Abstract
Objective
To evaluate the frequency of emergency department (ED) revisits among elderly patients with gastrointestinal bleeding secondary to anticoagulant treatment and identify factors associated with an increased risk of ED revisits.
Methods
A 3-year retrospective observational study was designed, including elderly patients (≥65 years) with atrial fibrillation and undergoing oral anticoagulation therapy who visited the ED for gastrointestinal bleeding. To evaluate the risk factors for 30-day revisit, a multivariate analysis was designed including comorbidities, concomitant treatment, change in anticoagulant treatment and prescription of direct-acting oral anticoagulants.
Results
80 patients were included. At discharge, anticoagulation therapy was modified in 21 (26.2%) patients; and changed from an oral anticoagulant to heparin in 17 (21.2%) patients and to another oral anticoagulant in 4 (5.0%) patients. Anticoagulant treatment was withdrawn in 5 (6.3%) patients at discharge. Eleven (13.7%) patients revisited the ED 30 days after hospital discharge for bleeding episodes. No differences in the frequency of revisit to the ED were observed in the patients who changed their anticoagulant treatment at discharge. In the multivariate analysis, chronic kidney disease was the only factor significantly associated with revisits at 30 days.
Conclusions
Elderly patients who experience a first episode of gastrointestinal bleeding have a high risk of revisiting the ED for a bleeding episode, with no particular differences between the types of anticoagulant prescribed at discharge.
Keywords: anticoagulants, emergency medicine, geriatrics, drug-related side effects and adverse reactions, safety
Introduction
Drug-related problems (DRPs), defined as pharmacotherapy failures due to lack of efficacy, safety or need for non-prescribed treatments, are major health problems, accounting for approximately 30% visits to the emergency department (ED).1 2 Oral anticoagulants (OACs) are one of the therapeutic groups most frequently involved in these DRPs,2–4 and gastrointestinal bleeding is one of the main causes of ED consultation.5 6 Gastrointestinal bleeding occurs in 8%–15%7 of patients treated with vitamin K antagonists (VKA), not having observed significant differences when compared with direct oral anticoagulants (DOACs).8 9
Although other studies have analysed the frequency of ED visits for gastrointestinal bleeding related to the use of OACs,6 10 to our knowledge, the effect of the treatment prescribed to elderly patients at discharge on the risk of ED revisits is unknown. Moreover, data regarding the risk factors involved in the onset of new bleeding episodes associated with new anticoagulant treatment after the first episode are scarce. Given the increase in the use of anticoagulants among the elderly population,11 12 the identification of risk factors associated with new bleeding episodes is particularly relevant.
Thus, we proposed the present study to describe the frequency of 30-day ED revisit among elderly patients with atrial fibrillation and gastrointestinal bleeding episodes secondary to anticoagulant treatment, to evaluate the differences in revisit according to the anticoagulant treatment prescribed and to identify factors associated with increased risk of ED revisit.
Materials and methods
A retrospective cohort study was designed which included elderly patients (≥65 years) with atrial fibrillation and undergoing OAC treatment, who visited the ED for a first gastrointestinal bleeding episode from January 2017 to December 2019. Patients who required hospitalisation, diagnosed with malignant neoplasms after the episode or died during their stay in the ED were excluded from the study.
The study was conducted in an ED of an urban teaching, tertiary referral hospital from Catalonia (Spain) serving about 407.000 inhabitants, with an annual volume of approximately 150.000 ED attendances. Of these, 115 000 correspond to adult emergencies, 40% of them are over 65 years old and more than 30% of them are vulnerable patients (dementia, dependence, active oncological disease, chronic diseases and comorbidities, disability).13 Patients with gastrointestinal bleeding secondary to OACs included in the study were selected from the DRP registry database in the ED. This database is filled in from Monday to Friday by clinical pharmacists assigned to the ED of the hospital based on the data collected from the morning daily ward round, where the pharmacists are present. DRPs are included in this database if the information included in the discharge summary form indicates that the reason for attending the ED has been caused directly or indirectly to a DRP.
