Abstract
Background:
The End Stage Renal Disease (ESRD) is irreversible impairment of renal function, to the extent that the patient becomes permanently dependent on alternative therapies, especially in children. We aimed to evaluate the graft and patient survival rate among iranian pediatric recipients of kidney transplantation through a systematic review and meta-analysis.
Methods:
National (SID, MagIran, IranMedex, IranDoc) and international (Cochrane, Embase, ScienceDirect, Scopus, PubMed, and Web of Science) databases of, were searched to find studies published electronically from 1985 until Nov 2019. Heterogeneity between the collected studies was determined using the Cochran’s test (Q) and I2. Meta-regression was used to investigate the factors affecting statistical heterogeneity in 1, 5, and 10-year survival of kidney transplantation in addition to subgroup analysis based on cities.
Results:
Ten studies were qualified to enter the meta-analysis. The total participants in the study were 2673 people with an average age of 13.71±3.65 years. In the random-effects model, the survival rate of 1, 3, 5 and 10 yr of kidney transplantation were 91, 88, 81 and 70%, respectively.
Conclusion:
By providing the documented and comprehensive evidence, can be the basis of many plans, policies, and decisions of various sectors of development. These sectors include the evaluation of treatment programs and health interventions in the pediatric kidney transplantation. The results of the present study can provide an acceptable estimate of the survival rate of transplanted children in Iran and will be useful for planning prevention and treatment programs.
Keywords: Kidney transplantation, End stage renal disease, Graft survival, Patient survival, Meta-analysis
Introduction
Chronic Kidney Disease (CKD) involves a range of different pathophysiological processes associated with abnormal renal function and progressive decline in glomerular filtration rate (1, 2). The end stage renal disease is irreversible impairment of renal function, to the extent that the patient becomes permanently dependent on alternative therapies, especially in children (1, 3). The incidence rate of chronic kidney disease among children in Iran is 16.8 per million, and the rate of kidney transplantation among children is 7.2 per million (4). Treatment options in patients with the end-stage renal disease include hemodialysis and kidney transplantation (1). Since kidney transplantation is the treatment of choice for patients with end-stage renal disease (5–10), it is considered the most effective treatment for end-stage renal disease in many cases (11). Kidney transplantation improves the quality of life, as well as the chance of patients’ survival (12–15).
Despite the advantages, performing kidney transplants in children and adolescents has its challenges. At least 20% of kidney failure at this age is related to urinary tract abnormalities. Regarding these challenges, the abdominal space of children is small for organs and vascular anastomosis is challenging for small kidneys. Maintaining hemodynamic stability and fluid therapy at the time of transplantation, as well as prescribing and controlling medications for children, can be difficult. Despite all the efforts made to increase the survival rate of the transplanted kidney in children, most children need an alternative transplant over time.
And if a transplanted kidney is taken from a living child donor, it will have a longer survival rate than a transplanted kidney from a cadaver (16, 17).
Prophylactic renal transplantation is currently recommended as a treatment and accounts for about 30% of pediatric kidney transplants in the United States and the United Kingdom. Not performing dialysis can keep blood vessels healthy and can increase the survival rate of a transplanted kidney (18). Many recent advances in the management of pediatric kidney transplantation, immunosuppressive drugs, and surgical techniques have led to an increase in the survival of transplanted kidneys (19–21). The survival rate of transplanted kidneys in children has not been high in previous studies due to infections, transplanted kidney rejection, and improper use of drugs (22, 23).
One-year uncensored graft survival of patients who were ABO-incompatible was 96% versus 98% in ABO-compatible. Three-year uncensored graft survival of patients who were ABO-incompatible was 92% versus 94% in ABO-compatible (18, 24).
Up to now, no comprehensive study has been conducted on the survival rate of kidney transplant patients and the allograft in Iran. We aimed to evaluate the graft and patient survival rate among iranian pediatric recipients of kidney transplantation through a systematic and meta-analysis review. Especially, there is insufficient data related to the results of pediatric kidney transplantation and the factors affecting it in Iran.
Methods
Search strategy
This study is a systematic and meta-analysis review. It was based on the reporting system of systematic and meta-analysis review studies “Preferred reporting items for systematic reviews and meta-analyses” (PRISMA). PRISMA is an evidence-based minimum set of items for reporting in systematic reviews and meta-analyses. PRISMA focuses on the reporting of reviews evaluating randomized trials. However, it can also be used as a basis for reporting systematic reviews of other types of research, particularly evaluations of interventions. Based on the PRISMA checklist, in the first stage by searching the database of Jihad Danesshgahi (Database Information Scientific), The Iranmedex database, MagIran and the database of medical science articles from 1985 until Nov 2020 by using the keywords Iran, kidney, kidney transplant, age, children and survival, internally published documents were collected and related items were extracted.
