Abstract
Background
Total hip arthroplasty (THA) for hip disorders helps to alleviate pain and improve active daily life. When determining the effects of medical therapy and the subsequent clinical results, patient quality of life (QOL) also needs to be assessed. Recently, patient-reported outcomes (PRO) have become important as evaluation criteria. This study aimed to evaluate patient QOL and various PRO between different types of cementless stems and to clarify the relationship between PRO and stem-cortical bone contact.
Methods
The study comprised 138 consecutive patients undergoing cementless THA for hip osteoarthritis. We assessed three different types of PRO: the Japanese Orthopaedic Association Hip-Disease Evaluation Questionnaire (JHEQ), patient's joint perception, and peri-hip articular joint pain (PHAP). We measured the state of contact between femur and implant by density mapping.
Results
No significant difference was noted in PRO between stem types based on the JHEQ and patient's joint perception. PHAP occurred more frequently in the patients with a taper wedge stem versus a fit-and-fill stem. In both groups, distal contact was associated with PHAP but not with JHEQ results and patient's joint perception.
Conclusion
The difference in PHAP between the two stem types groups was significant, with postoperative PHAP being higher with the taper wedge stem because of the more distal contact between the taper wedge stem and femur cortical bone.
Keywords: Total hip arthroplasty, Cementless stem, Patient-reported outcomes, Thigh pain, Density mapping
Abbreviations: THA, total hip arthroplasty; QOL, quality of life; PRO, patient-reported outcomes; JHEQ, Japanese Orthopaedic Association Hip-Disease Evaluation Questionnaire; PHAP, peri-hip articular joint pain; CT, computed tomography; JOA, Japanese Orthopaedic Association; HU, Hounsfield unit
1. Introduction
Total hip arthroplasty (THA) for hip disorders helps to alleviate pain and improve patients’ active daily life. THA has made it possible to obtain stable results in both the early postoperative period and the long-term postoperative period. Cementless stems have achieved excellent long-term clinical outcomes1 with many cementless stems reported to have favorable long-term outcomes.2, 3, 4, 5, 6 Kusano et al. showed good results for the fit-and-fill stem, which achieved a 97% survival rate over an average follow-up period of 10.2 years.7 Peitgen et al. also showed good results with the taper wedge stem over a 26- to 32-year follow-up period.8
When determining the effects of medical therapy and the subsequent clinical results, patient quality of life (QOL) also needs to be assessed. Recently, patient-reported outcomes (PRO) have become important as evaluation criteria.9 Various measures of PRO have been developed, such as the Oxford hip score,10 WOMAC,11,12 and the Japanese Orthopaedic Association Hip-Disease Evaluation Questionnaire (JHEQ),13 which assess pain, function, and mental status of patients; joint perception,14 which focuses on the patient's joint awareness; and thigh pain,15 which assesses pain in a specific area. Further, a previous retrospective study showed the initial contact state of a cementless stem to be associated with postoperative peri-hip articular pain (PHAP) including thigh pain. The postoperative state can be reproduced from preoperative computed tomography (CT) data, and the contact between implant and femur can be measured by density mapping using ZedHip (LEXI Co., Ltd., Tokyo, Japan).16 Differences in stem-cortical bone contact due to different stem designs may also affect QOL and PRO in cementless THA.
It is necessary to critically examine what factors related to surgery, including the implants themselves, contribute to QOL. As there are many kinds of cementless stems on the market, this is one of the modifiable factors that deserves special attention. To our knowledge, there are no reports on QOL and PRO when using different type of stems.
Thus, this study evaluated patient QOL and types of PRO between different types of cementless stems and clarified the relationship between PRO and stem-cortical bone contact.
2. Materials and methods
Informed consent for participation in and publication of this study was provided by all study patients. The local ethics committee approved this study, which comprised 138 consecutive patients receiving cementless THA for hip osteoarthritis between January 2014 and March 2018. Exclusion criteria included previous femoral osteotomy (hip), THA with femoral shortening osteotomy (hip), fractures, systemic bone disease (hip), and patient inaccessibility. The flow of the study is illustrated in Fig. 1.
Fig. 1.
Flowchart of patients across the study. PRO, patient-reported outcomes; THA, total hip arthroplasty.
