Abstract
Objective
To study the impact of Medicaid funding structures before and after the implementation of the Affordable Care Act (ACA) on health care access for Latinos in New York (Medicaid expansion), Florida (Medicaid non‐expansion), and Puerto Rico (Medicaid block grant).
Data Sources
Pooled state‐level data for New York, Florida, and Puerto Rico from the 2011–2019 Behavioral Risk Factor Surveillance System and data from the 2011–2019 American Community Survey and Puerto Rico Community Survey.
Study Design
Cross‐sectional study using probit with predicted margins to separately compare four health care access measures among Latinos in New York, Florida, and Puerto Rico (having health insurance coverage, having a personal doctor, delayed care due to cost, and having a routine checkup). We also used difference‐in‐differences to measure the probability percent change of having any health insurance and any public health insurance before (2011–2013) and after (2014–2019) the ACA implementation among citizen Latinos in low‐income households.
Data Collection
The sample consisted of Latinos aged 18–64 residing in New York, Florida, and Puerto Rico from 2011 to 2019.
Principal Findings
Latinos in Florida had the lowest probability of having health care access across all four measures and all time periods compared with those in New York and Puerto Rico. While Latinos in Puerto Rico had greater overall health care access compared with Latinos in both states, health care access in Puerto Rico did not change over time. Among citizen Latinos in low‐income households, New York had the greatest post‐ACA probability of having any health insurance and any public health insurance, with a growing disparity with Puerto Rico (9.7% any [1.6 SE], 5.2% public [1.8 SE]).
Conclusions
Limited Medicaid eligibility (non‐expansion of Florida's Medicaid program) and capped Medicaid funds (Puerto Rico's Medicaid block grant) contributed to reduced health care access over time, particularly for citizen Latinos in low‐income households.
Keywords: health services accessibility, Hispanic or Latino, medically uninsured, minority groups, Patient Protection and Affordable Care Act, poverty
What is known on this topic
While Latinos continue to have the lowest insurance coverage rates, the Affordable Care Act (ACA) has improved health care access inequities for Latinos across the United States.
Medicaid expansion has been associated with improved health care access for Latinos.
While state Medicaid is funded through uncapped dollar‐for‐dollar matching, as a US territory, Puerto Rico's Medicaid is funded through annually fixed block grants.
What this study adds
Health care access for Latinos in Puerto Rico did not improve over time, which is likely due to the exclusion of the territory from the ACA's coverage programs.
Compared with New York, Florida's choice of not to expand its Medicaid program has continued to limit access to public health insurance for its large low‐income Latino population.
1. INTRODUCTION
Despite substantial improvements in access to health care following the Patient Protection and Affordable Care Act (ACA), 1 , 2 Latinos, the largest minoritized ethnic group in the United States, 3 continue to face major health care inequities, including high uninsured rates, delayed care, and forgone care. 2 Medicaid is an important source of health insurance coverage for many Latinos, who account for approximately one‐third of enrollees. 4 Since Medicaid programs operate differently in each state, with varying income eligibility and covered benefits, inequities can be exacerbated based on where a person resides within the United States. In 2014, the ACA originally required states to expand their Medicaid programs' eligibilities by using 100% federal dollars from 2014 to 2016. 5 However, following the US Supreme Court's decision to make Medicaid expansion optional for states, despite the ongoing federal share of these additional costs, which is 90% as of 2021, 12 states (including Florida) have opted not to expand their Medicaid programs. 6 Yue et al 7 found that low‐income adults living in Medicaid expansion states had statistically significant improvements in three of four health care access outcomes: health insurance coverage, having a personal doctor, and delayed care due to cost. Latinos, however, had the fewest coverage gains from Medicaid expansion, which increased the inequity with other racial/ethnic groups. The ACA also provided states with the option of implementing a Basic Health Program (BHP) to replace health insurance marketplace tax credits for individuals with incomes just above the Medicaid eligibility threshold, including lawful permanent residents ineligible for Medicaid due to their recent (<5 years) immigration status. As of 2022, only two states (New York and Minnesota) have implemented the program and two more (Oregon and Kentucky) are in the process of implementing it. 8 , 9 , 10
The growing body of evidence regarding health care inequities for Latinos has largely overlooked Latinos living in the US territory of Puerto Rico (PR). Puerto Rico is 99% Latino and almost half of its population lives under the federal poverty threshold. 11 Despite having a large Medicaid‐eligible population, the local Medicaid program is funded differently from the states. 12 While state Medicaid is funded as an entitlement program, where federal financial support is guaranteed for a percentage of expenditures based on local eligibility, 6 Medicaid in the US territories, such as Puerto Rico, is funded through annually fixed block grants determined by the US Congress. 12 , 13 , 14 , 15 , 16 Unlike states that do not have a spending cap, the Puerto Rico government is responsible for covering all Medicaid costs that exceed the allocated block grant amount, which often runs out mid‐year.
The ACA was intended to address national health care inequities in access and quality, but much of the provisions in the law were not applied to US territories. 13 , 15 Territories could choose to enact similar provisions under their own laws 17 , 18 ; however, they continue to receive constrained funds, which limited Puerto Rico's capability to improve its Medicaid program. 14 While the ACA permanently raised the island's statutory Federal Medical Assistance Percentage (FMAP) from 50% to 55%, using the state FMAP formula (based on average per capita income relative to the national average), Puerto Rico would have an 83% FMAP if it was treated like other states and Washington, DC, which is the statutory maximum. Furthermore, Puerto Rico does not receive unlimited funding at a 55% matching rate; instead, the federal government uses this rate to estimate the annually capped federal block grant based on predicted spending. 12 Finally, the ACA did not provide 100% (and subsequently 90% for 2020 and on) matched funds for Puerto Rico to expand its Medicaid eligibility to 138% of the federal poverty level (FPL) as it did for the states. 12 This current block grant funding structure has forced the Puerto Rico Medicaid program to use a local eligibility threshold of roughly 43% of the FPL. 12 , 13 , 16 , 19 While multiple temporary supplements have been provided to Puerto Rico across recent years, these funds have barely contributed to improving the current Medicaid program, and the “expansion” in eligibility had limited impact using the local Puerto Rico poverty level. 20 More details on the Puerto Rico Medicaid program are provided in Section 1 (Supplemental Materials).
