Abstract
Background:
Racial/ethnic minorities are more likely than non-Hispanic whites (NHW) to be diagnosed with advanced stage hepatocellular carcinoma (HCC). We examined the role of neighborhood disadvantage as a mediator of the association between race/ethnicity and HCC stage at diagnosis.
Methods:
We used data from HCC cases diagnosed in Texas from 2007 to 2015. HCC cases were classified as local versus regional/advanced stage. A mediation model approach was used to estimate the average direct effect, average mediated (indirect) effect, total effect, and proportion mediated by the Area Deprivation Index (ADI), a composite measure of disadvantage.
Results:
7,622 had local while 6303 had regional/advanced HCC. 46.1% of cases were NHW, 15.0% non-Hispanic Black (NHB), and 38.9% Hispanic. NHBs were less likely than NHWs to be diagnosed with local stage HCC [total effect RR, 0.921; 95% confidence interval (95% CI), 0.898–0.947]; however, only 2.26% of this effect was mediated through ADI. Conversely, Hispanics were more likely than NHWs to be diagnosed with local stage HCC (total effect RR, 1.019; 95% CI, 1.001–1.037) and ADI mediated 12.56% of the effect of race/ethnicity on HCC stage. ADI was not associated with HCC stage and therefore was not a mediator of the association with HCC stage when we compared Hispanics with NHBs.
Conclusions:
Neighborhood socioeconomic disadvantage may explain/mediate some of the association between race/ethnicity and HCC stage; however, the mediating effect was not uniform across populations.
Impact:
For NHBs, other individual and neighborhood level factors, not reflected in the ADI, contribute to their lower likelihood of being diagnosed with local HCC.
Introduction
Hepatocellular carcinoma (HCC) is an increasingly important health problem in the United States. HCC incidence rates increased 3-fold between 1975 and 2014 (1), and rates continue to rise (2, 3). A highly fatal disease, HCC has nearly identical incidence and mortality rates and has the fastest increasing cancer-related mortality rate among all solid tumors in the United States (4). HCC incidence and mortality rates vary by race/ethnicity (5), with Hispanics and African Americans disproportionately affected compared with non-Hispanic whites in the United States (3). Hispanics in Texas, especially south Texas, have the highest HCC rates in the United States (6). Despite advances in diagnosis and treatment, most patients with HCC present with advanced disease and have low survival (5-year survival <20%; ref. 7). Compared with non-Hispanic whites with HCC, 5-year survival rates are significantly lower for African Americans and higher for Asian and Pacific Islanders (5).
Reasons for the greater burden of HCC in minority populations are multifactorial, including genetic susceptibility (8, 9), differences in the prevalence or severity of known risk factors for HCC [e.g., hepatitis C virus (HCV) infection, hepatitis B virus (HBV) infection, alcohol, obesity, diabetes, NAFLD, smoking; refs. 10–12], or disparities in prevention and treatment of HCC (13). In recent years, in the United States, renewed attention has been directed toward the significance of the social determinants of health (SDoH) in health disparities. The SDoH potentially have significant impact on HCC outcomes and its risk factors, and they may influence healthcare accessibility, healthcare quality, adherence to provider prescriptions, and mortality. Together, HCC, its precursor, cirrhosis and risk factors, and the continuum of care patients undergo are complex, multifaceted, and multifactorial, and they can be organized under three major domains of etiologic agents: proximal, intermediate, and distal. Proximal determinants operate at the individual level (e.g., genetic makeup, sex, race/ethnicity, or personal income), while intermediate determinants include the socioenvironmental context within which an individual experience their routine/daily activities (e.g., neighborhood social environment and neighborhood physical environment) and distal determinants include policies that affect the availability, receipt of, and quality of healthcare. Given the fact that residential neighborhood-level socioeconomic disadvantage has both direct and indirect effects on health (14–16), including cancer outcomes, the SDoH are best operationalized as intermediate determinants that are measured at the neighborhood level.
There is some evidence that SDoH are associated with risk for HCC, both overall and within racial/ethnic subgroups of the population (17, 18). To date, we are aware of few epidemiologic studies that focused on the roles of SDoH in stage of HCC at diagnosis, though other more common cancers have been examined. For breast cancer, neighborhood-level socioeconomic disadvantage, along with other measures of SDoH, plays an important role in stage at diagnosis, especially for immigrants (19). Similar findings have been observed for late-stage prostate cancer (20). As with other screening-sensitive cancers, the emphasis in case of HCC would be on the availability and use of surveillance (involving frequent imaging and measurement of serum alpha-fetoprotein among those considered high risk, predominantly cirrhosis) to detect HCC at an early stage. Therefore, disparities in making a diagnosis of risk factors (HCV, HBV, NAFLD) would lead to dipartites in identifying cirrhosis, and these would lead to less surveillance altogether or less follow up surveillance with use of definitive tests (e.g., CT, MRI, and biopsy), eventually causing disparities in HCC stage at diagnosis.
In the current analysis, we used the Area Deprivation Index (ADI), a measure of neighborhood disadvantage, to determine if neighborhood socioeconomic disadvantage mediates the relationships between race/ethnicity and the stage of HCC at diagnosis. Socioeconomic disadvantage can be used as a measure of place-based (or, neighborhood) stressors, incorporating important aspects of poverty, low educational attainment, substandard housing, and lack of employment opportunities (21, 22). The ADI is a composite area-based index that can be applied as a proxy for socioeconomic status (23). It has been associated with disease risk factors (24), healthcare utilization (25), and disparities in healthcare (26). We hypothesized that the magnitude and significance of the race/ethnicity-HCC stage relationships will change significantly depending upon the value of the neighborhood ADI measure (mediator).
Methods
Study population
Our study population and accompanying data were drawn from two major sources: The Texas Cancer Registry (TCR) and the U.S. Census Bureau (U.S. Census). The TCR provided data on individual patients that were diagnosed with first primary HCC in Texas between 2007 and 2015. We chose 2007 to 2015 dates to match the TCR individual-level data with the U.S. Census data that were used to compute ADI. We excluded 3570 subjects with missing HCC stage and 2 transsexual subjects from the analysis. Furthermore, we restricted our analyses to non-Hispanic whites, non-Hispanic Blacks and Hispanics because of low numbers of patients from other racial/ethnic subgroup (we excluded 936 patients from other racial/ethnic subgroups or who had missing race/ethnicity). This left 13,925 individuals for the primary analysis. The protocols for this study have been reviewed and approved by the Committee for the Protection of Human Subjects at the Baylor College of Medicine (IRB #: H-43274) and the Texas Cancer Registry (IRB #: 18–032).
