [Google Scholar]
- 42.Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50(2):179–211. [Google Scholar]
- 43.Lowe R., Norman P. Attitudinal approaches to health behavior: integrating expectancy‐value and automaticity accounts. Social and Personality Psychology Compass. 2013;7(8):572–584. [Google Scholar]
- 44.Eagly A.H., Chaiken S. Harcourt brace Jovanovich college publishers; 1993. The Psychology of Attitudes. [Google Scholar]
- 45.Bakanauskas A.P., Kondrotienė E., Puksas A. 2020. The Theoretical Aspects of Attitude Formation Factors and Their Impact on Health Behaviour. Published online. [Google Scholar]
- 46.Ajzen I., Fishbein M. Attitudes and the attitude-behavior relation: Reasoned and automatic processes. Eur Rev Soc Psychol. 2000;11(1):1–33. [Google Scholar]
- 47.Rosenstock I.M. The health belief model and preventive health behavior. Health Educ Monogr. 1974;2(4):354–386. doi: 10.1177/109019817800600406. [DOI] [PubMed] [Google Scholar]
- 48.Fishbein M. 1979. A Theory of Reasoned Action: Some Applications and Implications. Published online. [PubMed] [Google Scholar]
- 49.Ajzen I. The theory of planned behaviour: reactions and reflections. Psychol Health. 2011;26(9):1113–1127. doi: 10.1080/08870446.2011.613995. [DOI] [PubMed] [Google Scholar]
- 50.Taylor D., Bury M., Campling N., et al. The Theory of Planned Behaviour (TPB) and the Trans-theoretical Model (TTM) to Study and Predict Health Related Behaviour Change. National Institute for Health and Clinical Excellence; London, UK: 2006. A review of the use of the health belief model (HBM), the theory of reasoned action (TRA) pp. 1–215. Published online. [Google Scholar]
- 51.Michie S., Johnston M., Abraham C., Lawton R., Parker D., Walker A. Making psychological theory useful for implementing evidence based practice: a consensus approach. BMJ Qual Saf. 2005;14(1):26–33. doi: 10.1136/qshc.2004.011155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Michie S., Van Stralen M.M., West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. 2011;6(1):1–12. doi: 10.1186/1748-5908-6-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wan B.K., Cheung W.H., Ball P.A., Jackson D.M., Maynard G.J. Beliefs about medicines among Hong Kong hospital outpatients. Int J Pharm Pract. 2017;25(6):447–453. doi: 10.1111/ijpp.12353. [DOI] [PubMed] [Google Scholar]
- 54.Blaakman S.W., Cohen A., Fagnano M., Halterman J.S. Asthma medication adherence among urban teens: a qualitative analysis of barriers, facilitators and experiences with school-based care. J Asthma. 2014;51(5):522–529. doi: 10.3109/02770903.2014.885041. [DOI] [PubMed] [Google Scholar]
- 55.Weinman J., Petrie K.J., Moss-Morris R., Horne R. The illness perception questionnaire: a new method for assessing the cognitive representation of illness. Psychol Health. 1996;11(3):431–445. [Google Scholar]
- 56.Horne R., Weinman J. Patients' beliefs about prescribed medicines and their role in adherence to treatment in chronic physical illness. J Psychosom Res. 1999;47(6):555–567. doi: 10.1016/s0022-3999(99)00057-4. [DOI] [PubMed] [Google Scholar]
- 57.Santana M.J., Manalili K., Jolley R.J., Zelinsky S., Quan H., Lu M. How to practice person‐centred care: a conceptual framework. Health Expect. 2018;21(2):429–440. doi: 10.1111/hex.12640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hyland M.E., Lewith G.T., Westoby C. Developing a measure of attitudes: the holistic complementary and alternative medicine questionnaire. Compl Ther Med. 2003;11(1):33–38. doi: 10.1016/s0965-2299(02)00113-9. [DOI] [PubMed] [Google Scholar]
- 59.Pallivalappila A.R., Stewart D., Shetty A., Pande B., McLay J.S. Complementary and alternative medicines use during pregnancy: a systematic review of pregnant women and healthcare professional views and experiences. Evid base Compl Alternative Med. 2013;2013 doi: 10.1155/2013/205639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Barnes L.A., Barclay L., McCaffery K., Aslani P. Complementary medicine products: information sources, perceived benefits and maternal health literacy. Women Birth. 2019;32(6):493–520. doi: 10.1016/j.wombi.2018.11.015. [DOI] [PubMed] [Google Scholar]