2.1. Surgical procedures
All surgery was conducted via a standard posterior approach by the senior surgeon or junior surgeons as supervised by the senior surgeon. There was no difference between the surgical and preoperative conditions among the surgeons (Supplemental Table 1). All patients received a cementless cup (Trident® hemispherical acetabular shell; Stryker, NJ, USA) on the acetabular side, with a ceramic-on-cross-linked polyethylene (BIOLOX delta® ceramic femoral head, X3® polyethylene liner; Stryker) used as the bearing surface. The patients receiving the fit-and-fill stem (Super Secur-Fit HA® stem and Secur-Fit advanced® stem; Stryker) comprised the group F, and the patients receiving a taper wedge stem (Accolade II® stem; Stryker) comprised group T. We used the Super Secur-Fit HA stem from January 2014 to December 2015, Accolade II stem from January 2016 to December 2017, and Secur-Fit advanced stem from January 2017 to December 2018. We provided all patients with information on posture guidance to prevent dislocation. All patients began full weight bearing on postoperative day 1.
2.2. Outcome measures
2.2.1. Clinical evaluation
The Japanese Orthopaedic Association (JOA) score was used for clinical scoring,17 with scores of 40 points for pain and 20 points each for range of motion, walking ability, and activities of daily living, thus combining objective evaluation with PRO. A normal hip scores 100 points. JOA scores were determined before surgery and at final follow-up.
2.2.2. Patient-reported outcomes
We assessed three different types of PRO: the JHEQ, patient's joint perception, and PHAP. These results were obtained by sending a questionnaire to the THA patients in August 2020.
2.2.3. JHEQ
The JOA established the JHEQ as a new PRO by the JOA in 2012. The JHEQ has been used in many studies for clinical evaluation of patients with hip disease18, 19, 20, 21 and is also validates the validity of its use.22 It has the feature of being able to measure both mental health and satisfaction. It includes pain, movement, and mental subscales, each scored at 28 points. Better outcome is indicated by a higher score.13 The JHEQ can assess the right and left hip joint separately and focuses on activities of daily life according to the Asian lifestyle. Determination of laterality for analysis was according to the following criteria: criterion 1, use the side having problems with the hip joint; criterion 2, if problems in the hip joint are bilateral, use the score on the side with greater pain; criterion 3, if laterality cannot be determined with criterion 1 or 2, use the side with lower scores for each item. The JHEQ satisfaction scale is measured by dissatisfaction = 100 and satisfaction = 0, similar to the VAS pain scale.
2.2.4. Patient's joint perception
Patient's joint perception was evaluated with a question asked after surgery to determine whether the patient considers the operated joint to be ‘‘natural’’ or ‘‘artificial’’ and if the joint is associated with a feeling of functional restriction.14 The single question for this PRO can have 5 answers, with the best result being “like a native or natural joint” and the worst result being “a non-functional joint”.
2.2.5. Peri-hip articular pain
Thigh pain has been defined as anterior and/or lateral thigh pain.15,23,24 We modified and used the questionnaire of Gielis et al. for a more accurate diagnosis.25 To assess the degree of pain in the same way as before, patients with pain were asked to specifically assess their pain on a 0 to 10 visual analog scale (VAS), with no pain = 0 and greatest pain experienced in their life = 10.15,23 If the patient feels pain in the back of the thigh or buttocks or radial pain in the lower leg, the condition of the patient's lumbar spine is carefully checked to exclude it from the diagnosis. We have defined PHAP as that which meets both the previous definition of thigh pain and that defined by Gielis et al.
2.2.6. Radiographic evaluation
Radiographic images were obtained before and after surgery on the frontal hip, centering on the pubis symphysis at a height of 1.1 m in the supine position. The canal flare index26 was measured to illustrate femoral morphology before surgery. Stem alignment was assessed by determining angular deviation of the central tip of the stem from the true anatomic axis of the femur. For assessment of coronal alignment, the neutral group comprised patients measured between a valgus of 3 and varus of 3 in terms of the anatomic axis (i.e., 0 ± 3), and the outlier group comprised those with measurements outside the range of these values.27 Radiographs were obtained at the latest follow-up for screening of 2 mm or more of subsidence,28 stress shielding,29 and cortical hypertrophy.30 Mean values of three repetitions of imaging measurements taken by the surgeon were used. Two surgeons checked the reliability of the imaging measurements by evaluating them on 20 randomly extracted hips. If a mismatch in measurements occurred, the images were reexamined.
