Highlights
-
•
We assessed perceived changes in diet, exercise, and sleep during the pandemic.
-
•
Most participants (84%) experienced at least one unfavorable behavior change.
-
•
Women and Hispanics were disproportionately affected.
-
•
Policies needed to mitigate the effects on women and vulnerable ethnic minorities.
Keywords: Pandemic, Diet, Physical activity, Sleep, Lifestyle factors, Health disparities, Behavioral risk factors
Abstract
The COVID-19 pandemic has been disruptive, unevenly impacting health behaviors in different geographical regions and population groups. We examined how COVID-19 affected perceived changes in physical activity, sleep, and diet and the impact of socio-demographic variables on a calculated health risk behavior score. In this cross-sectional study, 505 residents of northern California completed a web-based survey from August to November of 2020. Chi-square and multivariable linear regression analyses examined the association between socio-demographic variables and the health risk behavior score. Approximately 84 % of respondents experienced at least one unfavorable behavior change after the pandemic, with 49.5 % indicating a reduction in physical activity, 29.7 % a decrease in sleep, 33.1 % an increase in sugary snack consumption, and 29.3 % a decrease in fruit and vegetable intake. Multivariate analyses indicated a higher health risk behavior score (less favorable) for females compared to males (male beta = -0.815, p < 0.0001) and Hispanics compared to Whites (Hispanics beta = 0.396, p = 0.033). The negative changes in health behavior observed in females could be attributed to a higher reduction in fruit and vegetable consumption, and a larger increase in sugary and salty snacks when compared to males. A higher reduction in exercise, sleep, and fruit and vegetable intake were the main drivers of the unfavorable results seen for Hispanics when compared to Whites. Findings highlight the detrimental behavioral changes during the COVID-19 pandemic and the disproportionate impact on Hispanics and women. These results are valuable to policymakers to identify ways to support those most affected by the pandemic and its potential long-term effects.
1. Introduction
The global coronavirus disease 2019 (COVID-19) pandemic declared as such by the World Health Organization in March 2020 continues to drastically impact socio-economic stability and healthcare systems around the globe. In the U.S., people of color, including Blacks, Hispanics, Native Americans, those with lower educational attainment, and younger workers have been disproportionately affected, widening the health disparities that were already present pre-pandemic (Falk et al., 2021, Lopez et al., 2021). Health outcomes are determined by a wide array of factors, including policymaking, social factors, health services, and biology and genetics. In addition, individual behaviors, including diet quality, physical activity, alcohol use, and sleep, have a significant impact on health outcomes and are themselves affected by socio-economic variables (Office of Disease Prevention and Health Promotion, 2021, Singu et al., 2020). According to national surveillance data, adherence to recommendations for physical activity, nutrition, and sleep are suboptimal (Chen and Sturm, 2021, Du et al., 2019, Sheehan et al., 2019) and disruptions caused by the pandemic have likely shifted many health-related behaviors.
California issued the first statewide stay-at-home order in the United States due to the COVID-19 outbreak, on March 19, 2020 (State of California, 2020). While these measures have shown to be effective in limiting the spread of the virus (Fowler et al., 2021), it severely disrupted economic and daily activities for residents such as transportation services, access to indoor exercising facilities and State parks, restaurants, schools, social gatherings, etc. Unemployment in the state reached its historic maximum of 16 % in April 2020, and has remained higher than average for months to follow (U.S. Bureau of Labor Statistics, 2021), with potential effects on food access, housing, physical and mental health, and health risk behaviors. Local policies imposed by the pandemic led to more time spent at home, which may have translated into negative changes, such as emotional eating, or positive changes, such as preparing more meals at home. Thus, emerging studies assessing the impact of the COVID-19 pandemic on health behaviors and outcomes have shown varying results and warrant additional exploration.
A growing body of research on the effects of the pandemic suggests that home confinement and social distancing policies led to increased sedentary behaviors (Ammar et al., 2020, Meyer et al., 2020). Overall, there was a decrease in physical activity levels, especially among adults who were active prior to the pandemic (Ammar et al., 2020, Meyer et al., 2020, Smith et al., 2020), while improvements in exercise habits were reported among previously inactive participants (Cancello et al., 2020). For diet related changes, results are less consistent. For example, findings from international surveys suggested that the meal patterns and types of foods chosen after the pandemic were unhealthier (Ammar et al., 2020, Ingram et al., 2020, Marty et al., 2021, Robinson et al., 2020). In the U.S., a 14 % increase in added sugar intake was observed (Cummings et al., 2021). However, 34 % of respondents reported a self-perceived improvement in diet quality in Italy and 85 % in India (Cancello et al., 2020, Madan et al., 2021). Findings on alcohol consumption and sleep were also mixed: according to a national survey of U.S. adults, there was a 14 % increase in alcohol consumption early in the pandemic compared to the previous year (Pollard et al., 2020), while a decline in alcohol consumption was observed in many countries in Europe, except for Ireland and the UK over this same period (Kilian et al., 2021). In some studies, an increase in sleep duration was observed (Giuntella et al., 2021, Sparks et al., 2021), while worsening sleep quality was noted in others (Cancello et al., 2020, Ingram et al., 2020, Ismail et al., 2020, Robillard et al., 2021). Poor sleep quality was often associated with depression, anxiety, and negative mood (Ingram et al., 2020, Kocevska et al., 2020, Robillard et al., 2021). However, changes in health behaviors as a result of the pandemic have also differed within the same region when comparing different age groups, gender, race/ethnicities, and income (Chen et al., 2021, Gallè et al., 2020, Gallè et al., 2021, Lamarche et al., 2021, Zhang et al., 2021).
