Abstract
INTRODUCTION
Stroke, as a common cerebrovascular disease, has a high mortality and disability rate. Although many studies have reported that using e-cigarettes was associated with occurrence of stroke, some studies have concluded that e-cigarettes may help smokers stop using combustible cigarettes and reduce the risk of stroke. Therefore, we aimed to validate the hypothesis that e-cigarette use might be an independent risk factor for stroke occurrence by performing a systematic review and meta-analysis of clinical epidemiology studies.
METHODS
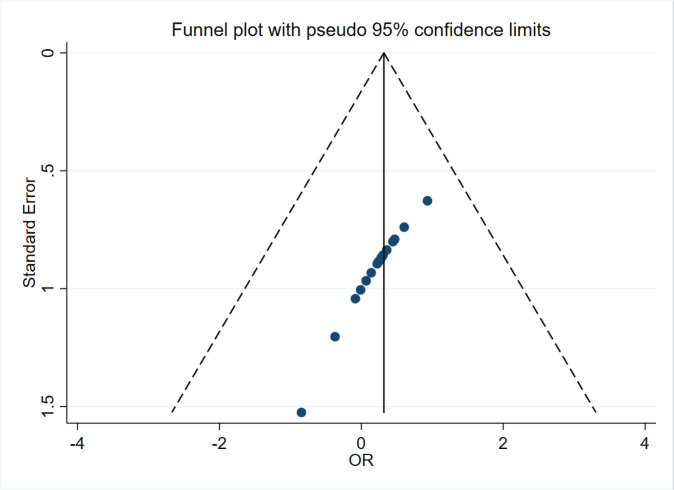
The pooled effect was calculated by the random effects model. I2 was used to test for heterogeneity. Sensitivity analysis was performed to evaluate the stability of the overall results. Funnel plot symmetry or Egger’s regression was used to evaluate publication bias. All p values were two-sided with significance level at 0.05.
RESULTS
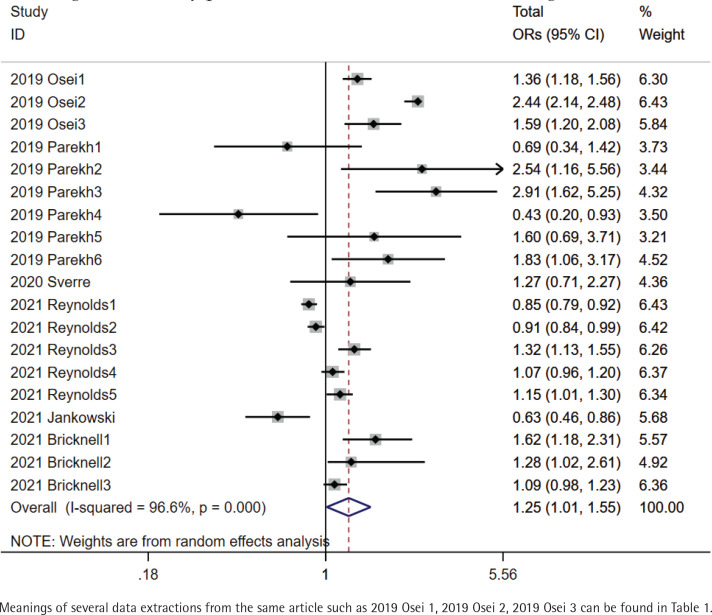
Six cross-sectional studies with high quality were finally included in the meta-analysis, which included a total of 1134896 participants. Analysis with random effects model showed that the total pooled odds ratio (OR) of stroke occurrence in e-cigarette users was 1.25 (95% CI: 1.01–1.55) (I2=96.6%, p<0.001). A stable result was revealed by sensitivity analysis. There was no publication bias. Due to high heterogeneity, we performed subgroup analysis. Compared to neither e-cigarette nor combustible cigarette users, pooled OR of stroke occurrence in e-cigarette only users was 1.13 (95% CI: 0.99–1.29) (I2=45.9%, p=0.116). Compared to combustible cigarette only users, pooled OR of stroke occurrence in both of e-cigarette and combustible cigarette users was 1.39 (95% CI: 1.19–1.64) (I2=5.6%, p=0.303). In addition, pooled OR in currently e-cigarette only users who were formerly combustible cigarette only users was 1.59 (95% CI: 1.22–2.07) (I2=0.0%, p=0.989).
CONCLUSIONS
The role of e-cigarette use in the development of stroke is inconclusive, due to the strong effect of prior tobacco use as a risk factor for stroke in the included studies.