Measures and data sources
Dependent measure: HCC stage at diagnosis
The TCR data contains individual-level data with verified HCC diagnosis. We received SEER Summary Stage for all patients with HCC and created a binary outcome variable for this mediation analysis and compared local stage patients with a combined group of regional and advanced stage patients because knowing about the determinants of local stage may be particularly valuable in terms of increasing early detection rates and by providing curative therapeutic interventions to individuals diagnosed with HCC.
Independent measure: race/ethnicity
The TCR database included separate variables characterizing the self-reported primary race and Spanish/Hispanic origin for individual participants. We used these two variables to recategorize patients as non-Hispanic white, non-Hispanic Black and Hispanic. We compared the HCC stage distributions and examined for mediation by ADI between (i) non-Hispanic whites and non-Hispanic Blacks; (ii) non-Hispanic whites and Hispanics; and (iii) non-Hispanic Blacks and Hispanics.
Potential mediator: ADI
The ADI is a composite measure of “neighborhood” socioeconomic disadvantage that is based on 17 U.S. Census indicators from the following four categories: poverty, housing, employment, and education (27, 28). To assemble the 17 U.S. Census indicators, we used the U.S. Census American Community Survey (ACS) 5-year Estimates data that were summarized to the census tract (neighborhood) level. The ACS is a nationwide survey that collects and produces information on social, economic, housing, and demographic characteristics about the U.S. population every year (29). To properly align individual-level data with neighborhood-level, we used two non-overlapping ACS versions. Therefore, data from the 2007 to 2011 ACS Estimates were assigned to individuals diagnosed with HCC between 2007 and 2011, while 2012 to 2016 ACS Estimates’ data were assigned to those diagnosed between 2012 and 2015. The research data file from the TCR included location reference data for each HCC patient; these were longitude (X) and latitude (Y) coordinate points. We used overlay analysis in ArcGIS Pro 2.2 (Esri, Redlands, CA) to assign the ADI score of any census tract to the participants whose X, Y coordinates were located inside the tract. To compute ADI scores for all the census tracts in Texas, similar to our previous efforts (28), we specifically followed the steps described in detail by Knighton and colleagues (23). First, we calculated a base score for each census tract in Texas (N = 5,265) by multiplying each census indicator with the applicable Singh coefficient for that indicator (23). The overall base score was the sum of the 17 weighted measures. The base score for each census tract was thereafter converted to a standardized score such that the eventual ADI scores for Texas census tracts ranged from −31.8 (minimum) to 128.6 (maximum). Higher ADI score indicates a more deprived census tract. See Supplementary Table S1 for related data.
Description of the mediation model
The proposed mediation model for this analysis is shown in Fig. 1. Race/ethnicity represents the predictor (X), stage of HCC at diagnosis was the outcome (Y), and ADI was the mediator (M). The effect of race/ethnicity on local stage of HCC at diagnosis was considered as the mediator-unadjusted effect or total effect (c). Comparing each racial/ethnic group, we determined the direct effect (c’) of the mediator-adjusted (i.e., ADI) race/ethnicity has on local stage of HCC. The indirect effect (ab) of race/ethnicity was captured through the combination of the effect of race/ethnicity on ADI (a) and the effect of the race/ethnicity-adjusted ADI on local stage of HCC (b). A mediation effect was considered present when the total effect (c) and indirect effect (ab) was statistically significant and the direct effect (c’) was smaller than the total effect (c). Partially or fully mediated effects were determined by direct effect significance (i.e., significance indicates a partially mediated effect). We hypothesized that the magnitude of the mediating effect depended on some moderators. Particularly, we accounted for age at HCC diagnosis and primary payer/insurance carrier at HCC diagnosis (uninsured, any Medicaid, insured, insured no specifics, and insurance status unknown) in the outcome and mediator models. Additionally, we adjusted for the clustering effect due to the data being collected from the same census tract by adding a random intercept effect in the mediator regression model. For a binary and common outcome, we fitted a log linear model for stage of HCC,
| (A) |
where Y = Stage of HCC at diagnosis, X = Race/Ethnicity, M = ADI, and C = vector of additional covariates. For a continuous mediator variable, we used a linear mixed model,
| (B) |
where A = Race/Ethnicity, M = the continuous ADI variable, C = the additional covariates, and υj ~ N(0, D) is a random intercept that reflects the residual variability for each census tract. The outcome and mediator models helped calculate the point estimates, 95% confidence intervals (CI), and the P value for the average direct effects, the average indirect effects, total effect, and average proportion mediated. For simplicity, we contrasted specific race/ethnicity categories to compare one of these group to another. The direct effects are easily interpreted as relative risk (RR). Interactions between race/ethnicity and ADI were also tested for in the models.
Figure 1.
