Abstract
New vaccines against tuberculosis are urgently required because of the impressive incidence of this disease worldwide and the highly variable protective efficacy of the current vaccine. The possibility of creating new live vaccines by the rational attenuation of strains from the Mycobacterium tuberculosis complex was investigated. Two auxotrophic mutants of M. tuberculosis and M. bovis BCG were constructed by disruption of one of their purine biosynthetic genes. These mutants appeared unable to multiply in vitro within mouse bone-marrow derived macrophages. They were also attenuated in vivo in the mouse and guinea pig animal models. In guinea pigs, the two mutants induced strong delayed-type hypersensitivity response to purified protein derivative. In a preliminary experiment, the two mutants were compared to the BCG vaccine for their protective efficacy in a challenge against aerosolized virulent M. tuberculosis in the guinea pig model. Both mutants conferred some level of protection. These experiments demonstrate that the rational attenuation of M. tuberculosis could lead to the design of new candidate live vaccines against tuberculosis.
Mycobacterium tuberculosis, the etiological agent of tuberculosis (TB), remains an important cause of human mortality and morbidity. Worldwide, 60 million people suffer from active TB and annually 7 million new cases arise (10). The World Health Organization estimate is about 3 million deaths per year due to TB, of which more than 95% occur in developing countries. In industrialized countries, the declining incidence which had been observed since the beginning of the century was reversed in the mid-1980s due in part to impaired social conditions and the increasing frequency of AIDS (15).
Efficient chemotherapy exists but requires lengthy and expensive treatments, making its widespread use and control difficult to achieve in developing countries. Prophylactic vaccination against TB with the attenuated strain of bovine mycobacteria, BCG (Mycobacterium bovis Bacillus Calmette-Guérin), is more cost-effective and has indeed been used worldwide. Although BCG vaccination has provided protection against TB in certain populations, the variation in efficacy of this vaccine in different field trials and its modest protective effect against the adult form of the disease (estimated by meta-analysis to be about 50%) (8) are points of major concern. These considerations have led the World Health Organization to place TB control efforts, notably through the development of new vaccines, among its top priorities.
In the recent years, considerable efforts have been made toward the identification of individual mycobacterial antigens involved in the immune response to TB (25) with the aim of developing subunit vaccines. An alternative strategy to develop novel vaccines consists of constructing mutant strains of mycobacteria that are rationally attenuated. The recent development of genetic tools for performing site-specific and random-site mutagenesis (4, 22) in organisms from the M. tuberculosis complex now renders feasible the accomplishment of such a goal. Live vaccines should have advantages over subunit vaccines in that (i) they represent a greater pool of antigens which presumably should cover a wider range of T-cell repertoires and (ii) they are generally more cost-effective to produce. Moreover, attenuated mutants of M. tuberculosis should express homologous protective antigens which other mycobacterial strains lack and thus elicit a more specific and perhaps stronger protective immune response against virulence challenge. In support of this hypothesis, the molecular analysis by Mahairas and collaborators (16) of genetic differences between M. bovis BCG and its virulent counterparts M. bovis and M. tuberculosis clearly established the existence of regions of deletion in the genome of BCG (representing about 30 kb in all), some of which contain the open reading frames encoding the highly immunogenic ESAT 6 and mpt64 antigens (the latter being absent from certain BCG strains only [21]).
Among attenuated strains of intracellular bacterial pathogens, such as salmonellae, yersiniae, brucellae, and corynebacteria (6, 9, 12, 18, 20, 23), auxotrophic mutants carrying defects in the shikimate or the purine biosynthetic pathways were shown to be of particular interest as potential live vaccines candidates because they are attenuated in vivo and have the ability to retain their immunogenicity.
In mycobacteria, the only available attenuated auxotrophs are M. bovis BCG derivatives (11, 17). A BCG auxotroph carrying a defect in the leucine biosynthetic pathway was unable to grow in C57BL/6 mice (17) and to replicate inside human THP1 macrophages (2). This mutant, as well as other leucine, methionine, and isoleucine-leucine-valine auxotrophs of BCG, were also shown to be cleared from the organs of mice with severe combined immunodeficiency disease (SCID mice); in contrast, the mice succumbed to the wild-type BCG within 8 weeks. In addition, immunization with these mutants provided BALB/c mice protection against a challenge with M. tuberculosis (11). These results led the authors to propose that the attenuated BCG strains could represent potentially safe and useful vaccines against TB for populations at risk for infection with human immunodeficiency virus. In M. tuberculosis, a leucine auxotroph was obtained by allelic exchange (1), but unlike its BCG counterpart, it showed no significant difference from the parental wild-type strain with respect to growth in SCID mice, producing a fatal infection (3).
In a previous report, we described the isolation and characterization of two genes from the M. tuberculosis purine biosynthetic pathway, purC and purL (13). We also reported the construction by allelic exchange of a purC mutant of M. tuberculosis (22). In this paper, we describe the construction of a purC mutant of M. bovis BCG and provide evidence that both the M. tuberculosis and M. bovis purine auxotrophs are affected in their survival inside mouse bone marrow macrophages and in vivo in mice and guinea pigs. The delayed-type hypersensitivity (DTH) responses to purified protein derivative (PPD) induced by both mutants in a guinea pig model was investigated at 9 weeks postvaccination. Finally, the level of protective immunity elicited by the two auxotrophs against low-dose pulmonary challenge with virulent M. tuberculosis was evaluated in a guinea pig model of TB.