The patient’s demographic and clinical information was obtained from the electronic medical records available in the hospital. The patient’s comorbidities and chronic treatment were obtained from the hospital admission report and from the electronic prescription registry in primary care. Differences between the percentage of patients who revisited the ED 30 days after discharge based on the anticoagulant treatment prescribed and changes in anticoagulation therapy at discharge were evaluated using the χ2 test.
A multivariate analysis was designed to assess the risk factors associated with 30-day ED revisit for all causes and bleeding episodes that included variables with a p value <0.2 in a previous univariate analysis. The factors analysed in this study included very elderly patients (>80 years), sex, comorbidities (chronic kidney disease (CKD) stage 3 or worse (estimated glomerular filtration rate <60 mL/min/1.73 m2),14 heart failure, diabetes mellitus type 2, hypertension, HAS-BLED score ≥3), major polypharmacy (≥10 drugs, included medication prescribed as regular and ‘if needed’),15 concomitant use of gastrolesive drugs (including antiplatelet drugs, corticosteroids and non-steroidal anti-inflammatory drugs), gastroprotective drugs at discharge, change in the anticoagulation therapy (defined as change in anticoagulant drug at discharge relative to anticoagulant drug involved in bleeding episode) and anticoagulant treatment prescribed after discharge from the ED. With respect to discharge with heparin, treatment with this drug was considered when the patient continued the treatment for more than 7 days after the bleeding episode or revisit to the ED during heparin treatment.
Results
The characteristics of the 80 patients included in this study are outlined in table 1. Before the first episode of bleeding, 45 (56.2%) patients were treated with VKA (5 (6.3%) with warfarin and 40 (50.0%) with acenocoumarol), and 35 (43.8%) with DOACs (16 (20.0%) with apixaban, 6 (7.5%) with edoxaban, 8 (10.0%) with rivaroxaban and 5 (6.3%) with dabigatran).
Table 1.
Characteristics of patients included in the study based on the anticoagulation treatment at discharge
| Total | VKA (n=31) |
DOACs (n=27) | LMWH (n=17) | Withdrawn (n=5) | P value | |
| Age (mean; SD) | 83.6 (6.6) | 83.1 (6.1) | 84.4 (6.6) | 82.3 | 84.8 | 0.656 |
| Female (%) | 30 (68.5) | 21 (67.7) | 20 (74.1) | 5 (52.9) | 5 (100.0) | 0.353 |
| Comorbidities (%) | ||||||
| Hypertension | 62 (77.5) | 24 (77.4) | 20 (74.1) | 15 (8.2) | 3 (60.0) | 0.542 |
| Chronic heart failure | 31 (38.7) | 10 (32.3) | 13 (48.2) | 7 (41.2) | 1 (20.0) | 0.493 |
| Diabetes mellitus type 2 | 27 (59.3) | 13 (41.9) | 10 (37.0) | 4 (23.5) | 0 (0.0) | 0.427 |
| COPD | 14 (17.5) | 7 (22.6) | 3 (11.1) | 4 (23.5) | 0 (0.0) | 0.429 |
| Chronic kidney disease | 28 (35.0) | 13 (41.9) | 8 (29.6) | 7 (41.2) | 0 (0.0) | 0.581 |
| Cognitive disorders | 21 (26.3) | 5 (16.3) | 11 (40.7) | 3 (17.7) | 2 (40.0) | 0.131 |
| Discharge (%) | 0.022 | |||||
| Home | 51 (63.7) | 17 (54.8) | 18 (66.7) | 14 (82.3) | 2 (40.0) | |
| Nursing home | 11 (13.7) | 5 (16.3) | 4 (14.8) | 0 (0.0) | 2 (40.0) | |
| Long-term healthcare centre | 18 (22.6) | 9 (29.0) | 5 (18.5) | 3 (17.7) | 1 (20.0) | |
| Number of drugs at discharge (mean; SD) | 10.1 (3.14) | 9.9 (3.2) | 11.0 (3.0) | 9.2 (4.3) | 9.4 (2.3) | 0.643 |
COPD, chronic obstructive pulmonary disease; DOACs, direct oral anticoagulants; LMWH, low-molecular-weight heparin; VKA, vitamin K antagonist.