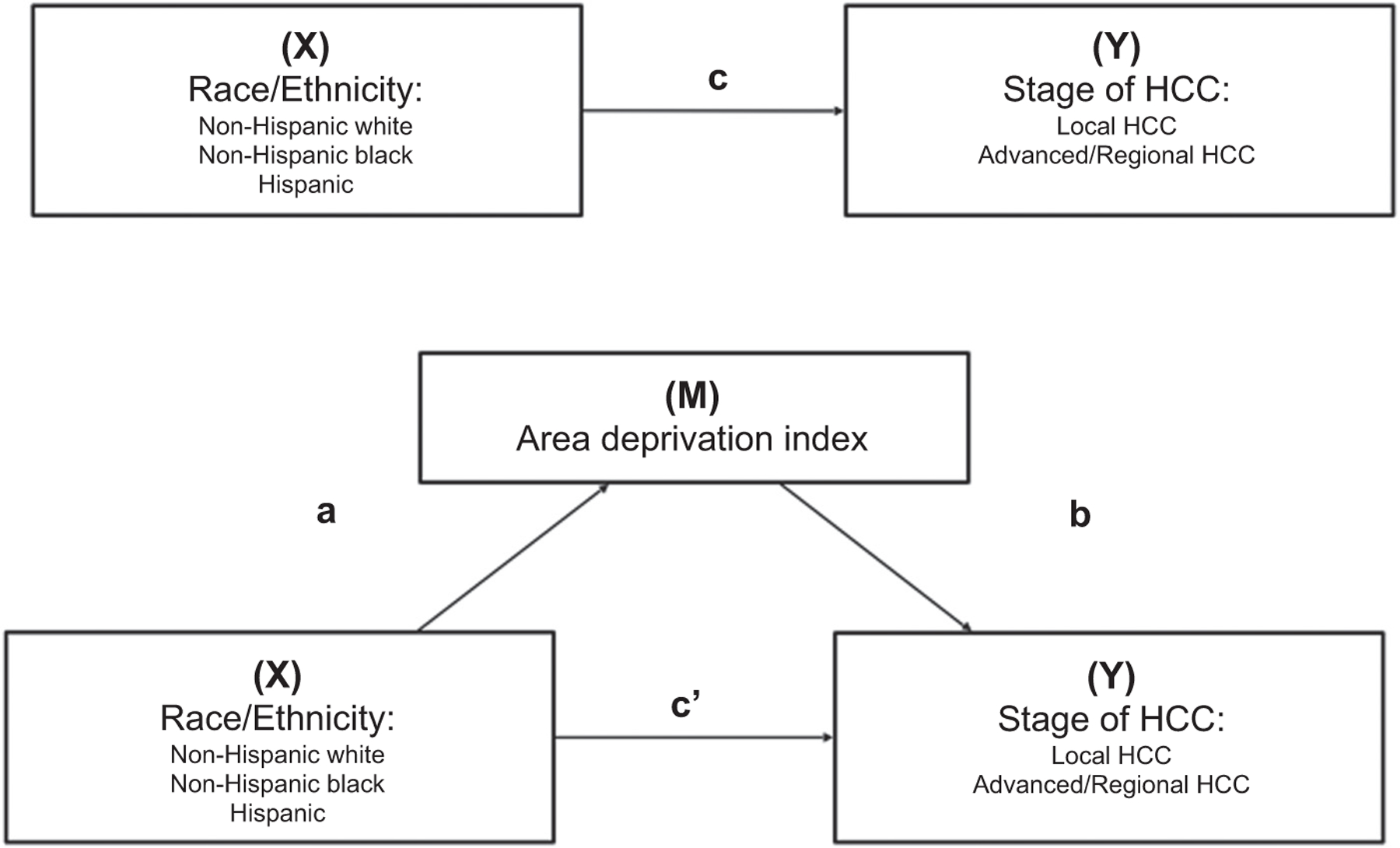
Proposed mediation model to estimate the effect of race/ethnicity on stage of HCC. The effect of race/ethnicity on stage of HCC is represented by the total effect (c). The direct effect (c′), and indirect effect (ab) are the effect of race/ethnicity has on stage of HCC and the effect of race/ethnicity on stage of HCC through ADI, respectively.
Statistical analysis
Descriptive analyses were conducted for the entire study population using a combination of statistical software’s including R 3.6.2. and SAS 9.4. χ2 tests and independent t tests were used to compare individual characteristics across stage of HCC for categorical and continuous variables, respectively. We also reported the association between (i) the outcome and predictor, (ii) the outcome and mediator; and (iii) the mediator and predictor in a series of tables. These steps help support the possible mediating effect of ADI on the relationship of race/ethnicity with local stage of HCC at diagnosis. To estimate the causal mediation effects, the mediate function was utilized in the mediation R package by a quasi-Bayesian Monte-Carlo Simulation approximation (simulations = 1,000; ref. 30). The simulation based approach (31) allowed us to consider a more complex model that accounted for (i) a multi-level predictor variable (i.e., race/ethnicity) and (ii) a mediator linear mixed model for the group-level variable, ADI. Using the models specified in equations (A) and (B), we estimated the average direct effect, average mediated (indirect) effect, total effect, and proportion mediated. Finally, we performed analyses stratified by sex (males vs. females), age group (≤65 vs. >65 years) and urbanicity (rural vs. urban) to examine for potential effect modification. All significance tests were conducted at the 0.05 α-level.
Data availability statement
The datasets used and/or analyzed during this study are available from the corresponding author on reasonable request.
Results
Table 1 presents select characteristics of the 13,925 patients with HCC included in the analyses. The average age of the participants was 62.7 years (SD = 10.8), 75.9% were male, 46.1% non-Hispanic whites, 15.0% non-Hispanic Blacks, and 38.9% Hispanics. Approximately one-quarter of patients were insured (24.3%), 50.8% had any type of Medicaid, and 14.1% were uninsured. Among all patients, the average ADI was 103.9 (SD = 17.2).
Table 1.
Characteristics of HCC cases diagnosed in Texas between 2007 and 2015, overall and by stage at diagnosis.