COVID-19 and its repercussions are disproportionately affecting lower-income communities, racial and ethnic minorities, and individuals with comorbidities (Kim et al., 2020). These groups can face additional challenges to develop or maintain positive health behaviors which may explain some of the contradicting results on the impact of the pandemic. Furthermore, region-specific restrictions implemented during the pandemic may have varying effects on health behaviors. In California stricter orders were imposed compared to other states in the U.S., requiring further investigation. Northern California is one of the most diverse populations in the U.S. and the housing costs are among the highest in the nation. Considering the limited studies and conflicting results on the topic, a deeper understanding of the effects of the COVID-19 pandemic on health behaviors is needed, especially for marginalized groups. Therefore, the purpose of this cross-sectional study was to assess how the COVID-19 outbreak affected perceived health behavior changes, specifically exercise, sleep habits, alcohol consumption, and diet quality, among residents of a metropolitan area in northern California. A secondary objective was to identify social and demographic variables associated with adverse behavior changes, as calculated by a health risk behavior score, to inform policies and programs aiming to reduce health disparities.
2. Materials and methods
2.1. Study design and participants
In this cross-sectional study, a convenience sample of San Francisco Bay Area residents were recruited through Social Media posts (Facebook, Instagram, Linkedin, Craigslist, Nextdoor, Twitter, and Yelp Talk) and emails to various community groups asking them to complete a self-administered online questionnaire using Qualtrics. The survey was also advertised on Facebook and on El Tecolote, a free bilingual publication based in San Francisco. Recruitment and survey completion occurred from August 1st until November 30th 2020. There were three inclusion criteria: (1) being 18 years of age or older; (2) being a San Francisco Bay Area Resident; (3) living in the United States since at least January 1st, 2020. The area defined included ten counties: Alameda, Contra Costa, Marin, Napa, San Francisco, San Mateo, Santa Clara, Santa Cruz, Solano, and Sonoma, this represents an adult population of about 6.4 million people. A total of 1457 participants started the survey, of which 505 provided complete information for all the health-behavior related variables and were included in the current study. According to sample size calculations for the adult population, a sample of 384 participants or greater would provide 95 % confidence interval and 5 % margin error.
2.2. Data collection
The questionnaire included Niles et al. 2020 survey version 2.1 (Niles et al. 2020) about the impact of COVID-19 on food access challenges and related concerns, demographics, and 17 additional questions related to health behaviors (physical activity, diet, and sleep) and presence of chronic diseases. The survey was offered in both English and Spanish. The median completion time was 26.1 min (interquartile range, 20.4–39.0). Participants were given a choice to be entered in a raffle to receive a $20 Amazon gift card. The first page of the online questionnaire provided information about the study and informed consent. The study was approved by the San Jose State University Institutional Review Board (IRB Protocol Tracking Number: 20162).
2.3. Measures
Participants were asked to indicate how their health behaviors changed compared to before the COVID-19 outbreak (more, less, or about the same). Unfavorable changes of modifiable risk factors during COVID-19 were consolidated into a health risk behavior score for a total of 7 possible points with a higher score representing more unfavorable changes in health behaviors. The following responses for the dependent variable increase the score by one unit: 1) decreased physical activity and 2) decreased sleep, 3) decreased fruits and vegetable intake, 4) increased red and processed meat intake, 5) increased sugary snacks intake, 6) increased salty snacks intake, 7) increased alcoholic beverage intake.
Independent variables included 1) gender, 2) age, 3) income, 4) education, 5) race/ethnicity, 6) height (feet and inches) and weight (pounds), which were used to calculate body mass index and categorize participants as normal weight (18.5 to <25.0 kg/m2), overweight (25.0 to <30.0 kg/m2), or obese (30.0 kg/m2 or higher), and 7) presence of chronic conditions. These variables were included as they were hypothesized to influence health behaviors. The chronic conditions selected were those the CDC listed on July 2020 as ones that could increase one’s risk of severe COVID-19 illness and included asthma, cancer, chronic obstructive pulmonary disease, chronic kidney disease, chronic liver disease, high blood pressure, neurologic conditions, other chronic lung diseases, serious heart condition, type I diabetes, type II diabetes and other diseases that might compromise the immune system.
2.4. Statistical analysis
Descriptive statistics were calculated for all independent and dependent variables and are presented as means (standard deviations) or frequency counts and percentages. To evaluate the impact of the independent variables on changes in health behaviors post-COVID-19, a health behavior score was calculated where each adverse behavior contributed one point, resulting in a maximum possible score of 7. Bivariate analyses were performed to evaluate the impact of individual independent variables on the health risk behavior score. Variables that were significant in the bivariate analysis at a p-value of <0.2 were included in the final model. This p-value was selected so as not to miss important variables in the final model. Chi-squared tests were performed to determine if differences were statistically significant. The association between independent variables and the health risk behavior score was modeled using multivariable linear regression analyses. Reported heights above 7 feet and below 4 feet were excluded from the analysis (n = 4). Those with a calculated BMI below 10 and 70 or greater were also excluded (n = 6). Statistical analyses were performed using the SAS software (SAS® OnDemand for Academics: User’s Guide, 2014).
3. Results
The demographic characteristics of respondents are summarized in Table 1. A majority (81.8 %) of respondents were women, and the predominant age group was 21 to 40 years old (41.0 %), followed by those in the 41–60 age group (37.2 %). Approximately half of the participants had an annual income between $35,000 to $150,000, with 20.2 % having an income below this range, and 26.9 % earning more than $150,000. Education level was more evenly distributed among the three categories (Associate, Bachelor’s, or Advanced degree). Forty-five percent of respondents self-identified as White, with the second largest group being those who self-identified as Hispanic (25 %). Forty-one percent of the study participants were classified as normal weight based on BMI, and 54.2 % of them were in the overweight and obese categories. In terms of chronic conditions, over half of the study participants reported having at least one.