To our knowledge, only one other study has compared access to care in the US states with Puerto Rico following the early implementation of the ACA. Portela and Sommers 13 used 2011–2012 Behavioral Risk Factor Surveillance System (BRFSS) and 2012 American Community Survey (ACS) data to measure health insurance coverage, having a personal doctor, delaying care due to cost, having a routine checkup, multiple preventive services, and several measures of health, including self‐reported health. Puerto Rico residents reported significantly better health care access for all outcomes and preventive measures compared with US mainland residents, but their self‐reported health was significantly worse. While this study contributed to the scarce literature on access to health care in Puerto Rico, it did not capture the long‐term effects of the ACA or the key ACA provisions nationally implemented in 2014.
Using BRFSS, we measured four health care access outcomes: having health insurance coverage; having a personal doctor; delayed care due to cost; and having a routine checkup. To estimate the state‐level impact of Medicaid funding and expansion decisions on health care access for Latinos in the United States, we compared pre‐ and post‐ACA outcomes among Latinos living in New York (Medicaid expansion), Florida (Medicaid non‐expansion), and Puerto Rico (Medicaid block grant). These states were selected because of their large Latino populations and similar Latino subgroup compositions (i.e., Puerto Rican, Dominican, and Cuban). Section 2 (Supplemental Materials) contains more information on the selection of state samples. While New York has been identified as a “pre‐expansion” state, with some ACA provisions being implemented as early as 2011, Denham and Veazie 21 showed that 2014 was a major turning point for health care outcomes, such as health insurance coverage, following the formal Medicaid expansion, which markedly increased the eligibility threshold. 22 Furthermore, New York implemented its BHP (“Essential Plan”) in 2016, which serves as a reference for the impact of extended ACA benefits. 23 Prior work has suggested that ACA gains began to reverse in 2016 and worsened in 2019 with the elimination of the individual mandate. 24 , 25 , 26 Due to a limited study sample, we were unable to separately study 2019 changes. To capture all other changes described, we measure access to care within three key time periods: pre‐ACA (2011–2013), post‐ACA 1 (2014–2015), and post‐ACA 2 (2016–2019).
In this study, we aim to build off the previous Medicaid expansion and non‐expansion comparisons by (1) limiting the sample to Latinos and (2) adding another Medicaid funding category for comparison (the Puerto Rico Medicaid block grant). As the first study, to our knowledge, to assess health care access for Latinos across three different Medicaid funding structures, our findings will contribute to the scant scientific literature on Latino and Puerto Rico health care access. We also provide a discussion on policy solutions to address health care access inequities.
2. METHODS
2.1. Data
Repeated cross‐sectional survey data were obtained from the 2011–2019 BRFSS and the 2011–2019 ACS and Puerto Rico Community Survey (PRCS). BRFSS is a publicly available health‐related telephone survey administered by the Centers for Disease Control and Prevention (CDC) that collects monthly data on risk behaviors, chronic health conditions, health care access, and use of preventive services for non‐institutionalized US residents aged 18 or older living in any of the 50 states, District of Columbia, and 3 territories, including Puerto Rico. 27 , 28 The ACS and its Puerto Rico equivalent, the PRCS, are publicly available annual surveys conducted by the US Census Bureau. 29 The ACS and PRCS collect nationally representative data on population demographic, economic, and social characteristics. 29 , 30 For this study, we have consolidated ACS and PRCS data into a single dataset and refer to it as ACS/PRCS. BRFSS and ACS/PRCS 2020 data were excluded from the sample due to comparability issues resulting from the COVID‐19 pandemic; details are provided in Section 3 (Supplemental Material).
The study sample (BRFSS, n = 48,748; ACS/PRCS, n = 193,867) consisted of adults aged 18–64 residing in New York, Florida, or Puerto Rico at the time of interview who self‐identified as Latino. Participants aged 65 or older were excluded to minimize biased effects from Medicare insurance coverage, which is delivered via a federal social insurance program across all states and territories. Considering Puerto Rico's 99% Latino population, 11 non‐Latino participants were excluded from the sample for all three states/territories. For the secondary analysis using ACS/PRCS data, the sample was limited to Latinos who were US citizens (by birth or naturalized) to prevent skewed results from the small non‐citizen sample in Puerto Rico (see Section 4, Supplemental Material). BRFSS does not capture citizenship.
2.2. Variables
We used the following four health care access variables available in BRFSS as separate, binary (yes/no) outcome measures: having health insurance coverage; having a personal doctor; delayed care due to cost; and having a routine checkup. While BRFSS captures time to routine checkup, for this study, we dichotomized having a routine checkup, with “yes” representing at least one visit within the past 2 years. For the secondary analyses using ACS/PRCS data, any health insurance coverage and any public health insurance coverage were used as health care access outcomes. Any health insurance coverage includes both private and public health insurance estimates to capture possible changes from non‐Medicaid‐specific ACA provisions, such as the individual mandate. The year variable was used as the primary time measure, which ranged from 2011 to 2019 for both BRFSS and ACS/PRCS. To model the impact of both the ACA changes and Medicaid expansion over time, a binary pre‐/post‐variable was created to operationalize 2011–2013 as the pre‐ACA period and 2014–2019 as the post‐ACA period, while a three‐level categorical variable operationalized ACA time periods as follows: pre‐ACA (2011–2013), post‐ACA 1 (2014–2015), and post‐ACA 2 (2016–2019).
Although the ACA was officially implemented earlier, for the purpose of this paper, we use 2014 to define the pre‐ and post‐intervention periods due to the significant impact of the key ACA provisions enacted that year, including the national implementation of the health insurance mandate and Medicaid expansion. 31 The state variable (New York, Florida, and Puerto Rico) was used as the exposure representing the different Medicaid funding structures: Medicaid expansion, Medicaid non‐expansion, and block grant, respectively. Florida was used as the reference group since the state rejected key ACA provisions, such as Medicaid expansion.
Using BRFSS, self‐reported health status (excellent/very good, good, and fair/poor) and having at least one chronic condition were included in all adjusted models as health care access mediators. The following covariates were also included to adjust for diverging characteristics between states/territory: age, marital status, educational attainment, employment status, annual household income (in dollars), and mode of survey interview. For the secondary analysis using ACS/PRCS, the following covariates were included: age, marital status, educational attainment, employment status, annual household income (as % of the FPL), and English language proficiency. Health care need measures are not collected in ACS/PRCS, so they are not part of the secondary analyses.
