Abstract
Purpose
The goal of this study was to provide recent data on incidence of spinal cord injuries (SCI) in Germany.
Methods
The source of information was data collected via the mandatory submission of ICD-10 GM Codes by German public hospitals after patient discharge. Data from 2013 to 2020 were retrieved from the databases of the Federal Bureau of Statistics. ICD-10 Codes for acute SCI were identified. Statistical analysis was performed using Jamovi and Excel.
Results
A total of 10,360 patients were reported, of whom 58.7% suffered from a cervical, 30.8% a thoracic and 10.4% a lumbar lesion. Two peaks in incidence were observed at approximately 30 and 70 years old. A population-size-adjusted overall incidence of 15.73 (SD 0.77) per million per year was calculated. We calculated the incidences in several subpopulations and discovered significantly higher incidences among males and among those over the age of 60. We discovered that differences in age groups mainly concerned injuries of the upper spine, with the incidence in the lumbar spine being similar among age groups. In addition, we found that while the probability of suffering from SCI increases with age, the relative risk of suffering from a complete injury decreases.
Conclusions
This study closes a long-lasting gap in epidemiological data regarding SCI in Germany, specifically by updating the incidence rates. We found that incidence depends on age, gender and type of lesion. We also provide some new angles for future research, especially considering the relative reduction in complete injuries among the elderly.
Keywords: Spinal cord injury, Incidence, Epidemiology, Germany
Introduction
Spinal cord injuries (SCI) are a worldwide phenomenon that were even mentioned in the scriptures of ancient Egypt [1]. Although significant improvements in acute care, specialized rehabilitation and prevention have been made since then, life expectancy for SCI victims in Germany remains limited and no cure has yet been found [2–4]. This underlines the importance of preventative measures and further research into all aspects of SCI and a constant necessity for re-evaluation of the current situation. This requires reliable epidemiological data at a local level, since cultural, economic and sociological aspects may differ drastically from country to country and therefore have a different influence on risks and benefits when it comes to SCI.
International data suggest an incidence of between 3.6 up and 195.4 per million [5]. More developed countries tend to have a lower incidence rate than their undeveloped counterparts [6]. However some studies have suggested that reported numbers may be unreliable, in particular in undeveloped countries, as national registries or databases are missing [7].
Unfortunately, there is a similar problem in Germany as there are very few epidemiological studies on SCI because there are no national clinical databases that could be used as a basis for such studies. The most reliable sources of data are studies that are using big but not all-encompassing databases like the TraumaRegister DGU. Such a study was performed by Stephan et al. in 2015 using data from 2002 to 2012 [8]. And while this study provides clinical details on patients with spinal cord injuries, it only allows for an indirect approach to incidence which again leads to an approximation at best, as it cannot be expected to include all SCI patients. An older study published in 2004 by Exner provided data from all SCI specialized centres in Germany from 1976 to 2003. An average of 1780 new admissions per year were reported [9]. And although very commendable for its long research period as well as the wide range of hospitals included, incidences may have changed within the last 20 years. The scarcity of information remains unsatisfactory. This study aimed to change the uncertainty when it comes to the basic incidence and age distribution of traumatic spinal cord injuries.
Methods
Data collection
Data were retrieved from the German Federal Bureau of Statistics (Statistisches Bundesamt), Department of the Interior. The Federal Bureau of Statistics collects the ICD-10 GM and OPS Codes of all patients admitted to a German hospital every year and is therefore able to provide detailed information on how many patients were treated as a result of distinct illnesses or injuries [10].
Datasets from 2013 to 2020 of all patients released from hospitals with an S-code diagnosis, corresponding to the WHO group XIX (Injury, poisoning and certain other consequences of external causes) were provided and specific injury types were identified [11]. In particular, injuries to the cervical, thoracic and lumbar spinal cord were identified and extracted.
The ICD-10 GM codes S14.10 to .13 for cervical injuries, S24.10 to .12 for thoracic injuries and S34.10 to.11 and S34.18 for lumbar injuries were identified as targets of interest.
S14.11, S24.11 and S34.10 are complete or AIS type A lesions. S14.10, S24.10 and S35.18 are considered to be SCI of interest but are not considered to be potentially complete (ASIA Impairment Scale type A) lesions.