In addition, 51 (63.7%) patients were discharged from the ED to their homes, 11 (13.7%) to nursing homes and 18 (22.5%) to community health centres. At discharge, anticoagulation therapy was modified in 21 (26.2%) patients, changed to heparin in 17 (21.2%) patients and to a different OAC in 4 (5.0%) patients. Anticoagulant treatment was withdrawn in 5 (6.3%) patients at discharge. These changes are described in figure 1. At discharge, 31 (38.8%) patients were undergoing treatment with VKA, 27 (33.8%) with DOAC and 17 (21.0%) with low-molecular-weight heparin. Ten (12.5%) patients were undergoing bridging therapy with heparin less than 7 days before starting OACs.
Figure 1.
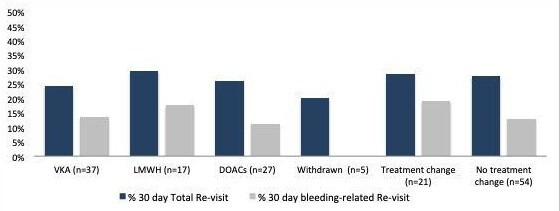
Percentage of 30-day readmission based on the anticoagulation treatment at discharge. DOACs, direct-acting oral anticoagulants; LMWH, low molecular weight heparin; VKA, vitamin K antagonists.
Twenty-two (27.5%) patients revisited the ED 30 days after hospital discharge, including 11 (13.7%) related to bleeding events, of whom 3 (27.2%) had changed their anticoagulant therapy at discharge. One patient died and another patient suffered a cardioembolic stroke during this period. Change in anticoagulation therapy at discharge did not result in a lower frequency of 30-day revisit to the ED (27.8% vs 28.5%; p=0.952). Moreover, no significant changes in the number of revisits were observed at 30 days depending on anticoagulant treatment at discharge (p=0.068).
Factors associated with all-cause revisits at 30 days (p<0.200) were age >80 years, major polypharmacy, HAS-BLED score ≥3 points, sex and CKD. In the multivariate analysis (table 2), none of the variables differed were significantly associated with all-cause revisits. Regarding readmissions after 30 days related to bleeding episodes, major polypharmacy, HAS-BLED score ≥3, sex and CKD were the factors associated with a higher risk of revisits. CKD was the only factor showing a significant association in the multivariate analysis (OR 5.74 (1.09–19.02)).
Table 2.
Results from the univariate and multivariate analyses
| Total 30-day revisit | 30-day revisit due to bleeding episode | |||||
| Univariate (P value) |
Multivariate | P value | Univariate (P value) |
Multivariate | P value | |
| Age >80 years | 0.183 | 1.91 (0.65–5.65) | 0.237 | 0.831 | ||
| Female | 0.096 | 0.54 (0.18–1.68) | 0.292 | 0.019 | 0.37 (0.08–1.70) | 0.202 |
| Hypertension | 0.976 | 0.713 | ||||
| Chronic heart failure | 0.807 | 0.861 | ||||
| Diabetes mellitus type 2 | 0.822 | 0.844 | ||||
| Chronic kidney disease | 0.027 | 2.92 (0.98–8.81) | 0.057 | 0.011 | 5.74 (1.09–19.02) | 0.032 |
| COPD | 0.321 | 0.432 | ||||
| DOACs | 0.875 | 0.919 | ||||
| Treatment change | 0.945 | 0.506 | ||||
| Other gastrolesive drugs | 0.921 | 0.341 | ||||
| ≥10 drugs | 0.197 | 1.60 (0.53–4.76) | 0.397 | 0.177 | 3.69 (0.79–17.2) | 0.096 |
| HAS-BLED score ≥3 | 0.031 | 1.55 (0.65–3.65) | 0.331 | 0.052 | 1.30 (0.36–4.59) | 0.383 |
COPD, chronic obstructive pulmonary disease; DOACs, direct oral anticoagulants.
Discussion
According to the results from our study, patients with gastrointestinal bleeding secondary to OACs attending in ED do not have a lower risk of revisit after switching to another anticoagulant treatment. CKD was a risk factor for ED revisit related to bleeding episodes 30 days after discharge.