Table 1.
Demographic characteristics of study participants (N = 505).
| Characteristics | Frequency | Percent |
|---|---|---|
| Gender | ||
| Male | 75 | 14.9 |
| Female | 413 | 81.8 |
| Transgender/Non Binary | 7 | 1.4 |
| Other/Missing | 10 | 1.9 |
| Age | ||
| 18–20 years | 29 | 5.7 |
| 21–40 | 207 | 41.0 |
| 41–60 | 188 | 37.2 |
| 60+ | 81 | 16.0 |
| Annual household income (US$) | ||
| <35 K | 102 | 20.2 |
| 35 - < 150 K | 237 | 46.9 |
| ≥150 K | 136 | 26.9 |
| Missing | 30 | 5.9 |
| Educational level | ||
| Associate's or less | 180 | 35.6 |
| Bachelor's | 134 | 26.5 |
| Advanced degree | 186 | 36.8 |
| Missing | 5 | 1.0 |
| Race/ethnicity | ||
| White | 228 | 45.2 |
| Hispanic | 126 | 25.0 |
| Asian | 81 | 16.0 |
| Other | 70 | 13.9 |
| BMI category | ||
| Normal weight (18.5 to <25 kg/m2) | 206 | 40.8 |
| Overweight (25 to <30 kg/m2) | 128 | 25.3 |
| Obese (≥30 kg/m2) | 146 | 28.9 |
| Missing | 25 | 5.0 |
| Presence of Chronic Condition | ||
| None | 231 | 45.7 |
| One chronic condition | 129 | 25.5 |
| Two or more chronic conditions | 87 | 17.3 |
| Missing | 58 | 11.5 |
Abbreviations: BMI - Body Mass Index.
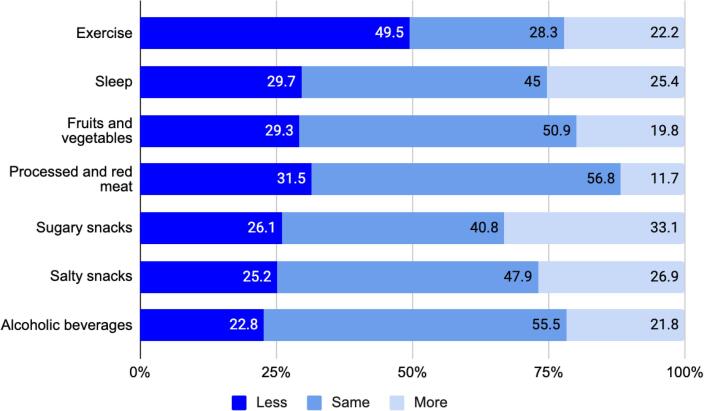
After the COVID-19 outbreak, approximately 84 % of the respondents experienced at least one unfavorable behavior change. The observed values for the health risk behavior score ranged from 0 to 6 (mean 2.02; standard deviation 1.54). A notable change was observed for exercise, with 49.5 % of participants indicating a reduction in physical activity, as compared to 22.2 % reporting an increase (Fig. 1). A larger proportion of survey respondents reported reducing their processed and red meat (31.5 %) and fruit and vegetable (29.3 %) intake, than an increase (11.7 and 19.8 % respectively). While changes were reported for the other health behaviors, the proportions of participants reporting increased and reduced amounts of sleep and consumption of sugary and salty snacks and alcohol were more evenly distributed.
Fig. 1.
The proportion of respondents in percentages indicating a reduction, no change, or increase in exercise, sleep, and specific dietary habits after the COVID-19 outbreak.
Based on the bivariate analyses performed to study the impact of the independent variables on the health risk behavior score, we excluded only the presence of chronic conditions at a p-value threshold of > 0.20 from subsequent analyses (Table 2). Gender and race/ethnicity were significantly associated with the health risk behavior score. In the multivariable analyses, gender and race/ethnicity remained significantly associated with the health risk behavior score after adjusting for all other variables in the model (Table 2). A lower score (beta = −0.815) was associated with being male, while being Hispanic was associated with higher scores (+0.396).
Table 2.
Association between health risk behavior score and sociodemographic factors among respondents.
|
Crude |
Adjusteda |
|||||||
|---|---|---|---|---|---|---|---|---|
| Parameter estimate | Lower 95 % CL | Upper 95 % CL | Pr > |t|b | Parameter estimate | Lower 95 % CL | Upper 95 % CL | Pr > |t|c | |
| Age | ||||||||
| 21–40 years old | 0.508 | −0.084 | 1.099 | 0.092 | 0.323 | −0.411 | 1.058 | 0.387 |
| 41–60 years old | 0.356 | −0.239 | 0.951 | 0.241 | 0.200 | −0.550 | 0.951 | 0.601 |
| >60 years old | −0.280 | −0.925 | 0.366 | 0.395 | −0.194 | −0.988 | 0.600 | 0.631 |
| Gender | ||||||||
| Male | −0.783 | −1.154 | −0.412 | <0.001 | −0.815 | −1.207 | −0.423 | <0.001 |
| Body mass index | ||||||||
| Overweight | 0.018 | −0.315 | 0.351 | 0.915 | −0.067 | −0.415 | 0.280 | 0.704 |
| Obese | 0.277 | −0.042 | 0.597 | 0.089 | 0.026 | −0.324 | 0.377 | 0.882 |
| Annual household income | ||||||||
| Mid income | ||||||||
| (35 to <150 K US$) | −0.102 | −0.458 | 0.255 | 0.575 | 0.007 | −0.369 | 0.382 | 0.971 |
| High income | ||||||||
| (≥150 K US$) | −0.547 | −0.941 | −0.152 | 0.007 | −0.365 | −0.823 | 0.093 | 0.118 |
| Education | ||||||||
| Bachelor’s degree | 0.057 | −0.285 | 0.400 | 0.742 | 0.036 | −0.339 | 0.410 | 0.851 |
| Advanced degree | −0.237 | −0.551 | 0.076 | 0.138 | 0.055 | −0.315 | 0.426 | 0.769 |
| Race/Ethnicity | ||||||||
| Hispanic | 0.542 | 0.210 | 0.875 | 0.001 | 0.396 | 0.032 | 0.761 | 0.033 |
| Asian | −0.007 | −0.395 | 0.381 | 0.972 | −0.057 | −0.468 | 0.355 | 0.787 |
| Other | 0.282 | −0.128 | 0.692 | 0.177 | 0.202 | −0.245 | 0.649 | 0.374 |
| Chronic conditions | ||||||||
| One condition | −0.137 | −0.457 | 0.183 | 0.401 | N/Ad | |||
| >2 conditions | 0.198 | −0.172 | 0.567 | 0.294 | ||||
Abbreviations: CL - confidence level.
