Abstract
Background:
Irritable bowel syndrome (IBS) is a highly prevalent disorder of the gut interaction characterized by abdominal discomfort and pain associated with altered bowel habits in the absence of structural abnormalities. In spite of IBS' high prevalence and disease burden across the globe, no explanations have been given as to its underlying pathophysiology. As for the treatment of IBS, there is no specific medication, and the most beneficial treatment is usually supportive therapy. Recent animal and human studies have demonstrated the therapeutic potential of curcumin or turmeric in the treatment of IBS.
Methods:
We systematically reviewed all available evidence supporting curcumin and turmeric's therapeutic potential in relieving IBS symptoms in the present study. For this purpose, a database search was performed using curcumin, turmeric, and IBS and all their equivalents as of the search terms in Web of Science, Pub-Med, Scopus, Ovid, Embase, and Google Scholar from1990 up to Feb 2021. The investigation was then limited to clinical trials, and then nine articles were collected for data analysis.
Results:
The findings of the included literature showed that curcumin and turmeric alone or in combination with other medications could improve the severity of IBS as well as the quality of life among people who suffer from IBS symptoms.
Conclusion:
Overall, medications containing curcumin and turmeric extract due to these compounds' anti-inflammatory effects may improve IBS symptoms, particularly abdominal pain and life quality.
Keywords: Irritable bowel syndrome, Curcumin, Turmeric, Curcuma longa, Gastrointestinal disorders
Introduction
Irritable bowel syndrome (IBS) is a functional bowel disorder characterized by chronic abdominal pain and bloating that affects the large intestine. Besides abdominal pain, the most common IBS symptoms include cramping, diarrhea or constipation, or even both in some circumstances (1).
Symptoms of IBS may change over time, and the severity of the symptoms may also vary. Although community-based studies have shown that the prevalence of IBS increases with age, the disease is more common in young people. According to community-based studies, the prevalence of IBS is 13–26% among the different populations (2). The prevalence of IBS is almost twice greater in females (3). Despite the inconvenience, IBS does not usually lead to serious complications; however, it can seriously impact a patient’s daily activities and quality of life (4, 5).
Foods and hormones and genetic and environmental factors such as stress may be involved in the onset or exacerbation of IBS. Psychological and emotional factors may play a significant role in IBS (6).
Common food stimulants that may lead to IBS include beans, celery, onions, carrots, raisins, bananas, apricots, plums, Brussels sprouts, dairy products, chocolates, and caffeinated products. Because the nervous system and gastrointestinal system are involved in the pathobiology of IBS, there is no specific treatment for this condition, and most of the therapeutic management is supportive or based on diet therapy (7, 8).
Many in vitro and in vivo studies have shown that herbal medicines may be a safe therapeutic option for managing digestive and nervous system disorders (9, 10). Turmeric (Curcuma longa) is one of the medicinal plants used in traditional medicine to treat gastrointestinal diseases, including IBS (11). This product contains compounds that have medicinal properties and are known as curcuminoids. Curcumin is the most crucial compound and the active ingredient in turmeric, responsible for the yellow color turmeric. It is known as a powerful antioxidant and for strong anti-inflammatory properties.
Traditional medicine has recommended turmeric for a wide range of health conditions, including chronic pain and inflammation. Due to its anti-inflammatory properties, we believe that curcumin or turmeric may help manage IBS and the associated symptoms. Hence, the present article aimed to systematically review all available scientific and population-based documents about the efficiency of this herbal product in the treatment of IBS. To date, this is the first study aiming at comprehensively reviewing and collecting all available literature on the efficiency of turmeric in patients with IBS.
Methods
Database search and inclusion criteria
The present study aimed to review the evidence for potential therapeutic effects of curcumin or turmeric in treatment or relieving IBS symptoms. For this purpose, a systematic search was performed for articles in Web of Science, PubMed, Scopus, Ovid, Embase, and Google Scholar 1990 up to Feb 2021. The search terms used for this purpose were “curcumin or turmeric” and “IBS,” including all their equivalents. The search was first limited to clinical trials. Afterward, English articles were selected for further evaluation, but items with other languages were also included if the report contained English abstract and the provided data were enough and extractable. Likewise, irrelevant documents were excluded from further assessment. Two authors performed all the procedures, including article search and selection, and possible disagreement between the authors was resolved in each step.
