Abstract
Objectives
The effective implementation of a fast-changing healthcare delivery innovation, such as robotic-assisted surgery (RAS), into a healthcare system, can be affected (both positively and negatively) by external contextual factors. As part of a wider project investigating ways to optimise the implementation of RAS, this qualitative study aimed to uncover current issues of RAS and predictions about the future of robotic surgery. We refer to ‘current issues’ as the topical and salient challenges and opportunities related to the introduction of RAS in the UK healthcare system, from the perspectives of key stakeholders involved in the delivery and implementation of RAS.
Design
Semi-structured interviews and focus groups were conducted. A thematic analysis was conducted to summarise salient issues that were articulated by the participants.
Setting and participants
The interview sample (n=35) comprised surgeons, wider theatre staff and other relevant personnel involved in the introduction and delivery of RAS services across the UK, including service managers and policymakers/commissioners. Two focus groups were also conducted with surgical trainees (n=7) and members of the public (n=8), respectively.
Results
The results revealed a largely positive attitude towards the introduction of RAS technology and an expectation of continued rapid expansion. Areas perceived to be particularly pertinent and requiring ongoing attention were also highlighted, including the need to achieve improved quality control, expertise quantification and training issues and the need to educate the public. Issues of centralisation, service organisation and equity of access were also emphasised.
Conclusions
Our study has highlighted a range of issues perceived to be particularly pertinent to the current and future provision of RAS which should be addressed. The areas outlined can enable healthcare managers and surgeons to plan for the adoption and/or expansion of RAS services.
Keywords: qualitative research, surgery, health services administration & management
Strengths and limitations of this study.
This qualitative research provides insights into specific areas of focus for surgeons and managers currently planning adoption or expansion of robotic-assisted surgery.
Stakeholders from several specialties were sampled, as well as surgical trainees, members of the public and health service managers.
The sample for interview comprised mostly of surgeons; the lack of variation in roles within our interview sample could be regarded as a limitation.
Introduction
There is increasing global adoption of robotic-assisted surgery (RAS) as a result of the suggested benefits for ergonomics, surgical precision, enhanced tissue visibility, reduced requirement for surgical assistance, improved training and workflow practices.1–5 Further expansion of robotic surgical systems is also forecast.4 6 7 The implementation of RAS, as a relatively new technology and having substantial differences to existing surgical healthcare delivery, can be considered ‘disruptive’ (it requires system change), and several areas of new knowledge may be required to facilitate widespread implementation.8 9 Furthermore, the introduction of fast changing technology can be susceptible to misinformation, sensationalism and early adoption bias.10 11 It is therefore critical to obtain a balanced and representative picture of current issues that could potentially affect wider implementation or roll out. This information can help with decision-making, inform evolving implementation plans and ongoing clinical pathway development, ultimately leading to better patient care.
This study was part of a wider project set up to formally explore the barriers and facilitators to the implementation/scale up of RAS services at different stages of the implementation process, focusing on both technology-specific and behavioural influences. The broad aim of this element was to uncover and report current issues of RAS and predictions about the future of robotic surgery. We refer to current issues as the topical and salient challenges and opportunities related to the introduction of RAS in the UK healthcare system, from the perspectives of key stakeholders involved in the delivery and implementation of RAS.
Methods
Study design
This was a qualitative study using semi-structured interviews and focus groups. The COnsolidated criteria for REporting Qualitative research was employed for the study report.12 This study was part of a wider project13 examining the barriers and enablers to the implementation of RAS using approaches from behavioural and implementation science. The questions within the interview topic-guide (see online supplemental file 1) were primarily developed to examine the factors that affect the implementation of RAS from a behavioural and technology-specific perspective, but also included broader questions about general perceptions of RAS. The present study reports findings from the concurrent inductive analysis of the data regarding current contextual issues surrounding RAS.
bmjopen-2022-067427supp001.pdf (85.1KB, pdf)
The present study also involved two focus groups with surgical trainees and the public, respectively. Focus group questions were designed to gauge general perspectives in terms of participants’ understanding of RAS (most notably for the public focus group), the advantages and disadvantages of RAS (relevant to both focus groups), the future of RAS and the consequences of RAS adoption on skills development (Surgical Trainees focus group).
Initial key informant/pilot interviews were conducted with individuals who had significant experience of RAS to test the suitability of our interview topic guide (in terms of comprehensibility, acceptability and relevance). The key informant interviews included a highly experienced RAS surgeon, an industry representative and a scrub nurse. Interview guides were adapted as a result of these interviews to ensure that the questions were relevant to each participant role (eg, surgeons, nurses and industry partners). The topic-guide was iteratively updated as the interviews progressed.