In the next step, by using PubMed, Scopus, ISI web of knowledge, and Direct Science from 1985 until Nov 2020, keywords were searched by employing OR and AND. For example, Kidney Transplantation OR Renal Transplantation AND Survival Rate OR Survival Analysis AND Pediatric OR Child AND Iran, documents, articles, and abstracts of articles related to the research topic were collected and its full text was extracted. Besides, the sources of the obtained documents were examined to obtain the relevant titles. Similarly, specialized journals in the field of nephrology were also reviewed at the same time. For articles whose full text was not available, to obtain the full text, an email was sent to the authors. After extracting the documents, article specifications, and article abstracts, were entered in the EndNote software, and duplicates were removed using the software. In the next step, by reviewing the titles, studies unrelated to the aim of this study were excluded, then the full text of the article was ensured to be relevant to the purpose of the study, and irrelevant items were removed.
Inclusion and exclusion criteria
The main inclusion criteria in this research were the survival of kidney or nephrology patients in the population of children and adolescents in Iran. Population criteria based on age were considered under 18 yr old. In addition, survival rates for the population studied should be reported in the articles. Exclusion criteria included not being relevant to the topic, not reporting survival index, adult population, and non-Iranian sample.
Quality assessment and data extraction
The authors assessed the quality of the studies using an edited checklist from the prestigious Joanna Bridges Institute tailored to the descriptive studies (25). This checklist consists of 9 questions which are: a study of sample survey appropriate to the target population, sample collection method, sample size, characteristics of participants and place of study, analysis of samples and subgroups, tools used, the conditions of the research, proportional and accurate statistical analyzes, and at the end, about the response rate mentioned in the sample. The answer to each question is three options (yes, no, unspecified) and only the option “yes” is given a score of 1 and the other options are given a score of zero.
Statistical analysis
In each study, considering the survival rate as a probability of binomial distribution, its variance was calculated through binomial distribution and Cochran test (Q) and I2 the index was used to evaluate the heterogeneity of the studies. Keeping in mind the methodological heterogeneity in the studies included for meta-analysis, a stochastic effects model was used to combine the results of the studies. In the case of heterogeneity, a random effect model along with the inverse-variance method were used. A fixed effect model was applied in the absence of heterogeneity.