Keywords: electronic cigarette, stroke, meta-analysis, odds ratio
INTRODUCTION
Electronic cigarettes (e-cigarettes) are an electronic product consisting of 3 major components: a rechargeable battery, a smoke producing device, and an inhalation box1. The ingredients of inhalation mainly consist of edible glycerol, edible propanediol, edible propanetriol and edible essential oils2. Compared to combustible cigarettes, e-cigarettes have no tar, nicotine, or carbon monoxide in inhalation. Therefore, the initial purpose of e-cigarettes is to help smokers or nicotine dependents quit smoking and reduce organ damage caused by smoking3. To obtain a more realistic feeling as if smoking combustible cigarettes, different proportions of nicotine are added to e-cigarettes4. In addition, a plethora of design features have led to an increase in smoking e-cigarettes among youth5. However, e-cigarette use may be related to other substances6,7. Ingredients of smoke produced by e-cigarettes may not only injure the lung but also can enter the circulatory system via gas exchange in alveoli, thus inducing cardiovascular risk8,9.
Stroke, as a common cerebrovascular disease, has a high mortality and disability rate. Although many studies have reported that using e-cigarettes was associated with occurrence of stroke, some studies have concluded that e-cigarettes may help smokers stop using combustible cigarettes and reduce the risk of stroke10,11. Therefore, we aimed to perform a systematic review and meta-analysis of clinical epidemiology studies that assessed the association between stroke and e-cigarette use.
METHODS
This systematic review and meta-analysis was performed referring to the protocol published in the database of International Platform of Registered systematic review and Meta-analysis Protocols (INPLASY, https://inplasy.com/, registration number: INPLASY202180086, DOI number: 10.37766/inplasy2021.8.0086.)
Search strategy
Literature search was performed in three public electronic databases of PubMed, Embase and Cochrane. The strategy of literature search is available in the Supplementary file.
Data extraction
Before data extraction, the quality assessment of included articles was performed via the Newcastle-Ottawa Quality Assessment Scale Cohort Studies (NOQAS-CO) for cohort studies, Newcastle-Ottawa Quality Assessment Scale Case-control Studies (NOQAS-CA) for case-control studies, and Agency for Healthcare Research and Quality (AHRQ) for cross-sectional studies. For studies with the same quality assessed by the above evaluation standards, studies with larger number of included patients were considered to have higher quality. Under the premise that e-cigarette use was an independent exposure factor, all the data used to assess risk degree of stroke occurrence were extracted, including hazard ratio (HR), risk ratio (RR) in a prospective observational study, and odds ratio (OR) in a retrospective observational study. In addition, some confounders, which might result in errors, were adjusted, including gender, age, solutions of combustible cigarette smoking and e-cigarette use, definition of endpoints, period of observation, and other factors.
Study selection
Inclusion criteria were: 1) language, region or publication year, were not restricted; 2) clinical epidemiological studies included a cross-sectional study, a case-control study, and cohort study; 3) exposed group and non-exposed group differed in e-cigarette use; 4) baseline characteristics were not statistically different between exposed group and non-exposed group; 5) endpoint of observation was stroke; 6) a complete analysis of the outcomes of cohort studies was performed. Exclusion criteria were: 1) duplication; 2) reviews, comments, letters, case reports, protocols, notes and conference papers; 3) animal experiments; and 4) contents of articles that were irrelevant to this meta-analysis.
Meta-analysis
Relative numbers and their 95% confidence intervals were used to describe count data. Meta-analysis was performed using corresponding modules in Software for Statistics and Data Science (Stata, version 15.1; College Station, Texas 77845 USA). The pooled effect with 95% CI was calculated by a random effects model. I2 was used to test for heterogeneity. Sensitivity analysis was performed to evaluate the stability of overall results by recalculating the pooled effect of the remaining studies after omitting the study with the highest quality or the random effects model was switched to fixed effects model. Funnel plot symmetry or Egger’s regression was used to evaluate publication bias. To reduce heterogeneity, we recalculated the pooled effect of the remaining studies after omitting the study with the lowest quality or perform subgroup analysis directly. All p values were two-sided with a significance level set at 0.05.
Patient and public involvement
There were no patients or applicable public involved in this review.