| Comparing local HCC with regional/advanced |
|||||||
|---|---|---|---|---|---|---|---|
| Variable | Overall (N = 13,925) | Local HCC (n = 7,622) | Regional/advanced HCC (n = 6,303) | p | |||
| Age; mean (SD) | 62.71 | (10.84) | 63.20 | (10.89) | 62.12 | (10.74) | <0.001 |
| Sex, n (%) | |||||||
| Male | 10,572 | (75.9) | 5,536 | (72.63) | 5,036 | (79.90) | <0.001 |
| Female | 3,353 | (24.1) | 2,086 | (27.37) | 1,267 | (20.10) | |
| Race/Ethnicity, n (%) | <0.001 | ||||||
| Non-Hispanic white | 6,425 | (46.1) | 3,604 | (47.28) | 2,821 | (44.76) | |
| Non-Hispanic Black | 2,082 | (15.0) | 955 | (40.19) | 1,127 | (37.36) | |
| Hispanic | 5,418 | (38.9) | 3,063 | (12.53) | 2,355 | (17.88) | |
| Primary payer/insurance carrier, n (%) | <0.001 | ||||||
| Uninsured | 1,968 | (14.1) | 854 | (11.2) | 1,114 | (17.7) | |
| Any medicaid | 7,074 | (50.8) | 4,001 | (52.5) | 3,073 | (48.8) | |
| Insured | 3,382 | (24.3) | 1,940 | (25.5) | 1,442 | (22.9) | |
| Insured, no specifics | 965 | (6.9) | 593 | (7.8) | 372 | (5.9) | |
| Insurance status unknown | 523 | (3.8) | 225 | (3.0) | 298 | (4.7) | |
| Missing | 13 | (0.1) | 9 | (0.1) | 4 | (0.1) | |
| ADI; mean (SD) | 103.92 | (17.16) | 103.5 | (17.32) | 104.43 | (16.96) | 0.002 |
| ADI Quartiles, n (%) | 0.007 | ||||||
| Quartile 1 | 2,356 | (16.92) | 1,333 | (17.49) | 1,023 | (16.23) | |
| Quartile 2 | 3,210 | (23.05) | 1,785 | (23.42) | 1,425 | (22.61) | |
| Quartile 3 | 3,713 | (26.66) | 2,053 | (26.94) | 1,660 | (26.34) | |
| Quartile 4 | 4,646 | (33.36) | 2,451 | (32.16) | 2,195 | (34.82) | |
| Variables used for ADI, mean (SD) | |||||||
| Median family income | $56,997.84 | $28494.13 | $57,681.53 | $28,695.48 | $56,171.21 | $28,228.95 | 0.002 |
| Income disparity, mean (SD) | 0.7003 | (1.407) | 0.69 | (1.52) | 0.72 | (1.25) | |
| % Families below poverty level | 17.04 | (12.39) | 16.67 | (12.34) | 17.47 | (12.44) | <0.001 |
| % Population below 150% poverty threshold | 33.01 | (17.47) | 32.44 | (17.46) | 33.7 | (17.47) | <0.001 |
| % Single parent households with dependents <18 | 39.34 | (16.47) | 38.92 | (16.25) | 39.85 | (16.72) | 0.001 |
| % Households without a motor vehicle | 7.86 | (7.65) | 7.67 | (7.52) | 8.09 | (7.81) | 0.001 |
| % Households without a telephone | 3.3 | (2.72) | 3.27 | (2.70) | 3.33 | (2.75) | |
| % Occupied housing units without complete plumbing | 0.72 | (1.29) | 0.70 | (1.27) | 0.74 | (1.31) | 0.033 |
| % Owner occupied housing units | 62.42 | (20.58) | 62.69 | (20.50) | 62.08 | (20.68) | |
| % Households with >1 person per room | 6.07 | (5.46) | 5.94 | (5.42) | 6.22 | (5.51) | 0.002 |
| Median selected monthly owner costs; Mortgage ($) | $1,271.38 | $430.10 | $1,278.66 | $432.69 | $1,262.58 | $426.82 | 0.029 |
| Median gross rent ($) | $857.05 | $283.60 | $859.43 | $290.19 | $854.17 | $275.41 | |
| Median home value ($) | $123,380.07 | $85,552.97 | $125,298.28 | $88,121.93 | $121,058.83 | $82,284.35 | 0.004 |
| % Employed person 16+ in white collar occupation | 28.39 | (14.6) | 28.96 | (14.61) | 27.69 | (14.55) | <0.001 |
| % Civilian labor force unemployed (aged 16+) | 7.92 | (4.47) | 7.76 | (4.36) | 8.1 | (4.59) | <0.001 |
| % Population 25+ y.o.; <9 yr education | 5.55 | (5.15) | 5.46 | (5.14) | 5.66 | (5.15) | 0.021 |
| % Population 25+ y.o.; at least a high school education | 76.24 | (15.35) | 76.74 | (15.32) | 75.63 | (15.36) | <0.001 |
Of all the individuals included, 7,622 (54.7%) had local HCC while 6303 (45.3%) had regional/advanced HCC (Table 1). Compared with patients with regional/advanced HCC, patients with local HCC were older (P < 0.001) and more likely female (P < 0.001) but were less likely to be uninsured (P < 0.001). Importantly, we found a statistically significant association between race/ethnicity and stage of HCC (P < 0.001; step 1 satisfied), such that, for example, non-Hispanic Blacks were more likely to have regional/advanced HCC at diagnosis than non-Hispanic whites. Patients with regional/advanced HCC at diagnosis were more likely to live in more deprived areas (i.e., areas with a higher ADI on average) than patients with local HCC (P = 0.002; step 2 satisfied; Table 1). Compared with non-Hispanic whites, non-Hispanic Blacks and Hispanics lived in an area with higher ADI (108.7, and 109.3 vs. 97.9; P < 0.001; step 3 satisfied; Table 2; Supplementary Table S2). Primary payer/insurance carrier was also associated with ADI (P < 0.001) and race/ethnicity (P < 0.001); highest average ADI was observed among uninsured patients and lowest among insured patients. However, sex was not associated with ADI. All individual Census indicators differed between patients with local versus regional/advanced HCC (Table 1).
Table 2.
Mean (SD) ADI by subpopulations for HCC cases diagnosed in Texas between 2007 and 2015.
| Variables | N | ADI | P |
|---|---|---|---|
| Sex | 0.746 | ||
| Male | 10,572 | 103.89 (17.23) | |
| Female | 3,353 | 104.00 (16.93) | |
| Race/ethnicity | <0.001 | ||
| Non-Hispanic white | 6,425 | 97.85 (19.30) | |
| Non-Hispanic black | 2,082 | 108.67 (13.07) | |
| Hispanic | 5,418 | 109.29 (12.97) | |
| Primary payer/insurance carrier | <0.001 | ||
| Uninsured | 1,968 | 106.29 (15.63) | |
| Any Medicaid | 7,074 | 104.86 (16.73) | |
| Insured | 3,382 | 100.62 (18.55) | |
| Insured, no specifics | 965 | 104.43 (16.13) | |
| Insurance status unknown | 523 | 102.65 (18.04) |
Two statistical models were constructed for the mediation analysis. Interaction terms between ADI and race/ethnicity group were not statistically significant and were dropped from the models. All estimates are adjusted by age and primary payer/insurance carrier. The mediating analysis results are presented in Table 3 by race/ethnicity and illustrated in Fig. 2. The direct, indirect, and total effects were statistically significant when comparing non-Hispanic Blacks versus non-Hispanic Whites, and Hispanics versus non-Hispanic Whites.
Table 3.