MATERIALS AND METHODS
Bacterial strains and culture conditions.
Escherichia coli XL1-Blue and the mycobacterial strains M. bovis BCG strain Pasteur 1173P2, M. tuberculosis MT103 (isolated from a TB patient), and H37Rv (ATCC 27294) were cultured as previously described (22). When required, kanamycin (20 μg/ml), gentamicin (10 μg/ml), or hypoxanthine (20 μg/ml), a purine precursor, was added to the growth medium.
Plasmid construction.
Plasmid pMJ110 was constructed by inserting the 3.7-kb BamHI fragment containing purC::Km from pMJ101 into the BamHI site of pJQ200 (22). This plasmid is unable to replicate in mycobacteria. Plasmid pMJ111 was created by excising the 1,090-bp EcoRV-HincII fragment from plasmid pMJ1, harboring the purC gene flanked by 120 bp upstream and 80 bp downstream, and cloning it into plasmid pOMK (13). pMJ111 is able to replicate in mycobacteria.
Preparation and infection of mouse bone marrow macrophages.
Bone marrow cells were flushed from the femurs of 7- to 8-week-old BALB/c mice (purchased from Iffa Credo, l’Arbresle, France) and suspended in Dulbecco medium with low glucose (1 g/liter) and high carbonate (3.7 g/liter) concentrations (Gibco BRL) and enriched with 10% heat-inactivated fetal calf serum (Dominique Dutscher), 10% L-cell conditioned medium, and 2 mM glutamine. For the infection assays, mouse bone marrow macrophages were seeded in eight-well Lab-Tek chamber slides (Nalgene Nunc International) (5 × 104 cells/well) and infected with bacterial suspensions of either MT103, BCG 1173P2, MYC1551, or MYC1552 at a multiplicity of infection of 1:1. Cultures were incubated at 37°C in a 5% CO2 atmosphere. After 18 h, infection was terminated by removing the overlaying medium and washing each well three times with 500 μl of Hanks’ buffered salt solution (Gibco BRL) before adding 400 μl of fresh culture medium per well. At days 1 (18 h), 4, 7, and 11, the number of intracellular CFU was evaluated by plating appropriate dilutions of lysed macrophages (in cell culture lysis reagent [Promega]) onto 7H10 or 7H10 supplemented with hypoxanthine. At each time point, a Lab-Tek chamber slide containing infected macrophages and cultivated in the same conditions was subjected to staining for acid-fast bacilli in order to check macrophage viability. This infection experiment was carried out in duplicate.
Mycobacterial multiplication in mice.
C57BL/6j or BALB/c female mice (6 to 8 weeks old; purchased from CERJ, Le Genest St Isle, France, or Iffa Credo) were infected intravenously either with 105 CFU of MYC1551 and MT103 or with 107 CFU of MYC1552 and BCG in 0.5 ml of phosphate saline buffer. At every time point, mice were euthanized with CO2, and the spleen, lung, and liver were removed aseptically and homogenized either manually, using two glass slides (for the spleen and lung), or in a Stomacher 80 (Seward) homogenizer (for the liver). Bacteria in the organs of infected animals were enumerated by plating 10-fold serial dilutions of organ homogenates onto 7H11 medium (supplemented with hypoxanthine for the auxotroph mutants). The data were expressed as the geometric means ± standard errors of the means (SEM) of counts obtained with five to six mice.
Vaccination, challenge, and necropsy of guinea pigs.
Male and female outbred Hartley strain guinea pigs (Charles River Laboratories, Inc., Wilmington, Mass.) were used. Guinea pigs were injected subcutaneously into the inguinal region with approximately 107 CFU of either wild-type BCG, the corresponding BCG auxotrophic strain MYC1552, or the M. tuberculosis auxotrophic mutant MYC1551 in a volume of 0.2 ml. Three, six, and nine weeks postvaccination, three animals from each of the three vaccine groups were euthanized. The number of viable mycobacteria carried by one-half of the spleen and the right lower lobe of the lung was determined by inoculating appropriate dilutions of organ homogenates onto duplicate 7H10 plates supplemented with hypoxanthine. Nine weeks postvaccination, all animals were infected via the respiratory route with an infecting inoculum of viable H37Rv (empirically adjusted to result in the inhalation of 5 to 10 viable organisms per animal) by use of an aerosol chamber as previously described (24). Five weeks after respiratory challenge, animals were euthanized, and the spleen and right lower lobe of the lung were removed for bacterial culture.
Tuberculin skin test.
The DTH reaction was evaluated by the intradermal injection of 0.1 ml of PPD containing 100 tuberculin units (RT-23; Statens Seruminstitut) on a shaved area of the abdomen. The mean diameter of induration was measured in millimeters and recorded 24 h later.
Statistical methods.
Analysis of variance was used to test the effects of vaccination on tissue bacterial load. When significant treatment effects were indicated, differences between means were assessed by Duncan’s multiple-range test. A 95% confidence level was set for all tests. All analyses were performed with PC SAS 6.12 (SAS Institute, Cary, N.C.).
RESULTS
Construction of purC mutants of M. bovis BCG and M. tuberculosis.
