Key summary points
Aim
Antimicrobials are the most frequently prescribed drugs in long-term care facilities (LTCF). Antibiotic stewardship programs (ASP) are coordinated interventions promoting the responsible use of antibiotics to improve patient outcomes and reduce antibiotic-resistant bacteria. The objectives are to evaluate the effectiveness of a pharmacist-led ASP in a LTCF, to characterize antibiotic therapy and assess the appropriateness of antibiotic prescriptions.
Findings
Educational interventions and weekly prospective audits and feedback have resulted in significant decreases in antibiotic use and costs of antibiotics.
Message
Inappropriate use of antibiotics is high in LTCF so it is essential to implement an ASP to improve appropriateness.
Keywords: Antibiotic stewardship, Drug resistance, Long-term care, Inappropriate prescribing, Pharmacists
Abstract
Methods
A prospective quasi-experimental study to implement an ASP in a LTCF. Antibiotic prescriptions for suspected infections initiated in any setting for LTCF residents were included. We assessed appropriateness and prospective audits and feedback of each inappropriate antimicrobial prescription were carried out. Associations of variables with appropriate antibiotic prescribing were estimated using logistic regression.
Results
A total of 416 antibiotic prescriptions were included. The mean consumption of antibiotics was reduced from 63.2 defined daily doses per 1000 residents days (DRD) in the preintervention period to 22.8 in the intervention period (− 63.8%), with a significant drop in fluoroquinolones (81.4%). Overall, 46.6% of antibiotic prescriptions were judged inappropriate, mainly because of a use not recommended in treatment guidelines (63.2%). Multivariable analysis showed that empirical therapy, some classes of antibiotics (cephalosporins, fluoroquinolones, fosfomycin calcium, macrolides) and prescription initiation in the emergency department were independent predictors of antimicrobial inappropriateness.
Conclusions
Pharmacist-led ASP in a LTCF has being effective in reducing consumption of antibiotics by improving appropriateness of treatment decisions. However, ASP should include interventions in the emergency department because of the high inappropriate use in this setting.
Introduction
As a result of the increase in the population age, the number of long-term care facilities (LTCF) beds has raised. Residents in LTCF are at high risk of infections due to multiple comorbidities, frailty and immunosenescence that lead to frequent antibiotic prescribing [1]. Roughly between one-half and two-thirds of LTCF residents are prescribed antimicrobials each year [2]. The particular characteristics of elderly contribute to difficulties in diagnosing and treating infections in LTCF residents, including the lack of typical signs (fever, leukocytosis), the presence of concurrent illnesses with associated nonspecific symptoms and the high prevalence of cognitive impairment that make it difficult to communicate symptoms [3]. In addition, most of LTCF do not have on-site laboratory and radiological facilities. It may lead to unnecessary, suboptimal or inappropriate antimicrobial prescription in LTCF. Up to 75% of antibiotic prescriptions may be unnecessary, even when necessary, the antibiotics prescribed are often excessively broad spectrum or longer duration [4]. The overuse and misuse of antibiotics are associated with increased rates of adverse drug events and future infections such as those caused by Clostridium difficile and antimicrobial resistance bacteria (AMR) [5]. Furthermore, given that one-third of residents are estimated to be colonized with multidrug-resistant organisms (MDRO), LTCF serve as reservoirs [6]. Thus, there is an immediate need to optimize antibiotic use in this population to slow the emergence and spread of antimicrobial-resistant organisms [7].
In the acute care hospital, antibiotic stewardship programs (ASP) have been successful at improving the quality of patient care and safety, reducing potentially inappropriate prescribing [8]. Although, it is less likely that LTCF can implement a formal ASP within this resource limited environment, growing attention has been given to improving antibiotic use in LCTF [9–12]. However, little is known about the contribution and appropriateness of antibiotic therapy initiated in other settings such as the emergency department (ED) [13]. As recommended by guidelines published by the Infectious Diseases Society of America (IDSA) and the Society for Healthcare Epidemiology of America (SHEA), ASP teams should include an infectious disease (ID) physician and a clinical pharmacist with ID training [14]. LTCF may not have access to the traditional ASP team given resource restraints. In this environment, where ID physician support is not available, the clinical pharmacist who has a consistent presence in LTCF can play a key role in promoting the optimal use of antimicrobial agents, monitoring and auditing the prescriptions, and educating health professionals [15, 16].
Therefore, the objectives of this study are to evaluate the effectiveness of a pharmacist-led ASP in optimizing antimicrobial use in a LTCF by educational interventions, to characterize antibiotic therapy for LTCF residents and assess the appropriateness of antibiotic prescriptions.