The study protocol followed the recommendations of the PRISMA checklist 2009 (12, 13).
Data synthesis
The information from collected articles, including the author’s name, date, types of study, dosage, and medication formula, were extracted and summarized for data synthesis. Moreover, the measured variables and the primary outcomes in each study were extracted. The most critical variables assessed in the literature include quality of life, severity score, IBS symptom, discomfort, gut microbiota profile, abdominal pain, and the number of pain locations. Moreover, some studies reported anxiety and depression, compliance, self-reported effectiveness, and safety as secondary outcomes. In the majority of the articles, the severity score and the diagnosis of the disease were based on ROME-II and III criteria for IBS and radiography and clinical evaluation. The Rome criteria are an international standard for diagnosis, treatment, and functional gastrointestinal disorders, including IBS. The diagnostic algorithm may include additional tests to minimize the diagnostic errors and prevent other diseases from being recognized as IBS (14, 15).
Quality assessment
Two quality assessment scales recommended to verify the quality of randomized controlled trials were used for quality evaluation of the included articles. For this purpose, Newcastle-Ottawa and Oxford quality scoring systems (generally known as the Jadad scale) were used. In the Newcastle-Ottawa scoring system, there are three different parts with overall eight questions (maximum nine stars) that scores each article based on “selection,” “comparability,” and “outcome.” In the Oxford quality scale, five questions indicate the studies’ randomization, blinding, and follow-up, wherein a survey with a score ≥of 3 of 5 is of high quality. For quality assessment, a star is given for each numbered item. An article with appropriate design and reports can obtain a maximum of 9 and 5 stars on Newcastle-Ottawa and Jadad scales, respectively.
Results
Literature search results
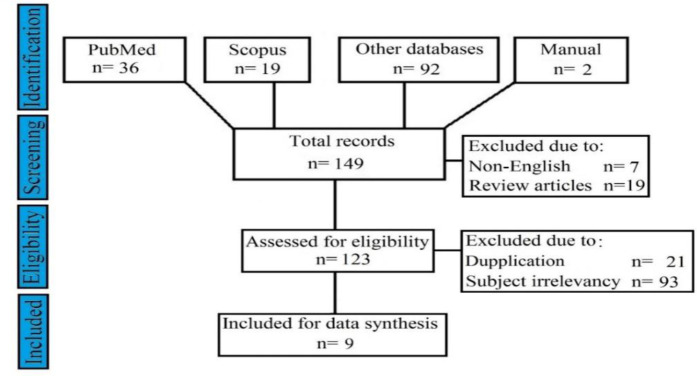
Of 149 articles achieved in the first step of database search, 19 studies were found in Scopus, and 36 pieces were from PubMed. Additional 92 items were also found through a search in other databases. Two articles were also found through manual reference list screening of the previously included articles. After limiting the records to clinical trials and removing irrelevant articles, nine articles were achieved, and their full texts were obtained for data synthesis. The step-by-step selection procedure of articles is demonstrated in Fig. 1. The included articles’ quality assessment also showed that all articles were middle to high quality (Table 1).
Fig. 1:
Schematic diagram of article selection
Table 1:
Quality assessment of articles according to Newcastle-Ottawa and Oxford (Jadad) quality scales
| No | Authors | Newcastle Ottawa score | Jadad score |
|---|---|---|---|
| 1 | Lopresti AL, 2021 | 6 | 5 |
| 2 | Ried K, 2020 | 6 | 3 |
| 3 | Lior O, 2019 | 6 | 5 |
| 4 | Di Ciaula A, 2018 | 5 | 2 |
| 5 | Alt F, 2017 | 5 | 5 |
| 6 | Lauche R, 2016 | 5 | 5 |
| 7 | Portincasa P, 2016 | 6 | 4 |
| 8 | Pilipenko VI, 2015 | 6 | 3 |
| 9 | Bundy R, 2004 | 5 | 3 |
The maximum scores for Newcastle-Ottawa and Oxford quality scales are 9 and 5, respectively.