2.2.7. Density mapping
To enable measurement of contact between the implant and femur according to Gruen zones by density mapping as previously described, we adjusted preoperative CT data to show insertion angle of the postoperative implant (Fig. 2A). Briefly, we used ZedHip (LEXI Co., Ltd.) to superimposed computer-aided design models of femoral stems on postoperative multiplanar reconstruction CT images obtained 2 weeks after surgery.16 When postoperative CT data is used, implant insertion causes metal halation that makes accurate measurement of the contact state difficult. Density mapping indicates contact state by color according to Hounsfield unit (HU) values that are calculated from the CT data. The contact region is shown by three colors: yellow for cortical bone contact; red for dense cancellous bone contact; and green for sparse cancellous bone contact. Results are displayed as percentages in relation to Gruen zone and total stem area. The effective contact region was defined as the area of contact between implant and cortical bone (as shown in yellow). A density threshold of 543 HU for the cortico-cancellous interface was used as was described previously.31 The density mapping function is useful to quantify contact between implant and femur, and previous studies reported its use to clearly confirm cementless stem fit-and-fill parameters.32,33 We included cases of contact between stem and cortical bone in the distal part of the stem (zone 3 or 5) in the Distal Contact (DC) group (Fig. 2B). Other cases were included in the Normal Contact (NC) group (Fig. 2C). We investigated the differences in PRO results between these two groups.
Fig. 2.
(A) Measuring the contact state of the stem and femoral cortical bone by density mapping using ZedHip. Effective contact region: yellow area in which the implant is in contact with the cortical bone. (B) Distal Contact (DC) group: Contact is present between stem and cortical bone of the femur in the distal part of the stem (zones 3, 5) as well as in the proximal part. (C) Normal Contact (NC) group: Contact between stem and cortical bone of the femur in the distal part of the stem is not similar to that in the proximal part.
3. Results
Patient demographic data are listed in Table 1. Sex, body mass index, preoperative JOA score, age at surgery, and follow-up period were not statistically different between the patients in group F and group T.
Table 1.
Patient demographics.
| Number, n | Group F |
Group T |
P value |
|---|---|---|---|
| 90 | 48 | ||
| Sex, M/F, n | 21/69 | 11/37 | 1 |
| BMI, kg/m2 (±SD) | 22.5 ± 8.3 | 23.9 ± 4.0 | 0.834 |
| Age, years (±SD) | 64.7 ± 10.0 | 64.1 ± 10.81 | 0.727 |
| Follow-up period, months (range) | 39.0 (21.0–80.0) | 50.5 (24.00–66.0) | 0.21 |
| Pre-operation JOA score, points (±SD) | 54.6 ± 16.7 | 56.7 ± 14.8 | 0.532 |
| Pre-operation JHEQ | |||
| Pain (±SD) | 6.6 ± 5.7 | 7.8 ± 6.7 | 0.232 |
| Movement (±SD) | 7.6 ± 6.3 | 7.2 ± 5.9 | 0.862 |
| Mental (±SD) | 8.3 ± 5.7 | 8.1 ± 6.2 | 0.580 |
| Total (±SD) | 20.6 ± 12.7 | 19.8 ± 11.4 | 0.424 |
| Satisfaction scale (±SD) | 80.0 ± 19.5 | 81.3 ± 19.8 | 0.322 |
BMI, body mass index; JHEQ, Japanese Orthopaedic Association hip disease evaluation questionnaire; JOA, Japanese Orthopaedics Association SD, standard deviation.
3.1. Patient-reported outcomes
Pain, movement, mental and total JHEQ scores and JHEQ satisfaction scale were not statistically different between group F and group T (Table 2). Regarding patient's joint perception, 46 patients (51.1%) in group F and 23 (47.8%) in group T felt that they had a natural joint (Table 2). The prevalence of PHAP in group F was significantly lower compared with that in group T (Group F vs Group T: 11 [12.2%] vs 13 [27.1%]). The PHAP VAS was not statistically different between the two groups (Table 2).
Table 2.
Patient-reported outcomes for each stem group.
| Group F | Group T | P value | |
|---|---|---|---|
| JHEQ | |||
| Pain (±SD) | 24.8 ± 4.9 | 22.8 ± 5.8 | 0.056 |
| Movement (±SD) | 13.8 ± 7.7 | 14.2 ± 8.4 | 0.768 |
| Mental (±SD) | 20.5 ± 7.1 | 18.7 ± 7.8 | 0.154 |
| Total (±SD) | 59.1 ± 16.7 | 55.7 ± 19.1 | 0.253 |
| Satisfaction scale (±SD) | 14.1 ± 15.6 | 16.7 ± 14.8 | 0.437 |
| Patient's joint perception | 2.21 ± 0.95 | 2.09 ± 0.91 | 0.462 |
| Natural joint (<2), n (%) | 46 (51.1%) | 23 (47.9%) | 0.858 |
| Peri-hip articular pain | |||
| Number, n (%) | 11 (12.2%) | 13 (27.1%) | 0.035* |
| VAS (±SD) | 4.94 ± 2.94 | 3.80 ± 2.24 | 0.226 |
JHEQ, Japanese Orthopaedic Association hip disease evaluation questionnaire; SD, standard deviation; VAS, Visual Analog Scale.