Participants
Semi-structured interviews
The sample was purposively selected to contain surgeons, wider theatre staff and other relevant personnel involved in the introduction and delivery of RAS services across the UK, including service managers and policymakers/commissioners. We aimed to interview stakeholders from a range of hospital sites across the UK and include a range of views (eg, proponents and opponents) and experiences of RAS (ie, variations in specialty and duration of RAS experience). A prespecified sample of 35 was included to ensure full representation of stakeholders and saturation of themes. We also judged the sufficiency of our sample size based on the principles outlined by Francis and colleagues.14 Participants were identified through clinical and research networks, such as the Royal College of Surgeons of England Robotic and Digital Research (RADAR) group, surgical research networks, industry connections and local hospital knowledge. A broad range of disciplines and representation was sought.
Focus group: surgical trainees
Early career surgical trainees from various specialties were purposefully selected to complement the interview data—which mostly represented clinical viewpoints from established surgeons at later stages of their careers or other non-surgical staff. The trainee group was accessed and invited through National Surgical Trainee Collaboratives.
Public focus group
A further focus group was held with members of the public (linked to the Health Services Research Unit) to establish their perspectives about RAS, including the outcomes they thought were important to them when evaluating RAS.
Data collection
Following piloting, the interviews were led by LL, accompanied by MC or DB to ensure that all technical aspects of issues related to RAS were covered. This was also conducted to allow clarification of issues for both interviewer and interviewee, using the expertise of the authors. All interviews were conducted via Microsoft Teams15 and audio-recorded. Data collection took place between October 2020 and March 2021. The interviews were transcribed verbatim by an external transcription company, anonymised and reviewed for accuracy (LL) by (re)checking against the audio recordings where necessary (eg, where extracts of the transcripts were highlighted as ‘inaudible’). Transcripts were subjected to the analysis process outlined below.
Data analysis
A thematic data-driven inductive approach to analysis16 was adopted to explore wider contextual perspectives on current and potential future issues of RAS. Following review/refinement of themes, a thematic framework was developed (LL, reviewed by KG, MC, DB) which described the content of all themes with illustrative quotes to facilitate data analysis. A double coder (LD) checked the themes to accurately describe the content of participants’ responses in five diverse transcripts. Any coding discrepancies identified during this process were discussed (between LL and LD) to reach consensus. Data analysis was supported through using NVivo17 and Microsoft Excel.18
Patient and public involvement
None.
Results
Demographics
Sample demographics are provided in table 1. In total, 35 stakeholders were interviewed. Twenty-two clinical stakeholders (including surgeons, wider theatre staff and service managers) across a range of clinical specialties were sampled from a total of 16 National Health Service (NHS) hospital sites located across England, Scotland and Wales. The robotic operations conducted (or assisted) by clinical stakeholders varied and included body cavity-based work (most often cancer) in colorectal, upper gastrointestinal, thoracic, head and neck, urology, gynaecology and orthopaedics. Orthopaedics is slightly different (knee, hip and spine), as it is mainly related to accuracy of cutting bone rather than the manipulation of instruments inside a body cavity.
Table 1.
Demographic data for the interviewees and focus group (trainee) participants
| Characteristic | Interviews | Trainee focus group |
| N=35 | N=7 | |
| Age | ||
| Median | 50 | 35.5 |
| Range | 30–70 | 31–37 |
| Gender | ||
| Female | 7 | 4 |
| Male | 27 | 2 |
| Ethnicity (self-identified) | ||
| Asian British | 3 | – |
| Caucasian | 29 | 5 |
| Indian | 1 | – |
| Other white background | 1 | – |
| Chinese Asian | – | 1 |
| Role | ||
| National surgical specialty leader | 5 | – |
| Surgeon (RAS user) | 11 | – |
| Surgeon (non-RAS user) | 2 | – |
| Scrub nurse | 2 | – |
| Industry representative | 5 | – |
| Policy commissioner | 5 | – |
| Surgical trainee | 2* | 7 |
| Anaesthetist | 1 | – |
| Service manager | 2 | – |
| Specialty (leaders, surgeons, trainees) | N=20 | |
| Urology | 5 | – |
| Colorectal | 8 | 1 |
| General | 2 | 1 |
| Orthopaedics | 3 | 2 |
| Gynaecology | 1 | 1 |
| Thoracic | 1 | 2 |
Age, gender and ethnicity was not recorded for one interview participant and one focus group (trainee) participant.
*Trainees in the interview sample were not in the trainee focus group.
RAS, robotic-assisted surgery.
Seven surgical trainees participated in the trainee focus group. Five trainees were sampled from five different UK hospital sites, two were from international institutions at the time of interview (but acquired previous clinical practice in the UK). Trainee specialties are summarised in table 1. All trainees had experience of assisting in at least one robotic case, and two were undertaking robotic surgical fellowships.