In this study, meta-regression was used to investigate the factors affecting statistical heterogeneity in 1, 5, and 10-year survival of kidney transplantation in addition to subgroup analysis based on cities. Evaluation of diffusion bias for only 1-year survival due to the adequacy of the number of studies was first evaluated with a funnel plot and then using Egger and Begg tests the significance of diffusion bias was examined. Data analysis was performed using Stata (StataCrop, College Station, Texas, USA) software ver. 14.1.
Results
After study selection process, 10 studies conducted between 1985 and Nov 2020 were qualified to enter the meta-analysis (Fig. 1). The total participants in the study were 2673 people with an average age of 13.71±3.65 yr. The highest sample size was reported in the study with 907 people and the lowest sample size was reported in the study with 21 people. Six studies (60%) were performed in Tehran Province, 2 studies in Mash-had, and 2 studies in Shiraz. In these studies, 9 studies reported one-year survival, 4 studies 3-year survival, 8 studies 5-year survival, and 5 studies reported10-year survival of kidney transplantation. In addition, only 3 studies reported 1-year survival and 2 studies reported 5-year survival of kidney transplant patients. Table 1 shows the general characteristics and data for each study.
Fig. 1:
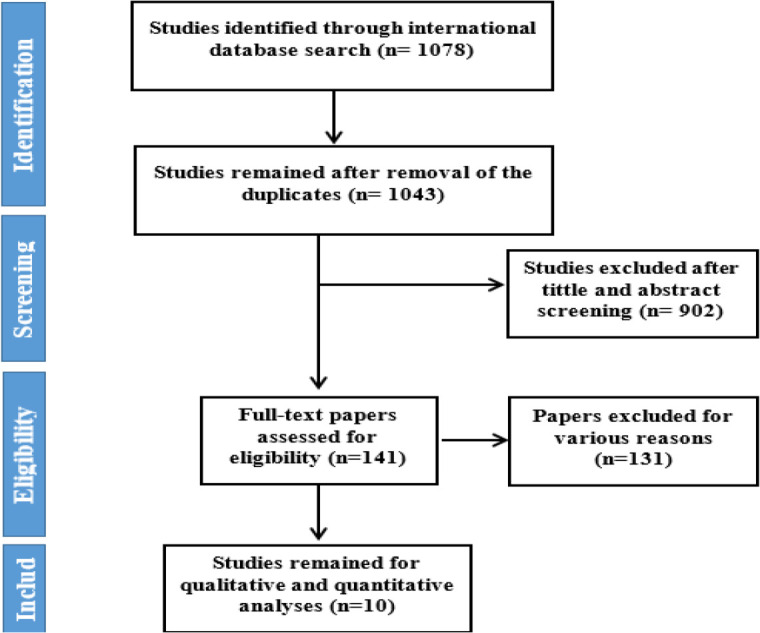
Flowchart of the included eligible studies in systematic review
Table 1:
Characteristics of the included studies in systematic review of the survival rate of graft and patient
| First Author, Publication year | Location | Time Period | Age of recipient | Mean dialysis mont h | Mea n follow up mont h | Sample size | Survival Rate of Graft | Survival Rate of patients | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||||
| 1 | 2 | 3 | 5 | 7 | 10 | 1 | 5 | |||||||
| Hashemi, G. et al, (40) | Shiraz, Iran | 1989–1994 | 12 | 5.50 | 32 | 0.89 | 0.71 | 0.93 | ||||||
| Khammar, M. A. et al, (41) | Mashhad, Iran | 1989–1996 | 12 | 2 | 41 | 0.93 | 0.90 | |||||||
| Mahdavi, R. et al, (42) | Mashhad, Iran | 1989–1999 | 12 | 3 | 66 | 450 | 0.95 | 0.84 | 0.76 | 0.62 | ||||
| Otukesh, H. et al, (43) | Tehran, Iran | 1985–2003 | 11.60 | 32.90 | 85 | 278 | 0.70 | |||||||
| Otukesh, H. et al, (44) | Tehran, Iran | 1985–2005 | 17 | 300 | 0.95 | 0.91 | 0.65 | 0.50 | ||||||
| Otukesh, H. et al, (45) | Tehran, Iran | 1987–2009 | 18 | 14.75 | 49.37 | 907 | 0.89 | 0.80 | 0.72 | 0.59 | ||||