*P<0.05.
3.2. Radiographic evaluation
Results of radiographic evaluation were not statistically different between group F and group T in terms of femoral shape, stress shielding, cortical hypertrophy, spot welds, and subsidence of 2 mm and above (Table 3).
Table 3.
Radiographic evaluation.
| Group F | Group T | P value | |
|---|---|---|---|
| Canal flare index | 4.09 ± 0.80 | 3.85 ± 0.58 | 0.075 |
| Stem alignment | |||
| Neutral, n, (%) | 88 (97.8%) | 44 (91.7%) | 0.183 |
| Outlier, n, (%) | 2 (2.2%) | 4 (8.3%) | |
| Stress shielding | 0.521 | ||
| Grade 1, n, (%) | 34 (37.8%) | 13 (27.1%) | |
| Grade 2, n, (%) | 43 (47.8%) | 25 (52.1%) | |
| Grade 3, n, (%) | 2 (2.2%) | 1 (2.1%) | |
| Cortical hypertrophy | 11 (12.2%) | 10 (21.3%) | 0.212 |
| Zone 2, n | 4 | 2 | |
| Zone 3, n | 5 | 9 | |
| Zone 4, n | 1 | 3 | |
| Spot welds | 36 (40.0%) | 15 (31.2%) | 0.357 |
| Zone 2, n | 17 | 6 | |
| Zone 6, n | 29 | 10 | |
| Subsidence (≥2 mm), n | 0 | 0 | 1 |
3.3. Density mapping
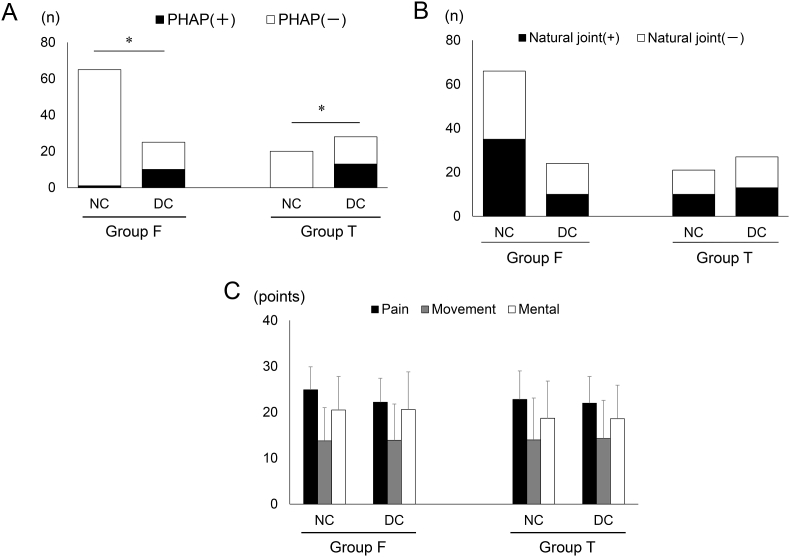
In group F, 65 patients (72.2%) comprised the NC group and 25 patients (27.8%) comprised the DC group and in group T, 20 patients (37.6%) comprised the NC group and 28 patients (62.4%) comprised the DC group (p < 0.001). In both groups, the appearance of PHAP was associated with distal contact between stem and cortical bone of the femur (p < 0.001) (Fig. 3A). However, there was no association between joint perception and JHEQ results and contact between stem and cortical bone of the femur (Fig. 3B and C).
Fig. 3.
Contact area between stem and cortical bone by density mapping for PRO of each stem group. (A) PHAP (B) Joint perception (C) JHEQ. p*>0.001. JHEQ, Japanese Orthopaedic Association hip disease evaluation questionnaire; PHAP, peri-hip articular pain; PRO, patient-reported outcomes.
4. Discussion
The present study showed that when comparing PRO such as JHEQ, patient's joint perception, and PHAP between a fit-and-fill stem and taper wedge stem, the differences between the two stem types in JHEQ and patient's joint perception were not significant. However, the frequency of PHAP was higher in the patients implanted with a taper wedge stem rather than a fit-and-fill stem. In both groups, distal contact was associated with PHAP but not with JHEQ results and patient's joint perception.
JHEQ and joint perception did not differ between the cementless stems. A previous study on the relationship between PRO and cementless stem selection showed that only head diameter affects activity levels.34 Cementless stems have achieved excellent results regardless of their design, and there is no significant difference between them in general PRO.