Eight individuals participated in the public focus group. Prior to the public focus group, participants attended an information session led by a surgeon. This session was designed to introduce RAS, provide information regarding the conduct of RAS and acted as an opportunity for the public to ask questions. None of the participants reported having had a robotic assisted procedure, although some indicated their patient experience of other types of keyhole surgery.
Findings
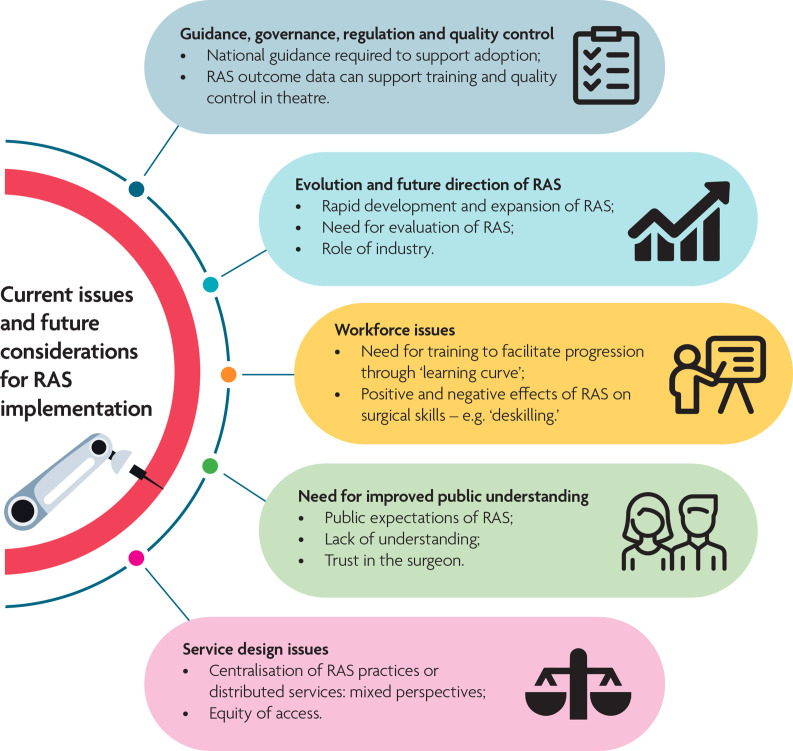
Participants raised several key issues influencing the current provision and implementation of RAS in the NHS. The issues identified related to the evolution and future direction of RAS services, as well as issues that affect service implementation including workforce training, governance and the potential for deskilling. The impact of external influences, particularly public perceptions, was also highlighted. These are discussed in more detail below and summarised in figure 1.
Figure 1.
Summary of the key themes arising from the interview and focus group data. RAS, robotic-assisted surgery.
Evolution and future direction of RAS
Rapid evolution of RAS
RAS was perceived to be evolving at a rapid pace in terms of both widespread adoption and robotic technological advancements. Some participants positively highlighted the need for healthcare systems to embrace this evolutionary process:
…As robotics are evolving, the NHS needs to be involved because the surgeons and clinicians and all NHS staff would be left behind if they weren’t involved now. Industry stakeholder, P2I26.
However, others emphasised the need for the wider system and evaluation (evidence) to catch up to allow a more joined-up roll-out going forward. Some noted that the rapid uptake of RAS meant that evaluative studies investigating the technology often lagged the adoption:
… so I think that’s where the big data, where the registries and where the collaborative multi-centre cohort studies data will be very useful….by the time you get level one data it will have moved on…, people would have learned the technology, they would have believed in it and they would have [already] moved on to the next thing. RAS Surgeon, P11S.
However, participants also acknowledged the challenges associated with conducting meaningful evaluation alongside rapid roll-out, particularly in learning curve phases but also when clinician equipoise might be evolving or where patient preference is strong:
….you will have more robotic surgeons who are experienced, trained and on the learning curve… over the learning curve they’ll find it difficult to recruit patients into the laparoscopic arm of the study. RAS Surgeon, P12S.
The need to demonstrate the benefits of RAS, particularly longitudinally and those that are not immediately visible was stressed. While this is not unique to RAS, it was acknowledged that good cost-effectiveness data would aid the greater implementation of RAS:
It’s quite important I think to actually quantify this benefit economically…. So it’s not just the length of stay in hospital, it’s also their return of function in the community and it’s the lesser or the sparing of community resources. RAS Surgeon, P11S.