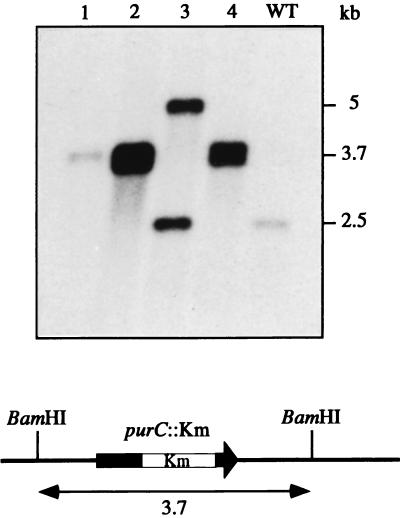
An M. bovis BCG purC mutant was obtained by using a classical allelic exchange procedure consisting in the transformation of the wild-type strain M. bovis BCG 1173P2 with a suicide vector carrying a disrupted copy of the purC gene (purC::Km) and selecting for kanamycin-resistant (Kmr) transformants on 7H10 plates containing kanamycin and hypoxanthine. M. bovis BCG 1173P2 was electroporated by using 2 μg of plasmid pMJ110. Two Kmr transformants were obtained. Their genomic DNAs were extracted and analyzed by Southern blotting using the purC gene as a probe (Fig. 1). One of the two clones exhibited the correct hybridization pattern for an allelic exchange mutant. The other one corresponded to the wild type and was probably a Kmr mutant of M. bovis BCG. The candidate clone was phenotypically tested. As expected, it required purines or hypoxanthine (a precursor of purine bases) to grow on 7H9 or 7H10 (Fig. 2). This mutant was renamed MYC1552.
FIG. 1.
Southern blot analysis and hybridization profile of the M. bovis BCG purC mutant. The hybridization profiles of the DNA of Kmr transformants obtained in two independent experiments are shown. Lane 1 corresponds to the M. bovis BCG purC mutant MYC1552; lanes 2 to 4 correspond to transformants which have undergone a single crossover event at the purC locus in another experiment; lane 5 is the wild-type (WT) strain M. bovis BCG 1173P2. Chromosomal DNA were digested with BamHI and probed for hybridization with the purC gene (1,090-bp EcoRV-HincII fragment from pMJ1).
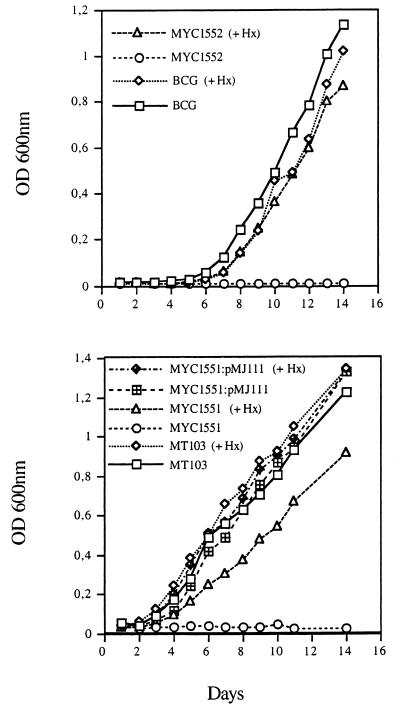
FIG. 2.
Growth kinetics of MYC1552, MYC1551, MYC1551(pMJ111), and their wild-type counterparts grown in 7H9 medium in the absence or presence of the purine precursor hypoxanthine. The different strains were grown in 7H9 medium (supplemented with hypoxanthine for MYC1551 and MYC1552) to an optical density at 600 nm (OD600) of close to 1. These cultures were diluted in fresh medium in the absence or presence of hypoxanthine (Hx) to reach an OD600 of 0.01 and then incubated at 37°C with 5% CO2. Growth of the strains was monitored by measuring the OD600 of the cultures every day.
The purC mutant of M. tuberculosis MT103, named MYC1551, was obtained as described by Pelicic et al. (22). Like MYC1552, MYC1551 is dependent on the presence of purines or hypoxanthine in the medium to multiply (Fig. 2).
Evaluation of the reversion frequency of MYC1551 and MYC1552.
To estimate the stability of the mutation introduced by allelic exchange in M. bovis BCG and M. tuberculosis, cultures of MYC1551 and MYC1552 grown in 7H9 containing kanamycin were plated on 7H10 with kanamycin and hypoxanthine or 7H10 alone. In all the experiments (repeated independently four and two times for MYC1552 and MYC1551, respectively), no CFU was detected on 7H10 whereas 2 × 108 and 4 × 108 CFU in all were obtained for MYC1551 and MYC1552, respectively, on 7H10 supplemented with hypoxanthine and kanamycin. Therefore, the reversion frequency was estimated to be lower than 10−8 events per cell and per generation. The same experiment was repeated with cultures grown in 7H9 liquid medium without kanamycin, and the same results were obtained.
Growth characteristics of the purine auxotrophs in macrophages.
The ability of the purine auxotrophs to persist and multiply within bone marrow macrophages from C57BL/6j mice was evaluated. Macrophages (5 × 104) were infected at a multiplicity of infection, of close to 1 with the parental and the mutant strains. Over a period of 15 days, the infection was followed by counting the viable bacteria (Fig. 3).