Mediation analysis of ADI on the association between race/ethnicity and local stage of HCC at diagnosis.
| Estimate | RR 95% CI | P | % Mediated | |
|---|---|---|---|---|
| Non-Hispanic Black vs. Non-Hispanic White | 2.26 | |||
| Average causal mediation effect | −0.0018 | 0.9982 (0.9963–0.9999) | 0.0400 | |
| Average direct effect | −0.0801 | 0.9230 (0.8992–0.9489) | <0.0001 | |
| Total effect | −0.0819 | 0.9214 (0.8978–0.9470) | <0.0001 | |
| Hispanic vs. Non-Hispanic White | 12.56 | |||
| Average causal mediation effect | −0.0023 | 0.9977 (0.9955–0.9999) | 0.0400 | |
| Average direct effect | 0.0208 | 1.0210 (1.0021–1.0394) | 0.0300 | |
| Total effect | 0.0184 | 1.0186 (1.0005–1.0366) | 0.0440 | |
| Non-Hispanic Black vs. Hispanic | 0.22 | |||
| Average causal mediation effect | 0.0003 | 1.0003 (0.9999–1.0007) | 0.1040 | |
| Average direct effect | −0.1014 | 0.9036 (0.8806–0.9267) | <0.0001 | |
| Total effect | −0.1011 | 0.9038 (0.8806–0.9271) | <0.0001 |
Figure 2.
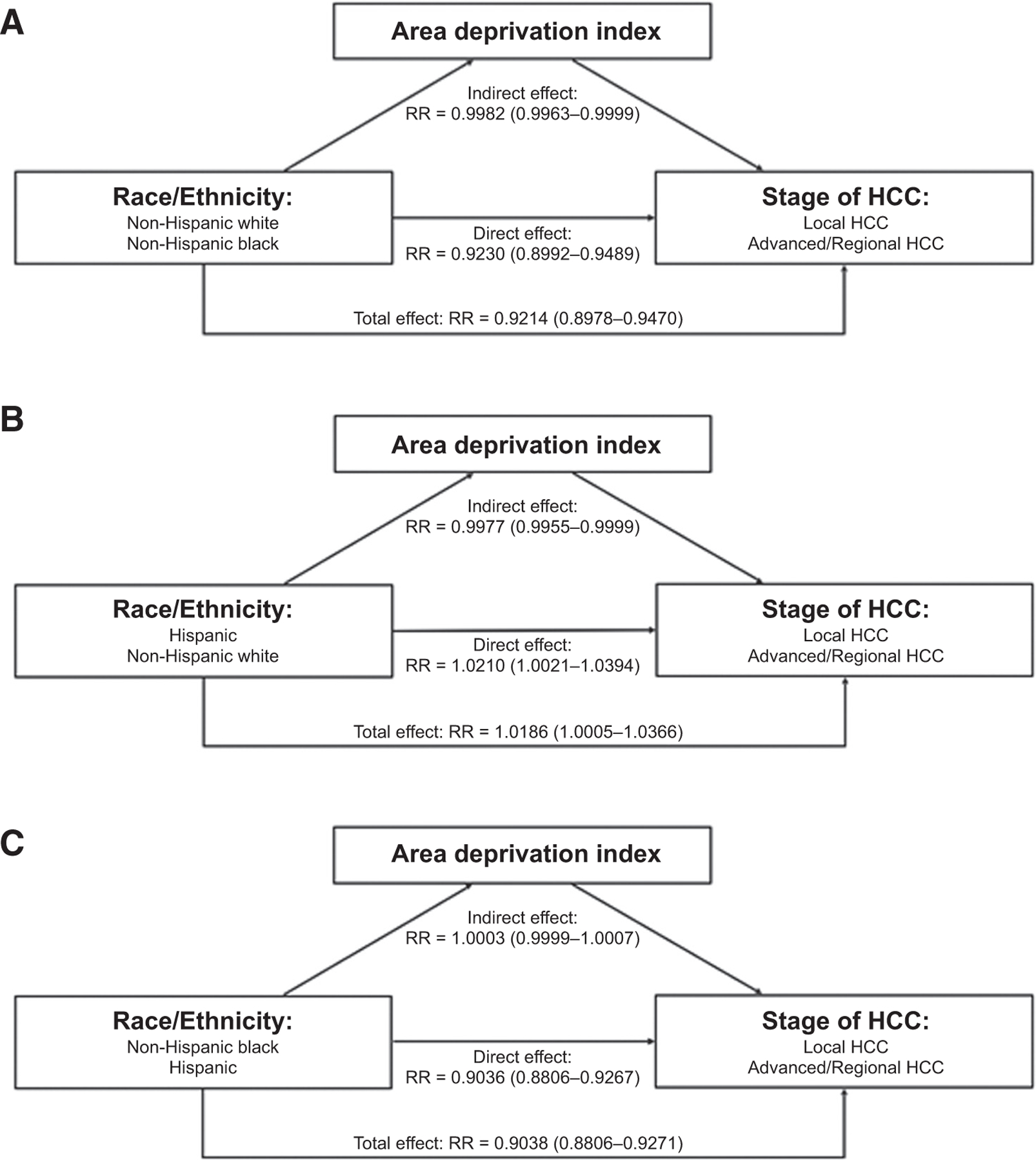
A–C, represent the results of ADI mediating on the relationship of stage of HCC and NHW/NHB, H/NHW, and NHB/H, respectively. The relative risk (RR) and 95% confidence interval are given for the direct, indirect, and total effects.
Overall, non-Hispanic Blacks were almost 10% less likely than non-Hispanic whites to be diagnosed with local stage HCC (total effect RR, 0.921; 95% CI, 0.898–0.947). Only 2.26% of this effect was mediated through ADI, leading to a direct effect RR of 0.923 (95% CI, 0.899–0.949). Conversely, ADI mediated 12.56% of the effect of race/ethnicity on HCC stage for the analysis comparing Hispanics and non-Hispanic whites. Hispanic patients were slightly more likely than non-Hispanic whites be diagnosed with local HCC (direct effect RR, 1.021; 95% CI, 1.002–1.039) after adjustment for the indirect effect of ADI. In both these analyses, higher index deprivation (i.e., ADI) was associated with lower likelihood of being diagnosed with local HCC. When contrasting non-Hispanic Blacks with Hispanics, the average mediating effect was not statistically significant (P = 0.1040), indicating that ADI was not associated with HCC stage (and there is not a mediating effect of ADI) when examined among only Hispanics and African Americans (Fig. 2C). On average, non-Hispanic Blacks were 10% (RR, 0.904; 95% CI, 0.881–0.927) less likely than Hispanics to be diagnosed with local HCC.
