Abstract
Ciprofol is a novel intravenous anesthetic agent and a highly selective gamma-aminobutyric acid-A receptor agonist, similar to propofol. This is the first report about ciprofol overdose occurring during the maintenance phase of anesthesia for a surgical intervention. The accidental administration of an excessive ciprofol dose to a 37-year-old woman admitted to our hospital for laparoscopic myomectomy occurred during the first 3 minutes of maintenance anesthesia, in which the administered dose was 3.67 mg/kg instead of 0.06 mg/kg. The patient’s bispectral index (BIS) decreased to 0 after 6 minutes and returned to 26 after 23 minutes, after which the surgery was restarted and successfully completed with the planned ciprofol maintenance anesthesia dose. During the 23 minutes after ciprofol overdose, the patient’s vital signs were stable with the lowest mean arterial pressure being 69.3 mmHg. The patient regained consciousness quickly and recovered well after myomectomy. The patient’s BIS decreased progressively, whereas her blood pressure, heart rate, and oxygen saturation did not change significantly. In the present case of ciprofol overdose, the observed stable blood pressure protected against organ injury during laparoscopic myomectomy.
Keywords: Propofol, ciprofol, anesthesia, overdose, bispectral index, myomectomy
Introduction
Ciprofol is a 2, 6-disubstituted phenol derivative1 that was developed for procedural sedation and general anesthesia. It is a gamma-aminobutyric acid-A (GABAA) receptor agonist,2,3 and previous in vitro studies recorded EC50 values of ciprofol and propofol for GABAA receptor-mediated current enhancements of 1.1 × 10−6 and 5.3 × 10−6 M, respectively, suggesting that ciprofol is a more potent sedative than propofol. Previous phase 1 trials revealed that single intravenous ciprofol injections at doses of 0.4 and 0.5 mg/kg had comparable clinical effects as 2.5 mg/kg propofol, and the former drug was well tolerated up to 0.9 mg/kg.4 In 12 completed phase 1 to 3 clinical studies, it was confirmed that ciprofol can be used for the induction and maintenance of anesthesia in adults undergoing surgery, including gastrointestinal endoscopy,5 and for the sedation of patients in the intensive care unit (ICU).6 Ciprofol has been approved in China by the National Medical Products Administration, but it has not yet been authorized by the US Food and Drug Administration. This report describes a case of ciprofol overdose under erroneous operations that did not cause clinically significant injury to the patient, and the findings support the good safety of ciprofol.
Case presentation
A 37-year-old woman with American Society of Anesthesiologists grade 1 uterine fibroids was scheduled to undergo laparoscopic myomectomy as a participant in a phase 3 trial for ciprofol use as an anesthetic for surgical interventions. The present intervention was her first instance of anesthesia and surgery. The patient never smoked, and she had a history of chronic gastritis, thyroid nodule, vitamin D deficiency, and Hashimoto’s thyroiditis but not hypertension, hypotension, allergy, or alcohol consumption. At baseline, the airway assessment (modified Mallampati score) was Class I.
After she entered the operating room, her vital signs were monitored, the peripheral veins of the upper extremity were opened, and catheterization of the lower left radial artery was performed under ultrasound guidance. The basic vital signs of the patient were as follows: blood pressure (BP), 119/77 mmHg; heart rate (HR), 67 beats/minute; respiration rate (RR), 15 breaths/minute; and bispectral index (BIS), 95. Induction anesthesia was initiated with 2 mg of midazolam, 15.25 µg of sufentanil, 0.4 mg/kg ciprofol, and 30 mg of rocuronium bromide, which were successively given as bolus injections according to the protocol requirements. Mechanical ventilation was immediately started following successful endotracheal intubation.