RESULTS
Totally, 1697 articles were retrieved from 3 databases according to the search strategy. After further screening according to the inclusion and exclusion criteria, 6 articles11-16 of cross-sectional studies were finally included (Figure 1). There were 1134896 participants in the 6 included studies (Table 1). The age range was 15–78 years. Males were close to 50%. Periods of observation were from 1 to 4 years. Different solutions of combustible cigarette smoking and e-cigarette use could be classified into 6 types: 1) neither e-cigarette nor combustible cigarette use; 2) currently e-cigarette use only but formerly combustible cigarette use only; 3) combustible cigarette use only; 4) e-cigarette use only; 5) both of e-cigarette and combustible cigarette use; and 6) solutions of combustible cigarette smoking and e-cigarette use were not separated, including 2), 4) and 5). Thus, different data were extracted from the same article. One study (2021 Reynolds) divided the type 6) solution into 3 sub-solutions: 1. Frequency of e-cigarette use > frequency of combustible cigarette smoking, 2. Frequency of e-cigarette use < frequency of combustible cigarette smoking, and 3. Frequency of e-cigarette use = frequency of combustible cigarette smoking, which produced 3 data extractions. One study (2021 Bricknell) divided the type 4) solution into 3 sub-solutions: e-cigarette use only every day, e-cigarette use only sometimes, e-cigarette use formerly.
Figure 1.
Process of literature search
Table 1.
Characters of studies included
| Articles | Male % | Age (years) | Participants n | Solutions of combustible cigarette smoking and e-cigarette use | Time of observation | Endpoints of observation |
|---|---|---|---|---|---|---|
| 2019 Osei | 48.10 | 30–34 | 449092 | 1. Combustible cigarette use only vs both of e-cigarette and combustible cigarette use | 2 | Stroke |
| 2. Neither e-cigarette nor combustible cigarette use vs both of e-cigarette and combustible cigarette use | ||||||
| 3. Currently e-cigarette use only but formerly combustible cigarette use only vs combustible cigarette use only | ||||||
| 2019 Parekh | 47.90 | 18-44 | 161529 | 1. Neither e-cigarette nor combustible cigarette use vs e-cigarette use only | 2 | Stroke |
| 2. Neither e-cigarette nor combustible cigarette use vs currently e-cigarette use only but formerly combustible cigarette use only | ||||||
| 3. Neither e-cigarette nor combustible cigarette use vs both of e-cigarette and combustible cigarette use | ||||||
| 4. Combustible cigarette use only vs e-cigarette use only | ||||||
| 5. Currently e-cigarette use only but formerly combustible cigarette use only vs combustible cigarette use only | ||||||
| 6. Combustible cigarette use only vs both of e-cigarette and combustible cigarette use | ||||||
| 2020 Sverre | 80.60 | 64-78 | 1789 | 1. Neither e-cigarette nor combustible cigarette use vs solutions of combustible cigarette smoking and e-cigarette use were not separated | 2 | Stroke or Transitory ischemic attacks |
| 2021 Reynolds | 51.50 | ≥18 | 32172 | 1. Neither e-cigarette nor combustible cigarette use vs frequency of e-cigarette use < frequency of combustible cigarette smoking | 4 | Stroke |
| 2. Neither e-cigarette nor combustible cigarette use vs frequency of e-cigarette use = frequency of combustible cigarette smoking | ||||||
| 3. Neither e-cigarette nor combustible cigarette use vs frequency of e-cigarette use < frequency of combustible cigarette smoking | ||||||
| 4. Neither e-cigarette nor combustible cigarette use vs e-cigarette use only | ||||||
| 5. Neither e-cigarette nor combustible cigarette use vs both of e-cigarette and combustible cigarette use | ||||||
| 2021 Jankowski | 47.90 | ≥15 | 1011 | 1. Neither e-cigarette nor combustible cigarette use vs solutions of combustible cigarette smoking and e-cigarette use were not separated | 1 | Stroke |
| 2021 Bricknell | 43.20 | ≥18 | 489303 | 1. Neither e-cigarette nor combustible cigarette use vs e-cigarette use only every day | 1 | Stroke |
| 2. Neither e-cigarette nor combustible cigarette use vs e-cigarette use only sometimes | ||||||
| 3. Neither e-cigarette nor combustible cigarette use vs e-cigarette use only formerly |
Because all the articles were cross-sectional studies, only AHRQ was used to assess their quality. One study (2019 Osei) was assessed as ‘Yes’ in every section, which had the highest quality (Table 2). In subjective influence section, one article (2020 Sverre) was assessed as ‘No’. Five articles were assessed as ‘No’ in the quality assurance section. In the data missed section, two articles were assessed as ‘No’. All the studies were assessed as ‘No’ in the follow-up section. Finally, one article (2020 Sverre) was assessed to have 6 ‘Yes’, which had the lowest quality. Only ORs directly appeared in articles, which were extracted by us to perform the next stage of data analysis.