Adjusted for: gender, weight status, age, income, education level and race/ethnicity.
Significance level for crude model: <0.2.
Significance level for adjusted model: <0.05.
Not significant in the bivariate model.
The impact of gender on the health risk behavior score can be explained by a higher reduction in fruit and vegetable consumption (31.2 vs 13.3 %, p = 0.006), and a higher increase in the consumption of sugary (36.1 vs 16 %, p = 0.001) and salty (28.3 vs 12 %, p = 0.008) snacks in women compared to men (Table 3). For ethnicity, the negative impact on the health risk behavior score can be attributed to a higher reduction in exercise (61.1 vs 42.1 %, p = 0.003), sleep (44.4 vs 25.4 %, p < 0.001), and fruit and vegetable consumption (42.9 vs 25 %, p = 0.001) in Hispanics compared to Whites (Table 4). Differences in the consumption of sugary and salty snacks and alcohol, although significant, were due to reductions in consumption (see “Less” category), which were not considered in the calculation of the health risk behavior score.
Table 3.
Association between gender and health risk behavior changes after the COVID-19 outbreaka.
|
Female |
Male |
Chi-square | |||||
|---|---|---|---|---|---|---|---|
| Less | Same | More | Less | Same | More | ||
| Exercise | 50.6 | 27.1 | 22.3 | 44.0 | 32.0 | 24.0 | 0.553 |
| Sleep | 31.2 | 43.3 | 25.4 | 21.3 | 54.7 | 24.0 | 0.139 |
| Fruits and vegetables | 31.2 | 48.9 | 19.9 | 13.3 | 64.0 | 22.7 | 0.006 |
| Red and processed meat | 33.2 | 55.0 | 11.9 | 22.7 | 69.3 | 8.0 | 0.069 |
| Sugary snacks | 26.6 | 37.3 | 36.1 | 24.0 | 60.0 | 16.0 | 0.001 |
| Salty snacks | 25.4 | 46.3 | 28.3 | 26.7 | 61.3 | 12.0 | 0.008 |
| Alcohol | 23.0 | 54.7 | 22.3 | 20.0 | 61.3 | 18.7 | 0.568 |
The health risk behavior score was calculated based on the values for “less” exercise, sleep, and fruit and vegetable intake, and for “more” red and processed meat, sugary and salty snacks and alcohol intake (highlighted in gray).
Table 4.
Association between race/ethnicity and health risk behavior changes after the COVID-19 outbreaka.
|
White |
Hispanic |
Chi-square | |||||
|---|---|---|---|---|---|---|---|
| Less | Same | More | Less | Same | More | ||
| Exercise | 42.1 | 33.8 | 24.1 | 61.1 | 21.4 | 17.5 | 0.003 |
| Sleep | 25.4 | 53.1 | 21.5 | 44.4 | 30.2 | 25.4 | <0.001 |
| Fruits and vegetables | 25.0 | 57.9 | 17.1 | 42.9 | 40.5 | 16.7 | 0.001 |
| Red and processed meat | 21.5 | 66.7 | 11.8 | 44.4 | 41.3 | 14.3 | <0.001 |
| Sugary snacks | 21.1 | 45.6 | 33.3 | 38.9 | 33.3 | 27.8 | 0.001 |
| Salty snacks | 20.2 | 55.7 | 24.1 | 38.1 | 37.3 | 24.6 | <0.001 |
| Alcohol | 14.9 | 62.3 | 22.8 | 36.5 | 39.7 | 23.8 | <0.001 |
The health risk behavior score was calculated based on the values for “less” exercise, sleep, and fruit and vegetable intake, and for “more” red and processed meat, sugary and salty snacks and alcohol intake (highlighted in gray).
4. Discussion
Our cross-sectional study has described important unfavorable changes in health risk behaviors in northern California in the months after the onset of the COVID-19 pandemic. Some groups appeared to be more vulnerable to unfavorable behavior changes during the pandemic, with females and Hispanics being disproportionately affected.
Consistent with our results, a reduction in physical activity was observed in all U.S. cities among the users of the wellness smartphone app Argus (Tison et al., 2020). Other studies conducted around the globe have also found similar results (Ammar et al., 2020, He et al., 2020, Meyer et al., 2020, Smith et al., 2020). The closure of indoor exercising facilities, increased stress, and fear of being in close contact with others may explain this reduction in physical activity. A study in the U.S. that investigated reasons for changes observed during the pandemic suggested that an increase in negative behaviors, such as physical activity, was largely attributed to stress, less motivation, and resource concerns (Knell et al., 2020). In contrast, Lopez-Bueno et al. found that after a two-week reduction, participants in Spain were more physically active three weeks after the onset of the pandemic, which they attributed to an increase in home-based physical activity (López-Bueno et al., 2020).