Method
A prospective quasi-experimental study was conducted to implement an ASP in a public 264-bed LTCF in Spain. The ASP team consisted of an ID physician, an ID trained clinical pharmacist, the facility medical director and a microbiologist. The study period was divided into two periods of 18 months each. During the preintervention period (January 1, 2018–June 30, 2019), baseline information of local patterns of antibiotic resistance and antimicrobial utilization were collected. Second phase, aimed at improving appropriate antibiotic use, took place from July 1, 2019 to December 31, 2020. The development of the intervention began with sessions between ASP team and LTCF physicians to present the guidelines on antibiotic prescribing for the most commonly encountered infections in LTCF [17] and provide educational materials (i.e. leaflet on hand hygiene, booklets for antibiotic prescribing) and antimicrobial consumption corresponding to the preintervention period. Furthermore, during the intervention period, the ID pharmacist identified residents with prescriptions of drugs belonging to Anatomical Therapeutical Chemical (ATC) class J01 (antibacterials for systemic use) for suspected infections through the electronic prescribing. Then, pharmacist made weekly site visits to LTCF to collect data by review of the medical records. We only included antibiotics associated with a diagnosis of lower respiratory tract infection (LRTI), skin and soft-tissue infection (SSTI) or urinary tract infection (UTI), given their high prevalence compared with other infections in LTCF. We excluded confirmed positive COVID-19 infections without suspected bacterial or fungal co-infection and also prophylactic antibiotic prescriptions (Fig. 1). Each antibiotic prescription was assessed for appropriateness by ID pharmacist according to the Loeb consensus criteria [18] and antimicrobial guidelines [19]. ID physician was consulted when necessary. Prospective audits and feedback of each inappropriate antimicrobial prescription were carried out. ID pharmacist interacted directly with the prescriber in person or by phone to discuss the treatment and formulate recommendations to improve antimicrobial therapy in next prescriptions, focused specially in fluoroquinolones and amoxicillin-clavulanic acid. The pharmacist carried out this activity during the daily working day along with other activities, that is, part-time.
Fig. 1.
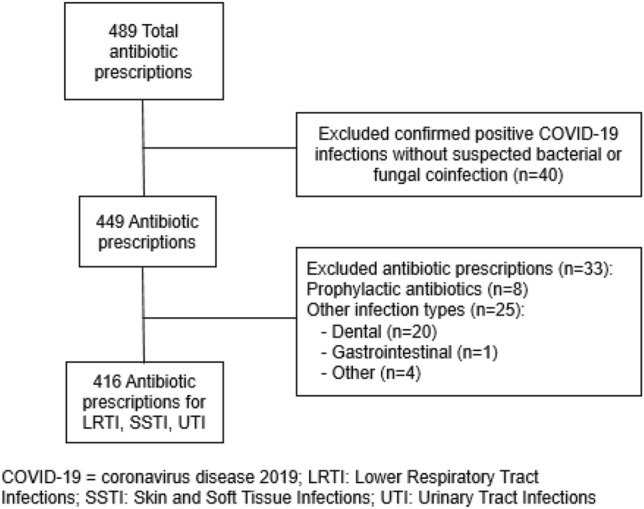
Antibiotic prescriptions flow chart
We obtained demographic and clinical characteristics of residents including sex, age, allergic reactions to antibiotics, comorbidities, Charlson comorbidity index age-adjusted score, functional status (fecal and/or urinary incontinence, functional dependence, pressure sores) and medical devices, including urinary catheter, vascular catheter for dialysis, tracheostomy and feeding tube. Also, other risk factors such as a surgery in the last thirty days and antibiotic exposure in the last 6 months were identified. Variables related to infection and antibiotic prescription were collected: type of treatment (empirical, targeted or prophylaxis), indication for antibiotic (LRTI, SSTI, UTI and others), antibiotic start and end date, antibiotic class, dosage, route and frequency, signs and symptoms on day of prescription and tracking, previous antibiotic therapy (last 2 weeks), microbiology data and setting of prescription initiation classified as ED, hospital or primary care (HPC) and LTCF and 30-day clinical outcome.
The primary outcome was change in antibiotic use measured as total consumption for preintervention period versus intervention period. Total consumption of antibiotics was measured as the mean defined daily doses (DDD) per 1000 residents per day (DRD). DDD were calculated using World Health Organization (WHO) definitions. Occupied beds were used in the denominator. Secondary outcomes were change in costs of antimicrobials, hospitalization and mortality, as well as appropriateness of antibiotic prescriptions classified as unnecessary, inappropriate and suboptimal antimicrobial use [19].