- 61.Bauml J.M., Chokshi S., Schapira M.M., et al. Do attitudes and beliefs regarding complementary and alternative medicine impact its use among patients with cancer? A cross‐sectional survey. Cancer. 2015;121(14):2431–2438. doi: 10.1002/cncr.29173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Keene M.R., Heslop I.M., Sabesan S.S., Glass B.D. Knowledge, attitudes and practices of health professionals toward complementary and alternative medicine in cancer care–a systematic review. J Commun Healthc. 2020;13(3):205–218. [Google Scholar]
- 63.Tangkiatkumjai M., Boardman H., Walker D.M. Potential factors that influence usage of complementary and alternative medicine worldwide: a systematic review. BMC complementary medicine and therapies. 2020;20(1):1–15. doi: 10.1186/s12906-020-03157-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Moher D., Liberati A., Tetzlaff J., Altman D.G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Page M.J., McKenzie J.E., Bossuyt P.M., et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg. 2021;88 doi: 10.1016/j.ijsu.2021.105906. [DOI] [PubMed] [Google Scholar]
- 66.Ouzzani M., Hammady H., Fedorowicz Z., Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Rev. 2016;5(1):1–10. doi: 10.1186/s13643-016-0384-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.National Institute of . Blood Institute. Study Quality Assessment Tools.; 2021. Health | National Heart, Lung.https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools [Google Scholar]
- 68.Mshana G., Mchome Z., Aloyce D., Peter E., Kapiga S., Stöckl H. Contested or complementary healing paradigms? Women's narratives of COVID-19 remedies in Mwanza, Tanzania. J Ethnobiol Ethnomed. 2021;17(1):1–12. doi: 10.1186/s13002-021-00457-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Pu J., Mei H., Lei L., et al. Knowledge of medical professionals, their practices, and their attitudes toward traditional Chinese medicine for the prevention and treatment of coronavirus disease 2019: a survey in Sichuan, China. PLoS One. 2021;16(3) doi: 10.1371/journal.pone.0234855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.AlNajrany S.M., Asiri Y., Sales I., AlRuthia Y. The commonly utilized natural products during the COVID-19 pandemic in Saudi Arabia: a cross-sectional online survey. Int J Environ Res Publ Health. 2021;18(9):4688. doi: 10.3390/ijerph18094688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Xia Y., Chang J., Miao hui, zhang H., Wang D. Impact of the COVID-19 pandemic on intention to use traditional Chinese medicine: a cross-sectional study based on the theory of planned behavior. Journal of integrative medicine. 2021;19(3):219–225. doi: 10.1016/j.joim.2021.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Karataş Y., Khan Z., Ç Bilen, et al. Traditional and Complementary Medicine use and beliefs during COVID-19 outbreak: a cross-sectional survey among the general population in Turkey. Advances in Integrative Medicine. 2021;8(4):261–266. doi: 10.1016/j.aimed.2021.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Kong Y., Shaver L.G., Shi F., et al. Attitudes of Chinese immigrants in Canada towards the use of Traditional Chinese Medicine for prevention and management of COVID-19: a cross-sectional survey during the early stages of the pandemic. BMJ Open. 2021;11(9) doi: 10.1136/bmjopen-2021-051499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Teke N., Özer Z., Bahçecioğlu Turan G. Analysis of health care personnel's attitudes toward complementary and alternative medicine and life satisfaction due to COVID-19 pandemic. Holist Nurs Pract. 2021;35(2):98–107. doi: 10.1097/HNP.0000000000000431. [DOI] [PubMed] [Google Scholar]