In our study, more respondents reported a reduction in consumption of fruit and vegetables and processed and red meat than an increase, suggesting that diet quality was both positively and negatively affected due to COVID-19, consistent with other studies. In France, despite both positive and negative changes in diet intake, there was an overall decrease in diet quality (Marty et al., 2021). While an increase in the diet quality of Canadian adults was observed, especially among younger individuals, participants with lower education, or with obesity (Lamarche et al., 2021). An increase in fruit and vegetable intake and a reduction in fast-food consumption were reported for adolescents living in Spain, Italy, Chile, Colombia, and Brazil, but there was also an increase in fried and sweet food intake, likely associated with boredom and stress (Ruiz-Roso et al., 2020). In California, the restaurant industry suffered major disruptions, with up to a third of the restaurants permanently closing (Yelp, 2020), and those that remained open had to deal with lower demand, limited capacity regulations, and shortages of workers (Gostin and Wiley, 2020, Yang et al., 2020), likely leading residents to consume more home-cooked meals. This, coupled with food supply chain disruptions, increased food prices, and a loss of income for many (Falk et al., 2021, Hobbs, 2020), could have resulted in lower-income residents limiting the consumption of more expensive items such as meat, fruit, and vegetables. In contrast, those not financially affected by the pandemic could have been positively impacted thanks to more free time to prepare high-quality home-made meals, but also a potential increase in the consumption of the less desirable sugary and salty snacks due to boredom and stress.
Consistent with our findings, survey results suggest that the COVID-19 pandemic has affected men and women differently around the world. Studies conducted in the U.S., United Emirates, and China, found that women were at increased risk for weight gain, sedentary lifestyle, sleep disturbance, and increased alcohol consumption during the pandemic (He et al., 2020, Ismail et al., 2020, Pollard et al., 2020, Zhang et al., 2021). Gender had an impact on the calculated unhealthy lifestyle behavior score in the United Arab Emirates, where women were more likely to decrease their physical activity and sleep, while increasing their dietary intake and their weight (Radwan et al., 2021). In contrast, a reduction in vigorous-intensity physical activity was seen only in Spanish males with chronic conditions (López-Sánchez et al., 2021), while other studies showed no impact of gender on various health risk behaviors (Cancello et al., 2020, Lamarche et al., 2021, López-Bueno et al., 2020, Robinson et al., 2020). In our study, being female resulted in a higher health risk behavior score, associated with a reduction in fruit and vegetable consumption and an increase in snack and meat intake. This increased risk is potentially associated with women’s expanded household responsibilities and unpaid care burden during the pandemic as well as holding less secure jobs (Connor et al., 2020, Power, 2020). According to the Public Policy Institute of California, the COVID-19 pandemic disproportionately affected female employment in the state (Public Policy Institute of California, 2020); this same trend was observed in the U.S., with an even greater burden for women of color (Power, 2020).
In our study, Hispanics presented more unfavorable changes in health risk behaviors as a result of the pandemic, being more likely to report reductions in physical activity, sleep, and fruit and vegetable consumption. This was also seen in a large survey of U.S. adults that indicated that Hispanics were 2.3 times more likely to reduce their physical activity when compared to Non-Hispanic Whites (Chen et al., 2021). For diet-related changes, an increase in sugar-sweetened beverages and fast food consumption, but not snacks and desserts, has been observed in Hispanics compared to non-Hispanic whites (Chen et al., 2021, Park et al., 2022). For sleep patterns, previous studies have described increase, decrease, or no change in the duration of sleep as a result of COVID (Cancello et al., 2020, Giuntella et al., 2021, Ismail et al., 2020, Robinson et al., 2021). According to a survey with a nationally representative sample of the U.S., average sleep duration did not change after the pandemic, with no clear patterns between races (Hisler and Twenge, 2021). Unfavorable behavioral changes observed among Hispanics in our study may be explained by the hardships affecting this population group. Although Latino workers in California represent 38 % of the workforce, they accounted for 50 % of the job losses seen between February and September of 2020. This group is overrepresented in close-contact industries which were hit the hardest, and among workers with lower education levels, which account for the vast majority of the job losses in the state (Alamos, 2020).
We acknowledge the existence of several limitations in our study. Firstly, our data are self-reported and were collected during the course of a four-month period (August to November of 2020), during which the effects of living under the COVID-19 pandemic could have changed for individual participants. Secondly, participants were asked to compare current habits with those of at least five months earlier, which is prone to recall bias and inaccuracies. Thirdly, our sample is prone to selection bias as respondents were recruited through social media platforms and newspaper ads. While the income distribution reflects that of the Bay Area, this is not a representative sample. For example, there was an overrepresentation of women among study participants, as well as those with advanced degrees. In addition, the calculated Health risk behavior score does not take into account beneficial behavior changes. Nonetheless, the present study assessed a comprehensive set of health behaviors risks and had a good representation of Hispanics, low-income households, and young adults. As such, its results could be valuable to policymakers in the region to identify ways to support those most affected by the pandemic.
Our data suggest that most participants were negatively impacted by the pandemic, reporting at least one unfavorable health behavior change. The groups most vulnerable were women and Hispanics, who were more likely to increase their health risk behaviors, mostly due to a worsening in diet quality, as well as reductions in physical activity and sleep. These results suggest that programs targeted to these more at-risk population groups could have a larger impact to mitigate the effects of this ongoing pandemic. In addition, policies to support at risk groups are needed to address disparities related to healthy food access, childcare, and economic opportunities. Nevertheless, future prospective studies should be conducted to better understand the mid-term and long-term impacts of the pandemic on at-risk populations to assess if these changes persist over time.
Funding financial disclosure
This work was supported by the Circle of Friends Molly and Gene Rauen Endowed Research Assistance Award.