Statistical analysis
Jamovi (Version 2.3.11, The Jamovi Project, Sydney, Australia) and Excel (Version 2205, Microsoft, Redmond, USA) were used to perform the statistical analysis.
Incidences were calculated using population data also provided by the German Federal Bureau of Statistics for each year of analysis.
The study population was divided into two age groups: those above the age of 60 and those below. Although this division was arbitrary, it was established in recent literature as a common cut-off to divide the population into a potential workforce and those who are close to or in retirement [4].
Statistical comparison between values was performed using Student’s t test. A difference was estimated to be statistically significant at p < 0.05. Effect size is stated as Cohen’s d. Cohen’s d > 0.8 is considered to represent a large effect [12].
Incidence rate is always stated as per million and per year.
Results
A total of 10,360 spinal cord injuries were reported, which translates to a mean of 1295 (SD 63.34) new SCI each year. Of these, 7746 patients (74.8%) were male. A total of 6086 patients (58.7%) suffered from a cervical lesion, 3194 (30.8%) from a thoracic lesion and 1080 (10.4%) from a lumbar lesion.
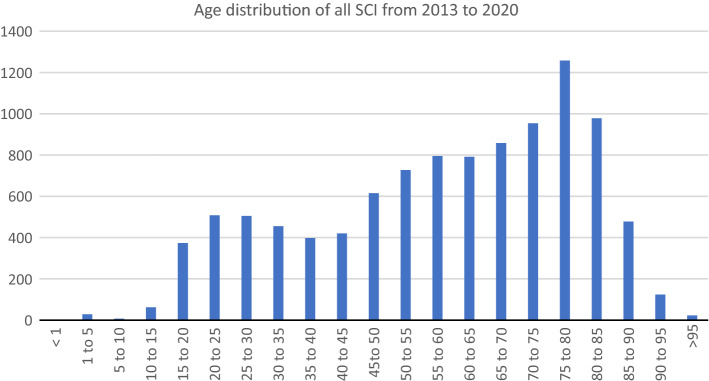
The age distribution is shown in Fig. 1. Two peaks are apparent—one between 20 and 30 years old and one after the age of 70; 5,464 of all patients (52.7%) were over the age of 60.
Fig. 1.
Age distribution of absolute SCI occurrence in 5-year intervals
The absolute number of new SCI each year without adjustment for population size is shown in Table 1.
Table 1.
New SCI each year
| All new SCI | < 60 years old | > 60 years old | |
|---|---|---|---|
| 2013 | 1210 | 610 | 600 |
| 2014 | 1333 | 608 | 725 |
| 2015 | 1321 | 600 | 721 |
| 2016 | 1374 | 663 | 711 |
| 2017 | 1325 | 605 | 720 |
| 2018 | 1294 | 641 | 653 |
| 2019 | 1314 | 599 | 715 |
| 2020 | 1189 | 570 | 619 |
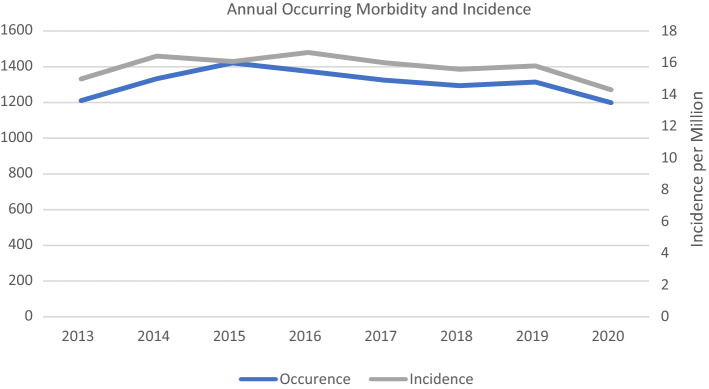
Adjusted for annual population size in each year, the mean total incidence was 15.73 (SD 0.77) per million. Incidences varied slightly and have declined in recent years while overall occurrence remained steady during the analysed period (Fig. 2).
Fig. 2.
Annual morbidity and incidence of SCI per million in Germany
The total incidence of SCI within the male population at a mean of 23.88 (SD 1.50) per million was significantly higher than in the general population throughout the analysed period (p < 0.001).