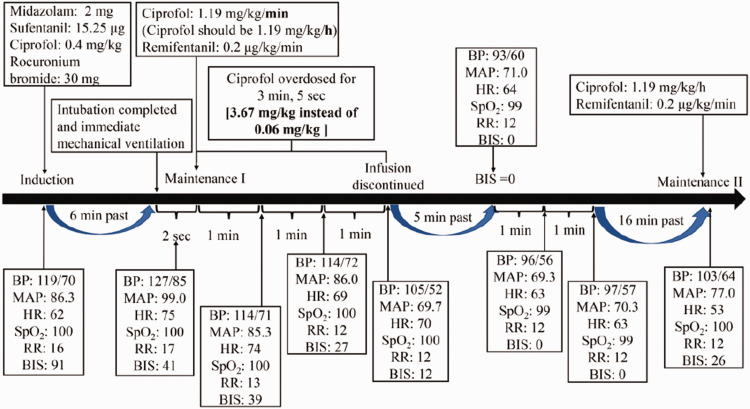
Following the induction of anesthesia, the patient’s vital signs were as follows: BP, 127/85 mmHg; HR, 75 beats/minute; RR, 17 breaths/minute; and BIS, 41. Continuous infusion of 0.2 µg/kg/minute remifentanil and 1.19 mg/kg/hour ciprofol as maintenance medication was initiated. After 1 minute, the patient’s vital signs were as follows: BP, 114/71 mmHg; HR, 74 beats/minute; RR, 13 breaths/minute; and BIS, 39. After 2 minutes, her BP, HR, RR, and BIS were 114/72 mmHg, 69 beats/minute, 12 breaths/minute, and 27, respectively. After her vital signs deteriorated (BP, 105/52 mmHg; HR, 70 beats/minute; RR, 12 beats/minute; and BIS, 12), we decided to decrease the ciprofol dose. During this adjustment, we found that the infusion pump was incorrectly set (the initial rate of the infusion was set at 1.19 mg/kg/minute instead of 1.19 mg/kg/hour) and the infusion was stopped immediately. The infusion speed was incorrectly set for 3.1 minutes, leading to a total dose of 3.67 mg/kg instead of 0.06 mg/kg. Within the next 5 minutes, the patient’s BIS dropped to 0 and remained below 0 for the next 2 minutes, after which the value began to rise gradually to 26 within the subsequent 16 minutes. During this period, the patient’s HR, BP and blood oxygen saturation fluctuated within the normal ranges with the lowest mean arterial pressure (MAP) being 69.3 mmHg (Figure 1). Because the patient’s vital signs other than BIS were stable during the 23-minute observation period, the multilateral communication consultation team decided to continue surgery as planned. Maintenance anesthesia was again initiated with continuous infusions of 0.2 µg/kg/minute remifentanil and 1.19 mg/kg/hour ciprofol when the patient’s vital signs were as follows: BP, 103/64 mmHg; HR, 53 beats/minute; RR, 12 breaths/minute; and BIS, 26. Surgery was resumed 1 minute later. During the operation, the dosage of ciprofol was adjusted over time according to changes in the patient’s vital signs. To reduce bleeding during the operation, 6 units of pituitrin were intravenously delivered 12 minutes after the skin incision. At 33 minutes after the skin incision, the patient’s HR decreased for 4 minutes, with the lowest value being 47 beats/minute. Therefore, 0.4 mg of atropine sulfate was injected. Until the subsequent skin suture after 1 hour, the patient’s vital signs were stable, and 14 minutes after the skin was sutured, the patient regained consciousness with immediate vital signs as follows: BP, 128/88 mmHg; HR, 68 beats/minute; RR, 12 breaths/minute; BIS, 88; and Modified Observer’s Assessment of Awareness/Sedation Scale, 5 points. Consequently, the endotracheal tube was removed. Ten minutes later, the modified Aldrete score was 10 points, and after 1 hour, the patient was returned safely to the ward. When the patient left the operation room, her vital signs were as follows: BP, 123/76 mmHg; HR, 87 beats/minute; RR, 13 breaths/minute; and BIS, 88. A non-blinded researcher went to the ward approximately 1 hour later to check the patient’s postoperative recovery. The patient was conscious; she did not complain of dizziness, nausea, vomiting, limb movement disorder, or other discomforts; and her vital signs were stable. On a subsequent examination, the patient was evaluated by a multidisciplinary team including physicians in neurology, general surgery, anesthesiology, and psychosomatic medicine, who all agreed that the patient’s condition had normalized without brain or other organ dysfunction.