Ethical statement
The study was approved by the Institutional Review Board of San Jose State University and all participants provided informed consent (IRB Protocol Tracking Number: 20162).
CRediT authorship contribution statement
Adriana Telias: Conceptualization, Methodology, Investigation, Writing – original draft, Writing – review & editing. Marcelle M. Dougan: Conceptualization, Methodology, Formal analysis, Writing – review & editing. Giselle A.P. Pignotti: Conceptualization, Methodology, Writing – review & editing, Supervision, Project administration.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Contributor Information
Adriana Telias, Email: adriana.telias@sjsu.edu.
Marcelle M. Dougan, Email: marcelle.dougan@sjsu.edu.
Giselle A.P. Pignotti, Email: giselle.pignotti@sjsu.edu.
Data availability
The data that has been used is confidential.
References
- Alamos C. Legislative Analyst’s Office; 2020. COVID-19 and the labor market: which workers have been hardest hit by the pandemic?https://lao.ca.gov/LAOEconTax/article/Detail/531 [Google Scholar]
- Ammar A., Brach M., Trabelsi K., Chtourou H., Boukhris O., Masmoudi L., Bouaziz B., Bentlage E., How D., Ahmed M., Müller P., Müller N., Aloui A., Hammouda O., Paineiras-Domingos L., Braakman-Jansen A., Wrede C., Bastoni S., Pernambuco C., Mataruna L., Taheri M., Irandoust K., Khacharem A., Bragazzi N., Chamari K., Glenn J., Bott N., Gargouri F., Chaari L., Batatia H., Ali G., Abdelkarim O., Jarraya M., El Abed K., Souissi N., Van Gemert-Pijnen L., Riemann B., Riemann L., Moalla W., Gómez-Raja J., Epstein M., Sanderman R., Schulz S., Jerg A., Al-Horani R., Mansi T., Jmail M., Barbosa F., Ferreira-Santos F., Šimunič B., Pišot R., Gaggioli A., Bailey S., Steinacker J., Driss T., Hoekelmann A. Effects of COVID-19 home confinement on eating behaviour and physical activity: results of the ECLB-COVID19 International Online Survey. Nutrients. 2020;12(6):1583. doi: 10.3390/nu12061583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cancello R., Soranna D., Zambra G., Zambon A., Invitti C. Determinants of the Lifestyle Changes during COVID-19 Pandemic in the Residents of Northern Italy. Int. J. Environ. Res. Public Health. 2020;17(17) doi: 10.3390/ijerph17176287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen L., Li J., Xia T., Matthews T.A., Tseng T.-S., Shi L., Zhang D., Chen Z., Han X., Li Y., Li H., Wen M., Su D. Changes of exercise, screen time, fast food consumption, alcohol, and cigarette smoking during the COVID-19 Pandemic among Adults in the United States. Nutrients. 2021;13(10) doi: 10.3390/nu13103359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen A.Y., Sturm R. Diet quality in the United States improved during the great recession and deteriorated during economic recovery. J. Acad. Nutrit. Dietetics. 2021 doi: 10.1016/j.jand.2021.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connor J., Madhavan S., Mokashi M., Amanuel H., Johnson N.R., Pace L.E., Bartz D. Health risks and outcomes that disproportionately affect women during the Covid-19 pandemic: A review. Soc. Sci. Med. 2020;266 doi: 10.1016/j.socscimed.2020.113364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cummings J.R., Ackerman J.M., Wolfson J.A., Gearhardt A.N. COVID-19 stress and eating and drinking behaviors in the United States during the early stages of the pandemic. Appetite. 2021;162 doi: 10.1016/j.appet.2021.105163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Du Y., Liu B., Sun Y., Snetselaar L.G., Wallace R.B., Bao W. Trends in Adherence to the Physical Activity Guidelines for Americans for Aerobic Activity and Time Spent on Sedentary Behavior Among US Adults, 2007 to 2016. JAMA Network Open. 2019;2(7):e197597. doi: 10.1001/jamanetworkopen.2019.7597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Falk, G., Romero, P. D., Nicchitta, I. A., & Nyhof, E. C. (2021). Unemployment rates during the COVID-19 pandemic: Vol. Version 21 (No. R46554). Congressional Research Service. https://crsreports.congress.gov/product/pdf/R/R46554/21.