The present study showed the incidence of postoperative PHAP to be higher with the taper wedge stem than with the fit-and-fill stem. Correlation between thigh pain and the contact state of the stem was shown in one previous study,35 and another study used density mapping to evaluate the correlation between these two factors.16 The etiology of thigh pain was categorized in previous reports based on the mechanisms of micromotion of the stem tip at the interface between the bone and the prosthesis36,37 and excessive transfer of stress to the tip of the stem.38,39 Contact between stem and bone cortex of patients with PHAP in the present study was more distal in both stem groups.
The fit-and-fill stem has a low degree of freedom of installation when inserting the stem due to the concept of obtaining strong initial fixation by occupying the medullary cavity.40 The taper wedge stem features a thin, flat body to maintain bone stock in the proximal femur. Low stem occupancy in the medullary cavity allows for adjustable alignment during stem placement.41 Stem malalignment was found to be associated with its instability in cementless stems.42 The risk of stem malalignment with the taper wedge stem has been pointed out, and stem subsidence and instability have been reported.43,44 Several studies have found no statistically significant difference in clinical findings between varus and neutral alignment of the femoral component when using a taper wedge stem.45,46 We also found no significant difference in stem alignment in the outlier group, but the difference tended to be greater in the taper wedge group. As shown by density mapping, the taper wedge stem was in contact with the bone cortex more distally than was the fit-and-fill stem. Distal stem cortical contact was associated with the appearance of PHAP, which may have influenced the difference in appearance between the two groups with PHAP.
This study has limitations. First, this was a retrospective study with no randomization, but despite our rigorous approach, potential bias may exist. Second, the definition of PHAP was ambiguous. We made efforts to accurately diagnose PHAP, but the diagnosis may be inaccurate because it is a questionnaire-based result. Third, the choice of stem was determined by the timing of the surgery, but it may be biased because we sometimes chose to use other stems. Fourth, the timing of sending the questionnaire varied from patient to patient, which might have affected the study results.
5. Conclusion
The difference in PHAP between the fit-and-fill stem group and taper wedge stem group was significant, with postoperative PHAP occurring more frequently with the taper wedge stem versus fit-and-fill stem. This was due to the more distal contact of the taper wedge stem with cortical bone of the femur.
Ethics approval
Authors are responsible for correctness of the statements provided in the manuscript. See also Authorship Principles. The Editor-in-Chief reserves the right to reject submissions that do not meet the guidelines described in this section.
Consent to participate
All patients provided informed consent to participate in this study.
Consent for publish
All participants provided informed consent for the publication of this study.
Availability of data and materials
Not applicable.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Contributions
Daisaku Kato designed the study, conducted statistical analyses, and drafted the manuscript. All authors contributed to data interpretation, manuscript preparation, and manuscript review; all approved the version for publication; and all agree to be accountable for all aspects of the work.
Declaration of competing interest
All authors declare that they have no conflict of interest or competing interest.
Acknowledgments
We gratefully acknowledge the work of past and present members of our department.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jor.2022.10.014.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Khanuja H.S., Vakil J.J., Goddard M.S., Mont M.A. Cementless femoral fixation in total hip arthroplasty. J Bone Joint Surg Am. 2011;93:500–509. doi: 10.2106/JBJS.J.00774. [DOI] [PubMed] [Google Scholar]