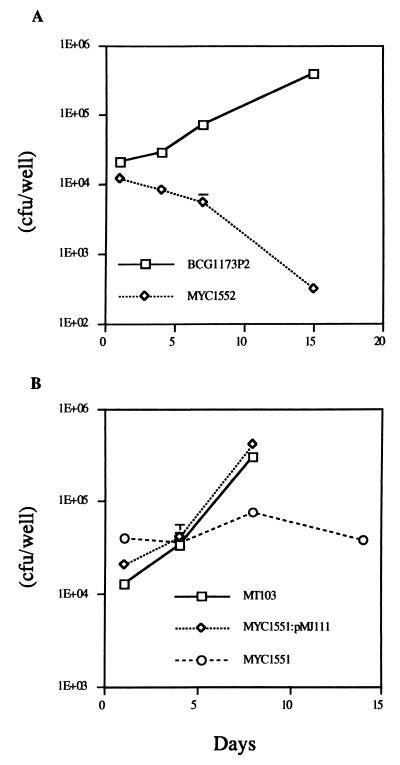
FIG. 3.
Persistence of MYC1551 and MYC1552 within bone marrow macrophages. In this representative experiment, 5 × 104 macrophages were infected with 5 × 104 viable bacilli and growth was measured over time. (A) M. bovis BCG 1173P2 or the BCG auxotroph (MYC1552) was used to infect the macrophages. (B) An M. tuberculosis virulent strain (MT103), its auxotroph counterpart (MYC1551), or MYC1551 harboring plasmid pMJ111 (carrying the purC gene) was used to infect the macrophages. Each point represents the geometric mean ± SEM of six (experiment with M. bovis BCG) or four (experiment with M. tuberculosis) independent cultures.
M. tuberculosis MT103 and M. bovis BCG 1137P2 multiplied within the macrophage with apparent doubling times of 36 and 59 h, respectively. At 8 days postinfection, macrophages were packed with M. tuberculosis, and most of them lysed. With M. bovis BCG, the infection was followed for 15 days without apparent lysis of the macrophages. The purine auxotrophs exhibited growth characteristics totally different from those of their parental strains. In both cases, infections were contained. The M. tuberculosis purC mutant MYC1551 persisted, but the number of viable bacteria did not increase. The M. bovis BCG purC mutant MYC1552 was gradually eliminated, and after 15 days less than 3% of the inoculum was still viable. These results demonstrate that disruption of the purC gene alters the ability of M. tuberculosis and M. bovis BCG to multiply within mouse bone marrow macrophages.
To confirm that this phenotype was due to the mutation of the purC gene and not to a polar effect of the kan gene insertion, a complementation experiment was performed. Plasmid pMJ111 containing purC was electrotransferred into MYC1551. Transformants no longer required purines to grow in 7H9 or 7H10 (Fig. 2). MYC1551 (pMJ111) was used to infect macrophages (Fig. 3B). As expected, the presence of purC on the plasmid fully restored the ability of MYC1551 to multiply within macrophages.
Persistence of the auxotroph mutants and their parental counterparts in mice.
M. tuberculosis (105 CFU) and M. bovis BCG (107 CFU) were used to infect BALB/c mice intravenously. The mice were killed at different time points, and viable bacteria in the liver, spleen, and lung were counted (Fig. 4 and 5).
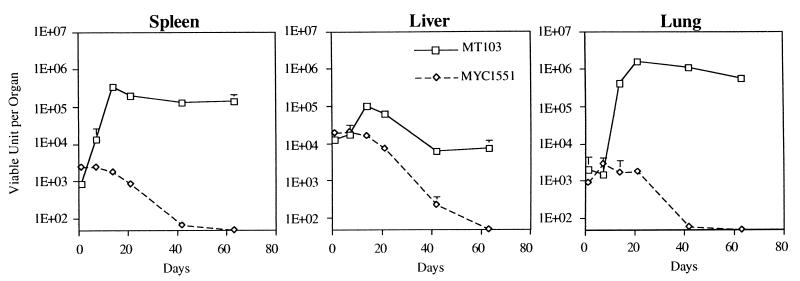
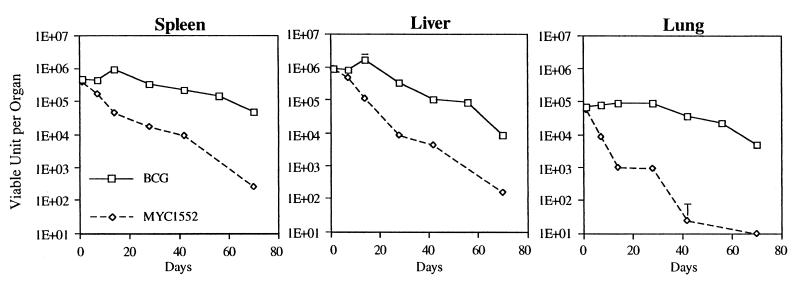
FIG. 4.
Persistence of M. tuberculosis MT103 and the purine auxotroph MYC1551 in mice. BALB/c mice were infected intravenously with 107 viable units of either an M. tuberculosis virulent strain (MT103) or MYC1551, and the persistence of bacteria in three organs was measured over time. Each value represents the geometric mean ± SEM obtained with five different mice.
FIG. 5.