- 75.Li L., Meng Y., Wang J., et al. Attitudes about the Efficacy of Traditional Chinese Medicine: Survey on Supermarket Staff in Huanggang. Frontiers in public health; China: 2021. Effect of knowledge/practice of COVID-19 prevention measures on return-to-work concerns; p. 1328. Published online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Alyami H.S., Orabi M.A., Aldhabbah F.M., et al. Knowledge about COVID-19 and beliefs about and use of herbal products during the COVID-19 pandemic: a cross-sectional study in Saudi Arabia. Saudi Pharmaceut J. 2020;28(11):1326–1332. doi: 10.1016/j.jsps.2020.08.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Altun H.K., Ermumcu M.S.K., Kurklu N.S. Evaluation of dietary supplement, functional food and herbal medicine use by dietitians during the COVID-19 pandemic. Publ Health Nutr. 2021;24(5):861–869. doi: 10.1017/S1368980020005297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Abdullah Alotiby A., Naif Al-Harbi L. Prevalence of using herbs and natural products as a protective measure during the COVID-19 pandemic among the Saudi population: an online cross-sectional survey. Saudi Pharmaceut J. 2021;29(5):410–417. doi: 10.1016/j.jsps.2021.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Alshammari S.A., Alwakeel L.S., Alghtani J.A., Alsabbagh L.M. Effect of COVID-19 on awareness and consumption of dietary supplements in Saudi Arabia. Journal of Nature and Science of Medicine. 2021;4(2):190. [Google Scholar]
- 80.Nguyen P.H., De Tran V., Pham D.T., Dao T.N.P., Dewey R.S. Use of and attitudes towards herbal medicine during the COVID-19 pandemic: a cross-sectional study in Vietnam. European Journal of Integrative Medicine. 2021;44 doi: 10.1016/j.eujim.2021.101328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.d'Arqom A., Sawitri B., Nasution Z., Lazuardi R. Anti-COVID-19” medications, supplements, and mental health status in Indonesian mothers with school-age children. Int J Wom Health. 2021;13:699. doi: 10.2147/IJWH.S316417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Mohsen H., Yazbeck N., Al-Jawaldeh A., et al. Knowledge, attitudes, and practices related to dietary supplementation, before and during the COVID-19 pandemic: findings from a cross-sectional survey in the Lebanese population. Int J Environ Res Publ Health. 2021;18(16):8856. doi: 10.3390/ijerph18168856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Puścion-Jakubik A., Bielecka J., Grabia M., et al. Consumption of food supplements during the three COVID-19 waves in Poland—focus on zinc and vitamin D. Nutrients. 2021;13(10):3361. doi: 10.3390/nu13103361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Bhol A., Sanwalka N., Imani J.T., et al. An online survey to evaluate knowledge, attitude and practices regarding immuno-nutrition during COVID pandemic in Indians staying in different countries. Curr Res Nutr Food Sci. 2021;9(2):390. [Google Scholar]
- 85.Casp U.K. Critical appraisal Skills programme (CASP). CASP - critical appraisal Skills programme. https://casp-uk.net/ Accessed.
- 86.Kapiga S., Harvey S., Mshana G., et al. A social empowerment intervention to prevent intimate partner violence against women in a microfinance scheme in Tanzania: findings from the MAISHA cluster randomised controlled trial. Lancet Global Health. 2019;7(10):e1423–e1434. doi: 10.1016/S2214-109X(19)30316-X. [DOI] [PubMed] [Google Scholar]
- 87.Chung V.C.H., Ma P.H.X., Lau C.H., Wong S.Y.S., Yeoh E.K., Griffiths S.M. Views on traditional Chinese medicine amongst Chinese population: a systematic review of qualitative and quantitative studies. Health Expect. 2014;17(5):622–636. doi: 10.1111/j.1369-7625.2012.00794.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Akers J., Aguiar-Ibáñez R., Baba-Akbari A. Centre for Reviews and Dissemination, University of York; York, UK: 2009. Systematic Reviews: CRD's Guidance for Undertaking Reviews in Health Care. [Google Scholar]
- 89.Rollnick S., Mason P., Butler C. Churchill livingstone Edinburgh; UK: 2001. Health Behavior Change: A Guide for Practitioners. [Google Scholar]
- 90.Ryan P. Integrated theory of health behavior change: background and intervention development. Clin Nurse Spec. 2009;23(3):161–172. doi: 10.1097/NUR.0b013e3181a42373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Evans J.R., Mathur A. Internet research; 2018. The Value of Online Surveys: A Look Back and a Look Ahead. Published online. [Google Scholar]
- 92.Shenton A.K. Strategies for ensuring trustworthiness in qualitative research projects. EFI. 2004;22(2):63–75. doi: 10.3233/EFI-2004-22201. [DOI] [Google Scholar]