In the present review, nine articles with 850 populations were included and used for qualitative data description. The age of patients varied from 18 to 70 years. The eldest and recent articles among the collected literature were published in 2004 and 2021, respectively. In the included studies, curcumin or turmeric’s therapeutic potential alone or in combination with other medications was evaluated in patients with IBS. The most repeated variables measured in these studies were quality of life, severity score, IBS symptom, and abdominal pain.
Curcumin or turmeric extract is helpful in improving IBS. Moreover, curcumin showed a significant reduction in IBS severity score as early as four weeks (16, 17). A mixture containing 42 mg of curcumin and 25 mg of essential fennel oil improved the IBS severity index and the quality of life in all IBS patients independent of age and sex (18). In addition, the prevalence of IBS significantly decreased up to 60% after daily taking two tablets (144 mg) of a standardized turmeric extract for eight weeks (14, 15). The herbal formula containing curcumin as the significant part significantly improved upper and lowered GI symptoms by 40%–60% (19).
On the other hand, turmeric did not significantly reduce the clinical symptoms of IBS compared to placebo; however, the use of turmeric improved the clinical manifestations of patients with IBS (20). One study with 32 patients indicated that treatment with a mixture containing turmeric extract does not differentiate between treatment and placebo for reducing IBS symptoms (21). General information of included articles is demonstrated in Table 2 in chronological order.
Table 2:
Demographic information and the treatment data of included articles
| No | Reference | Country | Number of Patients | Age (yr) | Male/Female | Variables | Dosage | Duration of Therapy |
|---|---|---|---|---|---|---|---|---|
| 1 | (22 ) | Australia | 79 | 40.69 | 10/69 | GSRS, DASS-21, intestinal microbial profile | 500 mg once daily | Eight weeks |
| 2 | (19 ) | Australia | 43 | 50 | 10/33 | Intestinal permeability and gut microbiota profile | 10 g/day of the mixture containing curcumin | Four weeks |
| 3 | (20 ) | Israel | 22 | 54.5 | 6/16 | QoL, IBSS, IBS symptom | Four oral tablets/day containing 500 mg curcumin | Ten weeks |
| 4 | (18 ) | Italy, Belgium | 211 | 51±17 | 63/148 | IBSS, QoL, number of pain locations | The mixture containing 42 mg of curcumin | Ten weeks |
| 5 | (16 ) | Germany, Malaysia | 90 | 18–70 | 27/63 | Pain and discomfort | The mixture containing 330 mg of curcuminoids | Eight weeks |
| 6 | (21 ) | Germany, Australia | 32 | 50.3±11. 9 | 13/19 | IBSS, QoL, anxiety, depression, compliance and safety | The mixture containing turmeric twice daily | Four weeks |
| 7 | (17 ) | Italy | 116 | 18–66 | 44/77 | IBSS, abdominal pain | The mixture containing 42 mg curcumin Two capsules/day | Four weeks |
| 8 | (23 ) | Russia | 50 | - | - | Abdominal pain, bloating and feeling of incomplete bowel emptying, frequency of bowel movement, QoL | The mixture containing 10 mg curcumin | Two weeks |
| 9 | (15 ) | UK | 207 | - | 62/145 | IBS prevalence, symptom-related QoL, effectiveness | 72–144 mg/day of turmeric | Eight weeks |
IBSS: IBS Severity, GSRS: Gastrointestinal Symptom Rating Scale, DASS-21: Depression Anxiety and Stress Scale - 21, QoL: Quality of Life.
Discussion
Gastrointestinal disorders in children and adolescents may continue until adulthood, among which IBS is an essential chronic disorder. This syndrome is an intestinal dysfunction mainly characterized by changes in bowel movements and abdominal pain in the absence of structurally identifiable abnormalities (24). The annual cost of IBS is estimated over millions of dollars in the United States alone (25). Given the high prevalence of this syndrome in societies and the disease’s burden on the patient, family, and health care system, it is necessary to find a cheap and healthy treatment strategy. It has been previously shown that curcumin has therapeutic potential for treating digestive disorders, including inflammatory bowel diseases (26).