Persistence of M. bovis BCG and its auxotroph counterpart, MYC1552, in mice. BALB/c mice were infected intravenously with 107 viable units of either M. bovis BCG or MYC1552, and the persistence of bacteria in three organs was measured over time. Each value represents the geometric mean + SEM obtained with five different mice.
For wild-type M. tuberculosis (Fig. 4), there was a large increase in the number of CFU in the three organs during the first 2 or 3 weeks: 2.5 logs in the spleen (day 14), 1 log in the liver (day 14), and 3 logs in the lung (day 21). At this time, the infection was controlled; the bacillary load was stabilized in both the lung and the spleen at 106 and 105 CFU per organ, respectively. In the liver, the bacterial burden decreased to reach a plateau at 104 CFU. For the M. tuberculosis purine auxotroph MYC1551, the situation was quite different. The initial multiplication was dramatically reduced, with less than 0.5-log increase in every organ at the peak occurring at day 7. The bacilli were then gradually eliminated from the three organs, becoming undetectable at day 63.
For BCG (Fig. 5), the initial multiplication was slower than for M. tuberculosis: only 0.5-log increase in the spleen at day 14 and almost no multiplication in the lung and the liver. From day 14 in both the liver and the spleen and from day 28 in the lung, the number of viable bacilli decreased gradually, reaching 5 × 103, 104, and 5 × 104 in the lung, liver, and spleen, respectively, at day 70, when the experiment was stopped. With the BCG auxotroph (MYC1552), the number of bacilli began to decrease immediately after the infection, and no bacteria were recovered from the lung at day 70. In the spleen and the liver, a few colonies were recovered at day 70, when the experiment was stopped.
These results established that the mutations in the purC gene of both BCG and M. tuberculosis attenuated the virulence of these strains in the mouse model. The experiment was repeated with a second susceptible mouse line, C57BL/6, with M. tuberculosis MT103 and MYC1551 but without any differences noted. MYC1551 and MYC1552 were eliminated very efficiently, becoming almost undetectable at the end of the experiment (day 63 for M. tuberculosis and day 70 for BCG). However, they persisted for a while since bacteria were recovered from every organ during the first 6 weeks. The main difference in the behavior of the two purine auxotrophs thus appears in the first week postinfection. While the M. tuberculosis purC mutant MYC1551 increased slightly in every organ tested, the M. bovis BCG purC mutant MYC1552 began to decline immediately after the infection. After this short lag time, MYC1551 was cleared as efficiently as MYC1552.
DTH induced by the purine auxotrophs and protective efficacy in the guinea pig model.
To evaluate the protective efficacy of the purine auxotrophs, the guinea pig was chosen because it is much more susceptible to M. tuberculosis infection than the mouse. Furthermore, BCG protection is easier to demonstrate in the guinea pig. While a maximum of 1 log of difference in the CFU number can be obtained in the lung and spleen of unimmunized compared to BCG-vaccinated mice, differences of 1 to 2 logs in the lung and 4 logs in the spleen are often obtained between naive and BCG-vaccinated guinea pigs following low-dose aerosol challenge (19).
Outbred Hartley strain guinea pigs were inoculated subcutaneously with 107 CFU of either BCG 1173P2, MYC1552, or MYC1551. Three animals from each treatment group were euthanized at 3, 6, and 9 weeks postinfection. The number of viable mycobacteria was determined in one half of the spleen and the right lower lobe of the lung. Three weeks postinfection, 870 ± 651 CFU of BCG 1173P2 was found in the spleens of three guinea pigs. In contrast, 90 CFU was recovered from only one of three guinea pigs infected with MYC1551, and no bacteria were found in any of the animals vaccinated with MYC1552. Six and nine weeks postinfection, no bacillus was recovered from the spleens of any animal of any of the three treatment groups. At no time point were bacilli recovered from the lungs of any vaccinated animal. These results show that the purine auxotrophs are attenuated even in the highly susceptible guinea pig as well as they were in the mouse model.
The cutaneous DTH response to PPD was evaluated 9 weeks postvaccination. All of the vaccinated animals exhibited a detectable skin test reaction against tuberculin (Table 1). The mean induration diameters, measured 24 h following the intradermal injection, were 13.9 ± 0.9, 15.5 ± 1.0, and 11.1 ± 2.2, respectively, for the BCG-, MYC1552-, and MYC1551-infected guinea pigs.
TABLE 1.
Tuberculin skin test on guinea pigs injected via the intradermal route with 100 tuberculin units 9 weeks postinfectiona
| Vaccination group | Induration diam (mm)
|
|
|---|---|---|
| Individual determinations | Mean ± SEM | |
| BCG | 13.0, 12.5, 17.5, 13.5, 13.0 | 13.9 ± 0.9 |
| MYC1552 | 16.0, 17.0, 13.5 | 15.5 ± 1.0 |
| MYC1551 | 5.0, 12.0, 18.5, 11.0, 9.0 | 11.1 ± 2.2 |
In all cases, the control group exhibited no reaction.