Statistical analysis
Qualitative variables are presented with their frequency distribution and percentages. Quantitative variables were summarized with mean and standard deviation or median and interquartile range in case of asymmetry. Chi-square or Fisher’s test was used to compare categorical data and Student’s t test for normally distributed continuous variables and Mann–Whitney U test for non-normally distributed continuous variables. To identify independent predictors of appropriateness, we performed an univariable logistic regression. We also analyzed the collinearity between the variables. Subsequently, variables that showed statistical significant in the univariable analysis and those with p value < 0.2 were included in a multivariate model. Relative risks were expressed as odds ratios (OR) and 95% confidence intervals. All reported p value < 0.05 were considered as statistically significant. The area under the receiver operating characteristic (ROC) curve was calculated to assess the discrimination of the prediction score. For the statistical analysis, the software SPSS Statistics for Windows, Version 21.0 (IBM Corp, Armonk, NY, USA) was used.
Ethics statements
The study was designed and performed according to the Helsinki Declaration and approved by the Ethics Committee of Jaén Province. The subjects who participated in the study signed and informed consent for data collection.
Results
A total of 416 antibiotic prescriptions were included during the 18-months study period (Fig. 1) corresponding to 159 residents. The characteristics of the population are shown in Table 1.
Table 1.
Demographic and clinical characteristics of total population
| Characteristic | Total N = 159 |
|---|---|
| Age (years), mean (SD) | 83.2 (9.6) |
| Sex, n (%) | |
| Male | 113 (43.6) |
| History of antibiotic allergy, n (%) | |
|
Penicillin allergy Other antibiotic allergy |
14 (8.8) 5 (3.1) |
| Charlson comorbidity index age adjusted, mean (SD) | 6.1 (2.0) |
| Comorbidities, n (%) | |
|
Myocardial infarction Congestive heart failure Peripheral vascular disease Cerebrovascular accident or transient isquemic attack Cognitive impairment COPD Peptic ulcer disease |
16 (10.1) 15 (9.4) 17 (10.7) 32 (20.1) 87 (54.7) 18 (11.3) 11 (6.9) |
| Liver disease | |
|
Mild Moderate to severe |
3 (1.9) 0 (0) |
| Diabetes mellitus | |
|
Uncomplicated End-organ damage Hemiplegia Moderate to severe chronic kidney disease Solid tumor Leukemia/lymphoma AIDS |
49 (30.8) 11 (6.9) 0 (0) 40 (25.2) 6 (3.8) 0 (0) 0 (0) |
| Functional status, n (%) | |
|
Bowel and/or bladder incontinence Functional dependence Pressure sores |
68 (42.8) 78 (49.1) 8 (5.0) |
| Medical devices, n (%) | |
|
Urinary catheter Vascular catheter for dialysis Tracheostomy Feeding tube |
6 (3.8) 0 (0) 1 (0.6) 5 (3.1) |
AIDS acquired immune deficiency syndrome, COPD chronic obstructive pulmonary disease, SD standard deviation
Changes in antibiotic use and costs of antibiotics for preintervention period versus intervention period are described in Table 2. The mean bed occupancy was 234.7 ± 8.6 in the preintervention period and 213.2 ± 9.2 in the intervention period. Total consumption of antibiotics was reduced from 63.2 DRD in the preintervention period to 22.8 DRD in the intervention period. In addition, there has been a significant drop in consumption of fluoroquinolones (81.4%) and amoxicillin-clavulanic acid (79.3%), also in fosfomycin calcium and macrolides. Costs of antibiotics decreased significantly to almost half (p = 0.013). No differences in hospitalization were found, with a total of 83 hospital admissions in the preintervention period and 86, in the intervention period, just like in mortality (82 vs. 76 deaths; p < 0.05).
Table 2.
Comparison of consumption and costs of antibiotics between periods
| DRD, mean/month (SD) | Preinterventiona | Interventionb | % reduction | p value |
|---|---|---|---|---|
| Total antibiotics | 63.2 (15.1) | 22.8 (13.7) | 63.8 | < 0.001 |
| Penicillins (amoxicillin, cloxacillin) | 4.6 (3.4) | 3.3 (2.2) | 28.3 | 0.282 |
| Amoxicillin-clavulanic acid | 20.8 (5.0) | 4.3 (3.3) | 79.3 | < 0.001 |
| Cephalosporins | 9.6 (6.9) | 5.8 (4.9) | 39.6 | 0.052 |
| Fluoroquinolones | 18.8 (9.5) | 3.5 (2.4) | 81.4 | < 0.001 |
| Fosfomycin calcium | 1.4 (0.9) | 0.6 (1.0) | 57.1 | 0.002 |
| Fosfomycin-tromethamine | 1.7 (1.0) | 1.1 (0.6) | 35.3 | 0.058 |