- 2.Bliss J.M., Law P.L., Patil S.S., Colwell C.W., Jr. Hydroxyapatite-coated femoral stem/porous- coated acetabulum survivorship at 15 years. J Arthroplasty. 2011;26:972e5. doi: 10.1016/j.arth.2010.09.009. [DOI] [PubMed] [Google Scholar]
- 3.Nakashima Y., Sato T., Yamamoto T., et al. Results at a minimum of 10 years of follow-up for AMS and PerFix HA-coated cementless total hip arthroplasty: impact of cross-linked polyethylene on implant longevity. J Orthop Sci. 2013;18:962e8. doi: 10.1007/s00776-013-0456-4. [DOI] [PubMed] [Google Scholar]
- 4.Takenaga R.K., Callaghan J.J., Bedard N.A., Liu S.S., Klaassen A.L., Pedersen D.R. Cementless total hip arthroplasty in patients. J Bone Joint Surg Am. 2012;94:2153e9. doi: 10.2106/JBJS.L.00011. [DOI] [PubMed] [Google Scholar]
- 5.Sandiford N.A., Butler-Manuel A., Apthorp H.D., East D.J., Hinves B.L., Shepperd J.A. Primary total hip arthroplasty with a proximally HA-coated titanium femoral component: results at 10-15-year follow-up. Eur J Orthop Surg Traumatol. 2014;24:1211e5. doi: 10.1007/s00590-013-1405-9. [DOI] [PubMed] [Google Scholar]
- 6.Meding J.B., Keating E.M., Ritter M.A., Faris P.M., Berend M.E. Minimum ten-year follow-up of a straight-stemmed, plasma-sprayed, titanium-alloy, uncemented femoral component in primary total hip arthroplasty. J Bone Joint Surg Am. 2004;86eA:92e7. doi: 10.2106/00004623-200401000-00014. [DOI] [PubMed] [Google Scholar]
- 7.Kusano T., Seki T., Higuchi Y., Takegami Y., Osawa Y., Ishiguro N. Preoperative canal bone ratio is related to high-degree stress shielding: a minimum 5-year follow-up study of a proximally hydroxyapatite-coated straight tapered titanium femoral component. J Arthroplasty. 2018;33:1764–1769. doi: 10.1016/j.arth.2017.12.019. [DOI] [PubMed] [Google Scholar]
- 8.Peitgen D.S., Innmann M.M., Merle C., Gotterbarm T., Moradi B., Streit M.R. Cumulative long-term incidence of postoperative periprosthetic femoral fractures using an uncemented tapered titanium hip stem: 26- to 32-year result. J Arthroplasty. 2019;34:77e81. doi: 10.1016/j.arth.2018.08. [DOI] [PubMed] [Google Scholar]
- 9.Siljander M.P., McQuivey K.S., Fahs A.M., Galasso L.A., Serdahely K.J., Karadsheh M.S. Current trends in patient-reported outcome measures in total joint arthroplasty: a study of 4 major orthopaedic journals. J Arthroplasty. 2018;33:3416–3421. doi: 10.1016/j.arth.2018.06.034. [DOI] [PubMed] [Google Scholar]
- 10.Murray D.W., Fitzpatrick R., Rogers K., et al. The use of the Oxford hip and knee scores. J Bone Joint Surg. 2007;89:1010–1014. doi: 10.1302/0301-620X.89B8.19424. [DOI] [PubMed] [Google Scholar]
- 11.Bellamy N., Buchannan W.W., Goldsmith C.H., Campbell J., Stitt L. Validation study of the WOMAC: a health status instrument of measuring clinically-important patient-relevant outcomes following total hip or knee arthroplasty in osteoarthritis. J Rheumatol. 1988;1:95–108. [PubMed] [Google Scholar]
- 12.McHorney C.A., Ware J.E., Jr., Lu F.H., Sherbourne C.D. The MOS 36-item short-form health survey (SF-36). III: tests of data quality, scaling assumptions, and reliability across diverse patient groups. Med Care. 2011;32:40–66. doi: 10.1097/00005650-199401000-00004. [DOI] [PubMed] [Google Scholar]
- 13.Matsumoto T., Kaneuji A., Hiejima Y., et al. Japanese orthopaedic association hip disease evaluation questionnaire (JHEQ): a patient-based evaluation tool for hip-joint disease. The subcommittee on hip disease evaluation of the clinical outcome committee of the Japanese orthopaedic association. J Orthop Sci. 2012;17:25–38. doi: 10.1007/s00776-011-0166-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Collins M., Lavigne M., Girard J., Vendittoli P.A. Joint perception after hip or knee replacement surgery. Orthop Traumatol Surg Res. 2012;98:275–280. doi: 10.1016/j.otsr.2011.08.021. [DOI] [PubMed] [Google Scholar]
- 15.Barrack L.B., Paprosky W., Butler R.A., Palafox A., Szuszczewicz E., Myers L. Patients' perception of pain after total hip arthroplasty. J Arthroplasty. 2000;15(5):590–596. doi: 10.1054/arth.2000.6634. [DOI] [PubMed] [Google Scholar]