Future direction of RAS
There was widespread perception that RAS is ‘here to stay’ and will be more commonplace in the future. A minority of interviewees felt RAS might be something of a fad that may go out of fashion. Overall, there was a perception that progress was strongly linked to the ongoing routine digitisation and technological advance in healthcare:
Everything has a screen on it now. Everything is digitised. We’re going down that path. Scrub Nurse, P12N
So yes, definitely evidence is a big part of that, but we all know we also need to see advances in the technology. But the advances in the technology will come as the robots become used more. Specialty Leader, P2S21
However, there were some concerns that COVID-19 might negatively influence the provision of RAS in the future, due to the financial constraints within the NHS exacerbated by the pandemic:
I do worry a little bit that constraints over the next two or 3 years are going to be quite daunting in terms of I think money [for RAS] is going to be tight and it is tight within the NHS… whether that’s with COVID-19 or I don’t know. Scrub Nurse, P12N.
Clinical participants provided insights on the dynamic nature of the RAS market, including perceptions on how RAS might evolve. Some participants indicated that surgical robots would likely become more autonomous in the future. There were also comments related to the potential of RAS to be conducted by surgeons who are located overseas/physically distant from the theatre:
So I could be in my office now doing work but one of my team could be in trouble in the operation and they could literally just log on to the computer and show me what they’re doing and I could say, “Okay, I’ll take over the controls and I’ll just fix that. Specialty Leader, P2S21.
One industry stakeholder indicated that surgeons may become more comfortable with the prospect of receiving virtual expert RAS guidance/assistance due to remote care becoming more commonplace during the COVID-19 pandemic:
…we’ve learnt a lot about how you can be more in places at once …so I think COVID-19 is helping us through that. I think a surgeon is going to be much more comfortable getting expert advice from somebody that’s nowhere even near them… Industry representative, P2I24.
However, some participants from the public focus group expressed concerns about the possibility of a more remote model of care, indicating that they would feel more comfortable in the presence of a surgeon during the entirety of a RAS procedure:
I think I’d want to be reassured that there was going to be a surgeon or any other kind of doctor there permanently throughout the entire operation in case something went south. Participant 5, public focus group.
So I’d probably what to ask what’s the plan B when things suddenly go pear shaped, I don’t want to end up in an operation theatre with all the robotic hands sticking in me and then no-one knows what to do… Participant 6, public focus group.
Many clinical participants indicated that the capital cost of RAS is expected to decrease, and some linked this to the potential introduction of new companies to the market:
I think the instruments, the prototypes, the equipment is going to evolve, it’s going to continue to change, it’s going to be more powerful, it’s going to be more intelligent, it’s going to be less expensive. Specialty Leader, P01S.
I can only see at some stage … the cost will come down further and is coming down because there’s more competition in the market. Scrub Nurse, P12N.
Role of industry
There were mixed views on the role and involvement of industry within current and future RAS service provision. Many participants indicated the positive opportunities that could arise from a collaborative relationship with industry, citing that the UK does not often embrace industry-led partnerships and perhaps should. The capability of industry to facilitate training, use better resources and form more of a collaborative approach to development was expressed by trainees:
Industry is traditionally almost a dirty word in surgery and even more with surgical academics. However, like many things I believe we are historically behind our European and US colleagues in our involvement with industry. Participant 7 Focus group Surgical Trainee.
Some participants, however, voiced a wish for greater independence about issues such as RAS training in the future and wished to have more control of the strategy:
…I think we need to…seriously think about taking control of our own training in robotics or at least having more of a role in collaborating with industry. Participant 6 Focus group Surgical Trainee.
Particular concerns regarding market dominance were also expressed:
…. The problem is a lot of robotic proponents are now employed by industry to become their proctors or key opinion leaders and that then becomes very awkward… I think right now, robotic surgery is industry driven, but I think we need to change that. And I think once we change that, you’ll see a huge upscaling. Surgical Trainee (Interviewee), P2S17.
Acknowledging that RAS was likely to be part of the NHS for some time to come, stakeholders raised a number of further points for discussion—as discussed below.
The need for guidance, governance, regulation and quality control
While RAS was acknowledged to be evolving at a rapid pace, clinical participants expressed the need for national guidance to support adoption and future expansion. Many suggested a national framework to support implementation, including training standards would be beneficial. Relatedly, many participants verbalised support for national regulatory mechanisms in place to ensure appropriate delineation of surgical responsibilities to avoid potentially problematic situations arising:
So my concern…. is the worry that if things do not go according to the plan it’s very easy to blame the technology…. We have seen that with certain technologies … and surgeons start to blame the equipment and the technique. So just there has to be some governance around the introduction and sudden…explosive expansion of that technology. RAS Surgeon, P12S.
You could imagine …if something were to go wrong in that [RAS] situation then that would cause a huge stir and would have a negative effect on ….trainees, certainly surgeons, and the public’s perception of robotic surgery. Surgical Trainee (Interviewee) P2S12.