| Macrolides | 2.8 (2.7) | 2.3 (7.0) | 17.9 | 0.013 |
| Sulfonamides | 1.6 (1.3) | 0.9 (0.6) | 43.8 | 0.070 |
| Other antibiotics | 1.9 (1.7) | 1 (1.6) | 47.4 | 0.055 |
| Costs of antibiotics (euros), median/trimester (IQR) | 818.9 (688.7–987.4) | 438.0 (237.7–720.6) | 46.5 | 0.013 |
DRD defined daily doses (DDD) per 1000 residents per day, IQR interquartile range, SD standard deviation
aJanuary 1, 2018–June 30, 2019
bJuly 1, 2019 to December 31, 2020
Overall, fosfomycin-tromethamine was the most commonly prescribed antibiotic (25.0%), followed by cephalosporins (18.8%), amoxicillin-clavulanic acid (15.9%) and fluoroquinolones (13.0%). Polytherapy was only used in 2.6% of episodes. The most common indication for antibiotic use was UTI (43.3%), followed by LRTI (34.6%), and SSTI (22.1%). For UTI, fosfomycin-tromethamine was the most commonly prescribed antibiotic (57.8%), followed by cephalosporins (11.1%). LRTI was treated with cephalosporins (36.8%), amoxicillin-clavulanic acid (24.3%) and fluoroquinolones (21.5%). Penicillins (amoxicillin or cloxacillin) were the most often prescribed class of antibiotics for SSTI (43.5%), followed by amoxicillin-clavulanic acid (17.4%). Targeted therapy involved 16.8% of prescriptions, UTI being the most frequent (62.9%). Intravenous route was used only in 4.8% of cases. Median treatment duration was 5 (IQR: 1–7) days. Only 9.4% prescriptions were for longer than 7 days of duration. Sample collection was carried out in 29.6%, the majority (88.6%) before initiating antibiotic therapy: 74.0% uroculture, 16.3% exudate culture, 4.1% sputum culture. A positive result was found in 82.9% of cultures (85.3% monomicrobial infection). The most prevalent microorganisms isolated were the Gram-negative bacteria (87.3%). The majority of antibiotic prescriptions were initiated within the LTCF (84.1%), while 12.7% by the ED and 3.2% by HPC.
Considering that antibiotic prescriptions may be inappropriate for one or more types, we found 231 different types of inappropriateness [20] in 194 unsuitable antimicrobial prescriptions:
Unnecessary (n = 39, 16.9%): use of antimicrobials for non-infectious syndromes or non-bacterial infections (n = 3; 1.3%), days of therapy beyond the indicated duration of therapy absent any clinical reason for a lengthened course (n = 31, 13.4%), use of redundant antimicrobial therapy and/or continuation of empiric broad-spectrum therapy when cultures have revealed the infecting pathogen (n = 5, 2.2%).
Inappropriate (n = 163, 70.6%): use of antimicrobials in the setting of established infection to which the pathogen is resistant (n = 17, 7.4%), use of antimicrobials not recommended in treatment guidelines (n = 146, 63.2%).
Suboptimal (n = 29, 12.5%): use of antimicrobials in the setting of established infection that can be improved in one of the following categories: drug choice (n = 9, 3.9%), drug route (n = 1, 0.4%), drug dose (n = 19, 8.2%).
Table 3 shows the variables included in the univariable analysis to identify predictors of antimicrobial appropriateness. Overall, 46.6% of antibiotic prescriptions were judged inappropriate, with significantly greater appropriate treatment decisions for UTI (66.7%) compared with LRTI (36.8%) and SSTI (53.3%). There were statistically significant differences in appropriateness between type of treatment (p = 0.012). Also, we found statistically significant differences between some classes of antibiotics: cephalosporins, fluoroquinolones, fosfomycin calcium, fosfomycin-tromethamine, macrolides. Of those, only fosfomycin-tromethamine was associated with an appropriate antimicrobial therapy. Other classes of antibiotics, penicillins (amoxicillin, cloxacillin), amoxicillin-clavulanic acid and sulfonamides, were not significantly associated with appropriate prescribing. Inappropriate antibiotic use varied significantly by setting: ED (84.9%), HPC (46.2%) and LTCF (40.9%). We found no differences in appropriate treatment decisions if the patient had antibiotic exposure in the last 6 months. Thirty-day clinical outcome was as follows (total; appropriate vs. inappropriate therapy): clinical improvement and symptoms resolution (66.1%); need for another course of antibiotic therapy (23.1%) not evaluable (2.4%); death (8.4%), half of cases of death (51.6%) because of the infection. No differences with appropriateness were found.
Table 3.