Managing anticoagulant therapy after a bleeding episode is a complex situation, where both the risk of a new bleeding episode and the onset of thromboembolic events have to be weighed in, and only limited data regarding this are available in the literature. According to the results from our study, 13% of patients revisited the ED for a bleeding episode 30 days after discharge, similar results than reposted in previous studies.16 17
Most patients in our study maintained their anticoagulant treatment after hospital discharge, being withdrawn in only five patients. Several studies have shown that continuing anticoagulant treatment after an episode of gastrointestinal bleeding significantly reduces the risk of thrombosis and mortality.16 17 Therefore, clinical practice guidelines advocate anticoagulation therapy after an episode of gastrointestinal bleeding.18 19 The difficulty lies in selecting the treatment to be used after the bleeding episode. Differences in the risk of bleeding between patients treated with VKA and those treated with DOACs have been continually discussed. A meta-analysis with 43 clinical trials found no difference in the incidence of bleeding between patients using DOACs and VKAs.19
Elderly patients are commonly associated with an increased risk of bleeding20 and they require a special attention. Data on the introduction of DOACs after a bleeding episode in this group of patients remain scarce. In a retrospective study, Sengupta et al 21 found no significant differences in the incidence of bleeding between patients who started DOAC and those in whom treatment was withdrawn at discharge. This finding was in line with our data. In another retrospective study, no significant differences in the recurrence of gastrointestinal bleeding were found between patients treated with warfarin at admission and those treated with DOAC during hospitalisation.22
Given the high short-term risk of bleeding, multidisciplinary interventions beyond change in treatment are necessary to prevent revisit. Increase in the patient’s knowledge and understanding on their anticoagulant treatment provided by healthcare professionals has been shown to be effective in reducing the incidence of bleeding11; hence, this should be included as the measures to be implemented in this group of patients.
In this study, patients with CKD have been identified as a group associated with an increased risk of revisit both for new episodes of bleeding. In this group of patients, the use of anticoagulants is known to increase the risk of bleeding.23 Although the use of DOACs in elderly patients with kidney failure has been associated with improved control of bleeding episodes,24 our study results do not reveal this advantage in this population group. Given the increase in the number of elderly patients on anticoagulant treatment10 11 and the high prevalence of CKD in this population group,25 further clinical experience is needed to contextualise the use of DOACs and VKAs in them.
The limitations of our study include its retrospective approach and the lack of data on adequate patient adherence to treatment. In addition, our study did not prospectively investigate the possible neoplasms or polyps as bleeding causes for different anticoagulant groups, which have been previously established as the causes of approximately 10% of gastrointestinal bleeding episodes.26 Because of the small group of patients taking DOACs at discharge, comparisons between them were not possible. On the other hand, the small sample size makes that the results obtained should be interpreted carefully. We have excluded those patients admitted to the hospital ward, which has prevented obtaining a larger sample size. However, these exclusion criteria made the results obtained valid for those patients directly discharged from the ED, a situation that occurs frequently in patients with less severe bleeding episodes. Furthermore, the fact that only those patients identified in the morning daily rounds were included in the study probably means that a number of relevant patients who came to the ED during the study period due to bleeding episodes have not been studied when they were treated in the emergency service in periods not covered by the personnel involved in the DRP registration.
In conclusion, our results show that elderly patients with atrial fibrillation and gastrointestinal bleeding have a risk of revisit close to 13%, with no significant differences between the types of anticoagulant prescribed at discharge. CKD may be a risk factor for new bleeding episodes and should be carefully analysed in future studies.
What this paper adds.
What is already known on this subject
Oral anticoagulants are one of the therapeutic groups most frequently involved in these drug-related problems and gastrointestinal bleeding is the main cause of emergency department consultation.
The effect of the treatment prescribed to elderly patients at discharge on the risk of emergency department revisits is unknown
What this study adds
In a retrospective study, we found that elderly patients with atrial fibrillation and gastrointestinal bleeding are at a higher risk of revisit for bleeding events, with no significant differences between the different anticoagulants prescribed at discharge.
Chronic kidney disease may be considered as a risk factor for new bleeding episodes.