The capability of RAS to automatically generate accurate and substantial mechanical and outcome data was seen as a strong positive and of significant benefit for training, quality assurance and accreditation purposes. The versatility of RAS and its incorporation with other technological advances (artificial intelligence (AI), machine learning, big data) further strengthened this position:
I think first of all you can train your surgical workforce better…It allows you to use new tools that is, augmented reality, mixed reality, simulation and robotics and use data for transition from one state to another and currently we don’t have. So data will also help us train our workforce differently and more effectively, that’s number one… RAS Surgeon, P15S.
However, the acceptability of standard data collection/monitoring facilitated by RAS within theatre practices still needs debate such that it would not be seen as a somewhat a ‘Big Brother’ development which could be misused:
…[some] people … wouldn’t necessarily want that…level of monitoring like you have in the black box in an aircraft is not appropriate for surgery. I think that’s an ongoing debate that needs to be addressed… it kind of introduces a Big Brother culture of what goes on in an operating theatre, a previously sacred environment, and essentially it’s eavesdropping on that. Industry representative, P03I.
Workforce issues: training to support RAS and future potential for deskilling
Workforce training needs
In addition to the need for increased governance, there was also a perceived ongoing need to adapt the capacity and the structure of NHS training for RAS to optimise readiness for further RAS expansion among the workforce. Both surgeons and trainees mentioned the imperative to be able to achieve minimal competence and overcoming the learning curve, especially while RAS surgery is not the norm within the NHS for most surgical specialties. While outside specialist training centres provide support, there was a suggestion that RAS surgery training may be in its infancy and required expansion. There was the perception that experienced surgeons are more easily accommodated in the RAS training setting currently, but that trainees should also be catered for.
But also outside of the theatre with the training modules and things you’d hope that there’s this opportunity to practice 100 times before you go near a patient. I do see this dichotomy between that promise, which has been around for a while now and what is actually available to trainees, and I think at the moment at least it’s seen as something which is for advance laparoscopic consultants. Focus Group Surgical Trainee, Participant 1.
Potential for workforce deskilling
Participants also highlighted the potential that the expansion of RAS may result in deskilling the workforce in other surgical approaches (especially open surgery) in the future—as was seen with the roll out of other minimally invasive surgery. Widespread adoption of RAS may limit exposure to, and create diminished skills of, open surgery or non-RAS endoscopic surgery among the surgical community:
There may be a loss of an open skill set and obviously trainees aren’t getting as much hands on during cases if they don’t have the basic robotic training done. Focus group Surgical Trainee, Participant 6.
However, this was countered by others who reported that performing minimally invasive procedures, in which RAS is embedded, enhanced overall surgical capability and proficiency. In such a case the emphasis is on upskilling, rather than deskilling:
…the reality is laparoscopic surgery is actually technically more challenging than open surgery. You have to have, in a way, a better understanding, or at least the same understanding, of the anatomy, and I don’t know any good laparoscopic surgeons who aren’t good open surgeons as well. RAS Surgeon, P2S11.
Service design issues: centralisation, and equity of access
Centralisation or distributed services
Some participants held strong views about the concept of centralisation: the idea that RAS should be delivered by specialist centres in specific regions of the UK. Proponents of centralisation cited that any fragmentation of RAS services could be detrimental because of the low case volumes of individual surgeons and a subsequent lack of quality control. They also argued that centralisation is a preferred model because of the team approach requirement:
…I think you need to centralise this practice [RAS], you need to invest more robotic platforms in selected hospitals. RAS Surgeon, P12S.
There was variability in the perception of suitability for centralisation for different specialties. One participant highlighted the value of centralisation in relation to RAS Urology services in the UK specifically, but expressed concerns regarding the practicalities of centralising practices for other specialties. They also highlighted the complexities associated with the fragmented development of multispecialty RAS services across the UK.
In line with the arguments for centralisation, some participants compared the organisation of services in the UK and USA, suggesting that centralisation of RAS practices can be an ideal method of maximising surgical volume with resultant positive clinical outcomes:
I would like to see the complex surgeries done in centres of excellence by teams, not by individuals, and moving through high volumes… Industry stakeholder, P2I13.
Relatedly, participants verbalised their views around the likely or ideal configuration of RAS service provision in the future. Some participants drew on their observations of surgical care during COVID-19, indicating that the lessons garnered from using mixed models of service delivery in the UK could be applied to RAS:
I think one of the things COVID has shown us that the way our model of mixing up emergency care and elective care has caused significant harm to people who didn’t have COVID sadly and that will die of other reasons that is, cancer not being treated and other things. I’d even look at models [of RAS] with elective care is separate from emergency care. Specialty Leader, P15S.