Univariable analysis of variables associated with appropriateness
| Total N = 416 |
Appropriate antibiotic prescriptions N = 222 |
Inappropriate antibiotic prescriptions N = 194 |
p value | Odds ratio (95% CI) | |
|---|---|---|---|---|---|
| Age (years), mean (SD) | 82.8 (9.8) | 82.9 (9.7) | 82.6 (9.9) | 0.792 | 1.003 (0.983–1.023) |
| Sex | |||||
| Male, n (%) | 134 (32.2) | 68 (30.6) | 66 (34.0) | 0.461 | 0.856 (0.567–1.293) |
| Therapy type, n (%) | |||||
| Targeted | 70 (16.8) | 47 (67.1) | 23 (32.9) | 0.012 | 1.997 (1.162–3.431) |
| Infection type, n (%) | |||||
|
SSTI UTI LRTI |
92 (22.1) 180 (43.3) 144 (34.6) |
49 (53.3) 120 (66.7) 53 (36.8) |
43 (46.7) 60 (33.3) 91 (63.2) |
0.013 < 0.001 |
1.957 (1.150–3.329) 3.434 (2.170–5.435) |
| Classes of antibiotics, n (%) | |||||
| Penicillins (amoxicillin, cloxacillin) | 46 (11.1) | 29 (63.0) | 17 (37.0) | 0.800 | 0.853 (0.250–2.916) |
| Amoxicillin-clavulanic acid | 66 (15.9) | 37 (56.1) | 29 (43.9) | 0.455 | 0.638 (0.196–2.073) |
| Cephalosporins | 78 (18.8) | 11 (14.1) | 67 (85.9) | < 0.001 | 0.082 (0.024–0.286) |
| Fluoroquinolones | 54 (13) | 15 (27.8) | 39 (72.2) | 0.008 | 0.192 (0.056–0.656) |
| Fosfomycin calcium | 16 (3.8) | 1 (6.3) | 15 (93.8) | 0.004 | 0.033 (0.003–0.330) |
| Fosfomycin-tromethamine | 104 (25) | 101 (97.1) | 3 (2.9) | < 0.001 | 16.833 (3.495–81.068) |
| Macrolides | 17 (4.1) | 2 (11.8) | 15 (88.2) | 0.004 | 0.067 (0.011–0.0413) |
| Sulfonamides | 20 (4.8) | 16 (80.0) | 4 (20.0) | 0.376 | 2.000 (0.431–9.273) |
| Other antibiotics | 15 (3.6) | 10 (66.7) | 5 (33.3) | ||
| Previous antibiotics (6 months), n (%) | |||||
| No | 146 (35.1) | 85 (55.8) | 61 (41.8) | 0.145 | 0.739 (0.492–1.110) |
| Location antibiotic initiated | |||||
| Hospital or primary care | 13 (3.1) | 7 (53.8) | 6 (46.2) | < 0.001 | 8.142 (3.726–17.792) |
| LTCF | 350 (84.1) | 207 (59.1) | 143 (40.9) | 0.005 | 6.562 (1.745–24.680) |
| Emergency department | 53 (12.7) | 8 (15.1) | 45 (84.9) |
IQR interquartile range, LRTI lower respiratory tract infections, LTCF long-term care facility, SD standard deviation, SSTI skin and Soft tissue infections, UTI urinary tract infections
Subsequently, multivariable analysis showed that empirical therapy, some classes of antibiotics (cephalosporins, fluoroquinolones, fosfomycin calcium, macrolides) and prescription initiation in the ED were independent predictors of antimicrobial inappropriateness (Table 4). Datasets showed adequate discrimination with an area under ROC curve of 0.908.
Table 4.
Multivariable analysis of variables associated with appropriateness
| p value | Odds ratio (95% CI) | |
|---|---|---|
| Targeted therapy | 0.045 | 3.396 (1.027–11.234) |
| Classes of antibiotics | ||
| Cephalosporins | < 0.001 | 0.059 (0.013–0.268) |
| Fluoroquinolones | 0.042 | 0.227 (0.054–0.949) |
| Fosfomycin calcium | 0.036 | 0.072 (0.006–0.839) |
| Fosfomycin-tromethamine | < 0.001 | 61.586 (9.335–406.295) |
| Macrolides | 0.001 | 0.025 (0.003–0.221) |
| Antibiotic initiated in the long-term care facility | < 0.001 | 5.771 (2.214–15.047) |
Discussion
Although data are limited, there are several studies that have begun to characterize the status of ASP in LTCF. In contrast to findings of ASP in hospitals, a recent systematic review did not find evidence that these programs in LTCF change the incidence of Clostridium difficile infections, rates of hospitalisations or mortality [12]. However, the studies indicate that ASP can reduce the number of antibiotic prescriptions and improve adherence to guidelines. This review includes fourteen studies, but only three are developed in Europe. Other later narrative review aimed to provide data about antibiotic consumption included ten studies carried out in Europe and four in other countries, all proposing educational interventions [20]. To the authors’ knowledge, our study is the first in Spain evaluating the role of a pharmacist-led ASP in elderly patients residing in a LTCF. Educational interventions and weekly prospective audits and feedback have resulted in significant decreases in antibiotic use and costs of antibiotics, but no changes in hospitalization and mortality have been found. Infection and sepsis related hospitalization and related death rates have unchanged during the ASP implementation versus preimplementation. In the preintervention period, mean total use of systemic antimicrobials is 63.2 DRD, in concordance with data reported in another Europe country, Netherlands (73 DRD) [21]. We found that total consumption of antibiotics has reduced by 63.8%, more than the decreases reported in other studies with educational interventions (12–30%) focused on appropriate diagnosis and treatment of common infectious syndromes [22, 23].