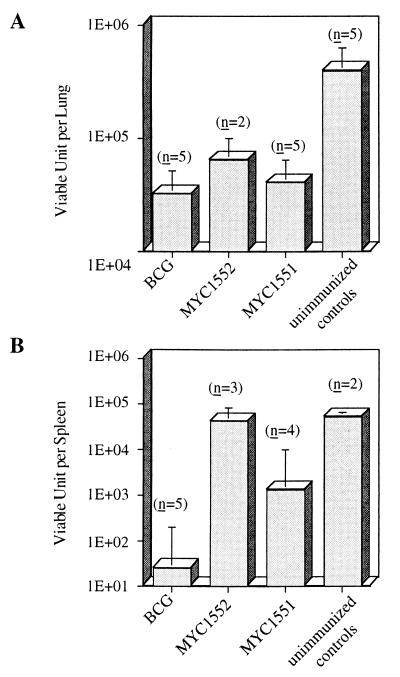
Nine weeks postvaccination, the remaining animals were infected via the aerosol route with a dose empirically adjusted to result in the inhalation of 5 to 10 viable M. tuberculosis H37Rv bacilli per animal. Five weeks later, viable M. tuberculosis were recovered quantitatively from the spleen and the lung (Fig. 6). In the lung, both MYC1551 and MYC1552 exhibited a level of protection comparable with the one obtained with BCG 1173P2, namely, 1 log of difference in the CFU count between the vaccinated and unimmunized animals. As expected, vaccine-induced protection was most visible in the spleen. M. tuberculosis purC mutant MYC1551 seemed to induce some level of protection, while there was no difference in unimmunized and M. bovis BCG purC mutant-vaccinated animals.
FIG. 6.
Protective efficacy of the different vaccine strains against low-dose pulmonary challenge in guinea pigs. Nine weeks postvaccination, guinea pigs were infected via the aerosol route with 5 to 10 viable M. tuberculosis organisms. Five weeks later, these animals were euthanized and the the number of CFU of M. tuberculosis was evaluated in the lung (A) and the spleen (B). The CFU-per-organ values indicated are the geometric means + SEM; n is the number of animals used.
The Duncan multiple-range test indicated that there was no significant difference in the number of tubercle bacilli recovered from the lung between different groups of vaccinated animals but that the difference between vaccinated and nonvaccinated groups was statistically significant (P < 0.05). In the spleen, the number of mycobacteria in BCG-vaccinated animals was significantly lower than the number in MYC1552-vaccinated and unimmunized controls and lower (although not significantly due to the heterogeneity of the guinea pig responses to infection in every vaccination group) than the number of mycobacteria recovered from MYC1551-vaccinated animals.
DISCUSSION
With the goal of developing a novel vaccine against TB, we constructed and evaluated the attenuation and protective efficacy of purC auxotroph mutant strains of M. tuberculosis and M. bovis BCG carrying a defect in the purine biosynthetic pathway. This approach was justified by the fact that attenuated strains are generally more potent than nonliving vaccines in stimulating cell-mediated immune responses which are effective against intracellular pathogens (7) and because, in theory, they produce most of the antigens normally expressed in vivo by the pathogens. Thus, immune responses are stimulated in ways which closely resemble those detected during normal infection. Moreover, by constructing an auxotrophic strain derived from M. tuberculosis, one would derive a vaccine candidate antigenically identical to the pathogen against which protection was desired.
As shown for other purine auxotrophs of intracellular pathogens which reside inside vacuoles (9, 18, 20), M. tuberculosis (MYC1551) and M. bovis BCG (MYC1552) purine-deficient mutants were attenuated both in an in vitro macrophage model and in vivo in mice and guinea pigs. Since the introduction of the purC gene on a plasmid into the M. tuberculosis auxotroph fully restores its ability to replicate and lyse the macrophages, one can conclude that restriction for growth inside these cells is due to the insertional disruption of the purC gene alone and not to polarity affecting the expression of adjacent genes.
In contrast to what was observed with their respective parental strains, the number of MYC1551 CFU in mouse bone marrow macrophages did not increase over a 15-day period of time but remained approximately constant, whereas the number of MYC1552 CFU steadily decreased from the first day postinfection. In the absence of purine bases in the medium, most likely resembling the situation within the phagosomal compartment, both auxotrophs were unable to multiply (Fig. 2). Thus, this difference in intracellular persistence between MYC1551 and MYC1552 probably reflects the different abilities of these M. tuberculosis and M. bovis BCG derivatives to resist phagocytic cells defenses and/or to make the phagosome in which they reside more hospitable.
The behavior of the auxotrophs in mice reflects the results obtained in isolated macrophages: the M. tuberculosis auxotroph MYC1551 was progressively eliminated after a lag period of 2 to 3 weeks during which the number of CFU in all organs remained almost constant, whereas elimination of the M. bovis BCG purC mutant MYC1552 began immediately after the infection. Overall, both strains were eliminated at about the same rate from mice. In guinea pigs, fewer MYC1551 than BCG and no MYC1552 were found in the spleens 3 weeks postimmunization. Finally, based on data obtained from the macrophage and guinea pig experiments in which the same infecting doses were used for all strains, it seems that both MYC1551 and MYC1552 are more attenuated than BCG.
The results of the protection studies, although preliminary because of the limited number of animals studied, indicated that all three strains (BCG, MYC1551, and MYC1552) had equal protective effects against an aerosol challenge with virulent M. tuberculosis H37Rv, as assessed by the reduction in CFU in the lungs of vaccinated guinea pigs. In the spleen, where more extensive protection is obtained, MYC1551 seemed to induce a protective effect compared to results for unimmunized controls, although it seemed slightly less efficient than that conferred by BCG. In the same organ, MYC1552 seemed to induce no protective response at all. The finding that MYC1552 shows a protective effect in the lungs but not in the spleen, unlike its M. tuberculosis counterpart and BCG, which show protective efficacy in both organs, could reflect the inability of the BCG auxotroph to control the dissemination of M. tuberculosis H37Rv following the aerosol infection and, thus, its inability to stimulate protective immunity with the same efficiency as the two other immunizing strains.