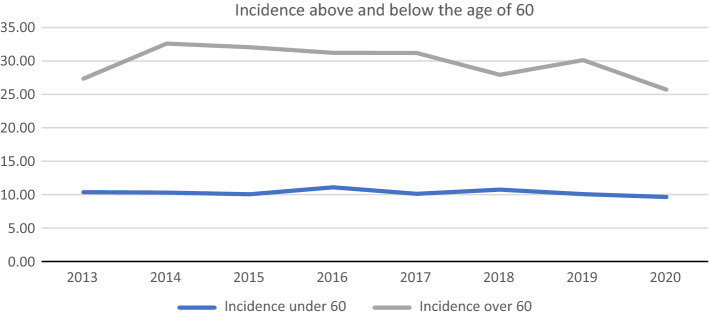
Incidence rates above and below the age of 60 were also calculated (Fig. 3).
Fig. 3.
Incidence per million above and below the age of 60
While the incidence in those below the age of 60 remained roughly the same at a mean of 10.31 (SD 0.45) per million with a very limited range, the incidence in those above the age of 60 has dropped relatively steadily since 2014 from 27.34 to 25.7 in 2020. The mean incidence was 29.77 (SD 2.48) per million, which again differed significantly (p < 0.001) from the incidence in those under the age of 60.
At the same time however, population size is increasing with the main body of growth being made up by those over the age of 60 (Table 2). With an increase in population size of almost 10% in that group alone, the reduction in incidence of only about 4.5% was essentially nullified. Considering the overall incidence only dropped from 14.98 to 14.30 in the observed period, while population size increased by about 3.0%, a decrease in absolute SCI occurrence due to reduced incidence rates is unlikely and was not observed.
Table 2.
Changes in population size above and below the age of 60
| Population size | < 60 years old | > 60 years old | |
|---|---|---|---|
| 2013 | 80,767,463 | 58,819,703 | 21,947,760 |
| 2014 | 81,197,537 | 58,955,849 | 22,241,688 |
| 2015 | 82,175,684 | 59,673,450 | 22,502,234 |
| 2016 | 82,521,653 | 59,730,668 | 22,790,985 |
| 2017 | 82,792,351 | 59,707,587 | 23,084,764 |
| 2018 | 83,019,213 | 59,641,767 | 23,377,446 |
| 2019 | 83,166,711 | 59,428,258 | 23,738,453 |
| 2020 | 83,155,031 | 59,065,258 | 24,089,773 |
The change in absolute occurrence and incidence in all age groups can be seen in Fig. 4a, b. Only the group comprising those between the age of 70–80 showed a relevant decrease over the observed period, while the incidence in those between the age of 60 to 70 seemingly increased. Considering the sideways trend of incidences in all age groups, this may be due to ongoing changes within the demographic structure, as some generations showed a higher birth rate than others.
Fig. 4.
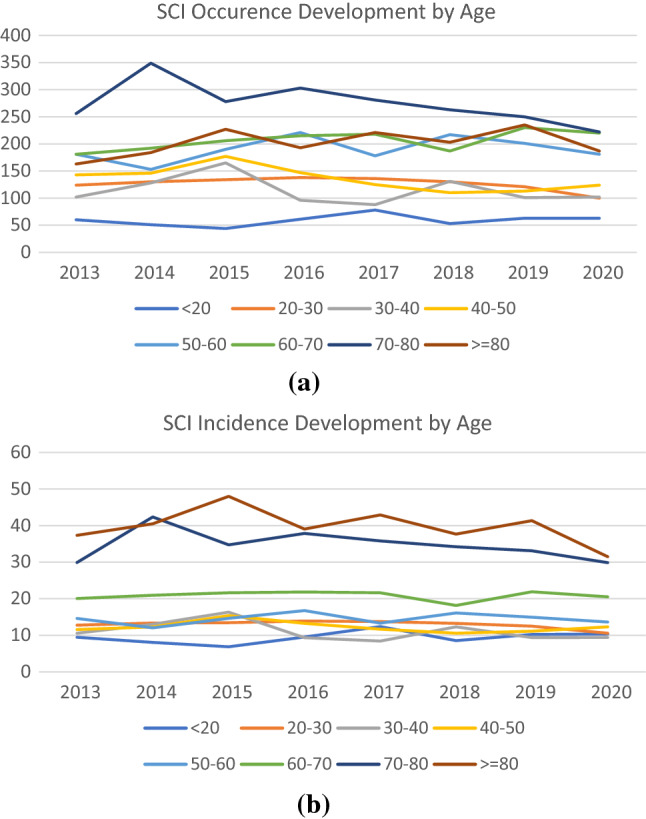
a Change in SCI occurrence by year and age. b Change in SCI incidence per million by year and age
The mean incidence of complete (ASIA Impairment Scale type A) SCI in the two age groups was also calculated and a t test was performed [13]. The incidence of complete SCI was 5.08 (SD 0.65) per million and differed significantly from the overall SCI incidence (p < 0.001). Additional incidence rates for each spinal region and a general overview are presented in Table 3.