2.3. Statistical analyses
Using BRFSS, we ran weighted bivariate analyses for each variable by state/territory to describe unadjusted differences. Chi‐squared tests were used to test for significance. Additionally, we ran unadjusted and adjusted marginal probit regressions for each health care access outcome (having health insurance coverage, having a personal doctor, delayed care due to cost, and having a routine checkup) using the three‐level ACA time variable to compare the pre‐ and post‐ACA changes by state/territory. Sensitivity analyses replicating these findings using the top 10 states with the largest Puerto Rican population were included in the Supplemental Material, Section 5. Using ACS/PRCS data, the sample was restricted to citizen Latinos in low‐income households using a 200% FPL threshold to capture Medicaid expansion eligibility and New York's Essential Plan maximum eligibility as the poverty level. Descriptive statistics were reported for citizen Latinos in low‐income households by state/territory. A quasi‐experimental difference‐in‐differences (DiD) design was applied to compare the three Medicaid funding structures. We separately analyzed the estimated marginal probability of having any health insurance and having any public health insurance among citizen Latinos living at or below 200% of the FPL. DiD changes in marginal probabilities were analyzed using two states/territories at a time (i.e., NY vs. FL, FL vs. PR, and NY vs. PR). Robust SEs were used to manage serial correlation from consecutive year samples. For visual interpretation, results were also presented for both outcomes as trend line graphs by state/territory and year. A regression estimator and visual assessment of parallel trends were used as a post‐estimation diagnostic to ensure estimates did not account for changes that began before the ACA implementation (see Section 6, Supplemental Material). All analyses were conducted using StataIC 16.1 and accounted for complex survey sampling design using BRFSS and ACS/PRCS weights. As recommended by IPUMS USA, we used replicate weights for proper SE estimation when jointly analyzing ACS and PRCS data. 32
3. RESULTS
Table 1 presents descriptive statistics by state/territory and Medicaid funding structure. Latinos in Puerto Rico had better unadjusted health care access outcomes than Latinos in New York and Florida: 90.8% of Latinos in Puerto Rico had health insurance coverage; 80.0% had a personal doctor; 17.4% experienced delayed care due to cost; and 87.9% had a routine checkup. Latinos in Florida had the worst health care access across all four unadjusted measures. Florida had a greater proportion of Latinos self‐reporting their health as “Excellent/Very Good” (46.2%) compared with Latinos in New York (38.1%) and Puerto Rico (34.2%). Puerto Rico had the highest proportion of Latinos with at least one chronic condition (40.5%) followed by New York (34.9%) and Florida (31.8%). In New York (59.3%), most Latinos had an educational attainment of high school or less. A greater proportion of Latinos in all three locations were employed (FL: 68.7%; NY: 65.7%; and PR: 52.0). Most Latinos in Florida earned an annual household income of $50,000 or more (30.7%), while most Latinos in Puerto Rico had an income of less than $14,999 (44.2%). Across all three sites, most Latinos responded to the interview via cellphone mode.
TABLE 1.
Descriptive statistics for Latinos living in New York, Florida, and Puerto Rico, Behavioral Risk Factor Surveillance System (BRFSS) 2011–2019 (n = 48,748)
| Total | New York | Florida | Puerto Rico | |
|---|---|---|---|---|
| ACA time periods | ||||
| Pre‐ACA (2011–2013) | 33.1% | 32.7% | 31.8% | 35.2% |
| Post‐ACA 1 (2014–2015) | 22.2 | 22.6 | 21.7 | 22.3 |
| Post‐ACA 2 (2016–2019) | 44.8 | 44.7 | 46.4 | 42.5 |
| Health insurance coverage | 76.4 | 73.1 | 68.4 | 90.8 |
| Having a personal doctor | 68.4 | 68.0 | 60.4 | 80.0 |
| Delayed care due to cost | 23.0 | 23.2 | 26.9 | 17.4 |
| Having a routine checkup | 83.8 | 84.4 | 80.4 | 87.9 |
| Self‐reported general health | ||||
| Excellent/very Good | 40.3 | 38.1 | 46.2 | 34.2 |
| Good | 35.3 | 38.1 | 33.1 | 35.5 |
| Fair/poor | 24.4 | 23.8 | 20.6 | 30.2 |
| At least one chronic condition | ||||
| Yes, at least one | 35.3 | 34.9 | 31.8 | 40.5 |
| Age (in years) | ||||
| 18–34 | 38.0 | 42.2 | 37.5 | 34.7 |
| 35–54 | 45.0 | 42.8 | 46.2 | 45.4 |
| 55–64 | 17.0 | 14.9 | 16.3 | 19.9 |
| Marital status | ||||
| Married | 40.9 | 35.9 | 46.4 | 38.2 |
| Separated/divorced/widowed | 20.6 | 18.0 | 17.8 | 27.3 |
| Never married | 38.5 | 46.1 | 35.9 | 34.5 |
| Educational attainment | ||||
| High school or less | 50.6 | 59.3 | 48.1 | 45.5 |
| At least some college studies | 49.4 | 40.7 | 51.9 | 54.5 |
| Employment status | ||||
| Employed | 62.9 | 65.7 | 68.7 | 52.0 |
| Currently not employed | 37.1 | 34.3 | 31.3 | 48.0 |
| Annual household income | ||||
| Less than $14,999 | 26.9 | 24.1 | 16.3 | 44.2 |
| $15,000‐24,999 | 28.7 | 29.4 | 27.7 | 29.4 |
| $25,000‐49,999 | 22.3 | 22.2 | 25.3 | 18.1 |
| $50,000 or more | 22.2 | 24.3 | 30.7 | 8.3 |
| Mode of survey interview | ||||
| Landline | 28.7 | 36.3 | 22.2 | 29.9 |
| Cellphone | 71.3 | 63.7 | 77.8 | 70.1 |
Note: Data are shown in column percent. All variables had a statistically significant association with state/territory (p‐value < 0.001).
Abbreviation: ACA, Affordable Care Act.
Source: BRFSS, 2011–2019.
Table 2 shows the adjusted predicted marginal effects of Medicaid funding structure on health care access for Latinos. Latinos in both Florida (Medicaid non‐expansion) and New York (Medicaid expansion) had significant improvements in having health insurance coverage during both post‐ACA periods compared with pre‐ACA. Latinos in Puerto Rico (Medicaid block grant) had a significantly different probability of having health insurance during early post‐ACA; however, this change was small (1.7%) and was not significant for the later post‐ACA period (2016–2019). Latinos in Florida experienced a 4.1% significant increase in the probability of having a personal doctor during early post‐ACA (2014–2015). Meanwhile, Latinos in Puerto Rico experienced a 2.5% increase in the probability of having a personal doctor during the later post‐ACA period (2016–2019). Latinos in New York did not experience a significant change in having a personal doctor during neither post‐ACA periods. Latinos across all three locations experienced significant decreases in the probability of delayed needed care due to cost during post‐ACA. Latinos in all three locations experienced significant increases in the probability of having a routine checkup in the past 2 years during the later 2016–2019 post‐ACA period compared with pre‐ACA (FL: 6.7%; NY: 5.6%; and PR: 1.9%). Across all access to care outcomes, significant changes among Latinos in Puerto Rico represented smaller percentage shifts (<3%) than those reported by Latinos in New York and Florida (>4%).