- 16.Yoshitani J., Kabata T., Kajino Y., et al. The use of density mapping in the analysis of thigh pain after total hip arthroplasty in patients with well-fixed tapered wedge stems. J Orthop Surg. 2020;28(2) doi: 10.1177/2309499020930306. [DOI] [PubMed] [Google Scholar]
- 17.Kuribayashi M., Takahashi K.A., Fujioka M., Ueshima K., Inoue S., Kubo T. Reliability and validity of the Japanese orthopaedic association hip score. J Orthop Sci. 2010;15(4):452–458. doi: 10.1007/s00776-010-1490-0. [DOI] [PubMed] [Google Scholar]
- 18.Osawa Y., Hasegawa Y., Seki T., Takegami Y., Amano T., Ishiguro N. Patient-reported outcomes in patients who undergo total hip arthroplasty after periacetabular osteotomy. J Orthop Sci. 2018;23(2):346–349. doi: 10.1016/j.jos.2017.11.001. [DOI] [PubMed] [Google Scholar]
- 19.Osawa Y., Seki T., Takegami Y., Kusano T., Makida K., Ishiguro N. Cementless total hip arthroplasty for osteonecrosis and osteoarthritis produce similar results at ten years follow-up when matched for age and gender. Int Orthop. 2018;42(7):1683–1688. doi: 10.1007/s00264-018-3987-7. [DOI] [PubMed] [Google Scholar]
- 20.Takegami Y., Seki T., Higuchi Y., Osawa Y., Ishiguro N. Measurement of equivalence between the web and paper versions of the Japanese orthopaedic association hip disease evaluation questionnaire. Mod Rheumatol. 2020;30(2):397–401. doi: 10.1080/14397595.2019.1592799. [DOI] [PubMed] [Google Scholar]
- 21.Takemoto G., Osawa Y., Seki T., et al. Factors influencing inconsistent leg length discrepancy in dysplastic hip osteoarthritis: a retrospective study. BMC Muscoskel Disord. 2022;23(1):381. doi: 10.1186/s12891-022-05348-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Seki T., Ishiguro N., Hasegawa Y., Ikeuchi K., Hiejima Y. Reliability and validity of the Japanese Orthopaedic Association hip disease evaluation questionnaire (JHEQ) for patients with hip disease. J Orthop Sci. 2013;18(5):782–787. doi: 10.1007/s00776-013-0436-8. [DOI] [PubMed] [Google Scholar]
- 23.Butler R.A., Rosenzweig S., Myers L., Barrack R.L. The Frank Stinchfield Award: the impact of socioeconomic factors on outcome after THA: a prospective, randomized study. Clin Orthop Relat Res. 2011;469(2):339–347. doi: 10.1007/s11999-010-1519-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nam D., Nunley R.M., Sauber T.J., Johnson S.R., Brooks P.J., Barrack R.L. Incidence and location of pain in young, active patients following hip arthroplasty. J Arthroplasty. 2015;30(11):1971–1975. doi: 10.1016/j.arth.2015.05.030. [DOI] [PubMed] [Google Scholar]
- 25.Gielis W.P., van Oldenrijk J., Ten Cate N., Scholtes V.A.B., Geerdink C.H., Poolman R.W. Increased persistent mid-thigh pain after short-stem compared with wedge-shaped straight-stem uncemented total hip arthroplasty at medium-term follow-up: a randomized double-blinded cross-sectional study. J Arthroplasty. 2019;34(5):912–919. doi: 10.1016/j.arth.2019.01.014. [DOI] [PubMed] [Google Scholar]
- 26.Noble C., Alexander W. The anatomic basis of femoral component design. Clin Orthop Relat Res. 1988;235:148e65. [PubMed] [Google Scholar]
- 27.Reina N., Salib C.G., Perry K.I., Hanssen A.D., Berry D.J., Abdel M.P. Mild coronal stem malalignment does not negatively impact survivorship or clinical results in uncemented primary total hip arthroplasties with dual-tapered implants. J Arthroplasty. 2019;34(6):1127–1131. doi: 10.1016/j.arth.2019.01.055. [DOI] [PubMed] [Google Scholar]
- 28.Loudon J.R., Charnley J. Subsidence of the femoral prosthesis in total hip replacement in relation to the design of the stem. J Bone Joint Surg Br. 1980;62eB:450e3. doi: 10.1302/0301-620X.62B4.7430222. [DOI] [PubMed] [Google Scholar]
- 29.Engh C.A., Bobyn J.D., Glassman A.H. Porous-coated hip replacement: the factors governing bone ingrowth, stress shielding and clinical results. J Bone Joint Surg Br. 1987;69:45e55. doi: 10.1302/0301-620X.69B1.3818732. [DOI] [PubMed] [Google Scholar]
- 30.Ritter M.A., Fechtman R.W. Distal cortical hypertrophy following total hip arthroplasty. J Arthroplasty. 1988;3:117e21. doi: 10.1016/s0883-5403(88)80076-7. [DOI] [PubMed] [Google Scholar]