Table 3.
Incidences per million per year (SD = Standard Deviation)
| Mean | Median | SD | Minimum | Maximum | |
|---|---|---|---|---|---|
| Incidence of all SCI | 15.727 | 15.902 | 0.770 | 14.299 | 16.650 |
| Incidence of complete SCI | 5.180 | 5.059 | 0.659 | 4.353 | 6.240 |
| Incidence over 60 | 29.765 | 30.655 | 2.484 | 25.700 | 32.600 |
| Incidence under 60 | 10.305 | 10.220 | 0.449 | 9.650 | 11.100 |
| Incidence male | 23.877 | 723.762 | 1.502 | 21.492 | 26.595 |
| Incidence female | 7.535 | 8.646 | 2.271 | 3.810 | 9.309 |
| Incidence cervical | 9.238 | 9.352 | 0.626 | 8.262 | 10.058 |
| Incidence thoracic | 4.849 | 4.926 | 0.211 | 4.413 | 5.038 |
| Incidence lumbar | 1.639 | 1.651 | 0.185 | 1.241 | 1.823 |
| Incidence cervical under 60 | 4.942 | 4.937 | 0.378 | 4.405 | 5.609 |
| Incidence cervical over 60 | 20.362 | 21.433 | 1.971 | 17.061 | 22.049 |
| Incidence thoracic under 60 | 3.738 | 3.822 | 0.262 | 3.352 | 4.120 |
| Incidence thoracic over 60 | 7.727 | 7.596 | 0.634 | 7.015 | 8.992 |
| Incidence lumbar under 60 | 1.626 | 1.646 | 0.263 | 1.022 | 1.878 |
| Incidence cervical complete | 2.326 | 2.391 | 0.275 | 1.958 | 2.611 |
| Incidence thoracic complete | 2.368 | 2.441 | 0.264 | 2.012 | 2.623 |
| Incidence lumbar complete | 0.540 | 0.305 | 0.488 | 0.195 | 1.407 |
| Incidence cervical complete | 2.326 | 2.391 | 0.275 | 1.958 | 2.611 |
| Incidence complete under 60 | 3.851 | 3.845 | 0.333 | 3.471 | 4.556 |
| Incidence complete > 60 | 7.610 | 7.421 | 0.968 | 6.517 | 9.307 |
The biggest differences from the mean SCI incidence were seen in males and in those aged over 60 years old.
A particularly big impact of age was apparent in cervical SCI as those who were over the age of 60 were about four times more likely to suffer from cervical SCI than those below the age of 60.
Patients of all ages were significantly less likely to suffer from a complete lumbar SCI, and while there was a twofold higher risk of suffering from a cervical lesion than from a thoracic lesion, there was no significant increase in risk of suffering from a complete cervical lesion than from a complete thoracic lesion (p = 0.363).
At the same time, those who were over 60 years old were only two times as likely to suffer from complete thoracic SCI, while the incidence of complete lumbar SCI did not differ between age groups (p = 0.41).
The incidence of complete SCI in those over the age of 60 was almost double that in those below the age of 60. However, this relationship did not reflect the overall ratio of SCI, which occurred almost three times as often over the age of 60. Incomplete injuries are therefore more uncommon among Germans under the age of 60, when adjusted for overall incidence.
Table 4 shows the results of one-sample t tests of some incidences against overall SCI incidence. The incidence in males and those over and under the age of 60 was shown to differ significantly (p < 0.05) from the overall mean SCI incidence with a large effect size of over 0.8 in all cases.
Table 4.