TABLE 2.
Marginal probability effects of Medicaid funding structure on Latino health care access, Behavioral Risk Factor Surveillance System (BRFSS) 2011–2019 (n = 48,748)
| New York | Florida | Puerto Rico | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Pre‐ACA (2011–2013) | Post‐ACA 1 (2014–2015) | Post‐ACA 2 (2016–2019) | Pre‐ACA (2011–2013) | Post‐ACA 1 (2014–2015) | Post‐ACA 2 (2016–2019) | Pre‐ACA (2011–2013) | Post‐ACA 1 (2014–2015) | Post‐ACA 2 (2016–2019) | |
| Health insurance coverage | Ref. | 6.6 ** [2.8, 10.4] | 8.6 *** [5.5, 11.7] | Ref. | 13.2 *** [9.3, 17.1] | 14.4 *** [11.0, 17.8] | Ref. | 1.7 ** [0.7, 2.8] | 0.4 [−0.6, 1.3] |
| Having a personal doctor | Ref. | −2.0 [−5.8, 1.8] | −1.1 [−4.1, 1.9] | Ref. | 4.1 * [0.2, 8.0] | 1.1 [−2.4, 4.7] | Ref. | −0.5 [−2.0, 1.1] | 2.5 *** [1.1, 3.8] |
| Delayed care due to cost | Ref. | −4.0 * [−7.8, −0.2] | −8.2 *** [−11.3, −5.2] | Ref. | −7.7 *** [−11.4, −4.0] | −9.9 *** [−13.4, −6.5] | Ref. | −2.8 *** [−4.0, −1.5] | −1.9 ** [−3.1, −0.8] |
| Having a routine checkup | Ref. | 0.6 [−2.7, 3.9] | 5.6 *** [3.1, 8.1] | Ref. | 2.5 [−1.0, 6.0] | 6.7 *** [3.7, 9.7] | Ref. | 0.1 [−1.3, 1.4] | 1.9 ** [0.8, 3.1] |
Note: Separate regressions were run for each health care outcome. Values are reported as percent with 95% confidence intervals in brackets. Pre‐ACA (2011–2013) was the reference group for each within‐state comparison. All models were adjusted for self‐reported health status, having at least one chronic condition, age, marital status, educational attainment, employment status, annual household income, and mode of survey interview.
Abbreviation: ACA, Affordable Care Act.
Significance level: p < 0.05,
Significance level: p < 0.01,
Significance level: p < 0.001.
Source: BRFSS, 2011–2019.
Table 3 shows descriptive statistics for Latinos with citizenship in low‐income households by state/territory. Citizen Latinos in low‐income households in Puerto Rico had the highest proportion of any health insurance (89.0%) and any public health insurance (60.8%) compared with Latinos in New York (any: 84.3%, public: 59.3%) and Florida (any: 63.0%, public: 23.9%). Puerto Rico also had the highest proportion of citizen Latinos in low‐income households who were currently not employed (59.2%), earned an annual household income of 0%–100% FPL (61.2%), and had low English language proficiency (67.6%). Across all three locations, citizen Latinos in low‐income households were mostly never married or single, had educational attainments of high school or less, and earned annual household incomes of 0%–100% FPL.
TABLE 3.
Descriptive statistics for US citizen Latinos in low‐income households (up to 200% federal poverty level [FPL]) in New York, Florida, and Puerto Rico, ACS 2011–2019 (n = 193,867)
| Total | New York (n = 42,902) | Florida (n = 54,813) | Puerto Rico (n = 96,152) | |
|---|---|---|---|---|
| Any health insurance | 80.6% | 84.3% | 63.0% | 89.0% |
| Any public health insurance | 50.0 | 59.3 | 23.9 | 60.8 |
| Age (in years) | ||||
| 18–30 | 37.7 | 43.8 | 38.9 | 34.1 |
| 31–50 | 40.7 | 37.3 | 41.9 | 41.7 |
| 51–64 | 21.6 | 18.8 | 19.1 | 24.3 |
| Marital status | ||||
| Married | 28.6 | 22.0 | 32.2 | 29.6 |
| Separated/divorced/widowed | 19.4 | 16.6 | 20.8 | 19.9 |
| Never married/Single | 52.0 | 61.4 | 47.0 | 50.5 |
| Educational attainment | ||||
| High school or less | 59.4 | 66.7 | 60.4 | 55.3 |
| At least some college studies | 40.6 | 33.3 | 39.6 | 44.7 |
| Employment status | ||||
| Employed | 46.5 | 45.4 | 57.4 | 40.8 |
| Currently not employed | 53.5 | 54.6 | 42.6 | 59.2 |
| Annual household income | ||||
| 0%–100% FPL | 53.6 | 53.2 | 40.8 | 61.2 |
| 101%–138% FPL | 18.4 | 18.4 | 21.0 | 16.8 |
| 139%–200% FPL | 28.0 | 28.3 | 38.2 | 22.0 |
| English proficiency | ||||
| Only English/very well/well | 60.3 | 87.8 | 86.2 | 32.4 |
| Not well/not at all | 39.7 | 12.2 | 13.8 | 67.6 |
Note: Data are shown in column percent. All variables had a statistically significant association with state/territory (p‐value < 0.001).
Source: American Community Survey (ACS) and Puerto Rico Community Survey (PRCS), 2011–2019.
Figure 1A shows the change in marginal probability of having any health insurance for Latinos in low‐income households. Latinos in both Florida and New York had a significant increase in the probability of having any health insurance during the post‐ACA period. Despite Latinos in Puerto Rico having the highest probability of having any health insurance in the pre‐ACA period, this probability did not change during the post‐ACA period. Starting in 2016, New York surpassed Puerto Rico in the probability of citizen Latinos having any health insurance. The parallel trends assumption was met for all three locations for the probability of having any health insurance (see Section 6, Supplemental Material).
FIGURE 1.