Footnotes
Contributors: Contributions were as follows: Conception and design: JR, LL, AJ, MAM; acquisition of data: JR, ARM, LL; interpretation and analysis: MAM, MP, AJ; statistics: JR; writing: JR, ARM.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: JR, AJ and MAM declare potential conflict of interest with Behringer.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
Data are available upon reasonable request. All data relevant to the study are included in the article or uploaded as supplementary information.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
This study was approved by the Clinical Research Ethics Committee of the Santa Pau Hospital (Hospital Santa Pau; reference number: IIBSP-COD-2018-25).
References
- 1. Nivya K, Sri Sai Kiran V, Ragoo N, et al. Systemic review on drug related hospital admissions - A pubmed based search. Saudi Pharm J 2015;23:1–8. 10.1016/j.jsps.2013.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Lazarou J, Pomeranz BH, Corey PN. Incidence of adverse drug reactions in hospitalized patients: a meta-analysis of prospective studies. JAMA 1998;279:1200–5. 10.1001/jama.279.15.1200 [DOI] [PubMed] [Google Scholar]
- 3. Baena MI, Faus MJ, Fajardo PC, et al. Medicine-related problems resulting in emergency department visits. Eur J Clin Pharmacol 2006;62:387–93. 10.1007/s00228-006-0116-0 [DOI] [PubMed] [Google Scholar]
- 4. Castro I, Guardiola JM, Tuneu L, et al. Drug-Related visits to the emergency department in a Spanish university hospital. Int J Clin Pharm 2013;35:727–35. 10.1007/s11096-013-9795-7 [DOI] [PubMed] [Google Scholar]
- 5. Pollack CV, Peacock WF, Bernstein RA, et al. The safety of oral anticoagulants registry (SOAR): a national, ED-based study of the evaluation and management of bleeding and bleeding concerns due to the use of oral anticoagulants. Am J Emerg Med 2020;38:1163–70. 10.1016/j.ajem.2019.12.023 [DOI] [PubMed] [Google Scholar]
- 6. Diener H-C, Aisenberg J, Ansell J, et al. Choosing a particular oral anticoagulant and dose for stroke prevention in individual patients with non-valvular atrial fibrillation: Part 2. Eur Heart J 2017;38:860–8. 10.1093/eurheartj/ehw069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Marmo R, Del Piano M, Rotondano G, et al. Mortality from nonulcer bleeding is similar to that of ulcer bleeding in high-risk patients with nonvariceal hemorrhage: a prospective database study in Italy. Gastrointest Endosc 2012;75:263–72. 10.1016/j.gie.2011.07.066 [DOI] [PubMed] [Google Scholar]
- 8. Chai-Adisaksopha C, Crowther M, Isayama T, et al. The impact of bleeding complications in patients receiving target-specific oral anticoagulants: a systematic review and meta-analysis. Blood 2014;124:2450–8. 10.1182/blood-2014-07-590323 [DOI] [PubMed] [Google Scholar]
- 9. Miller CS, Dorreen A, Martel M, et al. Risk of Gastrointestinal Bleeding in Patients Taking Non-Vitamin K Antagonist Oral Anticoagulants: A Systematic Review and Meta-analysis. Clin Gastroenterol Hepatol 2017;15:1674–83. 10.1016/j.cgh.2017.04.031 [DOI] [PubMed] [Google Scholar]
- 10. Diamantopoulou G, Konstantakis C, Skroubis G, et al. Acute lower gastrointestinal bleeding in patients treated with non-vitamin K antagonist oral anticoagulants compared with warfarin in clinical practice: characteristics and clinical outcome. Gastroenterology Res 2019;12:21–6. 10.14740/gr1115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Alalwan A, Voils S, Hartzema A. Trends in the utilization of warfarin and non-vitamin K oral anticoagulants in elderly patients with atrial fibrillation. Value in Health 2016;19:A42. 10.1016/j.jval.2016.03.084 [DOI] [PubMed] [Google Scholar]