One-sample t test against mean overall SCI incidence
| p | Effect size | |
|---|---|---|
| Incidence male | < 0.01 | 4.728 |
| Incidence under 60 | < 0.01 | − 12.083 |
| Incidence over 60 | < 0.01 | 5.651 |
Ha μ ≠ 15.727
In addition, incidences in those groups under and over the age of 60 were shown to differ significantly from each other for all types of SCI except lumbar SCI, where there was no significant difference between those under and over the age of 60 years old (p = 0.612). The incidence of lumbar SCI therefore does not appear to depend upon age.
Discussion
Knowledge about the incidence and distribution of SCI among the population as well as potential differences in risks of different injury types could lead to a new approach in prevention and aftercare. Reliable epidemiological data are the groundwork for future research addressing potential risk factors, preventative measures and the economic impacts of SCI.
This study’s aim was to close a long-lasting gap in SCI research in Germany, where imprecise approximations have been used to determine SCI incidence and reliable data are scarce.
We used a different approach to achieve a more precise estimation of incidences and distribution by relying on data collected by a federal authority instead of using a common single or multicentre approach. Besides delivering a more complete picture, this approach will be easier to reproduce in future research if newer data are required.
Even though this study has delivered some long-needed metrics, it is not without its limitations.
First of all, only hospitals that are using the diagnosis-related groups (DRG) system as their means of treatment compensation are required to submit data to the federal authorities. This however does not affect the study’s meaningfulness in a relevant way as essentially all primary care facilities in Germany are using and required to use the DRG system. The hospitals are also only required to submit diagnoses upon patient discharge or death, which means that a submitted SCI may not have occurred in the same year as it was documented. However, this should not significantly influence the overall statistics, as it is a recurring phenomenon, and it should therefore only influence the precision of individual datasets for each year.
Secondly, no clinical aspects that are not implicated within the analysed ICD-10 GM code could be included in the analysis, as there is no way to connect a patient to different diagnoses.
In addition, the codes identified for analysis include diagnoses that are not defined as precisely as they would need to be to fit into certain categories. These include S14.10, S24.10 and S34.18 in particular. S14.10 and S24.10 are indeterminable lesions of the respective spinal region but are most likely incomplete lesions and sometimes those that are diagnosed by radiological diagnostics without a respective clinical manifestation. S34.18 describes “other lesions of the lumbar spinal cord” and therefore may include a variety of lesions but again is most likely an incomplete lesion without clinical significance. These three diagnoses are uncommon (about 5% of all SCI each year) and are only used if no other diagnosis can reasonably be applied because their use has negative economic implications for the respective hospital.
Fifty-nine patients (0.6% of the total study population) were reported to be 5 or less years old at the time of their SCI. Diagnosis and determination of complete or incomplete injuries relies heavily on the ASIA Impairment Scale (AIS) or the international standards for neurological classification of spinal cord injury (ISNCSCI). Current literature suggests that ISNCSCI may however not be a reliable tool to assess children under the age of 6 and therefore misdiagnoses could have affected this study’s outcome [14, 15].
Overall, this study’s results are similar to those of Stephan et al., from 2014. Males were reported to make up 72.7% of SCI victims versus 74.8% in this study; 51.8% involved the cervical spine versus 58.7% in this study; 32.4% involved the thoracic spine versus 30.8% here and 18.4% versus 10.4% involved the lumbar spine [8].
However, Stephan et al. only reported 4,285 patients suffering from SCI within the period from 2002 to 2012. Considering this study’s findings and earlier incidence reports like those from Exner in 2004 suggests a far higher incidence than can be calculated from the TraumaRegister DGU data and shows the limitations of epidemiological studies that rely on limited registries [8, 9].
We also found that while Stephan et al. reported around 65.4% of cervical lesions to be complete SCI, only about 25.6% of the cervical lesions in our study were compete injuries. Differences in thoracic and lumbar lesions were less prominent [8]. This suggests either an overreporting of complete cervical lesions or more likely an underreporting of incomplete cervical lesions to the Trauma Register DGU. This discrepancy might best be addressed and further investigated in a future cohort study conducted in a specialized care centre.