| Almasi-Hashiani, A. et al, (46) | Shiraz, Iran | 1999–2009 | 18 | 164 | 0.97 | 0.89 | 0.83 | 0.78 | 0.78 | |||||
| Hoseini, R. et al, (47) | Tehran, Iran | 1985–2012 | 8.5 | 24 | 78.4 | 21 | 1.00 | 0.94 | 0.94 | 0.94 | ||||
| Gholamre-zaie, H.et al, (16) | Tehran, Iran | 2008–2015 | 10 | 24 | 166 | 0.94 | 0.93 | 0.99 | 0.97 | |||||
| Naderi, G. et al, (3) | Tehran, Iran | 1989–2013 | 18 | 14.50 | 15.80 | 314 | 0.90 | 0.81 | 0.62 | 1.00 | 0.99 | |||
Results obtained from kidney transplant survival meta-analysis
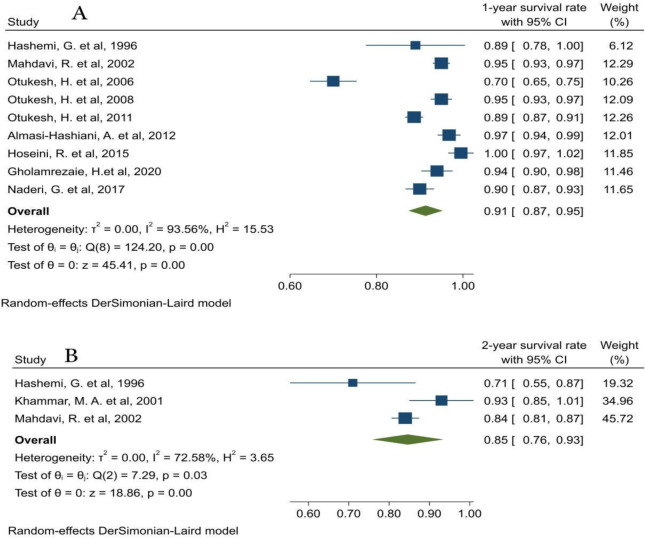
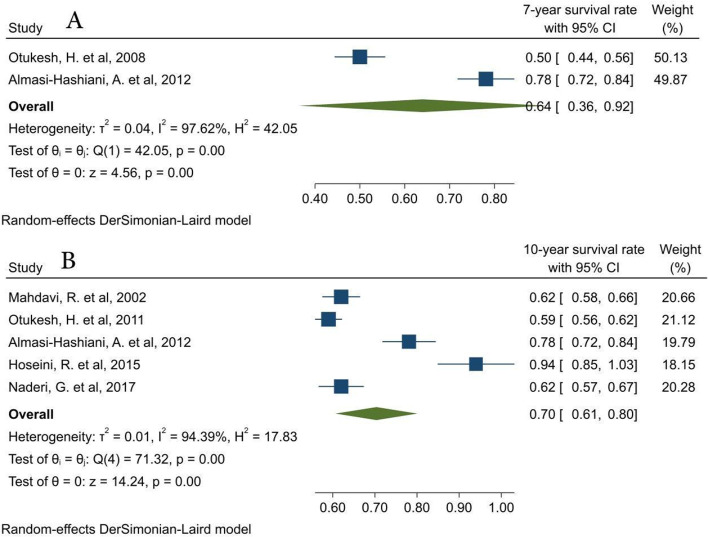
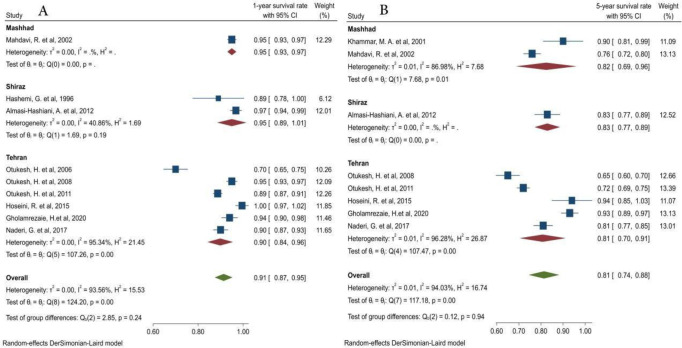
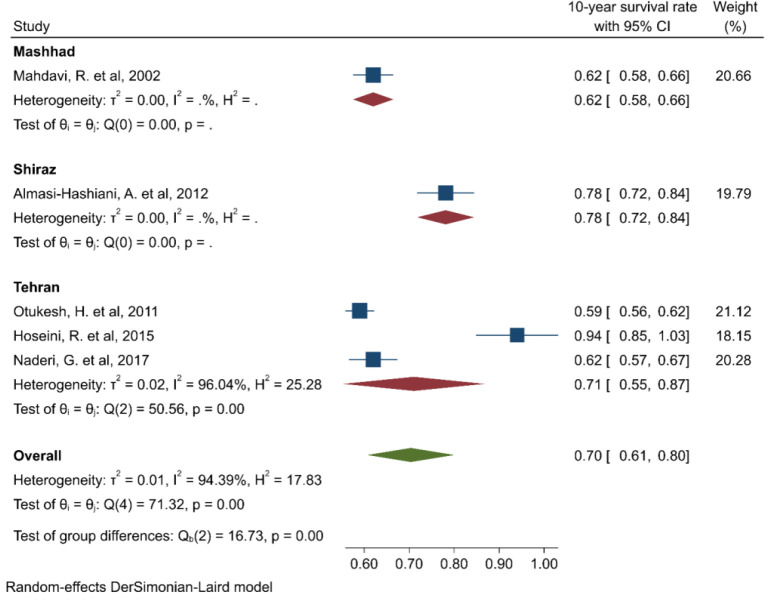
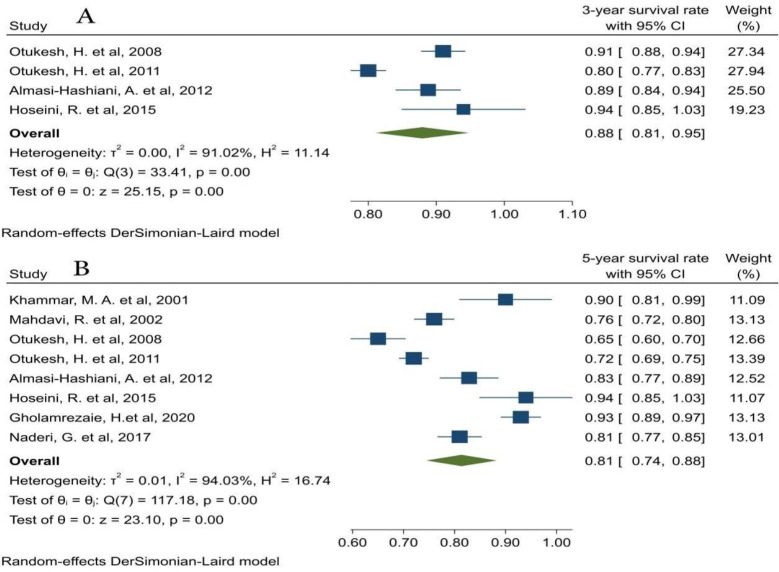
In the random-effects model, the survival rate of 1,2,3,5,7, and 10 yr of kidney transplantation were 91,85,88,81,64 and 70%, respectively (Fig. 2–4). In addition, the 1,5 and 10 year survival rates of kidney transplantation based on the cities under study showed in Fig. 5 and 6. The status of Publication bias for the one-year survival of kidney transplantation (which had the highest number of studies) is presented in the form of a funnel plot in Appendix 1 (Not published). In addition, due to the possibility of diffusion bias based on the proposed figure, however, the Egger test (P=0.36) and the Begg test (P=0.46) did not confirm the existence of this bias. Survival for other years, given that there was not enough power for publication bias test, was not presented.
Fig. 2:
A: 1-year Survival Rate of Iranian Pediatric Patients with Transplanted Kidney B: 2-year Survival Rate of Iranian Pediatric Patients with Transplanted Kidney
Fig. 4:
A: 7-year Survival Rate of Iranian Pediatric Patients with Transplanted Kidney, B: 10-year Survival Rate of Iranian Pediatric Patients with Transplanted Kidney
Fig. 5:
A: 1-year Survival Rate of Iranian Pediatric Patients with Transplanted Kidney by City, B: 5-year Survival Rate of Iranian Pediatric Patients with Transplanted Kidney by City
Fig. 6:
10-year Survival Rate of Iranian Pediatric Patients with Transplanted Kidney by City
Fig. 3:
A: 3-year Survival Rate of Iranian Pediatric Patients with Transplanted Kidney, B: 5-year Survival Rate of Iranian Pediatric Patients with Transplanted Kidney
Heterogeneity between studies was assessed using the Chi-square test and I2 index, seen in the figures. The reasons for the heterogeneity between studies for the one-year survival of kidney transplantation in meta-regression were that none of the recorded variables showed a significant effect. For the 10-year survival rate of kidney transplantation, the only sample size has a significant effect on the heterogeneity of studies (Table 2).