Table 2.
Quality assessment of studies via Agency for Healthcare Research and Quality
| Articles | Source of data | Inclusion and Exclusion criteria | Identification time | Continuous participants | Subjective effects | Quality assurance | Causes of exclusion | Confounders | Data missed | Data integrality | Follow-up |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 2019 Osei | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No |
| 2019 Parekh | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | No |
| 2020 Sverre | Yes | Yes | Yes | Yes | No | No | Yes | Yes | No | Yes | No |
| 2021 Reynolds | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | No |
| 2021 Jankowski | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | No | Yes | No |
| 2021 Bricknell | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | No |
The total pooled OR was 1.25 (95% CI: 1.01–1.55) with heterogeneity of I2=96.6% (p<0.001) (Figure 2). In the sensitivity analysis, after omitting the study with the highest quality (2019 Osei), pooled OR was 0.99 (95% CI: 0.96–1.04) with a heterogeneity of I2=83.4% (p<0.001). There was a symmetrical distribution in the funnel plot (Figure 3). The study with the lowest quality (2020 Sverre) might have resulted in the high heterogeneity of total pooled OR; after omitting this study, the pooled OR was 1.23 (95% CI: 1.19–1.28) with a heterogeneity of I2=96.8% (p<0.001). However, heterogeneity was still high. Referring to combined combustible cigarette smoking and e-cigarette use, we performed subgroup analysis of total ORs. Compared to neither e-cigarette nor combustible cigarette users, pooled OR of stroke occurrence in current e-cigarette only users was 1.13 (95% CI: 0.99–1.29) (I2=45.9%, p=0.116). Compared to combustible cigarette only smokers, pooled OR of stroke occurrence in dual e-cigarette and combustible cigarette users was 1.39 (95% CI: 1.19–1.64) (I2=5.6%, p=0.303). In addition, pooled OR in currently e-cigarette only users who were formerly combustible cigarette only smokers was 1.59 (95% CI: 1.22–2.07) (I2=0.0%, p=0.989). Compared to neither e-cigarette nor combustible cigarette users, pooled OR of stroke occurrence in e-cigarette users who did not clearly distinguish the use of combustible cigarettes was 0.94 (95% CI: 0.79–1.13) and pooled OR in both e-cigarette and combustible cigarette users was 1.95 (95% CI: 1.06–3.61) with a heterogeneity of I2=87.1% (p<0.001) and I2=98.1% (p<0.001) (Figure 4). Compared to combustible cigarette only smokers, only one OR of stroke occurrence in e-cigarette only users was 0.43 (95% CI: 0.20–0.93). Compared to neither e-cigarette nor combustible cigarette users, pooled OR in current e-cigarette only users who were formerly combustible cigarette only smokers was 2.54 (95% CI: 1.16–5.56).
Figure 2.
Totally pooled OR of stroke occurrence in e-cigarette users
Figure 3.
Funnel plot of all the ORs extracted from articles
Figure 4.
Subgroups analysis of totally pooled OR
DISCUSSION
Our results of total pooled OR showed that the role of e-cigarettes as a risk factor for stroke is inconclusive due to the strong effect of prior tobacco use. However, publication bias and the data from the study with the lowest quality were not the source of significant heterogeneity. Finally, results in subgroup analysis support that one source of heterogeneity was the ambiguous solutions of combustible cigarette smoking and e-cigarette use. Moreover, due to the specific limitations of the cross-sectional study, we could not judge the causal and chronological ordering relationship of e-cigarette use and other risk factors of stroke occurrence such as hypertension, diabetes, auricular fibrillation, which might be other sources of heterogeneity. Compared to combustible cigarette only use, current e-cigarette only users with formerly combustible cigarette only smoking would face the risk of stroke occurrence, which might confirm that e-cigarette use as a replacement or adjunctive therapy for quitting smoking, could not reduce the risk of stroke occurrence. However, compared to neither e-cigarette nor combustible cigarette users, e-cigarette only use might not be the risk factor for stroke occurrence.