As shown herein, certain groups within the population seem to be at a particular risk of SCI with significant deviations from the overall incidence within these groups (Table 3). Male sex as well as age were discovered to correlate positively with SCI incidence. These modalities have been independently reported as potential risk factors within the international literature. The age distribution with two peaks as shown in Fig. 1 is also a common finding among international studies [6, 16–18]. The cause of SCI in both age peaks is most likely different. However, the federal bureau of statistics does not differentiate between different causes of SCI. We therefore can only base our assumptions on data published by other working groups. As research regarding epidemiological characteristics of SCI patients, especially considering causes of injury in relation to age, is rare in Germany, we use data from neighbouring countries in Europe with similar standards of living, demographics and health care systems. Smith et al. found that in Ireland people who suffer from traumatic SCI because of falls are significantly older and in-line with our discovered age peak [18]. Jonviea et al. discovered that in Switzerland younger people between 16 and 30 years old suffer more often from traumatic SCI because of sports, leisure activity or transport related accidents. Whereas low-level falls were the main reason for people above the age of 76 years to suffer from SCI [19]. We conclude that the reason for SCI in both age peaks differs because of lifestyle and comorbidities. While younger people are taking a more active role in society and are more risk taking, older people are most likely mainly at risk because of deteriorating physical capabilities, e.g. bone density and muscle strength. The prevention of falls is therefore of considerable importance.
Interestingly, we found that while the overall incidence of SCI and complete SCI increased with age, the relative probability of suffering from a complete injury decreased from 37.4% under the age of 60 to 25.6% over the age of 60. This may be due to different injury mechanisms within the two age groups but requires further investigation in future research.
Incidence and occurrence showed a sideward trend up until 2019. A drop from 2019 to 2020 could be observed. Similar findings were made by Maleitzke et al. with regard to overall orthopaedic trauma injury incidence in a level 1 trauma centre [20]. These findings were directly related to the COVID-19 shutdown in Germany. We therefore conclude that our observed drop is most likely also related to the pandemic and its consequences. The reduction in workplace related injuries, motor vehicle accidents and overall decrease in leisure activities are the most likely causes for the decline in severe spinal injuries. Further research into the specific reasons behind the decrease in spinal cord injuries during the pandemic could help identify factors suitable for preventative measures in the future.
Overall, the sideways trend of SCI incidence within the observed period in combination with an increasing population size, especially among those over the age of 60 (Table 2), indicates a continuing need for specialized care and an increase in efforts regarding SCI prevention and rehabilitation.
Conclusions
This study was able to strengthen previous findings as well as close a long-lasting gap by delivering new data concerning the incidence of traumatic spinal cord injury in Germany.
We found that the incidence of SCI in Germany has decreased in comparison to findings from 20 years ago while remaining relatively steady over the research period. We also made some new observations on distribution in comparison to more recent studies addressing the epidemiological details of SCI patients.
Funding
Open Access funding enabled and organized by Projekt DEAL. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Data availability
The datasets generated and/or analysed during the current study are available from the corresponding author on reasonable request.
Declarations
Conflict of interest
There are no conflicts of interest present.
Ethical approval
Data were already completely anonymized before extraction from the national database and no ethical concerns needed to be addressed.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Hughes JT. The Edwin Smith surgical papyrus: an analysis of the first case reports of spinal cord injuries. Spin Cord. 1988;26(2):71–82. doi: 10.1038/sc.1988.15. [DOI] [PubMed] [Google Scholar]
- 2.Thietje R. Epidemiologie, Ätiologie und Mortalität bei Querschnittlähmung. Neuroreha. 2016;08(3):105–109. doi: 10.1055/s-0042-112079. [DOI] [Google Scholar]