Fluoroquinolones account for 13% of antimicrobial prescriptions in our LTCF, in contrast with 30–44% documented in other studies, likely because of their oral bioavailability and broad spectrum of activity [24]. They are the class of antibiotics with the largest DRD reduction, being one of the targets in our study for two reasons. First, although ciprofloxacin is one of the most effective antibiotic in UTI, there is a significantly high rate of UTI caused by E. coli and Klebsiella spp. resistant to fluoroquinolones in our area, so fosfomycin-tromethamine is the election treatment in the guidelines for UTI, [17] antibiotic with a slight reduction between periods. This fact is explained because of treatment cessation of some asymptomatic bacteriurias. Cefixime and sulfonamides are also an effective alternative in the guidelines for these infections. Second, amoxicillin-clavulanic acid is the first line therapy for LRTI, while levofloxacin is the recommended treatment if allergy to beta-lactams antibiotics and/or history of COPD [17]. On the other hand, amoxicillin-clavulanic acid, the other focus antibiotic, is the second with greatest diminution. Penicillins are the first election therapy for SSTI instead penicillins with beta-lactamase inhibitors. The corresponding decrease in both classes suggests that our pharmacist-led ASP successfully improve their use.
Furthermore, this study is the first to assess appropriateness of antibiotic prescriptions classified as unnecessary, inappropriate and suboptimal antimicrobial use [19], as well as identify predictors of antimicrobial appropriateness and specifically the influence of the setting of prescription initiation (ED, HPC, LTCF). The proportion of appropriate antibiotics prescribed in our study (53.4%) is consistent with other studies conducted in other LTCF [4, 27, 28]. Some classes of antibiotics (cephalosporins, fluoroquinolones, fosfomycin calcium, macrolides) are negatively associated with antibiotic prescription appropriateness in the multivariable analysis. We assume that it is correlated with reasons explained before. Cephalosporins and fluoroquinolones are often prescribed for LTCF infections instead of first line antibiotics and they are relationated with Clostridium difficile infection. In this facility, fosfomycin calcium has been used for UTI with longer durations than guidelines recommendations in place of fosfomycin-tromethamine. In the case of macrolides, they have been prescribed for suspected respiratory tract infections possibly caused by virus or for syndromes in which initiation of an antibiotic is not recommended. On the other hand, antibiotic prescription for LTCF residents initiated in the ED is an independent predictor of antimicrobial inappropriateness. To our knowledge, this is the first description of this association. Probably this result can be explained by two main arguments. First, unlike LTCF physicians, those working in the ED usually treat patients of different ages. Elderly patients, specially those living in LTCF, are medically complex patients with multiple comorbidities that increase the risk of infection (i.e. COPD, diabetes, medical devices, pressure sores,…). Besides, it can be difficult to recognize infections because of the presence of atypical signs and symptoms and the cognitive impairment. So, the dread of a clinical worsening can result in an earlier initiation of the antibiotics prescription, even in absence of clear evidence of bacterial infection. Second, there is not a formal ASP in the ED of the corresponding hospital. Therefore, LTCF ASP must consider also interventions focus on prescribers who are working outside of the facility.
Our study has several limitations. While the antibiotic prescriptions are prospectively identified, data of residents are retrospectively collected from medical records and may not have been consistently recorded. Also, we do not focus on antimicrobials prescribed for other infections such as dental infections where amoxicillin-clavulanic acid is frequently prescribed instead of amoxicillin. In addition, infections which have not been treated with antibiotics have not been included. We could also not control the antibiotic prescriptions initiated in ED and HPC frequently broad-spectrum antibiotics (fluoroquinolones, cephalosporins and amoxicillin-clavulanic acid) and this may have had a negative effect on antibiotic use. Despite the potential limitations previously mentioned and although the conclusions of this study are limited by the quasi-experimental study design, it is plausible that the intervention is associated with a significant lowering consumption of antibiotics. Nevertheless, generalisability to other LTCF must be taken with caution.
Overall, almost half of antimicrobials prescriptions are inappropriate. Evidence shows that educational interventions consisting of providing an antibiotic prescribing guide combined with physician antibiotic prescribing profiles are the most effective published ASP strategies [22, 23, 25], together with an audit and feedback [26], improving prescribing habits and reducing unnecessary antibiotic prescriptions [20]. Pharmacist-led ASP in a LTCF has been effective in reducing global consumption of antibiotics by improving appropriateness of treatment decisions. Inappropriate use is high in antibiotics initiated in the emergency department and it constitutes a small but not unimportant percent of all prescriptions. So, in attempts to improve antibiotic stewardship in LTCF, ASP should include interventions in this setting.