- Fowler, J. H., Hill, S. J., Levin, R., & Obradovich, N. (2021). Stay-at-home orders associate with subsequent decreases in COVID-19 cases and fatalities in the United States. PloS One, 16(6), e0248849. 10.1371/journal.pone.0248849. [DOI] [PMC free article] [PubMed]
- Gallè F., Sabella E.A., Da Molin G., De Giglio O., Caggiano G., Di Onofrio V., Ferracuti S., Montagna M.T., Liguori G., Orsi G.B., Napoli C. Understanding knowledge and behaviors related to CoViD-19 epidemic in Italian Undergraduate Students: The EPICO Study. Int. J. Environ. Res. Public Health. 2020;17(10) doi: 10.3390/ijerph17103481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallè F., Sabella E.A., Roma P., Ferracuti S., Da Molin G., Diella G., Montagna M.T., Orsi G.B., Liguori G., Napoli C. Knowledge and lifestyle behaviors related to COVID-19 pandemic in people over 65 years old from Southern Italy. Int. J. Environ. Res. Public Health. 2021;18(20):10872. doi: 10.3390/ijerph182010872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giuntella O., Hyde K., Saccardo S., Sadoff S. Lifestyle and mental health disruptions during COVID-19. Proc. Natl. Acad. Sci. U.S.A. 2021;118(9) doi: 10.1073/pnas.2016632118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gostin L.O., Wiley L.F. Governmental public health powers during the COVID-19 pandemic: stay-at-home orders, business closures, and travel restrictions. JAMA: J. Am. Med. Assoc. 2020;323(21):2137–2138. doi: 10.1001/jama.2020.5460. [DOI] [PubMed] [Google Scholar]
- He M., Xian Y., Lv X., He J., Ren Y. Changes in body weight, physical activity, and lifestyle during the semi-lockdown period after the outbreak of COVID-19 in China: an online survey. Disaster Med. Public Health Preparedness. 2020;1–6 doi: 10.1017/dmp.2020.237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hisler G.C., Twenge J.M. Sleep characteristics of U.S. adults before and during the COVID-19 pandemic. Soc. Sci. Med. 2021;276 doi: 10.1016/j.socscimed.2021.113849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hobbs J.E. Food supply chains during the COVID-19 pandemic. Canad. J. Agric. Econ. 2020;68(2):171–176. doi: 10.1111/cjag.12237. [DOI] [Google Scholar]
- Ingram J., Maciejewski G., Hand C.J. Changes in diet, sleep, and physical activity are associated with differences in negative mood during COVID-19 lockdown. Front. Psychol. 2020;11 doi: 10.3389/fpsyg.2020.588604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ismail L.C., Osaili T.M., Mohamad M.N., Marzouqi A.A., Jarrar A.H., Jamous D.O.A., Magriplis E., Ali H.I., Sabbah H.A., Hasan H., AlMarzooqi L.M.R., Stojanovska L., Hashim M., Obaid R.R.S., Saleh S.T., Dhaheri A.S.A. Eating habits and lifestyle during COVID-19 lockdown in the United Arab Emirates: a cross-sectional study. Nutrients. 2020;12(11) doi: 10.3390/nu12113314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilian C., Rehm J., Allebeck P., Braddick F., Gual A., Barták M., Bloomfield K., Gil A., Neufeld M., O'Donnell A., Petruželka B., Rogalewicz V., Schulte B., Manthey J. Alcohol consumption during the COVID-19 pandemic in Europe: a large-scale cross-sectional study in 21 countries. Addiction. 2021;116(12):3369–3380. doi: 10.1111/add.15530. [DOI] [PubMed] [Google Scholar]
- Kim E.J., Marrast L., Conigliaro J. COVID-19: magnifying the effect of health disparities. J. Gen. Intern. Med. 2020;35(8):2441–2442. doi: 10.1007/s11606-020-05881-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knell G., Robertson M.C., Dooley E.E., Burford K., Mendez K.S. Health behavior changes during COVID-19 pandemic and subsequent “stay-at-home” orders. Int. J. Environ. Res. Public Health. 2020;17(17) doi: 10.3390/ijerph17176268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kocevska D., Blanken T.F., Van Someren E.J.W., Rösler L. Sleep quality during the COVID-19 pandemic: not one size fits all. Sleep Med. 2020;76:86–88. doi: 10.1016/j.sleep.2020.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamarche B., Brassard D., Lapointe A., Laramée C., Kearney M., Côté M., Bélanger-Gravel A., Desroches S., Lemieux S., Plante C. Changes in diet quality and food security among adults during the COVID-19-related early lockdown: results from NutriQuébec. Am. J. Clin. Nutrition. 2021;113(4):984–992. doi: 10.1093/ajcn/nqaa363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez L., 3rd, Hart L.H., 3rd, Katz M.H. Racial and ethnic health disparities related to COVID-19. JAMA: J. Am. Med. Assoc. 2021;325(8):719–720. doi: 10.1001/jama.2020.26443. [DOI] [PubMed] [Google Scholar]
- López-Bueno R., Calatayud J., Casaña J., Casajús J.A., Smith L., Tully M.A., Andersen L.L., López-Sánchez G.F. COVID-19 confinement and health risk behaviors in Spain. Front. Psychol. 2020;11 doi: 10.3389/fpsyg.2020.01426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- López-Sánchez G.F., López-Bueno R., Gil-Salmerón A., Zauder R., Skalska M., Jastrzębska J., Jastrzębski Z., Schuch F.B., Grabovac I., Tully M.A., Smith L. Comparison of physical activity levels in Spanish adults with chronic conditions before and during COVID-19 quarantine. Eur. J. Pub. Health. 2021;31(1):161–166. doi: 10.1093/eurpub/ckaa159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madan J., Blonquist T., Rao E., Marwaha A., Mehra J., Bharti R., Sharma N., Samaddar R., Pandey S., Mah E., Shete V., Chu Y., Chen O. Effect of COVID-19 pandemic-induced dietary and lifestyle changes and their associations with perceived health status and self-reported body weight changes in India: a cross-sectional survey. Nutrients. 2021;13(11) doi: 10.3390/nu13113682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marty L., de Lauzon-Guillain B., Labesse M., Nicklaus S. Food choice motives and the nutritional quality of diet during the COVID-19 lockdown in France. Appetite. 2021;157 doi: 10.1016/j.appet.2020.105005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer J., McDowell C., Lansing J., Brower C., Smith L., Tully M., Herring M. Changes in physical activity and sedentary behavior in response to COVID-19 and their associations with mental health in 3052 US Adults. Int. J. Environ. Res. Public Health. 2020;17(18):1–13. doi: 10.3390/ijerph17186469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niles, M. T., Neff, R., Biehl, E., Bertmann, F., Belarmino, E. H., Acciai, F., & Ohri-Vachaspati, P. (2020). Food Access and Food Security During COVID-19 Survey- Version 2.1. https://search.datacite.org/works/10.7910/dvn/4ky9xz.
- Office of Disease Prevention and Health Promotion. (2021). Determinants of health. HealthyPeople. https://www.healthypeople.gov/2020/about/foundation-health-measures/Determinants-of-Health.