Equity of access
There were also concerns about the current set up of RAS and the need for equity of access for the population to the best interventions:
… there is a strong correlation between the poorer parts of the UK and the lack of access to any minimally invasive surgery, and then following on from that, robotic surgery… Industry representative, P03I.
This theme was also highlighted by commissioners who stressed the need to make the strategy for expanding RAS services across certain areas of the UK, equitable:
… a big problem in [one region of the UK], we have huge inequalities, and if it ends up that the middle-class get the robot and the rest get the other… down the road, well that’s not so good, is it? … Again, we don’t want to create more inequalities. Policymaker/commissioner, P2SM20.
In contrast, some also suggested that RAS can provide equitable surgery and improve patient access to minimally invasive surgery:
You could argue that if it [RAS] increases access to minimally invasive surgery, then that could fit in with that ethos of levelling things up, of providing equitable surgery that the best surgery to everyone. I think the difficulty is always going to be around the initial cost. Specialty Leader, P01S.
Need for improved public understanding
As well as perceived challenges associated with the NHS accommodating service and training issues, the interviews and focus groups highlighted the lack of public understanding of RAS and the importance of educating the public about what to expect from RAS:
…there’s a real patient expectation problem sometimes, where people felt it was going to be magical… it’s a common one… the ‘sparkle dust’ problem. People think it’s new and it’s going to have no problems. Surgeon (non-RAS user), P2S6.
So at the moment there’s a complete misunderstanding around robotics, and what it is. If you say to a patient, what’s their perception of it…not in a medical context, they think about big machines putting cars together in factories and Amazon packaging up parcels. As a result, artificial intelligence and robotics terminology has become mixed, and the perception of a robot is for surgery is actually largely around artificial intelligence. When you then talk through the fact that there’s a surgeon involved all the time, they’re connected, they’re in the operating theatre, a lot of the fears and things start to disappear. But the problem is, you have to have that conversation at an individual level at the moment. There’s not that common awareness that a robot that’s used for surgery is very different to a robot that, for instance, is used to assemble a car. Industry representative, P03I.
Participants in the public focus group indicated a need for greater information and understanding around RAS terminology, to avoid further misconceptions about what robotic (assisted) surgery actually entails, particularly to address misconceptions about issues such as the level of autonomy afforded to the surgeon and how dominated it is by independent AI technology. There was little true understanding of the ‘tool’ aspect of RAS and the primary control/replication model:
…I would be very keen to know what degree of control the doctor has, because whether you call it robotic assisted or robotic, the term “robot” is there, and if there’s a bit at the end saying “assisted” it’s not hugely relevant I think if you were quite fearful about going into surgery. So for me I would really want to know that there was (a) going to be a doctor present, …there’s no indication that if it’s robotic surgery that there will be, and also to know that it is still the doctor who’s in charge. So I think, I mean I think that point about language is a really significant one. Public focus group participant 7.
However, public focus group participants also highlighted the importance of continuing to place trust in the surgeon, regardless of the surgical method deployed. In terms of benefit, one participant perceived RAS to be more beneficial than other types of keyhole surgery.
It seems to be more or less the same thing inside the body, a tube with a tool at the end of it and I’d rely on the surgeon, I trust the surgeon and I’m sure they’re equally skilled in either manoeuvre. So I know that robotics could do more for me than keyhole, but I would be happy to leave the best choice to the surgeon. Public focus group participant 2.
Many clinical and industry stakeholders highlighted the notion that the public often perceive RAS in a disproportionately positive manner, often equating advanced technology with superior care. There were suggestions that there may be some value in educating the public to ensure appropriate expectations of RAS, especially in any roll out period. The undue influence of media was also highlighted, reinforcing the need for accurate public information to be developed and disseminated:
there was a huge media thing around it [a famous person getting robotic surgery]. Because they were treated robotically, there was a very large uptake in patients going to hospitals or going through screening, and so suddenly it went up. Industry representative, P03I.
Discussion
This study, derived from a broad sample of high engagement RAS personnel, highlighted a range of issues particularly pertinent to the current provision of RAS and to future service needs which require more urgent consideration.
The rapid evolution of RAS for an institution such as the NHS was largely welcomed but offset with the need to ensure that training capacity and patient education kept up in parallel. Such reservation was highlighted further by an expressed wish for greater evidence (effectiveness and cost effectiveness) to support more rapid adoption. It was reported that the escalating uptake of RAS meant that evaluative studies often lagged behind the adoption, an all too familiar phenomenon in healthcare delivery.11 19 20 There was a perception that much of the rapid development was somewhat fiscally driven, rather than driven by high quality evaluative evidence. This imbalance will need addressing, and likely quickly, to help commissioners make informed decisions about investment in RAS for the longer term.