Smoke produced by e-cigarettes could injure the blood-brain barrier17,18 and lead to neuroinflammation19. In addition, e-cigarette exposure could influence cognitive functions20 and decrease brain glucose utilization in ischemic stroke20, which might lead to an unfavorable prognosis for stroke patients. We considered that blood vessel endothelia had been damaged via smoking combustible cigarettes. E-cigarette use might further deteriorate the injury of cerebrovascular endothelium in current e-cigarette users who smoked combustible cigarettes currently or formerly. Although e-cigarette only use might not be the risk factor for stroke, it might be associated with other diseases such as cancer, heart and lung diseases21,22. Therefore, the better choice for quitting smoking or nicotine might be to immediately stop using e-cigarettes and smoking combustible cigarettes, which might be a better way to reduce organ injuries.
Limitations
The major limitation of our study was that although there were sufficient data from 6 studies, the quality of the data could have been higher. Second, stroke as the definition of endpoint covers a wide range. Subtypes including transient ischemic attack, hemorrhagic stroke, and ischemic stroke could not be clearly separated. In addition, only ORs were extracted, which were of lower quality to explain causal relationships. Cohort studies that include e-cigarette users with no history of tobacco use are needed to confirm if e-cigarettes are an independent factor for stroke, an assessment which cannot be currently made.
CONCLUSIONS
The role of e-cigarette use on the development of stroke is inconclusive, due to the strong effect of prior tobacco use as a risk factor for stroke, in the included studies.
Supplementary Material
CONFLICTS OF INTEREST
The authors have each completed and submitted an ICMJE form for disclosure of potential conflicts of interest. The authors declare that they have no competing interests, financial or otherwise, related to the current work. All the authors report that since the initial planning of the work, payments were made to Mingfei Yang and the Qinghai Provincial People’s Hospital from the Project of Science and Technology Department of Qinghai Province (No. 2020-ZJ-774) and to Mingfei Yang from Mingfei Yang-2020 Kunlun Talents of Qinghai Province High-End Innovation and Entrepreneurship Talent Project-Cultivate Leading Talents.
FUNDING
This work was funded by the Project of Science and Technology Department of Qinghai Province (No. 2020-ZJ-774) and Mingfei Yang from Mingfei Yang-2020 Kunlun Talents of Qinghai Province High-End Innovation and Entrepreneurship Talent Project-Cultivate Leading Talents.
ETHICAL APPROVAL AND INFORMED CONSENT
Ethical approval and informed consent were not required for this study.
DATA AVAILABILITY
The data supporting this research are available from the authors on reasonable request.
AUTHORS’ CONTRIBUTIONS
MY conceived the idea and designed the study. KZ screened studies and extracted the data independently. KZ analyzed and interpreted the data. KZ wrote the first draft of the manuscript. MY proofread the manuscript before submission. All authors reviewed the manuscript and approved the final version.
PROVENANCE AND PEER REVIEW
Not commissioned; externally peer reviewed.
REFERENCES
- 1.Lamb N. E-cigarettes. Lancet. 2019;393(10174):876. doi: 10.1016/S0140-6736(18)33196-9. [DOI] [PubMed] [Google Scholar]
- 2.Hammond S, Phillips J. E-Cigarettes and Vaping. Workplace Health Saf. 2020;68(6):301. doi: 10.1177/2165079920914635. [DOI] [PubMed] [Google Scholar]
- 3.Cook R, Davidson P, Martin R. NIHR Dissemination Centre E-cigarettes helped more smokers quit than nicotine replacement therapy. BMJ. 2019;365:l2036. doi: 10.1136/bmj.l2036. [DOI] [PubMed] [Google Scholar]
- 4.Rom O, Pecorelli A, Valacchi G, Reznick AZ. Are E-cigarettes a safe and good alternative to cigarette smoking? Ann N Y Acad Sci. 2015;1340:65–74. doi: 10.1111/nyas.12609. [DOI] [PubMed] [Google Scholar]
- 5.Fadus MC, Smith TT, Squeglia LM. The rise of e-cigarettes, pod mod devices, and JUUL among youth: Factors influencing use, health implications, and downstream effects. Drug Alcohol Depend. 2019;201:85–93. doi: 10.1016/j.drugalcdep.2019.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Breitbarth AK, Morgan J, Jones AL. E-cigarettes-An unintended illicit drug delivery system. Drug Alcohol Depend. 2018;192:98–111. doi: 10.1016/j.drugalcdep.2018.07.031. [DOI] [PubMed] [Google Scholar]