Figure 1.
Vital signs before, during, and after the ciprofol overdose.
On the next day, the patient was conscious, her vital signs were stable, and she had no complaints of special discomfort. She was subsequently discharged. The follow-up examination revealed normal findings on electrocardiogram, and apart from abnormal albumin and total protein concentrations in the blood biochemical report, other blood routine indices were normal. The patient approved publication of her case history.
The reporting of this study conforms to CARE guidelines.7
Discussion
Intraoperative hypotension (IH) is a common side effect during non-cardiac surgical interventions that results in increased risks of 30-day postoperative major adverse cardiac or cerebrovascular events.8 A previous study reported that even short periods with intraoperative MAP < 55 mmHg were associated with acute kidney and myocardial injuries.9 To avoid organ hypoperfusion during anesthesia, a previous study introduced individualized blood pressure management in which high-risk patients received treatments for maintaining systolic blood pressure (SBP) within 10% of their resting reference SBP versus standard-of-care therapy for patients with SBP < 80 mmHg or decreases of >40% of the reference SBP during major surgery. Consequently, individualized treatment led to significantly lower rates of postoperative renal dysfunction and altered consciousness compared with the standard treatment.10 However, another study concluded that to avoid myocardial and kidney injury, anesthetic management of blood pressure can be based on intraoperative MAP without considering the preoperative pressure.11 Propofol-related IH usually occurs after the induction of anesthesia and before the start of surgery, whereas the incidence of IH during propofol-based anesthesia has been reported to be 26%.12,13 Another study found that propofol was commonly administered at 1.8 to 2.2 mg/kg above the recommended doses for the induction of anesthesia, and these increased doses were associated with increased risks of post-induction hypotension, especially in elderly patients.14 In the present case, the patient received a ciprofol overdose of 60 times the planned dose over a period of 3 minutes, but the total amount administered was approximately 4.08-fold higher than the highest ciprofol dose (0.9 mg/kg), which was given as a bolus injection in previous phase 1 trials.4 After ciprofol overdose, the patient’s blood pressure dropped from 120/70 mmHg to 105/55 mmHg at the end of the overdose infusion and stabilized at 95/60 mmHg during the next few minutes before returning to 104/67 mmHg when the maintenance infusion was restarted with the proper ciprofol dose. The heart rate during this period was ranged from 55 to 70 beats/minute. The patient’s MAP decreased to as low as 69.3 mmHg at 9.5 minutes after the overdose injection was started, and MAP was 77 mmHg at the second maintenance anesthesia initiation. This value was far lower than that in a previous case report, which documented a 5-fold overdose of propofol in a 38-day-old infant decreased blood pressure to 60/20 mmHg (MAP ≈ 35 mmHg) before recovering 15 minutes later.15
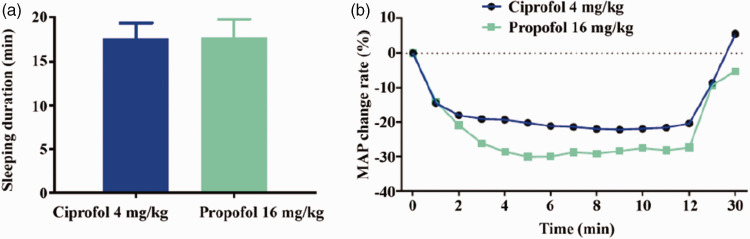
The present data indicated that ciprofol overdose appears to have weaker effects on hemodynamics than an overdose of propofol. To further examine the probability of this assumption, an anesthetic overdose experiment was performed in a recent animal study in which the effects of 4 mg/kg ciprofol were compared with a comparable overdose of 16 mg/kg propofol in a rat model.16 The results illustrated that despite the same effects on sleep duration (Figure 2a) ciprofol overdose led to essentially fewer MAP reductions than a comparable propofol overdose (Figure 2b).