Table 2:
Results of meta-regression for survival rate of graft
| 1-year survival rate | β | P-value |
|---|---|---|
| City | −0.019 | 0.39 |
| Year of publication | 0.003 | 0.31 |
| Age of recipient | 0.0001 | 0.97 |
| Average months of dialysis | −0.0041 | 0.16 |
| Follow up time | −0.0008 | 0.57 |
| Sample size | −0.00006 | 0.37 |
| 5-year survival rate | ||
| City | −0.006 | 0.84 |
| Year of publication | 0.005 | 0.27 |
| Age of recipient | −0.018 | 0.02 |
| Average months of dialysis | 0.004 | 0.31 |
| Follow up time | 0.001 | 0.54 |
| Sample size | −0.0002 | 0.03 |
| 10-year survival rate | ||
| City | 0.027 | 0.60 |
| Year of publication | 0.009 | 0.40 |
| Age of recipient | −0.02 | 0.13 |
| Average months of dialysis | 0.013 | 0.08 |
| Follow up time | 0.003 | 0.13 |
| Sample size | −0.0003 | 0.01 |
Results obtained from meta-analysis of survival of kidney transplant patients
For the survival of kidney transplant patients, considering that there was only enough data for 1-year and 5-year survival, an analysis was performed which showed that the 1-year survival of patients was 100% and 5-year survival was 99% (Information about this content is provided through the appendix. The interested readers may contact the corresponding author to reach them).
Checking the quality of articles imported for meta-analysis
Out of 10 studies submitted for meta-analysis, 6 studies had a score of 5 or higher, and one study had a score of 3 and was of low quality. Details of the quality assessment results of the articles submitted for meta-analysis are presented in Table 3.
Table 3:
Qualities of studies included in the systematic review and meta-analysis
| First Author/Year public | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Total |
|---|---|---|---|---|---|---|---|---|---|---|
| Hashemi, G. et al, 1996 | N | N | N | Y | Y | Y | Y | Y | N | 5 |
| Khammar, M. A. et al, 2001 | N | N | N | Y | N | Y | Y | Y | N | 4 |
| Mahdavi, R. et al, 2002 | N | N | Y | Y | Y | Y | Y | Y | U | 6 |
| Otukesh, H. et al, 2006 | N | N | Y | U | Y | Y | Y | Y | U | 5 |
| Otukesh, H. et al, 2008 | N | N | Y | U | Y | Y | Y | Y | U | 5 |
| Otukesh, H. et al, 2011 | N | N | Y | Y | Y | Y | Y | Y | Y | 7 |
| Almasi-Hashiani, A. et al, 2012 | N | N | N | Y | N | Y | Y | Y | N | 4 |
| Hoseini, R. et al, 2015 | N | N | N | U | N | Y | Y | Y | N | 3 |
| Gholamrezaie, H.et al, 2020 | N | N | N | Y | N | Y | Y | Y | N | 4 |
| Naderi, G. et al, 2017 | N | N | Y | Y | Y | Y | Y | Y | U | 6 |
Keys:
A. Q1-Q9 represents questions used to assess the quality of included studies, listed below.
Q1. Was the sample frame appropriate to address the target populations?
Q2. Were the study participants sampled in appropriate way?
Q3. Was the sample size adequate?
Q4. Were the study subjects and setting described in details?
Q5. Was the data analysis conducted with sufficient coverage of the identified sample?
Q6. Was a valid method used in the identification of conditions?
Q7. Was the condition measured in a standard, reliable way for all participants?
Q8. Was there an appropriate statistical analysis?
Q9. Was the response rate adequate, and if not, was the low response rate managed appropriately?
B. Y, yes; N, no; U, unclear; NA, not applicable
Discussion
The end stage renal disease is irreversible impairment of renal function, to the point that the patient becomes permanently dependent on alternative therapies, especially in children (1, 3). Kidney transplantation is one of the most effective treatments for patients with advanced kidney disease (3). In present study, the survival rate and influential factors that can exert a noticeable impact on transplanted kidney were investigated.
In the current study, the 1-year survival rate of the transplanted kidney came out to be 91%, which is consistent with the results of the other studies (3, 26, 27). Moreover, the results obtained are not only eligible for comparison with the results of the North American Pediatric Renal Trials and Collaborative Studies (NAPRTCS) annual report, but also our results demonstrate higher percentages for 1-year survival (28). Interestingly, 1-year survival rate was reported 94%, which is even higher. In Japan, this survival rate was 81%, which is much less than the result obtained in this study (29). The one-year survival rate of kidney transplant patients was 100%, while in Egypt; the rate was reported to be 94% (26).
A general comparative overview of the results obtained from the studies of other countries reveals that the one-year survival rate of transplanted kidneys and transplanted patients in children is at a high level and is consistent with the results of valid centers around the world. Monitoring the recovery and prevention from infections, paying more attention to cardiovascular risk factors, and updating clinical practice guidelines are also likely to improve the survival.