As shown in Supplementary Tables S3–S5, the mediating effect of ADI on associations of race/ethnicity with local HCC stage at diagnosis were consistent across subgroups defined by sex, age group, and urbanicity, respectively. In all subgroups, ADI had a greater mediating effect on the association with HCC stage when comparing Hispanics with non-Hispanic whites than when comparing non-Hispanic Blacks with non-Hispanic whites.
Discussion
The main findings from this population-based study of HCC in Texas are that (i) stage at HCC diagnosis varied by race/ethnicity, with non-Hispanic Blacks less likely than non-Hispanic whites and Hispanics to be diagnosed with local HCC; (ii) higher neighborhood-level disadvantage was associated with lower likelihood of being diagnosed with local HCC; and (iii) neighborhood-level disadvantage had a greater mediating effect on the association between race/ethnicity and HCC stage when we compared Hispanics with non-Hispanic whites (12.56%) than when we compared non-Hispanic Blacks with non-Hispanic whites (2.26%). These findings emphasize the important roles of race/ethnicity and socioeconomic disparities in HCC stage at diagnosis, but also highlights that those factors (individual and social) that explain racial/ethnic disparities in HCC stage are not uniform among minority populations.
For patients diagnosed with HCC, cure is possible in only a small proportion (<10%) of patients whose cancer is detected early and who receive a successful liver transplant or surgical resection (32). Despite a recent increase in palliative treatments for HCC, including local ablation, radiation, and systemic immunotherapy, the overall prognosis is dismal (overall 5-year survival <20%) because these treatments are non-curative and their palliative effect is short lived (33). Therefore, primary and secondary prevention, including early detection, is the only realistic way of reducing the burden of HCC mortality. However, primary prevention and early detection of HCC need to identify and target high-risk individuals for interventions to be effective and cost-efficient.
Others have established associations between residing in disadvantaged neighborhoods and a host of health outcomes (16, 34–37). Many, especially in Western Europe have used different types of geographic-based deprivation indexes as a proxy for individual’s socioeconomic condition, and applied knowledge gained to their health sector (38). The use of such indexes in the U.S. health sector is limited (39, 40) but growing (23, 41). Our study joins recent and growing research examining various aspects of the relationships between neighborhood-level demographic and socioeconomic factors and HCC outcomes in general (42, 43), and the handful doing so through spatial analytics approaches (44, 45).
While the race/ethnicity-HCC stage link is well-established, arguably, most studies have examined the association in isolation of neighborhood-level socioeconomic deprivation. However, since the 2000s, scholars have continued to emphasize the importance of a systems-oriented multilevel framework for addressing cancer health outcomes. Indeed, over the last decade, many have argued for and validated the importance of examining the impact of “place-based” socioenvironmental factors on health outcomes, including obesity and cancer (46, 47). In this regard, the places where people live, work, and play are frequently considered, though the residential neighborhood is mostly studied. Furthermore, race/ethnicity is a social construct and racism (including residential segregation) are the structural forces leading to large inequities, including those that impact cancer stage at diagnosis and cancer mortality.
In our study, we found that non-Hispanic Blacks were less likely than non-Hispanic whites to be diagnosed with local HCC; however, despite increasing ADI being associated with lower likelihood of local stage, ADI did not have a meaningful mediating effect on this association in analyses comparing non-Hispanic Blacks with non-Hispanic whites. On the other hand, and contrary to our hypotheses, we found that Hispanics were more likely than non-Hispanic whites to be diagnosed with local HCC. Nonetheless, the direction and magnitude of the indirect effect (through ADI) was the same as for the non-Hispanic Black vs. non-Hispanic white analysis, and that the mediating effect of ADI was more striking at over 12%. These findings of differential effects of ADI on race/ethnicity-HCC stage associations are similar to our findings in ongoing and published work on the ADI and several health outcomes. Here, as previously noted (48), our findings indicated that the underlying causes of disparities in health outcomes among racial/ethnic sub-populations in the United States derive from relationships among social structure, cultural norms, racial prejudices, and socioeconomic factors. For example, the limited mediating role of the ADI among non-Hispanic Blacks suggests that, potentially, certain non-socioeconomic factors may be of greater importance among non-Hispanic Blacks compared with Hispanics, at least in terms of HCC stage of diagnosis. Indeed, several authors have argued that allostatic load burden (49) among non-Hispanic Blacks, independent of socioeconomic status and health behaviors, contribute significantly to the disproportionally higher risks for negative health outcomes in non-Hispanic Blacks (50, 51). Another neighborhood-level factor not captured by the ADI but could be significant to the current topic is a measure of racial segregation. Of relevance, even when accounting for differences in socioeconomic status, one study found that that neighborhoods with highest (relative to lowest) Black racial concentration had higher relative risk of late HIV diagnosis among men and women independent of income inequality and socioeconomic deprivation (52). Overall, knowledge about the significant factors along the pathway between race/ethnicity and HCC diagnosis is useful for planning effective interventions for more local HCC diagnoses. However, additional studies with measures of, for example, racial segregation, social structure, norms, and prejudices are needed for interventions to be impactful.
Strengths of this analysis include the large sample size and that it is a population-based assessment of racial/ethnic disparities in HCC in Texas, one of the most racially, ethnically, and geographically diverse states in the United States. We used population-based registry data for case identification and obtained information about a patient’s cancer diagnosis, residency at diagnosis, insurance status, and other demographic characteristics that limited potential for selection and recall biases. In addition, to our knowledge, this is the only available study to date, investigating the mediating effect of neighborhood-level socioeconomic disadvantage (ADI) on the long-established relationship between race/ethnicity and HCC stage at diagnosis. However, our study has some limitations. We limited our analyses to non-Hispanic whites, non-Hispanic Blacks, and Hispanics due to smaller numbers of cases among other racial/ethnic subgroup of the population. The cancer registry design meant that we had limited individual level patient data, including other factors that may predispose to the development of HCC and impact access to care and stage of HCC diagnosis. As such, we were not able to investigate the effects of these potential confounders on our analyses.
In conclusion, this large registry-based study provides evidence that race/ethnicity is associated with HCC stage at diagnosis. We showed that neighborhood socioeconomic disadvantage may explain/mediate some of this association; however, the mediating effect is not uniform across minority populations. For non-Hispanic Blacks, other individual and neighborhood level factors, not reflected in the ADI, contribute to their lower likelihood of being diagnosed with local HCC compared to non-Hispanic whites and Hispanics. Further research is needed among the non-Hispanic Black population, who have disproportionately high rates of HCC, to identify HCC cases earlier and reduce HCC mortality.