All three strains elicited strong DTH responses 9 weeks postinfection, suggesting that both auxotrophs are able to induce cell-mediated immune responses as does the BCG vaccine. Therefore, the differences in the protective efficacies of BCG, MYC1551, and MYC1552 may have resulted from differences in the quality of the cellular immune responses that they induce rather than in their ability to induce such responses. In fact, it is probable that an attenuated strain of mycobacteria needs to retain a limited ability to multiply in host cells and to disseminate and persist within the host in order to be able to induce protective immune responses. This idea was originally pointed out by Kanai’s work (14), in which the protective efficacy of a streptomycin-dependent strain of M. tuberculosis was evaluated in guinea pigs and mice. In this system, streptomycin was used to induce the multiplication of the immunizing strain prior to challenge with virulent H37Rv tubercle bacilli. Experiments showed that only the M. tuberculosis that had multiplied during the immunization period conferred protection to the animals, with nonmultiplying bacteria displaying poor protection.
Thus, the way an attenuated strain establishes an infection in the host, probably more than persistence in itself, seems to be important for inducing protective immune responses. These observations highlight the difficulty inherent in using live vaccines to reach the right balance between attenuation and immunogenicity, since overattenuated bacteria may not produce in vivo some key antigens necessary for the induction of a protective immunity. The physiological state of the mutant bacilli might also influence the way their antigens are processed inside the macrophage and, thus, presented to the T lymphocytes.
Finally, this work provides evidence that rationally attenuated strains of M. tuberculosis can protect guinea pigs against pulmonary tuberculosis.
In further experiments with the MYC1551 and MYC1552 auxotrophs, it will be important to test whether immunizing the guinea pigs with higher doses of bacteria (108 CFU, for example) or with two or three doses of 107 CFU (injected 1 or 2 weeks apart) can improve the protective immune response that they induce. It will also be important to test whether MYC1551 and MYC1552 induce long-term protection by performing the aerosol challenge with virulent M. tuberculosis 4 or 6 months postimmunization. Also of great interest would be to evaluate the protective efficacy of the M. tuberculosis attenuated strains not only in the guinea pig model of tuberculosis but also in other models in which the BCG appears to be less potent and where improvements are thus required, such as models reflecting the case of individuals frequently exposed to environmental mycobacteria or developing TB from the reactivation of dormant bacilli.
ACKNOWLEDGMENTS
This work was supported by the Institut Pasteur, by European Economic Community grant BMH4-CT97-2134, and by NIH grant AI 35207. M.J. is a recipient of a Fondation Mérieux grant.
REFERENCES
- 1.Balasubramanian V, Pavelka M S, Bardarov S S, Martin J, Weisbrod T R, McAdam R A, Bloom B R, Jacobs W R., Jr Allelic exchange in Mycobacterium tuberculosis with long linear recombination substrates. J Bacteriol. 1996;178:273–279. doi: 10.1128/jb.178.1.273-279.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bange F C, Brown A M, Jacobs W R., Jr Leucine auxotrophy restricts growth of Mycobacterium bovis BCG in macrophages. Infect Immun. 1996;64:1794–1799. doi: 10.1128/iai.64.5.1794-1799.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bange F C, Mazzaccaro R J, Balasubramanian V, Bloom B R, Jacobs W R., Jr . Abstracts of the Third International Conference on the Pathogenesis of Mycobacterial Infection, Stockholm, Sweden. 1996. Leucine auxotrophy restricts growth of Mycobacterium bovis BCG but does not affect growth of Mycobacterium tuberculosis in SCID mice; p. 33. [Google Scholar]
- 4.Bardarov S, Kriakov J, Carriere C, Yu S, Vaamonde C, McAdam R A, Bloom B R, Hatfull G F, Jacobs W R., Jr Conditionally replicating mycobacteriophages: a system for transposon delivery to Mycobacterium tuberculosis. Proc Natl Acad Sci USA. 1997;94:10961–10966. doi: 10.1073/pnas.94.20.10961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bartow R A, McMurray D N. Vaccination with Mycobacterium bovis BCG affects the distribution of Fc receptor-bearing T lymphocytes in experimental pulmonary tuberculosis. Infect Immun. 1989;57:1374–1379. doi: 10.1128/iai.57.5.1374-1379.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bowe F, O’Gaora P, Maskell D, Cafferkey M, Dougan G. Virulence, persistence, and immunogenicity of Yersinia enterolitica O:8 aroA mutants. Infect Immun. 1989;57:3234–3236. doi: 10.1128/iai.57.10.3234-3236.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brown F, Dougan G, Hoey E M, Martin S J, Rima B K, Trudgett A. Vaccine design. Chichester, England: John Wiley & Sons; 1993. [Google Scholar]