The 3-year survival rate of kidney transplantation came out to be 88%, while the 3-year survival rate reported in Egypt was 89% (26). Moreover, in India, better results were reported, as the 3-year survival rate of the transplanted kidney was 93% (30). In Turkey, this rate is reported to be 75%, which is much lower than the survival rate computed in this study (31).
In this study, the 5-year survival rate of the transplanted kidney came out to be 81%, which is not only comparable with the results of other studies conducted in different parts of the world, but it is even more. In Greece, the rate was 81% (32) and 67% in Russia (33). While in Germany, this rate is reported to be 85.5% (27), the United States 85% (33), and Germany 91% (35) which is higher compared to that in our study. In Australia and New Zealand, the 5-year survival rate of transplanted kidneys is 99%, which is higher than the rate reported in many developed countries (36). One of the reasons reported for the low 5-year survival rate of transplanted kidneys is the consumption of combined medications (steroids, cyclosporine, and azathioprine) that suppress the immune system (3). Moreover, in this study, the 5-year survival rate of kidney transplant patients was computed 99%, which is more compared to other studies in the world, including Russia which is 86% (32), Germany which is 97.6% (35), and Greece which is 92.7% (32).
A comprehensive comparative analysis of the results obtained from studies in other countries proved that the 5-year survival rate of transplant patients in children is at a high level and is consistent with the results of authentic centers around the world. Regarding the 5-year survival of transplanted kidneys, by improving surgical techniques and regular and correct use of immunosuppressive drugs, acute rejection of transplanted kidneys can be prevented and the survival rate of transplanted kidneys can be increased.
In the present study, the 10-year survival rate of transplanted kidneys showed to be 70%, which in comparison with the results of other studies, is better and higher. Other countries with lower rates are Egypt 59% (36), Germany 71% (27), Russia 53% (33) and the United States is 68% (37). In contrast to our result, a study from Japan reported 89% for 10-year survival, which is more than that of the present study.
One of the factors affecting the 5-year survival rate of the transplanted kidneys was the age of the transplant recipient, so that in older ages, the probability of survival decreases and in younger ages, the probability of survival increases. In the US, younger age was one of the most important predictors of transplant survival (38). While in Spain, one of the factors affecting the survival rate is young age, the reason for which is an increase in the number of complications, venous thrombosis, and high rate of kidney transplant rejection over the age of 5 years (39). While due to the presence of only 5 children under 6 yr in the study population, no relationship was observed between the survival rate of the transplanted kidney and the age of the recipient (16).
Limitations
One of the limitations of the present study was that the information reported in the input articles was incomplete and therefore, many influencing factors such as recipient and donor sex and part of kidney received were not included in the subgroup analysis.
These factors can also explain the significant heterogeneity between studies, which even existed in the subgroups. In the present study, to access the required information, the authors of the articles were contacted but not enough response was received except for a few cases. In order to adjust the heterogeneity of the studies, we used a Stochastic Impact model. Due to limited number of studies reporting 2- and 7-year survivals and lower validity of their results, the survival rates followed an increasing trend.
Conclusion
Kidney transplantation is currently the best alternative treatment among patients with end-stage renal disease. Those patients who receive a kidney transplant have better survival rate as well as a better quality of life than patients who are being treated by dialysis. A general comparison of the results obtained from this study with the studies conducted in other countries show that the survival rate of the transplanted kidneys and transplanted pediatric patients is at a higher level. It is also consistent with the results of authentic centers around the world.
The results of this study, by providing the documented and comprehensive evidence, can be the basis of many plans, policies, and decisions of various sectors of development. These sectors include the evaluation of treatment programs and health interventions in the pediatric kidney transplantation. The present meta-analysis study also had valid pieces of evidence. In this study, in addition to examining the survival rate of the patient and pediatric kidney transplant in Iran, we examined the factors affecting the survival rate. The results of the present study can provide an acceptable estimate of the survival rate of transplanted children in Iran and will be useful for planning prevention and treatment programs.
Journalism Ethics considerations
Ethical issues (Including plagiarism, informed consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc.) have been completely observed by the authors.
Acknowledgements
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Footnotes
Competing interest
The authors declare that they have no competing interest.