- 93.Stewart D., Thomas B., MacLure K., et al. Perspectives of healthcare professionals in Qatar on causes of medication errors: a mixed methods study of safety culture. PLoS One. 2018;13(9) doi: 10.1371/journal.pone.0204801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Stewart D., Klein S. The use of theory in research. Int J Clin Pharm. 2016;38(3):615–619. doi: 10.1007/s11096-015-0216-y. [DOI] [PubMed] [Google Scholar]
- 95.Painter J.E., Borba C.P., Hynes M., Mays D., Glanz K. The use of theory in health behavior research from 2000 to 2005: a systematic review. Ann Behav Med. 2008;35(3):358–362. doi: 10.1007/s12160-008-9042-y. [DOI] [PubMed] [Google Scholar]
- 96.Boon H., Westlake K., Stewart M., et al. Use of complementary/alternative medicine by men diagnosed with prostate cancer: prevalence and characteristics. Urology. 2003;62(5):849–853. doi: 10.1016/s0090-4295(03)00668-x. [DOI] [PubMed] [Google Scholar]
- 97.Alderman C.P., Kiepfer B. Complementary medicine use by psychiatry patients of an Australian hospital. Ann Pharmacother. 2003;37(12):1779–1784. doi: 10.1345/aph.1C179. [DOI] [PubMed] [Google Scholar]
- 98.Visser R de, Grierson J. Use of alternative therapies by people living with HIV/AIDS in Australia. AIDS Care. 2002;14(5):599–606. doi: 10.1080/0954012021000005425. [DOI] [PubMed] [Google Scholar]
- 99.Bishop F.L., Yardley L., Lewith G. Developing a measure of treatment beliefs: the complementary and alternative medicine beliefs inventory. Compl Ther Med. 2005;13(2):144–149. doi: 10.1016/j.ctim.2005.01.005. [DOI] [PubMed] [Google Scholar]
- 100.Murray J., Shepherd S. Alternative or additional medicine? An exploratory study in general practice. Soc Sci Med. 1993;37(8):983–988. doi: 10.1016/0277-9536(93)90432-4. [DOI] [PubMed] [Google Scholar]
- 101.Boon H., Brown J.B., Gavin A., Kennard ary A., Stewart M. Breast cancer survivors' perceptions of complementary/alternative medicine (CAM): making the decision to use or not to use. Qual Health Res. 1999;9(5):639–653. doi: 10.1177/104973299129122135. [DOI] [PubMed] [Google Scholar]
- 102.Seidl M.M., Stewart D.E. Alternative treatments for menopausal symptoms. Qualitative study of women's experiences. Can Fam Physician. 1998;44:1271. [PMC free article] [PubMed] [Google Scholar]
- 103.Singh H., Maskarinec G., Shumay D.M. Understanding the motivation for conventional and complementary/alternative medicine use among men with prostate cancer. Integr Cancer Ther. 2005;4(2):187–194. doi: 10.1177/1534735405276358. [DOI] [PubMed] [Google Scholar]
- 104.George J., Kong D.C., Stewart K., Ioannides‐Demos L.L., Santamaria N.M. Use of complementary and alternative medicines by patients with chronic obstructive pulmonary disease. Med J Aust. 2004;181(5):248–251. doi: 10.5694/j.1326-5377.2004.tb06262.x. [DOI] [PubMed] [Google Scholar]
- 105.McFadden K.L., Hernández T.D., Ito T.A. Attitudes toward complementary and alternative medicine influence its use. Explore. 2010;6(6):380–388. doi: 10.1016/j.explore.2010.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Gupchup G.V., Abhyankar U.L., Worley M.M., Raisch D.W., Marfatia A.A., Namdar R. Relationships between Hispanic ethnicity and attitudes and beliefs toward herbal medicine use among older adults. Res Soc Adm Pharm. 2006;2(2):266–279. doi: 10.1016/j.sapharm.2006.02.002. [DOI] [PubMed] [Google Scholar]
- 107.McIntyre E., Saliba A.J., Wiener K.K., Bishop F.L. Predicting the intention to use herbal medicines for anxiety symptoms: a model of health behaviour. J Ment Health. 2017;28(6):589–596. doi: 10.1080/09638237.2017. [DOI] [PubMed] [Google Scholar]
- 108.General pharmaceutical Council. Standards for pharmacy professionals. 2017. https://www.pharmacyregulation.org/sites/default/files/standards_for_pharmacy_professionals_may_2017_0.pdf
- 109.Pirhonen L., Olofsson E.H., Fors A., Ekman I., Bolin K. Effects of person-centred care on health outcomes—a randomized controlled trial in patients with acute coronary syndrome. Health Pol. 2017;121(2):169–179. doi: 10.1016/j.healthpol.2016.12.003. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.