Acknowledgements
Authors thank Long-Term Care Facility staff members for their collaboration, to Rajneet Rehal for the English language review and corrections of this manuscript, to M. Carmen Rosa for the statistical analysis. This study will be part of the doctoral thesis of the first author admitted in the Pharmacy Doctoral Program at the University of Granada. To Cisneros JM and PROA-SENIOR study group, because some data are part of a clinical trial published on Clin Infect Dis (https://doi.org/10.1093/cid/ciac834).
Author contributions
MRCC contributed to the study design, data collection, interpretation of the data, writing and revising the manuscript and accepts responsibility for the corresponding author. MRCC, JEMP and AJM contributed to the interpretation of the data and revising of the manuscript. All authors read and approved the final manuscript.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declarations
Conflict of interest
All authors report no conflicts of interest.
Ethical approval
The study was designed and performed according to the Helsinki Declaration and approved by the Ethics Committee of Jaén Province.
Informed consent
The subjects who participated in the study signed and informed consent for data collection.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Nicolle LE. Infection prevention issues in long-term care. Curr Opin Infect Dis. 2014;27(4):363–369. doi: 10.1097/QCO.0000000000000071. [DOI] [PubMed] [Google Scholar]
- 2.Rhee SM, Stone ND. Antimicrobial stewardship in long-term care facilities. Infect Dis Clin N Am. 2014;28:237–246. doi: 10.1016/j.idc.2014.01.001. [DOI] [PubMed] [Google Scholar]
- 3.Nace DA, Drinka PJ, Crnich CJ. Clinical uncertainties in the approach to long-term care residents with possible urinary tract infection. J Am Med Dir Assoc. 2014;15:133–139. doi: 10.1016/j.jamda.2013.11.009. [DOI] [PubMed] [Google Scholar]
- 4.van Buul LW, Veenhuizen RB, Achterberg WP, Schellevis FG, Essink RTGM, de Greeff SC, et al. Antibiotic prescribing in Dutch nursing homes: how appropriate is it? J Am Med Dir Assoc. 2015;16(3):229–237. doi: 10.1016/j.jamda.2014.10.003. [DOI] [PubMed] [Google Scholar]
- 5.Daneman N, Bronskill SE, Gruneir A, et al. Variability in antibiotic use across nursing homes and the risk of antibiotic-related adverse outcomes for individual residents. JAMA Intern Med. 2015;175(8):1331–1339. doi: 10.1001/jamainternmed.2015.2770. [DOI] [PubMed] [Google Scholar]
- 6.van den Dool C, Haenen A, Leenstra T, Wallinga J. The role of nursing homes in the spread of antimicrobial resistance over the healthcare network. Infect Control Hosp Epidemiol. 2016;37(7):761–767. doi: 10.1017/ice.2016.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Medicare and Medicaid Programs (2016) Reform of requirements for long-term-care facilities. https://www.federalregister.gov/documents/2016/10/04/2016-23503/medicare-and-medicaid-programs-reformof-requirements-forlongterm-care-facilities. Accessed 13 Jan 2021 [PubMed]
- 8.Barlam T, Cosgrove S, Abbo L, et al. Implementing an antibiotic stewardship program: guidelines by the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America. Clin Infect Dis. 2016;62:e51. doi: 10.1093/cid/ciw118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Crnich CJ, Jump R, Trautner B, Sloane PD, Mody L. Optimizing antibiotic stewardship in nursing homes: a narrative review and recommendations for improvement. Drugs Aging. 2015;32:699–716. doi: 10.1007/s40266-015-0292-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nicolle LE. Antimicrobial stewardship in long term care facilities: what is effective? Antimicrob Resist Infect Control. 2014;3:1–7. doi: 10.1186/2047-2994-3-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dyar OJ, Pagani L, Pulcini C. Strategies and challenges of antimicrobial stewardship in long-term care facilities. Clin Microbiol Infect. 2015;21:10–19. doi: 10.1016/j.cmi.2014.09.005. [DOI] [PubMed] [Google Scholar]
- 12.Feldstein D, Sloane PD, Feltner C. Antibiotic stewardship programs in nursing homes: a systematic review. J Am Med Dir Assoc. 2018;19(2):110–116. doi: 10.1016/j.jamda.2017.06.019. [DOI] [PubMed] [Google Scholar]