Figure 2.
Results in a rat model comparing ciprofol and propofol overdoses. (a) Sleeping duration of the rats after injections and (b) MAP change rates in the rat groups after drug injections. In male Sprague–Dawley rats weighing 250 to 300 g, a pressure catheter was implanted 0.5 cm in the centripetal direction of the iliac artery branch for telemetry transmission of hemodynamic parameters. The treatments comprised injections of 4 mg/kg ciprofol (n = 4) and 16 mg/kg propofol (n = 3) in the tail veins.
MAP, mean arterial pressure.
One limitation of the present study is that a single patient’s data cannot be extrapolated to a wide range of patients because varying factors such as age and comorbidities are not included in the results of a single case.
In summary, ciprofol overdose did not lead to serious perioperative complications in our patient. Although BIS of the patient was 0 within 5 to 7 minutes, the patient’s orientation and consciousness recovered well after the operation as evaluated by an MDT, and these findings indicate that excessive infusion did not have serious consequences on the patient’s brain function.
Research Data
This article is distributed under the terms of the Creative Commons Attribution 4.0 License (http://www.creativecommons.org/licenses/by/4.0/) which permits any use, reproduction and distribution of the work without further permission provided the original work is attributed as specified on the SAGE and Open Access page (https://us.sagepub.com/en-us/nam/open-access-at-sage).
Research Data for A case report of ciprofol overdose during anesthesia/analgesia and literature review: clinical presentation, blood pressure, and management by Ai Wei, Lina Yang, Shijin Ma, Gang Jin, Mengchang Yang, Jiaojie Zhou in Journal of International Medical Research
The authors declare that there is no conflict of interest.
Funding: Funding information is not available.
Author’s contributions
Conceptualization: MY; Data curation: LY, AW, SM, GJ, MY and JZ; Investigation: MY; Supervision: MY; Validation: LY, AW, SM, GJ, MY and JZ; Writing – original draft: LY, AW, SM, GJ and MY; Writing – review & editing: MY and JZ.
Data availability statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics statement
The study was approved by the Ethical Committee of Sichuan Provincial People’s Hospital (Approval No. 2020-38-1) and written informed consent for treatment and publication of the case report was obtained from the patient.
ORCID iD
Mengchang Yang https://orcid.org/0000-0003-1607-6918
References
- 1.Qin L, Ren L, Wan S, et al. Design, synthesis, and evaluation of novel 2,6-disubstituted phenol derivatives as general anesthetics. J Med Chem 2017; 60: 3606–3617. 2017/04/22. DOI: 10.1021/acs.jmedchem.7b00254. [DOI] [PubMed] [Google Scholar]
- 2.Bai D, Pennefather PS, MacDonald JF, et al. The general anesthetic propofol slows deactivation and desensitization of GABA(A) receptors. J Neurosci 1999; 19: 10635–10646. DOI: 10.1523/JNEUROSCI.19-24-10635.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Babateen O, Jin Z, Bhandage A, et al. Etomidate, propofol and diazepam potentiate GABA-evoked GABAA currents in a cell line derived from human glioblastoma. Eur J Pharmacol 2015; 748: 101–107. 2014/12/17. DOI: 10.1016/j.ejphar.2014.12.001. [DOI] [PubMed] [Google Scholar]
- 4.Teng Y, Ou MC, Wang X, et al. Pharmacokinetic and pharmacodynamic properties of ciprofol emulsion in Chinese subjects: a single center, open-label, single-arm dose-escalation phase 1 study. Am J Transl Res 2021; 13: 13791–13802. 2022/01/18. [PMC free article] [PubMed] [Google Scholar]
- 5.Teng Y, Ou M, Wang X, et al. Efficacy and safety of ciprofol for the sedation/anesthesia in patients undergoing colonoscopy: Phase IIa and IIb multi-center clinical trials. Eur J Pharm Sci 2021; 164: 105904. 2021/06/12. DOI: 10.1016/j.ejps.2021.105904. [DOI] [PubMed] [Google Scholar]