- Park S., Lee S.H., Yaroch A.L., Blanck H.M. Reported changes in eating habits related to less healthy foods and beverages during the COVID-19 pandemic among US Adults. Nutrients. 2022;14(3):526. doi: 10.3390/nu14030526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollard M.S., Tucker J.S., Green H.D., Jr. Changes in adult alcohol use and consequences during the COVID-19 pandemic in the US. JAMA Network Open. 2020;3(9):e2022942. doi: 10.1001/jamanetworkopen.2020.22942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Power K. The COVID-19 pandemic has increased the care burden of women and families. Sustainability: Sci. Practice Policy. 2020;16(1):67–73. doi: 10.1080/15487733.2020.1776561. [DOI] [Google Scholar]
- Public Policy Institute of California. (2020). Gender Gaps in the COVID-19 Labor Market. https://www.ppic.org/blog/gender-gaps-in-the-covid-19-labor-market/.
- Radwan H., Kitbi M.A., Hasan H., Hilali M.A., Abbas N., Hamadeh R., Saif E.R., Naja F. Indirect health effects of COVID-19: unhealthy lifestyle behaviors during the lockdown in the United Arab Emirates. Int. J. Environ. Res. Public Health. 2021;18(4) doi: 10.3390/ijerph18041964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robillard R., Dion K., Pennestri M.-H., Solomonova E., Lee E., Saad M., Murkar A., Godbout R., Edwards J.D., Quilty L., Daros A.R., Bhatla R., Kendzerska T. Profiles of sleep changes during the COVID-19 pandemic: demographic, behavioural and psychological factors. J. Sleep Res. 2021;30(1):e13231. doi: 10.1111/jsr.13231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson E., Gillespie S., Jones A. Weight-related lifestyle behaviours and the COVID-19 crisis: An online survey study of UK adults during social lockdown. Obes. Sci. Pract. 2020;6(6):735–740. doi: 10.1002/osp4.442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson E., Boyland E., Chisholm A., Harrold J., Maloney N.G., Marty L., Mead B.R., Noonan R., Hardman C.A. Obesity, eating behavior and physical activity during COVID-19 lockdown: A study of UK adults. Appetite. 2021;156 doi: 10.1016/j.appet.2020.104853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruiz-Roso, M. B., de Carvalho Padilha, P., Mantilla-Escalante, D. C., Ulloa, N., Brun, P., Acevedo-Correa, D., Peres, W. A. F., Martorell, M., Aires, M. T., de Oliveira Cardoso, L., Carrasco-Marín, F., Paternina-Sierra, K., Rodriguez-Meza, J. E., Montero, P. M., Bernabè, G., Pauletto, A., Taci, X., Visioli, F., Dávalos, A. (2020). Covid-19 confinement and changes of adolescent’s dietary trends in Italy, Spain, Chile, Colombia and Brazil. Nutrients, 12(6). 10.3390/nu12061807. [DOI] [PMC free article] [PubMed]
- Sheehan C.M., Frochen S.E., Walsemann K.M., Ailshire J.A. Are U.S. adults reporting less sleep?: findings from sleep duration trends in the National Health Interview Survey, 2004–2017. Sleep. 2019;42(2) doi: 10.1093/sleep/zsy221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singu S., Acharya A., Challagundla K., Byrareddy S.N. Impact of social determinants of health on the emerging COVID-19 Pandemic in the United States. Front. Public Health. 2020;8:406. doi: 10.3389/fpubh.2020.00406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith L., Jacob L., Butler L., Schuch F., Barnett Y., Grabovac I., Veronese N., Caperchione C., Lopez-Sanchez G.F., Meyer J., Abufaraj M., Yakkundi A., Armstrong N., Tully M.A. Prevalence and correlates of physical activity in a sample of UK adults observing social distancing during the COVID-19 pandemic. BMJ Open Sport Exercise Med. 2020;6(1):e000850. doi: 10.1136/bmjsem-2020-000850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sparks J.R., Kebbe M., Flanagan E.W., Beyl R.A., Altazan A.D., Yang S., Redman L.M. Impact of COVID-19 Stay-at-home orders on health behaviors and anxiety in black and White Americans. J. Racial Ethnic Health Disparities. 2021 doi: 10.1007/s40615-021-01131-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- State of California. (2020). Executive Order N-33-20. https://www.gov.ca.gov/wp-content/uploads/2020/03/3.19.20-attested-EO-N-33-20-COVID-19-HEALTH-ORDER.pdf.
- Tison G.H., Avram R., Kuhar P., Abreau S., Marcus G.M., Pletcher M.J., Olgin J.E. Worldwide effect of COVID-19 on physical activity: a descriptive study. Ann. Intern. Med. 2020;173(9):767–770. doi: 10.7326/M20-2665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U S Bureau of Labor Statistics. (2021). Local area unemployment statistics. https://data.bls.gov/timeseries/LASST060000000000003?amp%253bdata_tool=XGtable&output_view=data&include_graphs=true.
- Yang Y., Liu H., Chen X. COVID-19 and restaurant demand: early effects of the pandemic and stay-at-home orders. Int. J. Contemp. Hospitality Manage. 2020;32(12):3809–3834. doi: 10.1108/IJCHM-06-2020-0504. [DOI] [Google Scholar]
- Yelp. (2020). Yelp: Local Economic Impact Report (Vol. 2021, Issue /10/14/16:02:06). https://www.yelpeconomicaverage.com/business-closures-update-sep-2020.
- Zhang X., Oluyomi A., Woodard L., Raza S.A., Adel Fahmideh M., El-Mubasher O., Byun J., Han Y., Amos C.I., Badr H. Individual-level determinants of lifestyle behavioral changes during COVID-19 lockdown in the United States: results of an online survey. Int. J. Environ. Res. Public Health. 2021;18(8) doi: 10.3390/ijerph18084364. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that has been used is confidential.