Recently, it has been suggested that turmeric extract or curcumin as a potent antioxidant and natural anti-inflammatory agent may reduce the severity of IBS by relieving the IBS-associated symptoms. Many animal studies have been performed and confirmed such effectiveness; however, minimal clinical trials have been conducted so far to evaluate the possible therapeutic effects of curcumin or turmeric extract on humans (27).
Due to its low bioavailability, poor absorption in the intestine, and rapid elimination, it is suggested that a combination of curcumin with enhancing agents such as other antioxidants or other herbal products may provide additional health benefits (28, 29). In this regard, findings have shown that a mixture of curcumin and fish oil, peppermint oil, caraway oil, thiamine, folic acid, and vitamin D3 helps relieve all IBS symptoms, especially abdominal pain and discomfort (16). A combination of turmeric extract and essential fennel oil was also shown to improve both IBS severity and the symptoms-associated quality of life (17, 18, 30).
A pilot study also reported that turmeric alone might significantly drop the IBS symptoms by 60% (15). Among the studies on humans, only one study showed that turmeric is no more effective in improving predominant diarrhea IBS, which may be due to a minimal amount of turmeric (1/10 w/w) in the medication mixture (21). Toxicological assessments indicated that herbal formula containing curcumin as a significant part was safe and tolerable in adult patients with digestive disorders (19). Although many human studies confirmed its safety even at high doses of 12 g/day (27), high doses of herbal compounds in long-term use have been shown to cause digestive problems or other acute toxicities (31). On a mechanistic view, curcumin can scavenge free radicals (32), and modulate the activity of enzymes involved in oxidative stress, including superoxide dismutase, catalase, and glutathione peroxidase (33), and inhibit free radical-generating enzymes, especially lipoxygenase and cyclooxygenase (28, 34, 35). Also, curcumin suppresses inflammation by downregulation of nuclear factor-kappa B and tumor necrosis factor α, the two significant inflammatory processes mediators (28).
An animal study suggested that curcumin may improve IBS symptoms by regulating neuro-transmitters such as serotonin, brain-derived neurotrophic factor, and cAMP response element-binding protein signaling pathways processes in the brain and peripheral intestinal system (36–38). Another study on albino rats showed that curcumin decreases intestinal motility, which explains its therapeutic effects in different gastrointestinal disorders such as like, abdominal pain and IBS (39).
Taken together and based on the results of studies included in this literature review, turmeric and its active ingredient, curcumin, may help treat digestive disorders, particularly IBS. In all the trials, curcumin and turmeric extract were also reported to be safe and well-tolerated even at a high dose of 20 mg. However, as the main limitation of this review, the current conclusions are only based on limited clinical trials; hence, more robust human studies on a large population are needed to confirm the efficiency of turmeric on IBS.
Conclusion
Curcumin and turmeric extract medications improve IBS symptoms, particularly abdominal pain and life quality. This evidence also demonstrated that turmeric alone or combined with other healthy and herbal products might be an effective treatment for relieving IBS-associated symptoms.
Journalism Ethics considerations
Ethical issues (Including plagiarism, informed consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc.) have been completely observed by the authors.
Acknowledgements
This research received no external funding.
Footnotes
Conflicts of interest
The authors declare no conflicts of interest.