- 7.Giroud C, de Cesare M, Berthet A, Varlet V, Concha-Lozano N, Favrat B. E-Cigarettes: A Review of New Trends in Cannabis Use. Int J Environ Res Public Health. 2015;12(8):9988–10008. doi: 10.3390/ijerph120809988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Goniewicz ML, Miller CR, Sutanto E, Li D. How effective are electronic cigarettes for reducing respiratory and cardiovascular risk in smokers? A systematic review. Harm Reduct J. 2020;17(1):91. doi: 10.1186/s12954-020-00440-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hartnett KP, Kite-Powell A, Patel MT, et al. Syndromic Surveillance for E-Cigarette, or Vaping, Product Use-Associated Lung Injury. N Engl J Med. 2020;382(8):766–772. doi: 10.1056/NEJMsr1915313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Allagbé I, Le Faou AL, Thomas D, et al. Tobacco-related cardiovascular risk in women: New issues and therapeutic perspectives. Arch Cardiovasc Dis. 2021;114(11):694–706. doi: 10.1016/j.acvd.2021.06.013. [DOI] [PubMed] [Google Scholar]
- 11.Bricknell RAT, Ducaud C, Figueroa A, et al. An association between electronic nicotine delivery systems use and a history of stroke using the 2016 behavioral risk factor surveillance system. Medicine (Baltimore) 2021;100(36):e27180. doi: 10.1097/MD.0000000000027180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Osei AD, Mirbolouk M, Orimoloye OA, et al. Association Between E-Cigarette Use and Cardiovascular Disease Among Never and Current Combustible-Cigarette Smokers. Am J Med. 2019;132(8):949–954. doi: 10.1016/j.amjmed.2019.02.016. [DOI] [PubMed] [Google Scholar]
- 13.Parekh T, Pemmasani S, Desai R. Risk of Stroke With E-Cigarette and Combustible Cigarette Use in Young Adults. Am J Prev Med. 2020;58(3):446–452. doi: 10.1016/j.amepre.2019.10.008. [DOI] [PubMed] [Google Scholar]
- 14.Sverre E, Peersen K, Perk J, et al. Challenges in coronary heart disease prevention - experiences from a long-term follow-up study in Norway. Scand Cardiovasc J. 2021;55(2):73–81. doi: 10.1080/14017431.2020.1852308. [DOI] [PubMed] [Google Scholar]
- 15.Reynolds LM, Zamora C, Lee UJ, et al. Tobacco Use Prevalence and Transitions From 2013 to 2018 Among Adults With a History of Cardiovascular Disease. J Am Heart Assoc. 2021;10(12):e021118. doi: 10.1161/JAHA.121.021118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jankowski M, Wrześniewska-Wal I, Ostrowska A, Lusawa A, Wierzba W, Pinkas J. Perception of Harmfulness of Various Tobacco Products and E-Cigarettes in Poland: A Nationwide Cross-Sectional Survey. Int J Environ Res Public Health. 2021;18(16):8793. doi: 10.3390/ijerph18168793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Heldt NA, Seliga A, Winfield M, et al. Electronic cigarette exposure disrupts blood-brain barrier integrity and promotes neuroinflammation. Brain Behav Immun. 2020;88:363–380. doi: 10.1016/j.bbi.2020.03.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Heldt NA, Reichenbach N, McGary HM, Persidsky Y. Effects of Electronic Nicotine Delivery Systems and Cigarettes on Systemic Circulation and Blood-Brain Barrier: Implications for Cognitive Decline. Am J Pathol. 2021;191(2):243–255. doi: 10.1016/j.ajpath.2020.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Prasedya ES, Ambana Y, Martyasari NWR, Aprizal Y, Nurrijawati, Sunarpi Short-term E-cigarette toxicity effects on brain cognitive memory functions and inflammatory responses in mice. Toxicol Res. 2020;36(3):267–273. doi: 10.1007/s43188-019-00031-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sifat AE, Vaidya B, Kaisar MA, Cucullo L, Abbruscato TJ. Nicotine and electronic cigarette (E-Cig) exposure decreases brain glucose utilization in ischemic stroke. J Neurochem. 2018;147(2):204–221. doi: 10.1111/jnc.14561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mravec B, Tibensky M, Horvathova L, Babal P. E-Cigarettes and Cancer Risk. Cancer Prev Res (Phila) 2020;13(2):137–144. doi: 10.1158/1940-6207.CAPR-19-0346. [DOI] [PubMed] [Google Scholar]
- 22.Cao DJ, Aldy K, Hsu S, et al. Review of Health Consequences of Electronic Cigarettes and the Outbreak of Electronic Cigarette, or Vaping, Product Use-Associated Lung Injury. J Med Toxicol. 2020;16(3):295–310. doi: 10.1007/s13181-020-00772-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data supporting this research are available from the authors on reasonable request.