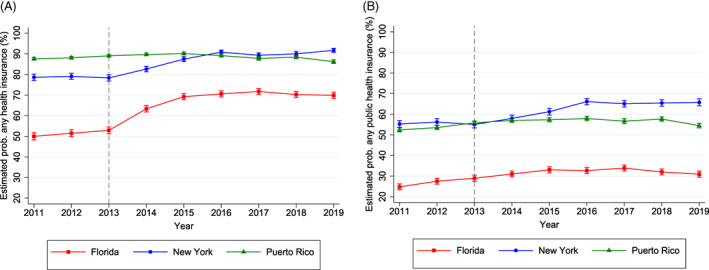
Estimated marginal probability of having any health insurance (A) and having any public health insurance (B) for US citizen Latinos in low‐income households (up to 200% federal poverty level), ACS/PRCS 2011–2019 (n = 193,867). 95% confidence intervals were reported for each data point (shown as tick marks). The gray dashed vertical line provides a reference point for pre‐ and post‐Affordable Care Act implementation. All models were adjusted for age, marital status, educational attainment, employment status, annual household income, and English proficiency. Source: American Community Survey (ACS) and Puerto Rico Community Survey (PRCS), 2011–2019 [Color figure can be viewed at wileyonlinelibrary.com]
In Figure 1B, which shows the change in having any public health insurance for citizen Latinos in low‐income households, New York had the highest probability of participants having any public health insurance during all sample years, except for 2013. Latinos in Florida (Medicaid non‐expansion) had the lowest probability of participants having any health insurance and any public health insurance throughout all sample years, despite the significant improvement in the probability of having any health insurance post‐ACA. The parallel trends assumption was met for Puerto Rico and Florida for having any public health insurance; however, New York did not have a pre‐ACA parallel trend with neither Puerto Rico nor Florida (see Section 6, Supplemental Material). While we understand this weakens the persuasiveness of our analyses, we argue that New York experienced a shift in its trajectory for the probability of having any public health insurance during the post‐ACA period. The transition from a decreasing trend pre‐ACA to an increasing trend post‐ACA could suggest the possible effect from the intervention (the ACA implementation). Nonetheless, we advise careful interpretation of the DiD findings for New York.
Table 4 shows the pre‐ and post‐ACA differences and DiD estimates of the marginal probability of having any health insurance and having any public health insurance among citizen Latinos in low‐income households living in New York, Florida, and Puerto Rico. The pre‐ACA and post‐ACA differences in the probability of having any health insurance and any public health insurance for Latinos in low‐income households living in New York (Medicaid expansion) versus Florida (Medicaid non‐expansion) were both statistically significant. The difference between the periods significantly decreased by 7.7% for the probability of having any health insurance; however, the difference in the probability of having any public health insurance was not significant. For citizen Latinos in low‐income households living in Puerto Rico (Medicaid block grant) versus Florida (Medicaid non‐expansion), the difference in the probability of having any health insurance significantly decreased by 17.4% post‐ACA. While the pre‐ACA (26.9%) and post‐ACA (24.6%) differences were both significant for the probability of having any public health insurance, the DiD was not statistically significant. For Latinos in New York versus Puerto Rico, the differences in the probabilities of having any health insurance (9.7%) and having any public health insurance (5.2%) increased significantly, which is consistent with the results from Figure 1.
TABLE 4.
Difference in differences of the marginal probability of having any health insurance and having any public health insurance pre‐ and post‐Affordable Care Act among US citizen Latinos in low‐income households, ACS/PRCS 2011–2019 (n = 193,867)
| New York versus Florida | Puerto Rico versus Florida | New York versus Puerto Rico | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Difference pre‐ACA [SE] | Difference post‐ACA [SE] | DiD [SE] | Difference pre‐ACA [SE] | Difference post‐ACA [SE] | DiD [SE] | Difference pre‐ACA [SE] | Difference post‐ACA [SE] | DiD [SE] | |
| Any health insurance | 27.2 *** [0.8] | 19.5 *** [1.9] | −7.7 ** [2.0] | 36.8 *** [0.9] | 19.4 *** [1.4] | −17.4 *** [1.6] | −9.6 *** [0.5] | 0.1 [1.5] | 9.7 *** [1.6] |
| Any public health insurance | 28.4 *** [1.2] | 31.4 *** [1.5] | 2.9 [1.9] | 26.9 *** [1.5] | 24.6 *** [0.7] | −2.3 [1.6] | 1.6 [1.0] | 6.8 *** [1.5] | 5.2 * [1.8] |
Note: Values are reported as percent. SEs were reported for each data point (reported within brackets). New York (Medicaid expansion) was always used as the treatment group. Florida (Medicaid non‐expansion) was always used as the control group. Puerto Rico (Medicaid block grant) was the treatment group when compared with Florida and the control group when compared with New York since it “expanded” its Medicaid eligibility but was constrained to the local poverty level, resulting in a substantially lower impact compared with state Medicaid expansion.
Abbreviations: ACA, Affordable Care Act; DiD, difference in differences.
Significance level: p < 0.05,
Significance level: p < 0.01,
Significance level: p < 0.001.
Source: American Community Survey (ACS) and Puerto Rico Community Survey (PRCS), 2011–2019.
4. DISCUSSION
To our knowledge, this study is only the second study to assess the ACA's impact on health care access in Puerto Rico compared with the states. While Portela and Sommers 13 observed the associations in the early ACA implementation period, we examined the long‐term associations of the ACA. In addition, to our knowledge, this is the first comparison of the impact of ACA Medicaid expansion on the magnitude of health care access disparities between Latinos in Puerto Rico and the states, especially those with large Caribbean Latino populations. Despite the implementation of the ACA, health care access inequities persist for Latinos in the United States. Similar to a prior study, 7 Latinos in Florida, a Medicaid non‐expansion state, lagged far behind Latinos in New York, a Medicaid expansion state, across all four health care access measures. Additionally, consistent with the findings of Portela and Sommers', 13 Latinos in Puerto Rico had better outcomes compared with Latinos in both states. However, while health care access for Latinos in the states significantly changed throughout the different ACA time periods, with an overall improvement as of 2014, Latinos in Puerto Rico, which has a Medicaid block grant, did not have large changes in health care access after the implementation of the ACA. Furthermore, we found that the ACA's minimal impact on Puerto Rico's block grant compared with New York's comprehensive expansion and generous federal matching funds led to an increased disparity in the probability of having any health insurance and any public health insurance post‐ACA among citizen Latinos in low‐income households; Latinos in New York had a greater probability of being insured than those in Puerto Rico, with the gap increasing in later post‐ACA periods.