References
- 1.Mousavi T, Nikfar S, Abdollahi M. (2020). An update on efficacy and safety considerations for the latest drugs used to treat irritable bowel syndrome. Expert Opin Drug Metab Toxicol, 16(7): 583–604. [DOI] [PubMed] [Google Scholar]
- 2.Pellissier S, Bonaz B. (2017). The place of stress and emotions in the irritable bowel syndrome. Vitam Horm, 103: 327–354. [DOI] [PubMed] [Google Scholar]
- 3.Coss-Adame E, Rao SS. (2014). Brain and gut interactions in irritable bowel syndrome: new paradigms and new understandings. Curr Gastroenterol Rep, 16(4): 379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sisay M, Bussa N, Gashaw T, et al. (2019). Investigating in vitro antibacterial activities of medicinal plants having folkloric repute in Ethiopian traditional medicine. J Evid Based Integr Med, 24: 2515690X19886276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kopczyńska M, Mokros Ł, Pietras T, et al. (2018). Quality of life and depression in patients with irritable bowel syndrome. Prz Gastroenterol, 13(2):102–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Te B, Yiming L, Tianwei L, et al. (2020). Polychlorinated biphenyls in a grassland food network: Concentrations, biomagnification, and transmission of toxicity. Sci Total Environ, 709: 135781. [DOI] [PubMed] [Google Scholar]
- 7.Mari A, Abu Baker F, Mahamid M, et al. (2020). The evolving role of gut microbiota in the management of irritable bowel syndrome: An overview of the current knowledge. J Clin Med, 9(3): 685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bonaz B, Lane RD, Oshinsky ML, et al. (2021). Diseases, disorders, and comorbidities of interoception. Trends Neurosci, 44(1):39–51. [DOI] [PubMed] [Google Scholar]
- 9.Panzarini E, Mariano S, Tacconi S, et al. (2020). Novel therapeutic delivery of nanocurcumin in central nervous system related disorders. Nanomaterials (Basel), 11(1):2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ghorani-Azam A, Sepahi S, Khodaverdi E, et al. (2018). Herbal medicine as a promising therapeutic approach for the management of vascular dementia: A systematic literature review. Phytother Res, 32(9): 1720–1728. [DOI] [PubMed] [Google Scholar]
- 11.Farzaei MH, Zobeiri M, Parvizi F, et al. (2018). Curcumin in liver diseases: a systematic review of the cellular mechanisms of oxidative stress and clinical perspective. Nutrients, 10(7): 855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Liberati A, Altman DG, Tetzlaff J, et al. (2009). The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol, 62(10):e1–34. [DOI] [PubMed] [Google Scholar]
- 13.Moher D, Shamseer L, Clarke M, et al. (2015). Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev, 4(1): 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lacy BE, Patel NK. (2017). Rome criteria and a diagnostic approach to irritable bowel syndrome. J Clin Med, 6(11): 99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bundy R, Walker AF, Middleton RW, et al. (2004). Turmeric extract may improve irritable bowel syndrome symptomology in otherwise healthy adults: a pilot study. J Altern Complement Med, 10(6): 1015–1018. [DOI] [PubMed] [Google Scholar]
- 16.Alt F, Chong PW, Teng E, et al. (2017). Evaluation of benefit and tolerability of IQP-CL-101 (xanthofen) in the symptomatic improvement of irritable bowel syndrome: A double-blinded, randomised, placebo-controlled clinical trial. Phytother Res, 31(7): 1056–1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Portincasa P, Bonfrate L, Scribano ML, et al. (2016). Curcumin and Fennel Essential Oil Improve Symptoms and Quality of Life in Patients with Irritable Bowel Syndrome. J Gastrointestin Liver Dis, 25(2): 151–7. [DOI] [PubMed] [Google Scholar]
- 18.Di Ciaula A, Portincasa P, Maes N, et al. (2018). Efficacy of bio-optimized extracts of turmeric and essential fennel oil on the quality of life in patients with irritable bowel syndrome. Ann Gastroenterol, 31(6): 685–691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ried K, Travica N, Dorairaj R, et al. (2020). Herbal formula improves upper and lower gastrointestinal symptoms and gut health in Australian adults with digestive disorders. Nutr Res, 76: 37–51. [DOI] [PubMed] [Google Scholar]
- 20.Lior O, Sklerovsy-Benjaminov F, Lish I, et al. (2019). Treatment of irritable bowel syndrome with a combination of curcumin, Green Tea and Selenomethionine has a positive effect on satisfaction with Bowel habits. J Biosci Med, 7(5): 170–179. [Google Scholar]