There was a clear perceived need for improved guidance, governance and regulation. As articulated by some interviewees, the roll out at present is not supported by a national framework (in the UK) and, while a ‘light touch’ approach can have many positives, it was clear that a governance framework would help should anything ‘go wrong’. The safety reassurance offered at present, especially from a central governance perspective, was not seen to be effective enough.
The surgical training aspect was another area of comment, especially from the trainee group. Achieving competence and experience of RAS using RAS platforms is very different to standard surgical training. There are currently capacity issues which limit opportunities to train on RAS systems—especially as the entire workforce requires training. Also, as with other minimally invasive approaches, becoming accredited in RAS for a procedure may reduce exposure of a trainee surgeon to non-RAS experience and competence. In contrast, the ability to quantify expertise and skill was seen as a strong positive feature for RAS. Both for trainees and experienced surgeons learning a new surgical method, the ability to gauge and grade competency in a much more quantitative way was welcomed. The need to adapt training to the changing needs for surgical trainees has been identified in the recent report commissioned by the Royal college of Surgeons (England).7
There were mixed views on whether centralisation of RAS services should become the model of choice within the health service. However, there was a strong wish that the way in which RAS should be rolled out should promote equity of access to treatment. RAS systems are scarce high value commodities, and currently more difficult to access for some than standard surgery. Centralisation has been shown to be highly effective for other areas of high-end healthcare provision such as specialist major trauma care,21 but this requires further research for the field of RAS.
The role of industry figured prominently in the interviews, both positively and sometimes less so. The main conflict was around perceptions of partiality and market dominance. A collaborative relationship with an energised and interested industry partner was thought to bring many benefits (as has been seen with this research project). Training, facilitation, information sharing and research opportunities/funding were all seen as positive contributions to RAS development. The perceived influence of industry in the RAS sphere was a concern voiced by some, especially outside the private sector. However, even in the limited time since data collection for this report, significant improvements have occurred with industry bodies providing a strong and united voice through institutions such as the Association of British HealthTech Industries and support of independent research.
There is a clear need for wider education among the public. The public often perceive RAS in a potentially disproportionately positive manner, often naively equating advanced technology (RAS or otherwise) with superior care—there is an assumption that because it is new, it is automatically good. Public focus group members also found it difficult to discern the levels of autonomy involved with RAS. Some respondents assumed a lack of surgeon input, highlighting misconceptions of current RAS systems where the surgeon remains in total control of both movement and decision-making. The ‘trust’ in the surgeon is, and remains, paramount. Future positioning of RAS, in terms of autonomy and technical hierarchy, and good descriptions of these for public education, are required. Platforms which aim to inform patients and the public, such as healthtalk.org, may be useful in this regard.
Strengths and limitations
Strengths of the study included the level of engagement and representation from a significant body of RAS-related experts and personnel, including open and deep insights gained from industry and hospital managers. There were some limitations to the study. The sample for interview comprised mostly of surgeons:—the lack of variation of roles within this sample could be regarded as a limitation. There were dedicated focus groups to ensure surgical trainees and public perspectives were also represented but the surgeon’s voice was prevalent. We attempted to sample multiple specialties to counter criticisms of other qualitative studies which only focus on a single specialty.22 We also aimed to recruit multiple stakeholders.
Although we deliberately invited interviewees that were both known to be more or less positive about RAS for balance, the natural sampling resulted in a preponderance of persons who were RAS supporters. This is worthy of further comment. The identification of any potential issues and problems with RAS outlined in this study has originated from those who are, in general, users of RAS and largely supportive, and who have substantial direct insight. As such, by amplifying the elements of RAS implementation that they have deemed to work well and by addressing early the elements that they believe still require refinement will likely head off any more troublesome aspects around future development. Sharing these insights and thoughts will further this ambition and allow the best possible environment for appropriate roll out of RAS.
Conclusions
Our study demonstrated a largely positive attitude towards the introduction of RAS and an expectation of continued rapid roll out. It highlighted a range of issues which stakeholders perceive to be particularly pertinent to the provision of RAS which require greater attention. These included issues of governance, workforce training, organisation delivery and a continuing need for public education. These provide useful areas of focus for healthcare managers and surgeons currently planning the adoption or future expansion of RAS services.
Supplementary Material
Acknowledgments
We thank the participants for their time, energy and invaluable insight to assist this research. Thanks to Clare Robertson for facilitating the public focus group.
Footnotes
Twitter: @LawrieLouisa, @GilliesKatie
Contributors: MC, DB and KG conceived the study. LL, DB, MC, KG and LD undertook data collection. LL, LD and KG conducted the data analysis. LL, DB, MC, KG and LD interpreted the data. LL, DB and MC drafted the manuscript and circulated it to the authors for contribution. LL, KG, LD, JT, JM, RK, AI, MC and DB edited the drafts and approved the current manuscript for publication. MC and DB acted as guarantors of this study.