4.1. Policy solutions for Florida
For Florida, adopting Medicaid expansion would likely result in a major increase in health insurance eligibility for Latino adults in low‐income households. A recent study estimated that if the current non‐expansion states extended Medicaid eligibility to low‐income adults living at or below 138% of the FPL, there would be a sixfold increase in eligible uninsured Latino adults. 33 In addition, implementing a Basic Health Plan, which would be supported in large part by federal funds (more than 90%) redirected from healthcare.gov tax credits for lower‐income enrollees, 9 could notably improve health insurance rates among Latinos considering that 32% of Florida residents live at or below 200% FPL (BHP eligibility threshold). 34 The Biden administration has integrated additional financial incentives for non‐expansion states to adopt Medicaid expansion as part of the recently signed American Rescue Plan, 35 which could greatly benefit a densely Latino‐populated state like Florida. Considering that these states will likely continue to reject Medicaid expansion policies, policymakers should consider enacting federal legislation that would help cover populations without insurance. The Center on Budget and Policy Priorities (CBPP) outlines various alternatives as a federal fallback for states that reject this newly offered expansion incentive. 36 First, the Build Back Better Plan proposes a “federalized Medicaid program,” or federally subsidized private insurance, for these non‐expansion states run by the Centers for Medicare and Medicaid (CMS) in collaboration with one or more managed care organizations. The plan would allow people in the Medicaid coverage gap to gain coverage through exchanges with little to no cost‐sharing or premiums. 36 , 37 , 38 Second, CBPP suggested readjustment of the current marketplace conditions to provide more flexible enrollment, modified benefits, cost‐sharing, and continuation of expanded tax credits under the American Rescue Plan.
4.2. Policy solutions for Puerto Rico
While Florida has multiple options to expand its Medicaid program and improve health care access for its large Latino population, the Puerto Rico's block grant funding limits its capacity to improve the delivery and quality of its Medicaid program. Although our study outcomes did not capture service delivery or the quality of the Puerto Rico healthcare system, it is important to consider these conditions when interpreting our findings. Due to limited and capped funds, the Puerto Rico Medicaid program has historically offered substantially fewer benefits, limited prescription drug coverage, has extensive wait times, and has lower provider reimbursement rates and annual wages compared with the states, 12 , 39 , 40 which has reduced provider retention. 41 Given the large proportion of people living in poverty in Puerto Rico relative to the states, an increase in Medicaid funding would expand the number of individuals eligible for public insurance and expand the covered benefits for the Puerto Rico Medicaid program. Despite the US Congress providing multiple temporary supplemental Medicaid funding to assist Puerto Rico during its economic crisis and increasing number and intensity of public health disasters (e.g., natural disasters, infectious disease outbreaks), these financial allocations have been inconsistent and mainly served to maintain current conditions rather than expand and improve the program and its systematic underfunding. 42 Major federal policy reforms such as the ACA tend to overlook territories like Puerto Rico, which can result in generally unchanged health care access outcomes over time, as observed in our findings. Due to Puerto Rico's large proportion of Latinos living in poverty, its high unemployment rate, and its large Medicaid‐dependent population, the current Medicaid block grant structure should be modified or eliminated. Not only does the block grant force Puerto Rico to take on much of the Medicaid financial weight and operate the program under poor conditions, block grants are highly unstable in the face of unexpected emergencies, like natural disasters, economic crises, and infectious disease outbreaks (e.g., tropical diseases, COVID‐19), to which Puerto Rico is constantly exposed. 12 , 20 While a change in the current territory status toward statehood or independence could help resolve much of these inequities, other options can be considered for US territories. It has been proposed to permanently replace the current block grant structure with a fixed percentage coverage of Medicaid costs similar to how state Medicaid operates. 12 , 20 The Puerto Rico Health Care Fairness, Accountability, and Beneficiary Access Act of 2019 (H.R. 3371), 43 which was reintroduced in the House in 2021, 44 proposes increasing the Puerto Rico matching rate to 83% and a 10‐year transition into the uncapped state Medicaid funding structure. This would not only allow a major increase in public insurance eligibility but would also improve the substantial flaws of the current Puerto Rico Medicaid program, including expanding covered benefits and improving provider payment rates and retention.
4.3. Limitations
There are limitations to this study. While health services outcomes (having health insurance coverage, having a personal doctor, delayed care due to cost, and having a routine checkup) for Latinos in Puerto Rico might appear better than they are for Latinos in New York and Florida, our study does not capture the major constraints and poor quality of the Medicaid program in Puerto Rico. 12 , 13 , 39 , 40 , 41 , 45 In addition, our study relies on the available access to care measures in the surveys; it is known that access to care is broadly conceptualized beyond health insurance coverage, having a personal doctor, delayed care due to cost, and having a routine checkup. 46 Missing variables should be considered when interpreting results. BRFSS does not collect citizenship status, which is a key predictor for health care access and utilization. ACS/PRCS does not include health care needs and other facilitating measures that could affect health insurance enrollment.
Another limitation to our study is the violation of the parallel trends assumption for one of our comparison states (New York) in the probability of having any public health insurance. Our analytic design for the ACS/PRCS data limited our capacity to fully interpret the DiD estimates for New York versus Florida and New York versus Puerto Rico. However, we highlighted how New York's trajectory for this outcome shifted post‐ACA, which is a possible indicator of the ACA's policy impact. Nonetheless, we continue to advise careful interpretation of the New York DiD estimates.
In this study, we were unable to separately study 2019 changes possibly resulting from the elimination of the individual mandate; we recognize the possible impact of this policy shift on health insurance enrollment patterns among Latinos not captured within our analyses. 26 In addition, this study does not account for the large migration numbers of Latinos from Puerto Rico to Florida and New York after Hurricane Maria in 2017, which could have affected health insurance rates and other observations of health care access outcomes. 47 Finally, considering that our sample was limited to only Latinos in three “states” (New York, Florida, and Puerto Rico), these results might not be generalizable to Latinos in all states. Despite these limitations, this study contributes to the limited literature studying health care inequities and policy implications on Latino health. Moreover, it provides insight into the implications of federal health policy for Latinos living in Puerto Rico, which is an understudied territory and population.
4.4. Conclusion
Differences in states' Medicaid funding structures and expansion decisions can exacerbate health care inequities among Latinos living in the United States. For Latinos in low‐income households, limited Medicaid eligibility (Florida Medicaid non‐expansion) and capped Medicaid funds (Puerto Rico Medicaid block grant) can further limit access to public health insurance over time. While there is room to improve Latino health care access across funding structures in the United States, local policy makers' willingness plays a critical role in minimizing health care inequities for this population. Our study shows the need to include Puerto Rico in Medicaid expansion to improve health care equity. Furthermore, we highlight how capped Medicaid funds and limited Medicaid eligibility are risk factors for poor health care access for Latinos, especially for Latinos living in poverty.