- 8.Colditz G A, Brewer T F, Berkey B S, Wilson M E, Burdick E, Fineberg H V, Mosteller F. Efficacy of BCG vaccine in the prevention of tuberculosis. JAMA. 1994;271:698–702. [PubMed] [Google Scholar]
- 9.Crawford R M, van der Verg L, Yuan L, Hadfield T L, Warren R L, Drazek E S, Houng H S H, Hammack C, Sasala K, Polsinelli T, Thompson J, Hoover D L. Deletion of purE attenuates Brucella melitensis infection in mice. Infect Immun. 1996;64:2188–2192. doi: 10.1128/iai.64.6.2188-2192.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dolin P J, Raviglione M C, Kochi A. Global tuberculosis incidence and mortality during 1990–2000. Bull W H O. 1994;72:213–220. [PMC free article] [PubMed] [Google Scholar]
- 11.Guleria I, Teitelbaum R, McAdam R A, Kalpana G, Jacobs Jr W R, Bloom B R. Auxotrophic vaccines for tuberculosis. Nat Med. 1996;2:334–337. doi: 10.1038/nm0396-334. [DOI] [PubMed] [Google Scholar]
- 12.Hoiseth S K, Stocker B A D. Aromatic dependent Salmonella typhimurium are non-virulent and effective as live vaccines. Nature. 1981;291:238–239. doi: 10.1038/291238a0. [DOI] [PubMed] [Google Scholar]
- 13.Jackson M, Berthet F X, Otal I, Rauzier J, Martin C, Gicquel B, Guilhot C. The Mycobacterium tuberculosis purine biosynthetic pathway: isolation and characterization of the purC and purL genes. Microbiology. 1996;142:2439–2447. doi: 10.1099/00221287-142-9-2439. [DOI] [PubMed] [Google Scholar]
- 14.Kanai K. Experimental studies on host-parasite equilibrium in tuberculosis infection, in relation to vaccination and chemotherapy. Jpn J Med Sci Biol. 1966;19:181–199. doi: 10.7883/yoken1952.19.181. [DOI] [PubMed] [Google Scholar]
- 15.Kaufmann S H E, van Embden J D A. Tuberculosis: a neglected disease strikes back. Trends Microbiol. 1993;1:2–5. doi: 10.1016/0966-842x(93)90015-j. [DOI] [PubMed] [Google Scholar]
- 16.Mahairas G G, Sabo P J, Hickey M J, Singh D C, Stover K. Molecular analysis of genetic differences between Mycobacterium bovis BCG and virulent M. bovis. J Bacteriol. 1996;178:1274–1282. doi: 10.1128/jb.178.5.1274-1282.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McAdam R A, Weisbrod T R, Martin J, Scuderi J D, Brown A M, Cirillo J D, Bloom B R, Jacobs W R., Jr In vivo growth characteristics of leucine and methionine auxotrophic mutants of Mycobacterium bovis BCG generated by transposon mutagenesis. Infect Immun. 1995;63:1004–1012. doi: 10.1128/iai.63.3.1004-1012.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McFarland W C, Stocker B A D. Effect of different purine auxotrophic mutations on mouse-virulence of a Vi-positive strain of Salmonella dublin and of two strains of Salmonella typhimurium. Microb Pathog. 1987;3:129–141. doi: 10.1016/0882-4010(87)90071-4. [DOI] [PubMed] [Google Scholar]
- 19.McMurray D N. Guinea pig model of tuberculosis. In: Bloom B R, editor. Tuberculosis: pathogenesis, protection, and control. Washington, D.C: American Society for Microbiology; 1994. pp. 135–147. [Google Scholar]
- 20.O’Callaghan D, Maskell D, Liew F Y, Easmon C S F, Dougan G. Characterization of aromatic- and purine-dependent Salmonella typhimurium: attenuation, persistence, and ability to induce protective immunity in BALB/c mice. Infect Immun. 1988;56:419–423. doi: 10.1128/iai.56.2.419-423.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Oettinger T, Andersen A B. Cloning and B-cell-epitope mapping of MPT64 from Mycobacterium tuberculosis H37Rv. Infect Immun. 1994;62:2058–2064. doi: 10.1128/iai.62.5.2058-2064.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pelicic V, Jackson M, Reyrat J M, Jacobs W R, Gicquel B, Guilhot C. Efficient allelic exchange and transposon mutagenesis in Mycobacterium tuberculosis. Proc Natl Acad Sci USA. 1997;94:10955–10960. doi: 10.1073/pnas.94.20.10955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Simmons C P, Hodgson A L M, Strugnell R A. Attenuation and vaccine potential of aroQ mutants of Corynebacterium pseudotuberculosis. Infect Immun. 1997;65:3048–3056. doi: 10.1128/iai.65.8.3048-3056.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wiegeshaus E H, McMurray D N, Grover A A, Harding G E, Smith D W. Host-parasite relationships in experimental airborne tuberculosis. III. Relevance of microbial enumeration to acquired resistance in guinea pigs. Am Rev Respir Dis. 1970;102:422–429. doi: 10.1164/arrd.1970.102.3.422. [DOI] [PubMed] [Google Scholar]
- 25.Young D B, Kaufmann S H E, Hermans P W M, Thole J E R. Mycobacterial protein antigens: a compilation. Mol Microbiol. 1992;6:133–145. doi: 10.1111/j.1365-2958.1992.tb01994.x. [DOI] [PubMed] [Google Scholar]