- 12. Garwood CL, Corbett TL. Use of anticoagulation in elderly patients with atrial fibrillation who are at risk for falls. Ann Pharmacother 2008;42:523–32. 10.1345/aph.1K498 [DOI] [PubMed] [Google Scholar]
- 13. Masnoon N, Shakib S, Kalisch-Ellett L, et al. What is polypharmacy? A systematic review of definitions. BMC Geriatr 2017;17:230. 10.1186/s12877-017-0621-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. National Kidney Foundation . K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis 2002;39:S1–266. [PubMed] [Google Scholar]
- 15. Boldt J. The concept of vulnerability in medical ethics and philosophy. Philos Ethics Humanit Med 2019;14:6. 10.1186/s13010-019-0075-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Witt DM, Delate T, Garcia DA, et al. Risk of thromboembolism, recurrent hemorrhage, and death after warfarin therapy interruption for gastrointestinal tract bleeding. Arch Intern Med 2012;172:1484–91. 10.1001/archinternmed.2012.4261 [DOI] [PubMed] [Google Scholar]
- 17. Sengupta N, Feuerstein JD, Patwardhan VR, et al. The risks of thromboembolism vs. recurrent gastrointestinal bleeding after interruption of systemic anticoagulation in hospitalized inpatients with gastrointestinal bleeding: a prospective study. Am J Gastroenterol 2015;110:328–35. 10.1038/ajg.2014.398 [DOI] [PubMed] [Google Scholar]
- 18. American College of Cardiology . Consensus for management of bleeding on oral anticoagulants. Available: http%3a%2f%2fwww.acc.org%2flatest-in-cardiology%2ften-points-to-remember%2f2017%2f11%2f29%2f17%2f23%2f2017-acc-expert-consensus-of-bleeding-on-oacs [Accessed 15 Apr 2020].
- 19. Radaelli F, Dentali F, Repici A, et al. Management of anticoagulation in patients with acute gastrointestinal bleeding. Dig Liver Dis 2015;47:621–7. 10.1016/j.dld.2015.03.029 [DOI] [PubMed] [Google Scholar]
- 20. Eikelboom JW, Wallentin L, Connolly SJ, et al. Risk of bleeding with 2 doses of dabigatran compared with warfarin in older and younger patients with atrial fibrillation: an analysis of the randomized evaluation of long-term anticoagulant therapy (RE-LY) trial. Circulation 2011;123:2363–72. 10.1161/CIRCULATIONAHA.110.004747 [DOI] [PubMed] [Google Scholar]
- 21. Sengupta N, Marshall AL, Jones BA, et al. Rebleeding vs thromboembolism after hospitalization for gastrointestinal bleeding in patients on direct oral anticoagulants. Clin Gastroenterol Hepatol 2018;16:1893–900. 10.1016/j.cgh.2018.05.005 [DOI] [PubMed] [Google Scholar]
- 22. Qureshi W, Mittal C, Patsias I, et al. Restarting anticoagulation and outcomes after major gastrointestinal bleeding in atrial fibrillation. Am J Cardiol 2014;113:662–8. 10.1016/j.amjcard.2013.10.044 [DOI] [PubMed] [Google Scholar]
- 23. Aursulesei V, Costache II. Anticoagulation in chronic kidney disease: from guidelines to clinical practice. Clin Cardiol 2019;42:774–82. 10.1002/clc.23196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hanon O, Jeandel C, Jouanny P, et al. Anticoagulant treatment in elderly patients with atrial fibrillation: position paper. Geriatr Psychol Neuropsychiatr Vieil 2019;17:341–55. [DOI] [PubMed] [Google Scholar]
- 25. Mallappallil M, Friedman EA, Delano BG, et al. Chronic kidney disease in the elderly: evaluation and management. Clin Pract 2014;11:525–35. 10.2217/cpr.14.46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Flack KF, Desai J, Kolb JM, et al. Major Gastrointestinal Bleeding Often Is Caused by Occult Malignancy in Patients Receiving Warfarin or Dabigatran to Prevent Stroke and Systemic Embolism From Atrial Fibrillation. Clin Gastroenterol Hepatol 2017;15:682–90. 10.1016/j.cgh.2016.10.011 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available upon reasonable request. All data relevant to the study are included in the article or uploaded as supplementary information.