Supporting information
Appendix S1. Supplementary information.
ACKNOWLEDGMENTS
This work was supported, in part, by a grant to Dr. Ortega from the National Institute on Minority Health and Health Disparities (NIMHD) at NIH (R01 MD013866).
Rivera‐González AC, Roby DH, Stimpson JP, et al. The impact of Medicaid funding structures on inequities in health care access for Latinos in New York, Florida, and Puerto Rico. Health Serv Res. 2022;57(Suppl. 2):172‐182. doi: 10.1111/1475-6773.14036
Funding information National Institute on Minority Health and Health Disparities, Grant/Award Number: R01 MD013866
REFERENCES
- 1. Ma A, Sanchez A, Ma M. Racial disparities in health care utilization, the Affordable Care Act and racial concordance preference. Int J Health Econ Manag. 2021;22:1‐20. doi: 10.1007/s10754-021-09311-8 [DOI] [PubMed] [Google Scholar]
- 2. Chen J, Vargas‐Bustamante A, Mortensen K, Ortega AN. Racial and ethnic disparities in health care access and utilization under the Affordable Care Act. Med Care. 2016;54(2):140‐146. doi: 10.1097/MLR.0000000000000467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. OMH . Profile: Hispanic/Latino Americans. US Department of Health and Human Services. 2021. Accessed January 17, 2022. https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=3&lvlid=64
- 4. NCPSSM . Medicare and Medicaid are important to Hispanic Americans. National Committee to Preserve Social Security and Medicare. 2020. Accessed January 17, 2022. https://www.ncpssm.org/documents/medicare‐policy‐papers/medicare‐and‐medicaid‐are‐important‐to‐hispanic‐americans/
- 5. Guth M, Artiga S, Pham O. Effects of the ACA Medicaid expansion on racial disparities in health and health care. KFF. 2020. Accessed January 17, 2022. https://www.kff.org/medicaid/issue‐brief/effects‐of‐the‐aca‐medicaid‐expansion‐on‐racial‐disparities‐in‐health‐and‐health‐care/
- 6. Center on Budget and Policy Priorities . Policy basics: introduction to Medicaid. CBPP. 2020. Accessed January 17, 2022. https://www.cbpp.org/research/health/introduction-to-medicaid
- 7. Yue D, Rasmussen PW, Ponce NA. Racial/ethnic differential effects of Medicaid expansion on health care access. Health Serv Res. 2018;53(5):3640‐3656. doi: 10.1111/1475-6773.12834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Norris L. Affordable Care Act's basic health program. Healthinsurance.org. 2021. Accessed April 27, 2022. https://www.healthinsurance.org/obamacare/affordable-care-acts-basic-health-program/
- 9. Dorn S, Tolbert J. The ACA's Basic Health Program option: federal requirements and state trade‐offs. KFF. 2014. Accessed April 27, 2022. https://www.kff.org/health-reform/report/the-acas-basic-health-program-option-federal-requirements-and-state-trade-offs/
- 10. Messerly M. Oregon, Kentucky dust off an Obama‐era policy to expand health insurance. Politico. 2022. Accessed May 5, 2022. https://www.politico.com/news/2022/04/29/oregon‐kentucky‐dust‐off‐an‐obama‐era‐policy‐to‐expand‐health‐insurance‐00029111
- 11. US Census Bureau . Quick facts: Puerto Rico. 2021. Accessed January 17, 2022. https://www.census.gov/quickfacts/PR
- 12. Park E. How states would fare under Medicaid block grants or per capita caps: lessons from Puerto Rico. The Commonwealth Fund. 2021. Accessed January 17, 2022. https://www.commonwealthfund.org/publications/issue‐briefs/2021/jan/how‐states‐fare‐medicaid‐block‐grants‐per‐capita‐caps‐puerto‐rico
- 13. Portela M, Sommers BD. On the outskirts of national health reform: a comparative assessment of health insurance and access to care in Puerto Rico and the United States. Milbank Q. 2015;93(3):584‐608. doi: 10.1111/1468-0009.12138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Perreira KM, Jones DK, Oberlander J. Capping Medicaid funding—lessons from Puerto Rico. Am J Public Health. 2017;107(12):1900‐1901. doi: 10.2105/AJPH.2017.304138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Roman J. The Puerto Rico healthcare crisis. Ann Am Thorac Soc. 2015;12(12):1760‐1763. doi: 10.1513/AnnalsATS.201508-531PS [DOI] [PubMed] [Google Scholar]
- 16. MACPAC . Fact Sheet: Medicaid and CHIP in Puerto Rico. Medicaid and CHIP Payment and Access Commission; 2021. https://www.macpac.gov/wp-content/uploads/2020/08/Medicaid-and-CHIP-in-Puerto-Rico.pdf [Google Scholar]
- 17. MACPAC . Testimony Medicaid and CHIP in the U.S. Territories. Medicaid and CHIP Payment and Access Commission; 2021. https://www.macpac.gov/wp‐content/uploads/2021/03/Testimony‐Medicaid‐and‐CHIP‐in‐the‐U.S.‐Territories.pdf [Google Scholar]
- 18. Sullivan Benefits . ACA overview: impact of the ACA in U.S. Territories. 2016. Accessed January 17, 2022. https://www.sullivan‐benefits.com/wp‐content/uploads/Impact‐of‐the‐ACA‐in‐US‐Territories‐10.31.16.pdf
- 19. MACPAC . Report to Congress on Medicaid and CHIP: Medicaid in Puerto Rico. Medicaid and CHIP Payment and Access Commission; 2018. https://www.medicaid.pr.gov/pdf/Congress/MACPAC%20MANDATED%20REPORT%20‐%20MEDICAID%20IN%20PUERTO%20RICO.pdf [Google Scholar]
- 20. Solomon J. Puerto Rico's Medicaid program needs an ongoing commitment of federal funds. CBPP. 2019. Accessed January 17, 2022. https://www.cbpp.org/research/health/puerto‐ricos‐medicaid‐program‐needs‐an‐ongoing‐commitment‐of‐federal‐funds
- 21. Denham A, Veazie PJ. Did Medicaid expansion matter in states with generous Medicaid? Am J Manag Care. 2019;25(3):129‐134. [PubMed] [Google Scholar]
- 22. Norris L. New York and the ACA's Medicaid expansion. Healthinsuranceorg. 2022. Accessed April 27, 2022. https://www.healthinsurance.org/medicaid/new-york/