- 21.Lauche R, Kumar S, Hallmann J, et al. (2016). Efficacy and safety of ayurvedic herbs in diarrhoea-predominant irritable bowel syndrome: a randomised controlled crossover trial. Complement Ther Med, 26: 171–177. [DOI] [PubMed] [Google Scholar]
- 22.Lopresti AL, Smith SJ, Rea A, et al. (2021). Efficacy of a curcumin extract (Curcugen™) on gastrointestinal symptoms and intestinal microbiota in adults with self-reported digestive complaints: a randomised, double-blind, placebo-controlled study. BMC Complement Med Ther, 21(1): 40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pilipenko V, Teplyuk D, Shakhovskaya A, et al. (2015). Dry jelly concentrate with vitamins and dietary fiber in patients with IBS with constipation: a comparative controlled study. Vopr Pitan, 84(6): 83–91. [PubMed] [Google Scholar]
- 24.Ikechi R, Fischer BD, DeSipio J, et al. (2017). Irritable bowel syndrome: clinical manifestations, dietary influences, and management. Healthcare (Basel), 5(2): 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hulisz D. (2004). The burden of illness of irritable bowel syndrome: current challenges and hope for the future. J Manag Care Pharm, 10(4): 299–309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dulbecco P, Savarino V. (2013). Therapeutic potential of curcumin in digestive diseases. World J Gastroenterol, 19(48): 9256–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gupta SC, Patchva S, Aggarwal BB. (2013). Therapeutic roles of curcumin: lessons learned from clinical trials. AAPS J, 15(1): 195–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hewlings S, Kalman D. (2017). Curcumin: A Review of Its Effects on Human Health. Foods, 6(10): 92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hassani S, Tavakoli F, Amini M, et al. (2013). Occurrence of melamine contamination in powder and liquid milk in market of Iran. Food Addit Contam Part A Chem Anal Control Expo Risk Assess, 30(3): 413–420. [DOI] [PubMed] [Google Scholar]
- 30.Hosseini A, Abdollahi M, Hassanzadeh G, et al. (2011). Protective effect of magnesium-25 carrying porphyrin-fullerene nanoparticles on degeneration of dorsal root ganglion neurons and motor function in experimental diabetic neuropathy. Basic Clin Pharmacol Toxicol, 109(5): 381–386. [DOI] [PubMed] [Google Scholar]
- 31.Hudson A, Lopez E, Almalki AJ, et al. (2018). A review of the toxicity of compounds found in herbal dietary supplements. Planta Med, 84(9–10): 613–626. [DOI] [PubMed] [Google Scholar]
- 32.Menon VP, Sudheer AR. (2007). Antioxidant and anti-inflammatory properties of curcumin. In: The molecular targets and therapeutic uses of curcumin in health and disease. Advances in Experimental Medicine and Biology. vol 595, Springer. Boston, MA, pp. 105–125. [DOI] [PubMed] [Google Scholar]
- 33.Marchiani A, Rozzo C, Fadda A, et al. (2014). Curcumin and curcumin-like molecules: from spice to drugs. Curr Med Chem, 21(2): 204–222. [DOI] [PubMed] [Google Scholar]
- 34.Lin YG, Kunnumakkara AB, Nair A, et al. (2007). Curcumin inhibits tumor growth and angiogenesis in ovarian carcinoma by targeting the nuclear factor-κB pathway. Clin Cancer Res, 13(11): 3423–3430. [DOI] [PubMed] [Google Scholar]
- 35.Shetty NP, Prabhakaran M, Srivastava AK. (2021). Pleiotropic nature of curcumin in targeting multiple apoptotic-mediated factors and related strategies to treat gastric cancer: A review. Phytother Res, 35(10): 5397–5416. [DOI] [PubMed] [Google Scholar]
- 36.Yu Y, Wu S, Li J, et al. (2015). The effect of curcumin on the brain-gut axis in rat model of irritable bowel syndrome: involvement of 5-HT-dependent signaling. Metab Brain Dis, 30(1): 47–55. [DOI] [PubMed] [Google Scholar]
- 37.Patel SS, Acharya A, Ray R, et al. (2020). Cellular and molecular mechanisms of curcumin in prevention and treatment of disease. Crit Rev Food Sci Nutr, 60(6): 887–939. [DOI] [PubMed] [Google Scholar]
- 38.Salek-Maghsoudi A, Hassani S, Momtaz S, et al. (2019). Biochemical and molecular evidence on the role of vaspin in early detection of the insulin resistance in a rat model of high-fat diet and use of diazinon. Toxicology, 411:1–14. [DOI] [PubMed] [Google Scholar]
- 39.Sözen S, Aziret M, Bali I, et al. (2015). The Effect of Curcumin on an Animal Intestinal Ischemia/Reperfusion Model for Bacterial Translocation and Inflammatory Response. Int Surg, 100(11–12): 1352–1359. [Google Scholar]