- 31.Inoue D., Kabata T., Maeda T., et al. Usefullness of three-dimensional templating software to quantify the contact state between implant and femur in total hip arthroplasty. Eur J Orthop Surg Traumatol. 2015;25:1293–1300. doi: 10.1007/s00590-015-1705-3. [DOI] [PubMed] [Google Scholar]
- 32.Inoue D., Kabata T., Maeda T., et al. The correlation between clinical radiological outcome and contact state of implant and femur using three-dimensional templating software in cementless total hip arthroplasty. Eur J Orthop Surg Traumatol. 2016;26:591–598. doi: 10.1007/s00590-016-1796-5. [DOI] [PubMed] [Google Scholar]
- 33.Wada H., Mishima H., Sugaya H., Nishio T., Yamazaki M. Three-dimensional analysis of the contact pattern between the cortical bone and femoral prosthesis after cementless total hip arthroplasty. Adv Orthop. 2016;2016 doi: 10.1155/2016/8052380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Campbell A., Emara A.K., Klika A., Piuzzi N.S. Does implant selection affect patient-reported outcome measures after primary total hip arthroplasty? J Bone Joint Surg Am. 2021;103(24):2306–2317. doi: 10.2106/JBJS.20.01931. [DOI] [PubMed] [Google Scholar]
- 35.Hayashi S., Hashimoto S., Matsumoto T., Takayama K., Niikura T., Kuroda R. Risk factors of thigh pain following total hip arthroplasty with short, tapered-wedge stem. Int Orthop. 2020;44(12):2553–2558. doi: 10.1007/s00264-020-04762-z. [DOI] [PubMed] [Google Scholar]
- 36.Engh C.A., Bobyn J.D., Glassman A.H. Porous-coated hip replacement. The factors governing bone ingrowth, stress shielding, and clinical results. J Bone Joint Surg Br. 1987;69:45–55. doi: 10.1302/0301-620X.69B1.3818732. [DOI] [PubMed] [Google Scholar]
- 37.Engh C.A., Sr., Culpepper W.J., 2nd Femoral fixation in primary total hip arthroplasty. Orthopedics. 1997;20(9):771–773. doi: 10.3928/0147-7447-19970901-09. [DOI] [PubMed] [Google Scholar]
- 38.Lavernia C., Apuzzo M.D., Hernandez V., Lee D. Thigh pain in primary total hip arthroplasty the effects of elastic moduli. J Arthroplasty. 2004;19(7 Suppl 2):10–16. doi: 10.1016/j.arth.2004.06.023. [DOI] [PubMed] [Google Scholar]
- 39.Namba R.S., Keyak J.H., Kim A.S., Vu L.P., Skinner H.B. Cementless implant composition and femoral stress. A finite element analysis. Clin Orthop Relat Res. 1998;347:261–267. [PubMed] [Google Scholar]
- 40.Geesink R.G., Hoefnagels N.H. Six-year results of hydroxyapatite-coated total hip replacement. J Bone Joint Surg Br. 1995;77(4):534–547. [PubMed] [Google Scholar]
- 41.Casper D.S., Kim G.K., Restrepo C., Parvizi J., Rothman R.H. Primary total hip arthroplasty with an uncemented femoral component five- to nine-year results. J Arthroplasty. 2011;26(6):838–841. doi: 10.1016/j.arth.2011.02.010. [DOI] [PubMed] [Google Scholar]
- 42.Vresilovic E.J., Hozack W.J., Rothman R.H. Radiographic assessment of cementless femoral components. Correlation with intraoperative mechanical stability. J Arthroplasty. 1994;9(2):137–141. doi: 10.1016/0883-5403(94)90062-0. [DOI] [PubMed] [Google Scholar]
- 43.Cooper H.J., Jacob A.P., Rodriguez J.A. Distal fixation of proximally coated tapered stems may predispose to a failure of osteointegration. J Arthroplasty. 2011;26(6 Suppl):78–83. doi: 10.1016/j.arth.2011.04.003. [DOI] [PubMed] [Google Scholar]
- 44.White C.A., Carsen S., Rasuli K., Feibel R.J., Kim P.R., Beaule P.E. High incidence of migration with poor initial fixation of the Accolade stem. Clin Orthop Relat Res. 2012;470(2):410–417. doi: 10.1007/s11999-011-2160-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mollan R.A., Watters P.H., Steele R., McClelland C.J. Failure of the femoral component in the Howse total hip arthroplasty. Clin Orthop Relat Res. 1984;190:142–147. [PubMed] [Google Scholar]
- 46.Min B.W., Song K.S., Bae K.C., Cho C.H., Kang C.H., Kim S.Y. The effect of stem alignment on results of total hip arthroplasty with a cementless tapered-wedge femoral component. J Arthroplasty. 2008;23(3):418–423. doi: 10.1016/j.arth.2007.04.002. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Not applicable.