- 13.Dwyer R, Gabbe B, Stoelwinder JU, Lowthian J. A systematic review of outcomes following emergency transfer to hospital for residents of aged care facilities. Age Ageing. 2014;43:759–766. doi: 10.1093/ageing/afu117. [DOI] [PubMed] [Google Scholar]
- 14.Dellit TH, Owens RC, McGowan JE, Jr, et al. Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America guidelines for developing an institutional program to enhance antimicrobial stewardship. Clin Infect Dis. 2007;44:159–177. doi: 10.1086/510393. [DOI] [PubMed] [Google Scholar]
- 15.ASHP statement on the pharmacist’s role in antimicrobial stewardship and infection prevention and control. Am J Health Syst Pharm. 2010;67(7):575–577. 10.2146/sp100001. PMID: 20237387. [DOI] [PubMed]
- 16.Waters CD. Pharmacist-driven antimicrobial stewardship program in an institution without infectious diseases physician support. Am J Health Syst Pharm. 2015;72(6):466–468. doi: 10.2146/ajhp140381. [DOI] [PubMed] [Google Scholar]
- 17.Guía de Terapéutica Antimicrobiana del Área Aljarafe. http://guiaterapeuticaaljarafe.sas.juntaandalucia.es/guiaTerapeuticaAljarafe/guia/guia.asp. Accessed 13 July 2020
- 18.Loeb M, Bentley DW, Bradley S, Crossley K, Garibaldi R, Gantz N, et al. Development of minimum criteria for the initiation of antibiotics in residents of long-term-care facilities: results of a consensus conference. Infect Control Hosp Epidemiol. 2001;22:120–124. doi: 10.1086/501875. [DOI] [PubMed] [Google Scholar]
- 19.Spivak ES, Cosgrove SE, Srinivasan A. Measuring appropriate antimicrobial use: attempts at opening the black box. Clin Infect Dis. 2016;63(12):1639–1644. doi: 10.1093/cid/ciw658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Falcone M, Paul M, Yahav D, Orlando G, Tiseo G, Prendki V, Study Group for Infections in the Elderly (ESGIE) et al. Antimicrobial consumption and impact of antimicrobial stewardship programmes in long-term care facilities. Clin Microbiol Infect. 2019;25(5):562–569. doi: 10.1016/j.cmi.2018.07.028. [DOI] [PubMed] [Google Scholar]
- 21.Roukens M, Verhoef L, Stobberingh E, Natsch S. Surveillance of antimicrobial use in Dutch long-term care facilities. J Antimicrob Chemother. 2017;72(5):1516–1520. doi: 10.1093/jac/dkw581. [DOI] [PubMed] [Google Scholar]
- 22.Schwartz DN, Abiad H, DeMarais PL, Armeanu E, Trick WE, Wang Y, et al. An educational intervention to improve antimicrobial use in a hospital-based long-term care facility. J Am Geriatr Soc. 2007;55(8):1236–1242. doi: 10.1111/j.1532-5415.2007.01251.x. [DOI] [PubMed] [Google Scholar]
- 23.Pettersson E, Vernby A, Mölstad S, Lundborg CS. Can a multifaceted educational intervention targeting both nurses and physicians change the prescribing of antibiotics to nursing home residents? A cluster randomized controlled trial. J Antimicrob Chemother. 2011;66(11):2659–2666. doi: 10.1093/jac/dkr312. [DOI] [PubMed] [Google Scholar]
- 24.Benoit SR, Nsa W, Richards CL, Bratzler DW, Shefer AM, Steele LM, et al. Factors associated with antimicrobial use in nursing homes: a multilevel model. J Am Geriatr Soc. 2008;56(11):2039–2044. doi: 10.1111/j.1532-5415.2008.01967.x. [DOI] [PubMed] [Google Scholar]
- 25.Monette J, Miller MA, Monette M, Laurier C, Boivin JF, Sourial N, et al. Effect of an educational intervention on optimizing antibiotic prescribing in long-term care facilities. J Am Geriatr Soc. 2007;55(8):1231–1235. doi: 10.1111/j.1532-5415.2007.01250.x. [DOI] [PubMed] [Google Scholar]
- 26.Daneman N, Gruneir A, Bronskill SE, Newman A, Fischer HD, Rochon PA, et al. Prolonged antibiotic treatment in long-term care: role of the prescriber. JAMA Intern Med. 2013;173(8):673–682. doi: 10.1001/jamainternmed.2013.3029. [DOI] [PubMed] [Google Scholar]
- 27.Peron EP, Hirsch AA, Jury LA, Jump RL, Donskey CJ. Another setting for stewardship: high rate of unnecessary antimicrobial use in a veterans affairs long-term care facility. J Am Geriatr Soc. 2013;61(2):289–290. doi: 10.1111/jgs.12099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dylis A, Boureau AS, Coutant A, Batard E, Javaudin F, Berrut G, et al. Antibiotics prescription and guidelines adherence in elderly: impact of the comorbidities. BMC Geriatr. 2019;19(1):291. doi: 10.1186/s12877-019-1265-1. [DOI] [PMC free article] [PubMed] [Google Scholar]