Funding: This work was supported by Intuitive Surgical (European Research Board) via an unrestricted grant.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplementary information.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and was approved by Life Sciences and Medicine Ethics Review Board (CERB) at the University of Aberdeen (CERB/2020/7/1984). Participants gave informed consent to participate in the study before taking part.
References
- 1.McLeod IK, Melder PC. Da Vinci robot-assisted excision of a vallecular cyst: a case report. Ear Nose Throat J 2005;84:170–2. 10.1177/014556130508400315 [DOI] [PubMed] [Google Scholar]
- 2.Moawad GN, Rahman S, Martino MA, et al. Robotic surgery during the COVID pandemic: why now and why for the future. J Robot Surg 2020;14:917–20. 10.1007/s11701-020-01120-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ng ATL, Tam PC. Current status of robot-assisted surgery. Hong Kong Med J 2014;20:241–50. 10.12809/hkmj134167 [DOI] [PubMed] [Google Scholar]
- 4.Matsuyama T, Kinugasa Y, Nakajima Y, et al. Robotic-Assisted surgery for rectal cancer: current state and future perspective. Ann Gastroenterol Surg 2018;2:406–12. 10.1002/ags3.12202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chan F. Robotic-Assisted surgical procedures are the future of gynaecology in Australasia. Aust N Z J Obstet Gynaecol 2018;58:371–4. 10.1111/ajo.12819 [DOI] [PubMed] [Google Scholar]
- 6.Brodie A, Vasdev N. The future of robotic surgery. Ann R Coll Surg Engl 2018;100:4–13. 10.1308/rcsann.supp2.4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Royal College of Surgeons . Future of Surgery [Internet]. Available: futureofsurgery.rcseng.ac.uk [Accessed 01 Jun 2021].
- 8.Damschroder LJ, Aron DC, Keith RE, et al. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci 2009;4:50. 10.1186/1748-5908-4-50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Arroyo NA, Gessert T, Hitchcock M, et al. What promotes surgeon practice change? A scoping review of innovation adoption in surgical practice. Ann Surg 2021;273:474–82. 10.1097/SLA.0000000000004355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rogers EM. Diffusion of innovations. New York: NY: The Free Press, 1995. [Google Scholar]
- 11.Paul S, McCulloch P, Sedrakyan A. Robotic surgery: revisiting "no innovation without evaluation". BMJ 2013;346:f1573. 10.1136/bmj.f1573 [DOI] [PubMed] [Google Scholar]
- 12.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care 2007;19:349–57. 10.1093/intqhc/mzm042 [DOI] [PubMed] [Google Scholar]
- 13.Lawrie L, Gillies K, Duncan E, et al. Barriers and enablers to the effective implementation of robotic assisted surgery. PLoS One 2022;17:e0273696. 10.1371/journal.pone.0273696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Francis JJ, Johnston M, Robertson C, et al. What is an adequate sample size? Operationalising data saturation for theory-based interview studies. Psychol Health 2010;25:1229–45. 10.1080/08870440903194015 [DOI] [PubMed] [Google Scholar]
- 15.Microsoft Corporation . Microsoft teams. Redmond, Washington: One Microsoft Way. [Google Scholar]
- 16.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77–101. 10.1191/1478088706qp063oa [DOI] [Google Scholar]
- 17.Jackson K, Bazeley P. Qualitative data analysis with NVivo. 3rd Edition. Sage Publications, 2019. [Google Scholar]
- 18.Microsoft Corporation . Microsoft Excel. Redmond, Washington. [Google Scholar]
- 19.Sedrakyan A, Collins R. Metal-on-metal failures--in science, regulation, and policy. Lancet 2012;379:1174–6. 10.1016/S0140-6736(12)60372-9 [DOI] [PubMed] [Google Scholar]
- 20.McCulloch P, Altman DG, Campbell WB, et al. No surgical innovation without evaluation: the ideal recommendations. Lancet 2009;374:1105–12. 10.1016/S0140-6736(09)61116-8 [DOI] [PubMed] [Google Scholar]
- 21.Metcalfe D, Bouamra O, Parsons NR, et al. Effect of regional trauma centralization on volume, injury severity and outcomes of injured patients admitted to trauma centres. Br J Surg 2014;101:959–64. 10.1002/bjs.9498 [DOI] [PubMed] [Google Scholar]
- 22.Randell R, Honey S, Hindmarsh J, et al. A realist process evaluation of robot-assisted surgery: integration into routine practice and impacts on communication, collaboration and decision-making. Health Services and Delivery Research 2017;5:1–140. 10.3310/hsdr05200 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2022-067427supp001.pdf (85.1KB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplementary information.