- 6.Hu C, Ou X, Teng Y, et al. Sedation effects produced by a ciprofol initial infusion or bolus dose followed by continuous maintenance infusion in healthy subjects: A phase 1 trial. Adv Ther 2021; 38: 5484–5500. 2021/09/25. DOI: 10.1007/s12325-021-01914-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gagnier JJ, Kienle G, Altman DG, et al. The CARE guidelines: consensus-based clinical case reporting guideline development. Headache 2013; 53: 1541–1547. 2013/11/26. DOI: 10.1111/head.12246. [DOI] [PubMed] [Google Scholar]
- 8.Gregory A, Stapelfeldt WH, Khanna AK, et al. Intraoperative hypotension is associated with adverse clinical outcomes after noncardiac surgery. Anesth Analg 2021; 132: 1654–1665. 2020/11/13. DOI: 10.1213/ane.0000000000005250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Walsh M, Devereaux PJ, Garg AX, et al. Relationship between intraoperative mean arterial pressure and clinical outcomes after noncardiac surgery: Toward an empirical definition of hypotension. Anesthesiology 2013; 119: 507–515. DOI: 10.1097/ALN.0b013e3182a10e26. [DOI] [PubMed] [Google Scholar]
- 10.Futier E, Lefrant JY, Guinot PG, et al. Effect of individualized vs standard blood pressure management strategies on postoperative organ dysfunction among high-risk patients undergoing major surgery: A randomized clinical trial. Jama 2017; 318: 1346–1357. 2017/10/04. DOI: 10.1001/jama.2017.14172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Salmasi V, Maheshwari K, Yang D, et al. Relationship between intraoperative hypotension, defined by either reduction from baseline or absolute thresholds, and acute kidney and myocardial injury after noncardiac surgery: a retrospective cohort analysis. Anesthesiology 2017; 126: 47–65. 2016/10/30. DOI: 10.1097/aln.0000000000001432. [DOI] [PubMed] [Google Scholar]
- 12.Farhan M, Hoda MQ, Ullah H. Prevention of hypotension associated with the induction dose of propofol: A randomized controlled trial comparing equipotent doses of phenylephrine and ephedrine. J Anaesthesiol Clin Pharmacol 2015; 31: 526–530. DOI: 10.4103/0970-9185.169083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mirenda J, Broyles G. Propofol as used for sedation in the ICU. Chest 1995; 108: 539–548. DOI: 10.1378/chest.108.2.539. [DOI] [PubMed] [Google Scholar]
- 14.Phillips AT, Deiner S, Mo Lin H, et al. Propofol use in the elderly population: Prevalence of overdose and association with 30-day mortality. Clin Ther 2015; 37: 2676–2685. 2015/11/10. DOI: 10.1016/j.clinthera.2015.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Seyedhejazi M, Abafattash G, Taheri R. Accidental five fold overdose of propofol for induction in a 38-days-old infant undergoing emergency bilateral inguinal hernia repair. Saudi J Anaesth 2011; 5: 417–418. DOI: 10.4103/1658-354X.87273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liao J, Li M, Huang C, et al. Pharmacodynamics and pharmacokinetics of HSK3486, a novel 2,6-disubstituted phenol derivative as a general anesthetic. Front Pharmacol 2022; 13: 830791. 2022/02/22. DOI: 10.3389/fphar.2022.830791. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This article is distributed under the terms of the Creative Commons Attribution 4.0 License (http://www.creativecommons.org/licenses/by/4.0/) which permits any use, reproduction and distribution of the work without further permission provided the original work is attributed as specified on the SAGE and Open Access page (https://us.sagepub.com/en-us/nam/open-access-at-sage).
Research Data for A case report of ciprofol overdose during anesthesia/analgesia and literature review: clinical presentation, blood pressure, and management by Ai Wei, Lina Yang, Shijin Ma, Gang Jin, Mengchang Yang, Jiaojie Zhou in Journal of International Medical Research
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.