- 3.Thietje R, Kowald B, Schulz AP, Northmann M, Hirschfeld S. Entstehungsursachen, Lebenserwartung und Todesursachen bei Menschen mit traumatischer Querschnittlähmung: eine monozentrische Analyse von 190 Fällen. Trauma Berufskrankh. 2018;20(2):151–156. doi: 10.1007/s10039-018-0383-x. [DOI] [Google Scholar]
- 4.Thietje R, Kowald B, Böthig R, et al. Long-term survival and causes of death in patients below the age of 60 with traumatic spinal cord injury in Germany. J Clin Med. 2022;11(1):26. doi: 10.3390/jcm11010026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jazayeri SB, Beygi S, Shokraneh F, Hagen EM, Rahimi-Movaghar V. Incidence of traumatic spinal cord injury worldwide: a systematic review. Eur Spine J. 2015;24(5):905–918. doi: 10.1007/s00586-014-3424-6. [DOI] [PubMed] [Google Scholar]
- 6.Kang Y, Ding H, Zhou H, et al. Epidemiology of worldwide spinal cord injury: a literature review. JN. 2017;6:1–9. doi: 10.2147/JN.S143236. [DOI] [Google Scholar]
- 7.Rahimi-Movaghar V, Sayyah MK, Akbari H, et al. Epidemiology of traumatic spinal cord injury in developing countries: a systematic review. NED. 2013;41(2):65–85. doi: 10.1159/000350710. [DOI] [PubMed] [Google Scholar]
- 8.Stephan K, Huber S, Häberle S, et al. Spinal cord injury–incidence, prognosis, and outcome: an analysis of the TraumaRegister DGU. Spine J. 2015;15(9):1994–2001. doi: 10.1016/j.spinee.2015.04.041. [DOI] [PubMed] [Google Scholar]
- 9.Exner G. Der Arbeitskreis „Querschnittlähmungen“ des Hauptverbandes der gewerblichen Berufsgenossenschaften in Deutschland. Trauma Berufskrankh. 2004;6(2):147–151. doi: 10.1007/s10039-004-0877-6. [DOI] [Google Scholar]
- 10.BfArM: ICD-10-GM Version 2022. Accessed May 30, 2022. https://www.dimdi.de/static/de/klassifikationen/icd/icd-10-gm/kode-suche/htmlgm2022/. Accessed 20 May 2022
- 11.ICD-10 Version 2010. https://icd.who.int/browse10/2010/en#/XIX. Accessed 2 June 2022
- 12.Lakens D. Calculating and reporting effect sizes to facilitate cumulative science: a practical primer for t-tests and ANOVAs. Front Psychol. 2013;4:863. doi: 10.3389/fpsyg.2013.00863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Roberts TT, Leonard GR, Cepela DJ. Classifications in brief: American spinal injury association (ASIA) Impairment Scale. Clin Orthop Relat Res. 2017;475(5):1499–1504. doi: 10.1007/s11999-016-5133-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mulcahey MJ, Gaughan J, Betz RR, Johansen KJ. The international standards for neurological classification of spinal cord Injury: reliability of data when applied to children and youths. Spinal Cord. 2007;45(6):452–459. doi: 10.1038/sj.sc.3101987. [DOI] [PubMed] [Google Scholar]
- 15.Mulcahey MJ, Gaughan JP, Chafetz RS, Vogel LC, Samdani AF, Betz RR. Interrater reliability of the international standards for neurological classification of spinal cord injury in youths with chronic spinal cord injury. Arch Phys Med Rehabil. 2011;92(8):1264–1269. doi: 10.1016/j.apmr.2011.03.003. [DOI] [PubMed] [Google Scholar]
- 16.Yang R, Guo L, Wang P, et al. Epidemiology of spinal cord injuries and risk factors for complete injuries in Guangdong, China: a retrospective study. PLoS ONE. 2014;9(1):e84733. doi: 10.1371/journal.pone.0084733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nijendijk JH, Post MW, van Asbeck FW. Epidemiology of traumatic spinal cord injuries in the Netherlands in 2010. Spin Cord. 2014;52(4):258–263. doi: 10.1038/sc.2013.180. [DOI] [PubMed] [Google Scholar]
- 18.Smith É, Fitzpatrick P, Lyons F, Morris S, Synnott K. Prospective epidemiological update on traumatic spinal cord injury in Ireland. Spin Cord Ser Cases. 2019;5(1):1–4. doi: 10.1038/s41394-019-0152-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chamberlain JD, Deriaz O, Hund-Georgiadis M, Meier S, Scheel-Sailer A, Schubert M, Stucki G, Brinkhof MW. Epidemiology and contemporary risk profile of traumatic spinal cord injury in Switzerland. Inj Epidemiol. 2015;2(1):28. doi: 10.1186/s40621-015-0061-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Maleitzke T, Pumberger M, Gerlach UA, Herrmann C, Slagman A, Henriksen LS, von Mauchenheim F, Hüttermann N, Santos AN, Fleckenstein FN, Rauch G, Märdian S, Perka C, Stöckle U, Möckel M, Lindner T, Winkler T. Impact of the COVID-19 shutdown on orthopedic trauma numbers and patterns in an academic Level I Trauma Center in Berlin. Germany PLoS One. 2021;16(2):e0246956. doi: 10.1371/journal.pone.0246956. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and/or analysed during the current study are available from the corresponding author on reasonable request.