References
- 1.Ghelichi Ghojogh M, Taghizadeh Afshari A, Salarilak S, et al. (2017). The Effect of Body Mass Index on Patient and Graft Survival Rate in Kidney Transplanted Patients in Iran. Nephro-Urol Mon, 9(4): e14386. [Google Scholar]
- 2.Ghelichi-Ghojogh M, Ghaem H, Mohammadizadeh F, et al. (2021). Graft and Patient Survival Rates in Kidney Transplantation, and Their Associated Factors: A Systematic Review and Meta-Analysis. Iran J Public Health, 50(8):1555–1563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Naderi G, Latif A, Karimi S, et al. (2017). The long-term outcome of pediatric kidney transplantation in Iran: Results of a 25-year single-center cohort study. Int J Organ Transplant Med, 8(2):85–96 [PMC free article] [PubMed] [Google Scholar]
- 4.Gheissari A, Hemmatzadeh S, Merrikhi A, et al. (2012). Chronic kidney disease in children: A report from a tertiary care center over 11 years. J Nephropathol, 1(3):177–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Einollahi B, Pourfarziani V, Ahmadzad-Asl M, et al. (2007). Iranian model of renal allograft transplantation in 3028 recipients: survival and risk factors. Transplant Proc, 39(4):907–10. [DOI] [PubMed] [Google Scholar]
- 6.Hariharan S, Johnson CP, Bresnahan BA, et al. (2000). Improved graft survival after renal transplantation in the United States, 1988 to 1996. N Engl J Med, 342(9):605–12. [DOI] [PubMed] [Google Scholar]
- 7.Salehipour M, Bahador A, Jalaeian H, et al. (2008). Comparison of right and left grafts in renal transplantation. Saudi J Kidney Dis Transpl, 19(2):222–6. [PubMed] [Google Scholar]
- 8.Simforoosh N, Basiri A, Fattahi M, et al. (2006). Living unrelated versus living related kidney transplantation: 20 years’ experience with 2155 cases. Transplant Proc, 38(2):422–5. [DOI] [PubMed] [Google Scholar]
- 9.van Walraven C, Austin PC, Knoll G. (2010). Predicting potential survival benefit of renal transplantation in patients with chronic kidney disease. CMAJ, 182(7):666–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wong G, Howard K, Chapman JR, et al. (2012). Comparative survival and economic benefits of deceased donor kidney transplantation and dialysis in people with varying ages and comorbidities. PLoS One, 7(1):e29591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Georgieva S, Mitov K, Dimitrova M, et al. (2012). Survival on pharmacotherapy analysis for patients after kidney transplantation. Int J Pharmaceutical Sci Rev Res, 16(2):30–4. [Google Scholar]
- 12.Ghojogh MG, Salarilak S, Afshari AT, et al. (2018). Impact of type of donor on graft and patient survival rate in kidney transplanted patients in Iran. J Renal Inj Prev, 7(4):264–8. [Google Scholar]
- 13.Heldal K, Hartmann A, Grootendorst DC, et al. (2010). Benefit of kidney transplantation beyond 70 years of age. Nephrol Dial Transplant, 25(5):1680–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nathan HM, Conrad SL, Held PJ, et al. (2003). Organ donation in the United States. Am J Transplant, 3 Suppl 4:29–40. [DOI] [PubMed] [Google Scholar]
- 15.Tekin S, Yavuz H, Yuksel Y, et al. (2015). Kidney transplantation from elderly donor. Transplant Proc, 47(5):1309–11. [DOI] [PubMed] [Google Scholar]
- 16.Gholamrezaie HR, Tabibi A, Nikravesh N, et al. (2020). Results of Pediatric Kidney Transplants in an 8-Year Period: A Retrospective Study. Transplant Proc, 52(3):793–99. [DOI] [PubMed] [Google Scholar]
- 17.Williams RC, West LJ, Opelz G. (2018). The risk of failure with HLA mismatch and recipient age in first pediatric (< 18 years) kidney transplants. Transplant Direct, 4(7): e365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Starzl T, Groth C, Putnam C, et al. (1970). Urological complications in 216 human recipients of renal transplants. Ann Surg, 172(1):1–22. [PMC free article] [PubMed] [Google Scholar]
- 19.Dharnidharka VR, Fiorina P, Harmon WE. (2014). Kidney transplantation in children. N Engl J Med, 371(6):549–58. [DOI] [PubMed] [Google Scholar]
- 20.Van Arendonk KJ, Boyarsky BJ, Orandi BJ, et al. (2014). National trends over 25 years in pediatric kidney transplant outcomes. Pediatrics, 133(4):594–601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Assadi F. (2013). Pediatric Kidney Transplantation Kids are Different. Iran J Kidney Dis. 7(6):429–31. [PubMed] [Google Scholar]
- 22.Torkaman M, Khalili-Matin-Zadeh Z, Azizabadi-Farahani M, et al. (2007). Outcome of living kidney transplant: pediatric in comparison to adults. Transplant Proc, 39(4):1088–90. [DOI] [PubMed] [Google Scholar]
- 23.Sert I, Yavascan Ö, Tugmen C, et al. (2013). A retrospective analysis of long-term graft survival in 61 pediatric renal transplant recipients: a single-center experience. Ann Transplant, 18:497–504. [DOI] [PubMed] [Google Scholar]