- 23. Office of Health Insurance Programs . Essential plan: New York's basic health program. NY Department of Health. 2018. Accessed April 27, 2022. https://www.health.ny.gov/health_care/managed_care/essential/docs/2018_basic_health_program.pdf
- 24. Collins SR, Gunja MZ, Doty MM, Bhupal HK. First look at health insurance coverage in 2018 finds ACA gains beginning to reverse. The Commonwealth Fund. 2018. Accessed April 27, 2022. https://www.commonwealthfund.org/blog/2018/first‐look‐health‐insurance‐coverage‐2018‐finds‐aca‐gains‐beginning‐reverse
- 25. Ortega AN, Pintor JK, Alberto CK, Roby DH. Inequities in insurance coverage and well‐child visits improve, but insurance gains for white and black youth reverse. Acad Pediatr. 2020;20(1):14‐15. doi: 10.1016/j.acap.2019.08.005 [DOI] [PubMed] [Google Scholar]
- 26. Ortega AN, Chen J, Roby DH, Mortensen K, Rivera‐González AC, Vargas Bustamante A. Changes in coverage and cost‐related delays in Care for Latino Individuals after Elimination of the affordable care Act's individual mandate. JAMA Netw Open. 2022;5(3):e221476. doi: 10.1001/jamanetworkopen.2022.1476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. NCCDPHP . About BRFSS. CDC. 2014. Accessed January 17, 2022. https://www.cdc.gov/brfss/about/index.htm
- 28. NIOSH . Behavioral risk factor surveillance system (BRFSS). CDC. 2021. Accessed January 17, 2022. https://www.cdc.gov/niosh/topics/surveillance/brfss/default.html
- 29. Ruggles S, Flood S, Foster S, et al. IPUMS USA: Version 11.0 [dataset]. IPUMS; 2021. doi: 10.18128/D010.V11.0 [DOI] [Google Scholar]
- 30. Torrieri N. American Community Survey Design and Methodology. US Census Bureau; 2014. https://www2.census.gov/programs‐surveys/acs/methodology/design_and_methodology/acs_design_methodology_report_2014.pdf [Google Scholar]
- 31. Institute of Medicine . The Impacts of the Affordable Care Act on Preparedness Resources and Programs: Workshop Summary. National Academies Press; 2014. [PubMed] [Google Scholar]
- 32. Replicate Weights in the American Community Survey/Puerto Rican Community Survey. IPUMS USA. Accessed May 5, 2022. https://usa.ipums.org/usa/repwt.shtml
- 33. ASPE . Issue Brief: Health Insurance Coverage and Access to Care among Latinos: Recent Trends and Key Challenges. US Department of Health and Human Services; 2021. https://aspe.hhs.gov/sites/default/files/documents/68c78e2fb15209dd191cf9b0b1380fb8/ASPE_Latino_Health_Coverage_IB.pdf [Google Scholar]
- 34. Distribution of the Total Population by Federal Poverty Level (above and below 200% FPL). KFF. 2020. Accessed April 27, 2022. https://www.kff.org/other/state‐indicator/population‐up‐to‐200‐fpl/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D
- 35. Musumeci M. Medicaid provisions in the American rescue plan act. KFF. 2021. Accessed January 17, 2022. https://www.kff.org/medicaid/issue-brief/medicaid-provisions-in-the-american-rescue-plan-act/
- 36. Solomon J. Federal action needed to close Medicaid “coverage gap,” extend coverage to 2.2 million people. CBPP. 2021. Accessed January 17, 2022. https://www.cbpp.org/research/health/federal-action-needed-to-close-medicaid-coverage-gap-extend-coverage-to-22-million
- 37. Sullivan J, Wagner J, Bailey A, Solomon J. New house build back better legislation would make long‐lasting Medicaid improvements. CBPP. 2021. Accessed January 17, 2022. https://www.cbpp.org/research/health/new‐house‐build‐back‐better‐legislation‐would‐make‐long‐lasting‐medicaid
- 38. Solomon J. Build back better legislation would close the Medicaid coverage gap. CBPP. 2021. Accessed January 17, 2022. https://www.cbpp.org/research/health/build‐back‐better‐legislation‐would‐close‐the‐medicaid‐coverage‐gap
- 39. Wachino V, Gronniger T. The insufficiency of Medicaid block grants: the example of Puerto Rico. Health Affairs Forefront. 2017. doi: 10.1377/forefront.20171022.984682 [DOI]
- 40. Patron M. Puerto Rico's exodus of doctors adds health care strain to dire financial crisis. NBC News. 2017. Accessed January 17, 2022. https://www.nbcnews.com/news/latino/puerto‐rico‐s‐exodus‐doctors‐adds‐health‐care‐strain‐dire‐n783776
- 41. Wilkinson E, Killeen D, Perez‐Lopez GJ, Jabbarpour Y. A shrinking primary care workforce in Puerto Rico. Am Fam Physician. 2020;101(1):13‐14. [PubMed] [Google Scholar]
- 42. Guasp G, Bigio G. Funding challenges of Medicaid in Puerto Rico. V2A Consulting. 2021. Accessed April 27, 2022. https://v2aconsulting.com/funding-challenges-of-medicaid-in-puerto-rico/
- 43. Puerto Rico Health Care Fairness, Accountability, and Beneficiary Access Act of 2019, HR 3371, 116th Cong, 1st Sess (2019).
- 44. Velázquez Reintroduces Bill to Provide Medicaid Parity for Puerto Rico [press release]. 2021. Accessed January 17, 2022. https://velazquez.house.gov/media‐center/press‐releases/vel‐zquez‐reintroduces‐bill‐provide‐medicaid‐parity‐puerto‐rico
- 45. Kovacs RJ, Rodríguez‐Vilá O. The challenges of inequitable care: A look at Puerto Rico versus US states. J Am Coll Cardiol. 2020;75(15):1857‐1859. doi: 10.1016/j.jacc.2020.03.007 [DOI] [PubMed] [Google Scholar]
- 46. Aday LA, Andersen RM. Equity of access to medical care: a conceptual and empirical overview. Med Care. 1981;19(12):4‐27. [PubMed] [Google Scholar]
- 47. Sutter JD, Hernandez S. ‘Exodus’ from Puerto Rico: a visual guide. CNN. 2018. Accessed January 17, 2022. https://edition.cnn.com/2018/02/21/us/puerto-rico-migration-data-invs/index.html
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. Supplementary information.