Supplementary Material
Acknowledgments
This research was supported in part by grants from the Cancer Prevention & Research Institute of Texas (CPRIT) to H.B. El-Serag (CAP-CAC RP190641) and A.P. Thrift (RP200537).
Footnotes
Supplementary data for this article are available at Cancer Epidemiology, Biomarkers & Prevention Online (http://cebp.aacrjournals.org/).
Authors’ Disclosures
No disclosures were reported.
References
- 1.Altekruse SF, Henley JS, Cucinelli JE, Mcglynn KA. Changing hepatocellular carcinoma incidence and liver cancer mortality rates in the United States. Am J Gastroenterol 2014;109:542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rahib L, Smith BD, Aizenberg R, Rosenzweig AB, Fleshman JM, Matrisian LM. Projecting cancer incidence and deaths to 2030: the unexpected burden of thyroid, liver, and pancreas cancers in the United States. Cancer Res 2014;74: 2913–21. [DOI] [PubMed] [Google Scholar]
- 3.White DL, Thrift AP, Kanwal F, Davila J, El-Serag HB. Incidence of hepatocellular carcinoma in all 50 United States, from 2000 through 2012. Gastroenterology 2017;152:812–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ryerson AB, Eheman CR, Altekruse SF, Ward JW, Jemal A, Sherman RL, et al. Annual Report to the Nation on the Status of Cancer, 1975–2012, featuring the increasing incidence of liver cancer. Cancer 2016;122:1312–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Islami F, Miller KD, Siegel RL, Fedewa SA, Ward EM, Jemal A. Disparities in liver cancer occurrence in the United States by race/ethnicity and state. CA Cancer J Clin 2017;67:273–89. [DOI] [PubMed] [Google Scholar]
- 6.El-Serag HB, Sardell R, Thrift AP, Kanwal F, Miller P. Texas has the highest hepatocellular carcinoma incidence rates in the USA. Dig Dis Sci 2021;66:912–6. [DOI] [PubMed] [Google Scholar]
- 7.Khalaf N, Ying J, Mittal S, Temple S, Kanwal F, Davila J, et al. Natural history of untreated hepatocellular carcinoma in a US cohort and the role of cancer surveillance. Clin Gastroenterol Hepatol 2017;15:273–81. [DOI] [PubMed] [Google Scholar]
- 8.Ge D, Fellay J, Thompson AJ, Simon JS, Shianna KV, Urban TJ, et al. Genetic variation in IL28B predicts hepatitis C treatment-induced viral clearance. Nature 2009;461:399–401. [DOI] [PubMed] [Google Scholar]
- 9.Tian C, Stokowski RP, Kershenobich D, Ballinger DG, Hinds DA. Variant in PNPLA3 is associated with alcoholic liver disease. Nat Genet 2010;42:21. [DOI] [PubMed] [Google Scholar]
- 10.Caetano R, Ramisetty-Mikler S, Rodriguez LA. The Hispanic Americans Baseline Alcohol Survey (HABLAS): the association between birthplace, acculturation and alcohol abuse and dependence across Hispanic national groups. Drug Alcohol Depend 2009;99:215–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee DJ, Markides KS, Ray LA. Epidemiology of self-reported past heavy drinking in Hispanic adults. Ethn Health 1997;2:77–88. [DOI] [PubMed] [Google Scholar]
- 12.Mandayam S, Jamal MM, Morgan TR. Epidemiology of alcoholic liver disease Paper presented at: Seminars in liver disease 2004. [DOI] [PubMed] [Google Scholar]
- 13.Singal AG, Li X, Tiro J, Kandunoori P, Adams-Huet B, Nehra MS, et al. Racial, social, and clinical determinants of hepatocellular carcinoma surveillance. Am J Med 2015;128:90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Adler NE, Rehkopf DH. US disparities in health: descriptions, causes, and mechanisms. Annu Rev Public Health 2008;29:235–52. [DOI] [PubMed] [Google Scholar]
- 15.Macintyre S, Ellaway A. Neighborhoods and health: an overview. Neighborhoods and Health 2003:20–42. [Google Scholar]
- 16.Robert SA. Socioeconomic position and health: the independent contribution of community socioeconomic context. Ann Rev Sociol 1999;25:489–516. [Google Scholar]
- 17.Kamath GR, Taioli E, Egorova NN, Llovet JM, Perumalswami PV, Weiss JJ, et al. Liver cancer disparities in New York city: a neighborhood view of risk and harm reduction factors. Front Oncol 2018;8:220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chang ET, Yang J, Alfaro-Velcamp T, So SKS, Glaser SL, Gomez SL. Disparities in liver cancer incidence by nativity, acculturation, and socioeconomic status in California Hispanics and Asians. Cancer Epidemiol Biomarkers Prev 2010;19: 3106–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Coughlin SS. Social determinants of breast cancer risk, stage, and survival. Breast Cancer Res Treat 2019;177:537–48. [DOI] [PubMed] [Google Scholar]
- 20.Clegg LX, Reichman ME, Miller BA, Hankey BF, Singh GK, Lin YD, et al. Impact of socioeconomic status on cancer incidence and stage at diagnosis: selected findings from the surveillance, epidemiology, and end results: National Longitudinal Mortality Study. Cancer Causes Control 2009;20:417–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shavers VL. Measurement of socioeconomic status in health disparities research. J Natl Med Assoc 2007;99:1013. [PMC free article] [PubMed] [Google Scholar]
- 22.Cederberg M, Hartsmar N, Lingärde S. Thematic report: Socioeconomic disadvantage. Report from the EPASI (Educational Policies that Address Social Inequality) project supported by the European Commission’s Department of Education & Culture, SOCRATES programme 2009;2. [Google Scholar]
- 23.Knighton AJ, Savitz L, Belnap T, Stephenson B, Vanderslice J. Introduction of an area deprivation index measuring patient socioeconomic status in an integrated health system: implications for population health. EGEMS 2016;4:1238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wardle J, Jarvis MJ, Steggles N, Sutton S, Williamson S, Farrimond H, et al. Socioeconomic disparities in cancer-risk behaviors in adolescence: baseline results from the Health and Behaviour in Teenagers Study (HABITS). Prev Med 2003;36:721–30. [DOI] [PubMed] [Google Scholar]
- 25.Phillips RL, Liaw W, Crampton P, Exeter DJ, Bazemore A, Vickery KD, et al. How other countries use deprivation indices—and why the United States desperately needs one. Health Aff 2016;35:1991–8. [DOI] [PubMed] [Google Scholar]
- 26.Singh GK, Jemal A. Socioeconomic and racial/ethnic disparities in cancer mortality, incidence, and survival in the United States, 1950–2014: over six decades of changing patterns and widening inequalities. J Environ Public Health 2017;2017:2819372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Singh GK. Area deprivation and widening inequalities in US mortality, 1969–1998. Am J Public Health 2003;93:1137–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Oluyomi A, Aldrich KD, Foster KL, Badr H, Kamdar KY, Scheurer ME, et al. Neighborhood deprivation index is associated with weight status among long-term survivors of childhood acute lymphoblastic leukemia. J Cancer Surviv 2021; 15:767–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Census. American Community Survey Information Guide; 2017. Available from: https://www.census.gov/content/dam/Census/programs-surveys/acs/about/ACS_Information_Guide.pdf.