- 24.de Weerd AE, Betjes MG. (2018). ABO-incompatible kidney transplant outcomes: a meta-analysis. Clin J Am Soc Nephrol, 13(8):1234–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Munn Z, Moola S, Lisy K, et al. (2015). Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data. Int J Evid Based Healthc, 13(3):147–53. [DOI] [PubMed] [Google Scholar]
- 26.Fadel FI, Bazaraa HM, Badawy H, et al. (2020). Pediatric kidney transplantation in Egypt: Results of 10-year single-center experience. Pediatr Transplant, 24(6):e13724. [DOI] [PubMed] [Google Scholar]
- 27.Friedersdorff F, Koch T-M, Banuelos-Marco B, et al. (2018). Long-Term follow-up after paediatric kidney transplantation and influence factors on graft survival: a single-centre experience of 16 years. Urol Int, 100(3):317–321. [DOI] [PubMed] [Google Scholar]
- 28.North American Pediatric Renal Trials and Collaborative Studies . 2010 Annual transplant report. Available from: https://emmes.com/projects/120
- 29.Aoki Y, Hamasaki Y, Satoh H, et al. (2020). Long-term outcomes of pediatric kidney transplantation: A single-center experience over the past 34 years in Japan. Int J Urol, 27(2):172–8. [DOI] [PubMed] [Google Scholar]
- 30.Bijalwan P, Sanjeevan KV, Mathew A, et al. (2017). Outcome and complications of living donor pediatric renal transplantation: Experience from a tertiary care center. Indian J Urol, 33(3):221–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Haberal M, Bereket G, Karakayalı H, et al. (2000). Pediatric renal transplantation in Turkey: a review of 56 cases from a single center. Pediatr Transplant, 4(4):293–9. [DOI] [PubMed] [Google Scholar]
- 32.Papachristou F, Stabouli S, Printza N, et al. (2016). Long-term outcome of pediatric kidney transplantation: A single-center experience from Greece. Pediatr Transplant, 20(4):500–6. [DOI] [PubMed] [Google Scholar]
- 33.Sushkov AI, Molchanova EA, Kaabak MM, et al. (2019). Pediatric kidney transplantation: early and long-term outcomes following 1187 procedures. Khirurgiia (Mosk), (1):14–26. [DOI] [PubMed] [Google Scholar]
- 34.Sigurjonsdottir VK, Grimm PC. (2019). Living or deceased donor kidney transplantation in children. Curr Opin Pediatr, 31(2):232–6. [DOI] [PubMed] [Google Scholar]
- 35.Mehrabi A, Golriz M, Khajeh E, et al. (2019). Surgical outcomes after pediatric kidney transplantation at the University of Heidelberg. J Pediatr Urol, 15(3): 221.e1–221.e8. [DOI] [PubMed] [Google Scholar]
- 36.Francis A, Johnson DW, Melk A, et al. (2020). Survival after kidney transplantation during childhood and adolescence. Clin J Am Soc Nephrol, 15(3):392–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Canning DA. (2017). Re: Gordon A. Mclorie. May 2, 1945–February 2, 2015. J Urol, 197(5):1355–7. [DOI] [PubMed] [Google Scholar]
- 38.Smith JM, Martz K, Blydt-Hansen TD. (2013). Pediatric kidney transplant practice patterns and outcome benchmarks, 1987–2010: A report of the N orth A merican P ediatric R enal T rials and C ollaborative S tudies. Pediatr Transplant, 17(2):149–57. [DOI] [PubMed] [Google Scholar]
- 39.Gander R, Asensio M, Royo GF, et al. (2017). Treatment of post-transplant lymphocele in children. Urology, 103:218–23. [DOI] [PubMed] [Google Scholar]
- 40.Hashemi GH, Malek Hosseini SA, Fallah-Zadeh MH, et al. (1996). Kidney transplantation in children and adolescents of Southern Iran. Med J Islam Repub Iran, 10(1):7–9. [Google Scholar]
- 41.Khammar MA, Mahdavi-Zafarghandi R. (2001). Renal transplantation in children: results of 9 years of renal transplantation in children at our center. Transplant Proc, 33(5):2825. [DOI] [PubMed] [Google Scholar]
- 42.Mahdavi R, Naghib M. (2002). Kidney transplantation in children: results of ten years exp erience in imam reza hospital. Med J Islam Repub Iran, 16(3):145–9. [Google Scholar]
- 43.Otukesh H, Basiri A, Simfrosh N, et al. (2006). Outcome of pediatric renal transplantation in Labfi Nejad Hospital, Tehran, Iran. Pediatr Nephrol, 21(10):1459–63. [DOI] [PubMed] [Google Scholar]
- 44.Otukesh H, Basiri A, Simfroosh N, et al. (2008). Kidney transplantation in children with posterior urethral valves. Pediatr Transplant, 12(5):516–9. [DOI] [PubMed] [Google Scholar]
- 45.Otukesh H, Hoseini R, Rahimzadeh N, et al. (2011). Outcome of renal transplantation in children: A multi-center national report from Iran. Pediatr Transplant, 15(5):533–8. [DOI] [PubMed] [Google Scholar]
- 46.Almasi-Hashiani A, Rajaeefard A, Hassanzade J, et al. (2012). Graft survival rate in pediatric renal transplantation: A single center experience. Pak J Med Sci, 28(5):806–11. [Google Scholar]
- 47.Hoseini R, Mirzaiee N, Rahimzadeh N. (2015). Renal transplantation outcome in children with cystinosis. Int J Child Adoles, 1(2):10–2. [Google Scholar]