- 30.Tingley D, Yamamoto T, Hirose K, Keele L, Imai K. mediation: R Package for causal mediation analysis. J Stat Softw 2014;59:1–38.26917999 [Google Scholar]
- 31.Imai K, Keele L, Tingley D. A general approach to causal mediation analysis. Psychol Methods 2010;15:309–34. [DOI] [PubMed] [Google Scholar]
- 32.Zhang X, El-Serag HB, Thrift AP. Predictors of five-year survival among patients with hepatocellular carcinoma in the United States: an analysis of SEER-Medicare. Cancer Causes Control 2021;32:317–25. [DOI] [PubMed] [Google Scholar]
- 33.Kulik L, El-Serag HB. Epidemiology and management of hepatocellular carcinoma. Gastroenterology 2019;156:477–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.House JS, Lepkowski JM, Kinney AM, Mero RP, Kessler RC, Herzog AR. The social stratification of aging and health. J Health Soc Behav 1994;35:213–34. [PubMed] [Google Scholar]
- 35.Berenson J, Shih A. Higher readmissions at safety-net hospitals and potential policy solutions. Issue Brief 2012;34:1–16. [PubMed] [Google Scholar]
- 36.Rau J Hospital treating the poor hardest hit by readmissions penalties Kaiser Health News; 2012. [Google Scholar]
- 37.Lantz PM, House JS, Lepkowski JM, Williams DR, Mero RP, Chen J. Socioeconomic factors, health behaviors, and mortality: results from a nationally representative prospective study of US adults. JAMA 1998;279:1703–8. [DOI] [PubMed] [Google Scholar]
- 38.Townsend P, Phillimore P, Beattie A. Health and deprivation: inequality and the North Routledge; 1988. [Google Scholar]
- 39.Butler DC, Petterson S, Phillips RL, Bazemore AW. Measures of social deprivation that predict health care access and need within a rational area of primary care service delivery. Health Serv Res 2013;48:539–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hofer TP, Wolfe RA, Tedeschi PJ, McMahon LF, Griffith JR. Use of community versus individual socioeconomic data in predicting variation in hospital use. Health Serv Res 1998;33:243. [PMC free article] [PubMed] [Google Scholar]
- 41.Nkoy FL, Stone BL, Knighton AJ, Fassl BA, Johnson JM, Maloney CG, et al. Neighborhood deprivation and childhood asthma outcomes, accounting for insurance coverage. Hosp Pediatr 2018;8:59–67. [DOI] [PubMed] [Google Scholar]
- 42.Danos D, Leonardi C, Gilliland A, Shankar S, Srivastava RK, Simonsen N, et al. Increased risk of hepatocellular carcinoma associated with neighborhood concentrated disadvantage. Front Oncol 2018;8:375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Shebl FM, Capo-Ramos DE, Graubard BI, Mcglynn KA, Altekruse SF. Socioeconomic status and hepatocellular carcinoma in the United States. Cancer Epidemiol Biomarkers Prev 2012;21:1330–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Major JM, Sargent JD, Graubard BI, Carlos HA, Hollenbeck AR, Altekruse SF, et al. Local geographic variation in chronic liver disease and hepatocellular carcinoma: contributions of socioeconomic deprivation, alcohol retail outlets, and lifestyle. Ann Epidemiol 2014;24:104–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ford MM, Ivanina E, Desai P, Highfield L, Qiao B, Schymura MJ, et al. Geographic epidemiology of hepatocellular carcinoma, viral hepatitis, and socioeconomic position in New York City. Cancer Causes Control 2017;28: 779–89. [DOI] [PubMed] [Google Scholar]
- 46.Cummins S, Curtis S, Diez-Roux AV, Macintyre S. Understanding and representing ‘place’ in health research: a relational approach. Soc Sci Med 2007;65: 1825–38. [DOI] [PubMed] [Google Scholar]
- 47.Janssen I, Boyce WF, Simpson K, Pickett W. Influence of individual-and area-level measures of socioeconomic status on obesity, unhealthy eating, and physical inactivity in Canadian adolescents. Am J Clin Nutr 2006;83: 139–45. [DOI] [PubMed] [Google Scholar]
- 48.Oluyomi AO, Gunter SM, Leining LM, Murray KO, Amos C. COVID-19 community incidence and associated neighborhood-level characteristics in Houston, Texas, USA. Int J Environ Res Public Health 2021;18:1495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Geronimus AT. The weathering hypothesis and the health of African-American women and infants: evidence and speculations. Ethn Dis 1992;2:207–21. [PubMed] [Google Scholar]
- 50.Tomfohr LM, Pung MA, Dimsdale JE. Mediators of the relationship between race and allostatic load in African and White Americans. Health Psychol 2016;35:322. [DOI] [PubMed] [Google Scholar]
- 51.Duru OK, Harawa NT, Kermah D, Norris KC. Allostatic load burden and racial disparities in mortality. J Natl Med Assoc 2012;104:89–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ransome Y, Kawachi I, Braunstein S, Nash D. Structural inequalities drive late HIV diagnosis: the role of black racial concentration, income inequality, socioeconomic deprivation, and HIV testing. Health Place 2016;42:148–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analyzed during this study are available from the corresponding author on reasonable request.


